Abstract
Background:
Lateral meniscal repair can endanger the nearby neurovascular structure (peroneal nerve or popliteal artery). To our knowledge, there have been no studies to evaluate the danger zone of all-inside meniscal repair through the anteromedial (AM) and anterolateral (AL) portals in relation to the medial and lateral edges of the popliteal tendon (PT).
Purpose:
To establish the risk of neurovascular injury and the danger zone in repairing the lateral meniscus in relation to the medial and lateral edges of the PT.
Study Design:
Descriptive laboratory study.
Methods:
Using axial magnetic resonance imaging (MRI) studies at the level of the lateral meniscus, lines were drawn to simulate a straight, all-inside meniscal repair device, drawn from the AM and AL portals to both the medial and lateral edges of the PT. In cases in which the line passed through the neurovascular structure, a risk of iatrogenic neurovascular injury was deemed, and measurements were made to determine the danger zones of neurovascular injury in relation to the medial or lateral edges of the PT.
Results:
Axial MRI images of 240 adult patients were reviewed retrospectively. Repairing the body of the lateral meniscus through the AM portal had a greater risk of neurovascular injury than repairs made through the AL portal in relation to the medial edge of the PT (P = .006). The danger zone in repairing the lateral meniscus through the AM portal extended 1.82 ± 1.68 mm laterally from the lateral edge of the PT and 3.13 ± 2.45 mm medially from the medial edge of the PT. Through the AL portal, the danger zone extended 2.81 ± 1.94 mm laterally from the lateral edge of the PT and 1.39 ± 1.53 mm medially from the medial edge of the PT.
Conclusion:
Repairing the lateral meniscus through either the AM or the AL portals in relation to the PT can endanger the peroneal nerve or popliteal artery.
Clinical Relevance:
The surgeon can minimize the risk of iatrogenic neurovascular injury in lateral meniscal repair by avoiding using the all-inside meniscal device in the danger zone area as described in this study.
Keywords: all-inside meniscal repair, iatrogenic injury, lateral meniscus, peroneal nerve, popliteal artery
The menisci are important structures of the knee joint. Patients with a meniscal injury are at high risk of developing knee osteoarthritis.8,9,13,16 When facing a meniscal injury during an arthroscopic procedure, most orthopaedic surgeons prefer performing a meniscal repair rather than a meniscectomy to decrease the risk of the patient’s later developing osteoarthritis.21,22 The all-inside technique is used widely in meniscal repairs, especially in the body and posterior horn of the meniscus, because it is a simple procedure with low operative time and does not require any additional skin incisions.2,3,12
In all-inside lateral meniscal repair of the body and posterior horn of the lateral meniscus, most surgeons usually repair the lateral meniscus in the area lateral to the lateral border of the popliteal tendon (PT) and medial to the medial border of the PT to avoid penetrating the PT. The surgeon can approach repairs to the body of the lateral meniscus through either an anteromedial (AM) or anterolateral (AL) portal. With either approach, there is a risk of iatrogenic peroneal nerve injury.6,14,18 The peroneal nerve passes the knee joint running obliquely from the lateral side of the popliteal fossa to the fibular head.7,25 At the knee joint level, the peroneal nerve is located at the posterolateral aspect of the knee joint, which is close to the PT.7 One study evaluated the risk to the peroneal nerve in all-inside meniscal repair through the AL portal using the medial and lateral edges of the popliteal hiatus as references and through the AM portal using the lateral edge of the popliteal hiatus as a reference6 and found no incidences of iatrogenic peroneal nerve injury. However, this study evaluated only 20 midthigh to midleg cadaveric knees and did not evaluate the risk of iatrogenic peroneal nerve injury in all-inside meniscal repair through the AM portal using the medial edge of popliteal hiatus as a reference, a procedure that is more common in surgical practice and more perpendicular to the meniscal fiber. In repairing the posterior horn of the lateral meniscus, there is a chance of injuring the popliteal artery because this structure is located posterolaterally to the midline of the knee joint.15,24 Both cadaver-based and magnetic resonance imaging (MRI) studies have reported a risk of iatrogenic popliteal artery injury in this procedure.1,4,10
To our knowledge, there have been no studies evaluating the risk of iatrogenic neurovascular injury and the danger zone of all-inside meniscal repair through the AM and AL portals in relation to the medial and lateral edges of the PT. The purpose of this study was to establish the risk of neurovascular injury and the danger zone in repairing the lateral meniscus in relation to the medial and lateral edges of the PT.
Methods
The study protocol for this retrospective review was approved by an institutional review board. This study included 324 patients aged between 18 and 60 years who had MRI knee imaging from January 2016 to December 2019. The imaging studies of 84 patients who had medial or lateral collateral ligament injury; a history of patellar tendon or quadriceps tendon injuries, patellar dislocation, or knee surgery; soft tissue or bone tumors; or rheumatoid diseases were excluded. The included MRIs were of noninjured knees as well as those with anterior cruciate ligament (ACL) injuries and combined ACL and meniscal injuries (medial, lateral, or both).
For all MRIs, the knee was in a slightly flexed position. Coronal MRI scouting images were used to confirm the location of the patellar tendon, lateral meniscus, and PT on axial MRI (Figure 1). At the level of the lateral meniscus on axial scans, the PT, peroneal nerve, and popliteal artery were then outlined in blue, yellow and white, respectively (Figure 1).
Figure 1.
Scouting MRI scans of coronal and axial views to confirm the location of the patellar tendon, lateral meniscus, and PT. The PT, peroneal nerve, and popliteal artery are outlined in blue, yellow and white, respectively. MRI, magnetic resonance imaging; PT, popliteal tendon.
Assessing the Risk of Neurovascular Injury and the Danger Zone Relative to the PT on MRI
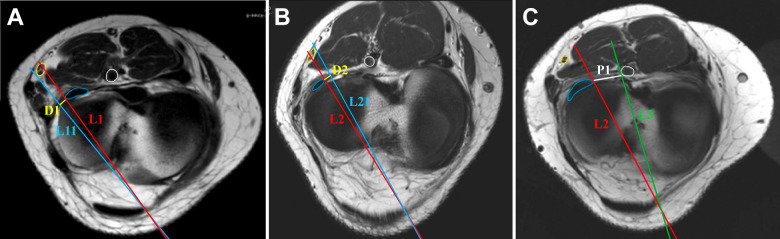
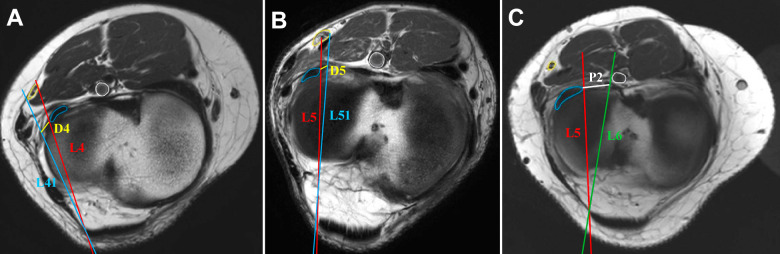
The medial and lateral edges of the patellar tendon were set as the imaginary AM and AL portals, respectively. In standard practice, most surgeons use an all-inside meniscal repair device inserted 15 mm from the joint capsule to avoid potential problems related to excessive penetration depth.5,11,17,20,23 In this study, we drew lines simulating a straight, all-inside meniscal repair device, with the distal end of each line representing the tip of the device and extending 15 mm past the joint capsule. The initial line was drawn from the imaginary AM (Figure 2) or AL (Figure 3) portal to either the lateral edge of the PT or the medial edge of the PT, passing through the joint capsule (red lines in Figure 2, A and B; and Figure 3, A and B). A risk of iatrogenic neurovascular injury was deemed to exist if this line passed through the peroneal nerve. In these cases, a second line was drawn passing the border of the peroneal nerve (blue lines in Figure 2, A and B; and Figure 3, A and B), and the danger zone was defined as the distance between the first and second lines along the meniscocapsular junction (yellow lines in Figure 2, A and B; and Figure 3, A and B).
Figure 2.
Assessing the danger zone from the AM portal as determined on axial magnetic resonance imaging. The PT, peroneal nerve, and popliteal artery are outlined in blue, yellow, and white, respectively. (A) A line was drawn from the AM portal to the lateral edge of the PT (L1). If this line passed through the peroneal nerve, another line was drawn from the AM portal to the lateral border of the peroneal nerve (L11); the danger zone was the distance between L1 and L11 along the meniscocapsular junction (D1). (B) A line was drawn from the AM portal to the medial edge of the PT (L2). If this line passed through the peroneal nerve, another line was drawn passing the medial border of the peroneal nerve (L21); the danger zone was the distance between L2 and L21 along the meniscocapsular junction (D2). (C) Line L3 was drawn from the AM portal to the lateral border of the popliteal artery, and the distance from L2 to L3 on the posterior edge of the lateral meniscus (P1), and the danger zone was the distance that P1 extended medially beyond L3. AM, anteromedial; PT, popliteal tendon.
Figure 3.
Assessing the danger zone from the AL portal as determined on axial magnetic resonance imaging. The PT, peroneal nerve, and popliteal artery are outlined in blue, yellow, and white, respectively. (A) A line was drawn from the AL portal to the lateral edge of the PT (L4). If this line passed through the peroneal nerve, another line was drawn from the AL portal to the lateral border of the peroneal nerve (L41); the danger zone was the distance between L4 and L41 along the meniscocapsular junction (D4). (B) A line was drawn from the AL portal to the medial edge of the PT (L5). If this line passed through the peroneal nerve, another line was drawn passing the medial border of the peroneal nerve (L51); the danger zone was the distance between L5 and L51 along the meniscocapsular junction (D5). (C) Line L6 was drawn from the AL portal to the lateral border of the popliteal artery, and the distance from L5 to L6 on the posterior edge of the lateral meniscus (P2), and the danger zone was the distance that P2 extended medially beyond L6. AL, anterolateral; PT, popliteal tendon.
To assess the risk of iatrogenic popliteal artery injury in all-inside meniscal repair, we drew a line from the AM/AL portal to the lateral border of the popliteal artery (green lines in Figure 2C and 3C), and the danger zone was the distance medial to this line. This distance was then defined relative to the medial edge of the PT.
Analysis
Each of the above distances was measured 3 times by a single orthopaedist (W.W.), and the results are presented as means ± SDs. The different distances and the incidence of iatrogenic neurovascular injury between repairing the lateral meniscus through the AM and AL portals were analyzed using a paired t test. The threshold for significance was set at P < .05. Statistical analysis was performed with the R program and epicalc package (Version 3.4.3; R Foundation for Statistical Computing).
Results
Overall, 240 knee MRI scans (159 [66.2%] men and 81 [33.8%] women) were included in the study. The mean age of the patients was 37.3 ± 13.2 years. Of the 240 MRIs, 147 (61.25%) were of noninjured knees, 25 (10.42%) were of knees with an ACL injury, 26 (10.83%) were of knees with combined ACL and medial meniscal injury, 26 (10.83%) were of combined ACL and lateral meniscal injury, and 16 (6.67%) were of combined ACL and both medial and lateral meniscal injuries.
Risk of Neurovascular Injury From the AM or AL Portal Relative to the Lateral Edge of the PT
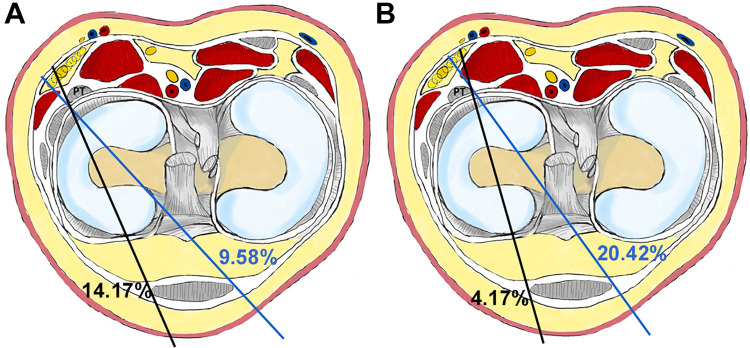
Repairing the lateral meniscus through either the AM portal or the AL portal in relation to the lateral edge of the PT using an all-inside meniscal repair device involved a risk of iatrogenic peroneal nerve injury. In our study, a risk of peroneal nerve injury was deemed when repairing through the AM portal in 23 of 240 knees (9.58%) and using the AL portal approach in 34 of 240 knees (14.17%) (Figure 4A). There was no difference in the risk of peroneal nerve injury between the AM and AL approaches in relation to the lateral edge of the PT (P = .11).
Figure 4.
Illustrations of the knee at the level of the meniscus showing the risk of iatrogenic neurovascular injury from the AM and AL portals in relation to (A) the lateral and (B) medial edge of the PT. The blue line simulates a straight all-inside meniscal repair device inserted through the anteromedial portal, the black line simulates a straight all-inside meniscal repair device inserted through the anterolateral portal. AL, anterolateral; AM, anteromedial; PT, popliteal tendon.
Risk of Neurovascular Injury From the AM or AL Portal Relative to the Medial Edge of the PT
We found that repairing the lateral meniscus through both AM and AL portals in relation to the medial edge of the PT could endanger the peroneal nerve. Potential peroneal nerve injury was indicated in 49 of 240 knees (20.42%) through the AM portal and 10 of 240 knees (4.17%) through the AL portal, respectively (Figure 4B). There was a significantly higher number of potential injuries using the AM approach compared with using the AL approach (P = .006).
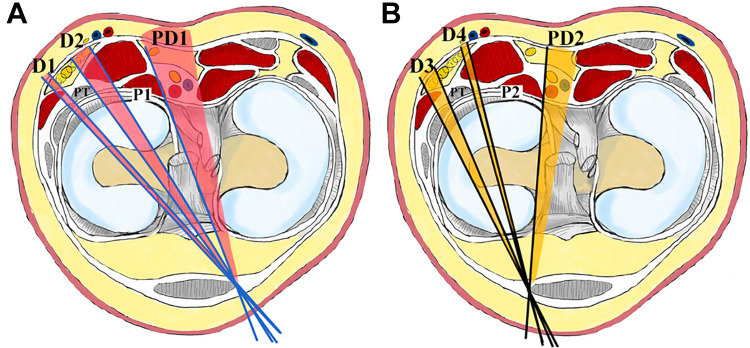
The Danger Zone Relative to the Medial and Lateral Edges of the PT
The danger zone in repairing the lateral meniscus through the AM portal extended 1.82 ± 1.68 mm laterally from the lateral edge of the PT and 3.13 ± 2.45 mm medially from the medial edge of the PT (D1 and D2 in Figure 5A, respectively). The danger zone for popliteal artery injury began 19.01 ± 4.67 mm from the medial edge of the PT (PD1 in Figure 5A).
Figure 5.
Illustrations of the knee showing the danger zones. (A) The danger zone in repairing the lateral meniscus through the AM portal (shaded pink). The blue lines simulate a straight all-inside meniscal repair device inserted through the AM portal, and D1 and D2 indicate the distances from the lateral and medial edges of the PT to the lateral and medial borders of the peroneal nerve along the meniscocapsular junction, respectively. P1 is the distance between the medial edge of the PT and the lateral border of the popliteal artery on the posterior edge of the lateral meniscus, and PD1 is the danger zone for popliteal artery injury. (B) The danger zone in repairing the lateral meniscus through the AL portal (shaded orange). The black lines simulate a straight all-inside meniscal repair device inserted through the AL portal, and D3 and D4 indicate the distances from the lateral and medial edges of the PT to the lateral and medial borders of the peroneal nerve along the meniscocapsular junction, respectively. P2 is the distance between the medial edge of PT and the lateral border of the popliteal artery on the posterior edge of the lateral meniscus, and PD2 is the danger zone for popliteal artery injury. AL, anterolateral; AM, anteromedial; PT, popliteal tendon.
The danger zone in repairing the lateral meniscus through the AL portal extended 2.81 ± 1.94 mm lateral to the lateral edge of the PT and 1.39 ± 1.53 mm medial to the medial edge of the PT (D3 and D4 in Figure 5B, respectively). The danger zone for popliteal artery injury began 16.53 ± 4.30 mm from the medial edge of the PT (PD2 in Figure 5B).
Discussion
The measurements in this MRI study examining all-inside meniscal repair through the AM and AL portals in relation to both the medial and lateral edges of the PT indicated some areas of potential iatrogenic peroneal nerve injury. Repairing the body of the lateral meniscus through the AM portal was found to be safer than through the AL portal based on measurements from the lateral edge of the PT, but the AM portal approach was more dangerous based on measurements from the medial edge of the PT. In repairs to the posterior horn of the lateral meniscus, it was safer to repair through the AM portal.
In lateral meniscal repair, there is a risk of peroneal nerve injury because the peroneal nerve is located at the posterolateral aspect of the knee joint, which is close to the PT.6,7,14,18 Our study found that repairing the body of the lateral meniscus with the all-inside technique through both AM and AL portals in relation to the medial edge and lateral edge of the PT endangered the peroneal nerve. The incidence of deemed iatrogenic peroneal nerve injury in relation to the lateral edge of the PT through the AM portal was 23 of 240 cases (9.58%) and through the AL portal was 34 of 240 cases (14.17%). Referencing the medial edge of the PT also involved potential damage to the peroneal nerve, with incidences of deemed injury through the AM portal of 49 of 240 knees (20.42%) and through the AL portal of 10 of 240 knees (4.17%). These results were similar to a study of Cuellar et al,6 which reported that repairing the lateral meniscus through the AL approach was safer than the AM approach, with an average distance from the medial side of the popliteal hiatus to the peroneal nerve of 7.00 ± 4.00 mm in the knee extension position.
In the current study, we calculated the following safe zones to avoid the risk of peroneal nerve injury. In relation to the lateral edge of the PT, the safe zones were lateral to the lateral edge of the PT by 1.82 ± 1.68 mm for the AM portal and by 2.81 ± 1.94 mm for the AL portal, and in relation to the medial edge of the PT, the safe zones were medial to the medial edge of the PT by 3.13 ± 2.45 mm for the AM portal and by 1.39 ± 1.53 mm for the AL portal.
The popliteal artery is located posterolateral to the midline of the knee joint.15,24 A study by Mao et al19 found that in the posterior horn of lateral meniscal repair, there was a risk of iatrogenic popliteal artery injury in all-inside meniscal repair through the AL portal, but there was no risk of popliteal artery injury in all-inside meniscal repair through the AM portal. The same study reported that the average distance from the tip of the all-inside meniscal device to the popliteal artery in repairing the posterior horn of the lateral meniscus through the AL portal using the point of 5 mm lateral to the lateral meniscus root insertion as a reference was 4.7 ± 2.3 mm.19 In our study, the average safe distance in repairing the lateral meniscus from the medial edge of the PT to the lateral edge of the popliteal artery along the posterior border of the posterior horn of the lateral meniscus through the AM portal (P1) was 19.01 ± 4.67 mm; through the AL portal (P2), it was 16.53 ± 4.30 mm. If the surgeon repairs the posterior horn of the lateral meniscus farther from the medial edge of the PT than these distances, there will be a risk of iatrogenic popliteal artery injury. Even though there is a risk of popliteal artery injury in repairs approached through the AL portal, some surgeons prefer this approach because the required direction of the all-inside meniscal repair device is perpendicular to the circumferential meniscal fiber. If the surgeon repairs the posterior horn of the lateral meniscus through the AM portal, the direction of the all-inside meniscal repair device will not be perpendicular to the meniscal fiber.
Limitations
There were several limitations to this study. First, the direction of the PT is oblique when it passes the knee joint, and thus, the level of measurement varied. We tried to minimize this problem by using axial MRI cuts that passed through the center of the meniscus. Second, the knees were in the slightly flexed position when the MRIs were performed, which is different from the arthroscopic position used in actual lateral meniscal repairs (the Figure 4 position, while applying varus force). In the flexion position, the neurovascular structure is less stretched and falls more posteriorly. Third, our MRI model might not represent the true distances during arthroscopic meniscal repair, because these distances may be affected by joint distension if an arthroscopic pump is used. Fourth, in this study, we evaluated the risk of an iatrogenic neurovascular injury in lateral meniscal repair by using a simulated line to represent a straight all-inside meniscal repair device. The risk of an iatrogenic neurovascular injury may be different if the surgeon uses a curved all-inside meniscal repair device in lateral meniscal repair. Fifth, in this study, we set the distance as viewed on the MRIs between the tip of each straight line and the joint capsule at 15 mm, a distance that is likely deeper than the normal penetration a surgeon would create starting from a meniscal tear.
Conclusion
All-inside meniscal repair through the AM and AL portals in relation to both medial and lateral edges of the PT were found to have a chance of iatrogenic neurovascular injury, but the procedure was more dangerous in repairing the lateral meniscus through the AM portal in relation to the medial edge of the PT. The surgeon can minimize this risk in repairing the lateral meniscus around the PT by referring to our danger zone measurements.
Acknowledgment
The authors sincerely thank Boonsin Tangtrakulwanich of the Orthopedics Department; Nannapat Pruphetkaew of the Epidemiology Unit, Faculty of Medicine, Prince of Songkla University for providing statistical support; Trisak Kingchan for his assistance with drawing demonstration; and Dave Patterson for his linguistic support.
Footnotes
Final revision submitted April 19, 2021; accepted May 19, 2021.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Prince of Songkla University (ID No. 63-132-11-1).
References
- 1.Abouheif MM, Shibuya H, Niimoto T, et al. Determination of the safe penetration depth during all-inside meniscal repair of the posterior part of the lateral meniscus using the FasT-Fix suture repair system. Knee Surg Sports Traumatol Arthrosc. 2011;19(11):1868–1875. doi:10.1007/s00167-011-1489-x [DOI] [PubMed] [Google Scholar]
- 2.Ahn JH, Kim CH, Lee SH. Repair of the posterior third of the meniscus during meniscus allograft transplantation: conventional inside-out repair versus fast-fix all-inside repair. Arthroscopy. 2016;32(2):295–305. doi:10.1016/j.arthro.2015.07.017 [DOI] [PubMed] [Google Scholar]
- 3.Albrecht-Olsen P, Kristensen G, Burgaard P, Joergensen U, Toerholm C. The arrow versus horizontal suture in arthroscopic meniscus repair: a prospective randomized study with arthroscopic evaluation. Knee Surgery, Sport Traumatol Arthrosc. 1999;7(5):268–273. doi:10.1007/s001670050162 [DOI] [PubMed] [Google Scholar]
- 4.Beck JJ, Shifflett K, Greig D, Ebramzadeh E, Bowen RE. Defining a safe zone for all-inside lateral meniscal repairs in pediatric patients: a magnetic resonance imaging study. Arthroscopy. 2019;35(1):166–170. doi:10.1016/j.arthro.2018.07.046 [DOI] [PubMed] [Google Scholar]
- 5.Cohen SB, Boyd L, Miller MD. Vascular risk associated with meniscal repair using Rapidloc versus FasT-Fix: comparison of two all-inside meniscal devices. J Knee Surg. 2007;20(3):235–240. doi:10.1055/s-0030-1248049 [DOI] [PubMed] [Google Scholar]
- 6.Cuéllar A, Cuéllar R, Cuéllar A, Garcia-Alonso I, Ruiz-Ibán MA. Neurovascular safety of all-inside lateral meniscus. Arthroscopy. 2015;31(11):2138–2144. doi:10.1016/j.arthro.2015.04.100 [DOI] [PubMed] [Google Scholar]
- 7.Deutsch A, Wyzykowski RJ, Victoroff BN. Evaluation of the anatomy of the common peroneal nerve: defining nerve-at-risk in arthroscopically assisted lateral meniscus repair. Am J Sports Med. 1999;27(1):10–15. doi:10.1177/03635465990270010201 [DOI] [PubMed] [Google Scholar]
- 8.Englund M. Meniscal tear—a feature of osteoarthritis. Acta Orthop Scand. 2004;75(suppl 312):1–45. doi:10.1080/03008820410002048 [PubMed] [Google Scholar]
- 9.Englund M, Lohmander LS. Risk factors for symptomatic knee osteoarthritis fifteen to twenty-two years after meniscectomy. Arthritis Rheumatol. 2004;50(9):2811–2819. doi:10.1002/art.20489 [DOI] [PubMed] [Google Scholar]
- 10.Gupta H, Ghasi RG, Kataria H, et al. Popliteal neurovascular bundle is safe during inside-out repair of medial meniscus without a safety incision. Knee Surg Sport Traumatol Arthrosc. 2019;27(1):153–165. doi:10.1007/s00167-018-5060-x [DOI] [PubMed] [Google Scholar]
- 11.Haas AL, Schepsis AA, Hornstein J, Edgar CM. Meniscal repair using the FasT-Fix all-inside meniscal repair device. Arthroscopy. 2005;21(2):167–175. doi:10.1016/j.arthro.2004.10.012 [DOI] [PubMed] [Google Scholar]
- 12.Hantes ME, Zachos VC, Varitimidis SE, Dailiana ZH, Karachalios T, Malizos KN. Arthroscopic meniscal repair: a comparative study between three different surgical techniques. Knee Surg Sport Traumatol Arthrosc. 2006;14(12):1232–1237. doi:10.1007/s00167-006-0094-x [DOI] [PubMed] [Google Scholar]
- 13.Johnson VL, Hunter DJ. The epidemiology of osteoarthritis. Best Pract Res Clin Rheumatol. 2014;28(1):5–15. doi:10.1016/j.berh.2014.01.004 [DOI] [PubMed] [Google Scholar]
- 14.Jurist KA, Greene PW, Shirkhoda A. Peroneal nerve dysfunction as a complication of lateral meniscus repair: a case report and anatomic dissection. Arthroscopy. 1989;5(2):141–147. doi:10.1016/0749-8063(89)90010-8 [DOI] [PubMed] [Google Scholar]
- 15.Keyurapan E, Phoemphunkunarak W, Lektrakool N. Location of the neurovascular bundle of the knee during flexed and extended position: an MRI study. J Med Assoc Thai. 2016;99(10):1102–1109. [PubMed] [Google Scholar]
- 16.Khan T, Alvand A, Prieto-Alhambra D, et al. ACL and meniscal injuries increase the risk of primary total knee replacement for osteoarthritis: a matched case-control study using the Clinical Practice Research Datalink (CPRD). Br J Sports Med. 2019;53(15):965–968. doi:10.1136/bjsports-2017-097762 [DOI] [PubMed] [Google Scholar]
- 17.Kotsovolos ES, Hantes ME, Mastrokalos DS, Lorbach O, Paessler HH. Results of all-inside meniscal repair with the FasT-Fix meniscal repair system. Arthroscopy. 2006;22(1):3–9. doi:10.1016/j.arthro.2005.10.017 [DOI] [PubMed] [Google Scholar]
- 18.Liao CP, Lee HM, Shih JT, Hung ST. Common peroneal nerve palsy as a postoperative complication in lateral meniscus repair. Formos J Musculoskelet Disord. 2013;4(2):48–50. doi:10.1016/j.fjmd.2013.04.004 [Google Scholar]
- 19.Mao DW, Upadhyay U, Thalanki S, Lee DYH. All-inside lateral meniscal repair via anterolateral portal increases risk of vascular injury: a cadaveric study. Arthroscopy. 2020;36(1):225–232. doi:10.1016/j.arthro.2019.07.023 [DOI] [PubMed] [Google Scholar]
- 20.Miller MD, Kline AJ, Gonzales J, Beach WR. Pitfalls associated with FasT-Fix meniscal repair. Arthroscopy. 2002;18(8):939–943. doi:10.1053/jars.2002.36146 [DOI] [PubMed] [Google Scholar]
- 21.Ro KH, Kim JH, Heo JW, Lee DH. Clinical and radiological outcomes of meniscal repair versus partial meniscectomy for medial meniscus root tears: a systematic review and meta-analysis. Orthop J Sports Med. 2020;8(11):2325967120962078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rönnblad E, Barenius B, Stålman A, Eriksson K. Failed meniscal repair increases the risk for osteoarthritis and poor knee function at an average of 9 years follow-up. Published online February 6, 2021. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-021-06442-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roos EM, Ostenberg A, Roos H, Ekdahl C, Lohmander LS. Long-term outcome of meniscectomy: symptoms, function, and performance tests in patients with or without radiographic osteoarthritis compared to matched controls. Osteoarthritis Cartilage. 2001;9(4):316–324. doi:10.1053/joca.2000.0391 [DOI] [PubMed] [Google Scholar]
- 24.Simons M, Schraut N, Moretti V, et al. Location of the popliteal artery in knee extension on magnetic resonance imaging. J Surg Orthop Adv. 2018;27(4):325–328. [PubMed] [Google Scholar]
- 25.Warren RF. Arthroscopic meniscus repair. Arthroscopy. 1985;1(3):170–172. doi:10.1016/s0749-8063(85)80005-0 [DOI] [PubMed] [Google Scholar]