Abstract
Background
During the coronavirus disease 2019 (COVID-19) pandemic period, the use of emergency services with pediatric non-COVID patients has decreased considerably. We aimed to examine whether there was a change in the demographic data, triage profile, causes, management, and cost of pediatric emergency department (PED) visits of non-COVID patients during the pandemic period.
Methods
This study was a retrospective, single-center, observational comparative study that was conducted at the PED. Patient records were examined during “the pandemic spring” and the same period of the previous year. Patient demographics, waiting time, and outcome of the PED visit were analyzed in the entire population of children admitted to the PED during the study period, whereas more precise data such as the reason for PED use, duration of symptoms, urgency levels according to the Emergency Severity Index (ESI), final diagnosis, management, and cost of patient care were analyzed in a sample of admitted patients. We used the chi-square test, Fisher's exact test, and Mann–Whitney U test for statistical analyses.
Results
A total of 62,593 PED visits occurred. During the pandemic period, PED visits showed a decrease of 55.8% compared to the previous year. Patients included in the sampling study group were selected using a systematic random sampling method. The median waiting time during the pandemic period was significantly shorter than the previous year (median 14 min [IQR: 5–32] vs. median 5 min [IQR: 2–16]; p<0.001). The median duration of symptoms was 1 day (1–2) in both groups. Emergency Severity Index (ESI) levels I, II, and III showed a significant increase (27.7% vs. 37.3%) in triage scoring compared to levels IV and V (72.3% vs. 62.7%) during the pandemic period (p<0.001). The median cost per patient during the pandemic period was statistically higher compared to the previous year ($19.57 [19.57–40.50] vs. $25.34 [31.50–52.01]; p<0.001). Overall costs during the pandemic period had a 1.6-fold decline.
Conclusion
We highlighted the changes in an ordinary PED profile during an extraordinary period. A shift in ESI levels in a more emergent direction was observed. While the number of nonurgent patients, especially those with infections, decreased, the rates of surgical cases, acute neurological and heart diseases, home accidents, and poisoning increased relative to the pre-pandemic period.
Keywords: COVID-19, Pandemic, Pediatric, Emergency
1. Introduction
In the spring of 2020, the coronavirus disease 2019 (COVID-19) pandemic peaked in Turkey. The first case of COVID-19 in Turkey was confirmed on March 11, 2020. The virus quickly spread throughout the country. During the spring 2020 pandemic period, the number of new cases per day increased to a peak on April 11 (13,976) and decreased to 2282 on May 31, ending the spring season with a total of 445,931 cases and 4540 deaths [1]. Lockdown was implemented on weekends and public holidays with healthcare strategies put in place. On March 16, educational institutions and day-care centers across the country closed. In addition, a curfew was imposed for people under the age of 20 from April 3 to June 10. In keeping with the policy of “stay at home” to prevent the spread of COVID-19, hospital outpatient visits were restricted. However, easy access to pediatric emergency departments (PEDs) was provided [2].
Today, it is well known that COVID-19 causes mild disease in children and rarely has a serious presentation. It is noteworthy that during the pandemic period, the use of emergency services with pediatric non-COVID patients decreased considerably [3]. This fact requires caution, as children may not be able to reach hospitals and there may be a risk of death in children with non-COVID. In many emergency centers, children and adults with suspected infections share a common isolation area [4]. The reduced visits may be due to anxiety about being infected at the hospital, a desire to obey the “stay at home” instructions, or delays in seeking medical care [5,6]. Following these measures, a significant reduction in airborne or fecal–oral infectious diseases was observed [7,8]. All these theories may be explained by comparing admissions during the pandemic with admissions during previous periods. There have been numerous reports recently about pediatric non-COVID patients who need emergency care [3,4,[6], [7], [8], [9], [10]]. However, to date there is no comprehensive study comparing the pandemic period with the pre-pandemic period in terms of PED visits.
The aim of this study was to evaluate the demographic data, triage profiles, causes, management, and cost of PED visits of non-COVID patients during the pandemic period.
2. Methods
2.1. Study design
This study was a retrospective, single-center, observational comparative study that was conducted at a PED of a tertiary children's hospital. In 2019, a total of 203,921 patients visited the PED. Our center is one of the largest children's hospitals in Turkey, and it served as a reference pediatric center for non-COVID patients during the pandemic period. Electronic medical records of patients visiting the PED were reviewed between March 1, 2020 and May 31, 2020, and between March 1, 2019 and May 31, 2019. Patient demographics, waiting time, and outcome of the PED visit were evaluated for all the children admitted to the PED during two study periods, retrospectively, from electronic hospital information systems. For feasibility reasons, more precise data were extracted from a sample of this entire population. The volume of PED visits was recorded daily.
2.2. Sampling design
The patients were chosen using a systematic random sampling method. The fifth patient who visited the PED was randomly selected as a starting point, and then the medical record of every 10th patient (5th, 15th, 25th etc.) was reserved. A list with patient names and registration numbers was compiled. All medical records selected were examined in detail. Inclusion was subject to the availability of the medical records in electronic hospital information systems. The exclusion criteria for this study were patients 18 years of age or older, insufficient data, and clinical information in the selected medical record. Among the medical records of these patients, 4341 records from the previous spring and 1919 records from the pandemic spring were selected for the study by systematic randomized sampling methods. The reason for PED use, time from symptom onset to hospital arrival, urgency level, final diagnosis, management, and cost of patient care were obtained. To measure the severity of the visit, we used the Emergency Severity Index (ESI), which is a proxy measure of how long a patient can safely wait for medical screening examination and treatment. The ESI is a five-level triage system that uses an algorithm with rankings from level I (most urgent) to level V (least urgent) [11]. This triage system was recorded by evaluating patients' clinical status, patients' vital signs, and the need to use resources. The cost of patient care included the costs incurred from the time of the patient's examination in the PED until he or she was discharged home. If the patient was hospitalized, this hospitalization was also included in the cost. The overall cost was calculated by multiplying the mean cost per patient by the total number of patients. This study received the approval of the local ethical committee.
2.3. Statistical analysis
The data were analyzed using the Statistical Package for Social Sciences (SPSS) v.20.0 for Windows. Continuous and categorical variables are reported using (median [interquartile range, IQR]) and number (%), respectively. Categorical data were examined using the chi-square test or Fisher's exact test. The Mann–Whitney U test was employed to compare the average values of the two groups (the 2019 study group vs. the 2020 study group). All p-values were two-tailed, and group differences with p<0.05 were considered to be statistically significant.
3. Results
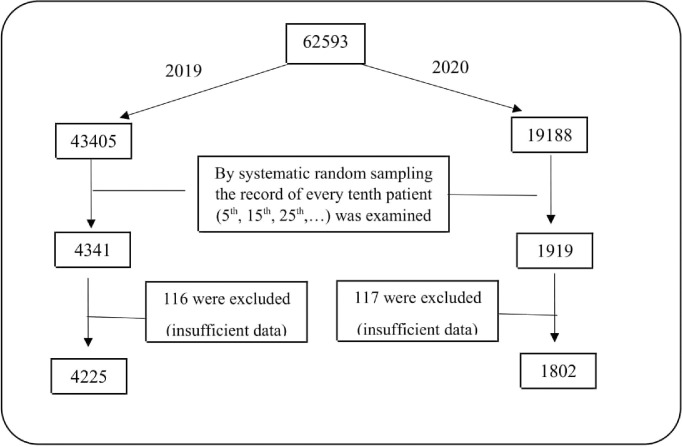
During the study period, a total of 62,593 PED visits occurred, with 43,405 during spring 2019 and 19,188 patients during the “pandemic spring” of 2020. Using a systematic randomized sampling method, among 4341 and 1919 records, 116 and 117 patients were excluded from the medical records due to lack of sufficient data or because of their age, respectively. The remaining 4225 and 1802 patients were enrolled in the sampling groups of this study. The chart of the study is shown in Fig. 1 .
Fig. 1.
Study flowchart.
There is a response rate of 96.13% and a sampling of 9.62%.
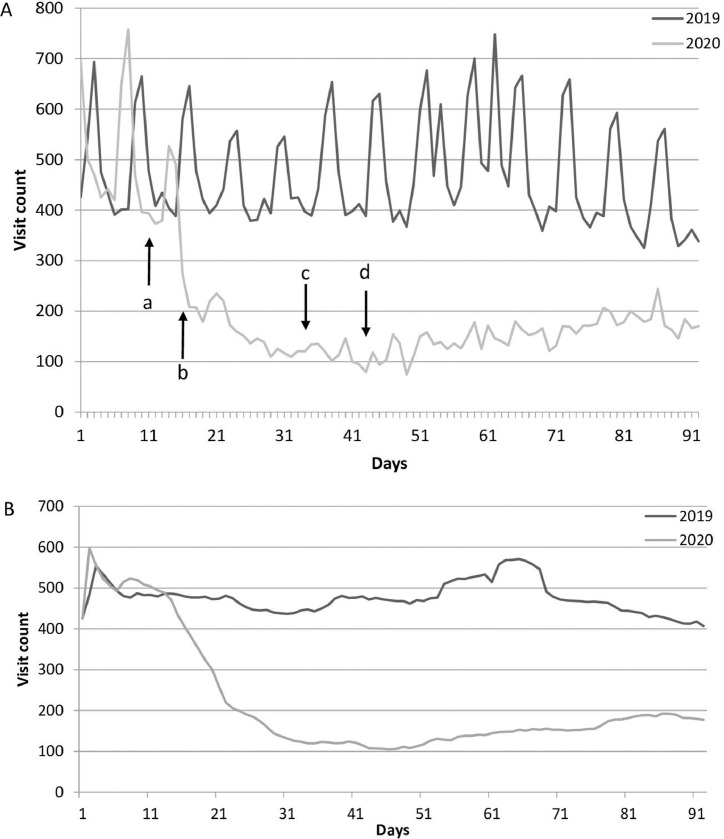
During the pandemic period, PED visits decreased by 55.8% compared to the previous year. Visits decreased drastically on the 16th day of the study period (day of school closure). This was 5 days after the first confirmed COVID-19 case; in total, 47 confirmed cases had been reported in total in Turkey by that day. The decrease in visits continued in the following days (Fig. 2 ). The number of visits decreased to the lowest level on April 11 (the 43rd day of the study), which is when the daily number of positive cases peaked in our country. Despite the gradual increase over the following days, it always remained lower than the lowest level of the previous year. The weekly moving average was also used to smooth out the fluctuations caused by weekend crowds.
Fig. 2.
Number of patients who visited the pediatric emergency department. A: Number of patients who visited the pediatric emergency department between March 1 and May 31, 2020 and the same period of the previous year (a. The first day of a confirmed case of COVID in Turkey. b. The first day that educational institutions and daycare centers closed. c. The first day of a curfew imposed for those under the age of 20. d. The day when the number of positive cases peaked in Turkey). B: Weekly moving average of the data.
3.1. Description and comparison of populations
Based on the results of the main groups, the median waiting time during the previous year was 14 min (IQR: 5–32), versus a median waiting time of 5 min (IQR: 2-16) for the pandemic period (p<0.001). The outcome of the PED visit was different between the two periods (p<0.001), with a smaller proportion of children being discharged in the pandemic period. The characteristics of the two main groups are shown in Table 1 .
Table. 1.
Demographical characteristics, waiting time percentiles, and outcome of PED visit during the two study periods.
| Study period |
|||
|---|---|---|---|
| Variables | 2019 | 2020 | p |
| Patient visits, n (%) | 43405 (69.34) | 19188 (30.66) | |
| Gender, n (%) [95% CI] | 0.029 | ||
| Male | 23314 (53.7) [53.2–54.2] | 10125 (52.8) [52.1–53.5] | |
| Female | 20091 (46.3) [45.8–46.8] | 9063 (47.2) [46.5–47.9] | |
| Age (months)[median (IQR)] | 42 (14–83) | 43 (12–100) | <0.001 |
| Nationality, n (%) [95% CI] | <0.001 | ||
| Turkish | 42256 (97.4) [97.2–97.5] | 18367 (95.7) [95.4–96.0] | |
| Others | 1149 (2.6) [2.5–2.8] | 821 (4.3) [4.0–4.6] | |
| Waiting time (min) Percentiles |
|||
| 5th | 1 | 0 | |
| 10th | 2 | 1 | |
| 25th | 5 | 2 | |
| 50th | 14 | 5 | |
| 75th | 32 | 16 | |
| 90th | 53 | 47 | |
| 95th | 68 | 67 | |
| Outcome, n (%) [95% CI] | <0.001 | ||
| Discharge home | 39151 (90.2) [89.9–90.5] | 16159 (84.2) [83.7–84.7] | |
| Admission | |||
| PED | 1933 (4.5) [4.3–4.6] | 918 (4.8) [4.5–5.1–] | |
| General wards | 1970 (4.5) [4.3–4.7] | 1771 (9.2) [8.8–9.6] | |
| PICU | 350 (0.8) [0.7–0.9] | 340 (1.8) [1.6–2.0] | |
| Death* | 8 (0.018) [0.006–0.031] | 3 (0.016) [-0.002–0.033] | |
IQR: interquartile range; CI: confidence interval; PED: pediatric emergency department; PICU: pediatric intensive care unit.
In the first 48 h.
3.2. Description and comparison of the sampling populations
According to the sampling group data, the median duration of symptoms was 1 day (IQR: 1–2) in both groups with a difference in mean rank (2936.12 for the previous period and 3112.79 for the pandemic period) (Supplemental Fig. S1). The distribution rates of the diagnoses during the visit periods varied. During the pandemic period, surgical diseases, home accidents, and poisoning were relatively more common than the rates of other diagnoses. All types of infections decreased.
ESI levels I, II, and III showed a significant increase (27.7% vs. 37.3%) in triage scoring compared to levels IV and V (72.3% vs. 62.7%) during the pandemic period (p<0.001). The median cost per patient during the pandemic period was statistically higher compared to the previous year ($19.57 [IQR: 19.57–40.50) vs. $25.34 [IQR: 31.50–52.01]; p<0.001). However, overall costs during the pandemic and the same period in the previous year were $418,000 and $681,970, respectively. A comparison of detailed data from patient medical records for the sampling groups is presented in Table 2 .
Table. 2.
Details of emergency visits for the two periods.
| Study period |
|||
|---|---|---|---|
| Variables | 2019 | 2020 | p |
| Patient visits, n (%) (by systematic sampling) | 4225 (70.10) | 1802 (29.90) | |
| Duration of symptoms (days) [median (IQR)] | 1 (1–2) | 1 [1–2] | <0.001 |
| Acute exacerbation of a chronic disease, n (%) [95% CI] | 95 (2.2) [1.8–2.7] | 51 (2.8) [2.1–3.6] | 0.20 |
| Final diagnosis, n (%) [95% CI] | < 0.001* | ||
| Infections | 3282 (77.7) [76.4–78.9] | 1190 (66.0) [63.9–68.2] | |
| URI | 2044 52.7 (51.1–54.2] | 690 (57.3) [55.2–60.8] | |
| LRI | 373 (11.4) [10.3–12.5] | 173 (14.5) [12.5–16.5] | |
| Fever without focus | 17 (0.5) [0.3–0.8] | 5 (0.4) [0.1–0.8] | |
| Acute gastroenteritis | 445 (13.6) [12.4–14.7] | 132 (11.1) [9.3–12.9] | |
| UTI | 93 (2.8) [2.3–3.4] | 33 (2.8) [1.8–3.7] | |
| Others | 308 (9.4) [8.4–10.4] | 171 (14.4) [12.4–16.4] | |
| Gastroenterological disease | 238 (5.6) [4.9–6.3] | 173 (9.6) [8.2–11] | |
| Allergic diseases | 117 (2.8) [2.3–3.3] | 55 (3.1) [2.3–3.8] | |
| Neurologic disease | 75 (1.8) [1.4–2.2] | 45 (2.5) [1.8–3.2] | |
| Surgery | 48 (1.1) [0.8–1.5] | 59 (3.3) [2.5–4.1] | |
| Endocrine diseases | 30 (0.7) [0.5–1] | 7 (0.4) [0.1–0.7] | |
| Renal diseases | 30 (0.7) [0.5–1] | 12 (0.7) [0.3–1] | |
| Cardiologic disease | 28 (0.7) [0.4–0.9] | 17 (0.9) [0.5–1.4] | |
| Poisoning | 19 (0.4) [0.2–0.7] | 10 (0.6) [0.2–0.9] | |
| Home accidents | 16 (0.4) [0.2–0.6] | 20 (1.1) [0.6–1.6] | |
| Metabolic diseases | 13 (0.3) [0.2–0.5] | 11 (0.6) [0.3–1] | |
| Psychiatric disorders | 5 (0.1) [0–0.2] | 5 (0.3) [0–0.5] | |
| Oncologic diseases | 3 (0.1) [0–0.2] | 1 (0.1) [–0.1–0.2] | |
| Other causes | 167 (4.0) [3.4–4.5] | 122 (6.8) [5.6–7.9] | |
| Healthy | 150 (3.6) [3–4.1) | 75 (4.2) [3.2–5.1) | |
| ESI, n (%) [95% CI] | < 0.001⁎⁎ | ||
| Level I | 2 (0.0) [0–0.1] | 1 (0.1) [–0.1–0.2] | |
| Level II | 82 (1.9) [1.5–2.4] | 41 (2.3) [1.6–3] | |
| Level III | 1087 (25.7) [24.4–27] | 630 (35.0) [32.8–37.2] | |
| Level IV | 1021 (24.2) [22.9–25.5] | 372 (20.6) [18.8–22.5] | |
| Level V | 2033 (48.1) [46.6–49.6] | 758 (42.1) [39.8–44.3] | |
| Cost per patient ($) [median (IQR)] |
19.57 (19.57–40.50) | 25,34 (31.50–52.01) | < 0.001 |
IQR: interquartile range; CI: confidence interval; URI: upper respiratory infection; LRI: lower respiratory infection; UTI: urinary tract infection.
Infectious disease vs. noninfectious diseases.
ESI level I, II and III vs. ESI level IV and V.
While the proportions of abdominal pain, ingestions, chest pain, and acute problems of infancy increased during the pandemic period, a decrease was found in nonspecific symptoms such as respiratory symptoms, fever, sore throat, diarrhea, vomiting, and headache. There was no change in nonurgent uses of the PED such as urinary catheter insertion, tracheostomy cannula replacement, or follow-up of patients needing palliative care (Table 3 ).
Table. 3.
Comparison of frequencies of reasons for visit for the two periods.
| Reasons for PED visits | 2019 n (%) | 2020 n (%) |
|---|---|---|
| Respiratory symptoms | 1932 (45.72) | 645 (35.79) |
| Fever | 1720 (40.70) | 648 (35.96) |
| Vomiting | 657 (15.55) | 210 (11.65) |
| Sore throat, earache | 603 (14.270) | 202 (11.21) |
| Diarrhea | 426 (10.08) | 145 (8.05) |
| Nonurgent use* | 395 (9.35) | 179 (9.93) |
| Abdominal pain | 277 (6.55) | 133 (7.38) |
| Problems in infancy | 132 (3.12) | 81 (4.5) |
| Hemorrhage | 64 (1.51) | 18 (1.00) |
| Headache | 53 (1.25) | 19 (1.05) |
| Seizure | 50 (1.38) | 36 (2.00) |
| Ingestion | 37 (0.88) | 23 (1.28) |
| Chest pain | 30 (0.71) | 27 (1.5) |
| Others | 634 (15.00) | 333 (18.48) |
PED: pediatric emergency department.
Urinary catheter insertion, tracheostomy cannula replacement, or follow-up of patients needing palliative care etc.
4. Discussion
In this study we evaluated the use of emergency services during the pandemic. During this period, the number of visits to the PED decreased by nearly 60%. The median waiting time in the PED was found to have decreased by threefold and twofold for 50% and 75% of patients, respectively. Significant decreases in the number of emergency room admissions have also been reported in other studies [12,13]. Reducing waiting time is often an important goal in PED reorganization and a significant metric that is monitored by health authorities [14]. The reduction in waiting time for more than half the visits was considered to be an important factor in the present study. Anxiety about becoming infected in the hospital and obedience to “stay at home” and the resulting reduction in infections may explain this drop in visits. Unlike adult emergency services, the decrease in the number of people in the PED during the pandemic period provided a comfortable working opportunity for pediatric emergency physicians. However, this situation should be carefully examined in terms of reluctance to go to the hospital, delayed diagnosis, and development of serious conditions.
In the pandemic period, there was a marked reduction in infections. Human parainfluenza virus, respiratory syncytial virus, and human rhinoviruses are the most common viral pathogens in the spring season in Turkey, and these infections bring children to the hospital by causing the common cold and acute bronchiolitis [15]. Close contact in community settings such as schools and day-care centers makes them ideal locations for the spread of viral infections [16]. The most important reason for the low number of emergency visits may be the lack of circulation of these spring pathogens due to restrictions, school closures, and the use of face masks and disinfection [7,8]. We believe these factors may have protected children from infections due to seasonal viruses. It has also been reported that the pandemic virus can replace normal seasonal viruses due to its high initial susceptibility and basic reproduction number [17,18].
During the pandemic period, while infectious diseases decreased considerably, the proportions of surgical cases and acute neurological and heart diseases increased relative to the pre-pandemic period. This may be explained by “real emergencies” that cannot be resolved by waiting at home. The increase in home accidents and poisoning was also remarkable. During the containment periods and as a result of anxiety about becoming infected, the number of exposures to chlorine and the amount of unproven medication use increased [19]. A significant increase in home accidents was reported in children during the school holidays, when they spent more time at home [20]. Reduced supervision and neglect may also have led to poisoning and other dangers and risks of injuries in children [21].
There was an approximately 10% shift in ESI levels toward more emergent levels (from level IV or V to level I, II, or III; p<0.001). During the pandemic period, there was a significant increase in the proportion of admission to hospital (p<0.001). This may be due to patients with minor disease who decreased their PED visits or avoided visiting altogether, while those with more severe conditions did not. Among all visits, the high admission rates and higher-acuity ESI levels were thought to be signs of effective use of the PED. Despite the increase in the median cost per patient, the total financial burden to the hospital decreased significantly.
4.1. Strengths and limitations
This study was a comprehensive study conducted in a tertiary pediatric hospital providing emergency care to nearly 200,000 patients annually during regular periods, and it served as a reference pediatric center for non-COVID patients during the pandemic period. Since a systematic random sampling method was used, the potential for bias in the information and the risk of favoritism were reduced. The data collected were more likely to be an authentic representation of the entire demographic.
The results of this study, however, should be interpreted taking into consideration the limitations. First, it was based on data from a single center; therefore, the conclusions may not reflect the profile of all emergency services. Second, it shows only the first 3 months of the epidemic. The third limitation is the lack of assessment of the evolution of other infections before and during the pandemic. Since the study was designed retrospectively, evaluation could only be made based on the data in the medical records.
5. Conclusion
This study is a snapshot of the functioning of pediatric emergency departments around the world during the pandemic and lockdown. During the pandemic period, waiting time decreased, and ESI levels shifted toward more emergency levels. More suitable medical care was provided for a reasonable number of patients and patients in need. While the number of nonurgent patients, especially those with infections, decreased, the rates of surgical cases, acute neurological and heart diseases, home accidents, and poisoning increased relative to the pre-pandemic period.
E-Component:
Supplemental Fig. S1. Distribution of duration of symptoms.
Declaration of Competing Interest
None.
Sources of funding
None.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.arcped.2021.09.014.
Appendix. Supplementary materials
References
- 1.Worldometer coronavirus. [Internet]. https://www.worldometers.info/coronavirus/country/turkey/. [Accessed 23.07. 2020 ].
- 2.Centers of Disease Control and Prevention (CDC). What to Do If You Are Sick Updated May 8, 2020 [Internet] https://www.worldometers.info/coronavirus/country/turkey/. [Accessed 23.07.2020].
- 3.Tartara F, Cofano F, Zenga F, et al. Are we forgetting non-COVID-19-related diseases during lockdown? Acta Neurochir (Wien) 2020;7:1. doi: 10.1007/s00701-020-04385-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choudhary B, Goyal JP. Management concern for Non-COVID children during the COVID pandemic. Indian Pediatr. 2020;57:591. doi: 10.1007/s13312-020-1874-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yuan R, Xu QH, Xia CC, et al. Psychological status of parents of hospitalized children during the COVID-19 epidemic in China. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Appleby J. What is happening to non-COVID deaths? BMJ. 2020;369:m1607. doi: 10.1136/bmj.m1607. [DOI] [PubMed] [Google Scholar]
- 7.Angoulvant F, Ouldali N, Yang DD, et al. COVID-19 pandemic: impact caused by school closure and national lockdown on pediatric visits and admissions for viral and non-viral infections, a time series analysis. Clin Infect Dis. 2020;72:319–322. doi: 10.1093/cid/ciaa710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parry MF, Shah AK, Sestovic M, et al. Precipitous fall in common respiratory viral infections during COVID-19. Open Forum Infect Dis. 2020;7:1–4. doi: 10.1093/ofid/ofaa511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gopal DP. Non-COVID-19 general practice and our response to the pandemic. BJGP Open. 2020;4 doi: 10.3399/bjgpopen20X101095. bjgpopen20X1010952020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Messac L, Knopov A, Horton M. Delayed care-seeking for non-COVID illnesses in Rhode Island. R I Med J. 2020;103:10–11. [PubMed] [Google Scholar]
- 11.Gilboy N, Tanabe P, Travers D, et al. Emergency severity index (ESI): a triage tool for emergency department care, version 4. Schaumburg, Implementation Handbook. 2020 https://www.ena.org/docs/default-source/education-document-library/esi-implementation-handbook-2020.pdf?sfvrsn=fdc327df_2 Edition. Accessed 6 July 2020. [Google Scholar]
- 12.Pines JM, Zocchi MS, Black BS, et al. Characterizing pediatric emergency department visits during the COVID-19 pandemic. Am J Emerg Med. 2021;41:201–204. doi: 10.1016/j.ajem.2020.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Raucci U, Musolino AM, Di Lallo D, et al. Impact of the COVID-19 pandemic on the emergency department of a tertiary children's hospital. Ital J Pediatr. 2021;47:21. doi: 10.1186/s13052-021-00976-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Drouin O, D'Angelo A, Gravel J. Impact of wait time during a first pediatric emergency room visit on likelihood of revisit in the next year. Am J Emerg Med. 2020;38:890–894. doi: 10.1016/j.ajem.2019.07.005. [DOI] [PubMed] [Google Scholar]
- 15.Aykaç K, Karadağ-Öncel E, Bayhan C, et al. Prevalence and seasonal distribution of viral etiology of respiratory tract infections in inpatients and outpatients of the pediatric population: 10 year follow-up. Turk J Pediatr. 2018;60:642–652. doi: 10.24953/turkjped.2018.06.004. [DOI] [PubMed] [Google Scholar]
- 16.Barker J, Stevens D, Bloomfield SF. Spread and prevention of some common viral infections in community facilities and domestic homes. J Appl Microbiol. 2001;91:7–21. doi: 10.1046/j.1365-2672.2001.01364.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Furuse Y, Oshitani H. Mechanisms of replacement of circulating viruses by seasonal and pandemic influenza A viruses. Int J Infect Dis. 2016;51:6–14. doi: 10.1016/j.ijid.2016.08.012. [DOI] [PubMed] [Google Scholar]
- 18.Olsen SJ, Azziz-Baumgartner E, Budd AP, et al. Decreased influenza activity during the COVID-19 pandemic — United States, Australia, Chile, and South Africa, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1305–1309. doi: 10.15585/mmwr.mm6937a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Le Roux G, Sinno-Tellier S. French poison control centre members, Descatha A. COVID-19: home poisoning through out the containment period. Lancet Public Health. 2020;5:e314. doi: 10.1016/S2468-2667(20)30095-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Al Rumhi A, Al Awisi H, Al Buwaiqi M, et al. Home accidents among children: a retrospective study at a tertiary care center in Oman. Oman Med J. 2020;35:e85. doi: 10.5001/omj.2020.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.CDC COVID-19 Response Team Severe outcomes among patients with coronavirus disease 2019 (COVID-19)-United States. MMWR Morb Mortal Wkly Rep. 2020;69:343–346. doi: 10.15585/mmwr.mm6912e2. February 12-March 16, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.