To The Editors
Coronavirus Disease 2019 (COVID-19) has raised clinical and logistical challenges in cardiovascular emergencies management. Medical centers around the world tailored individual preventive measures, regulations and adjustments in order to preserve high standard of care alongside maintaining a safe workplace environment [1,2].
We aimed to characterize different aspects of hospital admissions due to acute coronary syndrome (ACS) in the intensive cardiac care unit during the beginning of COVID-19 outbreak in Israel, compared with the same period the previous year.
Rabin medical center, a tertiary referral center, includes two independent hospitals: Beilinson and Hasharon. During the beginning of COVID-19 outbreak in Israel, these two hospitals were reorganized into a COVID-19 only hospital (Hasharon) and a COVID-19 free hospital (Beilinson). A common emergency department (ED) which was physically located at Beilinson hospital performed the initial triage. Patients diagnosed with COVID-19 in need of further hospital care, were transferred to the COVID-19 hospital.
The study included all consecutive patients who were admitted to Beilinson hospital due to ACS during March to April 2020, the initial COVID-19 outbreak in Israel (COVID-19 cohort), compared with the parallel period in March to April 2019 (pre-COVID-19 cohort). All patients were COVID-19 negative on a PCR test.
Data were collected retrospectively from medical records. The study was approved by the local institutional ethics committee.
Our cohort includes a total of 264 patients admitted with ACS, including 139 patients (mean age 65.4 ± 13.1 years, 75% male) in the COVID-19 cohort and 125 patients (mean age 63.8 ± 12.2 years, 80% male) in the pre-COVID-19 cohort. Patients’ baseline characteristics were similar in both groups. There were no significant differences in the presenting symptoms between the two cohorts. Non-ST-segment elevation myocardial infarction (NSTEMI) was the most frequent diagnosis and ST-segment elevation myocardial infarction (STEMI) was the second most frequent diagnosis, with no difference between the two time periods (for NSTEMI, 43% vs. 41% and for STEMI, 24% vs. 31% during COVID-19 compared with the pre-COVID-19 cohort, respectively, P = 0.50). There was no difference in the median levels of cardiac biomarkers or left ventricular (LV) function. The duration of hospitalization nor the rate of re-hospitalizations at 30 days differed between both time periods.
In a sub-analysis comparing STEMI and NSTEMI patients in the pre-COVID-19 and COVID-19 cohorts, we found no difference in hospitalization course and characteristics.
During the COVID-19 period, there were significantly more patients who presented to the ED ≥24 hours after symptoms onset compared with the pre-COVID-19 period (48% vs. 33%, P = 0.01; Table 1). Moreover, a delayed presentation was significantly more common among NSTEMI patients.
Table 1.
Hospital admission characteristics for ST-segment elevation myocardial infarction vs. non-ST-segment elevation myocardial infarction patients
| COVID-19 | Pre-COVID-19 | P-value for STEMI | P-value for NSTEMI | |||
|---|---|---|---|---|---|---|
| STEMIn = 33 | NSTEMIn = 85 | STEMIn = 39 | NSTEMIn = 69 | |||
| Time from symptoms onset to ED presentation | 0.53 | 0.04 | ||||
| ≤24 hours | 27 (82%) | 40 (47%) | 34 (87%) | 44 (64%) | ||
| >24 hours | 6 (18%) | 45 (53%) | 5 (13%) | 25 (36%) | ||
| Time from first medical contact to angiography (minutes ± SD) | 44.19 ± 44.40 | 1354.42 ± 1353.58 | 56.94 ± 95.94 | 1561.25 ± 2160.9 | 0.49 | 0.49 |
| Time from ED admission to ICCU admission (hours ± SD) | 0.8 ± 1.4 | 5.19 ± 4.06 | 1.35 ± 2.58 | 5.47 ± 4.09 | 0.28 | 0.70 |
| Re-admission in 30 days | 11 (33%) | 18 (21%) | 6 (15%) | 19 (27%) | 0.07 | 0.36 |
COVID-19, Coronavirus Disease 2019; ED, emergency department; ICCU, intensive cardiology care unit; NSTEMI, non-ST-segment elevation myocardial infarction; STEMI, ST-segment elevation myocardial infarction.
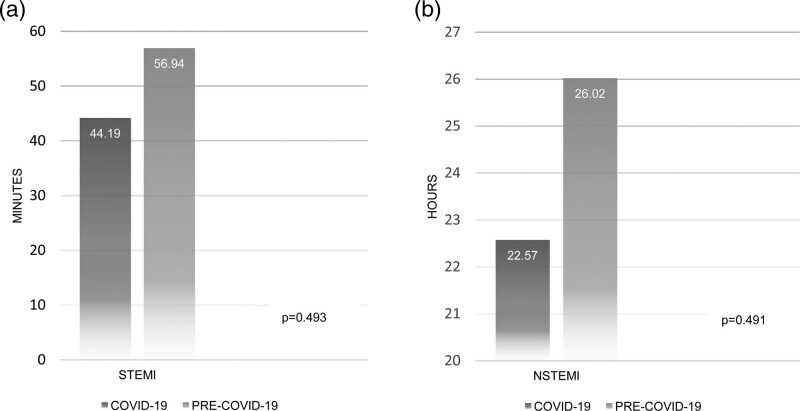
Time from first medical contact to angiography for STEMI was numerically shorter during COVID-19 compared to the pre-COVID-19 period, though not statistically significant (44.2 ± 44.4 minutes vs. 56.9 ± 95.9 minutes, respectively, P = 0.49; Table 1 and Fig. 1).
Fig. 1.
Time from admission to angiography for STEMI (panel a, in minutes) and NSTEMI (panel b, in hours) during COVID-19 compared with pre-COVID-19 period. COVID-19, Coronavirus Disease 2019; NSTEMI, non-ST-segment elevation myocardial infarction; STEMI, ST-segment elevation myocardial infarction.
In contrast with recent publications, we did not observe a significant decline in hospitalization rate for ACS during the beginning of COVID-19 pandemic [3–5]. Being a COVID-19 free hospital may have encouraged patients to seek emergent medical care at our facility. Yet, during the COVID-19 period, our hospital was the main referral enter for cardiac patients, therefore the actual hospitalization rate could not be compared to that of the previous year.
A recent study by Tam et al. [6] reported a four-fold increase in the median time from symptom onset to first medical contact for patients with STEMI and more than two-fold increase in median time from door to device. A similar trend was observed in our cohort mostly attributed to delayed presentation of NSTEMI patients. As previously suggested, we assume this patient-related delay was a result of the ‘Stay Home’ campaign, the temporary lockdown and patients’ fear of contracting COVID-19 in medical facilities.
In contrast, there was no significant delay in diagnosis and treatment as reflected by time from first medical contact to coronary angiography and reperfusion therapy during COVID-19 period compared with pre-COVID-19. There was no difference in the rate of recent MIs, clinical signs of heart failure at presentation and rate of cardiogenic shock in both periods. Moreover, we could not find any difference between the two periods in various parameters for MI severity, such as cardiac biomarkers level, LV systolic function, hospitalization duration or mortality in 30 days. Due to a low event rate in both groups (five deaths during pre-COVID-19 and six during COVID-19 period), we could not explore meaningful differences in the time to event and its significance.
Our study represents a single-centre unique experience that was successful in terms of short-term outcomes. Despite a significant delay in presentation to the hospital during the COVID-19 period, the hospitalization course and outcomes studied were not affected. Despite the challenges imposed by the pandemic, efficient hospital reorganization and adherence to ACS management guidelines should maintain a high level of care without compromising patients’ medical outcomes.
Acknowledgements
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cosentino N, Assanelli E, Merlino L, Mazza M, Bartorelli AL, Marenzi G. An in-hospital pathway for acute coronary syndrome patients during the COVID-19 outbreak: initial experience under real-world suboptimal conditions. Can J Cardiol 2020; 36:961–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Katz JN, Sinha SS, Alviar CL, Dudzinski DM, Gage A, Brusca SB, et al. COVID-19 and disruptive modifications to cardiac critical care delivery: JACC review topic of the week. J Am Coll Cardiol 2020; 76:72–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhatt AS, Moscone A, McElrath EE, Varshney AS, Claggett BL, Bhatt DL, et al. Declines in hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic: a multicenter tertiary care experience. J Am Coll Cardiol 2020; 76:280–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Solomon MD, McNulty EJ, Rana JS, Leong TK, Lee C, Sung SH, et al. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med 2020; 383:691–693. [DOI] [PubMed] [Google Scholar]
- 5.Mesnier J, Cottin Y, Coste P, Ferrari E, Schiele F, Lemesle G, et al. Hospital admissions for acute myocardial infarction before and after lockdown according to regional prevalence of COVID-19 and patient profile. SSRN Electron J 2020; 5:e536–e542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tam CCF, Cheung KS, Lam S, Wong A, Yung A, Sze M, et al. Impact of Coronavirus Disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes 2020; 13:e006631. [DOI] [PMC free article] [PubMed] [Google Scholar]