Abstract
Purpose:
Among human cancers that harbor mutant (mt) KRas, some, but not all, are dependent on mt KRas. However, little is known about what drives KRas dependency.
Experimental Design:
Global phosphoproteomics, screening of a chemical library of FDA drugs and genome-wide CRISPR/Cas9 viability database analysis were used to identify vulnerabilities of KRAS dependency.
Results:
Global phosphoproteomics revealed that KRas dependency is driven by a cyclin dependent kinase (CDK) network. CRISPR/Cas9 viability database analysis revealed that, in mt KRas-driven pancreatic cancer cells, knocking out the cell cycle regulators CDK1 or CDK2 or the transcriptional regulators CDK7 or CDK9 was as effective as knocking out KRas. Furthermore, screening of a library of FDA drugs identified AT7519, a CDK 1, 2, 7, and 9 inhibitor, as a potent inducer of apoptosis in mt KRas-dependent, but not in mt KRas-independent, human cancer cells. In vivo AT7519 inhibited the phosphorylation of CDK1, 2, 7 and 9 substrates and suppressed growth of xenografts from 5 pancreatic cancer patients. AT7519 also abrogated mt KRas and mt p53 primary and metastatic pancreatic cancer in 3D organoids from 2 patients, 3D co-cultures from 8 patients, and mouse 3D organoids from PanIN, primary and metastatic tumors.
Conclusion:
A link between CDK hyperactivation and mt KRas dependency was uncovered and pharmacologically-exploited to abrogate mt KRas-driven pancreatic cancer in highly relevant models, warranting clinical investigations of AT7519 in pancreatic cancer patients.
Keywords: KRas, patient-derived xenografts, patient-derived organoids, phosphoproteomics, pancreatic cancer, cyclin-dependent kinases, KRas dependency, genome-wide CRISPR/Cas9, gRNA, AT7519
Introduction
KRas is a member of the GTP/GDP-binding GTPase family that acts as a binary molecular switch, active when bound to GTP and inactive when bound to GDP, to transduce biological information from outside to inside cells. As such it regulates signal transduction pathways such as Raf/Mek/Erk, RalGDS/Ral, PI3K/Akt, p190/Rho, and TIAM1/Rac that are involved in biological processes such as cell proliferation, growth, differentiation, and survival1,2. In normal cells, this molecular switch is tightly regulated by guanine exchange factors (GEFs) that catalyze the release of GDP and the binding of GTP, and GTPase activating proteins (GAPs) that stimulate the hydrolysis of GTP to GDP3. In contrast, in tumors, KRas mutations interfere with GAP-stimulated GTP hydrolysis leading to GTP-locked and constitutively activated KRas, which in turn contributes to cancer hallmarks such as hyperproliferation, apoptosis evasion, invasion, and metastasis4.
KRas mutations are among the most prevalent mutations in human cancers, with an overall frequency of one in four patients. These frequencies are highest among the deadliest cancers with 90% in pancreatic ductal adenocarcinoma (PDAC), 40% in colorectal cancer (CRC), and 30% in non-small cell lung cancer (NSCLC)5,6. Human cancers harbor different types of KRas mutations with hot spots at amino acids G12, G13, and Q61. Common mutations in KRas are G12D, G12V, G12C, G13D, and Q61R5. Tumors that harbor KRas mutations are highly aggressive, invasive, metastatic, and associated with poor patient prognosis7–11. In addition, patients whose tumors harbor KRas mutations are resistant to chemotherapy and other treatment modalities, and a result the guidelines by the National Comprehensive Cancer Network (NCCN) are to test for KRas mutation status prior to treatment decisions. For example, NCCN recommends treatment with epidermal growth factor receptor inhibitors only when patient tumors harbor wild-type (wt) KRas10,12.
Although the significant contributions of KRas to human tumorigenesis, poor prognosis, and therapy resistance have been known for decades, to date there are no FDA-approved anticancer drugs that directly target KRas. This is partly due to difficulties in identifying small molecules that bind to the relatively flat surface of Kras, which lacks well-defined druggable binding sites. However, recent major accomplishments have been made in selectively targeting the KRas G12C isoform13,14. This was possible because the G12C mutation offered the possibility of covalent binding through the free SH thiol group of the cysteine in position 1213,15. Several inhibitors targeting G12C, such as AMG-510, MRTX849, and ARS-3248, are now in clinical trials with encouraging results16–18, although adaptive resistance has been reported with several of these17,19,20. The discovery of KRas G12C inhibitors represents a major milestone in the KRas drug discovery field, and if successful in clinical trials will have a major impact on our ability to treat cancers with high frequencies of the KRas G12C mutation such as NSCLC. However, the majority of KRas mutations in human cancers are G12D and G12V, and these have been much harder to target13.
An alternative approach to targeting mt KRas-driven cancers is to take advantage of vulnerabilities of these cancers by identifying druggable proteins that mt KRas requires to cause cancer21. A key observation that facilitates this approach is that among human tumors that harbor KRas mutations, some are KRas-dependent, whereas others are KRas-independent22. Understanding the mechanism of mt KRas dependency is critical to understanding how KRas drives tumorigenesis, and consequently identifying novel targets and developing innovative therapies against tumors that are addicted to KRas. In this study, we used comparative phosphoproteomics, genome-wide CRISPR/Cas9 viability screen database analysis, and FDA drugs library screening to identify differences in signal transduction pathways between KRas-dependent and KRas-independent human cancers. Together, our studies revealed that cyclin-dependent kinases (CDKs) 1, 2, 7, and 9 play a significant role in KRas dependency and that suppression of these CDKs selectively abrogates mt KRas pancreatic cancer in highly relevant models, including patient-derived organoids and xenografts.
Materials and Methods
Phosphoproteomics:
Phosphorylation profiles for mt KRas cancer cell lines were generated using 10 mg of total protein. After denaturation, digestion, and buffer exchange, tyrosine-phosphorylated peptides (pY) were immunoprecipitated using the PTMscan kit (p-Y-1000, Cell Signaling Technology), according to the manufacturer’s instructions. Tyrosine phosphorylated peptides were analyzed with label free LC-MS/MS and the peak apex of the extracted ion chromatogram was used for quantification. Using a 200 μg aliquot of total protein digest from each sample and pooled samples for batch-to-batch comparison, tryptic peptides were chemically labeled with tandem mass tags, mixed in equal amounts, and fractionated with basic pH reversed phase liquid chromatography prior to phosphopeptide enrichment with immobilized metal affinity chromatography (Cell Signaling Magnetic Beads) using a Kingfisher (Thermo). Because 10 cell lines were studied, two different TMT 6plex experiments were performed using a common pooled cell line sample in both TMT experiments to support comparison between the two batches. TMT-labeled, IMAC-enriched phosphopeptides were analyzed with liquid chromatography-tandem mass spectrometry peptide sequencing to identify peptide sequences, localize phosphorylation sites, and provide relative quantification in each sample. Data were analyzed with MaxQuant55, normalized, and statistically evaluated prior to NetworKIN and GeneGO/Metacore pathway analysis (Clarivate Analytics). Additional detailed descriptions are provided in the supplemental materials.
Phosphoproteomics data analysis:
As described above, phosphoproteomics data were processed with MaxQuant to both match spectra to phosphopeptides and quantify phosphopeptide intensities. Label free intensity data for tyrosine-phosphorylated peptides was normalized with IRON56 (iron_generic --proteomics) against the median sample (A549_Run1). TMT reporter ion intensity data for IMAC-enriched phosphopeptides were normalized within 6-plex against the shared pool (channel 126) using IRON56. Ratios were then calculated within each 6-plex for each sample vs. the shared pool channel. Separately, the pool channels from each 6-plex were normalized against one another, then averaged together using a geometric mean to generate an averaged pool intensity for each phosphosite. The phosphosite ratios were then scaled back into intensities again using the averaged pool intensities for each phosphosite to yield the final normalized phosphosite intensities. The normalized label free data for tyrosine phosphorylated peptides and TMT phosphopeptide intensities from IMAC global phosphopeptide enrichment were then merged together into a single spreadsheet to create a single view of overall kinase signaling and log2 transformed prior to further analyses.
Assessment of data quality was performed using principal component analysis (PCA). A two-group comparison was performed between the 5 KRAS-dependent and 5 KRAS-independent groups. For each phosphosite, the average was calculated within each group (Avgdep, Avgind), then the 2 averages were subtracted to yield the log2 ratio between groups. T-tests and Hellinger distances were also calculated. The following criteria was then used to select differentially expressed (DE) phosphosites: row is not a reverse sequence hit (used to establish false discovery rate) and does not contain any potential contaminants (e.g., bovine proteins from culture media), |log2 ratio| ≥ ~0.585 (which corresponds to a 1.5-fold change), T-test p value < 0.05, and Hellinger distance > 0.25. Phosphosites were then ranked by Score, calculated as the sign of the log2 ratio, multiplied by the geometric mean of |log2 ratio| and -log10(p value). A second series of two-group comparisons was performed within the site of origin (SOO), to filter out potential SOO-related effects. Within each SOO, all combinations of log2 ratios were calculated between individual KRAS-dependent and KRAS-independent samples. The majority sign was determined across all 8 comparisons (2 colon, 4 lung, 2 pancreas), and the fraction of log2 ratios exhibiting the majority sign was calculated. The list of DE phosphosites was then further filtered by requiring that the majority signs agree with the signs from the initial two-group comparison, and that the fraction of SOO-related comparison exhibiting the majority sign ≥ 0.75.
NetworKIN 3.057 was used to identify potential kinases that may have phosphorylated the DE phosphosites. The data for the heatmaps were ordered in Excel (Supplemental Table 1) prior to data export and graphical visualization. Columns were ordered by KRas dependence state (independent, dependent), followed by SOO within group, then alphabetically by cell line within SOO. Phosphosites were sorted by direction of change (positive, negative), then by |Score| within direction of change. Rows were mean-centered, then their magnitude away from zero capped at +/− 2 (4-fold) prior to visualization.
Cells lines, cell culture, and reagents:
Human lung (Calu-6, A549, H460, A427), colon (SW620, DLD-1, and HCT-8), pancreatic (MiaPaCa2, PANC-1, and L3.6pl) cancer cell lines were obtained from the American Type Culture Collection and cultured in Dulbecco’s modified Eagle’s medium (DMEM) or RPMI-1640 medium. Normal lung fibroblast cell lines WI-38, IMR-90, and MRC-5 were kindly provided by Eric Haura, MD (Moffitt Cancer Center, Tampa, FL) and were cultured in minimum essential medium. All media were supplemented with 10% heat-inactivated fetal bovine serum, 10 U/mL penicillin, and 10 μg/mL streptomycin. AT7519 was purchased from TargetMol, Boston, MA. The library of 294 clinically relevant FDA drugs (the majority of which are FDA approved or are/have been in clinical trials) was purchased from commercial vendors and put together by Dr. Uwe Rix (Department of Drug Discovery, Lung Cancer Center of Excellence, Moffitt Cancer Center, Tampa, FL). The list of all the FDA drugs used in the screen can be found in Supplemental Table 3. All cell lines were Mycoplasma free, monitored regularly with HEK-blue2 cells and Mycoplasma Detection Kit from InvivoGen (catalog No. rep-pt1). All cell lines were authenticated by the University of Arizona Genetics Core.
Cell viability assay:
Cell viability assays were carried out using the CellTiter-Glo Luminescent Cell Viability Assay (Promega, Madison, WI) as described by us23. Cells were seeded in 384-well plates at a density of 1000 cells/well, allowed to adhere overnight, and treated with vehicle or AT7519 for 72 h, after which they were processed for viability using CellTiter-Glo reagent.
Screening of FDA clinically relevant 294 compounds library:
Eight human cancer cell lines: 4 KRas-dependent (MiaPaCa2, L3.6pl, Calu-6, and SW620) and 4 KRas-independent (A549, H460, DLD-1, and HCT-8), were screened with the 294 FDA clinically relevant (the majority of which are FDA approved or are/have been in clinical trials) compound library to identify a potent compound that can selectively inhibit the viability of mt KRas-dependent over mt KRas-independent cells using the CellTiter-Glo Luminescent Cell Viability Assay (Promega, Madison, WI). Cells were cultured in 384-well plates at a density of 1000 cells/well and allowed to adhere overnight. The medium was then replaced with medium containing vehicle (0.1% DMSO) or 1 μM of each of 294 compounds for 72 hours in one compound-one well format. After which they were processed for viability using CellTiter-Glo reagent as described by us previously23.
Determining gene dependency across human cancer cell lines.
To determine the effects of knocking out KRas, HRas, NRas, and 41 CDKs on the viability of human cancer cell lines, we mined the BROAD institute genome-scale CRISPR/Cas9 essentiality screens across 342 cancer cell lines. To this end, we analyzed the dataset of Avana Ceres Gene Effect (BROAD institute, MIT. https://depmap.org/ceres/), which uses CERES, a computational method that estimates gene-dependency levels from CRISPR/Cas9 essentiality screens accounting for the copy number-specific effect (depletion values = sum of gene-knockout and copy number effects). First, we determined the effect of knocking out KRas by CRISPR guide RNA on cell viability of cancer cell lines from different human organs. We calculated the percentage of inhibition of cell viability using the following formula: [% inhibition of viability = (1–2CRISPR Gene Score)*100]. Next, we used the same dataset to determine the average effects of knocking out 41 CDKs by CRISPR guide RNA on the cell viability of 23 pancreatic cancer cell lines. Finally, we determined the effects of knocking out CDK1, CDK2, CDK7, and CDK9 by CRISPR guide RNA on cell viability of each of the 23 individual pancreatic cancer cell lines.
Western blot analysis:
To prepare whole-cell lysates, cells were trypsinized, washed twice with cold PBS, and lysed in mammalian protein extraction reagent (product No. 78501, Thermo Fisher Scientific) supplemented with protease inhibitor cocktail (product No. A32953, Thermo Fisher Scientific), 2 mmol/L phenylmethylsulfonyl fluoride, 2 mmol/L Na3VO4, and 6.4 mg/mL p-nitrophenylphosphate. Tumor tissue samples were lysed in tissue protein extraction reagent (product No. 78510, Thermo Fisher Scientific) with above supplements. The automatic hand-operated OMNI-TIP Homogenizer (Omni International, Inc., Kennesaw, GA) was used to homogenize the tumor tissues. Lysates from whole cells and tumor homogenates were cleared by centrifugation at 12,000 g for 15 minutes, and the supernatants were collected as whole-cell extracts. Protein concentrations were determined using the BCA protein assay kit. Proteins were separated by SDS-PAGE and transferred to nitrocellulose membranes which were then blotted with antibodies specific for Phospho-AKT (S473; Catalog No. 9271S), Phospho-Erk1/2 (Catalog No. 9101L), Total Erk1/2 (Catalog No. 9102L, phosphor-PP1α (T320) (Catalog No. 2581S), phospho-NPM (T199) (Catalog No. 3541S), cleaved-CASP-3 (Catalog No. 9664L), cleaved-PARP (Catalog No. 5625S from Cell Signaling Technology (Danvers, MA, USA); anti-β-ACTIN (Catalog No A5441-.2ML from Sigma Aldrich (St. Louis, MO, USA); Phospho RNA Pol II (Ser 5) (Catalog No. A304–408A); and Phospho RNA Pol II (Ser 2) (Catalog No. A300–654A) from Bethyl Laboratories, Inc., Montgomery, Tx), pRb (Catalog No. ab4787 from Abcam, Cambridge, MA); Mcl-1 (S-19) (Catalog No. sc-819), Total AKT1/2 (N-19; Catalog No. sc-1619 from SantaCruz Biotechnology, Santa Cruz, CA, USA).
Cell culture for 2D and 3D co-cultures for early passage pancreatic cancer patient-derived cell lines:
Human pancreatic cancer cell lines were derived from 8 patient pancreatic tumors using previously described methods29,30. The cells were plated 3,000 per well in triplicate in a 96-well flat bottom plate in RPMI-1640 medium with 10% FBS. Cells were subsequently treated for 72 hours with DMSO or AT7519 at 0.1, 0.3, 1, 3, 10, 30, and 100 μM. For 3D cultures, 15 μL of cold Matrigel (growth factor reduced, phenol red free) was added to wells of 96-well plates, spread evenly, and incubated at 37° C for 30 minutes to solidify. Pancreatic cancer cells (3,000/well) resuspended in RPMI-1640, 2% Matrigel medium with 10% FBS were overlaid on top of the solidified Matrigel, and cultured for 24 hours before treatment. For 3D co-culture, human pancreatic stellate cells (HPSCs) were grown until confluent in RPMI-1640 with 10% FBS. Matrigel was added as in 3D culture and pancreatic cancer cells and HPSCs were resuspended in RPMI-1640 plus 2% Matrigel medium supplemented with 10% FBS, and overlaid at a 1:1 ratio, 3,000 cells per well, and cultured for 24 hours before treatment.
Cell viability assay and live-cell imaging:
Cell viability was determined by CellTiter-Glo Luminescent Cell Viability Assay (Promega, Madison, WI) according to the manufacturer’s protocol. Briefly, cells (3×103 cells/well) were seeded in 96-well plates, allowed to adhere overnight, and treated with vehicle (Normal saline) or drug for 72 hours, after which they were processed for viability using the CellTiter-Glo reagent. Data were normalized to percentage of control, and IC50 values calculated using GraphPad Prism 7.02 software. Live-cell imaging was carried out with the IncuCyte S3 live-cell imaging system (Essen Bioscience, Michigan, USA) through a 4x objective lens at day 0 and 72 hours of treatment. The system is located in a 37˚C/5% CO2 cell culture incubator to maintain proper incubation conditions. Analysis was performed using the basic analyzer module within the IncuCyte S3 2018B software to determine cell growth confluency and a day 0 scan was used as a control.
Organoid culture and drug treatment:
Human organoid hM1a and hT3, and mouse organoid mP2, mT1, mT3, mT69a, mM1, mM2 were obtained from David Tuveson MD, PHD (Cold Spring Harbor Laboratory) and cultured in 100% GFR-Matrigel domes (Corning, 356231) with advanced DMEM/F12-based medium (Thermo Fisher, 12634010) following published protocols32,58. Briefly, the organoid cells were resuspended in 50 μL 100% GFR-Matrigel and slowly dropped to a pre-warmed 24-well plate to form a Matrigel dome. After incubating the dome for 15 minutes at 37°C to harden the Matrigel, the organoids were added with 500 μL of the complete medium and kept growing in a 37°C incubator. The human complete medium was prepared with Advanced DMEM/F12 medium supplemented with HEPES (1x, Invitrogen), Glutamax (1x, Invitrogen), penicillin/streptomycin (1x, Invitrogen), B27 (1x, Invitrogen), Primocin (1mg/mL, InvivoGen), N-acetyl-L-cysteine (1 mM, Sigma), Wnt3a-conditioned medium (50% v/v), RSPO1-conditioned medium (10% v/v, Calvin Kuo), Noggin recombinant protein (0.1 μg/mL, Peprotech), human epidermal growth factor (hEGF, 0.05 μg/mL, Peprotech), human Gastrin (10 nM, Sigma), fibroblast growth factor 10 (hFGF10, 0.1 μg/mL, Prepotech), Nicotinamide (10 mM, Sigma) and A83–01 (0.5 μM, Tocris). The mouse complete medium was prepared with Advanced DMEM/F12 medium supplemented with HEPES (1x, Invitrogen), Glutamax (1x, Invitrogen), penicillin/streptomycin (1x, Invitrogen), B27 (1x, Invitrogen), N-acetyl-L-cysteine (1 mM, Sigma), RSPO1-conditioned medium (10% v/v), Noggin recombinant protein (0.1 μg/mL, Peprotech), mouse epidermal growth factor (mEGF, 0.05 μg/mL, Peprotech), human Gastrin (10 nM, Sigma), human fibroblast growth factor 10 (hFGF10, 0.1 μg/mL, Prepotech), Nicotinamide (10 mM, Sigma) and A83–01 (0.5 μM, Tocris).
For AT7519 drug treatments, organoids were mechanically broken up to single cells by pipetting followed by TrypLE enzymatic dissociation at 37°C. The mouse organoid cells were counted under a microscope and plated in 96-well plates with 1,000–3,000 cells/well in the complete media containing 10% GFR-Matrigel and 10.5 μM Rho Kinase inhibitor Y-27632. These organoids were treated for 10 days with AT7519 at various concentrations in 96-well plates for viability assays. The human organoid cells (1,000 cells/well) were plated into 48-well plate in 15 μL 100% Matrigel supplied with 250 μL complete medium containing 10.5 μM Rho Kinase inhibitor Y-27632. After 4 days of recovering, the cells were treated with AT7519 for 7 days at the indicated concentrations. The viability of organoids under various concentration of AT7519 were imaged with an EVOS microscope and assayed with a Biotek synergy Neo2 plate reader after adding CellTiter-Glo 3D reagent. The CellTiter-Glo data were normalized to percentage of control, and IC50 values were calculated using GraphPad Prism 7.03 software.
Antitumor efficacy studies of PDXs from pancreatic cancer patients:
To assess the antitumor potential of AT7519 in PDXs, fresh tumor biopsies were obtained from 5 patients with pancreatic cancer (4 PDAC and 1 PASC) with KRas mutation (PDXs 1 through 4 from the University of Florida, IRB protocol 201600873; and the 5th PDX from Ohio State University, IRB protocol 2010C0051). Written consent was obtained from the subjects, and the research was conducted according to International Ethical Guidelines for Biomedical Research Involving Human Subjects. The fresh tumor biopsies were from the following 5 patients: Patient 1 (G148) was a 79-year-old female who underwent a radical antegrade modular pancreatosplenectomy. Pathology revealed a 4.5-cm, moderately differentiated, ductal adenocarcinoma with lymphovascular and perineural invasion, 0 out of 10 involved lymph nodes, and negative surgical margins (R0). Pathologic staging was T3N0. KRas mutation was G12D. She completed 4 cycles (Day 1, 8, and 15) of adjuvant gemcitabine over 6 months and radiotherapy. She had evidence of recurrence 10 months after her last cycle of chemotherapy. Patient 2 (G166) was a 50-year-old male who underwent a laparoscopic pancreaticoduodenectomy. Pathology revealed indeterminate size (greater than 2 cm but less than 4 cm), moderately differentiated, ductal adenocarcinoma with lymphovascular and perineural invasion, 1 out of 28 involved lymph nodes, and positive surgical margins (R1). Pathologic staging was T2N1. KRas mutation was G12D. He completed 8 cycles of adjuvant gemcitabine/capecitabine over 5 months. He had no evidence of disease 17 months after his last cycle of chemotherapy. Patient 3 (G174) was a 63-year-old female who underwent a distal pancreatectomy and splenectomy. Pathology revealed a 4.3-cm, poorly differentiated, adenosquamous carcinoma with lymphovascular and perineural invasion, 1 out of 21 involved lymph nodes, and positive surgical margins (R1). Pathologic staging was T3N1. KRas mutation was G12V. She had a presumed recurrence 6 weeks after surgery and died 8 weeks after surgery without receiving adjuvant therapy. Patient 4 (G160) was a 63-year-old male who underwent a laparoscopic pancreaticoduodenectomy. Pathology revealed a 1.5-cm, poorly differentiated, ductal adenocarcinoma with lymphovascular and perineural invasion, 3 out of 24 involved lymph nodes, and negative surgical margins (R0). Pathologic staging was T1N1. KRas mutation was G12D. He completed 5 cycles of 5-FU with radiotherapy over 5 weeks followed by 6 cycles of adjuvant gemcitabine with capecitabine over 5 months (capecitabine stopped after 2 cycles for rash). He had evidence of recurrence 8 months after his last cycle of chemotherapy. Patient 5 (G210) was an 83-year-old female who underwent a laparoscopic distal pancreatectomy and splenectomy. Pathology revealed a 3.5-cm moderate to poorly differentiated ductal adenocarcinoma with lymphovascular and perineural invasion, 3 out of 18 involved lymph nodes, surgical margins (R0). Pathologic staging was pT2N1. KRas mutation was G12R. She completed 6 cycles of gemcitabine and capecitabine over 6.5 months (1st cycle delays due to neutropenia and wound dehiscence). She developed recurrence 4 months after her last cycle of chemotherapy.
The mice were housed, maintained, and treated, and all the experiments were performed under protocols approved by the Moffitt Cancer Center, University of South Florida (protocol # R IS00006177), University of Florida (protocol # 201406590) and Ohio State University (protocol # 2013A00000058) Institutional Animal Care and Use Committees according to federal, state, and institutional guidelines and regulations. Upon pancreatic tumor resection, fresh 2-mm tumor pieces were taken on ice to the animal surgery suite for subcutaneous implantation into NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ (NSG) mice. A viable tumor piece was placed in the right flank subcutaneous tissue of anesthetized mice and the skin was closed (generation 1). Once tumors reached the end point (1.5 cm in diameter), tumors were divided evenly into 2-mm pieces and re-implanted into NSG mice as above (generation 2). Generation 3 was generated similarly as described previously28. When the tumor volumes from generation 3 reached ~200 mm3, the mice were randomized into 2 groups: vehicle (10% DMSO + 20% propylene glycol + 70% of 40% HPCD) and AT7519, which was reconstituted in the same vehicle. Patient 1–5 PDX mice were injected i.p. daily with vehicle or 15 mg/kg/day AT7519 for the indicated days in the figure legend. The vehicle-treated mice group for patient 3’s PDXs grew much faster than the other vehicle-treated groups and on day 17 the experiment was stopped due to protocol tumor-size guidelines. The number of mice in the vehicle-treated groups were 6 (PDX1), 7 (PDX2), 5 (PDX3), 10 (PDX4), and 4 (PDX5). The number of mice in the AT7519-treated groups were 6 (PDX1), 6 (PDX2), 6 (PDX3), 10 (PDX4), and 5 (PDX5).
Results
Global phosphoproteomics reveals a CDK 1 and 2 kinase-substrate network linked to mt KRas dependency
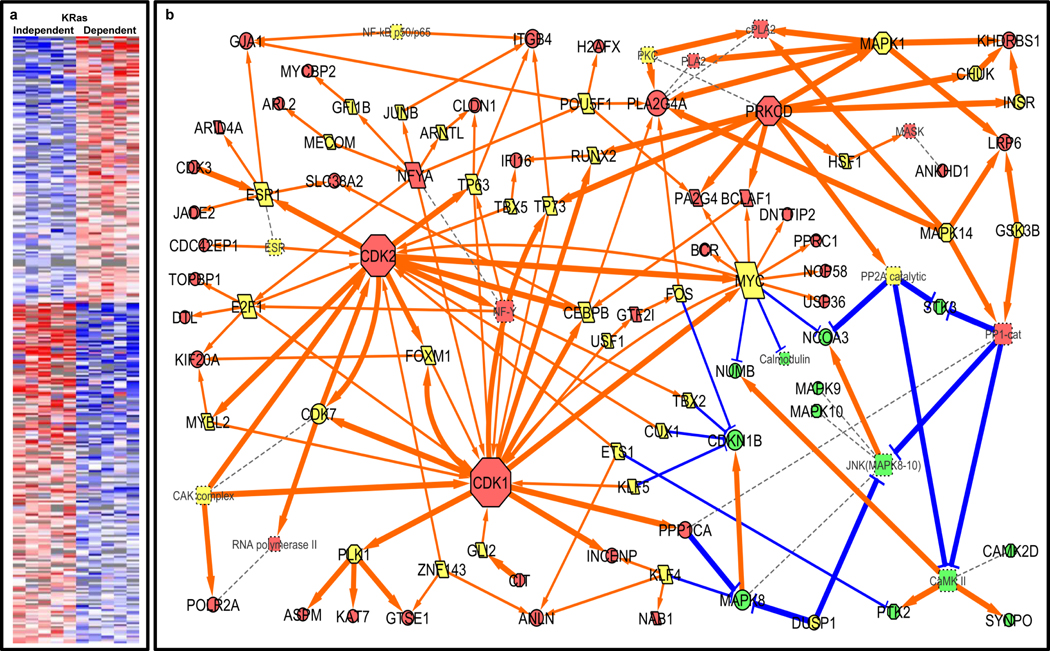
Comparative global phosphoproteomics was used to identify signaling networks and vulnerabilities related to oncogenic dependency on mt KRas using 10 human cancer cell lines from different cancer types, including PDAC (MiaPaCa2, Panc1), pancreatic adenosquamous carcinoma (PASC) (L3.6pl), NSCLC (A549, A427, H460, Calu6), and CRC (SW620, DLD1, HCT8). Although all 10 human cancer cell lines harbor mt KRas, 5 are mt KRas-dependent (MiaPaCa2, L3.6pl, SW620, A427, Calu6), whereas the other 5 are mt KRas-independent (Panc1, DLD1, HCT8, A549, H460), as shown by us and others23–25. To identify differences in signaling networks between mt KRas-dependent and mt KRas-independent cells, LC-MS/MS proteomics was performed on both immunoprecipitated pY peptides and IMAC-enrichment of phosphopeptides to study global phosphorylation (pSTY), as described in Methods. In total, 14,353 unique human phosphosites were identified between the 2 experiments (label free pY: 3,406, TMT pSTY: 11,183; 236 were identified in both datasets), with a false discovery rate of 0.6% at the phosphopeptide level. After independent processing and normalization of the label free pY and TMT pSTY quantitative data, the 2 datasets were merged for further comparison. The merged datasets were analyzed using log2 ratios, T-tests, and Hellinger distance metrics to identify differentially phosphorylated proteins and their specific phosphosites (see Methods). Principal component (PC) analysis showed that site of origin (SOO, pancreas, lung, colon) is linked to PC1 and PC2 for tyrosine phosphorylation, while PC3 is linked to KRas dependency. However, in the global phosphoproteomics data, KRas dependency is a stronger signal than SOO (Supplemental Figure 1).
Of the 14,353 total unique phosphosites, 318 were differentially phosphorylated between mt KRas-dependent and mt KRas-independent cells (Figure 1a and Supplemental Table 1). The selected phosphosites were then used, along with interactions reported in the literature, to generate a mt KRas-dependent vs. mt KRas-independent differential signaling network. CDK1/CDK2 activation was identified as a major component of the KRas-dependent signaling network by linking phosphorylated substrates to the putative kinases using NetworKIN (Supplemental Table 2) and pathway mapping using experimentally consistent literature networks using GeneGO Metacore (Clarivate Analytics), as shown in Figure 1b.
Figure 1: Oncogenic signaling related to KRas dependency revealed by phosphoproteomics.
(a) Comparison of the phosphoproteomes of 5 KRas-dependent and 5 KRas-independent cell lines indicated 318 differentially expressed phosphosites, as shown in the heat map. Data were sorted by direction of change and the magnitude of the differential expression score (see Supplemental Table 1). In the heat map, red and blue indicate higher levels of phosphorylation and lower levels of phosphorylation compared to the mean; gray indicates that the peptide was not detected in that cell line. (b) Differentially phosphorylated peptides were used to create a signaling network, which has CDK1 and CDK2 as central kinase hubs, using the NetworKIN algorithm57 (Supplemental Table 2) and GeneGO Metacore. The node color indicates direction of change between KRas-dependent and -independent cell lines: red = up, green = down. The node shape indicates class of protein: octagon = kinase, parallelogram = transcription factor, dashed square = protein complex, circle = other. Edge thickness, color, and shape indicate the type of interaction: orange pointed arrows = activation, blue T arrows = inhibition; thick lines = phosphorylation, thin lines = transcriptional regulation, dashed lines = membership within a complex.
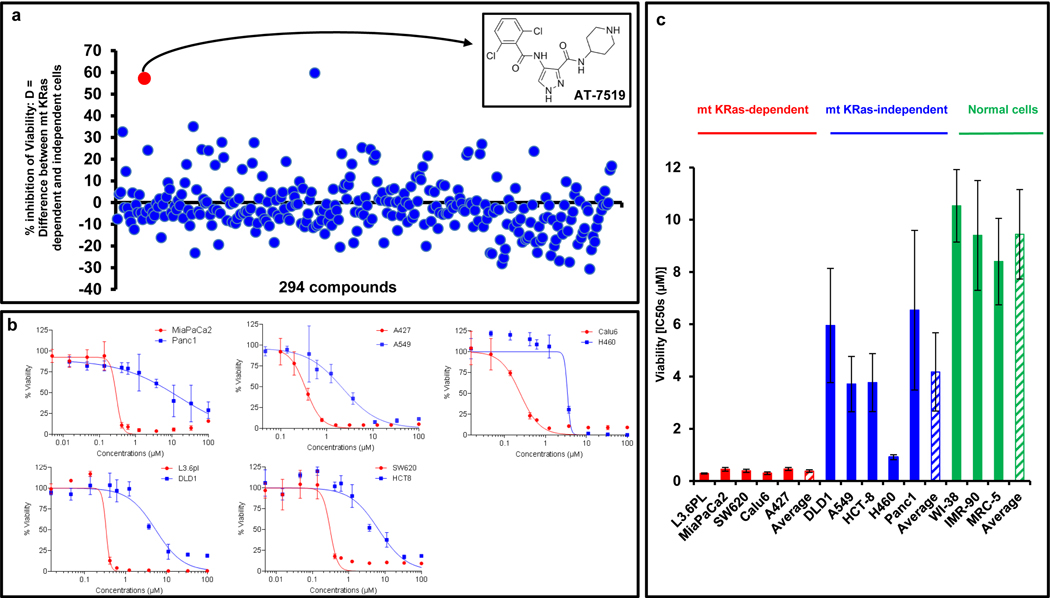
FDA drugs library screening identifies CDK 1, 2, 7, and 9 inhibitor, AT7519, as selective for abrogating mt KRas-dependent human tumors
A library of 294 clinically relevant drugs (the majority of which are FDA approved or are/have been in clinical trials) was used to identify compounds that selectively suppress the viability of 4 mt KRas-dependent (MiaPaCa2, L3.6pl, SW620, and Calu6) human cancer cell lines and not the viability of 4 mt KRas-independent (DLD1, HCT8, A549, H460) human cancer cell lines. To this end, the 294 compounds were evaluated in 3 independent screens against the 8 human cancer cell lines. The screens were performed in 384-well plates using a “one well-one drug” format at 1 μM for 72 hours, and cell viability was assessed by CellTiter-Glo. The difference (D) in the percent inhibition of viability between mt KRas-dependent and mt KRas-independent cells for each compound was calculated based on the average of 3 independent screens. Figure 2a shows that 200 out of the total of 294 compounds screened (68%) affected mt KRas-dependent and mt KRas-independent cell viability equally, with D values ranging from +10% to −10%. The CDK inhibitor AT751926,27 (Figure 2a, inset) was among 2 compounds that had the highest selectivity for inhibiting the viability of mt KRas-dependent over mt KRas-independent cells. To confirm the selectivity of AT7519 for mt KRas-dependent cells, we performed dose-response studies. Figure 2b (top panel) shows representative dose-response curves that demonstrate that AT7519 was more effective at inhibiting mt KRas-dependent cells than mt Ras-independent cells. Figure 2c shows the AT7519 average IC50 values of 4 to 6 independent dose-response experiments for each cell line. AT7519 inhibited the viability of mt KRas-dependent cells with average IC50 values of 0.45 ± 0.07 μM (MiaPaCa2), 0.29 ± 0.02 μM (L3.6pl), 0.39 ± 0.06 μM (SW620), 0.46 ± 0.06 μM (A427), and 0.30 ± 0.05 μM (Calu6). For the mt KRas-independent cells the average IC50 values were 6.54 ± 3.06 μM (Panc1), 3.71 ± 1.06 μM (A549), 5.95 ± 2.19 μM (DLD1), 0.91 ± 0.10 μM (H460), and 3.77 ± 1.1 μM (HCT8). Thus, AT7519 inhibited the viability of all 5 mt KRas-dependent cells with an average IC50 of 0.39 ± 0.03 μM, which was 10.5 times lower than that of the 5 mt KRas-independent cells (4.11 ± 0.77 ±M) (p<0.000005; Figure 2c). Figure 2c also shows that AT7519 was on average 24-fold less effective at inhibiting the viability of “normal” cells (lung fibroblasts) as compared to mt KRas-dependent cancer cells with IC50 values of 10.53 ± 1.39 μM (WI-38), 9.40 ± 2.10 μM (IMR-90), and 8.4 ± 1.66 μM (MRC-5).
Figure 2: FDA drug library screens identify AT7519, CDKs 1, 2, 7 and 9 inhibitor that selectively inhibits the viability of mt KRas-dependent cells.
(a)Mt KRas-dependent (MiaPaCa2, L3.6pl, SW620, and Calu6) and mt KRas-independent (A549, H460, DLD1, and HCT8) human cancer cells were treated for 72 h in 384-well plates with 294 FDA drugs (1 μM) using a one well-one inhibitor format. D [(% inhibition of viability of mt KRas-dependent cells)−(% inhibition of viability of mt KRas-independent cells)] was determined for each compound based on the average of 3 screens as described in Methods. (b) Effects of AT7519 on cell viability of 10 human cancer cell lines, 5 KRas-dependent (Red) and 5 KRas-independent (Blue). (c) IC50 values of AT7519 for inhibition of viability of 5 KRas-dependent (Red) and 5 KRas-independent (Blue) and 3 normal cell lines (Green). The values are averages of at least 3 independent experiments.
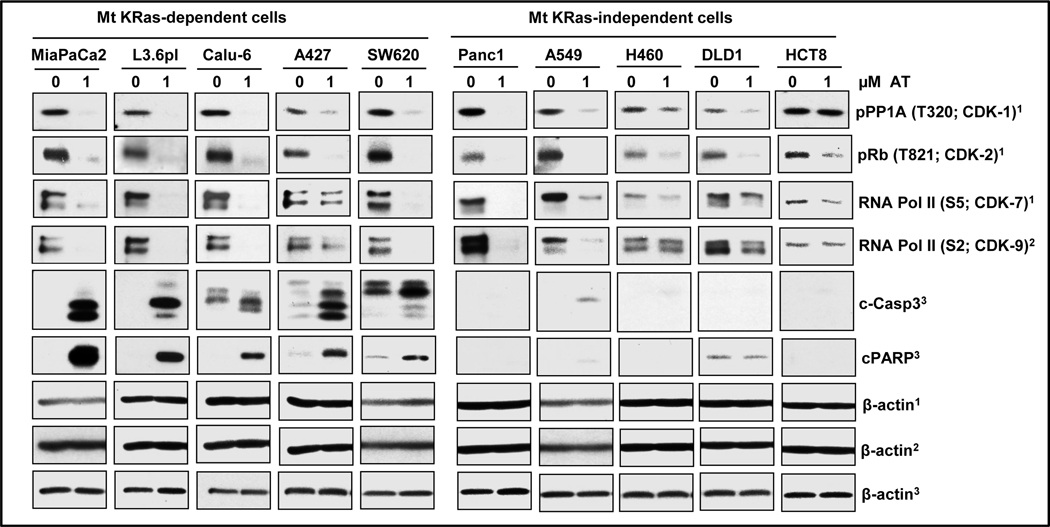
We next determined whether AT7519 inhibits the phosphorylation of the substrates of its targets (CDKs 1, 2, 7, and 9) and induces apoptosis. To this end, the 10 human cancer cell lines were treated with 1 μM AT7519 for 24 hours and processed for Western blotting as described in Methods. Figure 3 shows that AT7519 inhibited the phosphorylation of the substrates for CDK1 (PP1A; T320), CDK2 (Rb; T821), CDK7 (RNA-Pol II; S5), and CDK9 (RNA-Pol II; S2). Although AT7519 inhibited the phosphorylation of these substrates in all 10 cell lines (except for HCT8 cells where AT7519 inhibited CDKs 2, 7, and 9, but not CDK-1), AT7519 induced apoptosis (caspase-3 activation and PARP cleavage) only in MiaPaCa2, L3.6pl, SW620, A427, and Calu6 (mt KRas-dependent) but not in Panc1, A549, H460, DLD1, and HCT8 (mt KRas-independent) human cancer cells (Figure 3).
Figure 3: AT7519 induces apoptosis only in mt KRas-dependent human cancer cell lines.
Mt KRas-dependent (MiaPaCa2, L3.6pl, A427, SW620 and Calu6) and mt KRas-independent (A549, H460, Panc1, DLD1 and HCT8) human cancer cells were treated with AT7519 for 24 h, harvested and processed for Western blotting as described in the Methods. Shown are effects of AT7519 on the phosphorylation of the substrates for its targets CDK1 (PP1A; T320), CDK2 (Rb; T821), CDK7 (RNA-Pol II; S5) and CDK9 (RNA-Pol II; S2). AT7519 induced apoptosis (caspase-3 activation and PARP cleavage) only in MiaPaCa2, L3.6pl, SW620, A427 and Calu6 (mt KRas-dependent) but not in Panc1, A549, H460, DLD1 and HCT8 (mt KRas-independent) human cancer cells. Data are representative of 2 experiments.
CRISPR/Cas9-targeted knock out of CDK1, 2, 7 or 9 is as effective as KRas knock out in mt KRas-driven pancreatic cancer
Figures 1, 2, and 3 suggested that CDK suppression, and in particular AT7519 treatment, may be effective against mt KRas-dependent tumors, prompting us to search for human cancers that are driven by mt KRas and dependent on CDKs for survival. To this end, we first mined the available database of genome-wide CRISPR/Cas9 essentiality screening (https://depmap.org/ceres/) as described in the Methods, and found that among all cancer histopathologies, pancreatic cancer was the most dependent on KRas for survival followed by stomach, then colon and lung cancer (Figure 4a). We then mined the database for the dependence of 23 pancreatic cancer cell lines (all harboring mt KRas with nine G12D, seven G12V, four G12R, one G12C and two Q61H mutations) for each of the 41 CDKs and CDK-like kinases in the human genome. We found that the AT7519 targets, CDK1, CDK7, and CDK9, were the top 3 CDKs (with CDK2 as #5) and their CRISPR/Cas9-targeted knock out inhibited the viability of the 23 cell lines on average by 62%, 60%, and 52%, respectively (Figure 4b). This was similar to the 50% inhibition of viability after CRISPR/Cas9-targeted knock out of KRas (Figure 4b). In contrast, CRISPR/Cas9-targeted knock out of HRas or NRas only affected the viability of the 23 pancreatic cancer cell lines by an average of 11% and 0.5% (Figure 4b). To determine whether the dependency on CDKs 1, 2, 7, and 9 was universal among all the 23 pancreatic cancer cell lines, we mined the database and found that all 23 cell lines were similarly affected by CRISPR/Cas9-targeted individual knock out of CDK1, CDK2, CDK7, and CDK9, suggesting that these 4 CDKs play an important role in pancreatic cancer survival (Supplemental Figure 2).
Figure 4: knocking out CDKs 1, 2, 7 and 9 was as effective as knocking out KRas at inhibiting the viability of 23 human pancreatic cancer cell lines.
The effects of knocking out KRas, HRas, NRas, and 41 CDKs on the viability of human cancer cell lines, were determined by mining the BROAD institute genome-scale CRISPR-Cas9 essentiality screens across 342 cancer cell lines (dataset of Avana Ceres Gene Effect (BROAD institute, MIT; https://depmap.org/ceres/). Percentage of inhibition of cell viability was calculated as follows: % inhibition of viability = (1–2CRISPR Gene Score)*100. (a) Effects of knocking out KRas by CRISPR gRNA on cell viability of cancer cell lines from different human organs. (b) Effects of knocking out 41 CDKs, KRas, HRas and NRas by CRISPR gRNA on cell viability of 23 pancreatic cancer cell lines.
AT7519 is highly effective at suppressing the growth of patient-derived xenografts of mt KRas tumors from pancreatic cancer patients that were refractory to therapy
The observation that CRISPR/Cas9-targeted knock out of the AT7519 targets CDK1, CDK2, CDK7, and CDK9 has similar effects as KRas knock out on the viability of pancreatic cancer cell lines suggested that AT7519 could be effective at abrogating mt KRas-driven pancreatic cancer patient-derived xenografts (PDXs). To assess the antitumor efficacy of AT7519 in PDXs, we used fresh tumor biopsies from 5 pancreatic cancer patients, 3 PDACs with KRas G12D mutations (patient 1 [G148], patient 2 [G166], and patient 4 [G160]), one PASC with a KRas G12V mutation (patient 3 [G174]), and one PDAC with a G12R mutation (patient 5 [G210]). Freshly resected tumor biopsies were implanted subcutaneously in NSG mice that lack an intact immune system as previously described28 and when the tumor volumes reached ~200 mm3, the mice were randomized into vehicle or AT7519 (i.p. 15 mg/kg/day) groups for each the 5 PDXs (the number of mice in the vehicles for PDXs 1, 2, 3, 4 and 5 were 6, 7, 5, 10, and 4 mice, respectively. The number of mice in the AT7519-treated PDXs 1, 2, 3, 4 and 5 were 6, 6, 6, 10 and 5 mice, respectively). By day 24, PDXs from patients 1 and 2 in the vehicle-treated groups showed average growth of 401% and 433%, respectively (Figures 5a and 5b). PDXs from patient 3 in the vehicle-treated group grew much faster with an average growth of 802% by day 17 (Figure 5c). The experiment for this PDX had to be stopped by day 17 due to protocol specifications. The vehicle-treated group for patient 4’s PDXs also grew faster with an average growth of 791% by day 27 (Figure 5d). The vehicle-treated group for patient 5’s PDXs showed an average growth of 405% by day 21 (Figure 5e). AT7519 treatment suppressed tumor growth from average growth rates of 401% to 29% (PDX1), 433% to 32% (PDX2), 802% to 104% (PDX3), 791% to 205% (PDX4), and 405% to −8% (PDX5) (Figures 5a–e). Therefore, AT7915 inhibited tumor growth by 14-, 14-, 8-, and 4-fold, in patient PDXs 1, 2, 3, and 4, respectively. In the case of patient 5’s PDXs, AT7519 treatment actually caused tumor regression. Differences in tumor growth between vehicle- and AT7519-treated mice were statistically significant starting at days day 2 (PDX3, PDX5) or at day 3 (PDX1, PDX2, PDX4), as shown in Figures 5a–e.
Figure 5: AT7519 inhibits mt KRas xenografts from patients with refractory pancreatic cancer.
(a-e) Fresh tumor biopsies from 5 pancreatic cancer patients were implanted into NSG mice, and the mice were randomized when the average tumor volumes were 150–300 mm3, and treated daily with vehicle (V) or AT7519 (AT) (15 mg/kg/day) as described in Methods. (*P < 0.05; **P < 0.01; ***P < 0.001). P values determined by Student’s t-test. (f) An additional 6 mice from PDX 5 were treated with either vehicle (3 mice) or AT7519 (AT) for 2 hours and the tumors were harvested for western blotting as described in Methods.
AT7519 treatment blocks phosphorylation of CDK 1, 2, 7, and 9 substrates and induces apoptosis in PDXs in vivo
To determine whether AT7519 inhibited its target in vivo, we evaluated its effects on the phosphorylation of the different CDK substrates in patient-derived tumors. To this end, fresh tumor biopsies from patient 5 (G210) were implanted in NSG mice as described above. When the average tumor volumes reached about 300 mm3, the mice were randomized and treated either with vehicle (3 mice) or 15 mg/kg AT7519 (3 mice) as described in Methods. Two hours after treatment, tumors were harvested and lysates were processed for Western blotting as described in Methods. As shown in Figure 5f, AT7519 inhibited the phosphorylation of the substrates for CDK1 (PP1A; T320), CDK2 (NPM; T199), CDK7 (RNA Pol II; S5), and CDK 9 (RNA Pol II; S2), but did not inhibit the phosphorylation of Akt and Erk, suggesting that AT7519 selectively inhibited its targets in vivo. Furthermore, AT7519 also downregulated the anti-apoptotic protein Mcl-1 and induced apoptosis in vivo as measured by caspase-3 activation.
AT7519 suppresses the viability in 3D co-cultures of primary and metastatic mt KRas tumor cells derived from pancreatic cancer patients
We used eight low-passage (<20) human pancreatic cancer cell lines that we previously generated29,30 to evaluate the efficacy of AT7519 in standard 2D as well as 3D cell culture systems with and without human pancreatic stellate cells (HPSC). These 8 cell lines were derived from 6 primary and 2 metastatic mt KRas tumors (4 with G12D, 3 with G12V, and one with G13D KRas mutations)31. We confirmed that the 3D co-culture contained both the patient pancreatic cancer cells as well as the HPSCs by immunofluorescence staining with the cancer epithelial cell marker Cytokeratin-19 (CK-19) and Alpha-Smooth Muscle Actin (aSMA) antibodies, respectively (see Supplemental Figure 4). When the 8 patient-derived tumor cell lines were treated with AT7519 in 2D standard conditions, a dose-dependent inhibition of cell viability was observed with IC50 values ranging from 0.32 to 1.04 μM (Figures 6a and 6b). Importantly, AT7519 was just as effective when the patient-derived tumor cells were cultured in 3D conditions alone or when co-cultured with the chemoresistance-promoting human pancreatic stellate cells harvested from pancreatic adenocarcinomas (Figures 6a and 6b). There were no significant differences in the effectiveness of AT7519 in 2D, 3D or 3D + PSC. For example, for patient 107 cells, the IC50 values for AT7519 in 2 independent experiments were for 2D (0.46 and 0.76 uM), 3D (0.52 and 0.40 uM) and 3D + PSC (0.46 and 0.55 uM); for patient 102 cells, the IC50 values were for 2D (0.51 and 1.04 uM), 3D (0.37 and 1.06 uM) and 3D + PSC (0.39 and 0.97 uM); for patient 108 cells, the IC50 values were for 2D (0.80 and 1.02 uM), 3D (0.91 and 0.93 uM) and 3D + PSC (0.49 and 0.68 uM); for patient 69 cells, the IC50 values were for 2D (0.53 and 0.86 uM), 3D (0.87 and 0.47 uM) and 3D + PSC (0.66 and 0.80 uM). For patients 43, 53, 66 and 124 cells, the experiments were done once with the following IC50 values for 2D (0.91, 0.86, 0.36, 0.32 uM, respectively), for 3D (0.4, 0.41, 0.51, 0.34 uM, respectively) and for 3D + PSC (0.48, 0.75, 0.65, 0.48 uM, respectively).
Figure 6: AT7519 Inhibits the viability of primary and metastatic mt KRas cells derived from pancreatic cancer patients in 2D, 3D and 3D co-culture with pancreatic stellate cells (PSCs).
Cells were cultured for 2D, 3D, and 3D+PSC as described in Methods and were treated for 72 hours with AT7519. (a) Representative (patient 107) live-cell images obtained with the IncuCyte S3 at 72 hours. (b) Cell viability was determined using the CellTiter-Glo Assay; IC50 values (μM) for the 8 pancreatic cancer-derived cell lines treated for 72 hours with AT7519 are shown.
AT7519 suppresses the viability of 3D pancreatic tumor organoids from patients and mice that harbor KRas and p53 mutations.
Patient-derived organoids (PDOs) recapitulate more closely the tumor microenvironment, and hence provide an effective model for drug evaluation32,33. We therefore evaluated the efficacy of AT7519 to inhibit the viability of PDOs from 2 PDAC patients. To this end, the human pancreatic to lung metastatic tumor organoid, hM1a (KRasG12D, TP53R175H), and the human primary pancreatic tumor organoid hT3 (KRasQ61H)32,34 were grown in a 3D organoid culture system and treated with AT7519 for 7 days as described in Methods. As shown in Figure 7, AT7519 was highly effective at inhibiting the growth of hM1a and hT3 tumor organoids in a dose-dependent manner, with IC50 values of 0.35 and 0.26 μM, respectively. Next, we evaluated the effects of AT7519 on mouse pancreatic 3D organoids generated from various pancreatic cancer stages including pancreatic intraepithelial neoplasia (PanIN) and primary and metastatic tumors with KRas and p53 mutations. The mouse 3D organoids include PanIN mP2 (Kras+/LSL-G12DP53+/+); primary tumors mT1 (Kras+/LSL-G12DP53+/+), mT3 (Kras+/LSL-G12DP53+/R172H) and mT69a (Kras+/LSL-G12DP53R172H/R172H); and metastatic tumors mM1 (Kras+/LSL-G12DP53R172H/R172H) and mM2 (Kras+/LSL-G12DP53+/R172H). The organoids were treated with AT7519 at the indicated concentrations for 10 days. Supplemental Figure 3 shows that AT7519 inhibited the viability of all mouse organoids in a concentration-dependent manner. Furthermore, regardless of p53 status or stage of tumor progression, the potency of AT7519 was similar with IC50 values of 3.72 μM for the one PanIN, 3.82 μM, 5.28 μM, and 5.59 μM for the 3 primary tumors and 1.73 μM and 5.89 μM for the 2 metastatic tumors. Therefore, the CDK inhibitor AT7519 effectively inhibited the viability of both human and mouse pancreatic tumor organoids.
Figure 7. AT7519 Inhibits the viability of human primary (hT3) and metastatic (hM1a) organoids.
Human metastatic organoid hM1a and tumor organoid hT3 were treated with AT7519 at the indicated concentrations (1 well per concentration) for 7 days as descried in Methods. The images in (a) showed the whole well at 2x magnification and single organoid at 20x magnification upon AT7519 treatments. The CellTiter-Glo assays were performed after imaging to obtain the IC50 graphs in (b) for both organoids.
Discussion
The observation that not all tumors that harbor mt KRas are dependent on mt KRas22 offers an avenue to decipher the mechanism of KRas dependency, leading to a better understanding of how KRas drives cancer and hence to more efficacious therapies for patients whose tumors are addicted to KRas. In this study, we have taken systems biology and pharmacology approaches to address the KRas dependency conundrum. Global phosphoproteomics, genome-wide CRISPR/Cas9 viability screen database analysis, and FDA drug library screening revealed that CDKs 1, 2, 7, and 9 are required for the survival of mt KRas-dependent, but not mt KRas-independent human cancer cells. The CDK 1, 2, 7, and 9 inhibitor, AT7519, induced apoptosis in mt KRas-dependent but not mt KRas-independent human cancer cells. Consistent with this result, in pancreatic cancer, a disease known to be driven by mt KRas, gRNA knocking out CDK1, CDK2, CDK7, or CDK9 was as effective as gRNA knock out of KRas at inhibiting the viability of 23 human pancreatic cancer cell lines.
An important finding of our studies is that AT7519 abrogated pancreatic tumors in several highly relevant pancreatic cancer models including mouse PDXs from 5 patients, 3D primary and metastatic organoids from 2 patients, and 3D co-cultures of PSCs with patient-derived cells from 8 patients. Furthermore, the 3D co-cultures, PDXs and PDOs were derived from pancreatic cancer patients, the majority of whom relapsed while on conventional chemotherapy (5-fluorouracil, gemcitabine and/or capecitabine) and/or radiation therapy, suggesting that AT7519 may be effective against tumors where conventional therapies are not. Another key finding is the effectiveness of AT7519 to abrogate pancreatic tumors that harbor a broad spectrum of KRas mutations including G12D, G12V, and G12R (PDXs), G12D and Q61H (organoids); G12D, G12V and G13D (3D co-cultures) and G12D, G12V, G12C, and Q61K (cell lines). This is significant as the CDK inhibitor AT7519 provides a potential treatment for the unmet therapeutic need for patients with pancreatic cancer whose tumors present with a variety of KRas mutations. To date only KRas inhibitors that are selective for tumors that harbor the KRas G12C mutation have reached clinical trials16,17. Finally, AT7519 was equally effective at thwarting PanIN, primary and metastatic tumors in mouse 3D organoids derived from KPC (KRas+/LSL-G12DP53+/+, KRas+/LSL-G12DP53+/R172H and KRas+/LSL-G12DP53R172H/R172H) mice, suggesting AT7519 has broad therapeutic efficacy across all stages of pancreatic cancer progression. Although the efficacy of AT7519 is impressive, it is important to note that resistance to targeted agents has been observed in experimental models, and that resistance to AT7519 treatment over time is not presently known.
CDKs have been studied in many cancers but to a lesser degree in pancreatic cancer, and clinical trials with CDK inhibitors in pancreatic cancer patients have been rare. For example, although loss of the CDK4/6 inhibitor p16INK4a is common in KRas-driven PDAC35, p16INK4A-deficient PDAC where CDK4/6 are hyperactivated were shown to be resistant to CDK4/6 inhibitors36,37, such as palbociclib38, ribociclib39, and abemaciclib40, that have been FDA-approved for breast cancer. Furthermore, CDK9 overexpression in human pancreatic tumor tissue is associated with poor patient survival41, and preclinically CDK9 inhibition resulted in growth inhibition of mt KRas PDAC PDXs42, yet the CDK9 inhibitor SNS-032 is undergoing evaluation in clinical trials but not in pancreatic cancer43–45. Our results warrant investigating the CDK inhibitor AT7519 in pancreatic cancer patients as this agent induced tumor regression in PDAC PDXs from patients with refractory disease and inhibited the viability of 3D organoids from patients with primary and metastatic pancreatic cancer.
The contributions of CDKs to KRas dependency have not been explored. Although Costa-Cabral et al46 determined the effects of CDK1 depletion on 20 colon cancer cell lines, 10 with wt KRas and the other 10 with mt KRas, this study did not investigate the effects of CDK1 depletion on mt KRas dependency among mt KRas-harboring cancer cells that are either mt KRas-dependent or mt KRas-independent. Their results show that overall there is a correlation between KRas mutation status and sensitivity to CDK1 depletion. However, the most sensitive cell line to CDK1 depletion was a wt KRas cell line (RKO) and the second least sensitive was a mt KRas cell line (Lovo)46. In our studies, although AT7519 inhibited CDK1 activity, it did not induce apoptosis in the mt KRas-independent A549, H460, DLD1, and Panc1 human cancer cells, suggesting that in these mt KRas-harboring cells, CDK1 was dispensable. In contrast, in mt KRas-dependent MiaPaCa2, L3.6pl, SW620, Calu6 and A427 human cancer cells, AT7519 inhibited CDK1 and induced apoptosis.
The AT7519 in vivo effects on PDX signal transduction pathways and apoptosis are significant as they showed that 2 hours after mice treatment, AT7519 was able to engage its CDK targets and inhibit the phosphorylation of PP1A (T320) by CDK-1, NPM (T199) by CDK2, RNA Pol II (S5) by CDK7 and RNA Pol II (S2) by CDK9. These effects were highly selective in that AT7519 had no effects on the phosphorylation levels of Akt and Erk. Consistent with this, gRNA knock out of Akt1, 2 or 3, Mek1 or 2 and Erk1 or 2 had little effects on the viability of 23 human cancer cell lines (https://depmap.org/ceres/; data not shown). Furthermore, AT7519 treatment of mice also suppressed the levels of the anti-apoptotic protein Mcl-1 in the PDX tumors, and this was paralleled by activation of caspase 3. This result is consistent with the AT7519 inhibition of CDK9, a regulator of RNA Pol II-mediated transcription elongation through phosphorylation of S2 on RNAPol II27,47, the inhibition of which is known to decrease the transcription of Mcl-148. In addition, AT7519 also inhibited CDK7, a regulator of RNA Pol II transcription initiation (through S5 phosphorylation)49, which precedes CDK9-mediated elongation27,47. Taken together, the results suggest that one mechanism by which AT7519 induces apoptosis is by inhibiting CDK7 and CDK9, which leads to decreased Mcl-1 transcription, shifting the ratio of anti-apoptotic proteins relative to pro-apoptotic proteins in favor of apoptosis induction.
Our findings are highly significant as they revealed a new avenue to combat PDAC, a cancer with very poor prognosis due mainly to its resistance to conventional therapies. While AT7519 has been investigated in 5 clinical trials, none targeted pancreatic cancer. For example, AT7519 was investigated as a single agent in 2 phase I trials, one in patients with refractory solid tumors50, and the other with refractory solid tumors and non-Hodgkin’s lymphoma51, as well as one phase II trial in relapsed or refractory chronic lymphocytic leukemia (CLL) and mantle cell lymphoma (MCL)52. AT7519 was also investigated in combinations with the proteasome inhibitor bortezomib in a multiple myeloma phase I/II trial53, and with the heat shock protein-90 inhibitor onalespib (AT13387) in a phase I trial in advanced solid tumors54. In these trials, the majority of clinical activity observed was stable disease with few partial responses. One possible reason for this low clinical activity may be the patients tested with AT7519 did not include patients whose tumors are more likely to respond to AT7519. The data presented in this manuscript suggest that patients with mt KRas-driven tumors are more likely to respond to AT7519 and thus, warrant investigating AT7519 in pancreatic cancer, particularly PDAC. Furthermore, our finding that patient-derived xenografts and organoids from patients with PDAC who relapsed after chemo and radiation therapy, coupled with the ability of AT7519 to abrogate primary and metastatic PDAC (with both KRas and p53 mutations) in highly relevant pancreatic cancer models, suggest that AT7519 may be effective in patients with highly aggressive PDAC tumors. The selectivity of AT7519 for mt KRas human cancer cells over “normal” cells, coupled with its lack of toxicity in mice at doses that caused PDAC tumor growth suppression and regression suggests a favorable therapeutic index in patients with PDAC. Finally, the finding that AT7519 was selective for mt KRas-dependent human cancer across pancreatic, lung, and colon lineages suggests that, in addition to PDAC, AT7519 may also have significant clinical activity in patients with mt KRas CRC and NSCLC.
Supplementary Material
Statement of Translational Relevance:
Although mutant KRas drives oncogenesis and drug resistance, there are no FDA-approved drugs that directly target mutant KRas. Here, we discovered that KRas addiction depends on CDK hyperactivation and identified a drug to target this vulnerability and demonstrated its therapeutic efficacy in xenografts and organoids from 15 pancreatic cancer patients.
Acknowledgement
This work was funded in part by NIH grant R35 CA197731 (Said Sebti, PhD), NIH grant R01 CA242003 (Jose Trevino, MD), and Joseph & Ann Matella Fund for Pancreatic Cancer Research at the University of Florida, and was supported in part by the Proteomics & Metabolomics Core and the Biostatistics and Bioinformatics Core at the H. Lee Moffitt Cancer Center & Research Institute; an NCI-designated Comprehensive Cancer Center (P30 CA076292). We thank these cores for their outstanding assistance and expertise. We would also like to thank Dr. David Tuveson (Cold Spring Harbor Laboratory) for providing us with the human and mouse organoids, and Dr. Uwe Rix (Moffitt Drug Discovery Department and Moffitt Lung Cancer Center of Excellence) for providing the FDA drug library. We also thank Heidi Sankala for editorial assistance.
Footnotes
Conflict of interest disclosure statement: The authors disclose no conflict of interest.
References
- 1.Barbacid M. Ras genes. Annu Rev Biochem 56, 779–827 (1987). [DOI] [PubMed] [Google Scholar]
- 2.Simanshu DK, Nissley DV & McCormick F. RAS Proteins and Their Regulators in Human Disease. Cell 170, 17–33 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bos JL, Rehmann H. & Wittinghofer A. GEFs and GAPs: critical elements in the control of small G proteins. Cell 129, 865–877 (2007). [DOI] [PubMed] [Google Scholar]
- 4.Hanahan D. & Weinberg RA Hallmarks of cancer: the next generation. Cell 144, 646–674 (2011). [DOI] [PubMed] [Google Scholar]
- 5.Li S, Balmain A. & Counter CM A model for RAS mutation patterns in cancers: finding the sweet spot. Nat Rev Cancer 18, 767–777 (2018). [DOI] [PubMed] [Google Scholar]
- 6.Cox AD, Fesik SW, Kimmelman AC, Luo J. & Der CJ Drugging the undruggable RAS: Mission possible? Nat Rev Drug Discov 13, 828–851 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Slebos RJ, et al. K-ras oncogene activation as a prognostic marker in adenocarcinoma of the lung. N Engl J Med 323, 561–565 (1990). [DOI] [PubMed] [Google Scholar]
- 8.Chetty R. & Govender D. Gene of the month: KRAS. J Clin Pathol 66, 548–550 (2013). [DOI] [PubMed] [Google Scholar]
- 9.Pao W, et al. KRAS mutations and primary resistance of lung adenocarcinomas to gefitinib or erlotinib. PLoS Med 2, e17 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lievre A, et al. KRAS mutation status is predictive of response to cetuximab therapy in colorectal cancer. Cancer Res 66, 3992–3995 (2006). [DOI] [PubMed] [Google Scholar]
- 11.Jones RP, et al. Specific mutations in KRAS codon 12 are associated with worse overall survival in patients with advanced and recurrent colorectal cancer. Br J Cancer 116, 923–929 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dempke WC & Heinemann V. Ras mutational status is a biomarker for resistance to EGFR inhibitors in colorectal carcinoma. Anticancer Res 30, 4673–4677 (2010). [PubMed] [Google Scholar]
- 13.Moore AR, Rosenberg SC, McCormick F. & Malek S. RAS-targeted therapies: is the undruggable drugged? Nat Rev Drug Discov (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stalnecker CA & Der CJ RAS, wanted dead or alive: Advances in targeting RAS mutant cancers. Sci Signal 13(2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ostrem JM, Peters U, Sos ML, Wells JA & Shokat KM K-Ras(G12C) inhibitors allosterically control GTP affinity and effector interactions. Nature 503, 548–551 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Canon J, et al. The clinical KRAS(G12C) inhibitor AMG 510 drives anti-tumour immunity. Nature 575, 217–223 (2019). [DOI] [PubMed] [Google Scholar]
- 17.Hallin J, et al. The KRAS(G12C) inhibitor MRTX849 provides insight toward therapeutic susceptibility of KRAS-mutant cancers in mouse models and patients. Cancer Discovery 10, 54–71 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. https://clinicaltrials.gov/ct2/show/NCT04006301.
- 19.Ryan MB, et al. Vertical Pathway Inhibition Overcomes Adaptive Feedback Resistance to KRAS(G12C) Inhibition. Clin Cancer Res 26, 1633–1643 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lou K, et al. KRAS(G12C) inhibition produces a driver-limited state revealing collateral dependencies. Sci Signal 12(2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Downward J. RAS synthetic lethal screens revisited: Still seeking the elusive prize? Clin Cancer Res 21, 1802–1809 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aguirre AJ & Hahn WC Synthetic lethal vulnerabilities in KRAS-mutant cancers. Cold Spring Harb Perspect Med 8(2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kazi A, et al. GSK3 suppression upregulates beta-catenin and c-Myc to abrogate KRas-dependent tumors. Nat Commun 9, 5154 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fleming JB, Shen GL, Holloway SE, Davis M. & Brekken RA Molecular consequences of silencing mutant K-ras in pancreatic cancer cells: justification for K-ras-directed therapy. Mol Cancer Res 3, 413–423 (2005). [DOI] [PubMed] [Google Scholar]
- 25.Singh A, et al. A gene expression signature associated with “K-Ras addiction” reveals regulators of EMT and tumor cell survival. Cancer Cell 15, 489–500 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wyatt PG, et al. Identification of N-(4-piperidinyl)-4-(2,6-dichlorobenzoylamino)-1H-pyrazole-3-carboxamide (AT7519), a novel cyclin dependent kinase inhibitor using fragment-based X-ray crystallography and structure based drug design. J Med Chem 51, 4986–4999 (2008). [DOI] [PubMed] [Google Scholar]
- 27.Squires MS, et al. Biological characterization of AT7519, a small-molecule inhibitor of cyclin-dependent kinases, in human tumor cell lines. Mol Cancer Ther 8, 324–332 (2009). [DOI] [PubMed] [Google Scholar]
- 28.Delitto D, et al. Patient-derived xenograft models for pancreatic adenocarcinoma demonstrate retention of tumor morphology through incorporation of murine stromal elements. Am J Pathol 185, 1297–1303 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kang Y, et al. Two-dimensional culture of human pancreatic adenocarcinoma cells results in an irreversible transition from epithelial to mesenchymal phenotype. Lab Invest 95, 207–222 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim MP, et al. Generation of orthotopic and heterotopic human pancreatic cancer xenografts in immunodeficient mice. Nat Protoc 4, 1670–1680 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Koay EJ, et al. A visually apparent and quantifiable CT Imaging feature identifies biophysical Subtypes of pancreatic ductal adenocarcinoma. Clin Cancer Res 24, 5883–5894 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boj SF, et al. Organoid models of human and mouse ductal pancreatic cancer. Cell 160, 324–338 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wolff RA, et al. Dynamic changes during the treatment of pancreatic cancer. Oncotarget 9, 14764–14790 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tiriac H, et al. Organoid profiling identifies common responders to chemotherapy in pancreatic Cancer. Cancer Discovery 8, 1112–1129 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hruban RH, Wilentz RE & Kern SE Genetic progression in the pancreatic ducts. Am J Pathol 156, 1821–1825 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Heilmann AM, et al. CDK4/6 and IGF1 receptor inhibitors synergize to suppress the growth of p16INK4A-deficient pancreatic cancers. Cancer Res 74, 3947–3958 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Asghar U, Witkiewicz AK, Turner NC & Knudsen ES The history and future of targeting cyclin-dependent kinases in cancer therapy. Nat Rev Drug Discov 14, 130–146 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fry DW, et al. Specific inhibition of cyclin-dependent kinase 4/6 by PD 0332991 and associated antitumor activity in human tumor xenografts. Mol Cancer Ther 3, 1427–1438 (2004). [PubMed] [Google Scholar]
- 39.Rader J, et al. Dual CDK4/CDK6 inhibition induces cell-cycle arrest and senescence in neuroblastoma. Clin Cancer Res 19, 6173–6182 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gelbert LM, et al. Preclinical characterization of the CDK4/6 inhibitor LY2835219: in-vivo cell cycle-dependent/independent anti-tumor activities alone/in combination with gemcitabine. Invest New Drugs 32, 825–837 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kretz AL, et al. CDK9 is a prognostic marker and therapeutic target in pancreatic cancer. Tumour Biol 39, 1010428317694304 (2017). [DOI] [PubMed] [Google Scholar]
- 42.Allaway RJ, et al. Genomic characterization of patient-derived xenograft models established from fine needle aspirate biopsies of a primary pancreatic ductal adenocarcinoma and from patient-matched metastatic sites. Oncotarget 7, 17087–17102 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Conroy A, et al. SNS-032 is a potent and selective CDK 2, 7 and 9 inhibitor that drives target modulation in patient samples. Cancer Chemother Pharmacol 64, 723–732 (2009). [DOI] [PubMed] [Google Scholar]
- 44.Heath EI, Bible K, Martell RE, Adelman DC & Lorusso PM A phase 1 study of SNS-032 (formerly BMS-387032), a potent inhibitor of cyclin-dependent kinases 2, 7 and 9 administered as a single oral dose and weekly infusion in patients with metastatic refractory solid tumors. Invest New Drugs 26, 59–65 (2008). [DOI] [PubMed] [Google Scholar]
- 45.Tong WG, et al. Phase I and pharmacologic study of SNS-032, a potent and selective Cdk2, 7, and 9 inhibitor, in patients with advanced chronic lymphocytic leukemia and multiple myeloma. J Clin Oncol 28, 3015–3022 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Costa-Cabral S, et al. CDK1 is a synthetic lethal target for KRAS mutant tumours. PLoS One 11, e0149099 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang S. & Fischer PM Cyclin-dependent kinase 9: a key transcriptional regulator and potential drug target in oncology, virology and cardiology. Trends Pharmacol Sci 29, 302–313 (2008). [DOI] [PubMed] [Google Scholar]
- 48.Tibes R. & Bogenberger JM Transcriptional silencing of MCL-1 through cyclin-dependent kinase inhibition in acute myeloid leukemia. Front Oncol 9, 1205 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fisher RP Secrets of a double agent: CDK7 in cell-cycle control and transcription. J Cell Sci 118, 5171–5180 (2005). [DOI] [PubMed] [Google Scholar]
- 50.Mahadevan D, et al. A phase I pharmacokinetic and pharmacodynamic study of AT7519, a cyclin-dependent kinase inhibitor in patients with refractory solid tumors. Ann Oncol 22, 2137–2143 (2011). [DOI] [PubMed] [Google Scholar]
- 51.Chen EX, et al. A Phase I study of cyclin-dependent kinase inhibitor, AT7519, in patients with advanced cancer: NCIC Clinical Trials Group IND 177. Br J Cancer 111, 2262–2267 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Seftel MD, et al. The CDK inhibitor AT7519M in patients with relapsed or refractory chronic lymphocytic leukemia (CLL) and mantle cell lymphoma. A Phase II study of the Canadian Cancer Trials Group. Leuk Lymphoma 58, 1358–1365 (2017). [DOI] [PubMed] [Google Scholar]
- 53.Raje N, et al. A Phase I/II open-label multicenter study of the cyclin kinase inhibitor AT7519M alone and in combination with bortezomib In patients with previously treated multiple myeloma. Blood 122, 1976–1976 (2013). [Google Scholar]
- 54.Do KT, et al. Phase I trial of the combination of the heat shock protein-90 inhibitor onalespib (AT13387) and the cyclin-dependent kinase inhibitor AT7519M in patients with advanced solid tumors. J Clin Oncol 37, 2619–2619 (2019). [Google Scholar]
- 55.Cox J. & Mann M. MaxQuant enables high peptide identification rates, individualized p.p.b.-range mass accuracies and proteome-wide protein quantification. Nat Biotechnol 26, 1367–1372 (2008). [DOI] [PubMed] [Google Scholar]
- 56.Welsh EA, Eschrich SA, Berglund AE & Fenstermacher DA Iterative rank-order normalization of gene expression microarray data. BMC Bioinformatics 14, 153 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Horn H, et al. KinomeXplorer: an integrated platform for kinome biology studies. Nat Methods 11, 603–604 (2014). [DOI] [PubMed] [Google Scholar]
- 58.Huch M, et al. Unlimited in vitro expansion of adult bi-potent pancreas progenitors through the Lgr5/R-spondin axis. EMBO J 32, 2708–2721 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.