Abstract
Objectives. To explore whether beneficial health care policies, when implemented in the context of gender inequality, yield unintended structural consequences that stigmatize and ostracize women with HIV from “what matters most” in local culture.
Methods. We conducted 46 in-depth interviews and 5 focus groups (38 individuals) with men and women living with and without HIV in Gaborone, Botswana, in 2017.
Results. Cultural imperatives to bear children bring pregnant women into contact with free antenatal services including routine HIV testing, where their HIV status is discovered before their male partners’. National HIV policies have therefore unintentionally reinforced disadvantage among women with HIV, whereby men delay or avoid testing by using their partner’s status as a proxy for their own, thus facilitating blame toward women diagnosed with HIV. Gossip then defines these women as “promiscuous” and as violating the essence of womanhood. We identified cultural and structural ways to resist stigma for these women.
Conclusions. Necessary HIV testing during antenatal care has inadvertently perpetuated a structural vulnerability that propagates stigma toward women. Individual- and structural-level interventions can address stigma unintentionally reinforced by health care policies.
In Botswana, which has among the highest HIV prevalences worldwide (∼20%),1 national health care policies to reduce barriers to HIV services are necessary and beneficial strategies to address population burden of HIV. Such policies could also mitigate HIV stigma by making testing and treatment more socially normative.2, 3 Yet universal policies unintentionally risk benefitting socially privileged groups more than less privileged ones.4 In Botswana and many regions of sub-Saharan Africa (SSA), gender inequality means women experience higher risk for and prevalence of HIV.5 Because being associated with HIV results in stigma—which powerfully impedes antiretroviral therapy (ART) adherence6—untoward consequences for disenfranchised groups including women could be created.7 These dynamics can be investigated using theoretical perspectives that consider how unintentional disadvantage results from structural factors like health care policies (i.e., structural vulnerability framework) and interacts with culturally based stigma that excludes individuals from activities that “matter most” in everyday life (i.e., “what matters most” [WMM] stigma framework).
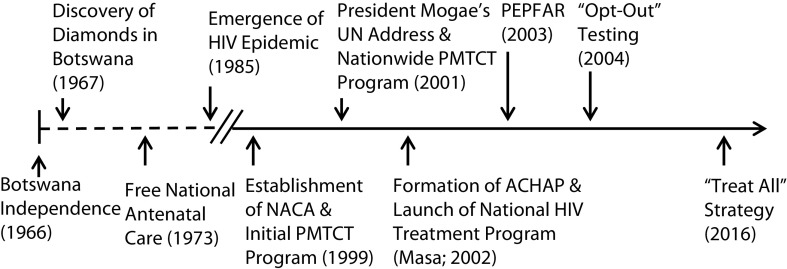
Botswana has implemented policies to address the HIV epidemic, notably a 2001 nationwide program to prevent mother-to-child transmission of HIV, followed in 2002 by routine HIV testing and universal access to ART (Figure 1), including in antenatal settings. These policies represent landmark public health achievements to address HIV in SSA; however, as a result of the epidemic’s urgency, stakeholder perspectives were not assessed before implementation.8 Thus, whether these vital policies could unintentionally reinforce disadvantaged positions for certain groups has not been examined. Botswana’s confluence of HIV policies and free antenatal care (since 1973) could inadvertently make women susceptible to structurally perpetuated HIV stigma.
FIGURE 1—
Timeline for Implementation of Policies to Address the HIV Epidemic in Botswana
Notes. ACHAP = African Comprehensive HIV/AIDS Partnership; NACA = National AIDS Coordinating Agency; PEPFAR = President’s Emergency Plan for AIDS Relief; PMTCT = prevention of mother-to-child transmission.
Gender inequality exacerbates HIV stigma for women in high-, middle-, and low-income contexts.7 In Botswana and SSA, HIV is linked with culturally based conceptions of promiscuity and immorality among women that elicit fears9 of abandonment by partners10 and impair ART adherence.9,11–13 Women with HIV are blamed for contracting it,11,14 as women are held accountable for any family wrongdoing.14,15 Detecting HIV during pregnancy may powerfully elicit these stigma dynamics, challenging ART adherence during pregnancy, postpartum,11 and throughout adulthood.12,13 However, to our knowledge, no studies have examined how positive policies could unintentionally intensify HIV stigma; studies of structural stigma instead focus on policies that perpetuate stigma (e.g., separate HIV clinics).
The structural vulnerability framework can help elucidate how beneficial HIV policies could reinforce preexisting vulnerabilities for women with HIV in Botswana. Drawing upon structural violence,16 structural vulnerability encompasses the political and institutional forces that constitute structural disadvantage17 produced via positions within relationships of power. Because of attributed promiscuity and immorality for women with HIV, health care policies could intensify disadvantage to locate these women in severely marginalized positions.18 Structurally vulnerable groups can internalize their devalued status (e.g., via self-concept),19 illuminating how structural circumstances could interact with local cultural processes of stigma.
Stigma has broad consequences for individuals, groups, and societies.20 Elucidating how cultural dynamics intersect to elicit structural vulnerability and stigma can be advanced via a theory that articulates how culture shapes stigma.21 According to the WMM framework, stigma is felt most acutely when people are unable to participate in the activities that “matter most” and determine “personhood” in their culture. Building upon research in Botswana and West Africa22 identifying that “a woman becomes a woman when she becomes able to bear children,”22 we proposed that achieving full status for women in Botswana is expressed by being a mother, which involves bearing and caring for children. We thus conceptualized that HIV stigma is most powerfully felt by threatening these cultural capabilities that determine “full womanhood.” The WMM perspective also identifies how cultural capabilities protect against HIV stigma; a woman with HIV who fulfills the capabilities of being a “good mother” (e.g., raising children in culturally endorsed ways) could effectively resist stigma.
Important intersections between culturally based dynamics and health care policies require clarification: do health care policies differentially elicit HIV identification among certain groups, thus reinforcing culturally based stigma? Moreover, does culturally based stigma increase the likelihood that certain groups will be disadvantaged by health care policies from the outset? Concurrently, we considered whether and how cultural dynamics associated with “being a good mother” could enable resistance to HIV stigma. We employed the structural vulnerability and WMM frameworks via deductive qualitative analysis, hypothesizing that gendered structural vulnerability and stigma interact with HIV policies for women living with HIV in Botswana. Our study represents a necessary evolution from evaluating policies for reducing the population burden of HIV to considering their sociocultural impacts upon disadvantaged groups.
METHODS
We used purposive sampling to recruit respondents (n = 84) for (1) 5 focus groups (FGs; n = 38), and (2) 46 in-depth, semistructured interviews (IDIs; Table 1). Because the interpersonal engagements that “matter most” are shared by the stigmatized (i.e., persons living with HIV/AIDS [PLWHA]) and stigmatizers (i.e., those not necessarily identified with HIV), both FGs and IDIs included PLWHA and community respondents with unknown HIV status. Men and women were sampled equally; while women’s perspectives were prioritized, we assessed men to determine whether they agreed. In 2017, we recruited PLWHA from a large, publicly funded HIV clinic and community respondents from the Main Mall in Gaborone, Botswana. Written informed consent was obtained. Participants were compensated approximately US $5.
TABLE 1—
Sociodemographic Characteristics of Participants at Baseline: Botswana, Africa, 2017
| Baseline Characteristic | Full Sample (n = 84), No. (%) or Mean ±SD | Female (n = 43), No. (%) or Mean ±SD | Male (n = 41), No. (%) or Mean ±SD |
| Interview method | |||
| Individual interviews | 46 (54.8) | 23 (53.4) | 23 (56.1) |
| Focus group participant | 38 (45.2) | 20 (46.6) | 18 (43.9) |
| HIV status | |||
| Living with HIV | 45 (53.6) | 24 (55.8) | 21 (51.2) |
| HIV status unknown | 39 (46.4) | 19 (44.2) | 20 (48.8) |
| Age, y | 41.8 ±13.1 | 42.2 ±12.5 | 41.4 ±14.1 |
| Education | |||
| < 7 y (< Form 1) | 17 (20.2) | 7 (16.3) | 10 (24.4) |
| ≥ 7 y (≥ Form 1) | 54 (64.3) | 29 (67.4) | 25 (61.0) |
| Unknown | 13 (15.5) | 7 (16.3) | 6 (14.6) |
| Employment | |||
| Unemployed | 29 (34.5) | 20 (46.5) | 9 (22.0) |
| Employed or self-employed | 43 (51.2) | 14 (32.6) | 29 (70.7) |
| Retired | 1 (1.2) | 0 (‒) | 1 (2.4) |
| Unknown | 11 (13.1) | 9 (20.9) | 2 (4.9) |
| Relationship status | |||
| Married or cohabitating | 21 (25.0) | 8 (18.6) | 13 (31.7) |
| Single | 43 (51.2) | 24 (55.8) | 19 (46.4) |
| Single with partner | 12 (14.3) | 6 (14.0) | 6 (14.6) |
| Unknown | 8 (9.5) | 5 (11.6) | 3 (7.3) |
| Children, no. | 2.2 ±1.0 | 2.2 ±1.1 | 2.2 ±1.0 |
Data Collection
FGs and IDIs were used sequentially. First, separate male and female FGs (4‒10 participants each) were held with PLWHA and community respondents (90‒120 minutes each) to elicit core themes. Sessions were conducted in private rooms in the HIV clinic (for known PLWHA; hereafter, “known HIV status”) and a community center (for community respondents). FGs were facilitated by the principal investigator (L. H. Y.) alongside a Setswana-speaking research assistant. FGs were used to iteratively modify the IDI guide by adding probes to questions; IDIs were then used to capture in-depth responses to core themes. Three senior interviewers (L. H. Y., M. B. B., and M. M. E.) trained 4 bilingual research assistants to conduct IDIs in Setswana or English, per interviewee preference (60‒90 minutes each). Sessions were audio-recorded, transcribed, and, if needed, translated into English.
Drawing from studies that elicited WMM and structural vulnerability,21,23 FG and IDI guides were adapted from the Devaluation‒Discrimination Scale24 using 6 original, plus 3 culturally tailored, items (Appendix A, available as a supplement to the online version of this article at http://www.ajph.org). These guides assessed perceptions of community stereotypes (e.g., blameworthiness) and how stigma affected participation in work, dating, and interactions with friends and family. One item assessed how health care policies could shape HIV identification and stigma (i.e., when a woman or man typically finds out they are HIV positive). One question elicited narratives describing personhood (i.e., being a proper woman in Botswana); in addition, respondents could spontaneously articulate examples illustrating WMM for each item.
Analysis
We used a primarily deductive qualitative analysis via a 2-step direct content analysis approach,25,26 which is suitable because it seeks to conceptually extend existing theoretical frameworks and utilizes theory to focus the research questions and guide initial codes. This primarily deductive approach (step 1) was followed by selected inductive analyses (step 2):
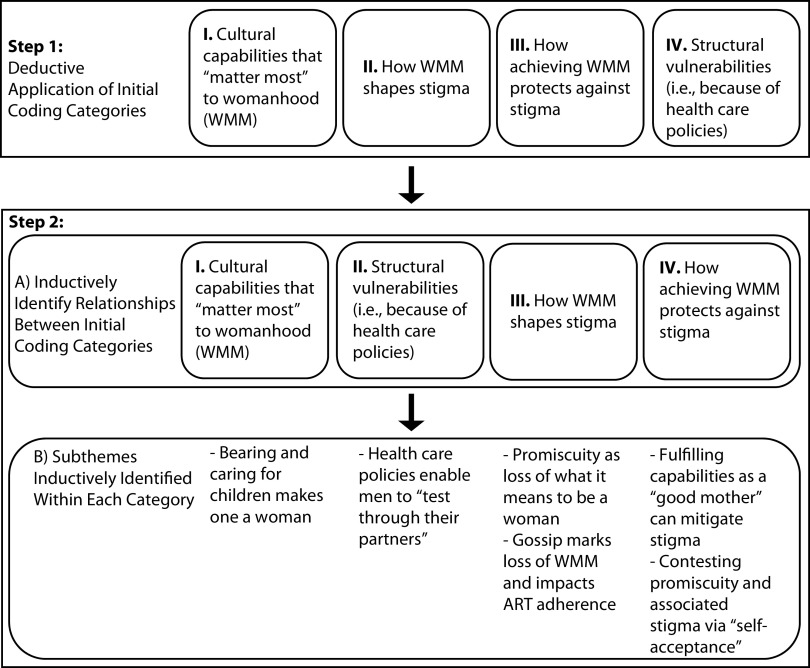
Step 1. Operationally defining coding categories. First, we identified initial codes from previously formulated theoretical analyses illustrating how stigma was worsened (or mitigated) in relation to WMM and how disparities could be perpetuated via structural vulnerability.27 We thereby identified when participants described key concepts of WMM and structural vulnerability as initial coding categories. Coders independently and deductively assigned predetermined categories to passages describing (1) cultural capabilities that “matter most” to womanhood (WMM), (2) how WMM shapes stigma, (3) how achieving WMM protects against stigma, and (4) structural vulnerabilities (i.e., attributable to health care policies; Figure 2, Step 1). Two coding pairs independently discussed 2 FG transcripts over 6 meetings and formulated theoretically based, operational definitions for each deductive category (Box 1). These definitions were used by 2 additional coding pairs (4 pairs total) to independently code remaining transcripts (3 FGs; 46 IDIs); pairs resolved discrepancies through consensus. Incorporated within our deductive approach, we also searched for disconfirming evidence within each category. Codes were presented to the multidisciplinary team (including a researcher and policy contributor [A. R. H.], a Botswana-based physician [T. A.-M.] and a counselor and native Botswana expert [S. R.]) during 70 calls (∼70 hours) over 18 months.
FIGURE 2—
Qualitative Analytic Approach Examining Key Concepts of “What Matters Most” and Structural Vulnerability
Note. ART = antiretroviral therapy; WMM = “what matters most.”
BOX 1—
Operational Definition of Coding Categories for “What Matters Most” and Structural Vulnerability
| Category | Operational Definition |
| Cultural capabilities that “matter most” to womanhood (“what matters most”) | Participating in the activities or capabilities that determine “personhood” (or “womanhood”) in Botswana by achieving full status as a woman including (but not limited to) being a mother, which involves bearing, raising, and caring for children; caring for and respecting her husband; and ensuring the well-being of the household. |
| How “what matters most” shapes HIV stigma | The ways in which the stigma of being identified as having HIV, via attributions of promiscuity and immorality, exerts its effects by threatening the capabilities that determine “full womanhood” in Botswana, including (but not limited to) being a mother, caring for her husband, and ensuring the well-being of the household. Includes core mechanisms that enabled culturally based stigma to persist, and ways in which these mechanisms impaired antiretroviral therapy adherence. |
| How achieving “what matters most” protects against HIV stigma | The ways in which achieving cultural capabilities can protect against HIV stigma; in other words, how HIV stigma can be potentially mitigated if a woman with HIV in Botswana fulfills the capabilities of being a “good mother” (including, but not limited to, bearing and raising children in culturally endorsed ways). Includes other ways in which stigma and attributions of promiscuity were contested outside of motherhood. |
| Structural vulnerability (health care policies reinforcing vulnerabilities) | The ways in which health care policies can inadvertently reinforce and intensify the marginalization associated with HIV identification to locate women differentially within disadvantaged hierarchical positions, either in the health care system or society at large. This includes the internalization of attributed devalued status via behaviors and self-concept. |
Step 2. Formulating relationships between categories and establishing subthemes. Second, we inductively identified relationships between categories28 to elucidate how structural conditions intersected with WMM to perpetuate positions of disadvantage27; we also explored whether culturally based stigma shaped structural vulnerability to health care policies. A subteam (L. H. Y., O. B. P., and S. R.) met 13 times (∼26 hours) to establish relationships between categories. This led to a conceptual reordering of categories, such that achieving WMM was identified as initiating earlier HIV testing and diagnosis for women (via structural vulnerability from health care policies); identification as having HIV then reinforced culturally based stigma (Figure 2, Step 2). This subteam then inductively formulated subthemes within each category, which were only retained when agreement was unanimous (Figure 2). Finally, subthemes were presented to the multidisciplinary team for refinement.
RESULTS
The conceptually reordered categories, and illustrative subthemes (Figure 2, step 2), are detailed here.
“What Matters Most” Among Batswana Women
Bearing and caring for children was essential to the concept of womanhood. Because this represented a fundamental capability signifying what was “most at stake” for women, to be childless initiated gossip about one’s “wholeness”:
With women, if you don’t have children, you are not really a woman. (Woman, known HIV status, IDI)
If you don’t have kids and are single, they [community members] don’t respect you. . . . They will gossip, “you are a barren woman, you don’t bear children, you are like a bull in a kraal [your purpose is to bear children], but you are a woman [you are denying your purpose].” (Woman, known HIV status, IDI)
Men agreed that women’s perceived competence in caretaking for children determined social standing:
A proper woman is judged in the community; [her standing] is reflected by the way she takes care of her children, especially bathing them, making sure they have food and go to school. . . . (Man, known HIV status, FG)
In upholding womanhood, women were viewed as the foundation of the household:
Someone said “The woman is the foundation,” because as a woman you are the one who has to care for the home, husband, and kids . . . that’s why most of the blame is placed on the woman [if she is promiscuous]. (Woman, known HIV status, FG)
When we examined disconfirming evidence, the centrality of marriage (although not motherhood) appeared to be weakening among a minority of women and warrants further investigation.
Structural Vulnerability Via Health Policies
Women’s core duties to bear and care for children intersected with structural vulnerability via health care policies offering free antenatal care accompanied by routine HIV testing; accordingly, HIV identification first occurred when women underwent HIV testing during pregnancy:
Most women found it [their HIV status] due to pregnancy and tests were done, and most men came into the hospital when they were weak; that is when they got diagnosed with HIV. (Man, known HIV status, IDI)
Following structurally initiated identification of HIV status, both genders noted that men used women’s testing as a proxy for their own status, enabling men to intentionally delay or completely avoid testing:
Men are reluctant to test, but women are required to do a routine HIV test during prenatal care. It’s not like men aren’t sick; it’s only that they don’t go for testing since they rely on the women’s status and assume it’s the same as theirs. (Woman, unknown HIV status, FG)
People are reluctant to test; women would mostly know [their HIV status] when they are pregnant. It’s compulsory that when you’re pregnant, you should go for tests. . . . Men are also reluctant to test, they would mostly go if their pregnant partner has also tested [and had HIV]; they basically rely on their partner’s results. (Man, known HIV status, IDI)
These structural conditions reinforce blame toward the individual officially diagnosed with HIV (i.e., female partner).
Stigma Shapes “What Matters Most”
Health care policies, by eliciting earlier HIV identification and blame for women, reinforced stigma that jeopardized the capabilities that “mattered most.”
Promiscuity as loss of what it means to be a woman. Stigma did not ensue solely with HIV status; instead, promiscuity was routinely attributed to women with HIV that molded their experience of stigma:
They [other people] think that someone living with HIV was very sexually active and promiscuous even though they may be wrong, they don’t think of other ways of HIV transmission. Batswana mostly think that if you have HIV, then it means you had unprotected sex with multiple partners. (Woman, known HIV status, FG)
Via perceived promiscuity and neglect of duties, gender-based stigma was exacerbated following HIV identification. Because of perceived disregard of WMM, women were judged as blameworthy for violating the essence of womanhood:
We take it that a woman belongs to the home, so we wonder if she has HIV, there is no woman in her. She is a lebelete [whore]; there is no woman. (Man, known HIV status, IDI)
The responsibility would be on the woman that she’s the one who’s at fault. . . . Even if I stay at home and he [male partner] is [going] around with many women, his family will say that I’m the one who gave him HIV. (Woman, known HIV status, IDI)
Gossip marks loss of “what matters most” and affects antiretroviral therapy adherence. Gossip emerged as the key cultural mechanism that marked loss of “womanhood.” Gossip’s effects were enduring and made community reintegration extremely challenging:
As a victim you will not forget [being called HIV positive] . . . there is a Setswana saying that, the perpetrator could forget, but the victim doesn’t forget (i.e., “a word that goes out of mouth never returns empty”) . . . you will never forget. (Women, known HIV status, IDI)
Gossip, and fear of its consequences, could threaten women’s capabilities to form romantic partnerships, jeopardizing the process by which “womanhood” is achieved:
They [neighbors] will gossip [about my HIV status]. . . . They will come to that person [my boyfriend] and say, “Hey why do you want that girl, she’s dangerous, she will infect you. . . .” He [boyfriend] never came [back]. (Woman, known HIV status, IDI)
Women’s attempts to avoid gossip, such as avoiding being seen at an HIV clinic, could compromise ART adherence:
Women, they seem to get hurt more when being gossiped about. . . . A woman can stop going to take medications, either completely or somewhere along the way. . . . My elder sister was going to take ARVs [antiretrovirals] at the clinic and she started seeing people she knew at the village . . . people were saying that they see that she takes medication. So she stopped going; she only started going back when her health became so bad that she had to go. (Woman, unknown HIV status, FG)
Achieving “What Matters Most” Reduces Stigma
Both genders reported that possessing the capabilities to fulfill “motherhood” could enable resistance to stigma:
I think the lady who is HIV positive, who’s got kids is much better [off than a childless, HIV-negative woman]. (Woman, known HIV status, IDI)
The woman who has HIV will be treated better, having children [than a childless, HIV-negative woman]. . . . Because that person has dignity. (Man, unknown HIV status, FG)
Fulfilling cultural capabilities central to “womanhood” could, in the absence of explicit promiscuity, preserve standing as a “whole woman”:
As long as the woman keeps [cares for] all the children like before [bathing, feeding, and ensuring they attend school], and nobody actually witnessed her sleeping around, and it happens that she’s HIV positive, and she stays that way [as a caretaker], people won’t change how they view her as a woman. (Man, known HIV status, IDI)
Contesting promiscuity and associated stigma via self-acceptance. Although not directly rooted in WMM via motherhood, an alternate means to resist gossip’s effects, achieved by some women, was to adopt self-acceptance (or “to be free”) by coming to terms with one’s status:
Gossip doesn’t affect me; personally I’m proud living with this disease [HIV] because I feel I have never been promiscuous in any way. . . . These people [like me] have accepted themselves, that they’re living with HIV. (Woman, known HIV status, IDI)
Yet this strategy was most effective when persons with a professional status were involved in promoting “self-acceptance”:
He/she will need social workers; they’re the ones who can manage because it’s their professional duty . . . that person [PLWHA] will “be free” [accept themselves] by talking to that person [social worker]; it’s not the same as when just a regular person does it [helps someone to accept themselves]. (Man, known HIV status, IDI)
DISCUSSION
Our theoretically informed qualitative approach revealed how beneficial health care policies can unintentionally reinforce stigma among groups who face structural vulnerability. Previous studies have suggested that universal provision of HIV care could ameliorate stigma by making HIV testing and treatment more routine.2,3 Yet we found that Botswana’s convergence of universal HIV testing and treatment with free nationwide antenatal care inadvertently generated structural vulnerability by eliciting earlier HIV identification for women, allowing male partners to forgo identification and avoid stigma. HIV diagnosis thus perpetuates blame toward women, leading them to bear the brunt of stigma. Our results yielded novel bidirectional findings, wherein the cultural dynamics of WMM influenced susceptibility to structural vulnerability posed by health care policies—attempting to achieve WMM (i.e., have children) increased the likelihood of structural vulnerability (i.e., antenatal HIV testing leading to diagnosis); this then perpetuated further vulnerability by activating perceptions of promiscuity and blame that jeopardized women’s capabilities to achieve WMM.
The WMM lens also extends findings27 regarding how culture shapes stigma. Per other studies,29 gossip comprised the main cultural mechanism marking women as promiscuous, blameworthy, and no longer meriting status as “whole women.” Nonetheless, identifying women’s urgency to preserve “womanhood” clarified why gossip’s effects (including abandonment by male partners) were so feared that some women risked ART nonadherence. Furthermore, the WMM framework provided a new way of conceptualizing how the capabilities that were most at stake (i.e., bearing and raising children) could protect women against HIV stigma; this conceptualization has received recent psychometric support.30 Our findings extend studies in SSA whereby resistance to HIV stigma was engendered by participating in valued social roles31 by identifying these cultural roles in the Botswana context.
Identifying how health care policies can inadvertently perpetuate stigma offers insights to rectify resulting inequities. We propose 2 strategies: the first to immediately mitigate this structurally reinforced stigma, and the second to evolve HIV policy from its initial emergency response toward sustained, antistigma-based care to promote social integration. First, individual-level interventions for pregnant women with HIV can be implemented to reduce stigma and improve ART adherence. For example, our team’s intervention integrates empirically based antistigma strategies with promoting the capabilities of WMM (e.g., being a good mother, promoting self-acceptance)32 to resist stigma.
Second, we propose acting at the site where structural vulnerability is reinforced by revising HIV policy to further integrate antistigma interventions into free nationwide antenatal services. In addition to the previously mentioned individual- and structural-level strategies for women, gender transformative interventions with men are needed to address inequitable gender norms33 that are further reified by enabling men to avoid testing; this could be further augmented by disseminating gender transformative messages via traditional (e.g., TV dramas) and social media that model equitable behaviors. As men do not visit health care facilities, structural change can also be achieved by integrating regular HIV testing and treatment into community spaces where men frequent (e.g., workplace, farms, bars, and shebeens).34 This structural change can facilitate gender parity for men in HIV testing, potentially shifting blame from female partners at the outset. Incorporating gender-informed HIV stigma reduction programs during schools’ existing sexual and reproductive curricula could further help reach adolescents of both genders before antenatal testing. We propose engaging stakeholders at multiple levels, including women with HIV and men in the community, in dialogue with policymakers and health care providers to reverse this unintended structural vulnerability from existing HIV policies while underscoring potential structural harms that could otherwise be perpetuated, including stigma.
Study limitations included sampling restricted to urban participants, which may underrepresent traditional views regarding the capabilities that “matter most” for women. While using deductive analysis may increase likelihood of finding supportive evidence, we mitigated this by searching for disconfirming evidence and having a binational, multidisciplinary team evaluate the findings. We included theoretically justified samples of men and women with known and unknown HIV status, which provided diverse perspectives to corroborate the aforementioned structural vulnerability for women; despite this, much of the confirmatory evidence was derived from people with known HIV status via IDIs, reflecting stigma’s salience in their lives. While we looked for differences by gender, we detected no major discrepancies in themes. Although we could have included other stakeholders, we focused on those most severely experiencing structurally perpetuated stigma and its consequences.
Our study is among the first to our knowledge to indicate how structural vulnerability to culturally based forms of stigma could be unintentionally reinforced by otherwise effective health care policies. In addition, the intersectional identities35 of being a woman and living with HIV, experienced within this context of structural vulnerability, produced a distinct lived experience of stigma within Setswana culture that should be considered in its entirety. As a leader in increasing access to lifesaving HIV services, Botswana can now take the lead in evolving biomedical HIV policies toward considering their sociocultural impacts. Insights gained from the WMM framework, including intersections with structural vulnerability, promise to facilitate beneficial structural changes in Botswana and across SSA to address these unintended inequities.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
ACKNOWLEDGMENTS
This research was supported by a grant and core support services from the Penn Mental Health AIDS Research Center, a National Institutes of Health (NIH)‒funded program (P30MH097488); a Fogarty International Center and National Institutes of Mental Health R21 grant (TW011084-01; PI: L. H. Yang); and the Focus for Health Foundation. O. B. Poku is supported by the T32 Global Mental Health Training Program at the Bloomberg School of Public Health, Department of Mental Health (5T32MH1032). The study also benefited from core support services provided by the Penn Center for AIDS Research, an NIH-funded program (P30AI045008).
We wish to thank the staff of the Princess Marina Hospital Infectious Disease Care Clinic, Vincent Ikageng Dipatane, MBBS, Letumile Rodgers Moeng, MD, Calvin Gonte, and Tuhto Salepito for supporting recruitment and data collection. We thank Evan Eschliman for his help with formatting.
HUMAN PARTICIPANT PROTECTION
Institutional review boards of the Botswana Ministry of Health, University of Botswana, Princess Marina Hospital, University of Pennsylvania, and New York University granted study approval.
Footnotes
See also Galea and Vaughan, p. 1202.
REFERENCES
- 1.UNAIDS. Botswana. 2019. Available at: https://www.unaids.org/en/regionscountries/countries/botswana. Accessed November 6, 2020.
- 2.Chan BT, Tsai AC, Siedner MJ. HIV treatment scale-up and HIV-related stigma in sub-Saharan Africa: a longitudinal cross-country analysis. Am J Public Health. 2015;105(8):1581–1587. doi: 10.2105/AJPH.2015.302716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wolfe WR, Weiser SD, Leiter K et al. The impact of universal access to antiretroviral therapy on HIV stigma in Botswana. Am J Public Health. 2008;98(10):1865–1871. doi: 10.2105/AJPH.2007.122044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.White M, Adams J, Heywood P. How and why do interventions that increase health overall widen inequalities within populations? In: Babones SJ, editor. Social Inequality and Public Health. Bristol, England: Bristol University Press; 2009. pp. 65–82. [DOI] [Google Scholar]
- 5.Phaladze N, Tlou S. Gender and HIV/AIDS in Botswana: a focus on inequalities and discrimination. Gend Dev. 2006;14(1):23–35. doi: 10.1080/13552070500518095. [DOI] [Google Scholar]
- 6.Rueda S, Mitra S, Chen S et al. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: a series of meta-analyses. BMJ Open. 2016;6(7):e011453. doi: 10.1136/bmjopen-2016-011453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Monteiro SS, Villela WV, Soares PS. The interaction between axes of inequality in studies on discrimination, stigma and HIV/AIDS: contributions to the recent international literature. Glob Public Health. 2013;8(5):519–533. doi: 10.1080/17441692.2013.779738. [DOI] [PubMed] [Google Scholar]
- 8.Ramogola-Masire D, Poku O, Mazhani L et al. Botswana’s HIV response: policies, context, and future directions. J Community Psychol. 2020;48(3):1066–1070. doi: 10.1002/jcop.22316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turan JM, Nyblade L. HIV-related stigma as a barrier to achievement of global PMTCT and maternal health goals: a review of the evidence. AIDS Behav. 2013;17(7):2528–2539. doi: 10.1007/s10461-013-0446-8. [DOI] [PubMed] [Google Scholar]
- 10.Oyugi JH, Byakika-Tusiime J, Ragland K et al. Treatment interruptions predict resistance in HIV-positive individuals purchasing fixed-dose combination antiretroviral therapy in Kampala, Uganda. AIDS. 2007;21(8):965–971. doi: 10.1097/QAD.0b013e32802e6bfa. [DOI] [PubMed] [Google Scholar]
- 11.Currier JS, Britto P, Hoffman RM et al. Randomized trial of stopping or continuing ART among postpartum women with pre-ART CD4≥ 400 cells/mm3. PLoS One. 2017;12(5):e0176009. doi: 10.1371/journal.pone.0176009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clouse K, Pettifor A, Shearer K et al. Loss to follow-up before and after delivery among women testing HIV positive during pregnancy in Johannesburg, South Africa. Trop Med Int Health. 2013;18(4):451–460. doi: 10.1111/tmi.12072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ngarina M, Popenoe R, Kilewo C, Biberfeld G, Ekstrom AM. Reasons for poor adherence to antiretroviral therapy postnatally in HIV-1 infected women treated for their own health: experiences from the Mitra Plus study in Tanzania. BMC Public Health. 2013;13(1):450. doi: 10.1186/1471-2458-13-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schuklenk U, Kleinsmidt A. Rethinking mandatory HIV testing during pregnancy in areas with high HIV prevalence rates: ethical and policy issues. Am J Public Health. 2007;97(7):1179–1183. doi: 10.2105/AJPH.2006.093526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Denison JA, McCauley AP, Dunnett-Dagg WA, Lungu N, Sweat MD. The HIV testing experiences of adolescents in Ndola, Zambia: do families and friends matter? AIDS Care. 2008;20(1):101–105. doi: 10.1080/09540120701427498. [DOI] [PubMed] [Google Scholar]
- 16.Galtung J. Violence, peace, and peace research. J Peace Res. 1969;6(3):167–191. doi: 10.1177/002234336900600301. [DOI] [Google Scholar]
- 17.Quesada J, Hart LK, Bourgois P. Structural vulnerability and health: Latino migrant laborers in the United States. Med Anthropol. 2011;30(4):339–362. doi: 10.1080/01459740.2011.576725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bourgois P, Holmes SM, Sue K, Quesada J. Structural vulnerability: operationalizing the concept to address health disparities in clinical care. Acad Med. 2017;92(3):299–307. doi: 10.1097/ACM.0000000000001294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holmes SM. Structural vulnerability and hierarchies of ethnicity and citizenship on the farm. Med Anthropol. 2011;30(4):425–449. doi: 10.1080/01459740.2011.576728. [DOI] [PubMed] [Google Scholar]
- 20.Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103(5):813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang LH, Kleinman A, Link BG, Phelan JC, Lee S, Good B. Culture and stigma: adding moral experience to stigma theory. Soc Sci Med. 2007;64(7):1524–1535. doi: 10.1016/j.socscimed.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 22.Musheke M, Ntalasha H, Gari S et al. A systematic review of qualitative findings on factors enabling and deterring uptake of HIV testing in sub-Saharan Africa. BMC Public Health. 2013;13(1):220. doi: 10.1186/1471-2458-13-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang LH, Thornicroft G, Alvarado R, Vega E, Link BG. Recent advances in cross-cultural measurement in psychiatric epidemiology: utilizing “what matters most” to identify culture-specific aspects of stigma. Int J Epidemiol. 2014;43(2):494–510. doi: 10.1093/ije/dyu039. [DOI] [PubMed] [Google Scholar]
- 24.Link BG, Cullen FT, Struening E, Shrout PE, Dohrenwend BP. A modified labeling theory approach to mental disorders: an empirical assessment. Am Sociol Rev. 1989;54(3):400–423. doi: 10.2307/2095613. [DOI] [Google Scholar]
- 25.Mayring P. Qualitative content analysis. FQS. 2000;1(2) doi: 10.17169/fqs-1.2.1089. [DOI] [Google Scholar]
- 26.Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 27.Yang LH, Chen F, Sia KJ et al. “What matters most”: a cultural mechanism moderating structural vulnerability and moral experience of mental illness stigma. Soc Sci Med. 2014;103:84–93. doi: 10.1016/j.socscimed.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 28.Potter WJ, Levine-Donnerstein D. Rethinking validity and reliability in content analysis. J Appl Commun Res. 1999;27(3):258–284. doi: 10.1080/00909889909365539. [DOI] [Google Scholar]
- 29.Kim MH, Zhou A, Mazenga A et al. Why did I stop? Barriers and facilitators to uptake and adherence to ART in Option B+ HIV care in Lilongwe, Malawi. PLoS One. 2016;11(2):e0149527. doi: 10.1371/journal.pone.0149527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yang LH, Ho-Foster AR, Becker TD et al. Psychometric validation of a scale to assess culturally-salient aspects of HIV stigma among women living with HIV in Botswana: engaging “what matters most” to resist stigma. AIDS Behav. 2021;25(2):459–474. doi: 10.1007/s10461-020-03012-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Goudge J, Ngoma B, Manderson L, Schneider H. Stigma, identity and resistance among people living with HIV in South Africa. SAHARA J. 2009;6(3):94–104. doi: 10.1080/17290376.2009.9724937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Poku OB, Ho-Foster AR, Entaile P et al. “Mothers moving towards empowerment” intervention to reduce stigma and improve treatment adherence in pregnant women living with HIV in Botswana: study protocol for a pragmatic clinical trial. Trials. 2020;21(1):832. doi: 10.1186/s13063-020-04676-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fleming PJ, Colvin C, Peacock D, Dworkin SL. What role can gender-transformative programming for men play in increasing men’s HIV testing and engagement in HIV care and treatment in South Africa? Cult Health Sex. 2016;18(11):1251–1264. doi: 10.1080/13691058.2016.1183045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Misra S, Mehta HT, Eschliman EL et al. Identifying “what matters most” to men in Botswana to promote resistance to HIV-related stigma. Qual Health Res. 2021 doi: 10.1177/10497323211001361. epub ahead of print March 25, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bowleg L. The problem with the phrase women and minorities: intersectionality—an important theoretical framework for public health. Am J Public Health. 2012;102(7):1267–1273. doi: 10.2105/AJPH.2012.300750. [DOI] [PMC free article] [PubMed] [Google Scholar]