Abstract
Objectives. To determine the magnitude of increases in monthly drug-related overdose mortality during the COVID-19 pandemic in the United States.
Methods. We leveraged provisional records from the Centers for Disease Control and Prevention provided as rolling 12-month sums, which are helpful for smoothing, yet may mask pandemic-related spikes in overdose mortality. We cross-referenced these rolling aggregates with previous monthly data to estimate monthly drug-related overdose mortality for January through July 2020. We quantified historical errors stemming from reporting delays and estimated empirically derived 95% prediction intervals (PIs).
Results. We found that 9192 (95% PI = 8988, 9397) people died from drug overdose in May 2020—making it the deadliest month on record—representing a 57.7% (95% PI = 54.2%, 61.2%) increase over May 2019. Most states saw large-magnitude increases, with the highest in West Virginia, Kentucky, and Tennessee. We observed low concordance between rolling 12-month aggregates and monthly pandemic-related shocks.
Conclusions. Unprecedented increases in overdose mortality occurred during the pandemic, highlighting the value of presenting monthly values alongside smoothed aggregates for detecting shocks.
Public Health Implications. Drastic exacerbations of the US overdose crisis warrant renewed investments in overdose surveillance and prevention during the pandemic response and postpandemic recovery efforts.
Unofficial data sources, proxies, and provisional records indicate that overdose deaths in the United States are spiking during the COVID-19 pandemic.1–4 National Emergency Medical Services (EMS) data—disaggregated by week—show very-large-magnitude increases in overdose during the pandemic period, reaching more than double baseline values by May 2020.2 Syndromic surveillance data from emergency departments show similar increases in visits for overdose, as well as mental health conditions and intimate partner violence.5 Several states have also published provisional mortality records for the same period, demonstrating large-magnitude spikes in overdose deaths.6,7 A similar pattern is likely to be present at the national level. However, given limitations of provisional overdose mortality reporting, the magnitude of the increase cannot yet be determined from official mortality statistics.
In December 2020, the Centers for Disease Control and Prevention (CDC) released an emergency advisory showing that from June 2019 to May 2020, 81 320 people died of a drug overdose in the United States—representing an increase of 18.0% over the previous 12 months.8 However, this 12-month period covered only the first 3 months of pandemic-related disruptions—March through May 2020. As provisional trends are disaggregated by month, any large spikes occurring during the pandemic would be combined with—and potentially masked by—9 months of lower prepandemic values.
In a typical year, the practice of providing rolling aggregate trends is useful for stabilizing rates—especially in states with small populations—given numerous challenges in overdose surveillance. Mortality records are contributed by all 50 US states and the District of Columbia to the National Center for Health Statistics, where they are analyzed centrally.9 The lag time between a death’s occurrence and the date upon which it is reported to the central repository is generally longer for overdose than other causes of death10 and can vary by state.9 Therefore, provisional estimates of overdose mortality are typically released on at least a 6-month lag. Even then, modeling is undertaken to correct estimates for additional underreporting.11 Provisional records consequently include both “reported” deaths for a given period as well as “predicted” deaths, which are estimated by observing previous reporting delays and assuming they will affect current death levels in a similar fashion.11 In this context, reporting rolling 12-month sums can help to insulate estimates against stochasticity or shocks, which could stem from shifts in reporting lags, and also adjust for seasonality, as all 12 months of each calendar year are always included in each estimated rate.9,11
Nevertheless, during an unprecedented event such as the COVID-19 pandemic—in which the potential exists for drastic month-to-month shifts—we argue that there is value in assessing the existing data for the presence of shocks alongside smoothed trends. We estimated the original monthly mortality values underlying aggregated provisional trends to determine how many individuals died of overdose in March through July of 2020, as the pandemic dramatically changed life in the United States.
METHODS
We estimated the original monthly mortality values underlying provisional aggregate trends. To accomplish this, we leveraged the fact that (1) precise monthly values are known through the end of 201912 and (2) provisional rolling sums are released for 12-month periods with end dates spanning January to July 2020.9 By cross-referencing these 2 time series, we can estimate monthly values for 2020, drawing on a straightforward algorithm.
For example, let us consider the case of overdose mortality for January 2020. We have a 12-month cumulative value (for a particular state) pertaining to February 2019 through January 2020. We subtracted off monthly values for February 2019 through December 2019, leaving only the monthly value for January 2020. We subsequently extracted the value for February 2020 using the 12-month data from March 2019 through February 2020 and subtracting off precise monthly values from March 2019 through January 2020. We repeated this exercise for March, April, May, June, and July 2020. In this way, we used each recovered value to help extract data from the next month, in a set of chained calculations. We did this for each US state, and aggregated them up to the level of census divisions and the national total.
We also quantified how precisely this algorithm can recover monthly values by assessing its performance on previously released provisional aggregates, for which we now have exact monthly values. This method can perfectly recover monthly values when the final and provisional statistics provided by the CDC are internally consistent. In practice, though, these 2 data sources do have small differences, largely because the provisional numbers use modeling to attempt to compensate for reporting lags of greater than 6 months, but these methods are imperfect. Furthermore, there are some small definitional differences between the 2 data sources that could introduce errors. For example, provisional records include all deaths occurring in a given state, whereas final numbers reflect the deceased’s state of residence. In addition, counts of fewer than 10 deaths per state‒month are suppressed in final death data, requiring assumptions about the distribution of deaths for the small number of state‒months with low values.
We quantified the errors stemming from these differences by comparing the data sources for the period for which both are complete, 2015 through 2019. We calculated the average degree to which our algorithmically derived values deviated from subsequently released final trends and used these errors to produce empirically derived 95% prediction intervals (PIs). The full set of recovered values can be seen in Table A (available as a supplement to the online version of this article at http://www.ajph.org), and the algorithm and all code used in this analysis is available in a public repository (https://github.com/akre96/cdc_overdose).
RESULTS
We found that 9192 (95% PI = 8988, 9397) people died of overdose in May 2020—making it the deadliest month on record—representing a 57.7% (95% PI = 54.2%, 61.2%) increase over May 2019 (Figure 1). Values remained elevated in June 2020, at 35.8% (95% PI = 32.8%, 38.8%) above June 2019. Mortality rates increased again in July 2020, reaching 43.6% (95% PI = 40.4%, 46.9%) above July 2019. Overall, values in the first 7 months of 2020 were elevated by 34.8% (95% PI = 31.9%, 37.8%) relative to the equivalent months of 2019.
FIGURE 1—
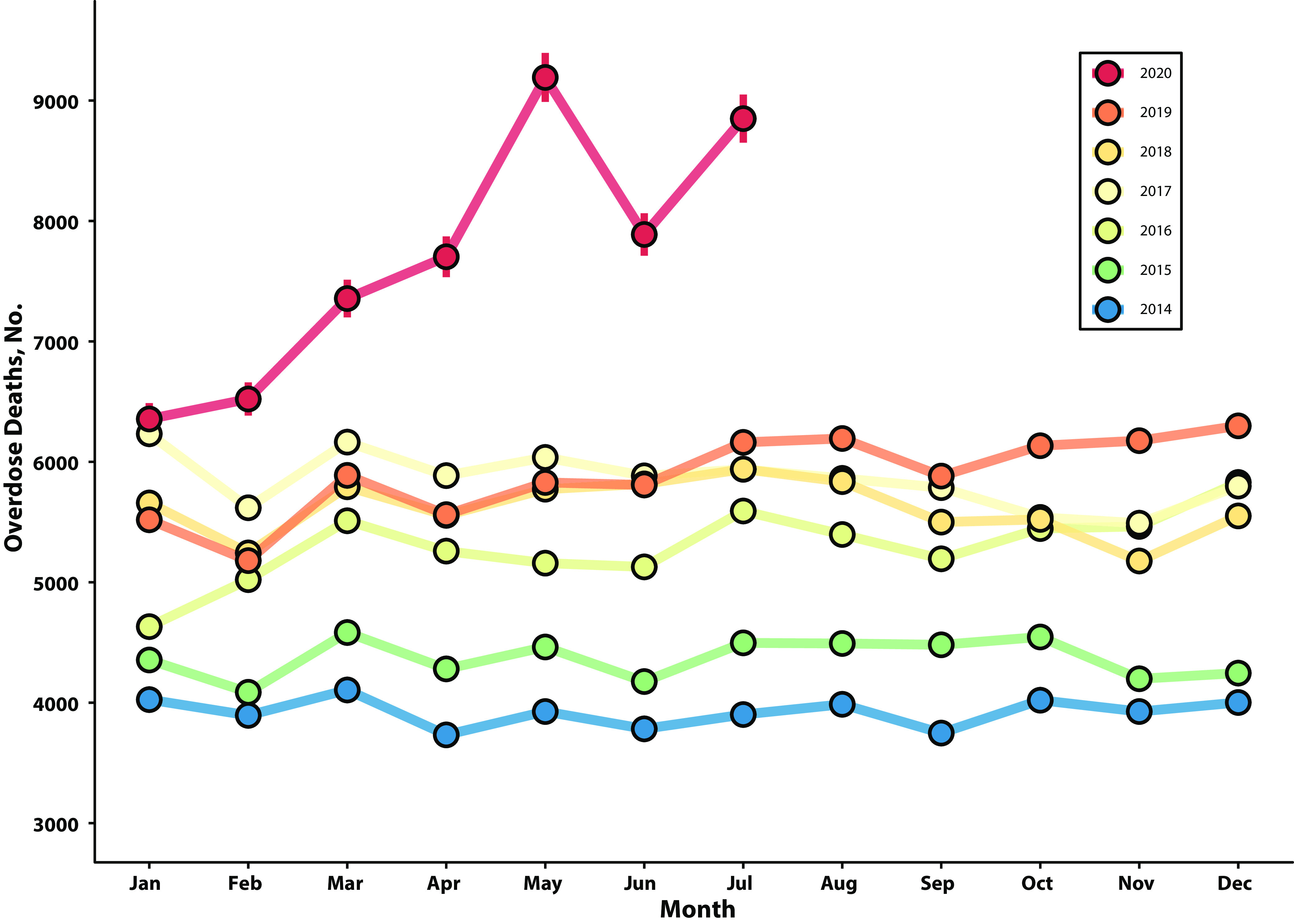
Monthly Overdose Deaths From January 2014 to July 2020: United States
Note. Overdose deaths in the United States are shown by month, from January 2014 to July 2020. For values in 2020, 95% prediction intervals are shown, recovered using the algorithm described in this analysis. This figure reveals that May 2020 was the deadliest month for overdose death in the United States in recent history, elevated above May 2019 by about 60%.
At the census division level, the largest relative increases in overdose deaths in May 2020 compared with May 2019 were seen in the East South Central, South Atlantic, and Pacific divisions, with increases of 99.2% (95% PI = 87.8%, 110.7%), 72.7% (95% PI = 66.6%, 78.8%), and 62.0% (95% PI = 56.4%, 67.7%), respectively (Table 1 and Figure C, available as a supplement to the online version of this article at http://www.ajph.org). New England had the smallest relative increase of 25.1% (95% PI = 17.8%, 32.3%).
TABLE 1—
Overdose Deaths in May 2020 by Census Division: United States
| Location | Deaths in May 2020, No. (95% PI) | % Change 2020 vs 2019, (95% PI) | Deaths per Million, No. (95% PI) |
| National | 9192 (8988, 9397) | 57.7 (54.2, 61.2) | 28.0 (27.4, 28.6) |
| East South Central | 779 (735, 824) | 99.2 (87.8, 110.7) | 40.6 (38.3, 43.0) |
| East North Central | 1706 (1665, 1748) | 55.4 (51.6, 59.2) | 36.4 (35.5, 37.3) |
| New England | 489 (461, 518) | 25.1 (17.8, 32.3) | 32.9 (31.0, 34.8) |
| South Atlantic | 2150 (2074, 2227) | 72.7 (66.6, 78.8) | 32.7 (31.5, 33.8) |
| Middle Atlantic | 1209 (1158, 1261) | 36.3 (30.5, 42.1) | 29.4 (28.1, 30.6) |
| Mountain | 637 (597, 678) | 53.5 (43.7, 63.3) | 25.6 (24.0, 27.3) |
| Pacific | 1097 (1059, 1136) | 62.0 (56.4, 67.7) | 20.5 (19.8, 21.2) |
| West North Central | 421 (405, 438) | 60.7 (54.4, 67.0) | 19.6 (18.9, 20.4) |
| West South Central | 704 (671, 738) | 52.1 (44.8, 59.3) | 17.3 (16.5, 18.2) |
Note. PI = prediction interval. Overdose deaths occurring in May 2020 are shown as counts, and rates per million people, nationally and by 9 US census divisions. The percent change between overdose deaths in May 2019 and May 2020 is also shown and used to sort the row order. Counts of deaths are rounded up to the nearest whole person. Maps showing these values graphically, as well as indicating the geographic location of each census division, are available in Figure C (available as a supplement to the online version of this article at http://www.ajph.org).
At the state level, a large-magnitude increase in May 2020 could be seen for nearly every state with a large-enough population to assess monthly trends (Figure 2). West Virginia, Kentucky, and Tennessee had the highest per capita monthly death rates in May 2020 of 93.2 (95% PI = 81.6, 104.8), 56.0 (95% PI = 52.1, 59.8), and 51.0 (95% PI = 48.3, 53.7) per million inhabitants, respectively, representing 178.3% (95% PI = 143.6%, 213.1%), 140.4% (95% PI = 123.8%, 157.0%), and 97.7% (95% PI = 87.2%, 108.2%) increases over May 2019, respectively. Precise values for all states, census regions, and census divisions can be seen in Table A (available as a supplement to the online version of this article at http://www.ajph.org).
FIGURE 2—
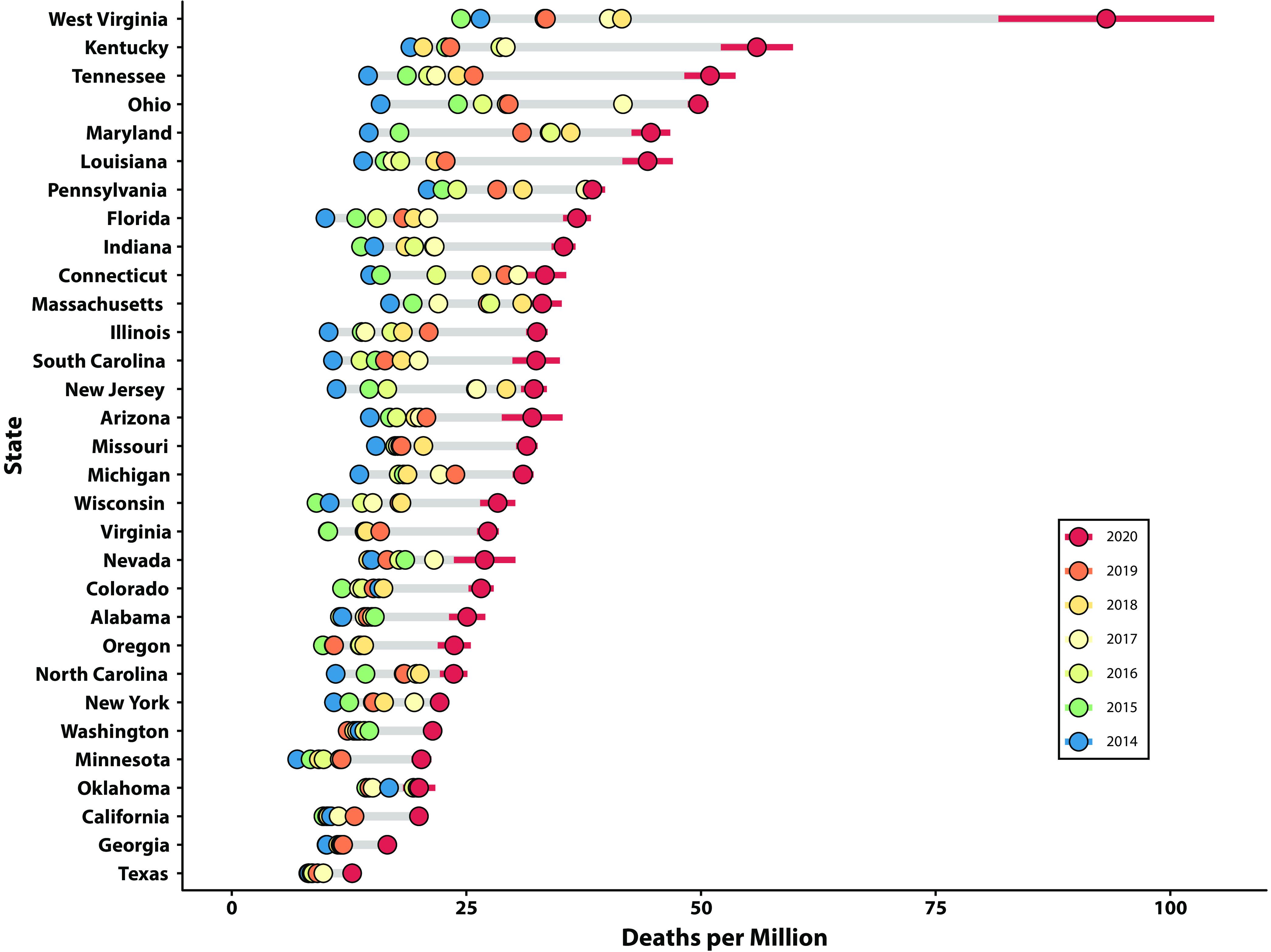
Monthly Overdose Deaths in May 2014 Through 2020: Selected US States
Note. Deaths per million people in the month of May are shown for 2014 through 2020, for a subset of states with the highest total number of overdose deaths in 2020 (to avoid states with small numbers, where trends are less stable). For values in 2020, 95% prediction intervals are shown, recovered using the algorithm described in this analysis. This figure highlights large-magnitude increases in overdose deaths in May 2020 compared with previous years, for nearly all states assessed. Particularly large increases were seen in West Virginia, Kentucky, and Tennessee.
The states with the greatest pandemic-related increases were, in many instances, not the same states with the largest 12-month increases in the latest CDC-produced aggregates ending in 2020. This is illustrated in Figure D (available as a supplement to the online version of this article at http://www.ajph.org). For example, West Virginia and Connecticut had similar percent increases in rolling aggregates ending in May 2020, of 22% and 24%, respectively. However, in monthly data from May 2020, West Virginia had an increase of 178% compared with only 14% in Connecticut. Nevada had a negative percent change of −4% in rolling 12-month trends ending in May 2020; nevertheless, monthly data from May 2020 showed a 63% increase. The overall R2 between the percent increase in monthly data from May 2020 and 12-month rolling sums ending in May 2020 was 0.272, reflecting a relatively low level of correlation.
On average, the algorithmic approach outlined here was able to estimate monthly values from provisional aggregates with a high level of precision, compared with subsequently released finalized monthly values, for the 2015–2019 period in which both could be compared. Errors are summarized in Table B (available as a supplement to the online version of this article at http://www.ajph.org). At the national level, for example, estimating from 1 to 7 months out from the most recent final monthly trends (the task necessary to recover values from January to July 2020), the median absolute percent error (MAPE) was 0.47%. In other words, the method predicted subsequently reported monthly values on average within half a percent. The standard deviation of the percent error was 1.1%. Therefore, a 95% PI for a national-level estimate would reflect that we expect the final monthly value to fall within a margin of approximately plus or minus 2% of the prediction made using our algorithm. MAPEs for division-level statistics also tended to be quite small, ranging from 0.7% in East North Central division to 2.8% in New England. State-level errors varied to a much larger degree. For example, Ohio and California had very low MAPEs of 1.1% and 1.3%, respectively. A handful of states with smaller populations—for which results are not highlighted in the main text of this analysis—had substantially larger MAPE values. For 44 states, the MAPE was found to be below 10%, indicating relatively reliable predictive performance.
DISCUSSION
By disaggregating monthly trends, we found that unprecedented increases in overdose mortality occurred during the early months of pandemic in the United States. At the peak, overdose deaths in May 2020 were elevated by nearly 60% compared with the previous year, and the first 7 months of 2020 were overall elevated by 35% compared with the same period for 2019. To put this in perspective, if the final values through December 2020 were to be elevated by a similar margin, we would expect a total of 93 000 to 98 000 deaths to eventually be recorded for the year. Values for the remaining 5 months of 2020 have yet to be seen; however, it is very likely that 2020 will represent the largest year-to-year increase in overdose mortality in recent history for the United States.
The very sharp increases observed in this analysis highlight the value of more granular data for detecting shocks related to major disruptive events. In many cases, smoothed rolling aggregates tell a very different story from monthly values that highlight pandemic-related shocks. In future epidemiological surveillance efforts of overdose mortality, the presentation of monthly or weekly values alongside smoothed trends may be helpful for more fully characterizing the available data. While this may be difficult for states with small populations, we found that the majority of US states, all census divisions, and certainly national-level statistics have relatively small prediction errors when data are displayed in a monthly format.
More generally, the COVID-19 pandemic has highlighted issues related to the timely reporting of publicly available data for key public health issues. In the case of direct COVID-19 mortality, the pandemic proved that daily, public reporting of mortality is feasible, given sufficient governmental coordination and political will. Yet, for the nation’s overdose crisis—which has increased constantly over the past several decades and claimed nearly 600 000 American lives in the decade before the pandemic12—mortality statistics lag by considerable margins for many jurisdictions.
Furthermore, provisional national records do not include any details about the race, ethnicity, or other social characteristics of the people dying of overdose. Just as with direct COVID-19 mortality, overdose death data disaggregated by race/ethnicity are often available only at a significant lag compared with total numbers. This is especially concerning because recent trends suggest a rapidly shifting social profile of the US overdose crisis, with racial/ethnic minorities most affected.13–15 Communities of color are likely facing a dual burden of disproportionate COVID-19 mortality and rapidly rising overdose deaths during the pandemic, yet the depth of this issue cannot yet be described in the available data.
The rapid reporting of overdose mortality is complicated by numerous challenges. The detection and registration of overdose deaths can be delayed by backlogs in medical examiners’ or coroners’ offices, lengthy toxicological analyses, or other bottlenecks in data processing.10 Many important efforts have been undertaken by a number of states to improve the timeliness of overdose death reporting,16 but results remain heterogenous among locations, and overdose mortality reporting still lags behind that of other causes nationally.10 Further investments in data infrastructure for vital records systems are therefore warranted to improve the speed of reporting on this critical public health issue.
The results presented here provide public information characterizing national and regional trends in monthly overdose mortality more rapidly than they would otherwise be available. In addition, for states that do not already provide expedited public data releases—which include many of the states that we find had the largest increases during March through July 2020—the trends presented here may also represent the first publicly available monthly values. These data may be most helpful when considered together with other forms of rapid surveillance, such as syndromic surveillance tools drawing on EMS and emergency department data. These forms of data are available in many states with short lags. Similar information is provided by the CDC National Syndromic Surveillance Program5 and the National EMS Information System,2 which are national samples of emergency departments and EMS agencies, respectively. Although they represent proxies of overdose mortality, they are available much more rapidly than final mortality numbers and can therefore provide a very useful early warning system for rapid increases.4
Importantly, these early data resources, as well as other forms of real-time overdose surveillance, are often available to decision-makers much more rapidly than they are made publicly available. Although the sensitive nature of these data and reporting lags can understandably delay public reporting, we argue that in the context of a large magnitude and growing public health crisis such as overdose in the United States, public data transparency is paramount. Many groups working on issues related to overdose such as harm reduction and other community organizations may not have access to early epidemiological information unless they are made publicly available. In addition, public statistics often garner significant media attention and can galvanize political conversations, public support, and additional resources to address public health challenges.
Limitations
Our results are limited in several important ways. Perhaps most notably, provisional overdose statistics leverage models that assume that historical levels of reporting lags will continue. If underreporting was exacerbated by pandemic-related strain on public health data systems, then provisional CDC records and, subsequently, our results could underestimate the true level of monthly mortality. Our results should perhaps therefore be regarded as a conservative estimate of the true burden of overdose during the COVID-19 pandemic. Reported decreases following peaks in May 2020, perhaps in particular, should be interpreted with caution, as underreporting may have worsened during this period, artificially deflating overdose mortality estimates. A key area of future research will entail assessing how reporting lags differed during the pandemic, once final numbers are available. For a limited set of states with small numbers of overdose fatalities, our methods rely on assumptions to distribute deaths when state‒month counts are below 10. Our empirically derived prediction intervals reflect the degree of uncertainty introduced by these limitations, yet they should be considered for the potential to affect emergent trends. Also, given the observational nature of the results, we cannot ensure that our findings were directly caused by the COVID-19 pandemic. Although timing and ubiquity of increases during the initial stages of COVID-19‒related lockdowns are highly suggestive of the pandemic playing a key role, we cannot rule out other contemporaneous factors that may have also contributed to the increases during this period.
Public Health Implications
Assessing the driving forces behind large increases in overdose mortality during the pandemic will be a complicated task, and it remains an important area for further study. Social isolation is likely playing a role,2 with a greater proportion of individuals using substances alone, where they are less likely to receive life-saving help quickly in the event of an overdose. Treatment of substance use disorder, and other medical care, has also been disrupted during the pandemic.17 With treatment limited—and in a context of increased levels of social and economic stress—many individuals may turn to illicit markets to purchase substances, which are increasingly contaminated with unpredictable quantities of powerful synthetic opioids such as fentanyl.18 Pandemic-related disruptions to the illicit drug supply may have also accelerated this trend.19,20 Furthermore, many upstream structural drivers of addiction and overdose mortality—such as precarious access to housing, employment, quality education, and health care—have been sharply exacerbated during the pandemic.21,22 In the wake of COVID-19, the social and economic fallout may continue to drive increasing rates of overdose mortality and other “deaths of despair.”5,23
The drastic exacerbations of the US overdose crisis described here warrant renewed investments in overdose surveillance and prevention during the pandemic response and postpandemic recovery efforts. Lowering logistical and financial barriers to accessing substance use treatment is paramount. Proposed strategies include facilitating pharmacy-based methadone prescription,19 eliminating special requirements for the prescription of buprenorphine,24 and providing financial support for patients to pay for these often costly medications and related medical visits.25 In the context of widespread and increasing fentanyl prevalence in the illicit drug supply, making substance use safer is also a key objective.26,27 This can be accomplished through harm-reduction strategies such as increasing the availability of naloxone to reverse overdoses,28,29 providing “drug checking” services to test substances for the presence of illicit fentanyl,8,30 providing individuals with a safe supply of opioid medications known to be free of contaminants,31 and creating overdose-prevention sites where individuals can use in the presence of medical professionals prepared to reverse overdoses.32 Investments in upstream social determinants will also represent a key aspect of postpandemic recovery for the prevention of overdose and a host of other related, socially bound public health concerns.22,23 Finally, to ensure that such efforts are guided by the best possible information, continued investments in public, transparent, and actionable overdose surveillance remain of paramount importance to equip a broad range of decision-makers, frontline organizations, and community members to work on this growing public health challenge.
ACKNOWLEDGMENTS
J. Friedman received support from the UCLA Medical Scientist Training Program (National Institute of General Medical Sciences training grant GM008042).
The authors are grateful to David Schriger, MD, MPH, and Alex Bui, PhD, for helpful conversations related to this work.
CONFLICTS OF INTEREST
The authors report that they have no conflicts of interest.
HUMAN PARTICIPANT PROTECTION
This study was a secondary analysis of aggregated, publicly available statistics, and was therefore deemed exempt from institutional ethics review at UCLA.
Footnotes
See also Fliss et al., p. 1194.
REFERENCES
- 1.Katz J, Goodnough A, Sanger-Katz M. shadow of pandemic, US drug overdose deaths resurge to record. New York Times. July 15, 2020. https://www.nytimes.com/interactive/2020/07/15/upshot/drug-overdose-deaths.html. Accessed September 6, 2020.
- 2.Friedman J, Beletsky L, Schriger DL. Overdose-related cardiac arrests observed by emergency medical services during the US COVID-19 epidemic. JAMA Psychiatry. 2020 doi: 10.1001/jamapsychiatry.2020.4218. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Medical Association. Issue brief: Reports of increases in opioid- and other drug-related overdose and other concerns during COVID pandemic. Available at: https://www.ama-assn.org/system/files/2020-12/issue-brief-increases-in-opioid-related-overdose.pdf. Accessed November 15, 2020.
- 4.Slavova S, Rock P, Bush HM, Quesinberry D, Walsh SL. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug Alcohol Depend. 2020;214:108176. doi: 10.1016/j.drugalcdep.2020.108176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holland KM, Jones C, Vivolo-Kantor AM et al. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiatry. 2021 doi: 10.1001/jamapsychiatry.2020.4402. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.North Carolina Department of Health and Human Services, Division of Public Health. IVP Branch: poisoning data. Available at: https://www.injuryfreenc.ncdhhs.gov/DataSurveillance/Poisoning.htm. Accessed February 13, 2021.
- 7.California Department of Public Health. California Opioid Overdose Surveillance Dashboard. Available at: https://skylab.cdph.ca.gov/ODdash. Accessed March 30, 2021.
- 8.Centers for Disease Control and Prevention. Increase in fatal drug overdoses across the United States driven by synthetic opioids before and during the COVID-19 pandemic. Health Alert Network. HAN–00438. December 17, 2020. Available at: https://emergency.cdc.gov/han/2020/han00438.asp. Accessed December 25, 2020.
- 9.National Center for Health Statistics. Provisional drug overdose death counts. Vital Statistics Rapid Release. December 8, 2020. Available at: https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm. Accessed December 25, 2020.
- 10.Spencer MR, Ahmad F. Timeliness of death certificate data for mortality surveillance and provisional estimates. Vital Statistics Rapid Release. Report No. 1. December 2016. Available at: https://www.cdc.gov/nchs/data/vsrr/report001.pdf. Accessed March 30, 2021.
- 11.Rossen LM, Ahmad F, Spencer MR, Warner M, Sutton P. Methods to adjust provisional counts of drug overdose deaths for underreporting. Vital Statistics Rapid Release . Report No. 6. August 2018. Available at: https://www.cdc.gov/nchs/data/vsrr/report006.pdf. Accessed March 30, 2021.
- 12.Centers for Disease Control and Prevention. CDC WONDER. Available at: https://wonder.cdc.gov. Accessed December 30, 2020.
- 13.Spencer M, Warner M, Bastian BA, Trinidad JP, Hedegaard H. Drug overdose deaths involving fentanyl, 2011–2016. March 21, 2019. National Center for Health Statistics. Available at: https://stacks.cdc.gov/view/cdc/77832. Accessed November 15, 2020. [PubMed]
- 14.James K, Jordan A. The opioid crisis in Black communities. J Law Med Ethics. 2018;46(2):404–421. doi: 10.1177/1073110518782949. [DOI] [PubMed] [Google Scholar]
- 15.Hansen H, Netherland J. Is the prescription opioid epidemic a White problem? Am J Public Health. 2016;106(12):2127–2129. doi: 10.2105/AJPH.2016.303483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Enhanced state opioid overdose surveillance. October 15, 2020. Available at: https://www.cdc.gov/drugoverdose/foa/state-opioid-mm.html. Accessed February 13, 2021.
- 17.Herring AA, Kalmin M, Speener M et al. Sharp decline in hospital and emergency department initiated buprenorphine for opioid use disorder during COVID-19 state of emergency in California. J Subst Abuse Treat. 2021;123:108260. doi: 10.1016/j.jsat.2020.108260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ciccarone D. Fentanyl in the US heroin supply: a rapidly changing risk environment. Int J Drug Policy. 2017;46:107–111. doi: 10.1016/j.drugpo.2017.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wakeman SE, Green TC, Rich J. An overdose surge will compound the COVID-19 pandemic if urgent action is not taken. Nat Med. 2020;26(6):819–820. doi: 10.1038/s41591-020-0898-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beletsky L, Davis CS. Today’s fentanyl crisis: Prohibition’s Iron Law, revisited. Int J Drug Policy. 2017;46:156–159. doi: 10.1016/j.drugpo.2017.05.050. [DOI] [PubMed] [Google Scholar]
- 21.Bambra C, Riordan R, Ford J, Matthews F. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health. 2020;74(11):964–968. doi: 10.1136/jech-2020-214401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dasgupta N, Beletsky L, Ciccarone D. Opioid crisis: no easy fix to its social and economic determinants. Am J Public Health. 2018;108(2):182–186. doi: 10.2105/AJPH.2017.304187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arena PJ, Malta M, Rimoin AW, Strathdee SA. Race, COVID-19 and deaths of despair. EClinicalMedicine. 2020;25:100485. doi: 10.1016/j.eclinm.2020.100485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stancliff S, Greene D, Zucker HA. Why 24 state and territorial health officials support buprenorphine deregulation. Am J Public Health. 2019;109(12):1678–1679. doi: 10.2105/AJPH.2019.305370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaplan-Dobbs M, Kattan JA, Tuazon E, Jimenez C, Saleh S, Kunins HV. Increasing access to buprenorphine in safety-net primary care clinics: the New York City Buprenorphine Nurse Care Manager Initiative. Am J Public Health. 2021;111(2):215–218. doi: 10.2105/AJPH.2020.306000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shover CL, Falasinnu TO, Dwyer CL et al. Steep increases in fentanyl-related mortality west of the Mississippi River: recent evidence from county and state surveillance. Drug Alcohol Depend. 2020;216:108314. doi: 10.1016/j.drugalcdep.2020.108314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Burris S. Research on the effects of legal health interventions to prevent overdose: too often too little and too late. Am J Public Health. 2020;110(6):768–770. doi: 10.2105/AJPH.2020.305678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Doe-Simkins M, Walley AY, Epstein A, Moyer P. Saved by the nose: bystander-administered intranasal naloxone hydrochloride for opioid overdose. Am J Public Health. 2009;99(5):788–791. doi: 10.2105/AJPH.2008.146647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Green TC, Davis C, Xuan Z, Walley AY, Bratberg J. Laws mandating coprescription of naloxone and their impact on naloxone prescription in five US States, 2014–2018. Am J Public Health. 2020;110(6):881–887. doi: 10.2105/AJPH.2020.305620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reed MK, Roth AM, Tabb LP, Groves AK, Lankenau SE. “I probably got a minute”: Perceptions of fentanyl test strip use among people who use stimulants. Int J Drug Policy. 2021 doi: 10.1016/j.drugpo.2021.103147. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ivsins A, Boyd J, Beletsky L, McNeil R. Tackling the overdose crisis: the role of safe supply. Int J Drug Policy. 2020;80:102769. doi: 10.1016/j.drugpo.2020.102769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Beletsky L, Baker P, Arredondo J et al. The global health and equity imperative for safe consumption facilities. Lancet. 2018;392(10147):553–554. doi: 10.1016/S0140-6736(18)31469-7. [DOI] [PubMed] [Google Scholar]


