Abstract
Background:
Wheelchair users often experience prolonged periods of stationary sitting. Such periods are accompanied with increased loading of the ischial tuberosities. This can lead to the development of pressure ulcers which can cause complications such as sepsis. Periodic pressure offloading is recommended to reduce the onset of pressure ulcers. Experts recommend the periodic execution of different movements to provide the needed pressure offloading. Wheelchair users, however, might not remember to perform these recommended movements in terms of both quality and quantity. A system that can detect such movements could provide valuable feedback to both wheelchair users as well as clinicians.
Purpose:
The objective of this study was to present and validate the WiSAT – a system for characterizing in-seat activity for wheelchair users. WiSAT is designed to detect two kinds of movements – weight shifts and in-seat movements. Weight shifts are movements that offload pressure on ischial tuberosities by 30% as compared to upright sitting and are maintained for 15 seconds. In-seat movements are shorter transient movements that involve either a change in the center of pressure on the sitting buttocks or a transient reduction in total load by 30%. This study validates the use of WiSAT in manual wheelchairs.
Methods:
WiSAT has a sensor mat which was inserted beneath a wheelchair cushion. Readings from these sensors were used by WiSAT algorithms to predict weight shifts and in-seat movements. These weight shifts and in-seat movements were validated against a high-resolution interface pressure mat in a dataset that resembles real world usage.
Results:
The proposed system achieved weight shift precision and recall scores of 81% and 80% respectively while in-seat movement scores were predicted with a mean absolute error of 22%.
Conclusion:
Results showed that WiSAT provides sufficient accuracy in characterizing in-seat activity in terms of weight shifts and in-seat movement.
2. Introduction
Wheelchair users, especially users with spinal cord injuries, experience limited sensory cues to move within their chairs. This leads to extended periods of stationary sitting (Sonenblum et al., 2016) which causes extensive loading of body tissues, particularly around the ischial tuberosities and sacrum and coccyx. Increased loading of tissues, both in magnitude and duration, can hinder blood and oxygen supply to tissues which can cause pressure ulcers. About 46% of 300,000 people with spinal cord injuries in the United Sates experience pressure ulcers (N.S.C.I.S.C, 2015). After sustaining spinal cord injuries, more than 20% require costly surgeries to manage these ulcers (Saunders et al., 2012). The recurrence rate for pressure ulcers can be up to 79% which further adds to healthcare costs(Bates-Jensen et al., 2009). These pressure ulcers can become infected, leading to life threatening complications such as sepsis - such complications are associated with mortality rates of 48%.(N.S.C.I.S.C, 2015).
Periodic movements reduce the duration of pressure applied to these tissues. Clinical experts often suggest the periodic usage of certain recommended pressure relief movements, called weight shifts (Consortium for Spinal Cord Medicine Clinical Practice, 2001; Sliwinski et al., 2009). It has been shown that such weight shifts lead to an increase in tissue blood flow, which may help prevent the development of pressure ulcers (Sonenblum et al., 2014). However, most wheelchair users fail to perform these movements with sufficient frequency. On a given day, the average wheelchair user spends 140 continuous minutes seated in their wheelchairs without performing any weight shifts (Sonenblum et al., 2016). This is a significantly lower number compared to the recommendations made by physicians, which vary between performing weight shifts every 15 minutes to performing weight shifts every 30 minutes(Consortium for Spinal Cord Medicine, 2014; Consortium for Spinal Cord Medicine Clinical Practice, 2001; Mayo Clinic, 2009; Sliwinski et al., 2009). Additionally, the users’ execution of these movements might not always lead to the recommended amount of offloading to constitute an effective weight shift.
A system that provides feedback to the users in terms of the number of successful weight shifts performed could potentially help improve the quality and quantity of weight shift movements performed. The earliest of such systems used wheel chairs equipped with pressure sensors that could only detect pushups (Fordyce et al., 1968). Subsequent systems were able to detect forward and lateral leans by comparing readings from multiple pressure sensors to a threshold (Roemer et al., 1976; Yang et al., 2009). Other publications describe systems which used pressure sensors on top of the seating cushion, which is not a suitable configuration for long term usage. Recent publications use different machine learning classifiers to identify specific postures such as leaning forwards, sideways, etc. for wheelchair occupants (Ma et al., 2017). These studies provide limited details for postures to be detected. Only a single posture for each lean type was used for training. It is likely that these postures correspond only to full leans which are performed rarely by wheelchair users as compared to partial leans. Other systems identify pressure relief movements for tilt-space chairs, but these systems do not extend to upright wheelchairs. A comprehensive survey of such systems can be found in (Vos-Draper et al., 2016)
One study used a pressure relief identification system to find the relationship between trunk strength and pressure offloading (Gabison et al., 2017). However, pressure reliefs were considered as instances when readings from one of the pressure sensors dropped to zero. Another paper addresses a similar question of absolute pressure-offloading in which a sufficient movement was deemed to have been performed if the pressure was reduced below 30 mmHg, as measured using a sophisticated high-resolution pressure sensing mat (Dowling et al., 2017).Note that this level of pressure reduction is nearly equivalent to completely exiting the seat, which can be detected without resorting to sophisticated machine learning tools. Previous studies have shown that users do not perform such movements frequently (Sonenblum et al., 2016).
Recent studies (Sonenblum et al., 2014) have shown that movements that relieve pressure by 30% relative to upright seating pressure can be sufficient to provide biomechanical benefits such as increased blood flow. Such movements, referred to as partial leans, are performed more frequently than the extreme leans of (Dowling et al., 2017; Sonenblum et al., 2016). These partial leans provide sufficient pressure offloading to constitute weight shifts. Weight shifts are movements, including partial and full leans, that relieve pressure at the ischial tuberosities by 30% or more as compared to pressure during upright sitting and provide an increase in blood flow to the ischial tuberosity (Sonenblum et al., 2016).
Several recent studies have explored the use of a novel system to quantify the number of weight shifts performed by users in their daily lives and identify differences in behavior between those with and without a history of pressure ulcers (Dai et al., 2012; Sonenblum et al., 2018; Sonenblum et al., 2016; Sprigle et al., 2019). Unfortunately, this system was individually trained by collecting novel training and simultaneous ground truth data for each user and then using a K nearest neighbor classifier that uses this individualized training data. This is likely to be infeasible in the context of a more widely usable system and/or commercial product, which would need to achieve good performance with minimal to no personalized training and truth data.
In-seat movements are transient movements which cause the center of pressure on the buttocks to travel 5 cm over a 5 second window. These movements provide temporary offloading of the buttocks. Such movements are more common than weight shifts and have also shown to increase blood flow (Sonenblum et al., 2018). Detecting such in-seat movements could further help characterize movements that help prevent the development of pressure ulcers.
In this study, we discuss the validation results of the Wheelchair In-Seat Activity Tracker (WiSAT), which is intended to be a prototype for in-seat activity characterization. This tracker detects weight shifts and in-seat movements. This tracker can be used with most commercially available skin protection wheelchair cushions. The aim of this paper is to validate the performance of the WiSAT on data that closely depicts data encountered in a real-world setting. By validation, we mean validating the performance of our proposed tracker to detect these movements. WiSAT performance was validated among manual wheelchair users. This tracker is intended for both manual wheelchairs and powered wheelchairs that lack power seat functionality - such as tilt, recline etc.
3. Methodology
3.1. Instrumentation
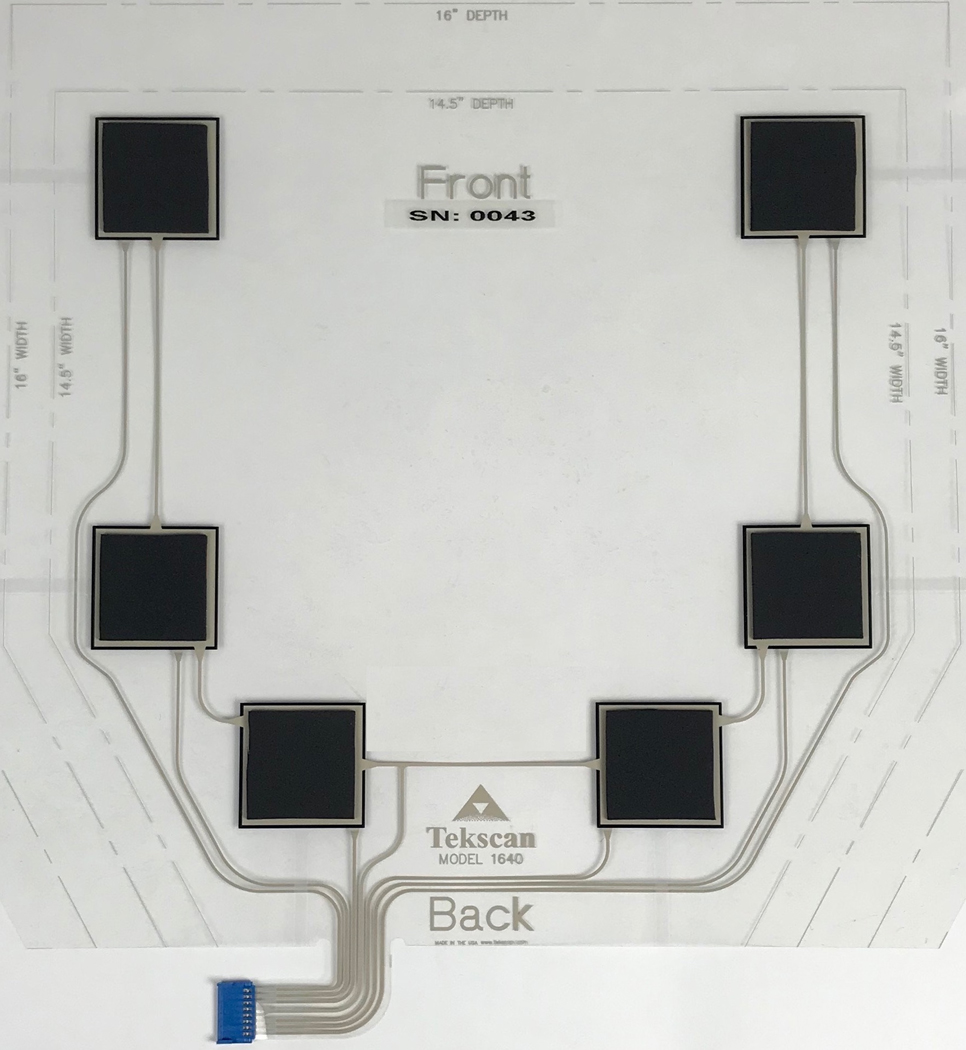
The WiSAT consists of three major components: a sensor mat, data logger, and mobile app. The sensor mat consists of six force sensitive resistors produced by Tekscan (Boston, MA), which is placed on the wheelchair beneath the wheelchair cushion (Figure 1). This mat is fully inserted within the cushion cover such that the mat is beneath the cushion but above the cushion cover’s bottom surface. Once the cushion cover is zipped, the mat is secured in its position. The readings from the sensors are recorded by a data logger at a frequency of 4 Hz and are synchronized in time. The current data logger weighs 10 grams, measures 5cm in width and 7cm in length. This data logger may be secured inside the cushion cover or in a bag attached outside of the cushion cover. This data logger is equipped with a Bluetooth module to transfer data to a mobile application. This application first calibrates the raw sensor values into force values. These values are then used to characterize weight shifts and in-seat movement. For validation, however, raw data stored on the data logger was downloaded to a computer via USB and processed using MATLAB.
Figure 1:
WiSAT sensor mat which is placed beneath a wheelchair cushion. The top of the picture corresponds to the mat section that lies at the front of the cushion while the bottom of the picture corresponds to the mat section that lies at the back of the cushion.
3.2. Dataset
The data collection protocol was reviewed by the institutional review board and all participants provided informed consent prior to participation. Participants were recruited throughout 2019 via posters, emails and social media posts. The participant inclusion criteria required participants to be aged 18 to 69, be able to transfer on and off their chair independently and be able to perform independent weight shifts. The participants were also required to communicate effectively in English to follow the data collection protocol. Datasets for training and validating the WiSAT were collected in a controlled laboratory setting. The training dataset was collected through an 8-minute protocol, while a validation dataset was collected through a 70-minute protocol.
The training dataset collection protocol involved movements such as push-ups, directional leans (in right, left, and forward directions), diagonal leans (in the forward-right and forward-left directions) along with intermittent periods of upright sitting separating many of the leans. Each of the directional leans were further categorized into two kinds of leans: partial leans and full leans (Sonenblum et al., 2014). For full leans, the participants were asked to lean in the respective directions until they were able to touch the ground, or as far as they could lean comfortably. Partial side (right and left) leans involved leaning until the participants were able to touch the center of the manual wheelchair wheel. Forward partial leans involved leaning forward and placing the elbows on the knees. Each of the directional leans mentioned before, including full/partial and diagonal leans, were maintained for 20 seconds, to provide a sufficient number of data points at each position. Pushups were maintained for 3 seconds while upright sitting segments lasted for 20 seconds.
The training dataset was collected using 20 participants, of whom 12 used a wheelchair as their primary mobility device, and 8 were able-bodied. Data from both wheelchair and able-bodied participants was processed identically. While wheelchair users may move differently than able-bodied individuals, force distribution through the cushion onto the sensor is a function of gravity and the material construction of the cushion, therefore, it is independent of the functional level of the participant. This was reflected in the training data where the classifier features and classifier performance showed no distinction between wheelchair users and able-bodied individuals. Wheelchair users performed the protocol using their own wheelchair and cushion, and if time allowed, they repeated the protocol using additional wheelchair cushions provided by the investigators. Able-bodied participants performed the protocol 3 times, seated on 3 different wheelchair cushions: Jay2 by Sunrise Medical (Fresno, CA), Roho High Profile by Permobil (Permobil, Bellevillle, IL), and Matrx Vi by Invacare (Elyria, OH). These cushions were selected because they are some of the most commonly prescribed cushions for full-time wheelchair users at risk of pressure ulcer development, and their material construction and load redistribution to the bottom surface of the cushion is very different. For example, the Jay2 uses a firm contoured foam with a fairly rigid base and a fluid filled pad on top; the Roho High Profile uses air-filled neoprene bladders to simulate floatation; while Matrx Vi uses multiple layers of contoured foam and is more flexible than the Jay2. The rigid base of the Jay2 distributes load onto the WiSAT quite differently than the very deformable base of the Roho High Profile. Wheelchair users used their personal manual wheelchairs, while able-bodied participants used one of 3 wheelchairs for the study: Invacare A-4, Action A-4, or Quickie GTX.
A 70-minute protocol was used to obtain the validation dataset. Twenty unique datasets were collected from 11 participants. Three of these participants also participated in the training protocol, but the remaining 8 were new. This protocol involved the same directional leans and pushups that were contained in the 8-minute training protocol but contained multiple repetitions of these movements. Each of these leans again lasted 20 seconds while pushups also lasted 3 seconds. All of these movements were repeated four times. Additionally, the upright sitting segments that separated the leans were 300 seconds in duration (as compared to 20 seconds in the training data protocol) to reflect real life wheelchair usage where occupants do not perform in-seat movements nearly as frequently. This protocol also contained additional movements to better represent daily life. These included leaning forward on a desk (to represent working or resting) for 30 seconds, as well as 30 minutes of free activity where participants could move about or remain stationary in the chair as they pleased.
A BodiTrak high-resolution interface pressure mat or IPM (VistaMedical, Winnipeg, Canada) was placed above the cushion at the interface between the participant and the cushion. This mat was used to provide ground truth to identify weight shifts and in-seat movements for both training and validation datasets. An area of size 3.4 by 3.4 inches corresponding to each ischial tuberosity was observed during the course of the protocol on this high-resolution mat. The Peak Pressure Index (PPI) was calculated for this area (Sprigle et al., 2003). This PPI was then used to obtain labels to validate the performance of detecting weight shifts. Details on obtaining these ground truth labels for weight shifts can be found in Section 3.3.1. Labels for evaluating in-seat movement detection performance were also obtained using the high-resolution mat. This was done by calculating the in-seat movement on the high-resolution mat and comparing it to the in-seat movement detected by WiSAT. Details for this can be found in Section 3.4.2.
3.3. Activity metrics
The WiSAT is used to provide two key metrics that characterize in-seat activity, summarized as follows.
3.3.1. Weight shifts
Weight shifts are used to identify instances when the pressure from either of the two ischial tuberosities (ITs) is offloaded by more than 30% for at least 15 seconds. Though the recommended duration of a pressure relief movement varies between 15–60 seconds (Walker, 2009), a 15 second duration was chosen to include most intentional and unintentional weight shifting behaviors. Unlike other works which use absolute pressure measured for labels (Dowling et al., 2017), the WiSAT defines a weight shift uniquely for each individual based on a reduction in pressure relative to upright sitting. To accomplish this, the data from the IPM is run through an averaging filter to provide a baseline estimate of upright sitting pressures. If the PPI values under either ischial tuberosity as measured by the high-resolution IPM are reduced by more than 30% as compared to the IPM baseline, and this reduction is maintained for at least 15 seconds, a successful weight shift has been performed. The minimum requirement of a 30% reduction was based on previous work, which showed that functional leans reduced pressure between 29–46% and increased blood flow on the order of 100–300% (Sonenblum et al., 2016; Sonenblum et al., 2014).
Since the training data is composed of a short segment of data with frequent movements, there is not enough time for the baselines to stabilize. For this reason, the upright segments are used as baselines for training data.
The validation data consists of longer upright segments which allow enough time for averaging baselines to stabilize, and therefore in the validation data these averaging-based estimates are used as the baseline, as would occur in the field.
Weight shift detection requires participants to perform an initialization routine at the start of the use of the WiSAT. During initialization, participants sit upright, and perform one full lean towards each direction: front, right and left. Participants were asked to lean as far as they are comfortable leaning. The entire initialization takes less than two minutes. The sensor values measured by the WiSAT were used to calculate the center of pressure in the medial-lateral (CoP ML) and anterior-posterior (CoP AP) directions, which were then normalized using the user’s initialization data. These center of pressure values were calculated using a weighted sum of force values in the medial-lateral (sideways) and anterior-posterior (front-backwards) directions as shown in equations 1 and 2. These weights correspond to sensor distances in the respective directions. In equation 1, Fx is the force measured by sensor x, while MLX is the distance of sensor x in the medial-lateral direction. CoP AP is measured similarly in equation 2 with APx is the distance of sensor x in the anterior-posterior direction:
| (1) |
| (2) |
Forces from all six sensors are added together to compute total sensor force. This total sensor force is passed through an averaging filter to obtain a baseline for total force during upright sitting. The total sensor force is divided by this baseline to obtain the normalized total load. CoP ML and CoP AP are also passed through an averaging filter to obtain baselines for CoP ML and CoP AP. The respective baselines are then subtracted from each CoP to obtain CoP ML and CoP AP that are centered at zero. This normalized total load is used along with centered CoP AP and centered CoP ML as features to develop the weight shift classifiers described below.
Building on previous classification efforts (Dai et al., 2012), a weight shift detector was built that requires only limited individualization. The training data described earlier was used to train three support vector machine (SVM) classifiers, with each a classifier corresponding to a different category of cushion. These three categories are air-cell cushions, rigid-bottomed cushions and soft-bottomed cushions. Users of the WiSAT are only asked if they are using an air-cell cushion or not. If an air-cell cushion is not used, sensor variance during upright sitting is used to automatically determine if a rigid bottomed or a soft bottomed cushion is used. Once the cushion type is determined, the corresponding SVM classifier is used for detecting weight shifts. It is important to note that only the normalization is individualized. Unlike prior efforts (Dai et al., 2012), which train a different nearest-neighbor classifier for each user, we obtain a single set of classifiers that can be used for any user and that is computationally simple to apply.
Examples of detected weight shifts can be seen in Figure 2. In Figure 2, the first subplot shows force values from each of the six sensors. These force values are converted into CoP AP, CoP ML and total load values. The third subplot shows that two weight shifts are correctly detected as these detected segments correspond to instances where the PPI values for either of the two ischial tuberosities decreases by 30% as seen in the fourth subplot. The first weight shift is caused by a diagonal forward-left lean and the second weight shift is a result of a diagonal forward-right leans during free movement segment within the validation protocol. The first subplot can be used to infer these movements. For each of these two weight shifts, it can be seen in the first subplot that force values for both back sensors decrease while force values for both front sensors increase. This is reflected in the increase of the CoP AP values in the second subplot which indicates that a person has leaned forward. It can be also seen that for the first weight shift, the force value for the middle right sensor decreases while the force value for the middle left sensor increases. This corresponds to a change in CoP ML in the negative direction, which indicates a person has leaned left. During the second weight shift, it can be seen that the force measured by middle left value slightly decreases while the force value increases for the middle right sensor. This can be seen in the second subplot where the CoP ML value changes in the positive direction which translates to a rightwards shift.
Figure 2:
Description of Weight Shift detection. The first subplot shows force values from all 6 sensors. These force values are converted into features (CoP ML, CoP AP and Total Load) which are provided to the weight shift classifier. The output for the weight shift classifier can be seen in the third subplot along with truth labels. The truth labels are obtained from peak pressure index (PPI) values for each ischial tuberosity. When PPI for either of the right or left ischial tuberosities decreases 30%, a weight shift label is identified.
3.3.2. In-seat movement
The in-seat movement metric is intended to measure transient movements that displace the center of pressure or transiently unload the buttocks. For example, this might include activities such as fidgeting, or micro-movements. The distance travelled by the center of pressure, which reflects how much the center of pressure changes, was measured using the WiSAT in the medial-lateral and anterior-posterior directions. If the resolved distance over a 5-second window was greater than 5 cm, a successful in-seat movement was performed. A successful in-seat movement is also performed when the normalized total load is reduced by 30%. Such movements transiently unload the buttocks.
Figure 3 shows examples of in-seat movements. The first subplot shows center of pressure values for both the medial-lateral (CoP ML) and anterior-posterior (CoP AP) directions. These CoP values depict center of pressure location measured on the sensor mat in centimeters. As a user moves in the chair, the center of pressure changes. As medial-lateral and anterior-posterior directions are perpendicular, the hypotenuse of CoP ML and CoP AP is taken to obtain a combined distance travelled by CoP. The combined distance travelled by CoP over a 5 second window is then computed which can be seen in the second subplot. Whenever this distance travelled exceeds 5 cm, an in-seat movement is detected. The distance travelled by CoP when out of chair is ignored as the corresponding CoP location values can behave erratically. The third subplot shows total load. An in-seat movement is also detected when the total load transitions from its normal value of 1.0 to a reduced offloading of 30% which corresponds to a value of 0.7. The fourth subplot shows that a total of two in-seat movements were detected. The first detected in-seat movement originates from CoP distance (subplot 2), while the second in-seat movement is caused by total load reduction (subplot 3).
Figure 3:
Example of in-seat movement detection. The first subplot shows the CoP ML and CoP AP location as measured on the sensor mat. These CoP values are then used to calculate the distance traveled by CoP over a 5 second window as shown in the second subplot. Whenever this distance is greater than 5 cm, in-seat movement is detected. The grayed values in the second subplot show CoP distance traveled when the user is out of chair. When the user is out of chair, CoP location values behave erratically, and the corresponding CoP distance is ignored when calculating in-seat activity. The third subplot shows normalized total load. Whenever, the normalized total load transitions to be below 0.7, an in-seat movement is also detected.
3.4. Evaluation criteria
3.4.1. Weight shifts
A standard way of evaluating the performance of our proposed weight shift classifier would be to compute sensitivity and specificity metrics (Trevethan, 2017). Sensitivity is the ratio of detected positives over all positives while specificity is the ratio of detected negatives over all negatives. These metrics are useful when applied to segments that correspond to user leans within the data collection protocol, where the protocol requests users to undertake a series of leans, some of which correspond to true weight shifts, and others which do not. However, this approach would be an unsuitable representation of the performance on the full 90-minute data as weight shifts might be performed within the free movement regions of the protocol which do not request the user to undertake leans. If the predictions and truth labels are evaluated at every set of samples from the sensors, the resulting scores would always be skewed in the direction of specificity over sensitivity, as very few of these samples actually correspond to a weight shift. For these reasons, we instead use precision and recall as our key metrics, which are known to be more appropriate in such settings (Saito et al., 2015). Precision represents the fraction of all detected weight shifts that correspond to true weight shifts. Recall represents the fraction of all true weight shifts that are detected as weight shifts. (Note that times during which no weight shift is performed, and no weight shift is detected do not contribute to the calculation of these metrics, and so long periods of inactivity in the validation data do not affect the results.) These metrics are described in detail in Figure 4.
Figure 4:
Evaluation Metrics for Weight Shift Classification.
3.4.2. In-seat movement
The in-seat movement score was also calculated using the high-resolution IPM (truth data). This was done in a manner which was identical to the method described in section 3.3.2 for the WiSAT. Segments were identified as active when the distance travelled by the center of pressure for the high-resolution IPM over a 5-second window was greater than 5 cm. Segments were also active when the total pressure on the high-resolution IPM was reduced by 30%. These segments were then counted to produce the IPM in-seat movement score (truth). The WiSAT in-seat movement score and the IPM in-seat movement score were then compared in the error metric given by:
| (3) |
4. Results
4.1. Weight shifts
Across the 20 datasets within the validation data, the weight shift detector had a precision score of 81% and recall score of 80% on the validation dataset. Figure 5 shows a scatter plot representing precision and recall scores for the weight shift classifier. Scores within this plot have been assigned different shapes for different cushions. It can be seen that the Roho cushion has performed worst. This is discussed in more details in the discussion section.
Figure 5:
Precision vs Recall scores for the validation dataset. The plot shows results for 20 datasets collected from 11 subjects. The markers with numbers imply that there are multiple markers with identical values overlaid on one another. For overlaid markers on the extreme right, a Roho marker overlays a Matrx marker while two Jay2 markers are overlaid at a precision and recall of 0.78 and 0.85, respectively.
We also evaluated the performance of another classifier trained using a deep neural network architecture: the so-called long short-term memory (LSTM) recurrent neural network. The results on the validation dataset for this classifier were comparable to that of our SVM approach. However, the features used by an SVM are more interpretable as compared to an LSTM which is constructed using learned (nearly impossible to interpret) features. Additionally, the SVM approach results in a simple polynomial equation that can be compared to a threshold to detect a weight shift. This involves relatively simple computations that are more feasible in the context of a mobile phone application.
4.2. In-seat movement
The movement score was measured on 17 datasets out of the 20. Scores on the remaining 3 datasets were dropped as the specific sensor mat used to collect these datasets was determined to be much less sensitive than the mats used to the other 17 datasets. Specifically, movements that caused transient offloading on the high-pressure interface mat caused no change in the center of pressure as measured by the sensors. For the remaining 17 datasets, the average absolute error for in-seat movement was 22.15%. A histogram representing the in-seat movement errors can be seen in Figure 6.
Figure 6:
Histogram for in-seat movement error.
5. Discussion
5.1. Weight shifts
The classifier attained a precision score of 81% and a recall score of 80%. These numbers are particularly good for a consumer device which requires no individualized training and works with multiple cushion types. Unlike other pressure relief technologies, this classifier was designed to detect a 30% reduction in pressure or partial leans, in the presence of a damper (cushion) between the sensors and the human body. Partial leans are important to detect because they are more frequently performed and provide biomechanical benefit (Sonenblum et al., 2018; Sonenblum et al., 2016; Sonenblum et al., 2014). Given this challenging task, precision and recall scores greater than 80% is respectable.
Errors were most frequently caused by partial leans. Partial leans cause offloadings that are often at the boundary of the required 30% offloading threshold to count as a weight shift. For example, users may offload 32% of the PPI, but this may not be detected as a weight shift by the WiSAT, creating a false negative. Included in Figure 5 was a dataset with a low recall score of 0.5, indicating many false negative weight shifts. These false negatives contributing to this score were caused by partial leans. An example of such false negatives can be seen in Figure 7. The intervals marked by green lines show partial leans. The classifier is incorrect on the first partial lean but correctly classifies the second partial lean. These partial leans correspond to same ischial tuberosity offloading of about 50% but correspond to different magnitude of the center of pressure displacement in the medial-lateral direction, which causes the errors. For aforementioned dataset in Figure 5, false negatives were also caused when the duration of a weight shift was longer than 15 seconds, but since the wheelchair cushion damped some of the response, the weight shifts measured by the WiSAT were slightly below the required threshold of 15 seconds and were not labelled as weight shifts. This damping behavior is most common in air-cell cushions with connected bladders, where the air redistributes in response to movement. The alternative scenario (i.e., false positives due to partial leans) occurs when a user offloads just below the boundary of the threshold (for example, 28%) of the PPI during a partial lean, but the WiSAT recognizes this as a weight shift, creating a false positive. Figure 8 provides an example of such a case. The second false positive weight shift contains significant periods where the true pressure offloading is just slightly below the required offloading of 30%. While initialization is used to adjust for consistency across participants, it is an imperfect approach; the amounts by which a person leans to obtain these scaling values may vary.
Figure 7:
Weight shift classification error on partial side leans. It can be seen in top subplot that the first partial lean has a lower CoP ML feature magnitude than the second partial lean, causing only the second partial lean to be detected. However, in the bottom subplot, the pressure offloading is almost identical causing both leans to be labelled as true weight shifts. Equivalent offloadings can cause different feature values leading to classification errors.
Figure 8:
False Positives corresponding to transient offloading. A lean is performed but the offloading is not maintained consecutively for 15 seconds as seen in the bottom subplot. The changes in offloading isn’t reflected by changes in the features (top subplot), causing false positives.
The overall performance was particularly downgraded by datasets which had low precision scores, which are caused by a high false positive score. In addition to partial leans occurring just below the boundary, additional false positive segments correspond to transient pressure offloadings that were not maintained for the 15 seconds required to count as a weight shift. Such a case can be seen in Figure 8. In the last subplot, the offloading drops below the required threshold for brief transients. The feature values within these segments are similar, making the classifier classify the entire segment as a weight shift. Such segments are common amongst the datasets that have a precision score lower than 70% in Figure 5 and are more common on air-cell or soft bottomed cushions such as Roho. Both sources of false positives, weight shifts that did not quite reach 30% offloading as measured by the IPM, and those which offloaded significantly but transiently, still indicated a movement by the user that was intended to offload the buttocks. While we would not detect such movements as weight shifts, occasionally detecting these intentional movements is still preferable compared to detecting stationary sitting as a weight shift, which was not seen in the validation testing.
5.2. In-seat movement
As seen in Figure 6, the errors for in-seat movement are skewed in the negative direction. This is because the cushion acts as a damper causing a smaller change in center of pressure for the sensors as compared to the high-resolution mat on top of the cushion. The main additional source of error tends to come from variability in the sensitivity of the mat sensors, with more sensitive sensors resulting in increased in-seat movement counts and less sensitive sensors resulting in lower counts. This variability is a function of the force sensitive resistors rather than the cushions or individual participants. In the future, improvements to the data logger circuitry to optimize the gain for each individual sensor should equilize the sensitivity and reduce the variability experienced in the in-seat movement measurements.
5.3. Validation Results
The validation results show that WiSAT is suitable for detecting weight shifts and in-seat movement. These two metrics correspond to in-seat activity, particularly partial leans and in-seat movement, which are more frequently performed by wheelchair users in everyday lives than the frequently prescribed full lifts and leans. This provides more meaningful in-seat activity characterization when compared to other systems (Dowling et al., 2017; Gabison et al., 2017) which detect large, relatively infrequent, pressure offloadings.
5.4. Potential Improvements
While increased accuracy would be possible with a more complex setup and initialization, simplicity was selected instead for a robust commercial application. Some future improvements to the system are possible. The in-seat movement score may be improved by developing a more consistent sensor or improved circuitry, or by utilizing initialization to normalize according to sensor sensitivity. Weight shifts provide a binary output for sufficient offloading. This is necessary for end users who want a metric which is easy to understand. However, for research applications, a regression-based output could be potentially more informative for characterizing pressure offloading.
Validation work presented here was completed on manual wheelchairs because it was designed to measure independent weight shifts. However, additional work has since been completed to extend the approach to include power wheelchairs with and without tilt-in-space. Detecting occupancy and weight shifts on complex seating systems with multiple power functions such as tilt, recline, and elevating leg rests may be more challenging using the WiSAT and has not yet been evaluated.
6. Conclusions
This paper characterizes the performance of a wheelchair in-seat activity tracker (WiSAT). Results were presented on a validation dataset that closely resembles real world usage. The tracker measures two metrics: weight shifts and in-seat movement. Validation testing suggests that the WiSAT performance is sufficiently accurate to inform a user about their in-seat activity. This in-seat activity corresponds to movements which are frequently performed by wheelchair users in their everyday lives. WiSAT provides a more meaningful in-seat movement characterization when compared to other systems (Dowling et al., 2017; Gabison et al., 2017) which can only detect large pressure offloadings that are infrequently performed. While the efficacy of the WiSAT to motivate users to meet self-selected in-seat activity goals and change behavior still needs to be evalauated, the validation presented in this manuscript was a necessary first step.
References
- Bates-Jensen BM, Guihan M, Garber SL, Chin AS, & Burns SP (2009). Characteristics of recurrent pressure ulcers in veterans with spinal cord injury. Journal of Spinal Cord Medicine, 32(1), 34–42. doi: 10.1080/10790268.2009.11760750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Consortium for Spinal Cord Medicine. (2014). Pressure ulcer prevention and treatment following injury: A clinical practice guideline for health-care providers. Paralyzed Veterans Association. [DOI] [PubMed] [Google Scholar]
- Consortium for Spinal Cord Medicine Clinical Practice. (2001). Pressure ulcer prevention and treatment following spinal cord injury: a clinical practice guideline for health-care professionals. Journal of Spinal Cord Medicine, 24 Suppl 1, S40–101. doi: 10.1080/10790268.2001.11753592 [DOI] [PubMed] [Google Scholar]
- Dai R, Sonenblum SE, & Sprigle S. (2012). A robust wheelchair pressure relief monitoring system. Conf Proc IEEE Eng Med Biol Soc, 2012, 6107–6110. doi: 10.1109/EMBC.2012.6347387 [DOI] [PubMed] [Google Scholar]
- Dowling AV, Eberly V, Maneekobkunwong S, Mulroy SJ, Requejo PS, & Gwin JT (2017). Telehealth monitor to measure physical activity and pressure relief maneuver performance in wheelchair users. Assist Technol, 29(4), 202–209. doi: 10.1080/10400435.2016.1220993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fordyce WE, & Simons BC (1968). Automated training system for wheelchair pushups. Public Health Rep, 83(6), 527–528. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/4968133 [PubMed] [Google Scholar]
- Gabison S, Mathur S, Nussbaum EL, Popovic MR, & Verrier MC (2017). Trunk Function and Ischial Pressure Offloading in Individuals with Spinal Cord Injury. Journal of Spinal Cord Medicine, 40(6), 723–732. doi: 10.1080/10790268.2017.1328345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma C, Li W, Gravina R, & Fortino G. (2017). Posture Detection Based on Smart Cushion for Wheelchair Users. Sensors (Basel), 17(4). doi: 10.3390/s17040719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayo Clinic. (2009). Mayo Clinic Guide to Living with a Spinal Cord Injury. New York: Demos Medical Publishing. [Google Scholar]
- N.S.C.I.S.C. (2015). Annual Statistical Report by the National Spinal Cord Injury Statistical Center. Retrieved from https://www.nscisc.uab.edu/PublicDocuments/reports/pdf/2015%20NSCISC%20Annual%20Statistical%20Report%20Complete%20Public%20Version.pdf
- Roemer R, Lee H, & Meisel H. (1976). Warning device for the prevention of ischaemic ulcers in quadriplegics. Med Biol Eng, 14(5), 580–581. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/979385 [DOI] [PubMed] [Google Scholar]
- Saito T, & Rehmsmeier M. (2015). The Precision-Recall Plot Is More Informative than the ROC Plot When Evaluating Binary Classifiers on Imbalanced Datasets. PLoS One, 10(3). doi:ARTN e0118432 10.1371/journal.pone.0118432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders LL, Krause JS, & Acuna J. (2012). Association of race, socioeconomic status, and health care access with pressure ulcers after spinal cord injury. Arch Phys Med Rehabil, 93(6), 972–977. doi: 10.1016/j.apmr.2012.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sliwinski MM, & Druin E. (2009). Chapter Seven - Intervention Principles and Position Changes. In Sisto SA, Druin E, & Sliwinski MM (Eds.), Spinal Cord Injuries (pp. 153–184). Saint Louis: Mosby. [Google Scholar]
- Sonenblum SE, & Sprigle SH (2018). Some people move it, move it... for pressure injury prevention. Journal of Spinal Cord Medicine, 41(1), 106–110. doi: 10.1080/10790268.2016.1245806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonenblum SE, Sprigle SH, Martin JS, & Pe. (2016). Everyday sitting behavior of full-time wheelchair users. J Rehabil Res Dev, 53(5), 585–598. doi: 10.1682/JRRD.2015.07.0130 [DOI] [PubMed] [Google Scholar]
- Sonenblum SE, Vonk TE, Janssen TW, & Sprigle SH (2014). Effects of Wheelchair Cushions and Pressure Relief Maneuvers on Ischial Interface Pressure and Blood Flow in People With Spinal Cord Injury. Archives of Physical Medicine and Rehabilitation, 95(7), 1350–1357. doi: 10.1016/j.apmr.2014.01.007 [DOI] [PubMed] [Google Scholar]
- Sprigle S, Dunlop T, & Press T. (2003). Reliability of bench tests of interface pressure. Assistive Technology, 15(1), 49–57. doi:Doi 10.1080/10400435.2003.10131889 [DOI] [PubMed] [Google Scholar]
- Sprigle S, Sonenblum SE, & Feng C. (2019). Pressure redistributing in-seat movement activities by persons with spinal cord injury over multiple epochs. PLoS One, 14(2), e0210978. doi: 10.1371/journal.pone.0210978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trevethan R. (2017). Sensitivity, Specificity, and Predictive Values: Foundations, Pliabilities, and Pitfalls in Research and Practice. Front Public Health, 5, 307. doi: 10.3389/fpubh.2017.00307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vos-Draper TL, & Morrow MMB (2016). Seating-Related Pressure Injury Prevention in Spinal Cord Injury: A Review of Compensatory Technologies to Improve In-Seat Movement Behavior. Curr Phys Med Rehabil Rep, 4(4), 320–328. doi: 10.1007/s40141-016-0140-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker J. (2009). Spinal cord injuries: acute care management and rehabilitation. Nurs Stand, 23(42), 47–56; quiz 58, 60. doi: 10.7748/ns2009.06.23.42.47.c7055 [DOI] [PubMed] [Google Scholar]
- Yang YS, Chang GL, Hsu MJ, & Chang JJ (2009). Remote monitoring of sitting behaviors for community-dwelling manual wheelchair users with spinal cord injury. Spinal Cord, 47(1), 67–71. doi: 10.1038/sc.2008.72 [DOI] [PubMed] [Google Scholar]