Abstract
Background and purpose
The Woven EndoBridge (WEB) is an intrasaccular flowdisruptor that is increasingly used for the treatment of (wide-necked) aneurysms. We present our experience with the WEB for unruptured aneurysms.
Materials and methods
Between April 2014 and August 2019, 93 patients with 95 unruptured aneurysms were primarily treated with the WEB. There were 69 women and 24 men, mean age 61 years (median 58, range 37–80).
Results
Of 95 aneurysms, 86 had been discovered incidentally, 3 were symptomatic and 6 were additional to another ruptured aneurysm. Location was anterior communicating artery 33, middle cerebral artery 29, basilar tip 19, carotid tip 8, posterior communicating artery 4, posterior inferior cerebellar artery 1, superior cerebellar artery 1. Mean aneurysm size was 6 mm (median 6, range 3–13 mm).
In one aneurysm additional coils were used and in another, a stent was placed. There was one procedural rupture without clinical sequelae. There were two thrombo-embolic complications leading to permanent deficit in one patient (mRS 2). Morbidity rate was 1.0% (1 of 93, 95%CI 0.01–6.5%) and mortality was 0% (0 of 93, 95%CI 0.0–4.8%). Angiographic follow-up at six months was available in 85 patients with 87 aneurysms (91%). Of 87 aneurysms, 68 (78%) were completely occluded, 14 (16%) had a neck remnant and 5 were incompletely occluded. Four aneurysms were retreated. Retreatment rate was 4.5% (4 of 87, 95%CI 1.7–13.6%).
Conclusion
WEB treatment of unruptured aneurysms is safe and effective. Additional devices are needed only rarely and retreatment at follow-up is infrequent.
Keywords: Aneurysm, flowdisruptor, endovascular treatment
Introduction
The endovascular treatment of wide-necked intracranial aneurysms with coils mostly requires the use of a temporary protection balloon or a stent. However, this makes the procedure more complicated with a higher chance of complications.1–4 With stents, periprocedural dual antiplatelet therapy is obligatory and has to be prolonged for three to six months. This anti-aggregation regimen results in an inherent higher risk if stent-assisted coiling is used in ruptured aneurysms.5 In the last decade, flow diverters are increasingly used for the treatment of wide-necked unruptured aneurysms. Flow diverters require the use of dual antiplatelet therapy and thus have high risks when used for the treatment of ruptured aneurysms. Although in recent years coated flowdiverters are available (for example P64/P48 HPC en PED Shield) which could potentially reduce the need for dual antiplatelet therapy. However very promising, these coated devices are still in an early stage and more research is still needed.6–9 Many meta-analyses have been published on the use of flow diverters.10 Morbi-mortality with flow diversion has been described with a broad range from almost 2–10% depending on the publication. This large range can be largely explained due to high variable risk of flowdiversion depending on the treatment difficulty of the target lesion. The efficacy at one year is also largely variable with means of around 80%.11–16
Recently, the intrasaccular flow disruptor Woven EndoBridge (WEB, MicroVention, Tustin, CA, USA) device has been developed, primarily for the treatment of (bifurcation) wide-necked aneurysms without the need for adjunctive devices and antiplatelet medication. The first clinical results of the WEB device show good safety and efficacy profiles. Most of the published series comprised wide-necked, unruptured aneurysms.17–24
In this paper, we present our clinical and angiographic results of WEB treatment of unruptured aneurysms in a single center.
Materials and methods
Woven EndoBridge
The WEB device is a self-expanding, spherical (WEB-SLS) or pumpkin-shaped (WEB-SL), braided mesh of platinum cored nitinol wires that can be deployed in the aneurysm sac. The WEB-SL device is available in diameters ranging between 4 and 11 mm and heights ranging between 3 and 9 mm. The WEB-SLS is available in diameters ranging between 4 and 11 mm, each with a fixed height ranging between 2.6 and 9.6 mm. Depending on the size of the WEB, they can be delivered through an 0.033; 0.027 or 0.021-in. microcatheter (Via 21, 27 or 33, Microvention) A lower profile range of WEBs is compliant with an 0.017-in. microcatheter (VIA 17) since 2016.
Placed in the aneurysm, the WEB modifies the blood flow at the level of the neck and induces aneurysmal thrombosis. The WEB can be fully retrieved until final detachment by an electrothermal detachment system.
Patients and aneurysms
A retrospective review was performed on medical records and angiographic studies of patients treated with a WEB device between April 2014 and August 2019 in our institution. We included all patients treated with a WEB device during this period. Patients with recurrent aneurysms after previous endovascular treatment or ruptured aneurysms were excluded. In this period, 93 patients with 95 unruptured aneurysms were primarily treated with the WEB device, ruptured aneurysms were excluded. Two patients had two aneurysms treated with WEB.
Each patient was discussed in a multidisciplinary neurovascular team. Patients were informed about the nature of their disease, the intended treatment and potential alternatives, with informed consent obtained at least 24 h before the procedure. General indication for treatment was unruptured intradural wide-necked aneurysms suitable for the WEB device. Smaller aneurysms in the anterior circulation were treated either because of familial history, high blood pressure, harboring previously ruptured aneurysm or multiplicity of aneurysms; or due the psychological stress of having an untreated aneurysm for the patient.
Endovascular procedure
Procedures were performed with the patient under general anesthesia on a biplane or a single plane Philips Allura angiographic system (Philips Healthcare, Best, the Netherlands). Either a 6 F guide catheter alone or triaxial access was used. After a suitable working projection was identified from 3D angiographic imaging, the target aneurysm diameter and height were measured in two directions. A VIA microcatheter was placed over a 0.014- or 0.016-in. micro guidewire in the aneurysmal sack.
The selection of the diameter and length of the WEB was made with the aid of computer simulation on the 3D workstation. From 3D rotational images, the aneurysm is measured in three dimensions. Oversizing the WEB is imperative to assure anchoring the device on the aneurysm walls. In general, the WEB is oversized with 1–2 mm from the mean of the width of the aneurysm in two perpendicular planes. In recent studies an oversizing of 2 mm is preferred to obtain less compaction risk of the WEB at follow up.25 We tended to oversize the WEB as much as possible in our patients. When a good WEB position is confirmed, the device is detached and the procedure terminated, despite the possible presence of some flow inside the WEB and aneurysm.
Anticoagulation protocol
Patients were not preloaded with antiaggregating therapy before treatment. In general, no antiplatelet medication was given after treatment. Periprocedural medication included systemic heparinization with ACT values aimed at 250.
Follow-up
Patients were scheduled for clinical and angiographic follow-up at six months and two and five years. Clinical assessment was performed according to the modified Rankin Scale. Angiographic results were graded as complete occlusion, neck remnant, or persistent flow. Also, aneurysm occlusion was graded according to the Web Occlusion Scale (WOS), based upon the modified Raymond Scale as a standard assessment scale for reporting aneurysm occlusion26 (Table 1).
Table 1.
Web Occlusion Scale (WOS).
| A | Complete occlusion |
| B | Complete occlusion. Visible collection of contrast within the marker recess |
| C | Residual neck filling. Contrast opacification of the aneurysm neck extending beyond the marker recess |
| D | Residual aneurysm filling. Contrast beyond the aneurysm neck and into the fundus. Either deep to the proximal recess or around the periphery of the device. |
Data collection and statistics
Patient demographics and treatment- and aneurysm characteristics were collected. A retrospective review was performed on medical records and radiographic studies of all patients with unruptured aneurysms primarily treated with the WEB between April 2014 and August 2019. Quantitative variables were expressed with descriptive statistics, and categorical variables were expressed as frequencies or percentages with 95% CIs.
Results
Demographic characteristics of patients and aneurysms
There were 69 women and 24 men with a mean age of 61 years (median 58, range 37–80 years). Of 95 aneurysms, 86 had been discovered incidentally, 3 were symptomatic by mass effect (n = 2) or stroke (n = 1), and 6 were additional to another ruptured aneurysm. Aneurysm location was anterior communicating artery 33, middle cerebral artery 29, basilar tip 19, carotid tip 8, posterior communicating artery 4, posterior inferior cerebellar artery 1, and superior cerebellar artery 1 (Table 2). Eighty-eight aneurysms (92%) had a wide neck, defined as 4 mm or a dome to neck ratio 1.5. The mean aneurysm size was 6 mm (median 6 mm, range 3–13 mm) with a mean neck size of 4.5 mm (median 4.3 mm; range 2.5–8.1 mm). Mean dome to neck ratio was 1.26 (median 1.23; range 1.00–2.11).
Table 2.
Aneurysm location and aspect ratio breakdown.
| Anterior circulation (n = 70) | Mean neck | Mean width to neck ratio | Posterior circulation (n = 25) | |
|---|---|---|---|---|
| ACA | 33 (47%) | 4.5 | 1.33 | |
| ACM | 29 (41%) | 4.15 | 1.22 | |
| Carotid tip | 12 (12%) | 5.00 | 1.17 | |
| Basilar tip | 4.94 | 1.25 | 19 (76%) | |
| PCA/SCA | 4.6 | 1.14 | 4/1 (20%) | |
| PICA | 4.6 | 1.74 | 1 (4%) |
Initial results and procedural complications
In general, after measurement one Web-device was sufficient to obtain an adequate sealing of the aneurysm. In 2% of aneurysms treated a second device with a different sizing was needed. The position of the WEB was considered as optimal when the neck was covered, ideally showing contrast stasis inside the aneurysm. Depending on the size of the aneurysm and the WEB we used a VIA-catheter ranging from 21 to 33, newer smaller profile WEB’s delivered with a 17-catheter were also used (Table 3).
Table 3.
Via-size used partial breakdown per aneurysm type.
| ACA |
ACM |
BASILAR |
||||
|---|---|---|---|---|---|---|
| Via size | N | Max mean size (mm) | N | Max mean size (mm) | N | Max mean size (mm) |
| 17 | 4 | 4.6 | 8 | 3.6 | 3 | 4.8 |
| 21 | 19 | 5.6 | 10 | 4.6 | 7 | 5.2 |
| 27 | 6 | 7.4 | 11 | 6.5 | 8 | 7.2 |
| 33 | 3 | 12 | 1 | 9.0 | ||
An additional 2% of patients the use of adjuctive devices was required during the embolization treatment. In one aneurysm additional coils were placed to completely occlude the aneurysm. In one aneurysm an additional stent was placed because of protrusion of the WEB into the parent vessel.
Periprocedural complications occurred in 3% of patients. In a 60-year-old woman with an unruptured 3 mm middle cerebral artery aneurysm, the aneurysm ruptured by the microcatheter during attempted WEB placement. Slack on the microcatheter due to vessel tortuosity made the microcatheter jump forward during the advancement of the WEB. This resulted in a perforation at the dome of the aneurysm. The WEB was removed and a second microcatheter was placed in the aneurysm to start coiling and subsequently withdrawing the Via after initial coil placement. An adequate occlusion was obtained following remodeling and stent placement. The patient outcome was excellent after three months (mRS 0). This patient is excluded from follow-up analysis.
There were two thrombo-embolic complications leading to a permanent deficit in one patient (mRS 2). Both thrombo-embolic complications occurred in a distal branch, probably due to the necessity of replacing the WEB a few times before obtaining an adequate position in the aneurysm. There was no mortality. Morbidity rate was 1.0% (1 of 93, 95%CI 0.01–6.5%), and mortality was 0% (0 of 93, 95%CI 0.0–4.8%).
Clinical and imaging follow-up
Angiographic follow-up at six months was available in 85 patients with 87 aneurysms (92%).
Of 87 aneurysms, 68 (78%) were completely occluded (Figures 1 and 2) (7 with proximal recess filling), 14 (16%) had a neck remnant and 5 (6%) were incompletely occluded. According to the WOS, 61 were completely occluded type A and 7 were occluded with a neck remnant type B (Table 4). Of five incompletely occluded aneurysms, four were retreated: three with a flowdiverter after 3, 24, and 24 months, respectively (Figure 3), and one with Y-stenting and coiling after 12 months. Eligibility for retreatment was decided after multidisciplinary discussion. In general, we retreat aneurysms with evolutive remnants on second angiography or with a neck remnant of more than 3 mm. At follow-up, occlusion was complete in all four additionally treated aneurysms. Retreatment rate was 4.5% (4 of 87, 95%CI 1.4–11.6%). Angiographic follow-up at two years was already done in 55% of treated aneurysms, these revealed no impaction of the WEB device.
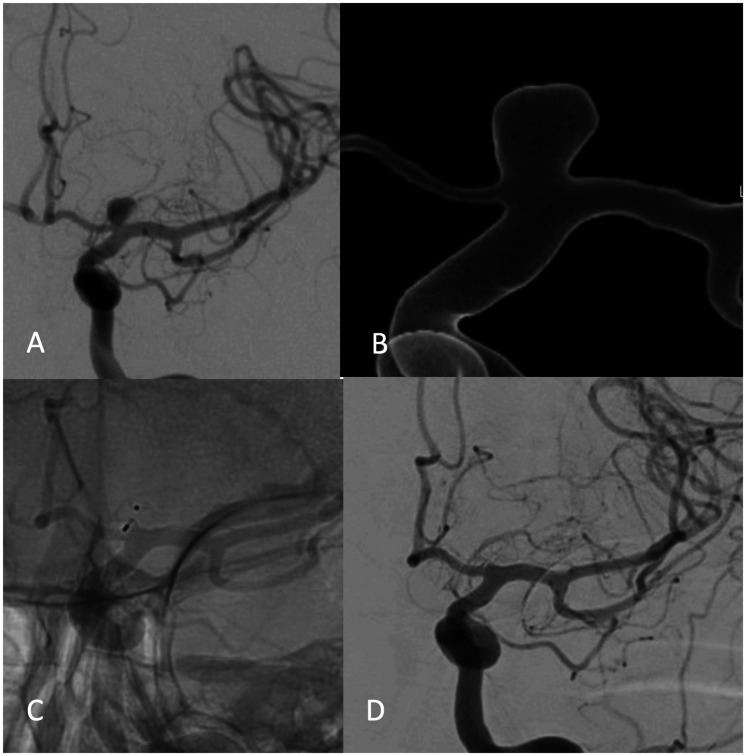
Figure 1.
49-year-old woman with an incidental carotid tip aneurysm: (a, b) 2D (a) and 3D (b) angiogram demonstrates wide-necked aneurysm; (c) WEB position after placement; (d) 5-years follow-up angiogram with stable complete occlusion.
Figure 2.
55-year-old woman with an unruptured middle cerebral artery aneurysm additional to another ruptured aneurysm: (a) oblique right internal carotid angiogram shows wide-necked middle cerebral artery aneurysm; (b) immediately after WEB placement; (c) complete occlusion on two years follow-up angiogram.
Table 4.
Results of follow-up angiography according to the Web Occlusion Scale (WOS).
| Aneurysm occlusion | Six months | Two years | Five years |
|---|---|---|---|
| WOS A | 61 (70%) | 41 (78%) | 4 (100%) |
| WOS B | 7 (8%) | 4 (8%) | |
| WOS C | 14 (16%) | 5 (10%) | |
| WOS D | 5 (6%) | 2 (4%) | |
| Total patients with follow-up (n = 95) | 87 (92%) | 52 (55%) | 4 (4%) |
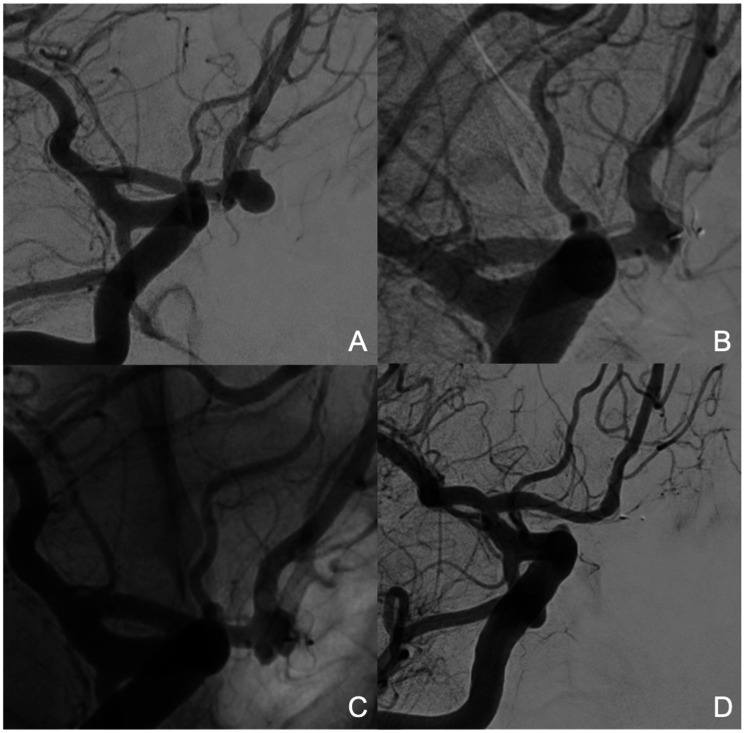
Figure 3.
51-year-old female patient with an incidental A1–A2 aneurysm: (a) aneurysm in oblique view with visible Acom. Good A1 on the left side; (b) Six months after treatment revealing impaction with a neck remnant of 2 mm; (c) control angiogram two years after initial treatment with further growing neck remnant to 3 mm. At that time, the decision was made to treat with a flow diverter (P48) to occlude the remnant; (d) control angiogram at six months shows a good occlusion of the remnant and occlusion of the Acom connection.
There were no hemorrhagic complications during the follow-up period.
Discussion
In this study of WEB treatment of wide-necked unruptured aneurysms, the safety and efficacy of the treatment were excellent. Morbidity was 1% and there was no mortality. At six months follow-up, 92% of aneurysms were adequately occluded and the retreatment rate was 4.5%. These results were generally obtained with the use of a single WEB device without additional devices. No antiplatelet therapy was needed in the peri- and postprocedural period.
Although confidence intervals are relatively wide in our study, results compare favorably with recent meta-analyses of WEB treatment of intracranial aneurysms.20,21,24 In the WEB single-layer review,24 cumulative morbi-mortality was almost 4% and the retreatment rate was over 8%. In a meta-analysis by Armoiry et al.,20 permanent morbidity and mortality were 2.2–6.7% and 0–17%, respectively. The adequate occlusion rate varied between 65 and 85% at midterm follow-up. In another meta-analysis,21 midterm complete and adequate occlusion rates after a median of seven months were 39% (95% CI, 26–52%) and 85% (95% CI, 78–91%), respectively. Perioperative morbidity and mortality rates were 4% (95% CI, 1–8%) and 1% (95% CI, 0–2%), respectively.
The safety of WEB treatment for unruptured (wide-necked) aneurysms is comparable with simple coiling but is better than both stent- or balloon-assisted coiling5,27–29 and flow diversion.10,14–16 In a meta-analysis by Algra,29 compared with standard coiling, the pooled OR for complications in stent-assisted coiling was 1.82 (95% CI, 1.16–2.85%) and in balloon-assisted coiling 1.25 (95% CI, 0.71–2.20%).
Between February 2013 and January 2020, 19 meta-analyses concerning the treatment of cerebral aneurysms with flow diverters have been published.10,15,16 Morbi-mortality of flow diversion has a broad range from almost 2–10% depending on the series. This large range can be largely explained due to high variable risk of flow diversion depending on the treatment difficulty of the target lesion. The efficacy at one year is also largely variable with means of around 80%.11,12,30
Since its introduction a decade ago, the WEB has proven to be a safe and effective device for both ruptured and unruptured (wide-necked) aneurysms. The WEB is increasingly used for all types of aneurysms, bifurcation or sidewall, wide-necked, or small-necked.26–28 The WEB may be used as an alternative for stent-assisted coiling or flow diverters in wide-necked unruptured aneurysms. The major advantage of the WEB is that peri-procedural and longstanding anti-platelet medication is not necessary. Moreover, the technique of WEB placement is relatively straightforward and comparable with standard coiling. Once the microcatheter is inside the aneurysm, WEB placement is relatively easy and quick. The WEB device is an innovative endovascular treatment device originally designed for wide-neck and bifurcation aneurysms that are technically challenging for endovascular treatment. With the progressive technical improvement of the WEB with lower profiles, smaller sizes, and low-profile catheters, indications are no longer limited to wide-neck bifurcation aneurysms. Also, sidewall aneurysms and aneurysms on distal locations are now more and more treated with the WEB.
A major concern is the retreatment rate after the use of WEB devices.30–32 Previous long-term series reported a rate in between 11.5 and 16.3%, however Lylyk et al recently reported a retreatment rate up to 19.5%.33–35 In our series we had a rather low retreatment rate of 4.5%. This lower retreatment rate can partly be explained due to our tendency to oversize the WEB as described recently by Guenego et al.26 However, Herbretau et al.36 did not find a relation between sizing and occlusion status. Unruptured aneurysms, location of the aneurysm in the anterior circulation and a wide neck size of 4-10 mm were shown to be more prone to aneurysmal remnants and the need for retreatment.37 Initial partial aneurysm thrombosis, recurrent aneurysms and combination treatment of WEB with coils seem to be associated with higher aneurysm reoccurrence.38 Kabbasch et al.38 described a higher recurrence rate in relation to the height of a treated aneurysm. The mean neck size (4.5–5 mm depending on the aneurysm location) of treated aneurysms in our series was rather low and this could be a reason for our lower retreatment rate.
Lately new “neck-reconstructing” devices emerged and are available for the treatment of wide necked and bifurcation aneurysms (Contour, P-Conus, PulseRider, eCLIPse, Medina ea.).39–47 These devices could be promising in those patients with a potential higher recurrence risk when using WEB treatment. However, the occlusion rate ranges from 50 to 83% depending on the device used.
Our results confirm the excellent safety and efficacy profiles, comparable with standard coiling, for the WEB in the treatment for unruptured aneurysms. Our study lacks the long-term follow-up to confirm our low retreatment rates. In our view, the WEB should be considered as a safe option for wide-necked, side-wall or bifurcation aneurysms. However, further research should be done to provide details concerning the best suited aneurysms to be treated with WEB and to determine the reasons for higher retreatment rates in some patients.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Tom De Beule https://orcid.org/0000-0002-2987-5818
Sam Heye https://orcid.org/0000-0001-8819-4847
Williem J van Rooij https://orcid.org/0000-0001-5931-1186
Wim van Zwam https://orcid.org/0000-0003-1631-7056
References
- 1.Piotin M, Blanc R, Spelle L, et al. Stent-assisted coiling of intracranial aneurysms: clinical and angiographic results in 216 consecutive aneurysms. Stroke 2010; 41: 110–115. [DOI] [PubMed] [Google Scholar]
- 2.Bartolini B, Blanc R, Pistocchi S, et al. Y” and “X” stent-assisted coiling of complex and wide-neck intracranial bifurcation aneurysms. Am J Neuroradiol 2014; 35: 2153–2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chalouhi N, Jabbour P, Singhal S, et al. Stent-assisted coiling of intracranial aneurysms: predictors of complications, recanalization, and outcome in 508 cases. Stroke 2013; 44: 1348–1353. [DOI] [PubMed] [Google Scholar]
- 4.Chung J, Lim YC, Suh SH, et al. Stent-assisted coil embolization of ruptured wide-necked aneurysms in the acute period: incidence of and risk factors for periprocedural complications. J Neurosurg 2014; 121: 4–11. [DOI] [PubMed] [Google Scholar]
- 5.Bechan RS, Sprengers ME, Majoie CB, et al. Stent-assisted coil embolization of intracranial aneurysms: complications in acutely ruptured versus unruptured aneurysms. Am J Neuroradiol 2016; 37: 502–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guzzardi G, Cossandi C, Carriero A, et al. Flow diverter stents with hydrophilic polymer coating for the treatment of acutely ruptured aneurysms using single antiplatelet therapy: preliminary experience. Interv Neuroradiol 2020; 26: 525–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pierot L, Soize S, Eker O, et al. Surface-modified flow diverter p48-MW-HPC: preliminary clinical experience in 28 patients treated in two centers. J Neuroradiol. Epub ahead of print 17 December 2020. DOI: 10.1016/j.neurad.2020.11.006. [DOI] [PubMed]
- 8.Aguilar-Perez M, Hellstern V, Henskens H, et al. The p48 flow modulation device with hydrophilic polymer coating (HPC) for the treatment of acutely ruptured aneurysms: early clinical experience using single antiplatelet therapy. Cardiovasc Intervent Radiol 2020. May; 43: 740–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Castro-Alfonso L, Nakiri G, Abud DG, et al. Aspirin monotherapy in the treatment of distal intracranial aneurysms with surface modified flow diverter: pilot study. J Neurointerv Surg. Epub ahead of print 29 Jan 2021. DOI: 10.1136/neurintsurg-2020-017024. [DOI] [PubMed]
- 10.Houdart E.Meta-analysis as a symptom: the example of flow diverters. Am J Neuroradiol 2020; 41: E51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.De Beule T, Boulanger T, Stockx L, et al. P64 flow diverter: results in 108 patients from a single center. Interv Neuroradiol 2021; 27: 51–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hanel R, Kallmes D, Puri A, et al. Prospective study on embolization of intracranial aneurysms with the pipeline device: the PREMIER study 1 year results. J NeuroInterv Surg 2020; 12: 62–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yan Y, Zhu D, Tang H, et al. Safety and efficacy of flow diverter treatment for aneurysms in small cerebral vessels: systematic review and meta-analysis. World Neurosurg 2018; 115: 54–64. [DOI] [PubMed] [Google Scholar]
- 14.Zhou G, Su M, Yin YL, et al. Complications associated with the use of flow-diverting devices for cerebral aneurysms: a systematic review and meta-analysis. Neurosurg Focus 2017; 42: E17. [DOI] [PubMed] [Google Scholar]
- 15.Arrese I, Sarabia R, Pintado R, et al. Flow diverter devices for intracranial aneurysms: systematic review and meta-analysis. Neurosurgery 2013; 73: 193–199. [DOI] [PubMed] [Google Scholar]
- 16.Zhou G, Su M, Zhu YQ, et al. Efficacy of flow diverting devices for cerebral aneurysms: a systematic review and meta-analysis. World Neurosurg 2016; 85: 252–262. [DOI] [PubMed] [Google Scholar]
- 17.Pierot L, Spelle L, Molyneux A, WEBCAST and French Observatory Investigators et al. Clinical and anatomical follow-up in patients with aneurysms treated with the WEB device: 1-year follow-up report in the cumulated population of 2 prospective, multicenter series (WEBCAST and french observatory). Neurosurgery 2016; 78: 133–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pierot L, Gubucz I, Buhk JH, et al. Safety and efficacy of aneurysm treatment with the WEB: results of the WEBCAST 2 study. Am J Neuroradiol 2017; 38: 1151–1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pierot L, Costalat V, Moret J, et al. Safety and efficacy of aneurysm treatment with WEB: results of the WEBCAST study. J Neurosurg 2016; 124: 1250–1256. [DOI] [PubMed] [Google Scholar]
- 20.Armoiry X, Turjman F, Hartmann DJ, et al. Endovascular treatment of intracranial aneurysms with the WEB device: a systematic review of clinical outcomes. Am J Neuroradiol 2016; 37: 868–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Asnafi S, Rouchaud A, Pierot L, et al. Efficacy and safety of the Woven EndoBrigde (WEB) device for the treatment of intracranial aneurysms: a systemic review and meta-analysis. Am J Neuroradiol 2016; 37: 2287–2292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Rooij WJ, Peluso JP, Bechan RS, Sluzewski M.WEB treatment of ruptured intracranial aneurysms. Am J Neuroradiol 2016; 37: 1679–1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arthur AS, Molyneux A, Coon AL, WEB-IT Study investigators et al. The safety and effectiveness of the Woven EndoBridge (WEB) system for the treatment of wide-necked bifurcation aneurysms: final 12-months results of the pivotal WEB intrasaccular therapy (WEB-IT) study. J Neurointerv Surg 2019; 11: 924–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Van Rooij SB, van Rooij WJ, Sprengers ME, et al. A systematic review and meta-analysis of Woven EndoBridge single layer for treatment of intracranial aneurysms. Interv Neuroradiol 2020; 26: 455–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fiorella D, Arthur A, Byrne J, et al. Interobserver variability in the assessment of aneurysm occlusion with the WEB aneurysm embolization system. J Neurointerv Surg 2015; 7: 591–595. [DOI] [PubMed] [Google Scholar]
- 26.Guenego A, Januel AC, Darcourt J, et al. Influence of WEB oversizing on aneurysm occlusion and device compaction. J Neuroradiol 2019; 46: 64. [Google Scholar]
- 27.van Rooij SB, van Rooij WJ, Peluso JP, Sluzewski M.The Woven EndoBridge (WEB) as primary treatment for unruptured intracranial aneurysms. Interv Neuroradiol 2018; 24: 475–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Rooij SBT, van Rooij WJ, Peluso JP, et al. WEB treatment of ruptured intracranial aneurysms: a single center cohort of 100 patients. Am J Neuroradiol 2017; 38: 2282–2287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Algra AM, Lindgren A, Vergouwen MDI, et al. Procedural clinical complications, case-fatality risks, and risk factors in endovascular and neurosurgical treatment of unruptured intracranial aneurysms: a systematic review and meta-analysis. JAMA Neurol 2019; 76: 282–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Greving JP, Wermer MJ, Brown RD, et al. Development of the PHASES score for prediction of risk of rupture of intracranial aneurysms: a pooled analysis of six prospective cohort studies. Lancet Neurol 2014; 13: 59–66. [DOI] [PubMed] [Google Scholar]
- 31.Chapot R, Mosimann PJ, Darsaut TE, et al. Retreatments must be included in the evaluation of device performance. J Neurointerv Surg. Epub ahead of print 14 September 2020. DOI: 10.1136/neurintsurg-2020-016619. [DOI] [PMC free article] [PubMed]
- 32.Pierot L, Molyneux A, Byrne J, et al. Retreatments are part of the evaluation of device performance … but have to be analyzed separately. NeuroIntervent Surg. Epub ahead of print 14 September 2020; DOI: 10.1136/neurintsurg-2020-016773. [DOI] [PubMed]
- 33.Mine B, Goutte A, Brisbois D, et al. Endovascular treatment of intra-cranial aneurysms with the Woven EndoBridge device: mid term and long term results. J Neurointerv Surg 2018; 10: 127–132. [DOI] [PubMed] [Google Scholar]
- 34.Fujimoto M, Lylyk I, Bleise C, et al. Long-term outcomes of the WEB device for treatment of wide-neck bifurcation aneurysms. Am J Neuroradiol 2020; 41: 1031–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pierot L, Klisch J, Liebig T, et al. WEB-DL endovascular treatment of wide-neck bifurcation aneurysms: long-term results in a European series. Am J Neuroradiol 2015; 36: 2314–2319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Herbreteau D, Bibi R, Narata AP, et al. Are anatomic results influenced by WEB shape modification? Analysis in a prospective, single center series of 39 patients with aneurysms treated with the WEB? Am J Neuroradiol 2016; 37: 2280–2286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang SM, Liu LX, Ren PW, et al. Effectiveness, safety and risk factors of Woven EndoBridge device in the treatment of wide-neck intracranial aneurysms: systematic review and meta-analysis. World Neurosurg 2019; 136: e1–e23. [DOI] [PubMed] [Google Scholar]
- 38.Kabbasch C, Goertz L, Siebert E, et al. Factors that determine aneurysm occlusion after embolization with the Woven EndoBridge (WEB). J Neurointerv Surg 2019; 11: 503–510. [DOI] [PubMed] [Google Scholar]
- 39.Dmytriw A, Salem M, Yang V, et al. Endovascular flow disruption: a new frontier in endovascular aneurysm management. Neurosurgery 2020; 86: 170–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Akhunbay-Fudge CY, Deniz K, Tyagi AK, et al. J. Endovascular treatment of wide-necked intracranial aneurysms using the novel contour neurovascular system: a single-center safety and feasibility study. J Neurointerv Surg 2020; 12: 987–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lylyk P, Chudyk J, Bleise C, et al. The pCONus2 neck-bridging device: early clinical experience and immediate angiographic results. World Neurosurg 2018; 110: e766–e775. [DOI] [PubMed] [Google Scholar]
- 42.Spiotta AM, Derdeyn CP, Liu KC, et al. Results of the ANSWER trail using the PulseRider for treatment of broad-necked, bifurcation aneurysms. Neurosurgery 2017; 81: 56–65. [DOI] [PubMed] [Google Scholar]
- 43.Chiu AH, De Vries J, Tippett et al. The second-generation eCLIPs endovascular clip system: initial experience. J Neurosurg 2017; 128: 1–8. [DOI] [PubMed] [Google Scholar]
- 44.Gory B, Aguilar-Pérez M, Pomero E, et al. One year angiographic results after pCONus stent-assisted coiling of 40 wide-neck middle cerebral artery aneurysms. Neurosurgery 2017; 80: 925–933. [DOI] [PubMed] [Google Scholar]
- 45.Sourour N-A, Vande Perre S, Maria FD, et al. Medina® embolization device for the treatment of intracranial aneurysms: safety and angiographic effectiveness at 6 months. Neurosurgery 2018; 82: 155–162. [DOI] [PubMed] [Google Scholar]
- 46.Bhogal P, AlMatter M, Hellstern V, et al. The combined use of intraluminal and intrasaccular flow diversion for the treatment of intracranial aneurysms: report of 25 cases. Neurointervention 2018; 13: 20–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Perez MA, Bhogal P, Moreno RM, et al. The medina embolic device: early clinical experience from a single center. J Neurointerv Surg 2017; 9: 77–87. [DOI] [PMC free article] [PubMed] [Google Scholar]