Abstract
Objectives
During the last quarter of 2020—despite improved distribution of personal protective equipment (PPE) and knowledge of COVID-19 management—nursing homes experienced the greatest increases in cases and deaths since the pandemic's beginning. We sought to update COVID-19 estimates of cases, hospitalization, and mortality and to evaluate the association of potentially modifiable facility-level infection control factors on odds and magnitude of COVID-19 cases, hospitalizations, and deaths in nursing homes during the third surge of the pandemic.
Design
Cross-sectional analysis.
Setting and Participants
Facility-level data from 13,156 US nursing home facilities.
Methods
Two series of multivariable logistic regression and generalized linear models to examine the association of infection control factors (personal protective equipment and staffing) on incidence and magnitude, respectively, of confirmed COVID-19 cases, hospitalizations, and deaths in nursing home residents reported in the last quarter of 2020.
Results
Nursing homes experienced steep increases in COVID-19 cases, hospitalizations, and deaths during the final quarter of 2020. Four-fifths (80.51%; n = 10,592) of facilities reported at least 1 COVID-19 case, 49.44% (n = 6504) reported at least 1 hospitalization, and 49.76% (n = 6546) reported at least 1 death during this third surge. N95 mask shortages were associated with increased odds of at least 1 COVID-19 case [odds ratio (OR) 1.21, 95% confidence interval (CI) 1.05-1.40] and hospitalization (1.26, 95% CI 1.13-1.40), as well as larger numbers of hospitalizations (1.11, 95% CI 1.02-1.20). Nursing aide shortages were associated with lower odds of at least 1 COVID-19 death (1.23, 95% CI 1.12-1.34) and higher hospitalizations (1.09, 95% CI 1.01-1.17). The number of nursing hours per resident per day was largely insignificant across all outcomes. Of note, smaller (<50-bed) and midsized (50- to 150-bed) facilities had lower odds yet higher magnitude of all COVID outcomes. Bed occupancy rates >75% increased odds of experiencing a COVID-19 case (1.48, 95% CI 1.35-1.62) or death (1.25, 95% CI 1.17-1.34).
Conclusions and Implications
Adequate staffing and PPE—along with reduced occupancy and smaller facilities—mitigate incidence and magnitude of COVID-19 cases and sequelae. Addressing shortcomings in these factors is critical to the prevention of infections and adverse health consequences of a next surge among vulnerable nursing home residents.
Keywords: COVID-19, nursing home, long-term care
The novel coronavirus (COVID-19) pandemic has disproportionately affected nursing home residents.1 , 2 According to the US Department of Health and Human Services, 2 in 5 Medicare beneficiaries in nursing homes were diagnosed with COVID-19 in 2020, and all-cause mortality in nursing homes increased from 17% to 22% from 2019 to 2020.3 As of the week starting August 16, 2021, the Centers for Medicare & Medicaid Services (CMS) data confirm 134,463 COVID-related nursing home resident deaths,4 accounting for 27% of total US COVID-19 deaths,5 and by the end of 2020, 94% of nursing homes had experienced more than 1 outbreak.6 During the “third surge” (October 2020–January 2021), nursing homes experienced significant and unprecedented rises in cases and deaths, even as distribution of PPE and collective knowledge of managing serious COVID-19 symptoms improved.7, 8, 9 The collection of factors that drove COVID-19 penetration and spread in nursing homes has been under increased scrutiny.
A limited body of literature suggests nursing home residents’ older age, frailty, multiple comorbidities, and declining immune function place them at risk for COVID-19 complications, including viral-induced respiratory failure and multisystem involvement.2 , 10 As a congregate care setting, the nursing home itself heightens risk of infection and adverse events because of close quarters and frequent interaction with and close proximity to staff and other residents.10, 11, 12 As well, staff turnover and infection control equipment shortages may exacerbate COVID-19 spread.10 , 13 , 14 In prior research, higher staffing levels were consistently associated with fewer cases and deaths.15, 16, 17, 18, 19
Other characteristics that have been found to increase risk of COVID-19 infection and deaths in nursing homes include large facility size,15 , 16 , 20 , 21 high percentage of nonwhite residents,14 , 15 , 17 , 18 , 20 , 22, 23, 24 lack of staff unionization,25 and urban location.15 , 20 , 24 Medicaid share,15 , 17 , 18 , 20 , 21 quality ratings,15 , 16 , 18 , 20 , 23 and for-profit status15 , 16 , 20 , 21 , 23 show mixed results. For instance, some studies suggest high Medicaid-share facilities are associated with increased cases17 , 18 and deaths,21 whereas others show no significant differences.15 , 20 Although not examined in nursing homes, evidence on the potential for influenza vaccinations to protect against COVID-19 infection is conflicting, with studies suggesting influenza vaccination is associated with lower COVID-19 infection26 , 27 and others suggesting the opposite.28
Studies to date have largely focused on the second and third quarters of 2020,14 , 16 , 17 , 19 , 23 , 25 and few have examined factors related to COVID-19 hospitalization19 or the magnitude of infection outbreaks,20 hospitalizations, and deaths. The only study measuring COVID-19 outbreak size in nursing homes found facilities with <50 beds had larger outbreaks per bed as of May 2020.20 No recent studies have considered whether more widely disseminated PPE and other mitigation efforts reduced infection rates and outcomes. In this study, we sought to evaluate the associations of facility-level infection control factors on the odds and magnitude of COVID-19 cases, hospitalizations, and deaths in the nursing home population during the pandemic's “third surge.” We focus the discussion on those factors that are “potentially modifiable” such as PPE availability.
Methods
Data Sources
Using the facility-level Federal Provider Identification number, we linked the Centers for Medicare & Medicaid Services (CMS) Nursing Home COVID-19 Public File4 with 3 databases: (1) Nursing Home Compare (NHC)29; (2) Long-Term Care: Facts on Care in the US (LTCFocus)30; and (3) The New York Times (NYT) county-level files of COVID-19 cases and deaths.31 We examined nursing homes during the last quarter of 2020 (the week beginning September 28, 2020, through the week ending December 27, 2020). The CMS COVID-19 file includes counts of COVID-19 outcomes and nursing facility variables such as staff and personal protective equipment (PPE) shortages, total beds, and occupancy rates.4 The NHC data regularly tracks nursing home organizational characteristics and quality of care, including influenza vaccination rates.29 The LTCFocus data provides facility-level sociodemographic and clinical characteristics.30 The New York Times national data provides information on county-level geographic variation in general population COVID-19 infections and deaths.31
Primary Outcomes
Primary outcomes assessed during the final quarter of 2020 included any incident and confirmed COVID-19 cases, hospitalizations, and deaths. Within facilities with at least 1 confirmed COVID-19 case, hospitalization, or death, respectively, we estimated the following secondary outcomes: the magnitude of COVID-19 cases, hospitalizations, and deaths. These were calculated as the total number of each specific COVID-19 outcome divided by the number of occupied beds in a facility.20
Independent Variables and Covariates
We focused on 3 potentially modifiable independent variables relevant to infection control: 1-week supply of N95 masks (yes/no) and shortages of nursing home aides (yes/no) at baseline, and adjusted total nursing staff hours (≥4.1 hours or <4.1 hours per resident per day) from 2017 LTCFocus.32 We further adjusted for covariates deemed important in relevant literature14 , 18 , 20 , 23 , 25: facility size (<50, 50-150, >150 beds) and occupancy level (≥75% or <75%) measured from the study period baseline week beginning September 28; and annual influenza vaccination rates (≥90% or <90% of residents vaccinated) as of 2020 quarter 2.33 Other data from LTCFocus at the facility level including profit status and chain affiliation, as well as sociodemographic characteristics of residents [average age; proportion of nonwhite residents (>25% or ≥25%); proportion of Medicaid (>85% or ≤85%)20; acuity of care (average Resource Utilization Groups Nursing Case Mix Index [RUGs NMCI])], were also included. For the baseline week of September 28, surrounding county-level COVID-19 case rates were computed by dividing county-level non–nursing home COVID-19–related cases by 2019 population estimates from the US Census Bureau, and surrounding county-level COVID-19 death rates were computed by dividing county-level non–nursing home COVID-19–related deaths by county-level COVID-19 cases for the same week.34
Statistical Analysis
We used chi-square and t tests to compare baseline demographic and clinical characteristics between nursing facilities that had any COVID-19 cases vs those that had none. For each outcome, we fit 2 models because of the large number of facilities that did not report a single incident of a respective outcome during the final quarter of 2020. First, multivariable logistic regression models were used to quantify the odds of having (1) any COVID-19 case, (2) any hospitalization, and (3) any death in a nursing home. These findings estimate the relationship between facility characteristics and any penetration of COVID-19 in nursing homes. Among facilities with at least 1 confirmed COVID-19 case, COVID-19–related hospitalization, and/or death, we then ran separate generalized linear models with a log link, assuming a gamma distribution, to quantify the association between nursing home facility characteristics on COVID-19 outbreak size, reported as relative risk ratios (RRRs). These results provide estimates of the relationship between facility characteristics and outbreak size relative to the number of occupied beds in a nursing home. Choice of distribution and link functions were dictated by the nature of the outcomes (ie, non-negative, continuous, right skewed), visual and statistical inspection, and minimization of Akaike information criterion. Statistical analyses were performed with SAS Studio, version 3.71. The institutional review board exempted this study.
Results
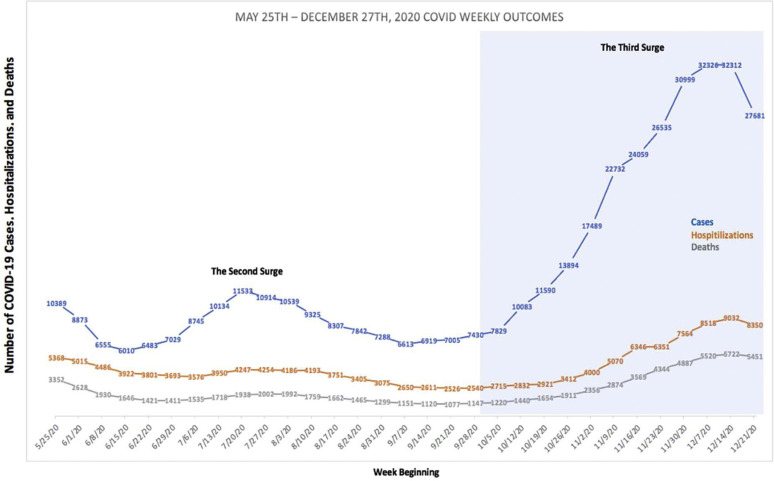
Of 15,392 nursing homes linked across all 3 data sources, 2236 were excluded because of missing covariate information, resulting in a final study sample of 13,156 nursing homes. Figure 1 illustrates weekly incident COVID-19 confirmed cases, hospitalizations, and deaths during the entire period such data were collected until wide-scale vaccination distribution (week starting May 25, 2020, through week ending December 27, 2020). Marked increases in all 3 outcomes occurred during the third surge, with COVID-19 cases, hospitalizations, and deaths peaking the week beginning December 14, 2020. That week, reports of cases (n = 32,312) and deaths (n = 5722) were nearly triple those of the peaks of the second surge (July 2020) for cases (n = 11,533) and deaths (n = 2002).
Fig. 1.
National trends in COVID-19 nursing home cases, hospitalizations, and deaths from May 25, 2020, to December 27, 2020.
Characteristics of Nursing Homes With and Without COVID-19 Cases
Compared to nursing homes with no reported COVID-19 cases, facilities with at least 1 COVID-19 case were more likely to report N95 mask shortages and provide fewer than 4.1 total nurse staffing hours per resident per day (Table 1 ). Facilities with at least 1 case were also more likely to be larger facilities, have higher occupancy rates, and have lower proportions of nonwhite and Medicaid-covered residents. In addition, nursing homes with COVID-19 cases had higher proportions of high-acuity patients and were more likely to be chain affiliated. The rates of COVID-19 cases in nursing homes reflected COVID-19 case rates in surrounding communities. The mean county COVID-19 case rates per 100,000 citizens were 108.8 (SD = 107) for nursing homes with any COVID-19 cases and 91.6 (SD = 101) for nursing homes with no COVID-19 cases.
Table 1.
Baseline Nursing Home Characteristics (N = 13,156)
| Variable Name (at Facility Level) | All NHs, n (Col %) (n = 13,156) |
NHs With COVID-19 Cases, n (Col %) (n = 10,592) |
NHs Without COVID-19 Cases, n (Col %) (n = 2564) |
|---|---|---|---|
| Average age, mean (SD) | 79.5 (6.9) | 79.5 (6.7)∗ | 79.2 (7.3)∗ |
| Proportion nonwhite | |||
| ≤25% | 9128 (69.4) | 7457 (70.4)∗ | 1671 (65.2)∗ |
| >25% | 4028 (30.6) | 3135 (29.6)∗ | 893 (34.8)∗ |
| Proportion Medicaid | |||
| ≤85% | 11,922 (90.6) | 9706 (91.6)∗ | 2216 (86.4)∗ |
| >85% | 1234 (9.4) | 886 (8.4)∗ | 348 (13.6)∗ |
| Clinical characteristics of residents | |||
| Average RUGs NCMI, mean (SD)† | 1.17 (0.17) | 1.18 (0.16)∗ | 1.17 (0.19)∗ |
| Influenza vaccination rate | |||
| <90% | 1157 (8.8) | 950 (9.0) | 207 (8.1) |
| ≥90% | 11,999 (91.2) | 9642 (91.0) | 2357 (91.9) |
| Adjusted total nurse staffing hours | |||
| <4.1 h/resident per day | 9291 (70.6) | 7556 (71.3)∗ | 1735 (67.7)∗ |
| ≥4.1 h/resident per day | 3865 (29.4) | 3036 (28.7)∗ | 829 (32.3)∗ |
| For-profit status | 3899 (29.6) | 3122 (29.5) | 777 (30.3) |
| Not for profit | 9257 (70.4) | 7470 (70.5) | 1787 (69.7) |
| Chain facility | 12,733 (96.8) | 10,283 (97.1)∗ | 2450 (95.6)∗ |
| Not a chain | 423 (3.2) | 309 (2.9)∗ | 114 (4.4)∗ |
| Size of facility (total number of beds) | |||
| Small (<50 beds) | 1243 (9.4) | 795 (7.5)∗ | 448 (17.5)∗ |
| Medium (50-150 beds) | 9804 (74.5) | 7932 (74.9)∗ | 1872 (73.0)∗ |
| Large (>150 beds) | 2109 (16.0) | 1865 (17.6)∗ | 244 (9.5)∗ |
| Shortage of 1-week supply of N95 masks | 1603 (12.4) | 1347 (13.0)∗ | 256 (10.3)∗ |
| No shortage | 11,290 (87.6) | 9052 (87.0)∗ | 2238 (89.7)∗ |
| Shortage of aides | 2472 (19.2) | 1982 (19.1) | 490 (19.6) |
| No shortage | 10,421 (80.8) | 8417 (80.9) | 2004 (80.4) |
| Occupancy rate (occupied beds/total bed) | |||
| <75% occupied | 6935 (52.7) | 5452 (51.5)∗ | 1483 (57.8)∗ |
| ≥75% occupied | 6221 (47.3) | 5140 (48.5)∗ | 1081 (42.2)∗ |
| County COVID-19 case rate (rate per 100,000 individuals), mean (SD)‡ | 105.5 (106) | 108.8 (107)∗ | 91.6 (101)∗ |
| County COVID-19 death rate (rate per 100,000 cases), mean (SD)‡ | 1789.72 (5171.77) | 1736.58 (5030.75)∗ | 2009.24 (5713.43)∗ |
COVID-19, coronavirus disease 2019; NHs, nursing homes; RUGs NCMI, Resource Utilization Groups Nursing Case Mix Index.
Confidence intervals that do not cross 1 indicate a statistically significant estimate at an alpha level of 0.05.
Statistical significance (P < .05).
Score that measures the average acuity of residents based on the amount of nursing and therapy time required to provide care. The higher the NCMI score, the more severe the average acuity profile of the residents in a facility (0 = residents are independent).
County COVID-19 case and death rates per 100,000 individuals (excluding cases and deaths among nursing home residents) based on data from the New York Times and US Census Bureau the week of September 28, 2020.
Odds of Having at Least 1 COVID-19 Case, Hospitalization, or Death per Facility
Four-fifths (80.51%; n = 10,592) of nursing homes reported at least 1 COVID-19 case, 49.44% (n = 6504) reported at least 1 hospitalization, and 49.76% (n = 6546) reported at least 1 death during the study period (data not shown). Table 2 reflects findings from the fully adjusted models. N95 mask shortages were associated with 1.21 [95% confidence interval (CI) 1.05-1.40] the odds of a case compared with no shortages. Aide shortages and nursing hours were not statistically significant factors. In addition, bed occupancy rates ≥75% (1.48, 95% CI 1.35-1.62), facilities with higher acuity residents (1.51, 95% CI 1.15-1.99), and chain status (1.13, 95% CI 1.03-1.24) were associated with increased odds of at least 1 COVID-19 case. Facilities with higher proportions of nonwhite residents (0.74, 95% CI 0.66-0.82) and high Medicaid share (0.65, 95% CI 0.56-0.75) had lower odds of at least 1 case.
Table 2.
Multivariable Adjusted Odds of Any COVID-19 Case, Hospitalization, and Death in US Nursing Homes (N = 13,156)
| Variable name (at facility level) | Probability of Any Case, Adjusted OR (95% CI) |
Probability of Any Hospitalization, Adjusted OR (95% CI) |
Probability of Any Death, Adjusted OR (95% CI) |
|---|---|---|---|
| Shortage of 1-wk supply of N95 masks | 1.214 (1.053-1.400)∗ | 1.259 (1.132-1.399)∗ | 1.037 (0.932-1.153) |
| Shortage of aides | 0.924 (0.825-1.034) | 0.991 (0.906-1.083) | 1.225 (1.120-1.339)∗ |
| Adjusted total nurse staffing hours ≥4.1 h (reference <4.1 h) | 0.964 (0.869-1.069) | 0.963 (0.887-1.045) | 0.831 (0.765-0.903)∗ |
| Influenza vaccination rate <90% (reference ≥90%) | 1.145 (0.974-1.346) | 1.108 (0.980-1.254) | 1.064 (0.939-1.204) |
| Average age | 1.002 (0.994-1.010) | 1.008 (1.002-1.014)∗ | 1.017 (1.011-1.024)∗ |
| Proportion nonwhite ≥25% (reference <25%) | 0.736 (0.662-0.817)∗ | 0.979 (0.900-1.066) | 0.603 (0.553-0.657)∗ |
| Proportion primary Medicaid ≥85% (reference <85%) | 0.648 (0.556-0.754)∗ | 0.755 (0.662-0.862)∗ | 0.713 (0.623-0.817)∗ |
| Average RUGs NCMI† | 1.511 (1.150-1.985)∗ | 1.201 (0.967-1.491) | 0.821 (0.654-1.031) |
| For-profit status | 1.009 (0.906-1.124) | 1.087 (0.999-1.184) | 0.940 (0.863-1.024) |
| Chain facility | 1.133 (1.032-1.244)∗ | 0.980 (0.911-1.055) | 1.116 (1.036-1.202)∗ |
| Size of facility (reference >150 beds) | |||
| <50 beds | 0.170 (0.141-0.206)∗ | 0.327 (0.281-0.381)∗ | 0.341 (0.293-0.397)∗ |
| 50-150 bed | 0.473 (0.409-0.548)∗ | 0.602 (0.546-0.664)∗ | 0.637 (0.578-0.704)∗ |
| Occupancy rate ≥75% (occupied beds/total bed) (reference <75% occupied) |
1.481 (1.352-1.621)∗ | 0.985 (0.918-1.056) | 1.252 (1.167-1.344)∗ |
| Weekly county case rate‡ | 1.003 (1.002-1.003)∗ | 1.001 (1.001-1.002)∗ | n/a |
| Weekly county death rate‡ | n/a | n/a | 1.0 (1.000-1.000) |
COVID-19, coronavirus disease 2019; NHs, nursing homes; RUGs NCMI, Resource Utilization Groups Nursing Case Mix Index.
Confidence intervals that do not cross 1 indicate a statistically significant estimate at an alpha level of 0.05.
Statistical significance (P < .05).
Score that measures the average acuity of residents based on the amount of nursing and therapy time required to provide care. The higher the NCMI score, the more severe the average acuity profile of the residents in a facility (0 = residents are independent).
County COVID-19 case and death rates per 100,000 individuals (excluding cases and deaths among nursing home residents) based on data from the New York Times and US Census Bureau the week of September 28, 2020.
N95 mask shortages were the primary factor associated with increased odds of a facility having at least 1 COVID-19–related hospitalization (1.26, 95% CI 1.13-1.40). Neither nursing hours nor aide shortages were associated with likelihood of a COVID-19 case. Small-sized (OR = 0.33, 95% CI 0.28-0.38) and mid-sized (0.60, 95% CI 0.55-0.66) facilities had lower odds of hospitalization, as did facilities with a higher Medicaid resident share (0.75, 95% CI 0.66-0.86).
Nursing aide shortages (1.23, 95% CI 1.12-1.34) increased the odds of at least 1 COVID-19–related death, while mask shortages were not associated. Conversely, facilities providing higher nursing hours per resident per day (0.83, 95% CI 0.76-0.90) exhibited a protective effect on odds of COVID-19–related death. Bed occupancy rates exceeding 75% (1.25, 95% CI 1.17-1.34), higher mean resident age (1.02, 95% CI 1.01-1.02), and chain affiliation (1.12, 95% CI 1.04-1.20) also increased odds of death. Other factors associated with lower odds of COVID-19–related mortality included high proportion of nonwhite residents (0.60, 95% CI 0.55-0.66) and high Medicaid-covered resident share (0.71, 95% CI 0.62-0.82).
Magnitude of COVID-19 Cases, Hospitalizations, and Deaths
Nursing homes with at least 1 confirmed COVID-19 case had an average of 23.24 (SD = 24.74) cases, whereas those with at least 1 hospitalization had a mean (SD) of 9.17 (17.89) hospitalizations, and those with at least 1 death related to COVID-19 had a mean (SD) of 6.02 (6.52) deaths (data not shown). Mean (SD) magnitude of outcomes was 2.59 (2.58) cases, 0.99 (2.05) hospitalizations, and 0.72 (0.99) deaths (data not shown).
Table 3 displays results from the generalized linear models. N95 mask shortages were associated with an 11% higher number of hospitalizations compared to no mask shortages (1.11, 95% CI 1.02-1.20). Nursing aide shortages were associated with lower case and death outbreaks, but more hospitalizations (1.09, 95% CI 1.01-1.17). Higher adjusted total nursing staff hours (≥4.1 hours per resident per day) were associated with 21% more cases (1.21, 95% CI 1.15-1.27) and 11% more deaths (1.11, 95% CI 1.05-1.17), but showed no significant association with number of hospitalizations.
Table 3.
Factors Associated With Outbreak Size of COVID-19 Cases, Hospitalizations, and Deaths, in US Nursing Homes (N = 13,156)
| Variable Name (at Facility Level) | Adjusted Outbreak Size of Cases (95% CI) | Adjusted Outbreak Size of Hospitalization (95% CI) | Adjusted Outbreak Size of Deaths (95% CI) |
|---|---|---|---|
| Number of nursing homes | n = 10,592 | n = 6504 | n = 10,656 |
| Shortage of 1-wk supply of N95 masks | 1.038 (0.976-1.104) | 1.107 (1.013-1.170)∗ | 1.065 (0.996-1.139) |
| Shortage of aides | 0.922 (0.875-0.973)∗ | 1.089 (1.013-1.170)∗ | 0.894 (0.845-0.945)∗ |
| Adjusted total nurse staffing hours ≥4.1 h (reference <4.1 h) | 1.205 (1.147-1.265)∗ | 0.969 (0.906-1.036) | 1.110 (1.051-1.172)∗ |
| Influenza vaccination rate <90% (reference ≥90%) | 0.993 (0.924-1.068) | 1.227 (1.114-1.352)∗ | 0.985 (0.909-1.067) |
| Average age | 0.999 (0.995-1.003) | 0.990 (0.984-0.995)∗ | 1.015 (1.010-1.020)∗ |
| Proportion nonwhite ≥25% (reference <25%) | 0.690 (0.656-0.725)∗ | 1.102 (1.031-1.179)∗ | 0.696 (0.657-0.737)∗ |
| Proportion primary Medicaid ≥85% (reference <85%) | 1.125 (1.036-1.220)∗ | 1.301 (1.163-1.454)∗ | 1.128 (1.026-1.240)∗ |
| Average RUGs NCMI† | 0.653 (0.570-0.749)∗ | 1.656 (1.332-2.060)∗ | 0.544 (0.462-0.640)∗ |
| For-profit status | 0.879 (0.837-0.924)∗ | 0.899 (0.841-0.961)∗ | 0.957 (0.907-1.009) |
| Chain facility | 0.951 (0.910-0.993)∗ | 0.898 (0.847-0.952)∗ | 0.968 (0.923-1.015) |
| Size of facility (reference >150 beds) | |||
| <50 beds | 1.736 (1.582-1.905)∗ | 1.403 (1.231-1.599)∗ | 2.129 (1.923-2.357)∗ |
| 50-150 bed | 1.448 (1.371-1.530)∗ | 1.167 (1.086-1.254)∗ | 1.514 (1.427-1.606)∗ |
| Weekly county case rate‡ | 1.001 (1.001-1.001)∗ | 1.000 (1.000-1.001)∗ | n/a |
| Weekly county death rate‡ | n/a | n/a | 1.000 (1.000-1.000) |
COVID-19, coronavirus disease 2019; NHs, nursing homes; RUGs NCMI, Resource Utilization Groups Nursing Case Mix Index.
Confidence intervals that do not cross 1 indicate a statistically significant estimate at an alpha level of 0.05.
Statistical significance (P < .05).
Score that measures the average acuity of residents based on the amount of nursing and therapy time required to provide care. The higher the NCMI score, the more severe the average acuity profile of the residents in a facility (0 = residents are independent).
County COVID-19 case and death rates per 100,000 individuals (excluding cases and deaths among nursing home residents) based on data from the New York Times and US Census Bureau the week of September 28, 2020.
Smaller facilities exhibited higher magnitudes of cases, hospitalizations, and deaths compared with larger facilities. Nursing homes with high proportions of Medicaid residents experienced higher numbers of cases (13%), hospitalizations (30%), and deaths (13%) relative to facilities with <85% Medicaid residents.
Although nursing homes with ≥25% nonwhite populations showed fewer COVID-19 cases (0.69, 95% CI 0.66-0.73) and deaths (0.70, 95% CI 0.66-0.74), they experienced higher hospitalization numbers (1.10, 95% CI 1.03-1.18). Lower influenza vaccination rates were associated with a 23% higher number of hospitalizations (1.23, 95% CI 1.11-1.35), though not a higher number of cases or deaths. Finally, high-acuity facilities were associated with fewer COVID-19 cases (0.65, 95% CI 0.57-0.75) and deaths (0.54, 95% CI 0.46-0.64) but 66% more hospitalizations (1.66, 95% CI 1.33-2.06), compared to facilities with less frail residents.
Discussion
Our study of more than 13,000 US nursing homes—representing 85% of all Medicare and Medicaid facilities—highlights the multifaceted challenges encountered in preventing COVID-19–related cases, hospitalizations, and mortality during the third surge of the pandemic spanning October 2020 to December 2020. Although understanding and treatment of COVID-19 has evolved as the pandemic progressed,7 , 8 shortages in PPE and staff remained problematic during the third surge. Specifically, shortages of N95 masks were associated with increased odds of at least 1 COVID-19 case or hospitalization in our study. The magnitude of hospitalizations also were associated with N95 shortages, further demonstrating that inadequate masking persistently contributed to increased COVID-19 spread and severity.
Likewise, nursing aide shortages were associated with increased odds of any COVID-19 hospitalization or death, as well as the size of hospitalizations. However, facilities with nursing aide shortages also experienced significantly fewer cases and deaths, potentially because they may have been more likely to hospitalize residents because of their inability to provide necessary intensive support. In turn, this may have helped slow viral spread while reducing mortality as a greater number of residents with COVID-19 infection received more intensive care at the hospital.
Finally, a complementary staffing measure—nurse hours per resident day—further demonstrates the competing staffing challenges faced by nursing facilities. Higher daily nursing hours per resident was associated with higher numbers of cases and deaths, perhaps indicating a resident population with greater frailty and comorbidity burden known to increase risk of symptomatic COVID-19 and related death.10 , 35 Additionally, the more frequently staff interact with residents and in greater proximity, the higher the transmission risk. Although resident vulnerability may inform findings related to increased staff hours, the significant challenge of balancing increased resident needs with the safety of both residents and staff in trying to contain COVID-19 within facilities cannot be overemphasized.
These unintended consequences should not overshadow the reality that staff shortages necessitate interaction with more residents by the remaining staff members and demonstrate a key mechanism of risk for COVID-19 spread. The pandemic brought long overdue attention to the plight and excessive burden placed on nursing home staff, who often work overtime and at multiple facilities to compensate for often “unlivable” wages.36 , 37 Beyond the implications of exacerbating potential for COVID-19 transmission by staff traveling between facilities, suboptimal working conditions are likely to contribute to staff stress and fatigue, which, in turn, may contribute to breached infection control protocols, thereby further exacerbating COVID-19 penetration and proliferation within and between facilities.
Similar to findings reported by research conducted in the early months of the pandemic,16 , 20 , 21 larger-capacity nursing homes had increased odds of all COVID-19 outcomes. This is likely due to the increased exposure risk as more residents and required staff in larger facilities engage in greater numbers and at higher frequency. Consistent with prior literature,20 however, we found larger facilities experienced smaller relative outbreaks. Nursing homes with more beds (regardless of whether they are occupied or not) may be able to more effectively isolate residents with COVID-19 and implement social distancing among residents and staff. Higher occupancy rates, however, increased odds of cases or deaths, likely owing to difficulty in providing better social distancing measures. Taken together, these findings further illustrate the environmental challenges faced by nursing homes in preventing COVID-19 spread.
Our findings that nursing facilities with higher proportions of nonwhite residents had lower cases and deaths vary from most studies conducted early in the pandemic that found such facilities fared worse than those with lower nonwhite resident proportions.14 , 17 , 18 , 20 , 22 , 23 One potential explanation underlying our discrepant finding is that the last surge markedly differed from earlier periods with respect to the facility demographics as the pandemic migrated toward the less racially diverse midwestern and central states in the latter half of 2020.38 Consistent with our findings, Gorges et al14 found a less pronounced marginal effect of racial and ethnic makeup in nursing homes on COVID-19 deaths; and a recent resident-level analysis found an increased risk of COVID-19 hospitalizations for nonwhite residents (Black, Hispanic, Asian American), whereas increased mortality risk was only found in Asian Americans.19 These results complement our finding that facilities with greater proportions of nonwhite residents experienced larger outbreaks of hospitalizations but not deaths.
In multiple instances, correlates of COVID-19–related hospitalizations were different than correlates of cases and deaths. Numerous mechanisms, several of which we were unable to measure, may be distinctly informing hospitalizations. These unmeasured factors may include staff turnover and reductions, limited resident-staff interactions due to COVID-19 precautions such as resident quarantine, severity progression, clinician or family discretion, and/or variability in triaging protocols of patients to the hospital.19
Although related literature is sparse regarding the role of influenza vaccination in mitigating COVID-19 outcomes,26, 27, 28 we found influenza vaccination not significantly associated with any outcomes except for hospitalization outbreak size. These findings may be due to our vaccination measure that had little heterogeneity (91.2% of facilities provide >90% vaccination to residents). Our findings also emphasize how characteristics that contribute to having at least 1 COVID-19 outcome may have a different association with the magnitude of those outcomes. For example, higher Medicaid share facilities had significantly lower odds of any COVID-19 case, hospitalization, or death, but larger numbers of cases, hospitalizations, and deaths compared with lower Medicaid share facilities. Finally, echoing prior literature, surrounding county-level case saturation informed nursing home COVID-19 rates and outcomes,14 , 19 , 39 which underscores the challenge of mitigating infectious disease spread in nursing homes situated within communities experiencing high rates of infection.
This study is not without limitations. Because this analysis is cross-sectional, the estimates of association may not be causal; additionally, the use of facility- rather than resident-level characteristics limits our ability to generalize beyond the facility level. Further, although the 2017 LTCFocus data set may not reflect current facility patient and staff mix, it remains the most current publicly available data that are uniformly used by other researchers in the field.14 , 17 , 18 , 20, 21, 22, 23, 24, 25 Because of the high missingness of reporting of covariates such as percentage of Black and Hispanic patients, these data points were not included in our study. We did not account for the time-varying nature of staffing and PPE shortage covariates in our models; rather, these variables were adjusted at baseline. Finally, we excluded nursing homes with any missing variables of interest; thus, our findings of more than 85% of available nursing homes may not be generalizable to all facilities. In addition, we did not control for prior counts of COVID-19 outcomes in our analysis owing to (1) the transience of residency in nursing homes, which has only been exacerbated by COVID-19, and because (2) the extent and durability of protection conferred by a prior COVID infection is still unknown, especially among vulnerable nursing home residents. Finally, although we did incorporate resident Resource Utilization Groups into both our analytic models, we did not have important information regarding staff case mix with respect to their relevant health status and comorbidities. Such information, in addition to information related to vaccination status, is important to incorporate in any future analyses.
Our research has notable strengths. First, our study uses multiple data sets during the dire third surge of the COVID-19 pandemic to examine those most vulnerable to adverse consequences—nursing home residents. Second, these data provide multiple facility-level and modifiable factors related to resident, staffing, and facility characteristics, including occupancy and influenza vaccination rates, which were seldom included in prior research. Third, this research uses more current data and assesses infection and outcomes until COVID-19 vaccination became widely established.40 Finally, our study investigates how nursing home factors influence not only resident COVID-19 cases and deaths but also hospitalizations.
Our findings have important implications for preventive measures and management of COVID-19 outcomes in nursing home settings. Although facility-level determinants of COVID-19 cases and outcomes are complex and multifactorial, modifiable factors such as staffing and PPE supported mitigation of COVID-19 spread. We also found that risk factors for cases and outcomes differed over time. Thus, policy makers and stakeholders should take an agile approach when designing public health intervention strategies. Key factors, such as N95 and staff shortages, are important modifiable risk factors that can—and must—be addressed to prevent COVID-19 penetration and spread in nursing homes in subsequent surges. Indeed, nursing facilities facing PPE and/or staff shortages, as well as larger facilities and/or those with high occupancy rates, should carefully review and revise current protocols to effectively prevent and contain COVID-19 outbreaks. Finally, future research is needed to evaluate the impact of staff and resident COVID-19 vaccination in conjunction with these modifiable risk factors on the prevention of future COVID-19 surges.
Conclusions and Implications
Our study found numerous, potentially modifiable characteristics associated with COVID-19 cases, hospitalizations, and deaths in the latter stage of the pandemic. Our findings largely align with current understandings of COVID-19 risk and outcomes in nursing homes, especially in regard to factors important to the mitigation of COVID-19. Other findings, however, such as those related to the association between racial composition and COVID-19, may differ from the narrative informed by earlier periods of the pandemic. As well, many factors that place facilities at risk for any COVID-19 case, hospitalization, or death may differ from those that contribute to increased magnitude of these outcomes. What remains apparent is that more than half a year into the pandemic—as knowledge of social distancing practices, infection prevention, and treatment became established and availability of PPE increased—nursing home facilities experienced the highest rates of infection, morbidity, and mortality, which were largely preventable through relatively simple interventions. Adequate high-quality interventions provide significant returns to nursing home resident health; their lack of availability and adoption late in the pandemic provides cause for alarm for future outbreaks.
Footnotes
This work was supported in kind by the University of Maryland, Baltimore. This research did not receive any specific grants from funding agencies in the commercial or not-for-profit sectors. S.F. is funded by an NIAT32 AG00262. A.W. was supported through a HEOR Fellowship sponsored by Novartis. L.S.-W. receives salary support through the National Institute on Aging1R01AG060939. D.M.Q. is funded as an ICTR KL2 Scholar from the University of Maryland Baltimore Institute for Clinical and Translational Research (1UL1TR003098-01). The funding sources had no role in any aspect of the design, method, data analysis and preparation of the manuscript.
The authors declare no conflicts of interest.
References
- 1.Cerullo M., Gibson Kate. COVID-19 again tearing through nursing homes, as death toll rises. 2020. https://www.cbsnews.com/news/nursing-homes-covid-vulnerability/ Available at: Accessed December 29, 2020.
- 2.Stockman F., Richtel M. “They’re death pits”: Virus claims at least 7,000 lives in U.S. nursing homes. 2020. https://www.nytimes.com/2020/04/17/us/coronavirus-nursing-homes.html Available at: Accessed December 29, 2020.
- 3.Office of Inspector General, U.S. Department of Health & Human Services COVID-19 had a devastating impact on Medicare beneficiaries in nursing homes during 2020. 2021. https://oig.hhs.gov/oei/reports/OEI-02-20-00490.asp#.YNKqKKGmhrg.gmail Available at: Accessed June 23, 2021.
- 4.Centers for Medicare & Medicaid Services COVID-19 nursing home data. 2021. https://data.cms.gov/covid-19/covid-19-nursing-home-data Available at: Accessed September 2, 2020. [PubMed]
- 5.Coronavirus (COVID-19) Deaths. Our world in data. 2021. https://ourworldindata.org/covid-deaths?country=∼USA#daily-confirmed-deaths-per-million-people Available at: Accessed June 2, 2021.
- 6.U.S. Government Accountability Office COVID-19 in nursing homes: Most homes had multiple outbreaks and weeks of sustained transmission from May 2020 through January 2021. 2021. https://www.gao.gov/products/gao-21-367 Available at: Accessed June 1, 2021.
- 7.Centers for Disease Control and Prevention Interim clinical guidance for management of patients with confirmed coronavirus disease (COVID-19) 2021. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html Available at: Accessed April 14, 2021.
- 8.National Institutes of Health Coronavirus disease 2019 (COVID-19) treatment guidelines. 2021. https://www.covid19treatmentguidelines.nih.gov/ Available at: Accessed May 18, 2021. [PubMed]
- 9.Centers for Disease Control and Prevention Trends in number of COVID-19 cases and deaths in the US reported to CDC, by state/territory. https://covid.cdc.gov/covid-data-tracker/#trends_dailytrendscases Available at: Accessed April 14, 2021.
- 10.Perrotta F., Corbi G., Mazzeo G., et al. COVID-19 and the elderly: Insights into pathogenesis and clinical decision-making. Aging Clin Exp Res. 2020;32:1599–1608. doi: 10.1007/s40520-020-01631-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fulop T., Pawelec G., Castle S., Loeb M. Immunosenescence and vaccination in nursing home residents. Clin Infect Dis. 2009;48:443–448. doi: 10.1086/596475. [DOI] [PubMed] [Google Scholar]
- 12.Brown K.A., Jones A., Daneman N., et al. Association between nursing home crowding and COVID-19 infection and mortality in Ontario, Canada. JAMA Intern Med. 2021;181:229–236. doi: 10.1001/jamainternmed.2020.6466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Travers J., Herzig C.T.A., Pogorzelska-Maziarz M., et al. Perceived barriers to infection prevention and control for nursing home certified nursing assistants: A qualitative study. Geriatr Nurs. 2015;36:355–360. doi: 10.1016/j.gerinurse.2015.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gorges R.J., Konetzka R.T. Factors associated with racial differences in deaths among nursing home residents with COVID-19 infection in the US. JAMA Netw Open. 2021;4:e2037431. doi: 10.1001/jamanetworkopen.2020.37431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ochieng N., Chidambaram P., Garfield R., Neuman T. Factors associated with COVID-19 cases and deaths in long-term care facilities: Findings from a literature review. Kaiser Family Foundation. 2021. https://www.kff.org/coronavirus-covid-19/issue-brief/factors-associated-with-covid-19-cases-and-deaths-in-long-term-care-facilities-findings-from-a-literature-review/ Available at: Accessed May 9, 2021.
- 16.Harrington C., Ross L., Chapman S., et al. Nurse staffing and coronavirus infections in California nursing homes. Policy Polit Nurs Pract. 2020;21:174–186. doi: 10.1177/1527154420938707. [DOI] [PubMed] [Google Scholar]
- 17.Chen A.T., Yun H., Ryskina K.L., Jung H.Y. Nursing home characteristics associated with resident COVID-19 morbidity in communities with high infection rates. JAMA Netw Open. 2021;4:e211555. doi: 10.1001/jamanetworkopen.2021.1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li Y., Temkin-Greener H., Shan G., Cai X. COVID-19 infections and deaths among Connecticut nursing home residents: Facility correlates. J Am Geriatr Soc. 2020;68:1899–1906. doi: 10.1111/jgs.16689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mehta H.B., Li S., Goodwin J.S. Risk factors associated with SARS-CoV-2 infections, hospitalization, and mortality among US nursing home residents. JAMA Netw Open. 2021;4:e216315. doi: 10.1001/jamanetworkopen.2021.6315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abrams H.R., Loomer L., Gandhi A., Grabowski D.C. Characteristics of U.S. nursing homes with COVID-19 cases. J Am Geriatr Soc. 2020;68:1653–1656. doi: 10.1111/jgs.16661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Unruh M.A., Yun H., Zhang Y., et al. Nursing home characteristics associated with COVID-19 deaths in Connecticut, New Jersey, and New York. J Am Med Dir Assoc. 2020;21:1001–1003. doi: 10.1016/j.jamda.2020.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li Y., Cen X., Cai X., Temkin-Greener H. Racial and ethnic disparities in COVID-19 infections and deaths across U.S. nursing homes. J Am Geriatr Soc. 2020;68:2454–2461. doi: 10.1111/jgs.16847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.He M., Li Y., Fang F. Is there a link between nursing home reported quality and COVID-19 cases? Evidence from California skilled nursing facilities. J Am Med Dir Assoc. 2020;21:905–908. doi: 10.1016/j.jamda.2020.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Travers J.L., Agarwal M., Estrada L.V., et al. Assessment of coronavirus disease 2019 infection and mortality rates among nursing homes with different proportions of black residents. J Am Med Dir Assoc. 2021;22:893–898.e2. doi: 10.1016/j.jamda.2021.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dean A., Venkataramani A., Kimmel S. Mortality rates from COVID-19 are lower in unionized nursing homes: Study examines mortality rates in New York nursing homes. Health Aff (Millwood) 2020;39:1993–2001. doi: 10.1377/hlthaff.2020.01011. [DOI] [PubMed] [Google Scholar]
- 26.Zanettini C., Omar M., Dinalankara W., et al. Influenza vaccination and COVID-19 mortality in the USA: An ecological study. Vaccines (Basel) 2021;9:427. doi: 10.3390/vaccines9050427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jehi L., Ji X., Milinovich A., et al. Development and validation of a model for individualized prediction of hospitalization risk in 4,536 patients with COVID-19. PLoS One. 2020;15:e0237419. doi: 10.1371/journal.pone.0237419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.EBMPHET Consortium COVID-19 severity in Europe and the USA: Could the seasonal influenza vaccination play a role? SSRN Electr J. 2020 Jun 16 [Epub ahead of print] [Google Scholar]
- 29.Centers for Medicare & Medicaid Services Nursing Home Compare. MDS Quality Measures. 2021. https://data.cms.gov/provider-data/dataset/djen-97ju Available at: Accessed March 5, 2021.
- 30.Long-Term Care: Facts on Care in the US. LTCFocus. Brown School of Public Health. https://ltcfocus.org Available at: Accessed April 26, 2021.
- 31.New York Times COVID-19 data. Github. https://github.com/nytimes/covid-19-data Available at: Accessed November 23, 2020.
- 32.Harrington C., Dellefield M.E., Halifax E., et al. Appropriate nurse staffing levels for U.S. nursing homes. Health Serv Insights. 2020;13 doi: 10.1177/1178632920934785. 1178632920934785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Immunization and Infectious Diseases. Office of Disease Prevention and Health Promotion. https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives Available at: Accessed November 4, 2020.
- 34.United States Census Bureau County population totals: 2010-2019. 2020. https://www.census.gov/data/datasets/time-series/demo/popest/2010s-counties-total.html#par_textimage_739801612 Available at: Accessed April 15, 2020.
- 35.Hewitt J., Carter B., Vilches-Moraga A., et al. The effect of frailty on survival in patients with COVID-19 (COPE): A multicentre, European, observational cohort study. Lancet Public Health. 2020;5:e444–e451. doi: 10.1016/S2468-2667(20)30146-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lepore M., Livingston I., Naden D., Ma M. Impacts of minimum wage increases on nursing homes: Final report. US Department of Health & Human Services: Office of the Assistant Secretary for Planning and Evaluation. 2020. https://aspe.hhs.gov/pdf-report/impacts-minimum-wage-increases-nursing-homes-final-report Available at: Accessed June 17, 2021.
- 37.How low nursing home wages are contributing to COVID-19's spread. ElderLawAnswers. 2020. https://www.elderlawanswers.com/how-low-nursing-home-wages-are-contributing-to-the-spread-of-covid-19-17702 Available at: Accessed June 17, 2021.
- 38.Centers for Disease Control and Prevention 2004 Current Resident Tables—Estimates. https://www.cdc.gov/nchs/nnhs/resident_tables.htm Available at: Accessed May 18, 2021.
- 39.Kosar C.M., White E.M., Feifer R.A., et al. COVID-19 mortality rates among nursing home residents declined from March To November 2020. Health Aff (Millwood) 2021;40:655–663. doi: 10.1377/hlthaff.2020.02191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Food and Drug Administration Fact sheet for recipients and caregivers: Emergency use authorization of the Pfizer-Biontech COVID-19 vaccine to prevent coronavirus disease 2019 in individuals 16 years of age and older. https://www.fda.gov/media/144414/download Available at: Accessed May 18, 2021.