Abstract
Introduction
Withholding the malignant bone tumors disclosure from patients is common in China. The purpose of the study was to explore the perceptions of patients, families, doctors, and nurses regarding the disclosure of malignant bone tumors in China.
Method
Semistructured interviews were conducted with 25 cases, consisting of 69 participants (14 patients, 25 family members, 17 doctors, and 13 nurses), and the transcripts were analysed using Colaizzi’s (1978) descriptive phenomenological analysis process.
Results
Five themes were identified: (1) doctors preferred to inform the family members first, (2) family members’ decisions depended on different situations, (3) the patients agreed that disclosure should be different for each person/personally, (4) care from nurses reduced the overreaction of patients, and (5) key points improve the informing quality.
Discussion
Family participatory cancer disclosure and multidisciplinary teams could improve the quality of cancer disclosure. Culturally congruent health care and culturally sensitive interventions in cancer disclosure are suggested.
Keywords: bone tumor, cancer disclosure, qualitative research
Introduction
In most Western countries, doctors always inform patients with cancer diagnoses directly (Liu et al., 2019; Temraz et al., 2019; Yang et al., 2018). However, withholding information on cancer diagnosis or prognosis from patients is a common practice in Asian and Middle Eastern countries (Ehsani et al., 2016; Ni & Alraek, 2017). In China, most patients, even in the late stage of cancer, are not informed of the malignant result; this decision is always determined by family members (Yang et al., 2018). Family caregivers’ truth disclosure opinions play an important role in the process of caring for cancer patients (Tang, 2018). However, if a patient is not informed, the patient loses autonomy in his care process.
With the development of medicine, medical ethics, and norms of law, the thinking of the current situation for cancer notification in China has begun to change from the ethical concern of “whether patients should be informed” to the technical concern of “how should patients be informed” (Wang et al., 2011). Some studies have focused on who should be the one to inform patients, when and how information should be given, and the quality of cancer disclosure in minimizing the side effects of “bad news” in China (Li et al., 2012; Zeng et al., 2011). Additionally, there is interest in how the patient’s age, education, and economic condition influence the decision of how the patient should be informed (Liu et al., 2018). There are also established protocols or guidelines in the United States, Britain, Canada, and Australia for delivering bad news effectively (Abazari et al., 2016; Gilligan et al., 2017; Stiefel et al., 2018). Moreover, the experience and skills of doctors are very important for cancer disclosure.
However, the present cancer communication guidelines from the West may not be suitable for the Chinese due to the family decision-making culture in China. In China, decisions taken jointly by the family are more important than individual decisions. Moreover, medical staff, patients, and family from different cultural and educational backgrounds may also have different preferences for cancer disclosure (Trenchard et al., 2016). Therefore, family members’ decisions play an important role in cancer disclosure (Hahne et al., 2020). Cancer disclosure is a complex process involving medical practice as well as a range of cultural, ethical, and legal factors (Wu et al., 2020). The quality of cancer disclosure is directly related to the patients’ stress and anxiety, the reaction to “bad news,” and the satisfaction with therapeutic outcomes (Jie et al., 2016; Seifart et al., 2014). Although malignant bone tumors account for less than 1% of all diagnosed cancers each year, the morbidity and mortality of malignant bone tumors are significant (Ferguson & Turner, 2018). Osteosarcoma or Ewing sarcoma with pulmonary metastasis has a survival rate of only 20% to 30% (Anderson, 2016). Additionally, serious disability risks, such as amputation and paralysis, should be mentioned during the informing process for malignant bone tumors (González-Rodríguez et al., 2014; Phukan et al., 2016). The strategy adopted for bone tumor disclosure is very important for the success of therapy. However, the guidelines for the disclosure of bone cancer are still unavailable in China.
In this study, the authors explored and described the preference, rationale, and procedure of the disclosure of malignant bone tumors by conducting interviews with patients, family members, and medical staff in China.
Method
Study Design and Participants
This study was conducted using the phenomenological research method for qualitative interviews. Data collection was performed using a semistructured interview questionnaire. Participants’ experiences, attitudes, thoughts, expectations, motives, and interactions were recorded (Ni & Alraek, 2017). A subjective interpretation of textual data and content was applied by using the systematic process of coding and identifying themes or categories. We conducted one-on-one interviews. All interviews were conducted by the first author of this study. All the authors completed the training course of the qualitative research method and interview skills at our university. The interviewer (Master of Public Health) had worked as an orthopedic nurse for 20 years. Participants were selected through purposive sampling. All participants in this study were recruited from a university-affiliated hospital in Chongqing, China. The inclusion criteria for patients were as follows: age ≥18 years, a pathological diagnosis of malignant bone tumor, no communication disorders or mental illness, and voluntary participation. Patients who were not informed of their condition were excluded. The inclusion criteria for family members were direct relatives and the main caregivers, participation in treatment decision making, and basic written and verbal communication abilities. The inclusion criteria for doctors and nurses were having more than 3 years of experience in the treatment and care of malignant bone tumor patients. The preliminary semistructured interview guide was designed by surveying the literature on seeking experts’ views. After preliminary interviews with four participants, the interview guide was amended, and modified guides and details of the interviews were confirmed by all authors. The interview guides are presented in Table 1.
Table 1.
Interview Guide.
| Interviewees | Interviews aspects with open-ended questions |
|---|---|
| All of the participants | The procedure of informing the patient about the illness condition |
| The reaction of patients and families after being informed about the illness condition | |
| The advantages and disadvantages of telling patients the truth or not | |
| How to inform | |
| The role of family members in the informing process | |
| Addition for doctors and nurses only | Cancer notification experience in the past work |
| If you were a family member of the cancer patient, what would you do? |
Data Collection
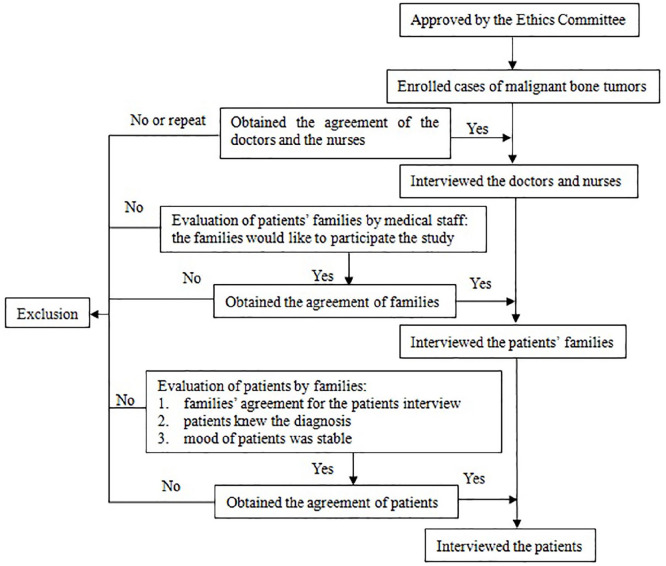
Data were collected by semistructured, face-to-face, and one-on-one interviews from June 2018 to July 2019. Patients and families were interviewed within a week after the tumor diagnosis. With a reflective, or even a self-reflective attitude, the researchers interviewed the informants in a nonjudgmental manner listening and open to all experiences of the participants. Researchers did not participate in the clinical treatment of the associated patients. Before the interview, the purpose and reasons of this study were explained to the interviewees, and their agreement for the recording was also obtained. All interviews were conducted with the written consent of the participants. We conducted semistructured individual interviews in a meeting room of the orthopedics department, Xinqiao Hospital. The interviewer confirmed that the interview environment was quiet and undisturbed. All interviews began with free talk first to make participants relax. Interview content was audio recorded. To protect the privacy of the interviewees, the results of the study were kept anonymous, and the names were replaced by numbers. Field notes with thoughts, feelings, responses, and nonverbal communication were made during interviews. Each interview lasted 20 to 50 minutes, and the median length was 35 minutes. There were three repeat interviews. Data saturation occurred when no new themes appeared by data analysis (Ehsani et al., 2016). Information saturation was reached after conducting interviews with 12 patients, 23 family members, 15 doctors, and 11 nurses. The process of determining interviewees is presented in Figure 1.
Figure 1.
The process of determining interviewees.
Data Analysis
Data collection and analysis were carried out simultaneously. The analysis method was used to manually analyze the data. First, data from the audio-recorded interviews were transcribed verbatim. All transcripts were returned to the participants for comment and correction. Then, the consensus transcripts were further processed by two individual researchers using Colaizzi’s (1978) descriptive phenomenological seven-stage framework as follows: (1) read and reread all the participants’ descriptions of the phenomenon under study, (2) extract significant statements from each description that directly pertain to the phenomenon, (3) formulate meanings from these significant statements, (4) organize these formulated meanings into themes, (5) integrate the results of the data analysis into a description of the phenomenon under study, (6) return the results to the participants for validation, and (7) incorporate any new, relevant data into the fundamental structure of the phenomenon.
Ethics Approval
This study was approved by the ethics committee of the Third Military Medical University (No. 2018-0601) and was conducted in accordance with the Declaration of Helsinki. We protected the right of informed consent of the interviewees. The purpose and significance of the research were introduced to the interviewees before the interview. Written informed consent forms were signed by all interviewees. Interviewees have the right to withdraw from the research at any time during the research process. The personal data of the interviewees were not disclosed in any form.
Results
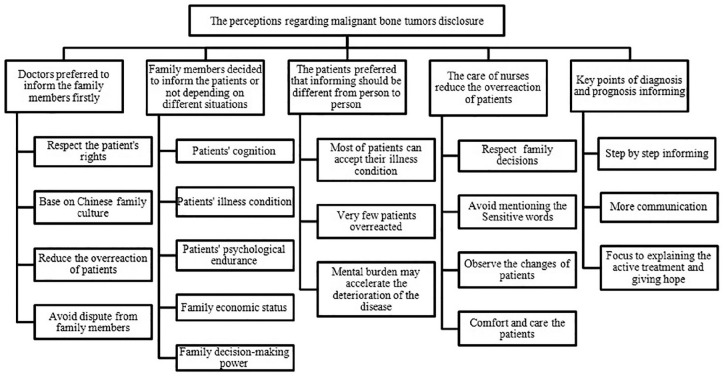
In this study, 69 participants, including 14 patients, 25 family members, 17 doctors, and 13 nurses, were enrolled from 25 cases. Six patients were not informed, and 5 patients declined to participate in this study. The participants had a wide range of ages: patients (18-60 years), family members (27-60 years), doctors (27-53 years), and nurses (28-50 years). The average work experience was approximately 11 years for doctors and 14 years for nurses. The details are shown in Table 2. Fifty-two meaning units were identified from the analysis of the recordings and transcripts. From these, the synthesized transformed meaning units were formed, and 19 subthemes and 5 themes unfolded. Figure 2 presents the themes in the form of a coding tree chart.
Table 2.
Participants’ Characteristics.
| Characteristics | Patient (n = 14); n (%) | Family member (n = 25); n (%) | Doctor (n = 17); n (%) | Nurse (n = 13); n (%) |
|---|---|---|---|---|
| Gender | ||||
| Male | 9 (64) | 7 (28) | 17 (100) | |
| Female | 5 (36) | 18 (72) | 13 (100) | |
| Age (years) | ||||
| 18-30 | 4 (29) | 3 (12) | 6 (35) | 3 (23) |
| 31-40 | 1 (7) | 3 (12) | 8 (47) | 9 (69) |
| 41-50 | 2 (14) | 8 (32) | 1 (6) | 1 (8) |
| 51-60 | 7 (50) | 11 (44) | 2 (12) | |
| Education | ||||
| Middle school | 3 (22) | 8 (32) | ||
| High school | 9 (64) | 15 (60) | ||
| University | 2 (14) | 2 (8) | 17 (100) | 13 (100) |
| Job status | ||||
| Student | 2 (14) | |||
| Farmer | 1 (7) | 3 (12) | ||
| Employee | 9 (64) | 19 (76) | ||
| Unemployed | 2 (14) | 3 (12) | ||
| Work experience (years) | ||||
| 1-10 | 13 (76) | 3 (23) | ||
| 11-20 | 1 (6) | 9 (69) | ||
| 21-30 | 2 (12) | |||
| 31-40 | 1 (6) | 1 (8) | ||
Figure 2.
Coding tree for thematic analysis.
Essence 1: Doctors Preferred to Inform the Family Members of the Diagnosis and Prognosis First
Doctors respect the patient’s rights and accept the benefit of knowing the diagnosis results: “About the right to know of the patients, I prefer to provide the full and true disclosure. It is not only a legal requirement but also the responsibilities of our medical staff” (Doctor 17). However, in China, most doctors informed the family members of the results first. Based on Chinese family decision-making culture, decisions taken jointly by the family are more important than individual decisions. The family members decided whether to inform the patients. Doctors thought that this is a better way to reduce the overreaction of patients and avoid dispute among family members according to Chinese culture and situations:
First, we would like to tell the family members. We suggest that family members should inform the patient tactfully first and talk with doctors for the details of diseases. In this way, cooperation may be more comprehensive, and the advantages outweigh the disadvantages. The family members will tell the patients or not depending on their willingness. Sometimes the family makes decisions for these patients. In view of the culture and economic conditions of China, most of the patients’ families will communicate with doctors about the way of cancer disclosure first; sometimes the families chose to hide the truth. Once the doctor informs the patient without the agreement of family members, disputes may occur between family members and doctors. (Doctor 3)
Essence 2: Family Members Decided to Inform the Patients or Not Depending on Different Situations
Factors that are considered in whether the family members should inform the patient include the patient’s cognition, illness condition, and psychological endurance; the family economic status; and the family decision-making power: “We usually notify the family members first, and then they will assess the patient’s psychological endurance. Some of the family members chose to give up the notification for economic reasons, and the others assessed the patient’s cognitive ability” (Doctor 13).
Among the patients who are not informed, most of the family members act out of kindness to protect the patients from psychological distress:
My daughter just underwent the surgery. She was paraplegic before the operation, and now her concern is whether she can move. If the doctor let her know the truth, as a young girl, she may not be able to afford it, even commit suicide. (Family member 1)
On the other hand, some family members withhold the truth because they cannot afford the payment of the therapy: “If the family members cannot afford the payment of the therapy, they will ask us not to inform the patient” (Doctor 5). A few elderly patients were not informed due to the lack of sufficient education: “My mother may not understand the meaning of cancer. She just thinks it is just a mass” (Family member 3). “He is senile and his condition is terminal, so we may not tell him” (Family member 9).
Essence 3: The Patients Preferred That Disclosure Should Be Different From Person to Person
Most of the patients believe that they can accept their illness condition and calm down soon, but sometimes they are a little worried:
It is better for me to know it. When I know the truth, I will make the decision to accept the therapy or not. Additionally, I will make the plan for the future life. If you do not tell me, I will have a kind of anxiety in mind, and my mentality will not be good. I will doubt what disease I have. (Patient 13)
“I think I must be told the truth. I should make my own decision on the treatment. If the condition deteriorates and metastasizes, I should also be informed” (Patient 14). “Sometimes, patients are more receptive than their families. I am worrying about the cost, the family burden, and the side effects of treatment” (Patient 2). Very few patients overreacted and could not accept the truth:
There was a patient with osteosarcoma. After knowing his condition, he did not want to have an amputation and was discharged from the hospital. Approximately half a year later, the tumor grew to a large size and metastasized to the lung. The patient lost the chance of surgery. (Nurse 12)
However, the patients also thought it should vary from person to person about disease disclosure. Patients’ mental burden may accelerate the deterioration of the disease: “It is not suitable for everyone. The doctor should communicate with the patient first and consider his personality. It is better not to tell those who have depression. I’m in favor of asking my family for advice first” (Patient 6).
It is up to the family to judge. It is also very important to listen to the opinions of family members. It is not only an issue between doctors and patients but also the family members. The patients have the right to know the truth. However, some old patients with insufficient education depend on their family members. Some of them will not ask the doctor about the illness. It is even worse if you tell them the truth. (Patient 10)
Essence 4: Care From Nurses Could Reduce the Overreaction and Excessive Behavior of Patients
Nurses respect family decisions for disease disclosure. Even if the patient is aware of the condition, it is necessary to avoid mentioning the sensitive words in front of the patient to avoid the patient’s overreaction:
In my opinion, nurses should first respect the decisions of patients’ families. Early confidentiality of patients is a kind of protection, and they should not suffer from the adverse effects of such excessive psychological stimulation. If patients cannot bear it, they will respond negatively. It may even lead to suicide. Then, the patient’s safety is certainly not guaranteed. (Nurse 5)
“In my opinion, it is not necessary for nurses to talk about the patient’s condition too much in the process of patient care. We should avoid strengthening their particularity and the role of patients” (Nurse 13).
Nurses should observe the psychological and behavioral changes of patients to prevent excessive behavior: “When nurses know the diagnosis of a suspected tumor, they will communicate with doctors and family members. Nurses will pay attention to observing the patient’s reaction, behavior changes, and whereabouts” (Nurse 1).
He is a patient who knows his condition and does not show obvious abnormal changes at ordinary times. However, one night, he tried to kill himself with the wire of the call bell. Fortunately, he was rescued by our nurses during the inspection. (Nurse 10)
Nurses need to comfort and care for the patients:
In fact, nurses can accompany, listen to, and comfort patients. The nurse can also encourage patients with some positive treatment or thoughts. Because the doctor’s communication time is short; after all, the nurse has more time to contact the patient, and the psychological support provided by the nurse is very important. (Nurse 11)
The nurse can give the patient a way to communicate, just like a friend. Maybe he does not need you to make a big decision for him, but he needs to talk to you about his conflicts; let him relieve the pressure. I think I can be a perfect listener for my patients. (Nurse 1)
Essence 5: Key Points of Diagnosis and Prognosis Disclosure
Step-by-Step Informing
The general method of diagnosis and prognosis disclosure is to downplay the patient’s condition, inform them of their condition little by little, and help the patient accept it slowly:
First, the disease still has a slow acceptance process. Second, we can dilute this matter. We will let the patients know that a lesion was identified with the potential risk of malignant tumor, and then, after a few days and the biopsy, we will tell the patient that it is a malignant tumor. That is how it goes step by step. (Doctor 11)
Improved Communication
In the process of diagnosis and prognosis disclosure, the most fundamental step is to communicate with the patients deeply:
For malignant bone tumors, I usually communicate with family members first. I will tell them the severity of the disease, the cost, and the expectation of the operation. On the good understanding of the family members, I will communicate with the patient. Some patients cannot bear it psychologically, or they are melancholy and worry too much. If you tell them, and they cannot bear the disease after listening too much, they even give up the therapy. Full communication could give the patients and their families strong psychological support and encourage them to make every possible effort. (Doctor 6)
Focus on Explaining the Active Treatment and Giving Hope
When patients are diagnosed with cancer, great psychological, physiological, economic and social pressures are faced (D. Wei et al., 2013). At the same time, doctors and nurses should fully consider that their patients would suffer from general cancer and the possibility of paraplegia and amputation. Therefore, when patients are confronted with a double strike, the challenge of doctors and nurses is not limited to simply informing and nursing:
On the one hand, doctors should inform of the severity of the disease. On the other hand, they should let the patients know what methods are available for effective treatment and give guidance for the patients to the process of active treatment. (Family member 18)
Knowing the cancer diagnosis always makes the patients feel like they were already dead. There was a large psychological fluctuation for these patients. At the same time, the points of view of these patients just shift from treatment to death, such as how long I could live, what I could do. Therefore, I would like psychological counseling to help patients refocus on the treatment by nurses. (Doctor 4)
Discussion
Family Member Information Is a Line of CHINESE Characteristics According to the Family Decision-making Culture
In China, many patients are not informed of the real condition when they are diagnosed with malignant tumors. With improvements in economic conditions, educational levels, access to information, and cancer treatment technology in China, an increasing number of patients can accept cancer diagnosis peacefully (Sun et al., 2015; S. S. Wei et al., 2016). In this study, patients with a cheerful personality and high education level preferred to take the initiative to know the diagnosis and prognosis of their disease and actively participate in treatment, which is consistent with Yang’s report (Yang et al., 2018). However, in this study, we found that all of the patients, families, and medical staff still preferred informing the family members first. Although the doctors acknowledged that the right to know should be respected, according to Chinese culture, family decision-making power always occurs prior to the personal power of the patient. Diagnosis and prognosis disclosure without the agreement of families may cause an overreaction of the patient and dissatisfaction of families, and a conflict between doctors and families will even occur. Therefore, doctors had to inform the families of the results first. Then, family members decided whether to inform the patients according to different situations, such as the family condition, patient psychological quality, and family decision-making power. Although all the patients in this study thought that they should know about the disease, they also preferred that their families should know it first. However, we did not interview the attitudes of the uninformed patients in this study. This phenomenon reflects a common Chinese family decision-making culture.
Family Participatory Cancer Disclosure Strategies Should Be Developed Based on the Chinese Family Culture
Our results indicated that all participants, including medical staff, patients, and family members, believed that family members should be involved. A family participatory cancer disclosure strategy may be a more suitable and feasible way for patients in China. Several models for bad news breaking, such as the American SPIKES and the Japanese SHARE, provide the reference for the procedure and skills of cancer disclosure (Baile et al., 2000; Fujimori et al., 2014). Additionally, some organizations in Europe and America continually updated guidelines of cancer patient–clinician communication (Gilligan et al., 2017; Stiefel et al., 2018). However, these guidelines with no family factors involved are not suitable for Chinese patients according to the family decision-making culture in China. The Chinese psychosocial oncology therapy guidelines for cancer patients published in 2016 still lack the family factors. Only a few Western communication skills-training model courses for cancer disclosure in China were held in the past decade (Pang et al., 2015). Therefore, we believe that the combination of these guidelines and Chinese family decision-making culture may be the direction for cancer diagnosis disclosure to take in China (Hahne et al., 2020).
Multidisciplinary Teams Including Doctors, Nurses, and Psychologists Can Improve the Quality of Cancer Information
Although different educational levels, personalities, and family conditions were found in this study, patients and their families still faced great psychological pressure during cancer disclosure. Psychological support could help them get through difficult times. In the report of Cao et al. (2017), the authors summarized some points of cancer disclosure on the cooperation of doctors and nurses to comfort and support patients and their families. In our study, the results showed that the cooperation of doctors and nurses for psychological support played an important role during cancer disclosure. The daily care of nurses can significantly reduce the overreaction of patients. Key points of diagnosis and prognosis disclosure, such as step-by-step informing, deep communication, explaining active treatment, and giving hope, are potential ways to help patients accept the results. However, psychological support from doctors and nurses always depends on personal experience. An integrated cancer notification requires not only the collaboration of doctors, nurses, and family members (Liu et al., 2018; Liu et al., 2019) but also the involvement of psychologists (Gan et al., 2018). It is important to develop a multidisciplinary team, including doctors, nurses, and psychologists, for cancer disclosure. In this way, psychological support will be more comprehensive and professional to help patients and families accept bad news peacefully.
Limitations
Although all participants were selected from a single medical center and all focused on only bone tumors, our study still may provide the reference for other regions and other diseases. Deep analysis and exploration must be considered according to the condition of different regions and cultures.
Conclusion
The authors presented the views of cancer diagnosis information disclosure from patients, family members, doctors, and nurses. The current strategy of cancer disclosure is based on the pattern of family decision making in China. However, many patients with a good education background have a sense of self-determination and prefer to know the cancer diagnosis directly. In this interview, the vast majority of interviewees believed that the disclosure of cancer should be provided or not according to different patients, and the determination of the family should be respected. Family participatory cancer disclosure strategies and multidisciplinary teams, including doctors, nurses and psychologists, can improve the quality of cancer disclosure.
Practice Implications
This study focuses on the core role of family decision making in cancer disclosure in China. It concluded that it should be explored scientific and reasonable family participation cancer disclosure strategies and multidisciplinary teams based on the Chinese cultural background. The results not only provide information on how the Chinese culture affect cancer disclosure but also could provide the global culturally congruent health care strategies. Health care providers should understand how culture affects the behaviors, attitudes, preferences, and decisions on cancer disclosure. It is suggested to develop decision-assisting tools that assess the conditions of education, economy, family, mental health, and illness according to different cultures. The preference of the patient and their family should be assessed, and culturally sensitive measures should be taken in different races (Cuellar et al., 2020).
Acknowledgments
We would like to thank all the participants who took part in this research.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the clinical nursing research project of Xinqiao Hospital, Army Medical University [2017XQHLYG-01], the nursing innovation fund of Nursing School of Army Medical University [2019hlcxz02], and the humanities and social sciences fund of Army Medical University [2019XRW17].
ORCID iDs: Chunmei Luo  https://orcid.org/0000-0002-6919-9711
https://orcid.org/0000-0002-6919-9711
References
- Abazari P., Taleghani F., Hematti S., Ehsani M. (2016). Exploring perceptions and preferences of patients, families, physicians, and nurses regarding cancer disclosure: A descriptive qualitative study. Support Care Cancer, 24(11), 4651-4659. 10.1007/s00520-016-3308-x [DOI] [PubMed] [Google Scholar]
- Anderson M. E. (2016). Update on survival in osteosarcoma. Orthopedic Clinic of North America, 47(1), 283-292. 10.1016/j.ocl.2015.08.022 [DOI] [PubMed] [Google Scholar]
- Baile W. F., Buckman R., Lenzi R., Glober G., Beale E. A., Kudelka A. P. (2000). SPIKES—a six-step protocol for delivering bad news: Application to the patient with cancer. Oncologist, 5(4), 302-311. 10.1634/theoncologist.5-4-302 [DOI] [PubMed] [Google Scholar]
- Cao W. D., Qi X. N., Yao T., Han X. Y., Feng X. J. (2017). How doctors communicate the initial diagnosis of cancer matters: Cancer disclosure and its relationship with patients’ hope and trust. Psycho-Oncology, 26(5), 640-648. 10.1002/pon.4063 [DOI] [PubMed] [Google Scholar]
- Colaizzi P. E. (1978). Psychological research as the phenomenologist views it. In Valle R. S., King M. (Eds.), Existential-phenomenological alternatives for psychology (pp. 49-71). Oxford University Press. [Google Scholar]
- Cuellar N. G., Aquino E., Dawson M. A., Garcia-Dia M. J., Im E., Jurado L. M., Lee Y. S., Littlejohn S., Tom-Orme L., Toney D. A. (2020). Culturally congruent health care of COVID-19 in minorities in the United States: A clinical practice paper from the National Coalition of Ethnic Minority Nurse Associations. Journal Transcultural Nursing, 31(5), 434-443. 10.1177/1043659620941578 [DOI] [PubMed] [Google Scholar]
- Ehsani M., Taleghani F., Hematti S., Abazari P. (2016). Perceptions of patients, families, physicians and nurses regarding challenges in cancer disclosure: A descriptive qualitative study. European Journal of Oncology Nursing, 25, 55-61. 10.1016/j.ejon.2016.09.003 [DOI] [PubMed] [Google Scholar]
- Ferguson J. L., Turner S. P. (2018). Bone cancer: Diagnosis and treatment principles. American Family Physician, 98(4), 205-213. [PubMed] [Google Scholar]
- Fujimori M., Shirai Y., Asai M., Akizuki N., Katsumata N., Kubota K., Uchitomi Y. (2014). Development and preliminary evaluation of communication skills training program for oncologists based on patient preferences for communicating bad news. Palliative Supportive Care, 12(5), 379-386. 10.1017/S147895151300031X [DOI] [PubMed] [Google Scholar]
- Gan Y. Q., Zheng L., Yu N. X., Zhou G. Y., Miao M., Lu Q. (2018). Why do oncologists hide the truth? Disclosure of cancer diagnoses to patients in China: A multisource assessment using mixed methods. Psycho-Oncology, 27(5), 1457-1463. 10.1002/pon.4545 [DOI] [PubMed] [Google Scholar]
- Gilligan T., Coyle N., Frankel R. M., Berry D. L., Bohlke K., Epstein R. M., Finley E., Jackson V. A., Lathan C. S., Loprinzi C. L., Nguyen L. H., Seigel C., Baile W. F. (2017). Patient-clinician communication: American Society of Clinical Oncology consensus guideline. Journal of Clinical Oncology, 35(31), 3618-3632. 10.1200/JCO.2017.75.2311 [DOI] [PubMed] [Google Scholar]
- González-Rodríguez E., Riveros A., Benjet C., González-Forteza C., León-Hernández S. R., Rico-Martínez G. (2014). Quality of life in patients with bone tumors, a comparison between different treatments. Revista de Investigación Clínica, 66(2), 121-128. [PubMed] [Google Scholar]
- Hahne J., Liang T., Khoshnood K., Wang X., Li X. (2020). Breaking bad news about cancer in China: Concerns and conflicts faced by doctors deciding whether to inform patients. Patient Education and Counseling, 103(2), 286-291. 10.1016/j.pec.2019.08.022 [DOI] [PubMed] [Google Scholar]
- Jie B., Qiu Y., Feng Z. Z., Zhu S. N. (2016). Impact of disclosure of diagnosis and patient autonomy on quality of life and illness perceptions in Chinese patients with liver cancer. Psycho-Oncology, 25(8), 927-932. 10.1002/pon.4036 [DOI] [PubMed] [Google Scholar]
- Li J., Yuan X. L., Gao X. H., Yang X. M., Jing P., Yu S. Y. (2012). Whether, when, and who to disclose bad news to patients with cancer: A survey in 150 pairs of hospitalized patients with cancer and family members in China. Psycho-Oncology, 21(7), 778-784. 10.1002/pon.1979 [DOI] [PubMed] [Google Scholar]
- Liu Y. X., Yang J. H., Huo D., Fan H. H., Gao Y. F. (2018). Disclosure of cancer diagnosis in China: The incidence, patients’ situation, and different preferences between patients and their family members and related influence factors. Cancer Management and Research, 10, 2173-2181. 10.2147/CMAR.S166437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y. X., Yang J. H., Song L., Yang X., Yin Y. L., Yan L. P. (2019). Nurses’ experiences and attitudes toward diagnosis disclosure for cancer patients in China: A qualitative study. Psycho-Oncology, 28(12), 2415-2421. 10.1002/pon.5273 [DOI] [PubMed] [Google Scholar]
- Ni Y. H., Alraek T. (2017). What circumstances lead to non-disclosure of cancer-related information in China? A qualitative study. Support Care Cancer, 25(3), 811-816. 10.1007/s00520-016-3464-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pang Y., Tang L. L., Zhang Y. N., Song L. L., Goelz T., Fritzsche K., Wuensch A. (2015). Breaking bad news in China: Implementation and comparison of two communication skills training courses in oncology. Psycho-Oncolo, 24(5), 608-611. 10.1002/pon.3698 [DOI] [PubMed] [Google Scholar]
- Phukan R., Herzog T., Boland P. J., Healey J., Rose P., Sim F. H., Yezsemski M., Hess K., Osler P., DeLaney T., Chen Y.-L., Hornicek F., Schwab J. (2016). How does the level of sacral resection for primary malignant bone tumors affect physical and mental health, pain, mobility, incontinence, and sexual function? Clinical Orthopaedics and Related Research, 474(3), 687-696. 10.1007/s11999-015-4361-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seifart C., Hofmann M., Bär T., Knorrenschild J. R., Seifart U., Rief W. (2014). Breaking bad news-what patients want and what they get: Evaluating the SPIKES protocol in Germany. Annals of Oncology, 25(3), 707-711. 10.1093/annonc/mdt582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stiefel F., Kiss A., Salmon P., Peters S., Razavi D., Cervantes A., Marguiles A., Bourquin C. (2018). Training in communication of oncology clinicians: A position paper based on the third consensus meeting among European experts in 2018. Annals of Oncology, 29(10), 2033-2036. 10.1093/annonc/mdy343 [DOI] [PubMed] [Google Scholar]
- Sun W. W., Wang Z. H., Fang S., Li M. M. (2015). Factors influencing the attitudes of Chinese cancer patients and their families toward the disclosure of a cancer diagnosis. Journal of Cancer Education, 30(1), 20-25. 10.1007/s13187-014-0687-x [DOI] [PubMed] [Google Scholar]
- Tang Y. (2018). Death attitudes and truth disclosure: A survey of family caregivers of elders with terminal cancer in China. Nursing Ethics, 26(7-8), 1968-1975. 10.1177/0969733018809805 [DOI] [PubMed] [Google Scholar]
- Temraz S., Hammoud M. S., Saleh A., Charafeddine M., Mukherji D., Shamseddine D. M. (2019). Perceptions of cancer status disclosure in Lebanon. Journal of Cancer Education, 34(5), 874-881. 10.1007/s13187-018-1389-6 [DOI] [PubMed] [Google Scholar]
- Trenchard L., Grath-Lone L. M., Ward H. (2016). Ethnic variation in cancer patients’ ratings of information provision, communication and overall care. Ethnicity & Health, 21(5), 515-533. 10.1080/13557858.2015.1126561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D. C., Guo C. B., Peng X., Su Y. J., Chen F. (2011). Is therapeutic non-disclosure still possible? A study on the awareness of cancer diagnosis in China. Support Care in Cancer, 19(8), 1191-1195. 10.1007/s00520-010-0937-3 [DOI] [PubMed] [Google Scholar]
- Wei D., Tian Y., Gao H., Peng J. J., Tan Y., Li Y. (2013). Patient distress and emotional disclosure: A study of Chinese cancer patients. Journal of Cancer Education, 28(2), 346-351. 10.1007/s13187-012-0404-6 [DOI] [PubMed] [Google Scholar]
- Wei S. S., Chen F. L., Chen H. Y., Guo Y., Hui D., Yennurajalingam S, Chisholm G., Liu E., Liao Z., Yang L., Cheng H., Zhou Y., Guo H., Bruera E. (2016). Patients’ and family members’ decision-making and information disclosure preferences in a single-center survey in China: A pilot study. American Journal of Hospice and Palliative Medicine, 33(8), 733-741. 10.1177/1049909115588302 [DOI] [PubMed] [Google Scholar]
- Wu J., Wang Y., Jiao X., Wang J., Ye X., Wang B. (2020). Differences in practice and preferences associated with truth-telling to cancer patients. Nursing Ethics, 28(2), 272-281. 10.1177/0969733020945754 [DOI] [PubMed] [Google Scholar]
- Yang F. M., Zhang Q., Kong W., Shen H. D., Lu J., Ge X. L., Zhuang Y. Y. (2018). A qualitative study on the attitudes of patients with gastrointestinal cancer toward being informed of the truth. Patient Preference and Adherence, 12, 2283-2290. 10.2147/PPA.S179465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng T. Y., Huang H. S., Zhao M. Z., Li Y., Fang P. Q. (2011). Health professionals’ attitude towards information disclosure to cancer patients in China. Nursing Ethics, 18(3), 356-363. 10.1177/0969733011398096 [DOI] [PubMed] [Google Scholar]