Abstract
Introduction
The first outbreak of coronavirus disease 2019 (COVID-19) in the United States resulted in a nationwide closure of dental offices that created an oral health crisis. The aim of this observational study was to analyze and compare the characteristics of patients who visited 2 private endodontics offices from March 16 to May 31, 2020, compared with the same period in 2019.
Methods
Demographic, diagnostic, and procedural data of 1520 (693 in 2020 and 827 in 2019) patient visits were collected. Bivariate and multiple logistic regression analyses were used to assess the impact of the COVID-19 outbreak on patient-related variables.
Results
Bivariate analyses showed that the number of patient visits decreased in April and May 2020 (P < .0001). In 2020, patients’ self-reported pain level was higher, they were more frequently diagnosed with pulp necrosis and acute apical abscess, and they received more incisions for drainage (P < .05). Multiple logistic regression analyses showed that the COVID-19 outbreak was associated with less visits for older patients (>49.5 years) (odds ratio [OR] = 0.720; 95% confidence interval [CI], 0.573–0.906), more patients with kidney diseases (OR = 2.690; 95% CI, 1.143–6.331), higher levels of pain on percussion (OR = 2.277; 95% CI, 1.718–3.016), less cases with previously initiated treatment (OR = 0.242; 95% CI, 0.080–0.731), less periapical diagnoses of asymptomatic apical periodontitis (OR = 0.510; 95% CI, 0.306–0.849), and a higher number of nonsurgical root canal treatments (OR = 2.073; 95% CI, 1.397–3.074) and apicoectomies (OR = 2.799; 95% CI, 1.367-5.729).
Conclusions
These findings show that the public health burden of endodontic infections was more intense during the initial outbreak of COVID-19.
Key Words: Coronavirus disease 2019, endodontics, oral systemic disease, pain, practice management
Significance.
This study describes significant changes in the private practice of endodontics that were caused by the disruption of oral health services during the initial outbreak of the COVID-19 pandemic.
The coronavirus disease 2019 (COVID-19) epidemic caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection was first reported in Wuhan, China, in December1. It rapidly spread to other countries including the United States. On March 11, 2020, the World Health Organization declared COVID-19 a global pandemic. According to the Coronavirus Resource Center at Johns Hopkins University, so far, the United States has reported more than 36 million cases of infection with more than 622,000 deaths (https://coronavirus.jhu.edu/us-map). Based on the recommendations by the American Dental Association (ADA) and the Centers for Disease Control and Prevention on March 16, 2020, dentists were advised to close their practices to all but emergency dental care (https://www.ada.org/en/publications/ada-news/2020-archive/march/ada-recommending-dentists-postpone-elective-procedures). However, this recommendation resulted in complete closure of most dental offices nationwide due to a lack of preparedness and/or fear of contracting the virus by staff or clinicians. Polls by the ADA Health Policy Institute showed that only 3% of dental offices were open in early April 2020. The percentage of open dental offices rebounded to 90% in the week of June 1, 2020 (https://www.ada.org/en/publications/ada-news/2020-archive/june/hpi-polling-shows-robust-sustained-rebound-in-dental-care). Although it was reported that most endodontic offices stayed open for dental emergencies in different capacities2, the advent of this pandemic led to nationwide lack of public access to emergency endodontic care for several weeks.
Dental clinics and institutions reported changes in the presentation and management of endodontic/dental emergencies during the initial outbreak of COVID-19. There were changes in policies at these institutions that limited their patient flow to those with true emergencies (eg, severe pain and/or swelling or life-threatening infections) that could not be managed remotely3, 4, 5, 6. Centreville Endodontics and Capitol Endodontics, 2 private offices in Washington, DC and the Northern Virginia area that are about 25 miles apart, serve a similar population of patients, and are operated by 1 team of endodontists, stayed fully operational during the period of March 16 to May 31, 2020. This allowed for a unique opportunity to observe changes in the pattern of endodontic patient visits that were driven purely by the outbreak of COVID-19, rather than by institutional policy restrictions.
There is a lack of objective data regarding the changes in patients’ presenting symptoms, pulpal and periapical diagnoses, and procedures rendered in the initial phase of the pandemic compared with information before the pandemic. Data on endodontic practice trends during the period when most general dental offices were closed are also lacking. Furthermore, little is known regarding the number of dental procedures performed on patients with systemic diseases, which could make them more susceptible to SARS-CoV-2, in the initial phase of the pandemic. The aim of this study was to retrospectively analyze the demographic, diagnostic, and procedural data for patient visits from March 16 to May 31, 2020 (COVID era) compared with patients seen in the same period in 2019 (pre-COVID era) in these 2 private endodontics offices.
Materials and Methods
This cohort study conformed to Strengthening the Reporting of Observational Studies in Epidemiology guidelines. The study protocol was reviewed by the institutional review board (IRB) at the University of Alabama at Birmingham and received IRB exempt approval (IRB-300006461).
Study Population and Design
The study group included all patients who received endodontic care in 2 private practices (Centreville Endodontics and Capitol Endodontics) during the period of March 16, 2020, to May 31, 2020 (COVID 2020 group). The control group included all patients who received endodontic care in the same 2 offices during the period of March 16, 2019, to May 31, 2019 (pre–COVID 2019 group).
To follow ADA guidelines, beginning March 16, 2020, a screening strategy was put in place in both offices to screen high-risk patients who had symptoms of COVID-19 or may have been exposed to a confirmed case of SARS-CoV-2 infection. This screening strategy included a questionnaire and temperature check upon arrival. The questionnaire focused on 3 areas: symptoms, travel history, and exposure to known COVID-19 patients.
Patients’ appointments were made over the phone. During the phone calls, a “call sheet” was filled out by administrative staff in which they recorded patients’ demographic data and self-reported pain level using a 4-point verbal rating system (no pain, mild, moderate, or severe). During the initial examination, the endodontists performed a series of endodontic and periodontal examinations to determine the tooth/teeth associated with the patients’ chief complaint and to make a diagnosis. This examination included percussion, palpation, thermal tests, electrical pulp tests, probing, biting, and mobility tests. The clinician recorded the pain level for percussion and palpation using the 4-point verbal rating system. They took periapical radiographs using Carestream Kodak digital sensors (Carestream Dental, Atlanta, GA) and the XCP paralleling device (Dentsply Sirona, Charlotte, NC) to determine the radiographic status of the tooth. The clinicians entered the examination, diagnostic, and procedural data into patients’ electronic charts in secure electronic record software (PBS Enterprise, Cedar Park, TX). Patient data were collected by accessing the day-to-day schedule of the clinic. The data were collected on a per-visit basis and anonymized before analyses.
Data Collection
The number of visits per month were recorded. The following 3 categories of data were then collected for both groups:
-
1.
Demographic data including age, sex, tooth type (molar, premolar, or anterior), self-reported pain level at the time of first contact with the office, self-reported systemic diseases (cardiovascular disease, diabetes, liver disease, and kidney disease), and the distance traveled to the office calculated based on the distance between the patient’s residential zip code to the office zip code using Google Maps (https://www.google.com/maps)
-
2.
Diagnostic data including pain level on percussion and palpation, pulpal diagnosis, and periapical diagnosis
-
3.
Procedural data including the type of procedure (evaluation, nonsurgical root canal treatment, retreatment, apicoectomy, or incision for drainage), the number of visits needed for definitive care of non-surgical root canal treatment or retreatment (single or multiple); type of restoration (temporary or permanent)
Statistical Analysis
Descriptive statistics were used to describe the main variables to be analyzed relative to the aims of the study. Bivariate comparisons, which allow for 1 covariate in a test, were performed using the chi-square test or the Fisher exact test for categoric data and using logistic regression for continuous data including age, distance, and pain levels (converted to numeric data: no and mild = 0, moderate and severe = 1). The distance was converted to a logarithmic scale because this rendered the data normally distributed (outliers [>100 miles] were excluded). The aim of bivariate analyses was to test the association between 1 variable and the binary COVID response variable, in that COVID will be the only explanatory variable.
To control for potential confounders, a multiple logistic regression model was fit in which COVID-19 year (ie, 2020) was the binary response variable, and all others were explanatory variables. All patient-related variables were included in the multiple logistic regression analysis, except the following variables: patients’ self-reported pain level due to the number of missing entries, incision for drainage, type of restoration, and single/multiple visits because they were limited to patients who received nonsurgical root canal treatment or retreatment or pulpotomy.
In multiple logistic regression analyses, all covariates were converted to binary variables. For multiple categoric variables, 1 major category was defined as a reference group—“premolar” for the tooth type, “normal pulp” for the pulpal diagnosis, “normal periapex” for the periapical diagnosis, and “evaluation” for the procedure type. Pain levels were converted to 0 (none–mild) or 1 (moderate–severe). Patients older than the average age of the entire cohort (49.5 years) were determined to be “old.” A patient who traveled a long distance was defined as having traveled more than an average distance in the cohort (12.47 miles), excluding outliers (ie, those who traveled >100 miles). Analyses were performed using SAS Version 9.4 (SAS Institute, Cary, NC), and the significance level was set at <.05.
Results
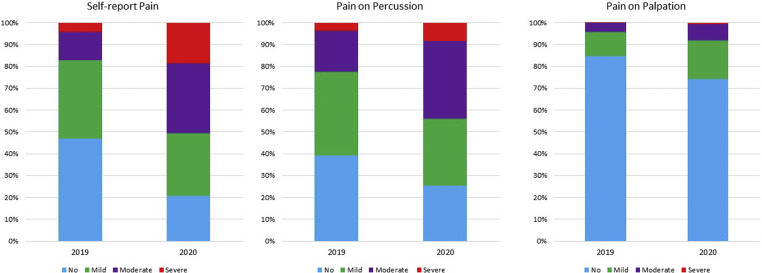
A total of 1520 patient visits were included in this study, 693 in 2020 and 827 in 2019 (Table 1 ). The category of cardiovascular disease was excluded from analyses because of the low number of entries (only 1 patient in 2019). The patients’ ages ranged from 7–94 years (48.21 ± 15.80 years) in 2020 and from 7–92 years (50.66 ± 15.62 years) in 2019. Patients traveled 0.70–81.60 miles (13.11 ± 10.52 miles) in 2020 and 0.70–77.80 miles (11.94 ± 9.897 miles) in 2019. These figures excluded those who traveled >100 miles (8 [1.1%] in 2020 and 5 [0.6%] in 2019). A summary of pain levels (self-reported pain, pain on percussion, and pain on palpation) is presented in Figure 1 . Summary statistics for variables of age, distance, and pain are shown in Table 2 .
Table 1.
The Results of Bivariate Analyses on Categoric Data
| Variable | Pre–COVID 2019, n (%) | COVID 2020, n (%) | P value |
|---|---|---|---|
| Visits per month | |||
| March | 133 (16.08) | 182 (26.26) | <.0001∗ |
| April | 328 (39.66) | 235 (33.91) | |
| May | 366 (44.26) | 276 (39.83) | |
| Demographic | |||
| Sex | |||
| Female | 470 (56.83) | 424 (61.18) | .0860 |
| Male | 357 (43.17) | 269 (38.82) | |
| Tooth type | .2358 | ||
| Anterior | 93 (11.25) | 89 (12.84) | |
| Premolar | 148 (17.90) | 141 (20.34) | |
| Molar | 586 (70.85) | 463 (66.81) | |
| Diabetes† | 56 (6.88) | 54 (7.92) | .443 |
| Liver disease† | 9 (1.11) | 2 (0.29) | .0758 |
| Kidney disease† | 9 (1.11) | 18 (2.60) | .0261∗ |
| Pulpal diagnosis | |||
| Normal pulp | 30 (3.66) | 28 (4.07) | .6792 |
| Reversible pulpitis | 14 (1.71) | 14 (2.03) | .6388 |
| Irreversible pulpitis | 251 (30.61) | 196 (28.63) | .4029 |
| Pulp necrosis | 186 (22.68) | 214 (31.1) | .00002∗ |
| Previously initiated | 24 (2.93) | 9 (1.31) | .0324∗ |
| Previously treated | 315 (38.41) | 226 (32.85) | .0248∗ |
| Periapical diagnosis | |||
| Normal periapex | 125 (15.28) | 95 (13.83) | .4268 |
| Symptomatic apical periodontitis | 479 (58.56) | 446 (64.92) | .0115∗ |
| Asymptomatic apical periodontitis | 147 (17.97) | 57 (8.30) | .0001∗ |
| Chronic apical abscess | 43 (5.26) | 45 (6.55) | .2868 |
| Acute apical abscess | 24 (2.93) | 44 (6.40) | .0012∗ |
| Procedure | |||
| Evaluation | 258 (31.2) | 156 (22.51) | .0002∗ |
| Root canal treatment | 381 (46.07) | 394 (56.85) | .0001∗ |
| Retreatment | 169 (20.44) | 116 (16.74) | .0659 |
| Apicoectomy | 18 (2.18) | 26 (3.75) | .0681 |
| Pulpotomy | 1 (0.12) | 1 (0.14) | .9003 |
| Incision for drainage‡ | 16 (2.9) | 33 (6.45) | .0058∗ |
| Restoration‡ | |||
| Temporary | 521 (94.55) | 307 (60.07) | <.00001∗ |
| Permanent | 30 (5.44) | 204 (39.92) | |
| Number of visits‡ | |||
| Single | 483 (87.65) | 439 (85.9) | .3999 |
| Multiple | 68 (12.34) | 72 (14.09) |
Chi-square analyses for the association between each categoric variable and the coronavirus disease binary variable. The Fisher exact test was used for comparison of “liver disease” and “pulpotomy” between the 2 groups.
Significant difference.
Categories with missing entries (13 in 2019 and 11 in 2020).
The total sample size is calculated as the total number of root canal treatments, retreatments, and pulpotomies (551 in 2019 and 511 in 2020).
Figure 1.
Proportional distribution of patient visits based on pain levels (no, mild, moderate, and severe) in 2019 and 2020: Self-report pain, pain on percussion and pain on palpation. The illustrations show how the proportion of moderate and severe pain dramatically increased in patient visits in 2020. The results of bivariate and multivariable analyses on pain levels are shown in Tables 2 and 3.
Table 2.
The Results of Bivariate Analyses: Logistic Regression Analyses on Age, Distance, and Pain
| Variable | Coefficient | P value | OR | 95% CI |
|---|---|---|---|---|
| Age | −0.2839 | .0060∗ | 0.753 | 0.615–0.922 |
| Log distance | 0.3280 | .0018∗ | 1.388 | 1.129–1.706 |
| Self-reported pain | 1.5854 | .0001∗ | 4.881 | 3.754–6.348 |
| Percussion pain | 0.9886 | .0001∗ | 2.687 | 2.147–3.364 |
| Palpation pain | 0.6770 | .0027∗ | 1.968 | 1.265–3.062 |
CI, confidence interval; OR, odds ratio.
Coronavirus disease 2019 is the binary response variable.
Significant difference.
Bivariate Analyses
Bivariate analyses showed several significant changes in the variables between 2020 and 2019 (Tables 1 and 2). The overall number of patient visits was significantly different in 2020 compared with 2019 (P < .0001). These visits significantly increased in March 2020 but significantly decreased in April and May 2020 (Table 1). There was no difference in patients’ sex or the tooth type between the 2 groups (Table 1). Patients with a history of kidney disease had a higher number of visits in 2020 (P < .05) (Table 1). In 2020, patients traveled longer distances; had lower age; and had higher levels of self-reported pain, pain on percussion, and pain on palpation (P < .05) (Table 2). In addition, patients with a pulpal diagnosis of pulp necrosis and with a periapical diagnosis of symptomatic apical periodontitis and acute apical abscess had significantly more visits in 2020 (P < .05) (Table 1). Patients with pulpal diagnoses of previously initiated and previously treated and patients with a periapical diagnosis of asymptomatic apical periodontitis had a significantly lower number of visits in 2020 (P < .05). The number of evaluations were significantly lower, and the number of nonsurgical root canal treatments, incisions for drainage, and permanent restorations were significantly higher in 2020 (P < .05) (Table 1).
Multiple Logistic Regression Analyses
Multiple regression analyses showed that the COVID-19 pandemic was associated with changes in several patient-related variables (P < .05) (Table 3 ). Patients who came in during the initial outbreak of COVID-19 in 2020 had significantly lower age (odds ratio [OR] = 0.720; 95% confidence interval [CI], 0.573–0.906), higher presentation with kidney diseases (OR = 2.690; 95% CI, 1.143–6.331), higher levels of pain on percussion (OR = 2.277; 95% CI, 1.718–3.016), less pulpal diagnosis of previously initiated (OR, 0.242; 95% CI, 0.080–0.731), and less periapical diagnosis of asymptomatic apical periodontitis (OR, 0.510; 95% CI, 0.306–0.849). The COVID-19 outbreak was associated with a higher number of nonsurgical root canal treatments (OR = 2.073; 95% CI, 1.397–3.074) and apicoectomy surgeries (OR = 2.799; 95% CI, 1.367–5.729) (Table 3).
Table 3.
The Results of Multiple Logistic Regression Analyses
| Variable | Coefficient | P value | OR | 95% CI |
|---|---|---|---|---|
| Older age | −0.3279 | .0049∗ | 0.720 | 0.573–0.906 |
| Sex | 0.1354 | .2400 | 1.145 | 0.914–1.435 |
| Diabetes | 0.1051 | .6298 | 1.111 | 0.725–1.703 |
| Liver disease | −1.7698 | .0994 | 0.170 | 0.021–1.399 |
| Kidney disease | 0.9895 | .0235∗ | 2.690 | 1.143–6.331 |
| Far distance | 0.2205 | .0552 | 1.247 | 0.995–1.562 |
| Anterior tooth | 0.0256 | .9054 | 1.026 | 0.672–1.566 |
| Molar tooth | −0.1207 | .4075 | 0.886 | 0.666–1.179 |
| Percussion pain | 0.8227 | .0001∗ | 2.277 | 1.718–3.016 |
| Palpation pain | −0.1303 | .6531 | 0.878 | 0.497–1.549 |
| Reversible pulpitis | −0.0260 | .9581 | 0.974 | 0.370–2.569 |
| Irreversible pulpitis | −0.6568 | .0719 | 0.518 | 0.254–1.060 |
| Pulp necrosis | −0.4369 | .2524 | 0.646 | 0.306–1.365 |
| Previously initiated | −1.4208 | .0120∗ | 0.242 | 0.080–0.731 |
| Previously treated | −0.1178 | .7513 | 0.889 | 0.429–1.841 |
| Symptomatic apical periodontitis | −0.2044 | .3192 | 0.815 | 0.545–1.219 |
| Asymptomatic apical periodontitis | −0.6739 | .0097∗ | 0.510 | 0.306–0.849 |
| Chronic apical abscess | 0.2309 | .4464 | 1.260 | 0.695–2.283 |
| Acute apical abscess | 0.2223 | .5519 | 1.249 | 0.601–2.597 |
| Root canal treatment | 0.7288 | .0003∗ | 2.073 | 1.397–3.074 |
| Retreatment | −0.0768 | .7056 | 0.926 | 0.622–1.379 |
| Apicoectomy | 1.0291 | .0049∗ | 2.799 | 1.367–5.729 |
CI, confidence interval; OR, odds ratio.
Coronavirus disease 2019 is the binary response variable.
Significant difference.
Discussion
The COVID-19 pandemic has had a tremendous impact on oral health care systems in countries around the world, including the United States. The impact was especially profound during the lockdown phase of the initial outbreak when most dental offices were closed nationwide and access to care was restricted. Although there is some information about the effects on oral health care providers2 , 7 , 8, large-scale data regarding the effects on patients are scarce. A report from Wuhan University Hospital of Stomatology on a limited number of patients (n = 96) for a short period of time (ie, 10 days in February 2020) showed a sharp increase in the proportion of endodontic emergencies9. The current study is the first report examining endodontic practice during the critical lockdown phase (ie, 2.5 months) of the initial outbreak of COVID-19 in the private sector in the United States. We showed that patients seen during this period reported significantly higher levels of pain, and they received incision for drainage more frequently. Our findings indicate that the public health burden from endodontic infections was more intense during the initial outbreak of COVID-19 than the year before. Severe pain and swelling have a substantial effect on patients’ quality of life, need for immediate care, and rapid escalation of infection control procedures. Therefore, all these aspects of oral health care were likely to be considerably impacted during the initial outbreak of COVID-19.
A critical factor that contributed to the more painful presentation of patients was the restricted access to emergency dental services. During the initial outbreak of COVID-19, most dental health care providers did not have adequate information and/or personal protective equipment to safely provide emergency patient care. This was due to a lack of action plans for a pandemic of respiratory disease as well as a lack of available regulatory resources, personal protective equipment procurement, and financial resources from health authorities. Even dental schools restricted their operations and clinical activities6. Therefore, the immediate response to the outbreak of COVID-19 was a nationwide closure of dental offices due to dentists’ anxiety about unknown risks of practicing. A study on the anxiety level of dental health care providers showed significantly higher levels of anxiety during the initial outbreak of COVID-19 due to fear of contracting the virus during dental procedures10. Studies on the positivity rate and prevalence of COVID-19 among dentists compared with the general population showed mixed results. A recent study showed a significantly higher prevalence of positive SARS-COV-2 antibodies among dental health care providers who provided dental services during the pandemic compared with the public in the United Kingdom11. A survey of 785 dentists practicing in the United States revealed that the COVID-19 infection prevalence rate was only 2.6%12. In addition, an analysis on the microbial load of aerosols generated during dental procedures showed that patient’s saliva is not a major source of SARS-CoV-2. Thus, the risk of viral transmission during dental procedures appears to be low13.
It is imperative for action plans to be prepared and to be made readily available to all oral health care providers to prevent such shutdowns in the future. Dentists must receive support from public health authorities to be able to safely continue their emergency services and to avoid closure. Oral health care must be an integral component of the health system’s essential services14. This means that local, state, and federal authorities must plan to always provide adequate public access to emergency dental services. This service should operate in a similar manner to hospital emergency rooms that continue to operate even during a respiratory disease pandemic.
The more clinical presentation of patients with pain during the initial outbreak of COVID-19 could also be related to the public’s apprehension and fear of contracting the virus in dental offices. It is likely that these patients tolerated the initial stages of mild toothache and, only when the pain became unbearable, did they rush to find a dental office. The 2 endodontic offices in the current study were open in the early weeks of the pandemic; therefore, they saw more of these patients. Several findings in the present study indirectly show changes in patients’ behavior toward dental visits. The number of patient visits reduced significantly during April and May 2020 compared with April and May 2019. Furthermore, the COVID-19 year had visits of significantly younger patients. In other words, older patients avoided dental visits in 2020 due to their apprehension, which was possibly because of their higher likelihood of developing severe symptoms15 and the higher mortality rate when infected with COVID-1916. An unstable economic perspective could have also played a role in patients’ behavior toward dental visits. A recent study showed that worsened socioeconomic conditions due to the COVID-19 pandemic resulted in deterioration of dental public health17. This survey showed that reductions in household income, reductions in work hours, and loss of jobs were independently associated with experiencing tooth pain among more than 25,000 respondents. Reduced household income was also associated with postponing dental visits17.
The COVID-19 outbreak resulted in less patient visits with asymptomatic apical periodontitis. Asymptomatic endodontic diseases are usually detected by radiographs and clinical examinations during routine visits, which prompts a referral to an endodontic specialist. These routine visits were considered “elective care” according to ADA and Centers for Disease Control and Prevention recommendations, and all general dental offices were urged to postpone such elective care during the initial outbreak of COVID-19. Therefore, far fewer cases of asymptomatic apical periodontitis were diagnosed and referred. Furthermore, it is likely that patients with asymptomatic diseases diagnosed at a routine visit before the lockdown did not pursue the treatment due to a lack of symptoms and the greater fear of contracting SARS-CoV-2 during their dental visit.
The present study showed several changes in the pattern of endodontic procedures during the initial outbreak of COVID-19. The COVID-19 outbreak resulted in a significant increase in the number of nonsurgical root canal treatments and apicoectomy surgeries. There was an increase in the number of incisions for drainage and the number of times the clinicians placed a permanent filling. The increase in the number of initial root canal treatments is consistent with other reports on the increased number of emergency visits during the initial outbreak of COVID-199. The increase in the number of apicoectomies on previously root canal–treated teeth with persistent infection shows how clinicians and patients chose a single-visit option (ie, apicoectomy) over nonsurgical retreatment to reduce the number of future visits. The increase in the number of permanent restorations was due to the uncertainty of clinicians and patients about the availability of general dentists to restore the treated teeth in a timely manner.
Previous reports showed that diabetes mellitus is associated with a significantly higher prevalence of apical periodontitis18. Also, apical periodontitis is significantly more prevalent in patients with end-stage renal disease19. Therefore, it is reasonable to assume that when there is limited access to emergency dental services, the number of dental visits by patients with diabetes and renal disease could increase due to a higher prevalence of endodontic diseases. However, the findings in the present study were mixed. Although patients with a history of kidney disease were more likely to visit a dental office during the initial outbreak of SARS-CoV-2, no differences were observed in patients with a history of diabetes mellitus and liver disease. Observational studies have shown that the risk of hospitalization and the severity of symptoms increase in COVID-19 patients with comorbidities such as diabetes, renal disease, and liver disease15 , 16. This means that patients with comorbidities might have avoided dental visits due to the high risk of consequences of contracting SARS-CoV-2. It is possible that in this study there was an association between kidney disease and symptomatic endodontic disease, which led to more patients with kidney disease presenting for treatment or that kidney disease patients were more conscious of their oral health, thereby seeking dental care despite the COVID-19 risks. One shortcoming of the present study is that the medical history of patients was self-reported. Patients frequently forget to report the details of their medical history, and they report what they assume to be the most important aspect of their medical status. The low report on cardiovascular disease may be related to this issue. Further studies with larger sample sizes in different regions are needed to thoroughly assess the effect of the COVID-19 pandemic on the dental health of patients with systemic diseases and comorbidities.
In the current study, we used a rather sophisticated statistical model to analyze the effect of the COVID-19 outbreak on patients in need of endodontic care. The multiple logistic regression analysis was aimed to control for confounders to help us better understand the pure effect of COVID-19 on demographic, diagnostic, and procedural changes. Multiple logistic regression analysis, like other models of multivariable analyses, has advantages and disadvantages. The main advantage of this model is that it can take all variables into account at the same time. This feature allows researchers to control for all confounders at the same time to better assess the effect of an independent variable (ie, COVID-19 outbreak) on multiple variables. A disadvantage of this model is that for variables with more than 2 categories (like pulpal and periapical diagnoses) it can only compare the variables with a reference group in the same category but not with other variables. Another issue is that procedural variables that are defined as a part of other procedures, like “restoration” that is done only after nonsurgical root canal treatment or retreatment, cannot be included in the analysis because they cannot be assessed for all patients.
CRediT authorship contribution statement
Ali Nosrat: Conceptualization, Methodology, Data acquisition, Data curation, Writing – original draft, Writing – review & editing. Omid Dianat: Methodology, Data acquisition, Writing – review & editing. Prashant Verma: Methodology, Writing – review & editing. Peter Yu: Data acquisition, Data curation, Writing – review & editing. Di Wu: Data acquisition, Data curation, Writing – review & editing. Ashraf F. Fouad: Conceptualization, Methodology, Data acquisition, Data curation, Writing – review & editing.
Acknowledgments
The authors thank Sahar Taheri, PharmD candidate, for her help with data collection and auditing.
The authors deny any conflicts of interest related to this study.
Footnotes
Supplementary material associated with this article can be found in the online version at www.jendodon.com (https://doi.org/10.1016/j.joen.2021.09.015).
Supplementary data
References
- 1.Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Martinho F.C., Griffin I.L. A cross-sectional survey on the impact of coronavirus disease 2019 on the clinical practice of endodontists across the United States. J Endod. 2021;47:28–38. doi: 10.1016/j.joen.2020.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beauquis J., Petit A.E., Michaux V., et al. Dental emergencies management in COVID-19 pandemic peak: a cohort study. J Dent Res. 2021;100:352–360. doi: 10.1177/0022034521990314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Langella J., Magnuson B., Finkelman M.D., Amato R. Clinical response to COVID-19 and utilization of an emergency dental clinic in an academic institution. J Endod. 2021;47:566–571. doi: 10.1016/j.joen.2020.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Salgarello S., Salvadori M., Mazzoleni F., et al. Urgent dental care during Italian lockdown: a cross-sectional survey. J Endod. 2021;47:204–214. doi: 10.1016/j.joen.2020.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Weintraub J.A., Quinonez R.B., Smith A.J.T., et al. Responding to a pandemic: development of the Carolina Dentistry Virtual Oral Health Care Helpline. J Am Dent Assoc. 2020;151:825–834. doi: 10.1016/j.adaj.2020.08.003. [DOI] [PubMed] [Google Scholar]
- 7.Yu J., Hua F., Shen Y., et al. Resumption of endodontic practices in COVID-19 hardest-hit area of China: a web-based survey. J Endod. 2020;46:1577–1583.e2. doi: 10.1016/j.joen.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meng L., Ma B., Cheng Y., Bian Z. Epidemiological investigation of OHCWs with COVID-19. J Dent Res. 2020;99:1444–1452. doi: 10.1177/0022034520962087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yu J., Zhang T., Zhao D., et al. Characteristics of endodontic emergencies during coronavirus disease 2019 outbreak in Wuhan. J Endod. 2020;46:730–735. doi: 10.1016/j.joen.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Olivieri J.G., de España C., Encinas M., et al. General anxiety in dental staff and hemodynamic changes over endodontists' workday during the coronavirus disease 2019 pandemic: a prospective longitudinal study. J Endod. 2021;47:196–203. doi: 10.1016/j.joen.2020.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shields A.M., Faustini S.E., Kristunas C.A., et al. COVID-19: seroprevalence and vaccine responses in UK dental care professionals. J Dent Res. 2021;100:1220–1227. doi: 10.1177/00220345211020270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Araujo M.W., Estrich C.G., Mikkelsen M., et al. COVID-2019 among dentists in the United States: a 6-month longitudinal report of accumulative prevalence and incidence. J Am Dent Assoc. 2021;152:425–433. doi: 10.1016/j.adaj.2021.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meethil A.P., Saraswat S., Chaudhary P.P., et al. Sources of SARS-CoV-2 and other microorganisms in dental aerosols. J Dent Res. 2021;100:817–823. doi: 10.1177/00220345211015948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Benzian H., Beltrán-Aguilar E., Mathur M.R., Niederman R. Pandemic considerations on essential oral health care. J Dent Res. 2021;100:221–225. doi: 10.1177/0022034520979830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bennett T.D., Moffitt R.A., Hajagos J.G., et al. Clinical characterization and prediction of clinical severity of SARS-CoV-2 infection among US adults using data from the US National COVID Cohort Collaborative. JAMA Network Open. 2021;4:e2116901. doi: 10.1001/jamanetworkopen.2021.16901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mehta H.B., Li S., Goodwin J.S. Risk factors associated with SARS-CoV-2 infections, hospitalization, and mortality among US nursing home residents. JAMA Network Open. 2021;4:e216315. doi: 10.1001/jamanetworkopen.2021.6315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Matsuyama Y., Aida J., Takeuchi K., et al. Dental pain and worsened socioeconomic conditions due to the COVID-19 pandemic. J Dent Res. 2021;100:591–598. doi: 10.1177/00220345211005782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yip N., Liu C., Wu D., Fouad A.F. The association of apical periodontitis and type 2 diabetes mellitus: a large hospital network cross-sectional case-controlled study. J Am Dent Assoc. 2021;152:434–443. doi: 10.1016/j.adaj.2021.01.005. [DOI] [PubMed] [Google Scholar]
- 19.Khalighinejad N., Aminoshariae A., Kulild J.C., et al. Association of end-stage renal disease with radiographically and clinically diagnosed apical periodontitis: a hospital-based study. J Endod. 2017;43:1438–1441. doi: 10.1016/j.joen.2017.04.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.