Abstract
Background
Even in the modern endovascular era, the treatment of Vein of Galen Malformations (VOGM) is extremely challenging. While their natural history is very poor, endovascular embolization has emerged as the standard of care. These lesions often require multiple treatment sessions to decrease shunting, with each treatment including multiple pedicles. Here we present the first reported use of the Scepter Mini (Microvention, Aliso Viejo, CA) in the treatment of vein of Galen malformations.
Clinical presentation
A 7 month old female presented with an enlarging VOGM that was initially identified on prenatal ultrasound. Given the enlarging size of the lesion and failure to meet developmental milestones, the patient underwent planned endovascular embolization of the VOGM. The novel Scepter Mini balloon catheter was used for treatment of this lesion affording easy access to the target pedicle and immediate flow arrest which allowed for immediate cure of the lesion.
Conclusion
The novel Scepter Mini Balloon (Microvention, Aliso Viejo, CA) afforded excellent distal access with subsequent immediate flow arrest therefore facilitating endovascular cure. Initially, a staged approach was favored for the treatment of the lesion, but the flow arrest achieved by the Scepter mini facilitated immediate occlusion from a single pedicle.
Keywords: Vein of Galen, Vein of Galen malformation, arteriovenous malformation, scepter mini balloon, dual lumen balloon
Background
Vein of Galen malformations (VOGM) are particularly difficult lesions to manage even in the modern endovascular era.1 A new balloon catheter, the Scepter Mini (Microvention, Aliso Viejo, CA), has recently been introduced. A dual lumen balloon catheter with 2.2 mm maximal dilation allows for excellent navigability and distal pedicle access with subsequent immediate flow arrest therefore optimizing delivery of liquid embolic agents in high flow lesions with small/distal feeding pedicles. We present a case of an infantile VOGM treated by a single pedicle embolization using n-BCA for complete occlusion of the fistula facilitated by the Scepter Mini (Microvention, Aliso Viejo, CA). The treatment was a technical success and the patient experienced no lasting periprocedural complications. Consent was obtained for this publication.
Case presentation
A 7-month-old female presented after a VOGM was found on prenatal ultrasound. The infant, born at 39 weeks, was monitored in the neonatal ICU and with medical management alone recovered from the heart failure. Therefore, treatment of the VOGM was initially deferred. Follow up imaging revealed increasing size of the malformation with worsening hydrocephalus and failure of the child to reach milestones (Figure 1(a) and (b)). Given these findings the infant was scheduled for angiography and embolization.
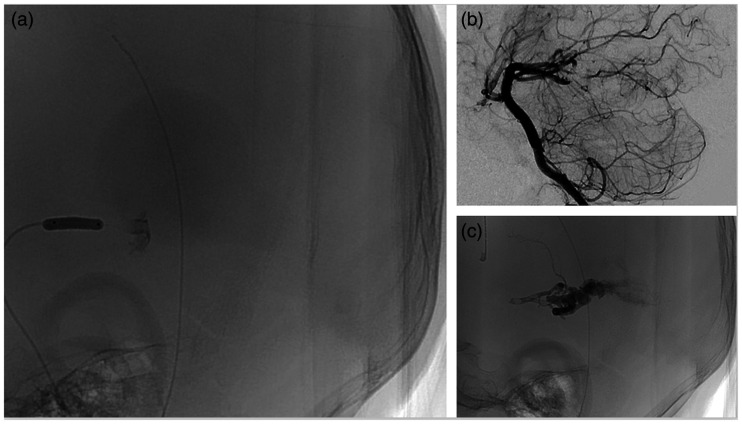
Figure 1.
(a) MR angiography demonstrates aneurysmal Vein of Galen malformation with a large aneurysmal venous dilation and associated stenosis with significant shunting through the malformation associated with subsequent growth in image (b). (c) Anterior posterior injection of the left vertebral artery demonstrating the VOGM with significant shunting fed mostly by the posterior cerebral arteries as seen in (d). Associated with a stenosis immediately proximal to the torcula.
The infant underwent diagnostic angiography revealing a mural type VOGM filled primarily by the posterior cerebral arteries (Figure 1(c) and (d)). Both posterior cerebral arteries supply the VOGM with an enlarged initial venous pouch (Figure 1(a) to (d)). The venous pouch drained into a falcine sinus, which harbored a stenosis into the torcula. There was retrograde flow in the superior sagittal sinus.
A Scepter mini balloon was navigated over a Hybrid 008 (Balt Irvine, CA) microwire into the right PCA via a 4 F Cordis vertebral (Cordis, Santa Clara, CA) diagnostic catheter. The diagnostic catheter was placed in the V2 segment. Microcatheter angiography with balloon inflation demonstrated direct flow into the venous pouch. (Figure 2(a)). A 1:1 mixture of Ethiodol:n-BCA Cordis Trufil (Cerenovus, Miami, FL) totaling 1.2 cc was injected. NBCA was injected into the venous pouch, temporarily halted then resumed until embolic material was seen to permeate into the other arterial supply of the lesion. Post procedure angiography demonstrated complete occlusion of the VOGM and no residual arteriovenous shunting (Figure 2(b) and (c)). The plan was not for complete occlusion via a single pedicle but nevertheless this was the outcome. The injection of n-BCA was halted as soon as reflux into a different arterial pedicle was demonstrated; no n-BCA went proximal to the distal marker of the balloon. Total balloon time was under 2 min. Total contrast used was 65 cc Omnipaque (GE Healthcare) 240 and radiation dose was 176.3 mGy. Of note, the venous sac was not completely occluded.
Figure 2.
(a) Inflation of the scepter balloon in a right posterior cerebral artery feeder with microcatheter injection demonstrating direct shunting to the VOGM. (b) Post n-BCA angiography demonstrating no arteriovenous shunting and (c) unsubtracted mask showing the glue cast.
Immediately post procedure the patient had a right ptosis that resolved prior to discharge. Post embolization MRI demonstrated small areas of diffusion restriction in the right mesial thalamus and persistent occlusion of the VOGM likely due to penetration of n-BCA through the nidus to all other arterial feeders (Figure 3(a) and (b)). Off target reflux through the nidus led to occlusion of a branch of the posterior choroidal artery. The patient was discharged home on aspirin and Lovenox as the post embolization MRI did suggestion some thrombosis of the venous sac. The patient was discharged post procedure day 6 at her neurological baseline. At 6-month follow up post procedure patient was found to be meeting developmental milestones and and MRV demonstrated persistent occlusion of the VOGM (Figure 3(c)).
Figure 3.
(a) Post embolization MRI demonstrating right thalamic diffusion restriction. (b) Post embolization MR angiography demonstrating no residual VOGM. (c) MR done 6 months post procedure demonstrating persistent occlusion of the VOGM.
Discussion
Endovascular embolization of VOGM is the standard treatment methodology; however, up to one third of patients will suffer major neurologic morbidity or mortality.2--5 A recent metanalysis demonstrated that 19% of cases may have technical complications with complete embolization occurring in only 56% of cases.2 Even with modern endovascular devices, technical complications such as arterial perforation and off target embolization continue to occur.3,6,7 This case describes the technical safety of a novel dual lumen balloon microcatheter resulting in the angiographic cure of a VOGM. In the setting of a high flow shunt such as these lesions, a small dual lumen balloon with the ability to tolerate liquid embolic is extremely advantageous.
Concern does exist about rapid angiographic cure of these lesions. Lasjaunias argued for staged treatment and reduction of the shunt, with the goal of a normally developing child.1,3,8 Immediate cure can lead to either rapid thrombosis of the venous system and venous infarction, or subsequent hemorrhage if an arterial pedicle remains patent in the setting of total venous occlusion.1,3 In this case, a single injection of n-BCA did lead to angiographic cure. This is not routinely recommended, but up until this point it would have been very challenging to cure a lesion like this in a single setting via a single pedicle. If complete arterial occlusion is achieved it may be feasible to cure these lesions in a single session although this requires further investigation. In this case the venous sac remained patent with minimal n-BCA penetrating the sac.
The Scepter mini (Microvention, Aliso Viejo, CA) is a dual lumen balloon microcatheter with a distal OD of 1.6 Fr. This is optimal for distal pedicle access facilitating targeted delivery of liquid embolic with maximal flow arrest. The use of this catheter has only been described three other times in the literature.9–11 This is the first described use in a VOGM.
One study found that catheters with a greater than 2 Fr OD were associated with poor outcomes therefore the Scepter Mini Balloon (Microvention, Aliso Viejo, CA) with an OD 1.6 Fr is optimal for the treatment of these lesions.3 Further advantages of precise targeting and established flow arrest include minimization of both contrast and radiation dosage. Clearly the Scepter mini offers benefits including flow arrest in high flow lesions, excellent manoeuvrability in small vessels, and a small OD for distal/small pedicle access. The balloon microcatheter in this case allowed for angiographic cure of a complex VOGM via a single injection of 1:1 n-BCA.
Conclusion
Given its small size and excellent navigability the Scepter Mini balloon will significantly advance the treatment of shunting lesions by enhanced delivery of liquid embolic agents due to the flow arrest afforded by the balloon and distal pedicle access.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Timothy G White https://orcid.org/0000-0002-3604-4334
References
- 1.Lasjaunias PL, Chng SM, Sachet M, Alvarez H, Rodesch G, Garcia-Monaco R. The management of vein of Galen aneurysmal malformations. Neurosurgery 2006; 59(5 SUPPL.). doi:10.1227/01.NEU.0000237445.39514.16 [DOI] [PubMed] [Google Scholar]
- 2.Brinjikji XW, Krings XT, Murad XMH, Rouchaud XA, Meila XD. Endovascular Treatment of Vein of Galen Malformations: A Systematic Review and Meta-Analysis 2017. doi:10.3174/ajnr.A5403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhatia K, Mendes Pereira V, Krings T, et al. Factors Contributing to Major Neurological Complications from Vein of Galen Malformation Embolization. JAMA Neurol 2020. doi:10.1001/jamaneurol.2020.0825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berenstein A, Fifi JT, Niimi Y, et al. Vein of Galen Malformations in Neonates. Neurosurgery 2012; 70(5): 1207–1214. doi:10.1227/NEU.0b013e3182417be3 [DOI] [PubMed] [Google Scholar]
- 5.Berenstein A, Paramasivam S, … MS-, 2019 undefined. Vein of Galen aneurysmal malformation: advances in management and endovascular treatment. academic.oup.com. https://academic.oup.com/neurosurgery/article-abstract/84/2/469/5026364 (Accessed June 29, 2020). [DOI] [PubMed] [Google Scholar]
- 6.Li AH, Armstrong D, TerBrugge KG. Endovascular treatment of vein of Galen aneurysmal malformation: Management strategy and 21-year experience in Toronto – Clinical article. J Neurosurg Pediatr 2011; 7(1): 3–10. doi:10.3171/2010.9.PEDS0956 [DOI] [PubMed] [Google Scholar]
- 7.Wagner, Kathryn M and Ghali, Michael GZ and Srinivasan, Visish M and Lam, Sandi and Johnson, Jeremiah and Chen, Stephen and Kan P. Vein of Galen malformations: the Texas Children’s Hospital experience in the modern endovascular era. Oper Neurosurg (Hagerstown, Md) 2019; 17(3): 286–292. [DOI] [PubMed] [Google Scholar]
- 8.Lasjaunias P, Hui F, Zerah M, et al. Cerebral arteriovenous malformations in children – Management of 179 consecutive cases and review of the literature. Child’s Nerv Syst 1995; 11(2): 66–79. doi:10.1007/BF00303807 [DOI] [PubMed] [Google Scholar]
- 9.Vollherbst DF, chapot rené, Wallocha M, et al. First clinical multicenter experience with the new Scepter Mini microballoon catheter New devices and technologies. J NeuroIntervent Surg 2020; 0: 1–7. doi:10.1136/neurintsurg-2020-016115 [DOI] [PubMed] [Google Scholar]
- 10.Pulli B, Sussman ES, Mayercik V, Steinberg GK, Do HM, Heit JJ. Initial experience with the Scepter Mini dual-lumen balloon for transophthalmic artery embolization of anterior cranial fossa dural arteriovenous fistulae. 2020; 0. doi:10.1136/neurintsurg-2020-016013 [DOI] [PubMed] [Google Scholar]
- 11.Clarenµon F, Shotar E, Pouvelle A, et al. Spinal epidural arteriovenous fistula embolization with ethylene vinyl alcohol (EVOH) copolymer using the Scepter Mini dual-lumen balloon. J Neurointerv Surg 2020; 0: neurintsurg-2020-016395. doi:10.1136/neurintsurg-2020-016395 [DOI] [PubMed] [Google Scholar]