Abstract
Superficial myofibroblastoma is a rare benign mesenchymal tumor which predominantly occurs in the female lower genital tract. Here we present a case of a 42-year-old female patient with prolonged vaginal bleeding. Radiological imaging revealed a well circumscribed mass in the vagina with a stalk. The patient underwent surgery and the tumor was histologically diagnosed as superficial myofibroblastoma. Notably, this is the first report of the radiological imaging of a superficial myofibroblastoma harboring a stalk arising from the vaginal wall. We compared the radiological images with histological findings and discuss major differential diagnosis of vaginal tumors. Despite the challenging nature of preoperative diagnosis of mesenchymal vaginal tumors, radiological features may aid in differentiating them from other more aggressive entities or malignant tumors.
Keywords: Superficial myofibroblastoma, Vaginal tumor, Vaginal mass
Introduction
Superficial myofibroblastoma of the lower female genital tract is a rare benign tumor, which is categorized as a genital stromal tumor [1], [2], [3]. To our knowledge, only 2 case reports within the English literature of have reported radiological image features [4,5]. Here we present a case of a superficial myofibroblastoma in the vagina with a stalk with their radiological findings. We then compared these images to their histological features.
Case report
A 42-year-old woman was referred to our hospital (Asahikawa Medical University, Asahikawa, Japan) with abnormal vaginal bleeding for 3 months. She had a history of one normal vaginal delivery and one artificial abortion of pregnancy. She was not on any current medication and had no history of tamoxifen or hormonal therapy.
Physical examination found a tender mass with a smooth surface on the anterior wall of the vagina.
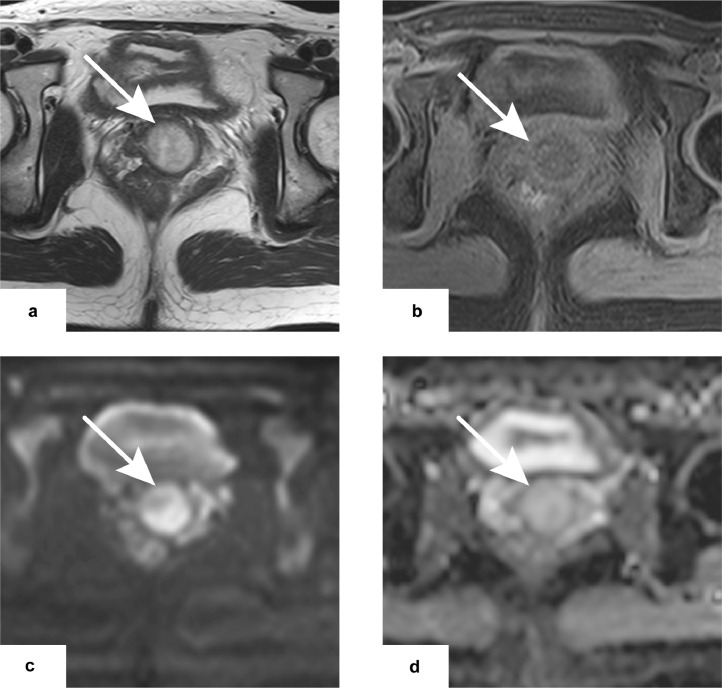
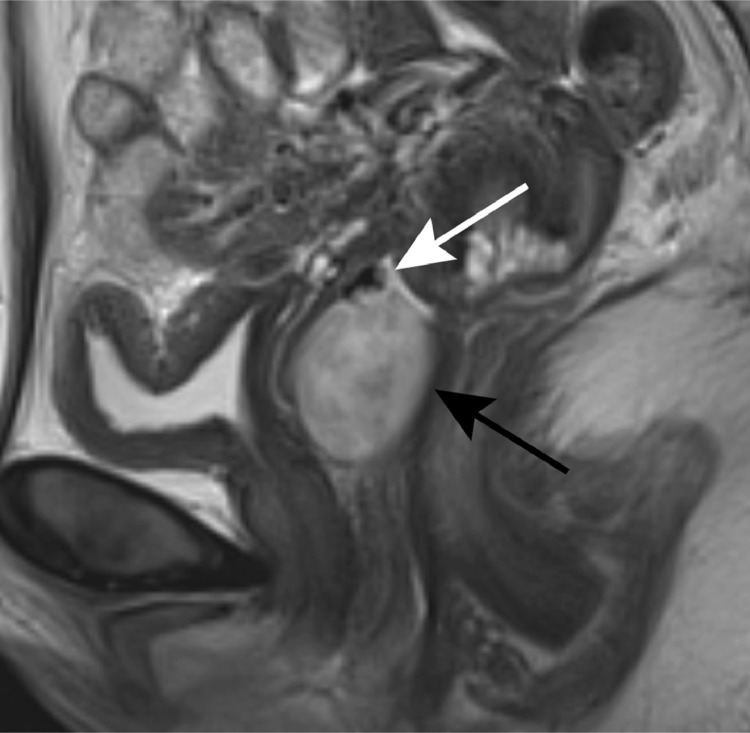
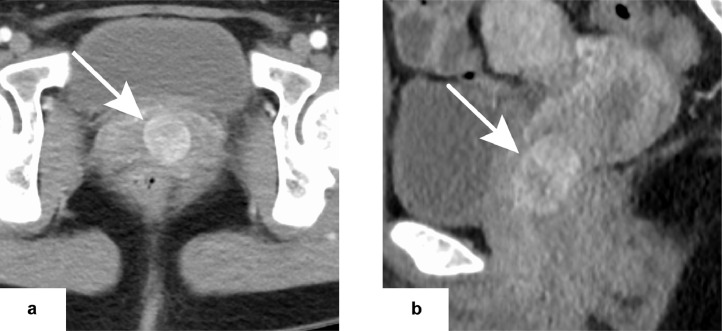
Transvaginal ultrasound showed a mass with a clear boundary. MRI confirmed a round, well-circumscribed 22×22×32mm tumor within the vagina. The tumor showed a heterogenous high signal on T2WI (Fig. 1-A) as well as intermediate signal intensity on both T1WI and fat suppressed T1WI (Fig. 1-B). A cord-like structure with a considerably low signal on T1WI and T2WI was observed between the anterior wall of the vagina and the tumor (Fig. 2). The tumor presented high-signal intensity on DWI and ADC maps, suggesting T2-shine through (Fig. 1-C, D). A CT scan with iodine contrast enhancement demonstrated strong enhancement of the tumor (Fig. 3). No malignant lesion were seen in either the pelvic or extragenital organs.
Fig. 1.
Axial images of pelvic MRI confirming a round, well-circumscribed tumor within the vagina (white arrow) . The tumor showed (A) heterogenous high signal on T2WI, and (B) intermediate signal on fat suppressed T1WI. The tumor presented high-signal on (c) DWI (b=1000) and (d) ADC maps (ADC values 1.8-1.9 × 10−3 mm2/s), suggesting T2-shine through.
Fig. 2.
Sagittal image of pelvic MRI. A cord-like structure showing a considerably low signal on T2WI (white arrow) observed between the anterior wall of the vagina and the tumor (black arrow).
Fig. 3.
CT scan with iodine contrast enhancement (a. axial image, b. sagittal image). The tumor (white arrow) demonstrated a heterogeneously strong enhancement. The area showing a relatively low signal on T2WI exhibited stronger enhancement compared to the high T2WI signal area.
The patient underwent surgery and the tumor was resected vaginally. The pedunculated tumor was arising from the anterior vaginal wall approximately 20mm proximal from the vaginal opening.
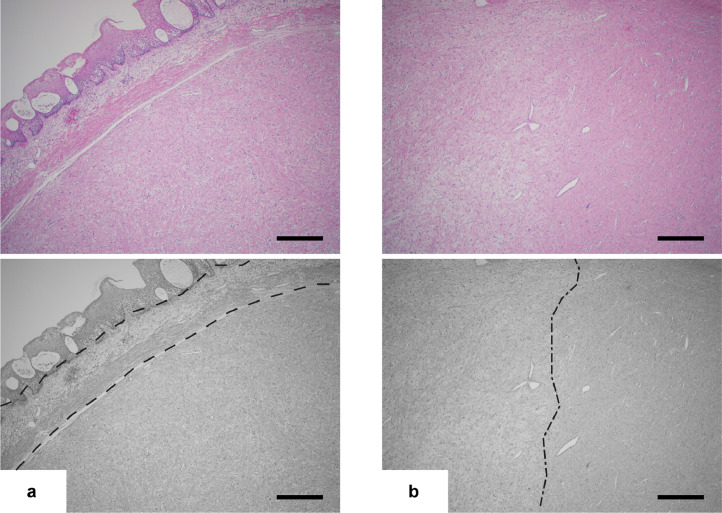
A well-circumscribed solid mass attached to a thick stalk measuring 20 mm in diameter was observed macrospically Figure 5. Microscopically, the unencapsulated tumor was composed of spindled and stellate-shaped cells with finely collagenous or myxoid stroma and no atypical mitosis was observed. A grenz zone was identified deep within the surface epithelium (Fig. 4). No necrosis or hemorrhage was identified. The stalk was composed of smooth muscle bundles while both the tumor and the stalk were covered with squamous epithelium. Immunohistochemical analysis found the tumor cells were positive for estrogen and progesterone receptors, desmin, and CD34. αSMA, EMA, and STAT6 were negative. The pathological diagnosis of superficial myofibroblastoma was rendered.
Fig. 5.
Desmin staining of the tumor and stalk. The tumor harbored a stalk composed of smooth muscle bundles that was strongly positive for desmin. The tumor was also positive for desmin. Both the tumor and the stalk were covered with squamous epithelium and the boundary between the tumor and stalk was well defined.
Fig. 4.
Hematoxylin and eosin preparation of the vaginal mass. (a) A Grenz zone (area between dash lines) was observed deep in the surface of the epithelium (Scale bar: 500μm). (b) Approximately half of the lesion was a hypercellular area with a spindled and stellate-shaped cell with finely collagenous stroma(right side of dot dash lines), and the other was myxoid, edematous stroma with few cells (left side of dot dash lines; Scale bar: 500 μm).
Discussion
Superficial myofibroblastoma is a rare benign mesenchymal neoplasm clinically presented as a polypoid or nodular mass of the lower female genital tract. It was first described in 2001 by Laskin et al. as a superficial cervicovaginal myofibroblastoma that was thought to occur only in the cervix and vagina. Later studies showed that they can also occur in the vulva [3,6]. This type of tumor has been reported in patients with a wide age range from 23 to 80 years [3]. Histologically they present spindled and stellate-shaped cells within a collagenous stroma, showing an expansive growth pattern with a clear margin and a grenz zone of uninvolved tissue is usually observed. The tumor has a specific immunohistochemical profile such as being strongly positive with desmin, vimentin, and estrogen and progesterone receptor, while reactivity for smooth muscle actin is limited [2,3,6].
Previous reports for radiological features of the superficial myofibroblastoma tumors are few. Atinga et al. reported a case presenting a solid component within a thin-walled vaginal cyst located in the vaginal fornix. The solid nodule had a low T1W1 signal and intermediate signal intensity with a hyperintense rim on T2WI [5]. Smith et al. reported a well-circumscribed mass in the upper vagina. The tumor signal was isointense to muscle on T1WI. On T2WI, it showed discrete zones within the lesion, which are high T2WI signal with no enhancement and low T2WI signal with strong enhancement, likely representing myxoid stroma and hypercellular sites, respectively. No restricted diffusion was observed [4].
The main differential diagnosis of superficial myofibroblastoma are other genital mesenchymal tumors such as fibroepithelial stromal polyps, angiomyofibroblastoma, myofibroblastoma, cellular angiofibroma and aggressive angiomyxoma. These tumors are thought to originate from hormonally responsive stroma of the lower genital tract and exhibit a considerable histologic overlap which may result in diagnostic challenges [1,2].
Fibroepithelial stromal polyps are polypoid or pedunculated masses which often develop within the vagina and vulva but may also occur in the cervix or arise from the anal mucosa [1]. They often harbor a hypocellular stalk and have a fibrovascular core. Although they have considerable similarity with superficial myofibroblastoma on their histological findings and immunohistochemical profiles, they lack the morphologic uniformity and architectural pattern compared to those of superficial myofibroblastoma and a grenz zone is usually not observed [2,3]. Previous reports have not described the radiological findings of fibroepithelial polyp in the vagina. Kato et al. reported the case of fibroepithelial polyps in the vulva which showed laminated low signal areas surrounded by multiple high signal areas on T2WI [7].
Angiomyofibroblastoma occur mainly in the vulva and vagina [1]. They are most often described as well circumscribed with vascular lesions, and showing a low signal on T1WI and homogenous or heterogenous high signal on T2WI with hyperenhancement on contrast enhanced imaging [8,9].
Cellular angiofibroma present intermediate signal intensity on T1WI. Their T2WI signal may vary from intermediate to hyperintense depending on the amount of fibrous tissue or myxoid component. They also show strong enhancement with contrast media reflecting prominent vascularity [10,11].
Aggressive angiomyxoma, which are also referred to as deep angiomyxoma, is a rare myxoid mesenchymal tumor that predominantly occurs in the vagina, vulva pelvic, and perineal regions of females. Their typical MRI findings are swirled or laminated in appearance on T2WI or contrast-enhanced images. Imaging features such as cystic degeneration, a fingerlike growth pattern, and collateral blood vessels are less common but are occasionally observed [12,13].
Leiomyoma may also demonstrate imaging features similar to superficial fibroblastoma. However, leiomyoma of the vulvovaginal area is uncommon compared to those arising from the uterine or cervix. Microscopic and radiologic appearance of vulvovaginal leiomyoma is comparable to tumors arising in other body sites such as a well circumscribed mass with variable T2WI signals [1,[14], [15], [16]].
Differential diagnosis of the vaginal tumor also includes malignant tumors. Primary malignant tumors of the vagina are rare and constitute approximately 1%-2% of gynecologic malignancies. More than 80% of those are squamous cell carcinoma, but other histologic types such as adenocarcinomas, malignant melanomas, and sarcomas also occur [17]. There are also reported cases for neuroendocrine carcinomas, lymphoma and extragastrointestinal stromal tumors though these are extremely rare [17], [18], [19], [20]. The radiological appearance of those malignant lesions are likely to be ill-defined and irregular with an infiltrative or a lobulated mass. MRI signals can be unspecific; an intermediate signal intensity on T2WI and a low signal on T1WI with the exception of melanoma which shows a high signal on T1WI. Sarcomas may present a heterogeneous signal on T1WI and T2WI corresponding to necrosis or hemorrhaging in the tumor [21,22]. Squamous cell carcinomas tend to occur in the upper one-third of the posterior vaginal wall, adenocarcinomas are more likely to occur in the upper one-third of the anterior vaginal wall, and melanoma in the lower one-third of the vagina [21]. Searching for malignancy in other organs are important to exclude the metastatic vaginal tumor, since direct extension from adjacent urogenital tumors are not uncommon compared to the rarity of primary vaginal tumors. Vaginal metastasis by lymphatic or hematogenous spread from extragenital cancers may also occur but less common. Metastatic tumors show similar radiologic features of the primary tumor [21].
The tumor reported here was a well-circumscribed mass showing a heterogeneously high signal in T2WI. The area showing a relatively low T2WI signal with strong enhancement may correspond to the fibrous rich component identified during histological examination, whereas a high T2WI signal area with weaker enhancement may correspond to the myxoid component. While MRI findings of the tumor were similar to the previously reported case of angiomyofibroblastoma and cellular angiofibroma to some extent, it differed from typical imaging features of aggressive angiomyofibroma due to a lack of infiltrative and laminated tumor morphology. Notably, the tumor harbored a stalk exhibiting a considerably low signal on both T2WI and T1WI. Although the imaging feature of the stalk was similar to the fibrous core of endometrial polyps, it was not connected to the uterine. It was microscopically composed of smooth muscle covered with squamous epithelium same as the vaginal wall which was histologically different from the fibrous core of endometrial polyps or fibroepithelial polyps.
The preoperative diagnosis of mesenchymal vaginal tumors can be challenging, because of their overlapping histological and radiological features. Also, their MRI signal and enhancement may vary depending on their component. Although definitive diagnosis should be based on histopathological assessment, radiological features such as well-defined morphology, no evidence of necrosis or degeneration, or no diffusion restriction may contribute to differentiating from more aggressive entities such as aggressive angiomyxoma or malignant tumors.
Footnotes
Competing Interest: None.
Patient consent: An informed consent was obtained from the patient for the educational and research use of this case and it is recorded in their medical record.
References
- 1.Fritchie KJ. Soft Tissue Tumors of the Skin. Springer New York; New York, NY: 2019. Genital Mesenchymal Tumors; pp. 383–403. [DOI] [Google Scholar]
- 2.Laskin WB, Fetsch JF, Tavassoli FA. Superficial cervicovaginal myofibroblastoma: Fourteen cases of a distinctive mesenchymal tumor arising from the specialized subepithelial stroma of the lower female genital tract. Hum Pathol. 2001;32(7):715–725. doi: 10.1053/hupa.2001.25588. [DOI] [PubMed] [Google Scholar]
- 3.Ganesan R, McCluggage WG, Hirschowitz L, Rollason TP. Superficial myofibroblastoma of the lower female genital tract: Report of a series including tumours with a vulval location. Histopathology. 2005;46(2):137–143. doi: 10.1111/j.1365-2559.2005.02063.x. [DOI] [PubMed] [Google Scholar]
- 4.Smith SA, Doyle V, Rutherford E, Elliot V, Blaquiere RM. Superficial myofibroblastoma of the lower female genital tract with description of the MRI features. BJR|case reports. 2017;3(1) doi: 10.1259/bjrcr.20160052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Atinga A, El-Bahrawy M, Stewart V, Bharwani N. Superficial myofibroblastoma of the genital tract: a case report of the imaging findings. BJR|case reports. 2019;5(1) doi: 10.1259/bjrcr.20180057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peng W-X, Wada R, Kure S, Fukunaga M, Naito Z. Superficial myofibroblastoma in the vulva mimicking aggressive angiomyxoma: a case report and review of the literature. Case Rep Pathol. 2019;2019:1–5. doi: 10.1155/2019/1582714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kato H, Kanematsu M, Sato E, Ito N, Furui T, Hirose Y. Magnetic resonance imaging findings of fibroepithelial polyp of the vulva: radiological-pathological correlation. Jpn J Radiol. 2010;28(8):609–612. doi: 10.1007/s11604-010-0465-6. [DOI] [PubMed] [Google Scholar]
- 8.Wolf B, Horn LC, Handzel R, Einenkel J. Ultrasound plays a key role in imaging and management of genital angiomyofibroblastoma: A case report. J Med Case Rep. 2015;9(1):1–5. doi: 10.1186/s13256-015-0715-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eckhardt S, Rolston R, Palmer S, Ozel B. Vaginal angiomyofibroblastoma: a case report and review of diagnostic imaging. Case Rep Obstet Gynecol. 2018;2018:1–8. doi: 10.1155/2018/7397121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koo PJ, Goykhman I, Lembert L, Nunes LW. MRI features of cellular angiomyofibroma with pathologic correlation. J Magn Reson Imaging. 2009;29(5):1195–1198. doi: 10.1002/jmri.21747. [DOI] [PubMed] [Google Scholar]
- 11.Miyajima K, Hasegawa S, Oda Y, Toyoshima S, Tsuneyoshi M, Motooka M, Matsuura Y, Ishioka H, Ono M. Angiomyofibroblastoma-like tumor (cellular angiofibroma) in the male inguinal region. Radiat Med. 2007;25(4):173–177. doi: 10.1007/s11604-006-0114-2. Epub 2007 May 28. PMID: 17514368. [DOI] [PubMed] [Google Scholar]
- 12.Outwater EK, Marchetto BE, Wagner BJ, Siegelman ES. Aggressive angiomyxoma: findings on CT and MR imaging. Am J Roentgenol. 1999;172(2):435–438. doi: 10.2214/ajr.172.2.9930798. [DOI] [PubMed] [Google Scholar]
- 13.Surabhi VR, Garg N, Frumovitz M, Bhosale P, Prasad SR, Meis JM. Aggressive angiomyxomas: A comprehensive imaging review with clinical and histopathologic correlation. Am J Roentgenol. 2014;202(6):1171–1178. doi: 10.2214/AJR.13.11668. [DOI] [PubMed] [Google Scholar]
- 14.Patil R, Vijay N, Joshi S. An unusual presentation of vaginal leiomyoma. J Midlife Health. 2019;10(4):204–205. doi: 10.4103/jmh.JMH_40_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Egbe TO, Kobenge FM, Metogo JAM, Manka'a Wankie E, Tolefac PN, Belley-Priso E. Vaginal leiomyoma: Medical imaging and diagnosis in a resource low tertiary hospital: Case report. BMC Womens Health. 2020;20(1):1–6. doi: 10.1186/s12905-020-0883-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Imai A, Furui T, Hatano Y, Suzuki M, Suzuki N, Goshima S. Leiomyoma and rhabdomyoma of the vagina Vaginal myoma. J Obstet Gynaecol (Lahore) 2008;28(6):563–566. doi: 10.1080/01443610802310333. [DOI] [PubMed] [Google Scholar]
- 17.Gadducci A, Fabrini MG, Lanfredini N, Sergiampietri C. Squamous cell carcinoma of the vagina: natural history, treatment modalities and prognostic factors. Crit Rev Oncol Hematol. 2015;93(3):211–224. doi: 10.1016/j.critrevonc.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 18.Howitt BE, Kelly P, Glenn McCluggage W. Pathology of neuroendocrine tumours of the female genital tract. Curr Oncol Rep. 2017;19(9) doi: 10.1007/s11912-017-0617-2. [DOI] [PubMed] [Google Scholar]
- 19.Bhagat N, Kalkur P, Kalkur S. Primary non-Hodgkin's lymphoma of the vagina (PNHLV): A gynaecologist's enigma! BMJ Case Rep. 2019;12(5):2018–2020. doi: 10.1136/bcr-2018-228544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sothornwit J, Temtanakitpaisan T, Aue-aungkul A, Likitdee N, Kleebkaow P. Extragastrointestinal stromal tumor in the rectovaginal septum associated with acute arterial occlusion. Gynecol Oncol Reports. 2020;33(July) doi: 10.1016/j.gore.2020.100609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parikh JH, Barton DPJ, Ind TEJ, Sohaib SA. MR imaging features of vaginal malignancies. Radiographics. 2008;28(1):49–63. doi: 10.1148/rg.281075065. [DOI] [PubMed] [Google Scholar]
- 22.Sahdev A, Sohaib SA, Jacobs I, Shepherd JH, Oram DH, Reznek RH. MR imaging of uterine sarcomas. Am J Roentgenol. 2001;177(6):1307–1311. doi: 10.2214/ajr.177.6.1771307. [DOI] [PubMed] [Google Scholar]