Abstract
The purpose of this study is to compare patient-specific quality assurance (PSQA) results between two dimensional (2D) diode (SRS MapCHECK®) and 3D diode (ArcCHECK®) arrays. Twenty-eight intracranial stereotactic radiosurgery (SRS) and 26 lung stereotactic body radiation therapy (SBRT) clinical plans with a single lesion were selected and categorized into 4 groups: 20 SRS dynamic conformal arc therapy (DCAT) plans (Group A), 8 SRS volumetric modulated arc therapy (VMAT) plans (Group B), 6 SBRT DCAT plans (Group C) and 20 SBRT VMAT plans (Group D). An individual field of each plan was delivered on SRS MapCHECK and ArcCHECK and QA analysis was performed using 4 gamma criteria of dose difference/distance-to-agreement of 3%/3 mm, 3%/2 mm, 2%/2 mm and 2%/1 mm. Statistical analysis was performed to compare PSQA results between the 2 QA devices. For all 4 groups and all 4 gamma criteria, average gamma passing rates were higher with SRS MapCHECK.
Keywords: Patient-specific quality assurance (PSQA), SRS MapCHECK, ArcCHECK, stereotactic radiosurgery (SRS), stereotactic body radiation therapy (SBRT)
INTRODUCTION
Stereotactic radiosurgery (SRS) and stereotactic body radiation therapy (SBRT) are fundamentally different from conventional radiotherapy because of higher fractional dose which makes a biological effect to cancer cells more potent1,2. SRS and SBRT plans are usually generated such that rapid dose fall-off gradients encompass targets. Due to steep dose gradients, minor deviations in radiation delivery can lead to critical errors with undesirable clinical outcomes1. Therefore, a robust quality assurance (QA) program for SRS and SBRT is essential in each clinic and as part of a QA program, patient-specific QA (PSQA) has been strongly advised prior to treatment1-3.
Various QA devices are commercially available for PSQA of SRS and SBRT treatments. They include diode arrays, ionization chamber arrays, small-volume ionization chambers, films, a portal imaging device and polymer gels3,4. Of these, diode arrays have been widely used as they are easy to use and provide accurate and reliable QA results5. Sun Nuclear Corporation (Melbourne, FL), one of the major QA device vendors, has produced two dimensional (2D) diode arrays (MapCHECK®, MapCHECK®2 and MapCHECK®3) and a 3D diode array (ArcCHECK®). Of these, ArcCHECK was designed for PSQA of arc fields in volumetric modulated arc therapy (VMAT) and intensity modulated radiation therapy (IMRT) with TomoTherapy (Accuray, Inc., Sunnyvale, CA)6. It has been reported that the ArcCHECK is used for PSQA of SRS and SBRT7-9 because VMAT and dynamic conformal arc therapy (DCAT) are widely used treatment planning techniques for SRS and SBRT10,11. In 2018, Sun Nuclear released SRS MapCHECK® which has a higher spatial resolution. This QA device inserted into a phantom, StereoPHANTM, was designed for PSQA and end-to-end testing of SRS treatment12,13. A multi-intuitional study validated this device as a PSQA/end-to-end testing tool for SRS13.
As aforementioned, studies on PSQA using SRS MapCHECK and ArcCHECK were published. To our knowledge, however, there has not been a study comparing PSQA between SRS MapCHECK and ArcCHECK. In this study, therefore, PSQA results performed using SRS MapCHECK (2D diode array) and ArcCHECK (3D diode array) were compared for single-lesion SRS and SBRT treatments.
MATERIALS AND METHODS
SRS MapCHECK versus ArcCHECK
A comparison of device specifications between SRS MapCHECK and ArcCHECK is shown in Table 1. SRS MapCHECK consists of 1013 diodes in a 7.7 cm × 7.7 cm 2D array with a diagonal center-to-center separation of 2.47 mm. Each diode has a 0.48 mm × 0.48 mm cross-section and an active volume of 0.007 mm3. The SRS MapCHECK resides inside Sun Nuclear’s end-to-end testing phantom named StereoPHANTM for PSQA13. On the other hand, ArcCHECK consists of 1386 diodes in a cylindrical array (21 cm in diameter and in length) with 10 mm detector spacing along cylindrical length and circumference. An active detector size is 0.8 mm × 0.8 mm.
Table 1.
Comparison of device specifications between Sun Nuclear SRS MapCHECK® and ArcCHECK®
| SRS MapCHECK | ArcCHECK | |
|---|---|---|
| Model No. | 1179 | 1220 |
| Dimension | 2D | 3D |
| Array size | 7.7 cm × 7.7 cm | 21.0 cm in diameter and in length |
| Total No. of detectors | 1013 | 1386 |
| Detector spacing | 2.47 mm (diagonally) | 10 mm (along cylindrical length and circumference) |
| Active detector area | 0.48 mm × 0.48 mm | 0.8 mm × 0.8 mm |
SRS and SBRT clinical plans
For this study, 28 intracranial SRS and 26 lung SBRT clinical plans with a single lesion were selected and categorized into 4 groups based on treatment planning techniques. All the plans were generated in the RayStation (version 8A, RaySearch Laboratories, Stockholm, Sweden) treatment planning system (TPS) using the 6 MV flattening-filter free beam of the Varian TrueBeam STx (Varian Medical Systems, Palo Alto, CA). Of 28 SRS plans, 20 plans were delivered with DCAT (Group A) and the rest with VMAT (Group B). Each SRS plan had 5-7 non-coplanar arc fields. Of 26 SBRT plans, 6 plans were delivered with DCAT (Group C) and the rest with VMAT (Group D). Each SBRT plan had 2-4 coplanar arc fields. A total number of plans, a total number of fields, fractional dose (range, Gy), delivered monitor units (MU) (range, MU) and planning target volume (PTV) (mean ± standard deviation (SD), cm3) for each group are listed in Table 2.
Table 2.
Classification of SRS and SBRT clinical plans based on treatment planning techniques
| Classification | Group A: SRS DCAT† |
Group B: SRS VMAT‡ |
Group C: SBRT DCAT |
Group D: SBRT VMAT |
|---|---|---|---|---|
| Total No. of plans | 20 | 8 | 6 | 20 |
| Total No. of fields | 123 | 47 | 12 | 50 |
| Prescribed dose/fraction (range) (Gy) | 15–24 | 12.5–22 | 10–18 | 8.5–12 |
| Delivered monitor unit/field (range) (MU) | 260–1372 | 312–2181 | 313 - 1638 | 125–2162 |
| PTV* (mean ± SD) (cm3) | 0.78 ± 0.70 | 1.23 ± 1.01 | 8.26 ± 3.71 | 12.88 ± 4.23 |
*Planning target volume
†Dynamic conformal arc therapy
‡Volumetric modulated arc therapy
PSQA comparison between SRS MapCHECK and ArcCHECK
PSQA plans for 54 clinical plans were generated on both SRS MapCHECK and ArcCHECK with a dose grid size of 1 mm × 1 mm. In RayStation, the outer surface of the StereoPHAN containing SRS MapCHECK and buildup acrylic spacers was contoured as a structure and the structure was overridden with a density of 1.2 g/cm3 following the recommendation of the Sun Nuclear SRS MapCHECK user guide. The isocenter of each clinical plan was set to the isocenter (i.e., intersection of X, Y and Z axes) of the StereoPHAN. Then each clinical plan was re-calculated on the StereoPHAN containing SRS MapCHECK and buildup spacers. Gantry and collimator angles and MU were kept the same as in clinical plans but a couch angle was collapsed to 0°. Planar dose for each field in each plan was exported for PSQA. The same procedures were repeated for ArcCHECK. For ArcCHECK, its outer surface was contoured and overridden with a density of 1.15 g/cm3 according to the ArcCHECK user guide.
PSQA was performed using SRS MapCHECK and ArcCHECK and QA results between the 2 devices were compared. Before PSQA, array calibration and dose calibration of the SRS MapCHECK were performed. The isocenter of the StereoPHAN containing SRS MapCHECK and buildup spacers was aligned to room lasers and its level was adjusted using the lasers. Then an individual field of each clinical plan (field-by-field method) was delivered with the couch angle overridden with 0°. For each field, measurement and calculation were compared based on 2D planar gamma analysis in Sun Nuclear SRS MapCHECK software (version 8.3.0). For comparison, 4 different gamma criteria of dose difference (DD)/distance-to-agreement (DTA) of 3%/3 mm, 3%/2 mm, 2%/2 mm and 2%/1 mm were applied. Absolute dose mode, global normalization and a threshold of 10% were used. During gamma analysis, to reduce setup uncertainty of the device, “Calc Shift” was applied if allowed in the software. The Calf Shift finds the best alignment between measured and planned dose maps, resulting in a lower number of failing points. The same procedures including device calibrations, measurement setups, PSQA and gamma analysis were repeated for ArcCHECK. For ArcCHECK, Sun Nuclear SNC Patient software (version 6.7.4) was used and 3D planar gamma analysis was performed without Calc Shift. After QA analysis, the non-parametric Wilcoxon matched pairs test between SRS MapCHECK and ArcCHECK was performed on each gamma criteria for each group. It is noted that dose volume histogram (DVH)-based analysis was not performed in this study due to unavailability of dedicated software (e.g., Sun Nuclear 3DVH®) in our institution.
For SBRT plans (Groups C and D), PSQA results between dose grid sizes of 1 mm × 1 mm and 2 mm × 2 mm were compared to investigate the impact of a dose grid size on PSQA. In RayStation, PSQA plans were re-calculated on ArcCHECK with a dose grid size of 2 mm × 2 mm. For each field, measurement and calculation were compared in SNC Patient software. As for a dose grid size of 1 mm × 1 mm, the same gamma criteria, normalization and threshold were used. After QA analysis, the Wilcoxon matched pairs test between the 2 dose grid sizes was performed on each gamma criteria for each group. This comparison was not made for SRS MapCHECK because SRS MapCHECK software only allows for a dose map calculated with a dose grid size of 1 mm × 1 mm.
RESULTS
Table 3 summarizes a comparison of PSQA results between SRS MapCHECK and ArcCHECK for each group. It is noted that when all the samples in a group have the same value, statistical analysis is not available because there is no variance among samples. For example, statistical analysis is unavailable for gamma criteria of 3%/3 mm and 3%/2 mm in Group A because gamma passing rates for all the fields delivered on SRS MapCHECK are 100%.
Table 3.
Comparison of patient-specific QA results between SRS MapCHECK and ArcCHECK for 4 different groups. The difference is statistically significant if a p value is <0.05.
| Group A: SRS DCAT† | ||||||||
|---|---|---|---|---|---|---|---|---|
| Gamma criteria | 3%/3 mm | 3%/2 mm | 2%/2 mm | 2%/1 mm | ||||
| QA device | SRS MC* |
AC° | SRS MC | AC | SRS MC | AC | SRS MC | AC |
| Gamma passing rate (mean ± SD) (%) | 100 | 99.96 ± 0.29 | 100 | 99.88 ± 0.52 | 99.95 ± 0.47 |
99.79 ± 0.75 |
99.54 ± 1.71 |
96.44 ± 3.56 |
| Statistically significantly different? (Y/N) | unavailable | unavailable | Y (p value = 0.0269) |
Y (p value <0.0001) |
||||
| Total No. of detectors irradiated (mean ± SD) | SRS MC: 178.0 ± 57.8; AC: 61.0 ± 29.7 | |||||||
| Group B: SRS VMAT‡ | ||||||||
| Gamma criteria | 3%/3 mm | 3%/2 mm | 2%/2 mm | 2%/1 mm | ||||
| QA device | SRS MC |
AC | SRS MC | AC | SRS MC | AC | SRS MC | AC |
| Gamma passing rate (mean ± SD) (%) | 99.79 ± 0.48 | 99.42 ± 1.40 | 99.16 ± 1.09 | 98.60 ± 2.34 | 98.42 ± 1.76 | 98.00 ± 2.60 | 93.71 ± 4.95 | 90.64 ± 5.68 |
| Statistically significantly different? (Y/N) | N (p value = 0.0599) |
N (p value = 0.1762) |
N (p value = 0.3264) |
Y (p value = 0.0013) |
||||
| Total No. of detectors irradiated (mean ± SD) | SRS MC: 246.7 ± 110.7; AC: 62.0 ± 26.5 | |||||||
| Group C: SBRT DCAT | ||||||||
| Gamma criteria | 3%/3 mm | 3%/2 mm | 2%/2 mm | 2%/1 mm | ||||
| QA device | SRS MC |
AC | SRS MC | AC | SRS MC | AC | SRS MC | AC |
| Gamma passing rate (mean ± SD) (%) | 100 | 100 | 100 | 99.80 ± 0.36 |
100 | 97.60 ± 2.41 |
100 | 86.39 ± 8.69 |
| Statistically significantly different? (Y/N) | unavailable | unavailable | unavailable | unavailable | ||||
| Total No. of detectors irradiated (mean ± SD) | SRS MC: 506.4 ± 135.6; AC: 263.4 ± 99.4 | |||||||
| Group D: SBRT VMAT | ||||||||
| Gamma criteria | 3%/3 mm | 3%/2 mm | 2%/2 mm | 2%/1 mm | ||||
| QA device | SRS MC |
AC | SRS MC | AC | SRS MC | AC | SRS MC | AC |
| Gamma passing rate (mean ± SD) (%) | 99.91 ± 0.35 | 99.82 ± 0.34 | 99.83 ± 0.64 | 99.71 ± 0.51 | 99.57 ± 1.13 | 99.00 ± 1.17 | 98.38 ± 3.27 | 93.60 ± 4.57 |
| Statistically significantly different? (Y/N) | N (p value = 0.0637) |
N (p value = 0.0917) |
Y (p value = 0.0030) |
Y (p value <0.0001) |
||||
| Total No. of detectors irradiated (mean ± SD) | SRS MC: 536.3 ± 119.6; AC: 180.8 ± 86.2 | |||||||
*SRS MapCHECK
°ArcCHECK
†Dynamic conformal arc therapy
‡Volumetric modulated arc therapy
Group A: SRS DCAT
Mean ± SD of gamma passing rates for SRS MapCHECK vs. ArcCHECK are 100% vs. 99.96% ± 0.29% (3%/3 mm), 100% vs. 99.88% ± 0.52% (3%/2 mm), 99.95% ± 0.47% vs. 99.79% ± 0.75% (2%/2 mm) and 99.54% ± 1.71% vs. 96.44% ± 3.56% (2%/1 mm). Average gamma passing rates for SRS MapCHECK are higher than those for ArcCHECK for all gamma criteria. The difference in average gamma passing rates between the 2 devices increases as gamma criteria become tighter. Average gamma passing rates for 2%/2 mm and 2%/1 mm are statistically significantly different between the 2 devices (p values <0.05) even though the absolute differences are not too large (0.16% for 2%/2 mm and 3.10% for 2%/1 mm).
Group B: SRS VMAT
Mean ± SD of gamma passing rates for SRS MapCHECK vs. ArcCHECK are 99.79% ± 0.48% vs. 99.42% ± 1.40% (3%/3 mm), 99.16% ± 1.09% vs. 98.60% ± 2.34% (3%/2 mm), 98.42% ± 1.76% vs. 98.00% ± 2.60% (2%/2 mm) and 93.71% ± 4.95% vs. 90.64% ± 5.68% (2%/1 mm). As in Group A, average gamma passing rates for SRS MapCHECK are higher than those for ArcCHECK for all gamma criteria. The differences in average gamma passing rates between the 2 devices are small (<0.6%) for gamma criteria of 3%/3 mm, 3%/2 mm and 2%/2 mm but the difference is noticeable (3.07%) for 2%/1 mm. As a result, average gamma passing rates for 2%/1 mm are statistically significantly different (p value <0.05) between the 2 devices whereas passing rates for the rest are not (p values >0.05). Average gamma passing rates for Group B are consistently lower than those for Group A for the same gamma criteria and the same device.
Group C: SBRT DCAT
Mean ± SD of gamma passing rates for SRS MapCHECK vs. ArcCHECK are 100% vs. 100% (3%/3 mm), 100% vs. 99.80% ± 0.36% (3%/2 mm), 100% vs. 97.60% ± 2.41% (2%/2 mm) and 100% vs. 86.39% ± 8.69% (2%/1 mm). As in Groups A and B, average gamma passing rates for SRS MapCHECK are higher than those for ArcCHECK for all gamma criteria. The difference in average gamma passing rates between the 2 devices increases as gamma criteria become tighter. The difference becomes noticeable (2.40%) for 2%/2 mm and is large (13.61%) for 2%/1 mm.
Group D: SBRT VMAT
Mean ± SD of gamma passing rates for SRS MapCHECK vs. ArcCHECK are 99.91% ± 0.35% vs. 99.82% ± 0.34% (3%/3 mm), 99.83% ± 0.64% vs. 99.71% ± 0.51% (3%/2 mm), 99.57% ± 1.13% vs. 99.00% ± 1.17% (2%/2 mm) and 98.38% ± 3.27% vs. 93.60% ± 4.57% (2%/1 mm). As in Groups A-C, 2 similar trends are observed: 1) Average gamma passing rates for SRS MapCHECK are higher than those for ArcCHECK for all gamma criteria. 2) The difference in average gamma passing rates between the 2 devices increases as gamma criteria become tighter (in Group B, the difference is similar among 3%/3 mm, 3%/2 mm and 2%/2 mm and then increases for 2%/1 mm). Average gamma passing rates for 3%/3 mm and 3%/2 mm are not statistically significantly different between the 2 devices (p values >0.05) whereas those for 2%/2 mm and 2%/1 mm are statistically significantly different (p values <0.05). In the SRS MapCHECK case, average gamma passing rates for Group D are consistently lower than those for Group C for the same gamma criteria with the maximum average gamma passing rate difference of 1.62% (Group D vs. Group C: 98.38% vs. 100%) for gamma criteria of 2%/1 mm. In the ArcCHECK case, the opposite (i.e., higher passing rates for Group D) is observed for gamma criteria of 2%/2 mm (Group D vs. Group C: 99.00% vs. 97.60%) and 2%/1 mm (Group D vs. Group C: 93.60% vs. 86.39%).
Dose grid size for SBRT plans: 1 mm × 1 mm versus 2 mm × 2 mm
Table 4 shows a comparison of ArcCHECK PSQA results between dose grid sizes of 1 mm × 1 mm and 2 mm × 2 mm for SBRT QA plans (Groups C and D). For Group C, mean ± SD of gamma passing rates for 2 mm vs. 1 mm are 100% vs. 100% (3%/3 mm), 99.71% ± 0.40% vs. 99.80% ± 0.36% (3%/2 mm), 97.22% ± 2.62% vs. 97.60% ± 2.41% (2%/2 mm) and 85.51% ± 9.32% vs. 86.39% ± 8.69% (2%/1 mm). Average gamma passing rates for 1 mm are higher than those for 2 mm for all gamma criteria but the differences between the 2 dose grid sizes are fairly small (0%-0.88%). Nonetheless, average gamma passing rates for 2%/2 mm and 2%/1 mm are statistically significantly different between the 2 dose grid sizes (p values <0.05). For Group D, mean ± SD of gamma passing rates for 2 mm vs. 1 mm are 98.83% ± 3.67% vs. 99.82% ± 0.34 (3%/3 mm), 97.73% ± 5.88 vs. 99.71% ± 0.51% (3%/2 mm), 95.96% ± 6.68% vs. 99.00% ± 1.17% (2%/2 mm) and 86.85% ± 13.55% vs. 93.60% ± 4.57% (2%/1 mm). As for Group C, average gamma passing rates for 1 mm are higher than those for 2 mm for all gamma criteria but the differences between the 2 dose grid sizes are larger (0.99%-6.75%) in Group D. For Group D, average gamma passing rates are statistically significantly different between the 2 dose grid sizes (p values <0.05) for all gamma criteria. In both groups, the difference in average gamma passing rates between the 2 dose grid sizes increases as gamma criteria become tighter.
Table 4.
Comparison of ArcCHECK patient-specific QA results between dose grid sizes of 1 mm × 1 mm and 2 mm × 2 mm for SBRT plans. The difference is statistically significant if a p value is < 0.05.
| Group C: SBRT DCAT† | ||||||||
|---|---|---|---|---|---|---|---|---|
| Gamma criteria | 3%/3 mm | 3%/2 mm | 2%/2 mm | 2%/1 mm | ||||
| Dose grid size | 2 mm | 1 mm | 2 mm | 1 mm | 2 mm | 1 mm | 2 mm | 1 mm |
| Gamma passing rate (mean ± SD) (%) | 100 | 100 | 99.71 ± 0.40 | 99.80 ± 0.36 |
97.22 ± 2.62 | 97.60 ± 2.41 |
85.51 ± 9.32 | 86.39 ± 8.69 |
| Statistically significantly different? (Y/N) | unavailable | N (p value = 0.4375) |
Y (p value = 0.0313) |
Y (p value = 0.0098) |
||||
| Group D: SBRT VMAT‡ | ||||||||
| Gamma criteria | 3%/3 mm | 3%/2 mm | 2%/2 mm | 2%/1 mm | ||||
| Dose grid size | 2 mm | 1 mm | 2 mm | 1 mm | 2 mm | 1 mm | 2 mm | 1 mm |
| Gamma passing rate (mean ± SD) (%) | 98.83 ± 3.67 | 99.82 ± 0.34 | 97.73 ± 5.88 | 99.71 ± 0.51 | 95.96 ± 6.68 | 99.00 ± 1.17 | 86.85 ± 13.55 | 93.60 ± 4.57 |
| Statistically significantly different? (Y/N) | Y (p value <0.0001) |
Y (p value <0.0001) |
Y (p value <0.0001) |
Y (p value <0.0001) |
||||
†Dynamic conformal arc therapy
‡Volumetric modulated arc therapy
DISCUSSION
SRS MapCHECK versus ArcCHECK
This study demonstrated that average gamma passing rates of PSQA are higher with SRS MapCHECK for single-lesion intracranial SRS and lung SBRT plans. As shown in Table 1, the 2 devices are different in terms of 1) geometry, 2) spatial resolution and 3) detector size and these differences in device specifications would affect QA results.
Detectors in SRS MapCHECK have more angular dependence during arc field delivery than those in ArcCHECK. In ArcCHECK, beam angles are almost perpendicular to the detectors because of the cylindrical geometry of ArcCHECK whereas this is not the case with SRS MapCHECK due to its intrinsic planar geometry. Nevertheless, SRS MapCHECK software corrects detectors’ angular dependence and therefore, the difference in angular dependence between the 2 devices would be small13.
A spatial resolution (detector spacing, 2.47 mm diagonally) of SRS MapCHECK is much higher than that (10 mm along cylindrical length and circumference) of ArcCHECK. For a given small radiation field of an SRS plan or an SBRT plan, if detector spacing is small (i.e., high spatial resolution), more number of detectors are irradiated and included for QA analysis and this can improve QA results. For example, if 7 detector points out of 50 fail, QA fails with a passing rate of 86% but if 7 points out of 200 fail, QA could pass. Table 3 shows a comparison of the average number of irradiated detectors between the 2 devices for each group. Due to the detector spacing (10 mm), ArcCHECK has a fewer number of detectors but it seems that it has enough number of detectors (on average, >61 detectors for SRS plans and >180 detectors for SBRT plans) for QA analysis because both SRS and SBRT plans have arc fields. PSQA results are fairly comparable between the 2 devices for 3%/3 mm, 3%/2 mm and 2%/2 mm regardless of statistical analysis results. However, PSQA results with ArcCHECK can be better than with SRS MapCHECK in high dose gradient regions of highly modulated VMAT plans when detectors of ArcCHECK are missing in high dose gradient regions due to the coarse detector spacing and thus, they cannot measure dose in the regions. In this study, for 6 out of 47 fields in Group B (SRS VMAT plans), the gamma passing rate was <90% with SRS MapCHECK but ≥90% with ArcCHECK for gamma criteria of 2%/1 mm.
Detectors in SRS MapCHECK have a smaller size (0.48 mm × 0.48 mm) and would have less volume averaging effects, meaning that dose would be measured more accurately at each detector in SRS MapCHECK, particularly in high dose gradient regions. Therefore, a smaller detector size can improve QA results especially for highly modulated plans which tend to have more heterogeneous dose distributions (i.e., have more high dose gradient regions).
Limitations of SRS MapCHECK and ArcCHECK as PSQA devices for SRS and SBRT treatments
Despite the better QA results, SRS MapCHECK has limitations. Due to the small array size (7.7 cm × 7.7 cm), PSQA for single-isocenter multi-target SRS treatment would not be feasible without device shifts when a distance between lesions is longer than the array size. Also, large PTVs of SBRT plans would not fit in the device. In this study, SBRT plans with PTV of <12.9 cm3 were selected (Table 2). Contrarily, ArcCHECK can be used for PSQA of any planning technique such as static IMRT, VMAT and DCAT and for PSQA of any size of lesions and any number of lesions. For this reason, ArcCHECK would be a PSQA device option for single-isocenter multi-target SRS treatment. Other device options include a film, an ionization chamber, a portal imaging device, Delta4 (ScandiDos AB, Uppsala, Sweden), Octavius 4D (PTW, Freiburg, Germany), and so on14. Most of these devices would require device repositioning/shifts for dose verification of each target depending on how far the targets are located from the isocenter. Although PSQA for any (single-lesion or multi-lesion) SRS and SBRT treatments can be performed with ArcCHECK, the ArcCHECK has its own limitations. The ArcCHECK does not have high sensitivity to gantry and collimator rotation errors and multi-leaf collimator (MLC) leaf positioning errors15,16. Liang et al. concluded that with 2%/2 mm gamma criteria, the minimum reliably detectable gantry rotation error and MLC leaf positioning error are 2° and 4 mm, respectively15. Szeverinski et al. reported sensitivity (ratio of a number of detected non-error-free plans to a total number of non-error-free plans) of 30.6% for a 2° collimator rotation error with 2%/2 mm gamma criteria16. On the other hand, ArcCHECK is more sensitive to couch translational and rotational setup errors17. Li et al. showed that with 2%/2 mm gamma criteria, gamma passing rates decreased by 6.7% ± 3.5% and by 14.5% ± 6.6% for 2 mm translational and 2° rotational setup errors, respectively17. These errors would be critical in SRS and SBRT treatments1. Sensitivity of SRS MapCHECK to setup errors or MLC leaf positioning errors has not been studied yet. In addition, for SRS and SBRT treatments which have non-coplanar arcs, True Composite (TC, i.e., composite beam delivery with the same delivery parameters as in a patient plan) PSQA might not be feasible with ArcCHECK depending on the gantry angle due to a collision between gantry and couch.
Discussion on each group, dose grid size and gamma criteria
Group A: SRS DCAT
High average gamma passing rates (>96.4% for all gamma criteria and for both QA devices) for Group A would be due to the treatment planning technique (DCAT) used in this group. DCAT is one of the 3D conformal radiation therapy techniques. In DCAT, as gantry rotates, a beam aperture created by MLCs changes in every certain degrees (e.g., 2°) according to the beam’s eye view of PTV but MLCs are not moving for modulation during beam delivery. Hence, dose distributions of DCAT plans are typically more homogeneous than those of VMAT plans, resulting in higher gamma passing rates with DCAT plans (Table 3). In our institution, a combination of full arc (360°) and partial arc (<180°) angles are chosen for SRS plans and a full arc field usually has the highest beam weighting. As a result, for ArcCHECK, most detectors in central areas within ±1.0 cm over 360° arcs are irradiated by entrance dose and the irradiated areas are mainly high dose regions (i.e., no distinct entrance and exit dose regions) (Figure 1 (b)). In contrast, due to its planar geometry, high dose regions are observed at the center of a coronal plane for SRS MapCHECK (Figure 1 (a)). Higher gamma passing rates with SRS MapCHECK would result from the higher spatial resolution and smaller detector size of SRS MapCHECK as discussed above. Since the DCAT plans have relatively homogeneous dose distributions, the difference in volume averaging effects between the 2 devices would not be large. The difference in average passing rates between the 2 devices is 3.10% (99.54% vs. 96.44%) even for the most stringent gamma criteria of 2%/1 mm in this study.
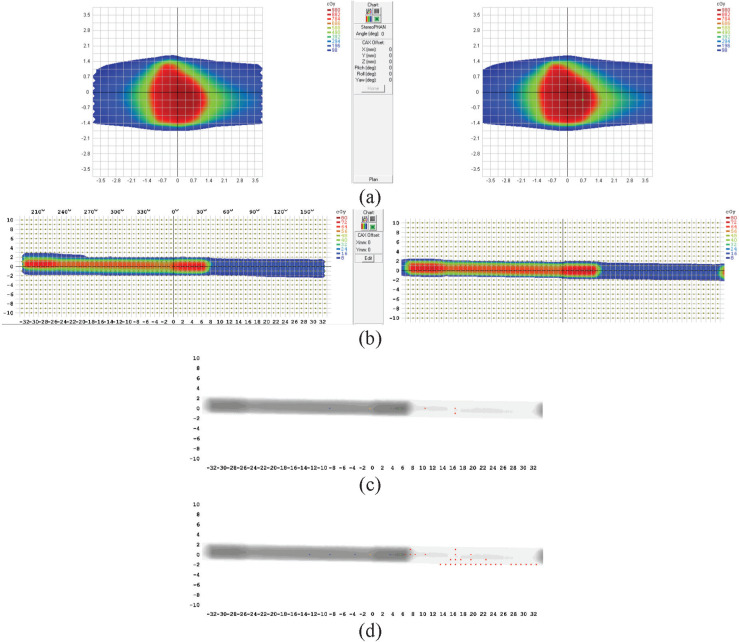
Figure 1.
Results of PSQA for an SRS DCAT plan in Group A performed using (a) SRS MapCHECK and (b) ArcCHECK. Left and right panels in (a) and (b) show measured and calculated dose maps, respectively.
Group B: SRS VMAT
The higher spatial resolution and smaller detector size of SRS MapCHECK improved average gamma passing rates in Group B as well (Table 3). Most patients selected for Group B had arteriovenous malformation and consequently, an irregularly shaped PTV. To conform to the PTV and spare surrounding critical structures (e.g., brainstem), VMAT was used (Figure 2). As mentioned above, VMAT plans have more heterogeneous dose distributions than DCAT plans. As a result, Group B has lower average gamma passing rates than Group A for the same gamma criteria and the same device (Table 3). This trend becomes noticeable for gamma criteria of 2%/1 mm in both QA devices: 99.54% ± 1.71% (Group A) vs. 93.71% ± 4.95% (Group B) for SRS MapCHECK and 96.44% ± 3.56% (Group A) vs. 90.64% ± 5.68% (Group B) for ArcCHECK. For the same reason (i.e., more homogeneous plans in Group A), an average gamma passing rate decreases more gradually as gamma criteria become tighter in Group A than in Group B for both devices.
Figure 2.
Results of PSQA for an SRS VMAT plan in Group B performed using (a) SRS MapCHECK and (b) ArcCHECK. Left and right panels in (a) and (b) show measured and calculated dose maps, respectively.
Group C: SBRT DCAT
The large differences in average gamma passing rates between the 2 devices for gamma criteria of 2%/2 mm (2.40%) and 2%/1 mm (13.61%) are notable. ArcCHECK has a lower spatial resolution and a larger detector size than SRS MapCHECK. However, compared with the results in Group A (SRS DCAT), average gamma passing rates for ArcCHECK in Group C are much lower for gamma criteria of 2%/2 mm (97.60%) and 2%/1 mm (86.39%). In addition, with ArcCHECK, average gamma passing rates for Group D (SBRT VMAT) are higher than those for Group C (SBRT DCAT) for gamma criteria of 2%/2 mm (99.00% vs. 97.60%) and 2%/1 mm (93.60% vs. 86.39%). These results can be explained by the PTV location, arc angles and treatment planning technique. In our institution, DCAT is typically used for lung SBRT when a target is roundly shaped and is located away from centrally located critical structures such as heart and blood vessels (i.e., away from the mediastinum). Partial arc angles (arc size: 180° - 220°) in an ipsilateral lung side are usually chosen to spare the contralateral lung. Due to the partial arcs and planning technique (DCAT, MLCs are always open during beam delivery), distinct high dose regions (entrance dose over 180° - 220°) and low dose regions (exit dose over 140° - 180°) are observed in ArcCHECK PSQA results (Figure 3 (b)). Most of the failing points occurred in low dose regions with gamma criteria of 2%/2 mm and 2%/1 mm (Figure 3 (c) and (d)). This trend is not observed with SRS MapCHECK because of its planar geometry (Figure 3 (a)).
Figure 3.
Results of PSQA for an SBRT DCAT plan in Group C performed using (a) SRS MapCHECK and (b) ArcCHECK. Left and right panels in (a) and (b) show measured and calculated dose maps, respectively. Failing points (blue and red) are shown in ArcCHECK QA analysis with gamma criteria of (c) 2%/2 mm and (d) 2%/1 mm.
The failing points in low dose regions from ArcCHECK QA results in Group C are due to the following reasons. Failing points in low dose regions are commonly observed in IMRT PSQA results. Most of the time, global normalization (i.e., normalization with respect to the maximum point in the reference dose map which is a measured dose map in SNC Patient software) and a threshold would help failing points pass in low dose regions6. In this study, global normalization was used in both devices because SRS MapCHECK software has only one option of global normalization and the American Association of Physicists in Medicine Task Group (AAPM TG) 218 recommends using global normalization for IMRT PSQA6. According to the Sun Nuclear MapCHECK user guide, SNC Patient software includes points at or above the user-defined threshold (e.g., 10%) in either a measured dose map or a TPS calculated dose map, meaning that points below the threshold can be included for comparison and this could lower passing rates. If a QA plan has large low dose regions like in Group C, a probability of having failing points in low dose regions increases. SNC Patient software counts points as “failing” points when the points do not meet both DD and DTA criteria but counts them as “passing” points when they meet either DD or DTA criterion. This concept is not the same as the gamma analysis proposed by Low et al18. As shown in Table 3, changing gamma criteria from 3%/2 mm to 2%/2 mm (i.e., lowering by DD of 1%) lowered an average passing rate by 2.20% (from 99.80% to 97.60%) whereas changing from 2%/2 mm to 2%/1 mm (i.e., lowering by DTA of 1 mm) lowered an average passing rate by 11.21% (from 97.60% to 86.39%). These results imply that there are some failing points which have a dose discrepancy (DD<3%) between measurement and calculation but there are much more failing points which do not satisfy the DTA criterion of 1 mm in low dose regions. The failing points include points in field edges (Figure 3 (d)). The DTA criterion of 1 mm seems to be difficult to achieve even in homogeneous plans. All the plans in Group C have similar patterns (i.e. partial arcs of 180° - 220° and distinct low and high dose regions) and the conclusion drawn for this group seems reasonable. Nonetheless, it is noted that only 12 fields were analyzed in Group C and a larger number of data are required for further investigation.
Group D: SBRT VMAT
As in the other groups, the difference in average gamma passing rates between the 2 devices exists in Group D and the difference is smaller in Group D than in Group C except for gamma criteria of 3%/3 mm. For the same reason (i.e., higher spatial resolution and smaller detector size), average gamma passing rates are higher with SRS MapCHECK. Most targets in Group D were located close to the mediastinum and VMAT was necessary to spare surrounding critical structures. Similar to the plans in Group C, partial arc angles (angle size: 145° - 240°) were chosen to spare the contralateral lung but distinct high and low dose regions are not observed in ArcCHECK PSQA results (Figure 4 (b)) because beams are modulated and MLCs are not widely open as gantry rotates and as a result, low dose regions occurring in an exit dose area do not seem to be as large as those in Group C (Figure 3(b) vs. Figure 4(b)), resulting in less failing points in low dose regions. In the SRS MapCHECK case, on the other hand, Group D has lower average gamma passing rates than Group C for all gamma criteria because plans in Group D are highly modulated. Still, the average passing rate is high (98.38%) for the tightest gamma criteria of 2%/1 mm in this study.
Figure 4.
Results of PSQA for an SBRT VMAT plan in Group D performed using (a) SRS MapCHECK and (b) ArcCHECK. Left and right panels in (a) and (b) show measured and calculated dose maps, respectively.
Dose grid size for SBRT plans: 1 mm × 1 mm versus 2 mm × 2 mm
A smaller dose grid size improves average gamma passing rates in PSQA performed using ArcCHECK (Table 4). In this study, all the QA plans in all 4 groups were calculated with a dose grid size of 1 mm × 1 mm because SRS MapCHECK software requires a dose map calculated with a dose grid size of 1 mm × 1 mm. The Medical Physics Practice guideline 9.a. states that a 1 mm dose grid size in TPS calculations might be necessary for very small targets3. AAPM TG 101 recommends a dose grid size of 2 mm or less for SBRT19. A smaller dose grid size would allow for more accurate dose calculations. As shown in Table 4, average gamma passing rates are higher for a dose grid size of 1 mm × 1 mm. A drawback of using a smaller dose grid size is longer calculation time. The differences in average gamma passing rates between the 2 dose grid sizes are small (0% - 0.88%) in Group C but the differences are larger (0.99% - 6.75%) in Group D. This would be attributed to modulated and more heterogeneous plans in Group D.
Gamma criteria
User defined gamma criteria (DD/DTA) would determine PSQA results and therefore, each clinic should choose proper gamma criteria. AAPM TG 218 recommends gamma criteria of 3%/2 mm with global normalization and a threshold of 10% for IMRT PSQA. The report does not have specific recommendations for SRS and SBRT PSQA but it states that tighter tolerances should be considered6. This study showed that both devices could achieve relatively high passing rates (≥97.6% ± 2.41% for 2%/2 mm and ≥86.36% ± 8.69% for 2%/1 mm) for gamma criteria tighter than 3%/2 mm (Table 3).
In this study, 2D planar and 3D planar gamma analyses were performed for SRS MapCHECK and ArcCHECK, respectively. As discussed in Group C: SBRT DCAT above, in 2D planar gamma analysis, calculated points which satisfy user defined DD/DTA criteria are searched in the selected 2D plane. According to the SNC Patient software reference guide, when “Use 3D Analysis for ArcCHECK” is turned on in Program Preferences, the TPS dose grid is interpolated to 1 mm × 1 mm × 1 mm. In 3D planar gamma analysis, therefore, an extra dimension is used to search for points, resulting in a higher gamma passing rate20,21 and better agreement between measurement and calculation than in 2D planar gamma analysis22. However, a single measurement plane selected for planar (2D or 3D) analysis does not always represent the entire target volume22,23. It has been reported that there is no correlation between planar (2D and 3D) and volumetric 3D gamma passing rates20,23 and there is a lack of correlation between gamma passing rates and DDs in target volumes and organs at risk in PSQA for VMAT24. Therefore, volumetric 3D gamma analysis or DVH-based dose verification which would complement planar gamma analysis could verify more clinically relevant dosimetric accuracy25.
Limitation of this study
The primary limitation of this study is that the TC method recommended by the AAPM TG 218 was not used. In the TC method, a measurement device is on the couch and radiation beams are delivered using the actual treatment parameters such as gantry, collimator, couch angles, jaws, MLC leaf positions and MUs to simulate the treatment delivery to the patient6. In this study, ArcCHECK was placed on the couch and some non-coplanar fields from the clinical SRS plans used in this study caused a collision between gantry and couch. On the other hand, SRS MapCHECK can be placed off the couch to avoid a collision. To keep consistency of PSQA between the 2 devices, in this study, PSQA was performed with a couch angle of 0 degree (co-planar delivery) for all the fields. The AAPM TG 2186 states, “IMRT QA measurements should be performed using the perpendicular field-by-field (PFF) delivery method if the QA device is not suitable for TC measurements or for TC verification error analysis.” The PFF method (i.e., the radiation beam is perpendicular to the plane of the measurement device) was possible with ArcCHECK because of its cylindrical geometry, whereas it was not possible with SRS MapCHECK because SRS MapCHECK cannot be mounted in the gantry. The TC method would be desirable for PSQA for SRS and SBRT treatments and therefore, the results and conclusion drawn in this study might not be accurate when compared with results of PSQA performed using the TC method.
CONCLUSION
This study compared PSQA results between SRS MapCHECK and ArcCHECK for single-lesion SRS and SBRT treatments and showed that average gamma passing rates were higher with SRS MapCHECK for all 4 gamma criteria of 3%/3 mm, 3%/2 mm, 2%/2 mm and 2%/1 mm and for all 4 groups of SRS DCAT, SRS VMAT, SBRT DCAT and SBRT VMAT clinical plans. This result would be due to the higher spatial resolution and smaller detector size of SRS MapCHECK. Based on the limitations of each device and average gamma passing rates that each device could achieve, each clinic/institution should choose the right device and set appropriate gamma criteria for PSQA to deliver SRS and SBRT treatments safely and accurately.
Nomenclature
AAPM: American Association of Physicists in Medicine; DCAT: dynamic conformal arc therapy; DD: dose difference; DTA: distance-to-agreement; DVH: dose volume histogram; IMRT: intensity modulated radiation therapy; MLC: multi leaf collimator; MU: monitor unit; PFF: perpendicular field-by-field; PSQA: patient-specific quality assurance; PTV: planning target volume; QA: quality assurance; SBRT: stereotactic body radiation therapy; SD: standard deviation; SRS: stereotactic radiosurgery; TC: True Composite; TG: task group; TPS: treatment planning system; VMAT: volumetric modulated arc therapy
ACKNOWLEDGMENTS
The authors would like to thank Mr. Zheng Gu for collecting some data.
Footnotes
Authors’ disclosure of potential conflicts of interest
The authors have nothing to disclose.
Author contributions
Conception and design: Yongsook C. Lee and Yongbok Kim
Data collection: Yongsook C. Lee
Data analysis and interpretation: Yongsook C. Lee and Yongbok Kim
Manuscript writing: Yongsook C. Lee
Final approval of manuscript: Yongsook C. Lee and Yongbok Kim
REFERENCES
- 1.Saglam Y, Bolukbasi Y, Atasoy AI, Karakose F, Alpan V, Selek U, Kucuk A, Pehlivan B, Topkan E. Quality assurance in stereotactic radiosurgery and stereotactic body radiotherapy. Advances in Research. 2020;21(7):22-33. [Google Scholar]
- 2.Benedict SH, Cai J, Libby B, Lovelock M, Schlesinger D, Sheng K, Yang W. SRT and SBRT: Current practices for QA dosimetry and 3D.. Journal of Physics: Conference Series. 2010;250:012057. [Google Scholar]
- 3.Halvorsen PH, Cirino E, Das IJ, Garrett JA, Yang J, Yin FF, Fairobent LA. AAPM-RSS Medical Physics Practice Guideline 9.a. for SRS-SBRT.. J Appl Clin Med Phys. 2017;18(5):10-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bruschi A, Esposito M, Pini S, Ghirelli A, Zatelli G, Russo S. How the detector resolution affects the clinical significance of SBRT pre-treatment quality assurance results. Phys Med. 2018;49:129-134. [DOI] [PubMed] [Google Scholar]
- 5.Both S, Alecu IM, Stan AR, Alecu M, Ciura A, Hansen JM, Alecu R. A study to establish reasonable action limits for patient-specific quality assurance in intensity-modulated radiation therapy. J Appl Clin Med Phys. 2007;8(2):1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miften M, Olch A, Mihailidis D, Mihailidis D, Moran J, Pawlicki T, Molineu A, Li H, Wijesooriya K, Shi J, Xia P, Papanikolaou N, Low DA. Tolerance limits and methodologies for IMRT measurement-based verification QA: Recommendations of AAPM Task Group No. 218.. Med Phys. 2018;45(4):e53-e83. [DOI] [PubMed] [Google Scholar]
- 7.Ramachandran P, Tajaldeen A, Taylor D, Wanigaratne D, Roozen K, Geso M. Evaluation and Performance of ArcCheck and Film using Gamma Criteria in Pre-treatment Quality Assurance of Stereotactic Ablative Radiotherapy. J Med Phys. 2017;42(4):251-257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abad D, Ruiz C, Candela-Juan C, Carmona V, Gimeno J, Lliso F, Ballester F, Perez-Calatayud J. Evaluation of ArcCHECK for pretreatment QA of VMAT for very small volumes in SRS and SBRT with FF and FFF beams. Radiother Oncol. 2015;115:S748. [Abstract] [Google Scholar]
- 9.Ezzell G, Foster M. Accuracy of and quality assurance for VMAT-based, single isocenter SRS for multiple targets. Radiother and Oncol. 2018;127:S1216-S1217. [Abstract] [Google Scholar]
- 10.Molinier J, Kerr C, Simeon S, Ailleres N, Charissoux M, Azria D, Fenoglietto P. Comparison of volumetric-modulated arc therapy and dynamic conformal arc treatment planning for cranial stereotactic radiosurgery. J Appl Clin Med Phys. 2016;17(1):92-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stathakis S, Narayanasamy G, Licon AL, Myers P, Li Y, Crownover R, Papanikolaou N. A dosimetric comparison between volumetric-modulated arc therapy and dynamic conformal arc therapy in SBRT. J BUON. 2019;24(2):838-843. [PubMed] [Google Scholar]
- 12.Ahmed S, Zhang G, Moros EG, Feygelman V. Comprehensive evaluation of the high-resolution diode array for SRS dosimetry. J Appl Clin Med Phys. 2019;20(10):13-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rose MS, Tirpak L, Van Casteren K, Zack J, Simon T, Schoenfeld A, Simon W. Multi-institution validation of a new high spatial resolution diode array for SRS and SBRT plan pretreatment quality assurance. Med Phys. 2020;47(7):3153-3164. [DOI] [PubMed] [Google Scholar]
- 14.McCulloch J, Pawlowski J, Kerby N, Rasmussen K, Shi Z, Myers P, Stathakis S, Papanikolaou N, Saenz DL. Patient-specific dose quality assurance of single-isocenter multiple brain metastasis stereotactic radiosurgery using PTV Octavius 4D.. J Appl Clin Med Phys. 2020;21(9):107-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liang B, Zhou F, Yin FF, Wu Q. Comparisons of volumetric modulated arc therapy (VMAT) quality assurance (QA) systems: sensitivity analysis to machine errors. Radiat Oncol. 2016;11:146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Szeverinski P, Kowatsch M, Künzler T, Meinschad M, Clemens P, DeVries AF. Error sensitivity of a log file analysis took compared with a helical diode arry dosimeter for VMAT delivery quality assurance. J Appl Clin Med Phys. 2020;21(11):163-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li G, Bai S, Chen N, Henderson L, Wu K, Xiao J, Zhang Y, Jiang Q, Jiang X. Evaluation of the sensitivity of two 3D diode array dosimetry systems to setup error for quality assurance (QA) of volumetric-modulated arc therapy (VMAT).. J Appl Clin Med Phys. 2013;14(5):13-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Low DA, Harms WB, Mutic S, Purdy JA. A technique for the quantitative evaluation of dose distributions. Med Phys. 1998;25(5):656-661. [DOI] [PubMed] [Google Scholar]
- 19.Benedict SH, Yenice KM, Followill D, Galvin JM, Hinson W, Kavanagh B, Keall P, Lovelock M, Meeks S, Papiez L, Purdie T, Sadagopan R, Schell MC, Salter B, Schlesinger DJ, Shiu AS, Solberg T, Song DY, Stieber V, Timmerman R, Tomé WA, Verellen D, Wang L, Ying FF. Stereotactic body radiation therapy: the report of AAPM Task Group 101.. Med Phys. 2010;37(8):4078-4101. [DOI] [PubMed] [Google Scholar]
- 20.Rajasekaran D, Jeevanandam P, Sukumar P, Ranganathan A, Johnjothi S, Nagarajan V. A study on correlation between 2D and 3D gamma evaluation metrics in patient-specific quality assurance for VMAT. Med Dosim, 2014;39(4):300-309. [DOI] [PubMed] [Google Scholar]
- 21.Zhang D, Wang B, Zhang G, Ma C, Deng X. Comparison of 3D and 2D gamma passing rate criteria for detection sensitivity to IMRT delivery errors. J Appl Clin Med Phys. 2018;19(4):230-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pulliam KB, Huan JY, Howell RM, Followill D, Bosca R, O’Daniel J, Kry SF. Comparison of 2D and 3D gamma analyses. Med Phys. 2014;41(2):021710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim JI, Choi CH, Wu HG, Kim JH, Kim K, Park JM. Correlation analysis between 2D and quasi-3D gamma evaluations for both intensity-modulated radiation therapy and volumetric modulated arc therapy. Oncotarget. 2017;8(3):5449-5459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jin X, Yan H, Han C, Zhou Y, Yi J, Xie C. Correlation between gamma index passing rate and clinical dosimetric difference for pre-treatment 2D and 3D volumetric modulated arc therapy dosimetric verification. Br J Radiol. 2015;88(1047):20140577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Visser R, Wauben DJL, Groot M, Steenbakkers RJHM, Bijl HP, Godart J, Veld AAV, Langendijk JA, Korevaar EW. Evaluation of DVH-based treatment plan verification in addition to gamma passing rates for head and neck IMRT. Radiother Oncol. 2014;112(3):389-395. [DOI] [PubMed] [Google Scholar]