Abstract
A 6-month-old, previously healthy boy presented with poor feeding and vomiting for 2 weeks. At presentation, his left supraorbital vein was found to engorge considerably. A cranial computed tomography (CT) scan revealed a large cyst in the posterior fossa with a prominent left superior ophthalmic vein (SOV). Magnetic resonance imaging delineated the well-demarcated cyst markedly compressing the right cerebellar hemisphere. The patient underwent microscopic fenestration of the cyst wall through lateral suboccipital craniotomy. The cyst wall, comprising multi-layered, opacified membranes, was extensively resected and communicated with the prepontine cistern. The histological appearance of the cyst wall was consistent with an arachnoid cyst. Engorgement of the left supraorbital vein resolved immediately after surgery. A postoperative CT scan did not identify the SOV in the left orbit. In the present case, engorgement of the supraorbital vein might reflect the increased venous pressure of the SOV caused by compression of the contralateral cerebellar hemisphere.
Keywords: Arachnoid cyst, Hydrocephalus, Infant, Posterior fossa, Supraorbital vein
Introduction
Arachnoid cysts (ACs) are commonly known as a benign entity arising in the intracranial and intraspinal cavities, containing cerebrospinal fluid-like clear fluid and lined by arachnoid membranes. They are thought to be mostly congenital in origin and prevalent in up to 2.6% of the pediatric population. The most frequent intracranial location is the middle cranial fossa, followed by the posterior fossa and interhemispheric fissure. Typical clinical presentations are symptoms of increased intracranial pressure, while most ACs have been estimated to be asymptomatic and with stable volume. Currently, fenestration through craniotomy is the most commonly adopted first-line treatment [1], [2], [3], [4], [5], [6]. The superior ophthalmic vein (SOV) is the largest venous channel in the orbit connecting the cavernous sinus and angular and supraorbital veins [7]. The SOV can enlarge in the Dural arteriovenous fistula in the cavernous and para cavernous regions and increases intracranial pressure [8], [9], [10]. However, to the best of our knowledge, the supraorbital vein has rarely been reported in association with pathognomonic signs [11]. Here, we present an infantile case of posterior fossa AC presenting with considerable engorgement of the contralateral supraorbital vein.
Case report
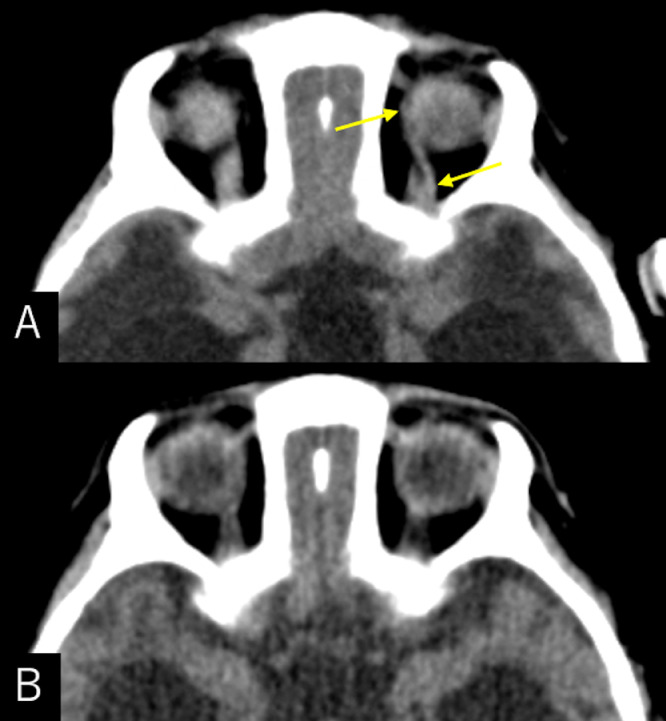
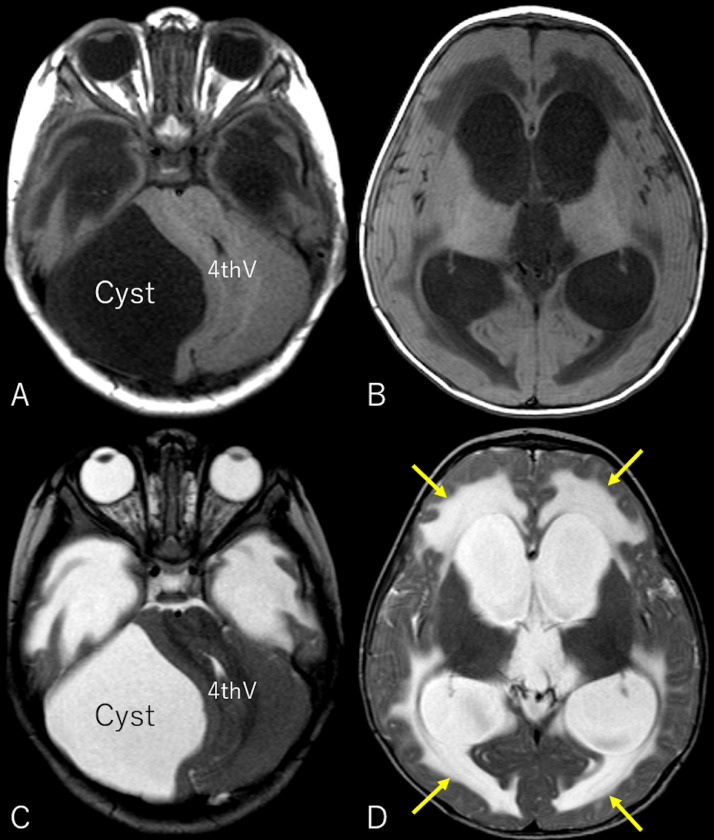
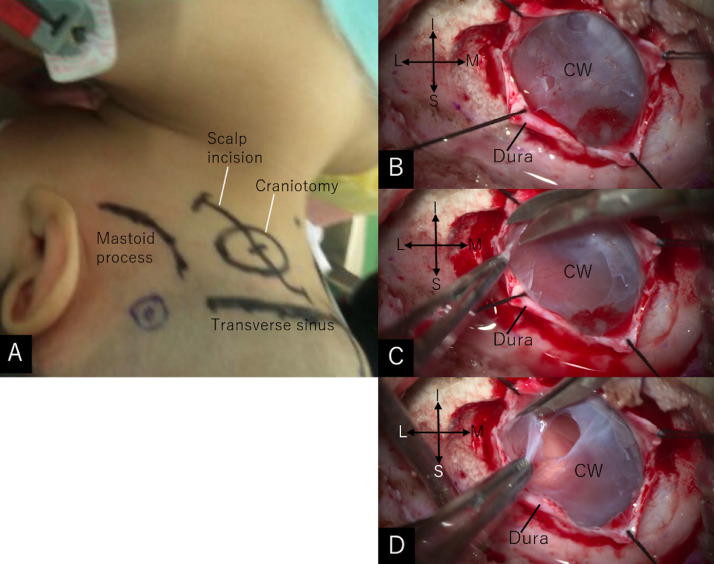
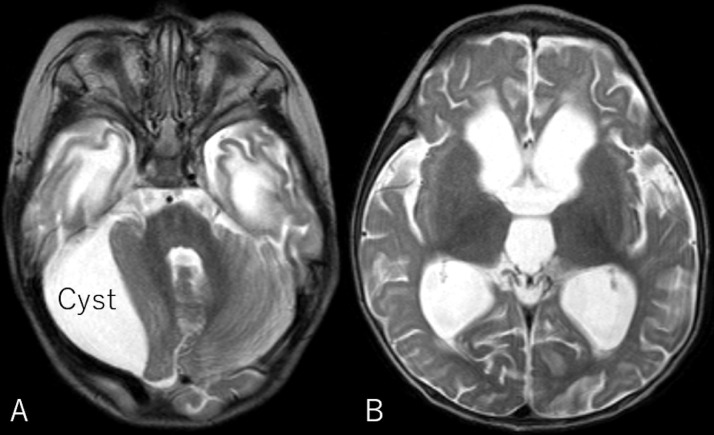
A 6-month-old, previously healthy boy presented with poor feeding and vomiting for 2 weeks. A cranial computed tomography (CT) scan taken at a local hospital revealed a large cyst in the posterior fossa and the patient was referred to our department. At presentation, the patient was lively but irritable. The head circumference of the boy was 48.2 cm, larger than +2 standard deviation (SD) with a tense anterior fontanelle, while the body weight and height were 7.9 kg (+0.75SD) and 70 cm (-0.08SD), respectively. The left supraorbital vein was found to engorge considerably (Fig. 1A). A CT scan revealed a prominent left superior ophthalmic vein, compared to that on the right side (Fig. 2A). Magnetic resonance imaging (MRI) revealed a well-demarcated cyst. It was 58 mm × 65 mm × 51 mm in maximal dimension, hypointense on T1- and hyperintense on T2-weighted imaging, respectively, and markedly compressed the right cerebellar hemisphere with periventricular hyperintensity and displacement of the fourth ventricle (Fig. 3). The patient underwent microscopic fenestration of the cyst wall, in the prone position, through a lateral suboccipital craniotomy 2 cm in dimension. It could be performed comfortably without placement of an external ventricular drain followed by release of the obstructive hydrocephalus for reopening of the aqueduct. The cyst contained pressurized clear fluid and was lined with multilayered, opacified membranes. The wall was extensively resected in the suboccipital and petrous surfaces and communicated with the prepontine cistern (Fig. 4). The histological appearance of the cyst wall was consistent with that of an arachnoid cyst. Engorgement of the left supraorbital vein resolved immediately after surgery (Fig. 1B). MRI performed 11 days after surgery showed a remarkable regression of the cyst and resolution of ventriculomegaly with periventricular hyperintensity (Fig. 5). CT scan performed at that time did not detect the superior ophthalmic vein in the left orbit (Fig. 2B).
Fig. 1.
(A) Patient's photo at the presentation showing a considerable engorgement of the left supraorbital vein (arrows). (B) Patient's photo immediately after surgery showing resolution of the venous engorgement
Fig. 2.
(A) Axial computed tomography at the presentation showing the prominent left superior ophthalmic vein (arrows), compared to that on the right. (B) Axial computed tomography performed 12 days after surgery showing the superior ophthalmic vein unidentifiable in the left orbit
Fig. 3.
Axial T1- (A, B) and T2-weighted (C, D) magnetic resonance images showing a well-demarcated cyst, 58 mm × 65 mm × 51 mm in maximal dimension, appearing hypointense on T1- and hyperintense on T2-weighted imaging, respectively, and markedly compressing the right cerebellar hemisphere, with considerable displacement of the fourth ventricle (4th V) and periventricular hyperintensity (D,arrows)
Fig. 4.
(A) Intraoperative photo, viewed from the caudal, right lateral aspect, showing the scalp incision and craniotomy line. (B-D) Intraoperative microscopic views showing the outer appearance of the cyst (B); cyst wall comprised by multi-layered, opacified membranes (C); and resection maneuver of the cyst wall (D). CW: cyst wall; I: inferior; L: lateral; M: medial; S: superior
Fig. 5.
(A, B) Axial T2-weighted magnetic resonance imaging performed 11 days after surgery showing a remarkable regression of the cyst and ventriculomegaly with resolution of periventricular hyperintensity
Discussion
In the present patient, the left supraorbital vein was observed to engorge considerably with prominent visualization of the ipsilateral SOV that was identified on the CT scan. Furthermore, the right cerebellar hemisphere was markedly compressed by the cyst. The engorgement of the left supraorbital vein resolved immediately after surgery, with undetected SOV on neuroimages. Therefore, we assumed that engorgement of the supraorbital vein might reflect the increased venous flow of the SOV that was caused by marked cerebellar compression of the cyst. In general, the veins of the posterior fossa can be divided into 4 groups: superficial, deep, brainstem, and bridging veins. The superficial veins are further divided based on which of the 3 cortical surfaces they drain: the tentorial, suboccipital, and petrous surfaces [12]. Given that these drainage routes could be severely interrupted on the right by cerebellar compression, it is probable that the venous flow in the left petrosal vein might have markedly increased. This could result in an increased pressure of the contralateral left cavernous sinus and SOV, which yielded engorgement of the connecting supraorbital vein. In addition, the parasellar venous structures of infants that have different topographical relationships from those of adults might influence the unusual engorgement of the supraorbital vein [13].
Most intracranial ACs are thought to be congenital in origin, asymptomatic, and stable in volume, while a fraction of them becomes symptomatic [2,4,5]. The present patient became symptomatic at the age of 6 months following uneventful growth. The reason is elusive. Further investigations are required to understand the biological behavior of ACs.
For pediatric patients with ACs, fenestration through craniotomy is the most frequently adopted first-line treatment [1,3,5]. In the present case, microscopic fenestration through a small craniotomy was chosen to provide satisfactory intraoperative views and release of cyst compression and obstructive hydrocephalus. Given that a small-sized patient, less invasive, endoscopic fenestration seems to be an alternative or adjunctive option. An endoscopic surgery was assumed to be the second-line treatment for the present patient when microscopic fenestration failed. An unusual but distinct external finding, such as engorgement of the supraorbital vein, can preface the recognition of the underlying pathophysiology that lead to an effective treatment.
Engorgement of the supraorbital vein may reflect the increased venous pressure of the SOV caused by compressing the contralateral cerebellar hemisphere.
Author contributions
All the authors contributed equally to the study.
Ethical standards
We declare that the present study has been approved by the institution's guidelines for human research and performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Footnotes
Acknowledgements: None.
Competing Interest: The authors have no conflict of interest to declare regarding the materials or methods in this study or the findings presented in this paper.
Patient Consent: We declare that the patient described in this study gave informed consent prior to inclusion in this study.
References
- 1.Chen JL, Tan ALJ, Ng LP, Low DCY, Tew SW, Low SYY. Paediatric arachnoid cysts: surgical outcomes from a Singapore children's hospital. J Clin Neurosci. 2021;85(3):122–131. doi: 10.1016/j.jocn.2020.12.030. [DOI] [PubMed] [Google Scholar]
- 2.Erdinçler P, Kaynar MY, Bozkus H, Ciplak N. Posterior fossa arachnoid cysts. Br J Neurosurg. 1999;13(1):10–17. doi: 10.1080/02688699944122. [DOI] [PubMed] [Google Scholar]
- 3.Fewel ME, Levy ML, McComb JG. Surgical treatment of 95 children with 102 intracranial arachnoid cysts. Pediatr Neurosurg. 1996;25(4):165–173. doi: 10.1159/000121119. [DOI] [PubMed] [Google Scholar]
- 4.Huang JH, Mei WZ, Chen Y, Chen JW, Lin ZX. Analysis on clinical characteristics of intracranial arachnoid cysts in 488 pediatric cases. Int J Clin Exp Med. 2015;8(10):18343–18350. [PMC free article] [PubMed] [Google Scholar]
- 5.Kirkpatrick M, Engleman H, Minns RA. Symptoms and signs of progressive hydrocephalus. Arch Dis Child. 1989;64(1):124–128. doi: 10.1136/adc.64.1.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marin-Sanabria EA, Yamamoto H, Nagashima T, Kohmura E. Evaluation of the management of arachnoid cyst of the posterior fossa in pediatric population: experience over 27 years. Childs Nerv Syst. 2007;23(5):535–542. doi: 10.1007/s00381-006-0284-3. [DOI] [PubMed] [Google Scholar]
- 7.Reis CV, Gonzalez FL, Zabramski JM, Hassan A, Deshmukh P, Albuquerque FC. Anatomy of the superior ophthalmic vein approach for direct endovascular access to vascular lesions of the orbit and cavernous sinus. Neurosurgery. 2009;64(5 Suppl 2):318–323. doi: 10.1227/01.NEU.0000340781.34122.A2. [DOI] [PubMed] [Google Scholar]
- 8.Khanna RK, Pham CJ, Malik GM, Spickler EM, Mehta B, Rosenblum ML. Bilateral superior ophthalmic vein enlargement associated with diffuse cerebral swelling. Report of 11 cases. J Neurosurg. 1997;86(5):893–897. doi: 10.3171/jns.1997.86.5.0893. [DOI] [PubMed] [Google Scholar]
- 9.Kim MJ, Shin YS, Ihn YK, Kim BM, Yoon PH, Oh SY. Transvenous embolization of cavernous and paracavernous dural arteriovenous fistula through the facial vein: report of 12 cases. Neurointervention. 2013;8(1):15–22. doi: 10.5469/neuroint.2013.8.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lirng JF, Fuh JL, Wu ZA, Lu SR, Wang SJ. Diameter of the superior ophthalmic vein in relation to intracranial pressure. AJNR Am J Neuroradiol. 2003;24(4):700–703. [PMC free article] [PubMed] [Google Scholar]
- 11.Han W, Kim JH, Kang HI, Kim DR, Moon BG, Kim JS. Transvenous embolization of dural carotid cavernous fistula through the supraorbital vein. J Cerebrovasc Endovasc Neurosurg. 2019;21(2):101–106. doi: 10.7461/jcen.2019.21.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matsushima T, Rhoton AL, Jr, de Oliveira E, Peace D. Microsurgical anatomy of the veins of the posterior fossa. J Neurosurg. 1983;59(1):63–105. doi: 10.3171/jns.1983.59.1.0063. [DOI] [PubMed] [Google Scholar]
- 13.Weninger WJ, Müller GB. The parasellar region of human infants: cavernous sinus topography and surgical approaches. J Neurosurg. 1999;90(3):484–490. doi: 10.3171/jns.1999.90.3.0484. [DOI] [PubMed] [Google Scholar]