Abstract
Purpose
The purpose of this review is to describe the role of altered joint biomechanics in reverse shoulder arthroplasty and to propose a rehabilitation protocol for a cuff-deficient glenohumeral joint based on the current evidence.
Methods and Materials: The proposed rehabilitation incorporates the principles of pertinent muscle loading while considering risk factors and surgical complications.
Results
In light of altered function of shoulder muscles in reverse arthroplasty, scapular plane abduction should be more often utilized as it better activates deltoid, teres minor, upper trapezius, and serratus anterior. Given the absence of supraspinatus and infraspinatus and reduction of external rotation moment arm of the deltoid in reverse arthroplasty, significant recovery of external rotation may not occur, although an intact teres minor may assist external rotation in the elevated position.
Conclusion
Improving the efficiency of deltoid function before and after reverse shoulder arthroplasty is a key factor in the rehabilitation of the cuff deficient shoulders. Performing exercises in scapular plane and higher abduction angles activates deltoid and other important muscles more efficiently and optimizes surgical outcomes.
Keywords: biomechanics, complications, cuff tear arthropathy, deltoid, rehabilitation
Introduction
The first shoulder replacement was performed for tuberculous arthritis by a French orthopedic surgeon, Jules E. Pean in 1893.1 The implant consisted of a platinum tube, a rubber ball coated with paraffin, and two metal loops that attached the ball to the scapula and the tube. The first generation of reverse total shoulder arthroplasty (RTSA) was introduced by German and French Surgeons in early 1970s but was discontinued quickly because of loosening, mechanical complications and inability to counter the superiorly directed force of the deltoid muscle in the absence of rotator cuff.2 A more efficient version of the RTSA was introduced by Paul Grammont, a French orthopedic surgeon2–4 in late 1970s. Grammont understood the importance of the balance between the supraspinatus-deltoid couple force and the role of the prosthesis’s centre of rotation (COR) in the cuff-deficient joint. Grammont felt that by medializing the COR of the glenohumeral joint and increasing the deltoid lever arm one could compensate for the lack of activity of the rotator cuff muscles, as cited by Baulot who worked closely with him.2 Grammont’s first modern prototype was manufactured in 1985 and was composed of an alumina ceramic sphered glenoid component with a medialized COR and a concave polyethylene cone cemented on the humeral site.2 The use of RTSA was approved in the United States by the Food and Drug Administration (FDA) in November 2003 and over the past two decades its indications which were initially limited to cuff tear arthropathy (CTA) have increased to include massive irreparable rotator cuff tears in the absence of osteoarthritis, proximal humerus fractures, glenohumeral osteoarthritis with excessive posterior glenoid erosion and revisions for failed anatomical arthroplasty.5–11
The literature on rehabilitation of the RTSA has been growing.12–18 Present guidelines are mostly based on the expert opinions and do not always address the influence of relevant muscle loading, altered joint biomechanics or unique complications of the RTSA.
The indications for RTSA have been increasing,19–24 but the post-surgical rehabilitation of cuff-deficient shoulders remains more challenging than those with a functioning rotator cuff.25 Therefore, further review of history, complications and muscle function will add to the body of knowledge in this area. The purpose of this article is to propose a rehabilitation protocol for a cuff-deficient glenohumeral joint following a RTSA by incorporating the principles of pertinent muscle loading and joint biomechanics while considering the potential for post-operative complications.
Impact of Altered Biomechanics on Muscle Recruitment
In the rotator cuff-deficient glenohumeral joint, the humeral head is migrated superiorly with respect to the glenoid fossa due to lack of compressive forces of rotator cuff muscles.26–28 Traditional anatomic total shoulder arthroplasty is not a viable option for a rotator cuff deficient shoulder due to accelerated glenoid loosening caused by eccentric joint loading, excessive shearing forces and superior tipping of the glenoid component, a phenomenon referred to as the “rocking horse glenoid.”29 To reduce the risk of glenoid failure in a cuff-deficient shoulder, the semi-constrained design of modern RTSA prosthesis is comprised of a glenoid hemisphere with no neck and a humeral cup with a non-anatomical valgus angle. By distalizing the humeral component in relation to acromion, the deltoid muscle fibers are tensioned and recruited to elevate the arm while compensating for the deficiency of the cuff muscles.8,30–33
Complications Following RTSA
Despite advantages of the RTSA, the reverse ball and socket model is associated with specific complications such as dislocation, scapular notching, acromion stress fracture and nerve palsy.8,34–38
Dislocation
The majority of post-operative dislocations after RTSA are anterior (Figure 1) and generally present within the first 5–12 weeks postoperatively. The most common risk factors for early dislocations are inadequate soft tissue tensioning, BMI >30, male gender, previous shoulder surgery and subscapularis deficiency.39–41 Late dislocations are mostly attributed to asymmetric wear of the polyethylene, male gender, rapid weight loss leading to excessive soft tissue with resultant lengthening or infection.37,42,43
Figure 1.
A, AP view of the right shoulder RTSA with humeral component displaced anteroinferiorly in a 53 year old woman. B, Transcapular view of the same patient showing anteroinferior dislocation of the humeral component.
In addition to the above risk factors, due to the unique semi constrained design of the RTSA, certain movements such as hyperextension, reaching across chest/abdomen or combined movements such as reaching behind back (adduction, internal rotation, extension) could increase the risk of anterior dislocation in the reverse model.44
Scapular Notching
Scapular notching is a radiographic abnormality that refers to an erosive lesion of the inferior scapular neck secondary to impingement of the humeral implant during adduction,45 combined movements of flexion/extension and internal/external rotation with the arm at the side46 or chronic foreign-body reaction in the joint capsule (Figure 2).47 Scapular notching is specific to RTSA and appears to be more prevalent in the non-dominant extremity and in patients with low body weight.48 Patients with a physically demanding life style are also more susceptible to this pathology.49 The non-demographic risk factors for scapular notching are decreased pre-operative acromiohumeral distance, increased fatty infiltration of the infraspinatus, diagnosis, and type of glenoid erosion.49 Levigne and colleagues reported that cuff tear arthropathy was associated with 71% scapular notching as compared with 47% in those with osteoarthritis and cuff deficiency. In their study, patients with superior glenoid erosion had an incidence of 83%, where inferior glenoid erosion was associated with 25% scapular notching.49 Scapular notching may lead to glenoid implant loosening,45,49 humeral radiolucent lines48 and deterioration of patient-oriented scores and functional outcomes.45,48,49 Role of comorbidities such as Parkinson disease in RTSA is worth nothing. The limited research in this area reports reduction of pain but inferior clinical function and a much higher complication rates such as glenoid notching in these patients.50,51
Figure 2.
A, AP view of the prosthesis showing an erosive lesion at the inferior scapular neck in a 91-year female at 2 and ½ years post reverse arthroplasty. B, Axillary view of the same shoulder showing a linear lucency anteriorly along the component-cement interface at 2 and ½ years post reverse arthroplasty.
Scapular Stress Fractures
Increasing the deltoid moment arm is associated with improving the superior stability of the implant in RTSA. However, the longer arm length and greater deltoid tension increases the force on the origin of the deltoid muscle putting significant stress on the acromion (via middle deltoid) or the lower lip of the spine of the scapula (via posterior deltoid).52,53 Thus, stress fractures after RTSA can occur at various locations from the acromion to the scapular spine (Figure 3). The prevalence of stress fractures has been reported to vary from 0.6% to 15.8% according to a recent systematic review with a fairly similar rate of 50% for the acromial and scapular spine fractures.54 Factors associated with postoperative acromial stress fractures include osteoporosis, steroid use, prosthesis design, surgical approach and technical factors such as excessive lateralisation and humeral lengthening.53,55,56 The scapular spine stress fractures are less studied and are reported to be related to the cuff status, osteoporosis, glenoid wear, baseplate screw orientation, and implant design56,57 but the definite role of risk factors in their development remains unclear.57 Post-operative acromial and spinal stress fractures have a significant negative impact on pain and function with increased risk for revision surgery.55–61
Figure 3.
A, No obvious signs of stress fracture on plain radiographs in a 74 year-old male at 3 and ½ months post reverse arthroplasty. B, 1.2 mm helical CT scan images taken two weeks later showing healing fracture of the base of the acromion without significant displacement. C, Healing fracture of the base of the acromion now obvious on plain radiographs, taken two weeks after the CT scan and 4 weeks after the initial plain radiographs.
Neurological Deficits
The non-anatomic design of RTSA can lead to brachial plexus or axillary nerve injury (neuropraxia) mostly due to lengthening of the involved arm and elongation of the brachial plexus.62Van Hoof et al.63 reported a strain of up to 15.3% and 19.3% for the lateral and the medial root of the median nerve related to reverse shoulder prosthesis. Intraoperative factors such as arm manipulation, excessive traction or lengthening of the arm have been noted to contribute to nerve injury following RTSA.64 Fortunately, majority of neurological complaints are transient and show a full recovery over time.62
Role of Pertinent Muscles in RTSA Rehabilitation
The non-anatomical design of RTSA alters the function of certain muscles which has implications for rehabilitation. Thus, to justify more specific strengthening exercises, we provide a short review of the anatomy and function of important muscles in the native shoulder and RTSA.
Deltoid
In the native shoulder, the anterior deltoid has the largest abduction moment arm in flexion.65 The anterior deltoid also works with the subscapularis to internally rotate the humerus.66In RTSA, the anterior deltoid maintains its role in forward flexion and abduction.67 Ackland at al.68 reported that the anterior deltoid was involved in flexion but was a prominent contributor to abduction. According to Walker et al.,69 regardless of the type of implant used, anterior deltoid had the highest activation in abduction.
The middle deltoid is the main abductor with the supraspinatus initiating abduction.70In higher positions of elevation, the deltoid acts synergistically with the functioning rotator muscles (teres minor and infraspinatus if present). In this position, the deltoid has no upward component and participates more effectively in articular coaptation71 and flexion in the native shoulder.65 In RTSA, the middle deltoid is the most prominent shoulder abductor and in association with anterior deltoid and subscapularis produces a comprehensive force in the scapular plane.68 In the study by Li et al., the middle deltoid maintained its role more efficiently in abduction and to some degree in external rotation.67 Walker et al., recommended to strengthen the anterior and middle deltoid to synergize recruitment of the middle deltoid and trapezius at higher levels of elevation in cuff-deficient shoulders.69
The posterior deltoid is involved in extension and has a large external rotation moment arm, particularly during early abduction and flexion.72 The altered biomechanics of the RTSA increases the deltoid moment arm and recruitment of posterior deltoid as an abductor, but this comes at the expense of reduced axial rotation causing decreased external rotation commonly observed following RTSA.73 This phenomenon is more appreciable in patients with a tear or fatty infiltration of the infraspinatus as the infraspinatus and teres minor are the only muscles with appreciable moment arms for external rotation torque generation.73,74 While strengthening of the posterior deltoid may slightly improve external rotation,67a significant postoperative recovery of external rotation is generally not expected in patients with CTA unless infraspinatus and terse minor are intact.69 EMG studies have shown that even mild pre-operative fatty degeneration of teres minor can have a negative impact on gaining active external rotation. Patients with high grade fatty infiltration of teres minor might even experience a loss in external rotation after RTSA.75 The combination of latissimus dorsi transfer with RTSA has been reported to restore external rotation in patients with CTA and teres minor dysfunction.76
The importance of a healthy deltoid on active elevation and to a lesser degree on external rotation should not be underestimated in RTSA. Li et al showed a significant correlation between anterior and middle deltoid and postoperative flexion and abduction and between the posterior deltoid and external rotation.67 Greiner at al. established a relationship between pre-operative degeneration of the deltoid and shoulder weakness following RTSA.77 Yoon et al indicated that the pre-operative deltoid muscle volume significantly affected the post-operative functional outcome in patients with cuff tear arthropathy or irreparable cuff tears.78 The negative effect of fatty infiltration of the deltoid and infraspinatus has further been emphasized on post-operative subjective outcome scores and range of motion.79 Therefore, improving the efficiency of deltoid function both prior to and after surgery is a key factor in the rehabilitation of patients with cuff deficient shoulders.18,31,32,68,73,80
Subscapularis Muscle
In the native shoulder, the subscapularis muscle functions predominantly as an internal rotator of the humeral head and is affected by the level of abduction of the shoulder joint.81 The lower subscapularis has been noted as a humeral head depressor and anterior stabilizer.82
The RTSA can be done through two approaches, the standard deltopectoral or the superolateral. The superolateral approach maintains the integrity of the subscapularis tendon and preserves the deltoid muscle which consequently minimizes postoperative immobilization and facilitates rehabilitation by allowing a more rapid active shoulder range of motion, without increasing the incidence of shoulder dislocation. Overall, the role of subscapularis muscle remains controversial in RTSA. While some studies support the subscapularis role in the prevention of prosthetic instability,38,41,83–85 others have stated that repair of the subscapularis does not affect the functional outcome after reverse total shoulder arthroplasty,84,86 particularly in a more lateralized design, raising concern over the potential impact on implant longevity due to its antagonistic effect on deltoid and external rotation.87 A recent systematic review has concluded that subscapularis repair after RTSA produces no clinically meaningful benefits, particularly using lateralized prosthetic designs.88Generally, should surgery include the release and repair of the subscapularis tendon from its insertion on the lesser tuberosity, the rehabilitation protocol should provide protection of the healing tendon.89,90For this reason, early passive external rotation that overstretches a healing tendon and active and resisted internal rotation exercises that strain the tendon should be limited.
Scapular Stabilizers
The main stabilizers of scapula are the trapezius, serratus anterior, rhomboids, and levator scapula muscles and each play an important role in facilitating the optimal function of the shoulder. The upper fibers of the trapezius muscle are active during elevation of the native shoulder.91In arthroplasty patients, the higher pre-operative EMG activity of upper trapezius and deltoid was correlated with a better recovery of abduction, flexion and external rotation.67The authors proposed to rehabilitate the upper trapezius muscle in the middle range of abduction to help the middle deltoid muscle more efficiently.67
The serratus anterior muscle contributes to the upward rotation of the scapula during arm elevation and is maximally activated at shoulder flexion above 90°.92–94 The greatest activation for upper trapezius, serratus anterior and anterior and middle deltoid is reported to occur with external rotation at 90 of abduction.95
The rhomboids assist with scapular retraction. In normal shoulders, full retraction is essential in overhead activities and pulling motions.96,97Limitation in retraction can lead to increased stress on the anterior structures of the shoulder97 and cause anterior instability.98 Although, there is no specific study of rhomboid function in shoulder arthroplasty, strengthening of this muscle group would likely help with improving anterior stability.
The levator scapulae helps to elevate the scapula and tilt the glenoid cavity inferiorly by rotating the scapula downward. Research has shown that specific exercises to target this muscle are not necessary because strengthening of rotator cuff and other scapulothoracic musculature is an effective way of eliciting activity of the levator scapulae in TSA.99 The significance of altered biomechanics of the reverse glenohumeral joint on serratus anterior, rhomboids, and levator scapula has not been studied.
Proposed Rehabilitation Following RTSA
In light of unique complications in RTSA and the altered role of muscles in a reverse arthroplasty, the rehabilitation should focus on strengthening of the relevant muscles while considering the potential post-surgical complications. At present, there are no guidelines with respect to consequences of exercise for scapular notching or stress fractures. Performing exercises in the scapular plane abduction with neutral humeral rotation helps to maintain optimal bony congruity between the humeral head and glenoid fossa as well as the optimal length-tension relationship of the scapulohumeral musculature.100,101 The rotator cuff muscles are more effective abductors in neutral and the deltoid is a more effective abductor at higher abduction angles.102 Therefore in CTA, where supraspinatus and infraspinatus are typically absent or dysfunctional, the abduction strengthening will be more beneficial with slight elevation in a more functional scapular plane. In addition, patient’s age, sex, BMI, comorbidity, bone stock and life-style/activity level have an impact on complication rate37,52,53,56,60 and need to be taken into consideration while prescribing an individualized management.
Phase I: Early Post-op (Day 1–6 Weeks)
Precautions
The prohibited movements that remain in the precaution list for Phase I are internal rotation, adduction and extension either in isolation or combined. The activities that should be limited are tucking in a shirt, reaching behind back, reaching across the abdomen and chest, and moving the arm backwards. Lifting greater than 0.5 kg (weight of a coffee cup) and supporting the body weight using the surgical arm should be limited during this period. To avoid straining the structures beyond their integrity, some protocols have proposed lifelong precautions for lifting of more than 15 lbs,15,18 however, the exact amount of this limitation is not clear at this time.
During phase I which is usually about 4–6 weeks, the shoulder is immobilized in an abduction sling. The hand/wrist/elbow exercises and passive or active assisted range of motion of the shoulder are encouraged to avoid stiffness. During phase I, gentle pendulum exercises, periscapular exercises, passive or active assisted flexion limited to 90° (in lying position) are performed. Active assisted exercises will continue with the goal of increasing flexion to 120° by the 16th week. Patients with good body mechanics may add flexion against a wall while using a towel or a ball to activate the serratus anterior muscle by pressing against the ball during the elevation.
Phase II (6–12 Weeks)
Precautions
The clinicians should continue to enforce precautions for dislocation, particularly in active males and those with a high BMI. Despite lack of guidelines with respect to consequences of exercise for scapular notching, extensive painful adduction exercises are not recommended especially in medialized implants.16,45 The combined internal rotation, adduction and extension should be avoided for another 6 weeks. Performing repeated active flexion/extension and internal/external rotation at 0° of abduction could cause scapular notching and impingement that can lead to polyethylene debris and osteolytic reaction and have to be limited as well.46 Of interest, the glenoid impingement does not appear to occur for the internal/external rotation at 90° of abduction.46 Lack of glenoid impingement at higher abduction angles, may be an option for younger workers who have to perform repeated rotations as a part of their occupation (e.g. store clerk at the checkout line).
In terms of scapular stress fractures, too much stress applied through deltoid strengthening exercises, particularly in osteoporotic patients (e.g. disuse or steroid use)52,53,56,60 or in those with a low BMI37 is to be avoided during this phase of rehabilitation. Any sudden new symptoms associated with a declined active range of motion, localized tenderness, and pain on resisted deltoid activation may indicate a stress acromial or scapular spine fracture which should be followed up with CT scan52,53,60 to assess the amount of displacement of the acromion or spine of the scapula. In these cases, active and isometric exercises should be halted for 6–8 weeks or until union is confirmed on re-imaging. An abduction sling to decrease the deltoid tension is helpful in pain management and potentially reducing further displacement of the fracture.
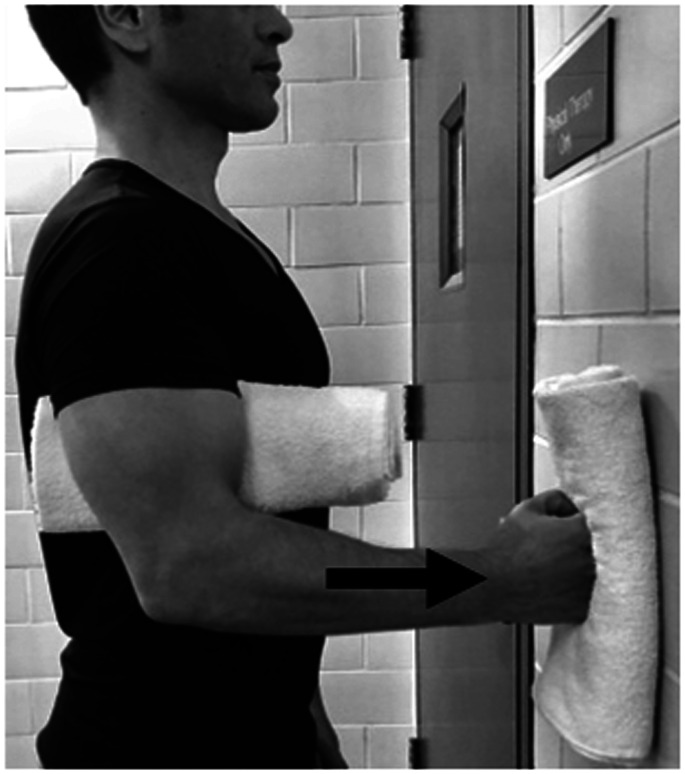
Active range of motion exercises and painfree submaximal isometrics in neutral position are initiated at this point. Isometric flexion and extension in neutral are the most basic exercises to activate anterior and post deltoid. Shoulder hyperextension while performing posterior deltoid strengthening should be avoided to minimize the risk of dislocation (Figures 4 and 5).
Figure 4.
Anterior deltoid, pectoralis major and coracobrachialis. Isometric flexionin neutral position.
Figure 5.
Posterior deltoid and latissimus dorsi. Isometric extension in neutral position. Hyperextension to be avoided at all times.
The face-clock exercise will help to strengthen the scapular stabilizers (Figure 6). In a cuff-deficient shoulder, the scapular plane abduction activates different components of the deltoid as suggested by the literature.68,69,71 Isometric strengthening could therefore be facilitated by elevating the arm to about 30° of the scapular plane while resting on a table and isolating the anterior deltoid (Figure 7: diagonal flexion and abduction) from middle deltoid (Figure 8: predominantly abduction) and posterior deltoid (Figure 9: abduction/extension and Figure 10: abduction/external rotation).Excessive abduction of the arm during elevation is common in cuff deficient joints and is to be avoided by pulling the elbows inward while performing external rotation (Figure 10C).
Figure 6.
Scapular exercises (upper, middle and lower trapezius muscles, levator scapulae, rhomboids, latissimus dorsi and serrates anterior). • Face-clock exercises are done in standing, facing the wall with the hand pointed straight up and at any height that is comfortable. • Without moving hand during the exercise, the scapula is moved towards the numbers on the clock, starting with 12:00, 3:00, 6:00 and back over to 9:00. This will isolate the scapular stabilizers.
Figure 7.
Anterior and middle deltoid. Isometric diagonal flexion and abduction in scapular plane.
Figure 8.
Middle deltoid. Isometric abduction in scapular plane to activate middle deltoid.
Figure 9.
Posterior deltoid. Isometric diagonal extension and abduction in scapular plane to activate posterior deltoid. A strap is held by the opposite hand to provide resistance.
Figure 10.
Posterior deltoid and teres minor. Isometric abduction and external rotation in the scapular plane. A, Initial position: affected arm is kept at 30° of scapular plane abduction and the forearm is pressed against the opposite hand outward. B, Progression: affected arm is externally rotated while resisting against the opposite hand and keeping the elbow inward. C, The hornblower sign, commonly seen in patients with CTA should be avoided by focusing on external rotation and moving the elbow inward.
In patients with a repaired subscapularis, submaximal isometric internal rotation may be started within 6–8 weeks according to surgeon’s preference to allow healing of the repaired tendon.89,90 If the subscapularis tendon was completely torn prior to surgery or was not repaired after surgery, this precaution does not apply. In the presence of subscapularis deficiency, teres major, latissimus dorsi and pectoralis major would play an important role in maintaining internal rotation.
Phase III (>12 Weeks)
Precautions
Considering the possibility of a traumatic dislocation even after 12 weeks, the static and dynamic combined movements remain limited in high risk patients. Sudden and repetitive lifting, jerking activities, throwing weights, jumping, extensive hammering, punching (ballistic exercises) should be avoided18 as they may cause subluxation or dislocation of the implant.
Isotonic exercises using rubber-based resistance bands may be commenced for younger patients or those with a more active life style at this point. When using resistance bands, one should consider the length-tension relationship, which describes how much tension (i.e. load) is provided when the band(s) is stretched to a particular length. McMaster et al.103 provide a table that represents of the amount of weight added when the bands are stretched to a particular length. For example, the first 10 cm of the yellow resistance band adds about 2.8 kg, the first 20 cm adds about 5.7 kg. This load for the first 10 and 20 cm of the red resistance band is 4.6 and 9.6 kg respectively. Therefore, it is important for the clinicians to be aware of the strength and length of band used in this population.
Most patients would have accomplished a painfree active range of motion and good deltoid activation and scapulothoracic rhythm. The stabilizing role of deltoid is more effective when the arm is elevated.71 Therefore, to better activate anterior deltoid, patient resists against a resistance band placed above the operated side elbow and held by the opposite hand at the hip level moving in a diagonal flexion and abduction direction (Figure 11). Middle deltoid isotonic strengthening involves resisting against a resistance band held by the opposite hand at the thigh level moving in the abduction direction (Figure 12). Forceful resistance band extension/abduction may not be safe for RTSA and in most cases an isometric posterior/extension as shown in Figures 4 and 5 is sufficient. The external rotation component of the posterior deltoid and the teres minor can be strengthened by placing a resistance band above the elbow and placing the second resistance band above the wrist, both held by the opposite hand. While the patient resists against abduction, the forearm externally rotates (Figure 13).
Figure 11.
Anterior deltoid. Isotonic diagonal flexion and abdduction against resistance band in the scapular plane.
Figure 12.
Middle deltoid. Isotonic abduction against resistance band in the scapular plane.
Figure 13.
Posterior deltoid and teres minor. Advanced isotonic abduction and external rotation against resistance band in the scapular plane. While above elbow strap provides resistance in isometric abduction, the affected forearm is externally rotated against the resistance band above the wrist. Caution: limit the amount of stretch when using two bands simultaneously to avoid strain.
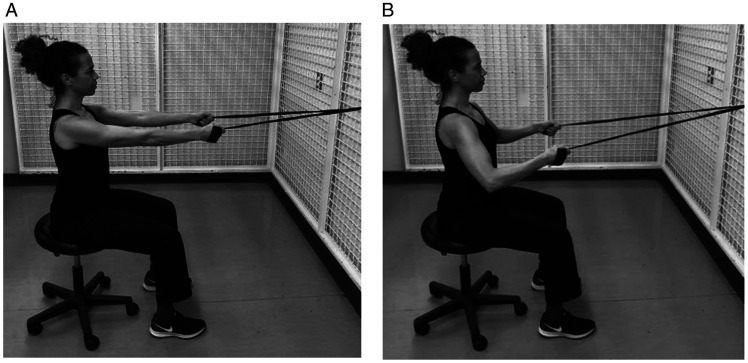
Performing bilateral symmetrical arm movements could help to improve proprioception via inter-hemispherical cerebral communication.71 The bilateral resistance band muscle strengthening is initiated at 30° of scapular plane abduction progressing to 90° while making the best effort to avoid the hornblower position commonly seen in this population (outward movement of the elbow) (Figure 14). Adding lats/pull down (Figure 15) and rowing (Figure 16) exercises would strengthen the posterior deltoid, latissimus dorsi, rhomboids and the overall trunk muscles. Patients are reminded to engage scapular muscles by squeezing their shoulder blades together during these exercises. It is suggested that if tolerated, these exercises be performed in standing with squats to help with core strengthening. Forceful shoulder hyperextension should be limited to neutral position at all times to avoid the risk of dislocation. A systematic review of rehabilitation protocols17 indicates that achieving 120°of active elevation is considered satisfactory as full active range of motion is not expected after reverse total shoulder arthroplasty. Following RTSA, potential for gaining significant external rotation remains small, particularly in the presence of fatty infiltration in teres minor.75
Figure 14.
Ttrapezius, rhomboids, teres minor, anterior, middle and posterior deltoid. Bilateral isotonic arm elevation with external rotation using a resistance band. Elbows should be kept inward during the elevation. A, Initial position with squeezing shoulder blades. B, Final position.
Figure 15.
Posterior deltoid and latissimus dorsi. Isotonic lats/pull downs is performed with a band placed over top of a door or secured on a wall and the resistance band held in both hands. Patient pulls down in scapular plane abduction with the elbows in a 90° angle. Hyperextension to be avoided at all times. A, Initial position. B, Final position.
Figure 16.
Posterior deltoid, rhomboids and latissimus dorsi. Isotonic rowing is performed with a band placed around a door knob or secured in the front. The resistance band is held in both hands and pulled backward maintaining the scapular plane abduction with the elbows in a 90° angle. Hyperextension to be avoided at all times. A, Initial position. B, Final position.
Limitations
Given the lack of prospective comparative studies, the evidence to recommend for or against a specific timing of immobilization and initiation of passive, active and strengthening exercises is insufficient. Similarly, conducting randomized controlled studies to evaluate the impact of postoperative immobilization or certain exercises following RTSA for occurrence of dislocation, scapular notching or proximal humeral fracture may not be feasible due to the rare frequency of these complications and variability of the rehabilitation protocols. In this review, we have provided an assessment of the relevant muscles in RTSA and provided recommendations based on how the muscle function may be enhanced after this surgery. While this information is helpful for clinicians, future prospective or RCT may be needed to better assess different components of the rehabilitation in this population.
Footnotes
Authors’ Note: Research ethics review was not required based on our institutional process for confirming that the project was deemed improvement in quality and not human subject research. Andrea Nunn, Ania Roszkowski and Analia Szafirwoicz are now not affiliated with Department of Physical therapy, Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Helen Razmjou https://orcid.org/0000-0002-3162-4241
References
- 1.Lugli T.Artificial shoulder joint by Pean (1893): the facts of an exceptional intervention and the prosthetic method. Clin Orthop Relat Res. 1978;133:215–218. [PubMed] [Google Scholar]
- 2.Baulot E, Sirveaux F, Boileau P.Grammont’s idea: the story of Paulgrammont’s functional surgery concept and the development of the reverse principle. Clin Orthop Relat Res. 2011; 469(9):2425–2431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grammont P, Laffay J, Deries X.Concept study and reaslization of a new total shoulder prosthesis [French]. Rhumatologie. 1987; 39:407–418. [Google Scholar]
- 4.Grammont P, Bourgon J, Pelzer P.Study of a Mechanical Model for a Shoulder Total Prosthesis: Realization of a Prototype [in French] [thèse de sciences de l’Ingénieur]. Dijon, France: Universitédijon; Lyon, France: ECAM de lyon; 1981.
- 5.Ernstbrunner L, Andronic O, Grubhofer F, Camenzind RS, Wieser K, Gerber C. Long-term results of reverse total shoulder arthroplasty for rotator cuff dysfunction: a systematic review of longitudinal outcomes. J Shoulder Elbow Surg. 2019; 28(4):774–781. [DOI] [PubMed] [Google Scholar]
- 6.Ho JC, Kane L, Stone MA, et al. Arthroscopic debridement of irreparable rotator cuff tears: predictors of failure and success. J Shoulder Elbow Surg. 2019; 29(4):e118–e123. [DOI] [PubMed] [Google Scholar]
- 7.Sevivas N, Ferreira N, Andrade R, et al. Reverse shoulder arthroplasty for irreparable massive rotator cuff tears: a systematic review with meta-analysis and meta-regression. J Shoulder Elbow Surg. 2017; 26(9):e265–e277. [DOI] [PubMed] [Google Scholar]
- 8.Boileau P, Watkinson D, Hatzidakis AM, et al. Neer award 2005: the grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg. 2006; 15(5):527–540. [DOI] [PubMed] [Google Scholar]
- 9.Frankle MA, Teramoto A, Luo ZP, et al. Glenoid morphology in reverse shoulder arthroplasty: classification and surgical implications. J Shoulder Elbow Surg. 2009; 18(6):874–885. [DOI] [PubMed] [Google Scholar]
- 10.Mizuno N, Denard PJ, Raiss P, et al. Reverse total shoulder arthroplasty for primary glenohumeral osteoarthritis in patients with a biconcave glenoid. J Bone Joint Surg Am. 2013; 95(14):1297–1304. [DOI] [PubMed] [Google Scholar]
- 11.Bois AJ, Knight P, Alhojailan K, et al. Clinical outcomes and complications of reverse shoulder arthroplasty used for failed prior shoulder surgery: a systematic review and meta-analysis. JSES Int. 2020; 4(1):156–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hagen MS, Allahabadi S, Zhang AL, et al. A randomized single-blinded trial of early rehabilitation versus immobilization after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2020; 29(3):442–450. [DOI] [PubMed] [Google Scholar]
- 13.Philippossian R, Luthi F, Farron A, et al. Update on the rehabilitation following anatomic and reverse total shoulder arthroplasty. Rev Med Suisse. 2019; 15(657):1340–1349. [PubMed] [Google Scholar]
- 14.Kirsch JM, Namdari S.Rehabilitation after anatomic and reverse total shoulder arthroplasty: a critical analysis review. JBJS Rev. 2020; 8(2):e0129. [DOI] [PubMed] [Google Scholar]
- 15.Wolff AL, Rosenzweig L.Anatomical and biomechanical framework for shoulder arthroplasty rehabilitation. J Hand Ther. 2017; 30(2):167–174. [DOI] [PubMed] [Google Scholar]
- 16.Buchmann S, Schoch C, Grim C, et al. Rehabilitation following reverse shoulder arthroplasty. A work of the rehabilitation commission of the German Society of Shoulder and Elbow Surgery (DVSE) e.V. in collaboration with the German Association for Physiotherapy (ZVK) e.V., the Physical Therapy Association—Association for Physical Professions (VPT) e.V. and the Rehabilitation Section—Physical Therapy of the German Society for Orthopaedics and Trauma e.V. (DGOU). ObereExtremität. 2019; 14:269–283. https://link.springer.com/article/10.1007/s11678-019-0513-5#citeas). Accessed April 10, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bullock GS, Garrigues GE, Ledbetter L, et al. A systematic review of proposed rehabilitation guidelines following anatomic and reverse shoulder arthroplasty. J Orthop Sports Phys Ther. 2019; 49(5):337–346. [DOI] [PubMed] [Google Scholar]
- 18.Boudreau S, Boudreau ED, Higgins LD, et al. Ehabilitation following reverse total shoulder arthroplasty. J Orthop Sports Phys Ther. 2007; 37(12):734–743. [DOI] [PubMed] [Google Scholar]
- 19.Schairer WW, Nwachukwu BU, Lyman S, et al. National utilization of reverse total shoulder arthroplasty in the United States. J Shoulder Elbow Surg. 2015; 24(1):91–97. [DOI] [PubMed] [Google Scholar]
- 20.Cvetanovich GL, Frank RM, Chalmers PN, et al. Surgical management of proximal humeral fractures: the emerging role of reverse total shoulder arthroplasty. Orthopedics. 2016; 39(3):e465-73–e473. [DOI] [PubMed] [Google Scholar]
- 21.Dillon MT, Prentice HA, Burfeind WE, et al. The increasing role of reverse total shoulder arthroplasty in the treatment of proximal humerus fractures. Injury. 2019; 50(3):676–680. [DOI] [PubMed] [Google Scholar]
- 22.Palsis JA, Simpson KN, Matthews JH, et al. Current trends in the use of shoulder arthroplasty in the United States. Orthopedics. 2018; 41(3):e416–e423. [DOI] [PubMed] [Google Scholar]
- 23.Klug A, Gramlich Y, Wincheringer D, et al. Trends in surgical management of proximal humeral fractures in adults: a nationwide study of records in Germany from 2007 to 2016. Arch Orthop Trauma Surg. 2019; 139(12):1713–1721. [DOI] [PubMed] [Google Scholar]
- 24.Sabesan VJ, Lombardo D, Petersen-Fitts G, et al. National trends in proximal humerus fracture treatment patterns. Aging Clin Exp Res. 2017; 29(6):1277–1283. [DOI] [PubMed] [Google Scholar]
- 25.Waterman BR, Dean RS, Naylor AJ, et al. Comparative clinical outcomes of reverse total shoulder arthroplasty for primary cuff tear arthropathy versus severe glenohumeral osteoarthritis with intact rotator cuff: a matched-cohort analysis. J Am Acad Orthop Surg. 2020; 28(23):e1042–e1048. [DOI] [PubMed] [Google Scholar]
- 26.Warner JJ, Higgins L, Parsons IM, 4th, et al. Diagnosis and treatment of anterosuperior rotator cuff tears. J Shoulder Elbow Surg. 2001; 10(1):37–46. [DOI] [PubMed] [Google Scholar]
- 27.Hansen ML, Otis JC, Johnson JS, et al. Biomechanics of massive rotator cuff tears: implications for treatment. J Bone Joint Surg Am. 2008; 90(2):316–325. [DOI] [PubMed] [Google Scholar]
- 28.Keener JD, Wei AS, Kim HM, et al. Proximal humeral migration in shoulders with symptomatic and asymptomatic rotator cuff tears. J Bone Joint Surg Am. 2009; 91(6):1405–1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Franklin JL, Barrett WP, Jackins SE, et al. Lenoid loosening in total shoulder arthroplasty. association with rotator cuff deficiency. J Arthroplasty. 1988; 3(1):39–46. [DOI] [PubMed] [Google Scholar]
- 30.Pegreffi F, Pellegrini A, Paladini P, et al. Deltoid muscle activity in patients with reverse shoulder prosthesis at 2-year follow-up. Musculoskelet Surg. 2017; 101(S2):129–135. [DOI] [PubMed] [Google Scholar]
- 31.Walker DR, Kinney AL, Wright TW, et al. How sensitive is the deltoid moment arm to humeral offset changes with reverse total shoulder arthroplasty? J Shoulder Elbow Surg. 2016; 25(6):998–1004. [DOI] [PubMed] [Google Scholar]
- 32.Walker DR, Struk AM, Matsuki K, et al. How do deltoid muscle moment arms change after reverse total shoulder arthroplasty? J Shoulder Elbow Surg. 2016; 25(4):581–588. [DOI] [PubMed] [Google Scholar]
- 33.Kontaxis A, Johnson GR.The biomechanics of reverse anatomy shoulder replacement–a modelling study. Clin Biomech (Bristol, Avon)). 2009; 24(3):254–260. [DOI] [PubMed] [Google Scholar]
- 34.Scarlat MM.Complications with reverse total shoulder arthroplasty and recent evolutions. Int Orthop. 2013. May; 37(5):843–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McFarland EG, Sanguanjit P, Tasaki A, et al. The reverse shoulder prosthesis: a review of imaging features and complications. Skeletal Radiol. 2006; 35(7):488–496. [DOI] [PubMed] [Google Scholar]
- 36.Erickson BJ, Shishani Y, Jones S, et al. Outpatient vs. inpatient reverse total shoulder arthroplasty: outcomes and complications. J Shoulder Elbow Surg. 2020; 29(6):1115–1120. [DOI] [PubMed] [Google Scholar]
- 37.Chalmers PN, Rahman Z, Romeo AA, et al. Early dislocation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014; 23(5):737–744. [DOI] [PubMed] [Google Scholar]
- 38.Gallo RA, Gamradt SC, Mattern CJ, et al. Instability after reverse total shoulder replacement. J Shoulder Elbow Surg. 2011; 20(4):584–590. [DOI] [PubMed] [Google Scholar]
- 39.Affonso J, Nicholson GP, Frankle MA, et al. Complications of the reverse prosthesis: prevention and treatment. Instr Course Lect. 2012; 61:157–168. [PubMed] [Google Scholar]
- 40.Boileau P, Watkinson DJ, Hatzidakis AM, et al. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005; 14(1 Suppl S):147S–161S. [DOI] [PubMed] [Google Scholar]
- 41.Oh JH, Shin SJ, McGarry MH, et al. Biomechanical effects of humeral neck-shaft angle and subscapularis integrity in reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014; 23(8):1091–1098. [DOI] [PubMed] [Google Scholar]
- 42.Kohan EM, Chalmers PN, Salazar D, et al. Dislocation following reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2017; 26(7):1238–1245. [DOI] [PubMed] [Google Scholar]
- 43.Bonnevialle N, Dauzeres F, Toulemonde J, et al. Periprosthetic shoulder infection: an overview. EFORT Open Rev. 2017; 2(4):104–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gerber C, Pennington SD, Nyffeler RW.Reverse total shoulder arthroplasty. J Am AcadOrthop Surg. 2009; 17(5):284–295. [DOI] [PubMed] [Google Scholar]
- 45.Friedman RJ, Barcel DA, Eichinger JK.Scapular notching in reverse total shoulder arthroplasty. J Am AcadOrthop Surg. 2019; 27(6):200–209. [DOI] [PubMed] [Google Scholar]
- 46.Ladermann A, Gueorguiev B, Charbonnier C, et al. Scapular notching on kinematic simulated range of motion after reverse shoulder arthroplasty is not the result of impingement in adduction. Medicine (Baltimore). 2015; 94(38):e1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nyffeler RW, Werner CM, Simmen BR, et al. Analysis of a retrieved Delta III total shoulder prosthesis. J Bone Joint Surg Br. 2004; 86(8):1187–1191. [DOI] [PubMed] [Google Scholar]
- 48.Mollon B, Mahure SA, Roche CP, et al. Impact of scapular notching on clinical outcomes after reverse total shoulder arthroplasty: an analysis of 476 shoulders. J Shoulder Elbow Surg. 2017; 26(7):1253–1261. [DOI] [PubMed] [Google Scholar]
- 49.Levigne C, Garret J, Boileau P, et al. Scapular notching in reverse shoulder arthroplasty: is it important to avoid it and how? Clin Orthop Relat Res. 2011; 469(9):2512–2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cusick MC, Otto RJ, Clark RE, et al. Outcome of reverse shoulder arthroplasty for patients with Parkinson’s disease: a matched cohort study. Orthopedics. 2017; 40(4):e675–e680. [DOI] [PubMed] [Google Scholar]
- 51.Dunn J, Byrne AN, Higgins LD.Reverse total shoulder arthroplasty in patients with Parkinson disease: a case series and review of the literature. Am J Orthop (Belle Mead NJ). 2011; 40(12):625–629. [PubMed] [Google Scholar]
- 52.Mayne IP, Bell SN, Wright W, et al. Acromial and scapular spine fractures after reverse total shoulder arthroplasty. Shoulder Elbow. 2016; 8(2):90–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Levy JC, Anderson C, Samson A.Classification of postoperative acromial fractures following reverse shoulder arthroplasty. J Bone Joint Surg Am. 2013; 95(15):e104. [DOI] [PubMed] [Google Scholar]
- 54.Cho CH, Jung JW, Na SS, et al. Is acromial fracture after reverse total shoulder arthroplasty a negligible complication?: a systematic review. Clin Orthop Surg. 2019; 11(4):427–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Walch G, Mottier F, Wall B, et al. Acromial insufficiency in reverse shoulder arthroplasties. J Shoulder Elbow Surg. 2009; 18(3):495–502. [DOI] [PubMed] [Google Scholar]
- 56.Neyton L, Erickson J, Ascione F, et al. Grammont award 2018: scapular fractures in reverse shoulder arthroplasty (grammont style): prevalence, functional, and radiographic results with minimum 5-year follow-up. J Shoulder Elbow Surg. 2019; 28(2):260–267. [DOI] [PubMed] [Google Scholar]
- 57.Ascione F, Kilian CM, Laughlin MS, et al. Increased scapular spine fractures after reverse shoulder arthroplasty with a humeral onlay short stem: an analysis of 485 consecutive cases. J Shoulder Elbow Surg. 2018; 27(12):2183–2190. [DOI] [PubMed] [Google Scholar]
- 58.Teusink MJ, Otto RJ, Cottrell BJ, et al. What is the effect of postoperative scapular fracture on outcomes of reverse shoulder arthroplasty? J Shoulder Elbow Surg. 2014; 23(6):782–790. [DOI] [PubMed] [Google Scholar]
- 59.Hattrup SJ.The influence of postoperative acromial and scapular spine fractures on the results of reverse shoulder arthroplasty. Orthopedics. 2010; 33(5). [DOI] [PubMed] [Google Scholar]
- 60.Otto RJ, Virani NA, Levy JC, et al. Scapular fractures after reverse shoulder arthroplasty: evaluation of risk factors and the reliability of a proposed classification. J Shoulder Elbow Surg. 2013; 22(11):1514–1521. [DOI] [PubMed] [Google Scholar]
- 61.Crosby LA, Hamilton A, Twiss T.Scapula fractures after reverse total shoulder arthroplasty: classification and treatment. Clin Orthop Relat Res. 2011; 469(9):2544–2549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kim HJ, Kwon TY, Jeon YS, et al. Neurologic deficit after reverse total shoulder arthroplasty: correlation with distalization. J Shoulder Elbow Surg. 2020; 29(6):1096–1103. [DOI] [PubMed] [Google Scholar]
- 63.Van Hoof T, Gomes GT, Audenaert E, et al. 3D computerized model for measuring strain and displacement of the brachial plexus following placement of reverse shoulder prosthesis. Anat Rec (Hoboken). 2008; 291(9):1173–1185. [DOI] [PubMed] [Google Scholar]
- 64.Cheung E, Willis M, Walker M, et al. Complications in reverse total shoulder arthroplasty. J Am AcadOrthop Surg. 2011; 19(7):439–449. [PubMed] [Google Scholar]
- 65.Kuechle DK, Newman SR, Itoi E, Morrey BF, et al. Shoulder muscle moment arms during horizontal flexion and elevation. J Shoulder Elbow Surg. 1997; 6(5):429–439. [DOI] [PubMed] [Google Scholar]
- 66.Yian EH, Sodl JF, Dionysian E, et al. Anterior deltoid reeducation for irreparable rotator cuff tears revisited. J Shoulder Elbow Surg. 2017; 26(9):1562–1565. [DOI] [PubMed] [Google Scholar]
- 67.Li H, Yoon SH, Lee D, et al. Relation between preoperative electromyographic activity of the deltoid and upper trapezius muscle and clinical results in patients treated with reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2020; 29(1):195–201. [DOI] [PubMed] [Google Scholar]
- 68.Ackland DC, Roshan-Zamir S, Richardson M, et al. Moment arms of the shoulder musculature after reverse total shoulder arthroplasty. J Bone Joint Surg Am. 2010. May; 92(5):1221–1230. [DOI] [PubMed] [Google Scholar]
- 69.Walker D, Wright TW, Banks SA, et al. Electromyographic analysis of reverse total shoulder arthroplasties. J Shoulder Elbow Surg. 2014; 23(2):166–172. [DOI] [PubMed] [Google Scholar]
- 70.Precerutti M, Garioni E, Madonia L, et al. US anatomy of the shoulder: pictorial essay. J Ultrasound. 2010; 13(4):179–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Collin PG, Gain S, Nguyen Huu F, et al. Is rehabilitation effective in massive rotator cuff tears? Orthop Traumatol Surg Res. 2015; 101(4 Suppl):S203–S205. [DOI] [PubMed] [Google Scholar]
- 72.Ackland DC, Pak P, Richardson M, et al. Moment arms of the muscles crossing the anatomical shoulder. J Anat. 2008; 213(4):383–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ackland DC, Richardson M, Pandy MG.Axial rotation moment arms of the shoulder musculature after reverse total shoulder arthroplasty. J Bone Joint Surg Am. 2012; 94(20):1886–1895. [DOI] [PubMed] [Google Scholar]
- 74.Werner CM, Steinmann PA, Gilbart M, et al. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005; 87(7):1476–1486. [DOI] [PubMed] [Google Scholar]
- 75.Simovitch RW, Helmy N, Zumstein MA, et al. Impact of fatty infiltration of the teres minor muscle on the outcome of reverse total shoulder arthroplasty. J Bone Joint Surg Am. 2007; 89(5):934–939. [DOI] [PubMed] [Google Scholar]
- 76.Sheth M, Ko JK, Namdari S.Reverse shoulder arthroplasty and latissimusdorsi tendon transfer. Am J Orthop (Belle Mead NJ). 2017; 46(5):E287–E292. [PubMed] [Google Scholar]
- 77.Greiner SH, Back DA, Herrmann S, et al. Degenerative changes of the deltoid muscle have impact on clinical outcome after reversed total shoulder arthroplasty. Arch Orthop Trauma Surg. 2010; 130(2):177–183. [DOI] [PubMed] [Google Scholar]
- 78.Yoon JP, Seo A, Kim JJ, et al. Deltoid muscle volume affects clinical outcome of reverse total shoulder arthroplasty in patients with cuff tear arthropathy or irreparable cuff tears. PLoS One. 2017; 12(3):e0174361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wiater BP, Koueiter DM, Maerz T, et al. Preoperative deltoid size and fatty infiltration of the deltoid and rotator cuff correlate to outcomes after reverse total shoulder arthroplasty. Clin Orthop Relat Res. 2015; 473(2):663–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jarrett CD, Brown BT, Schmidt CC.Reverse shoulder arthroplasty. Orthop Clin North Am. 2013; 44(3):389–408, x. [DOI] [PubMed] [Google Scholar]
- 81.Reed D, Cathers I, Halaki M, et al. Does load influence shoulder muscle recruitment patterns during scapular plane abduction? J Sci Med Sport. 2016; 19(9):755–760. [DOI] [PubMed] [Google Scholar]
- 82.Wickham J, Pizzari T, Balster S, et al. The variable roles of the upper and lower subscapularis during shoulder motion. ClinBiomech (Bristol, Avon. 2014; 29(8):885–891. [DOI] [PubMed] [Google Scholar]
- 83.Edwards TB, Williams MD, Labriola JE, et al. Subscapularis insufficiency and the risk of shoulder dislocation after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2009; 18(6):892–896. [DOI] [PubMed] [Google Scholar]
- 84.Friedman RJ, Flurin PH, Wright TW, et al. Comparison of reverse total shoulder arthroplasty outcomes with and without subscapularis repair. J Shoulder Elbow Surg. 2017; 26(4):662–668. [DOI] [PubMed] [Google Scholar]
- 85.Clark JC, Ritchie J, Song FS, et al. Complication rates, dislocation, pain, and postoperative range of motion after reverse shoulder arthroplasty in patients with and without repair of the subscapularis. J Shoulder Elbow Surg. 2012; 21(1):36–41. [DOI] [PubMed] [Google Scholar]
- 86.Wall B, Nove-Josserand L, O'Connor DP, et al. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007; 89(7):1476–1485. [DOI] [PubMed] [Google Scholar]
- 87.Routman HD.The role of subscapularis repair in reverse total shoulder arthroplasty. Bull HospJt Dis (2013). 2013; 71(Suppl 2):108–112. [PubMed] [Google Scholar]
- 88.De Fine M, Sartori M, Giavaresi G, et al. The role of subscapularis repair following reverse shoulder arthroplasty: systematic review and meta-analysis [published online ahead of print February 26, 2021]. Arch Orthop Trauma Surg. doi:10.1007/s00402-020-03716-9 [DOI] [PubMed]
- 89.Denard PJ, Ladermann A.Immediate versus delayed passive range of motion following total shoulder arthroplasty. J Shoulder Elbow Surg. 2016; 25(12):1918–1924. [DOI] [PubMed] [Google Scholar]
- 90.Romano AM, Oliva F, Nastrucci G, et al. Reverse shoulder arthroplasty patient personalized rehabilitation protocol. preliminary results according to prognostic groups. Muscle Ligam Tendons J. 2017; 7(2):263–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bull ML, Vitti M, de Freitas V.Electromyographic study of the trapezius (upper portion) and levator scapulae muscles in some movements of the shoulders. AnatAnz. 1985; 159(1–5):21–27. [PubMed] [Google Scholar]
- 92.Umehara J, Kusano K, Nakamura M, et al. Scapular kinematic and shoulder muscle activity alterations after serratus anterior muscle fatigue. J Shoulder Elbow Surg. 2018; 27(7):1205–1213. [DOI] [PubMed] [Google Scholar]
- 93.Lukasiewicz AC, McClure P, Michener L, et al. Comparison of 3-dimensional scapular position and orientation between subjects with and without shoulder impingement. J Orthop Sports Phys Ther. 1999; 29(10):574–586. [DOI] [PubMed] [Google Scholar]
- 94.Bandholm T, Rasmussen L, Aagaard P, et al. Force steadiness, muscle activity, and maximal muscle strength in subjects with subacromial impingement syndrome. Muscle Nerve. 2006; 34(5):631–639. [DOI] [PubMed] [Google Scholar]
- 95.Alizadehkhaiyat O, Hawkes DH, Kemp GJ, et al. Electromyographic analysis of the shoulder girdle musculature during external rotation exercises. Orthop J Sports Med. 2015; 3(11):232596711561398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Peat M.Functional anatomy of the shoulder complex. Phys Ther. 1986; 66(12):1855–1865. [DOI] [PubMed] [Google Scholar]
- 97.Kibler WB, Sciascia A.The role of the scapula in preventing and treating shoulder instability. Knee Surg Sports Traumatol Arthrosc. 2016; 24(2):390–397. [DOI] [PubMed] [Google Scholar]
- 98.Paine R, Voight ML.The role of the scapula. Int J Sports PhysTher. 2013; 8(5):617–629. [PMC free article] [PubMed] [Google Scholar]
- 99.Reinold MM, Escamilla RF, Wilk KE.Current concepts in the scientific and clinical rationale behind exercises for glenohumeral and scapulothoracic musculature. J Orthop Sports Phys Ther. 2009; 39(2):105–117. [DOI] [PubMed] [Google Scholar]
- 100.Ellenbecker TS, Davies GJ.The application of isokinetics in testing and rehabilitation of the shoulder complex. J Athl Train. 2000; 35(3):338–350. [PMC free article] [PubMed] [Google Scholar]
- 101.Alpert SW, Pink MM, Jobe FW, et al. Electromyographic analysis of deltoid and rotator cuff function under varying loads and speeds. J Shoulder Elbow Surg. 2000; 9(1):47–58. [DOI] [PubMed] [Google Scholar]
- 102.Escamilla RF, Yamashiro K, Paulos L, et al. Shoulder muscle activity and function in common shoulder rehabilitation exercises. Sports Med. 2009; 39(8):663–685. [DOI] [PubMed] [Google Scholar]
- 103.McMaster DT, Cronin J, McGuigan MR.Quantification of rubber and chain-based resistance modes. J Strength Cond Res. 2010; 24(8):2056–2064. [DOI] [PubMed] [Google Scholar]