Abstract
The outbreak of the COVID-19 pandemic is unarguably the biggest catastrophe of the 21st century, probably the most significant global crisis after the second world war. The rapid spreading capability of the virus has compelled the world population to maintain strict preventive measures. The outrage of the virus has rampaged through the healthcare sector tremendously. This pandemic created a huge demand for necessary healthcare equipment, medicines along with the requirement for advanced robotics and artificial intelligence-based applications. The intelligent robot systems have great potential to render service in diagnosis, risk assessment, monitoring, telehealthcare, disinfection, and several other operations during this pandemic which has helped reduce the workload of the frontline workers remarkably. The long-awaited vaccine discovery of this deadly virus has also been greatly accelerated with AI-empowered tools. In addition to that, many robotics and Robotics Process Automation platforms have substantially facilitated the distribution of the vaccine in many arrangements pertaining to it. These forefront technologies have also aided in giving comfort to the people dealing with less addressed mental health complicacies. This paper investigates the use of robotics and artificial intelligence-based technologies and their applications in healthcare to fight against the COVID-19 pandemic. A systematic search following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) method is conducted to accumulate such literature, and an extensive review on 147 selected records is performed.
Keywords: COVID-19, SARS-coV-2, Robotics, Artificial intelligence, Healthcare, Autonomous system
1. Introduction
The ravaging effects of Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV-2) Disease (COVID-19) are not just confined to claiming the lives of nearly 4.5 million people; it has created a depression across all the functional aspects of human lives. After being characterised as Global Pandemic by the World Health Organization (WHO) on 11 March, 2020 [1], The world has witnessed how this highly infectious disease has ceased normal life and made everything get beyond control around the globe. The outrageous transmissibility of Coronavirus can be substantiated by its average reproduction number of around 3.28 [2], which signifies the average number of infection cases caused by an already infected individual and is an indicator of a pathogen’s potential to cause a pandemic. This supports the exponential growth of the cases in the epicentres though it has a low fatality rate of 0.17 to 1.7% [3] among the infected people. The crown-like appearance of the Coronavirus (The membrane surface protein of Coronavirus looks a bit like a crown) justifies the prefix ‘Corona’ which is a Latin word for “Crown” and thus has been characterised as a member of the Corona Viridae family [4]. The novel Coronavirus, started in Wuhan City of Hubei Province of China, was transmitted through bats that can host the most viral genotypes of Coronavirus. Viruses transmitted from species to species can carry developed mutations in proteins on their envelope that have substantial capacity to bind cells in different specimens and acquire high contiguous potentialities through several mutations. These factors have led the Coronavirus to run rampant worldwide with 4.48 million deaths and 215 million confirmed cases as of 26 August 2021 [5].
The health sector has faced severe vulnerabilities in the COVID-19 pandemic. The public health challenges soared up higher than ever because of the unpreparedness of the health sectors for a global pandemic. The lack of standardised treatment protocol, guidelines, and manuals for such a crisis has made the practitioners in this field more incompetent. During the courses of this kind of emergencies, health professionals are subjected to set preferences in about all the aspects of their working grounds ranging from fixing research priorities to performing diagnosis and caregiving acts. From diagnosis to treatment, the caregivers are susceptible to danger in every phase of the cycle. The fragile protection measures for the doctors, nurses, and lab technicians can unsettle the spontaneity of preventive and curative care in due time. But hospitals are the hot spots for virus transmission, and monitoring the safety rules abidance by everyone there is more complex than it seems. Safety equipment paucity demarcates the protective measures considerably. Early detection and preventive measures according to it, can mitigate the risk of transmission to a greater extent. However, tracing out the most susceptible cases, arranging immediate testing, and isolating vulnerable communities are naturally dependent on the availability of test kits, expert physicians, isolation beds, ICU, CCU, and many other resources. WHO approves the Polymerase Chain Reaction (PCR) testing as the only diagnosis method for novel COVID-19 because of its higher accuracy [6]. Nevertheless, this convoluted method is expensive, time-consuming, and requires expert involvement resulting in a lower outreach for most countries. Constant disinfecting can also de-escalate the spread of the virus in hospitals and public places. However, manual disinfection jobs present a risk to the workers and fail to meet the standard operation of the task.
The frightful mortality rates and detrimental health issues of the COVID-19 pandemic have stressed the need for addressing its impact on physical health so hugely that the severe negative implications it has posed on mental health have often been disregarded. The havoc created for the emergence of this undesired phenomenon has incited panic, anxiety and trauma-related disorders [7]. The reduced social interaction owing to preventive measures like quarantine, lockdown, social distancing have enforced loneliness, solitude, and other common risk factors to mental well-being. Many studies and reports have revealed the increase in domestic violence and femicide during this period [8]. So it is foreshadowed the consequences of mental health degradation for this pandemic may trigger somatisation, phobic anxiety, obsessive-compulsive disorder, depression, and other mental illnesses.
It is undeniably true that the challenges for the Coronavirus require prompt and dynamic solutions. Health workers and policymakers are making constant efforts to address these challenges. Researchers around the world are applying the leading technologies with their scientific findings to find redress for this unprecedented peril. AI and Robotics have been substantiated to be a potential means for scientific research and have enforced the efficacy of these studies both empirically and theoretically [9].
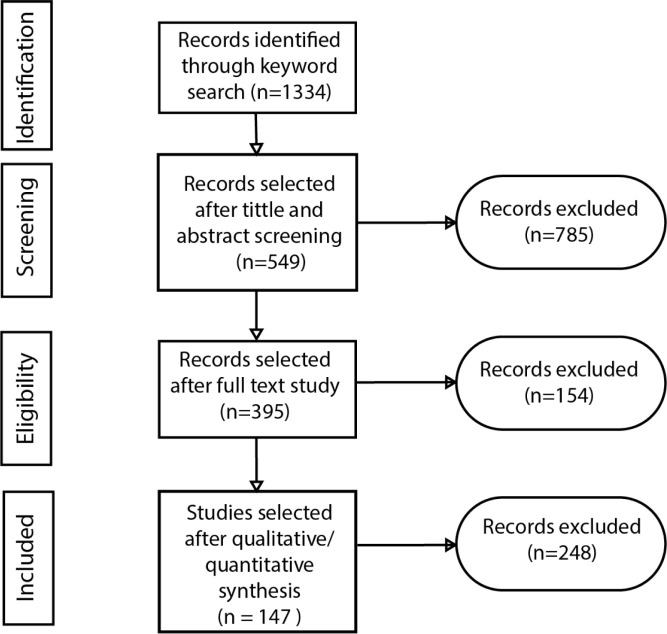
We conducted a systematic search to compile the scientific records related to our scope. The Mendeley database was chosen to perform the search on literature from January 2020 onwards with the combination of the keywords “Coronavirus”, “COVID-19”, “Healthcare”, “Robotics”, and “Artificial Intelligence”. Preprints and scientific reports were excluded. Selecting literature only from renowned journals, conferences proceedings, and book chapters, 1334 records were gathered from this stage. Then, the abstract and title of these 1334 were screened which resulted in 549 papers to be selected for the next stage. In the next stage, the full text of this set of articles were assessed. Many of the literature that were perceived as relevant to this subject-matter from the initial abstract screening was found to be more focused on biological, genetics, and different subject related findings rather than presenting any applicative work of Robotics and AI in facilitating the healthcare sector directly. 154 papers were ruled out from this stage. Finally, an in-depth analysis of the remaining 395 records was done. For inclusion assessment in this stage, the study characteristics were thoroughly analysed. Many authors had proposed conceptual ideas and methodologies of AI and robotics driven solutions for this pandemic time, some of which were yet to be materialised in real-world scenarios. Therefore, from the selected studies, the technologies that had been deployed in real-world settings or had the potential to be used in such environments were included for this study. Finally, 147 literatures were selected from the final stage of the literature search. The entire selection process is demonstrated in Fig. 1.
Fig. 1.
Flow diagram of the record selection process based on the PRISMA approach.
In this paper, we have listed some applications of artificial intelligence (AI) and robotics that have been tailored to serve in the COVID-19 situation. These technologies have scopes to be employed in practically every point of solution response to the pandemic. For early and rapid detection, community transmission tracing, AI has featured new algorithms for creating alternatives to the conventional approaches. Enthusiasts have addressed monitoring social distancing rules with the collaboration of computer vision and machine learning (ML) methodologies. The research for drugs of COVID treatment and the most anticipated vaccine discovery is also being accelerated with AI and its sub-field ML. Machine learning, regarded as the hot-spot of AI, has been leading the prediction modelling task such as determining the severity of the patients from initial symptoms, identifying high-risk and vulnerable individuals and predicting the virus spread in different locations. Innovators have been very active in coming up with numerous automation systems to alleviate the workloads of health professionals in high-risk jobs like disinfecting hospital areas, enforcing clinical care, testing prototypes, conducting healthcare training, and so on. The rest of the paper is organised as follows. Section 2 holds a detailed depiction of the healthcare spectral units during this pandemic. In Section 3, various applications of Robotics and AI in healthcare are elaborately described. A discussion on future directions is provided in Section 4. Finally, the paper marks the concluding remarks in Section 5.
2. Healthcare spectrum during COVID-19
The sudden outbreak of COVID-19 has resulted in a massive amount of additional work of operations to the health sector and related fields. The operational works require different stages of collaborative support and the service scopes are also not confined to a single field. Rather the related affairs in the health division can be divided into certain spectra and the proceedings can function following the spectral units of task forces [9]. Acknowledging the division of work with respect to the different patient categories, the point of services in healthcare departments can be divided into five spectra as shown in Fig. 2. These are discussed briefly as follows:
Fig. 2.
Division of the healthcare spectrum during COVID-19.
-
(A)
General care (Primary prevention and healthcare support): Primary prevention refers to the steps taken by the authorities or individuals including social distancing, wearing facial masks, washing hands, posing lockdown in cities, etc. It implies the imposition of strict laws for monitoring social distancing, observing people whether they are wearing masks, inspecting the lockdown areas so the public is bound to obey them. Primary prevention measure also includes the detection of the vulnerable areas with massive screening and rapid testing facility which will provide details to identify risk using contact tracing information and thus predict the spread of disease in different areas. Material supports such as sanitation and protective equipment are also included in primary prevention care.
-
(B)
Inpatient care (Acute and emergency care): This spectrum includes the diagnosis of the patients, evaluation of the diagnosis results, triage them to the proper level of care, sort out the appropriate treatment methods for the hospitalised patients, critical care and isolation support, predict the severity of the patient from initial symptoms to identify high-risk and vulnerable individuals and shift them to ICU or CCU for proper clinical care of them and arrange telemedicine opportunities for less severe patients.
-
(C)
Non-COVID-19 outpatient, home and long-term care: Secondary prevention measures and long-term disease management are included in this spectrum. As the contagious disease has a virus transmission possibility everywhere the infected person goes, there is no alternative to disinfecting the hospital areas. The safety rule maintenance’s by the hospital workers is essential for pursuing the treatment of non-COVID-19 outpatients.
-
(D)
Medical education: This spectrum involves the measures required for empowering the healthcare staff through hands-on training on up-to-the-date treatment and technologies for supporting the COVID-19 patients. So accelerating healthcare training and education for health workers and reducing the workload of the healthcare workers with advanced technologies are included here.
-
(E)
Research and development (R&D): Research and development in pandemic time incorporate identifying effective existing drugs, accelerating research and treatment, testing prototypes, developing drugs faster, developing vaccines, and creating personal protective equipment (PPE).
3. Robotics and AI technologies in COVID-19 Healthcare
The technological field of AI and Robotics has performed miracles to settle the dire needs of the health sector in this pandemic. Researchers and innovators are providing new solutions for the rising challenges in the healthcare sector due to the COVID-19 outbreak. In this section, we discuss some of the points of services where Robotics and AI have impacted enormously for the amelioration of the situations during this pandemic such as diagnosis, risk assessment, surveillance, telehealthcare, delivery and supply chain, service automation, disinfection, and accelerating research and drug development.
3.1. COVID-19 diagnosis
During the COVID-19 pandemic, rapid testing is being given higher priority to limit the contagion which helps to prevent virus spread. However, it is challenging due to the scarcity of medical resources and the increased chances of contagion by direct contact. Robotic technologies can be used to collect samples in a contactless way. Robots are also being used as a tool that enables doctors to remotely diagnosis the patients which minimises the chances of contamination. AI algorithms facilitate prioritising the faster scheduling of suspected patients and speed up the testing process while requiring minimal manpower. Fig. 3 illustrates some of the robotics and AI-based technologies for COVID-19 diagnosis.
Fig. 3.
COVID-19 diagnosis using robots and AI based technologies: (a) Contactless sample collection using robots (b) COVID-19 detection using AI.
Early detection can help to control the rapid spreading of the virus. A detailed study of different AI-empowered COVID-19 detection and prediction works of the recent time is provided in [10]. Significant studies have been done to establish relations between the early symptoms of COVID-19 and the test results which may facilitate the detection of the disease from those mild symptoms [11]. The routine test of COVID-19 is conducted with a positive test for SARS-CoV-2. However, this method is time-consuming and poses a higher chance of false-positive results.
A temperature screening system [12] can measure the temperature of the passengers in a vehicle in a contactless and autonomous way and can further assess if the person is eligible to enter a territory. Dr. Spot [13] can carry out a series of monitoring operations along with vital symptom evaluation and can further be teleoperated with trained clinical staffs accordingly with initial assessment which was deployed in several hospital settings.
As an alternative, artificial intelligent algorithms combining imaging techniques such as computer tomography (CT scans) can be used to evaluate the patients with COVID-19 symptoms [14], [15]. An end-to-end learning-based Coronavirus classification model with CT scan images was built by [16], the training set for the model was enhanced with the BigBiGAN and a linear classifier and two nonlinear classifier SVM and KNN algorithms were used in this work. Similar to this, the deep learning-based COVID detection models have shown promising results and were adopted in many investigation [17], [18], [19]. CNN-based COVID detection models with DenseNet-201 architecture were presented in [20], [21], [22]. Several works proposed their own architecture for CT-image based COVID detection as in [23] designed the FaNet architecture which reported 94.83% accuracy, the COVNet model from [24] distinguished COVID cases with high specificity and sensitivity, [25] had manifested FGCNet which claimed to be better performing than 15 state-of-the-art methods. An easy-to-operate ML-based COVID classification approach was presented in [26]. The authors designed a pipeline for the Medical decision support based on Google AutoML Cloud Vision, clinical data [27] and patient information [28]. Many smartphone app-based diagnosis systems have been developed for the diagnosis, treatment, control, and prevention of the disease [29], [30].
AI solutions are helping the radiologist to analyse the patterns of the radiology image and assess the probability of infection [31], [32]. A VGG Convolution Neural Network was presented in [33] that can aid the clinical decision support system for early detection of the disease. In [34], the authors proposed a DL algorithm based model COV19NET, for COVID detection from chest radio graphs.
A new AI-powered method is devised by UC Diego Health, which uses a machine learning model for the early diagnosis of pneumonia, a severer condition of COVID-19. This model is trained with 22,000 chest X-ray images annotated by human radiologists, which can depict the probability of pneumonia by coloured region in the chest X-ray [35].
The quest to discover the best methodology for the detection of COVID-19 from chest X-ray with the help of different machine learning and deep learning algorithms has been very prevalent among practitioners. The authors in [36], [37] presented a CNN architecture combined with transfer learning technique for COVID-19 diagnosis. The work in [38] had only used CNN to build a prediction model with training data of COVID-19 positive and negative X-rays.
The findings from [39] show that different architecture of CNN has great potential in detecting Coronavirus disease from chest X-ray. The authors concluded among different CNN models the ResNet-50 has the best performance on chest x-rays. In [40], the performance of a pre-trained neural network, DarkNet-19 was assessed. The model had an overall accuracy of 94.28% in COVID-19 radiographic feature detection. Deep learning based COVID detection models were also rendered in [41], [42]
The feature extraction of the chest x-ray with different Machine Learning algorithms such as CfsSubsetEval, K-nearest neighbours classifier etc. reported an average of 96.5% precision and recall was demonstrated in [43]. The structure of a novel fusion model FM-HCF-DLF was demonstrated in [44]. Three pre-trained CNNs AlexNet, GoogleNet, and SqueezeNet were fine-tuned and their performance in several publicly available datasets were evaluated in [45]. As transfer learning from these models gave acceptable results, the authors suggested that the existing models for diagnosing should be explored with more attention before developing a completely new architecture with different deep learning techniques for COVID-19 detection. In [46], the authors had developed a deep learning pipeline with local binary pattern, dual tree complex wavelet transform and convolutional neural networks for COVID-19 detection using chest X-ray images. Gupta et al. [47] had developed InstaCovNet-19 architecture with transfer learning from renowned architectures such as ResNet101, Xception, InceptionV3, MobileNet, and NASNet for COVID detection. The network achieved 100% precision and 99% recall on binary class COVID-19 classification. Similar transfer learning based studies were presented in [48], [49], [50].
The COVID detection methodology proposed in [51] had involved different machine learning algorithms such as CNN, support vector machine (SVM), and random forest (RF) for COVID infection identification. The insufficiency of the proper dataset for COVID detection research was addressed in [52]. The authors used weekly labelled data augmentation process to enhance the size of training data and their evaluation revealed adding augmented data impacted positively in the result of the classification as the average accuracy of the model increased by 21.04% from non-augmented training. Deep convolutional neural network (CNN) model, CVDNet was introduced in [53] which reported an average accuracy of 97.20% in COVID detection. Another deep learning based COVID detection model on chest radiographs, DeepCOVID-XR was proposed in [54]. The study in [55] provided a VGG-16 based Deep Learning model for COVID-19 classification. Zhang et al. [56] had trained, validated, and tested their CV19-Net model for differentiating Coronavirus disease from other viral pneumonia. In [57], the pipeline of COVID-19 detection involved the Fuzzy Colour technique for restructuring the dataset, Social Mimic optimisation method for feature selection and deep learning models namely MobileNetV2, SqueezeNet for dataset training. And then, with an SVM classifier, the model scored an accuracy of 99.27%. In [58], the lung x-ray images were analysed with CNN architecture to detect the infected tissues in the lungs.
Several researchers have carried out investigations on both CT and X-ray image modalities for COVID and non-COVID classification and reported satisfying accuracy [59], [60], [61]. Many transfer learning models were analysed and fine-tuned for extracting features of COVID-19 infected chest X-ray and CT image in [62], where the VGG-19 model gave out the best accuracy of 99%. [63] have proposed a decision tree based approach for COVID detection and achieved 93% and 88% accuracy for CT scan and chest x-ray respectively. In [64], a CNN model for COVID 19 detection with CT and X-ray images was presented, which attained better accuracy in X-ray images. Another stream of works focused on the acoustic signal features like cough, speech, breathing, voice, etc. for COVID screening [65], [66], [67].
Artificial Intelligence models can diagnose COVID-19 from symptoms of patients. Diagnosing from symptoms can substantially aid in carrying out an initial screening in places with lower outreach. The Mobile application COVID Symptom Study [68] can predict COVID-19 infection by comparing the symptoms of the user with COVID-19 positive patients. It had received a great response as over 3 million people reported about their health issues through this application.
Lab-on-a-chip technology integrates several laboratory functions on a single chip at most a few centimetres in size while reducing both the reagent cost and analysis time of a bio-medical examination. The advanced version of the LoC is a device called point of care (PoC) which performs tasks ranging from sample preparation to analysis in a cost-effective way while requiring no complicated equipment and trained professionals [69]. Such PoC devices can be used as a rapid on-site testing kit of COVID-19 where there is a scarcity of medical staff and costly equipment [70]. Biosensors contain semiconductor circuitry with a coating of biological material. This material attracts and binds to a target in the sample fluid which signals the presence of the COVID-19 RNA, antibody, or antigen. A biosensor chip contains multiple circuits, each containing different biological substances as a detector which enables the chip to perform different tests such as viral RNA, antibodies, and antigens at the same time. As a result, biosensors perform tests in an extremely short time, even within 60 s. Moreover, along with detecting the intended one, a biosensor provides information about other health issues of a patient while decreasing the false-positive results. For example, performing a test for the flu can simultaneously identify the Coronavirus at the earlier stage [71], [72]. Some of these AI-based diagnosis systems are summarised in Table 1.
Table 1.
A summary of notable works in the field of COVID-19 diagnosis using AI technologies.
| Research | Application | Modality | Methodology |
|---|---|---|---|
| [18], [19], [20], [24], [26] | Diagnosis of COVID-19 | Chest CT scan images | State-of-the-art CNN architectures (U-Net, AlexNet, VGG, Inception, ResNet, SqueezNet, DarkNet, ShuffleNet, Xception, MobileNet, DenseNet) |
| [23], [25], [28] | Diagnosis of COVID-19 | Chest CT scan images | Custom CNN architecture |
| [31], [32] | Differentiate COVID-19 infections from other abnormalities as well as normal cases | Chest CT scan images | State-of-the-art CNN architectures (U-Net, AlexNet, VGG, Inception, ResNet, SqueezNet, DarkNet, ShuffleNet, Xception, MobileNet, DenseNet) |
| [37], [39] | Diagnosis of COVID-19 | Chest X-ray images | State-of-the-art CNN architectures (U-Net, AlexNet, VGG, Inception, ResNet, SqueezNet, DarkNet, ShuffleNet, Xception, MobileNet, DenseNet) |
| [33], [40], [41], [43], [44], [47], [48], [49], [50], [55], [57] | Differentiate COVID-19 infections from other abnormalities as well as normal cases | Chest X-ray images | State-of-the-art CNN architectures (U-Net, AlexNet, VGG, Inception, ResNet, SqueezNet, DarkNet, ShuffleNet, Xception, MobileNet, DenseNet) |
| [34], [42], [46], [51], [54], [56], [58] | Diagnosis of COVID-19 | Chest X-ray images | Custom CNN architecture |
| [53] | Differentiate COVID-19 infections from other abnormalities as well as normal cases | Chest X-ray images | Custom CNN architecture |
| [59], [62] | Diagnosis of COVID-19 | Chest X-ray images, chest CT scan images | State-of-the-art CNN architectures (XCEPTION, VGG16, VGG19, RESNET, INCEPTIONV3 and MOBILENET) |
| [66], [67] | Diagnosis of COVID-19 | Coughing sounds | Custom CNN architecture |
| [65] | Diagnosis of COVID-19 | Coughing sounds, breathing sounds and voice | Long short-term memory (LSTM) |
3.2. COVID-19 risk assessment
The effect of Coronavirus damages the physical well-being of different individuals differently. To some patients, much medication and consultation are not required; for some groups, especially the elderly and vulnerable population need special care with a fast and prompt response from the service provider to survive. However, the assessment of the severity of this novel disease is not an easy task. AI platforms have extended hands to identify individuals who are at high risk based on their existing medical conditions [73].
In [74], the authors developed a COVID-19 vulnerability index considering the pre-existing medical conditions using machine learning models. A non-profit organisation in Chicago, named The Medical Home Network, uses AI solutions to identify vulnerable individuals based on their respiratory complications.
There have been several works focused on assessing the severity of infection in different individuals with AI-based chest imaging findings [75], [76]. The CT severity score of the patients was predicted with different deep-learning algorithms in [77], [78]. A CNN model was exploited to prognosticate the level of lung disease severity in [79].
Although over 80 percent of cases seem to be mild, those who develop severe symptoms often need oxygen and prolonged ventilation. AI tool can accurately predict from the newly infected with COVID-19 patients who can go on to develop severe respiratory disease. The AI model needs to use the data of severe and mild COVID patients and train it with a machine learning algorithm to define the patterns of COVID-19 and predict its severity. Many machine learning models are designed to predict the mortality chance of COVID patients with different samples [80], [81]. The AI model, EDRnet in [82], had an accuracy of 92% in predicting the mortality rate for COVID-19. The model was developed with ensemble learning based on deep neural network and random forest algorithms to implement the in-hospital mortality prediction. Mushtaq et al. [83] conducted a severity assessment study based on the chest X-ray using deep learning artificial intelligence (AI) system.
The development of machine learning-based applications by the researchers have been greatly facilitated with the availability of COVID-19 related data. Statistical studies identified important risk factors such as age, pre-existing conditions, personal hygiene, social habits, frequency, the number of human interactions, etc. which are correlated with the probability of being infected.
Machine learning models can be used to predict the likelihood of an infected person developing complications [87], [88]. In [84], a decision tree-based predictive modelling system was developed to portend the recovery period of COVID patients. It also assists in the decision process in the hospitals by forecasting about the individuals with high risk and thus helps to triage him/her for appropriate medical care. The authors in [89] constructed a deep-learning neural network algorithm to detect the peak clinical variable predictors, which can be further inferred for proper triaging of patients with risk scoring from blood samples.
A data-driven pre-hospital triage system was demonstrated in [85] that can aid in responding to the overwhelming demand of patient care in comparison to the healthcare system capacity. The authors in [90] presented an AI-empowered methodology for clinical decision support using CT data. The studies in [91], [92], [93] had demonstrated similar findings in their works to facilitate the management of patients.
In [86], authors used machine learning models that learn from patient’s historical data and predict the chance of developing acute respiratory distress syndrome (ARDS) with an accuracy of almost 80%. Machine learning models have already been used to predict the treatment outcome, such as cancer immunotherapy responses [94]. Similar prediction models can be used to assess the risk of COVID-19 treatment. Some of the AI-empowered application for risk assessment is outlined in Table 2.
Table 2.
A summary of notable works on risk assessment during the COVID-19 pandemic.
| Research | Application | Methodology | Performance |
|---|---|---|---|
| [73] | COVID-19 diagnosis from symptoms | Fuzzy Inference System | No metrics provided |
| [74] | Vulnerability assessment of individuals | Logistic regression, Gradient Boosted Trees and Closedloop platform | No metrics provided |
| [80] | Mortality risk assessment from COVID-19 | Artificial Neural Network | Accuracy: 86.25%, Sensitivity: 87.50%, Specificity: 85.94%, AUROC: 90.12% |
| [82] | COVID-19 mortality risk assessment using blood samples | Ensemble learning using deep neural network and random forest | Sensitivity 100%, Specificity 91% and Accuracy 92% |
| [84] | COVID-19 recovery period estimation and identification of high risk age groups | Decision tree, Support Vector Machine, Naive Bayes, Logistic Regression, Random Forest and K-nearest Neighbour | Accuracy 99.85% |
| [79] | COVID-19 severity assessment from chest x-ray images | Transfer learning with VGG16 | 0.90 and mean absolute error of 8.5% |
| [85] | Identification of high risk individuals that require hospitalisation and low risk individuals that can recover at home using a chatbot | AI chatbot | No metrics provided |
| [86] | Predict development of acute respiratory distress syndrome (ARDS) of COVID-19 patients from clinical data | Logistic Regression, KNN, Decision Tree, Random Forests and Support Vector Machine | Accuracy: 70% to 80% |
3.3. Surveillance during COVID-19
The first specimen of Coronavirus was detected in the Wuhan city of Hubei province of China. Then with the increase of spread, the hot spot of infection and death from the virus changed from time to time. Several countries of Europe, America, South America, and Asia had faced serious crises in healthcare departments for this unprecedented peril. The lack of preparation of the government of these states had made the situation worse. So the forecast about the spread of the virus to any region would definitely help the policymakers act proactively and take the necessary steps accordingly.
AI methods can analyse the geographical spread of the virus and identify the clusters and hot spots. [95] These data can be rendered to detect the vulnerable areas of different regions [96], [97]. AI-powered applications such as contact tracing apps have enabled the monitoring of individuals to identify the risk and predict the future course of action for the disease.
[98], [99] demonstrated the use of ML to analyse the time series using Nonlinear Regressive Network to estimate the spread of the virus, which can facilitate the forecasting for upcoming days. Manual contact tracing requires the involvement of thousands of experienced workers to identify the infected, track them and guide other individuals to keep them away from being exposed to the infected. Whereas AI-powered automatic contact tracing system can be customised to notify an individual if a person was in closer proximity to the infected ones. AI can be used as a tool to identify the transmission chains of the COVID-19 by processing the epidemiological data faster than the traditional medical data reporting system and determine the effective measures to control the spread [100], [101] demonstrated the application of SEIR (Susceptible, Exposed, Infectious, and Recovered) model to scale the pandemic outbreak in different regions with AI.
A 5G patrol robot developed by the Guangzhou Gosunch Robot Company [102] has already been deployed in China to monitor the COVID-19 prevention measures. Equipped with infrared thermometers, the robot is able to scan up to ten people for high temperatures within a 5 metres radius. MIC-770, an IoT edge computer (Intel 8th gen Core I processor, GPU iModule-MIC-75G20) and five high-resolution cameras empower the development of this IoT-based application.
Involving humans in prototype testing increases the risk of contamination. Thus robots can be a safer alternative to humans. A joint initiative of Apple and Google to develop a contract tracing app for the IOS and android platform is on its way. The prototype of this contact tracing application is validated at MIT. The signals were strengthened using robots containing required sensors. It was tested on Bluetooth range [103].
Social distancing is considered one of the most effective ways of limiting the spread of COVID-19. Different AI-enabled and vision-based robotic solutions can also be used to monitor social distancing [104], [105]. A pipeline for a real-time social distance monitoring system is shown in Fig. 4. AI-powered smartphone applications, wearable devices, CCTV cameras can be integrated to build a social distance monitoring system. It should be functioned to warn people in the workplace and public areas if they violate the social distancing rules. A deep learning-based automatic social monitoring system is proposed in [106] which identifies the humans separating them from the background in a surveillance video. That can monitor the social distancing abidance in public places.
Fig. 4.
Real-time social distance monitoring pipeline: (a) Data collection using robots/vision system (b) Processing and inferring using AI (c) Visualisation and feedback.
Patrol robots are fully autonomous or teleoperated mobile robots with great applicability in this COVID-19 time. Recently it has been customised to replace human patrols, especially in risky areas (i.e., high crime areas, highly infected zones). Equipped with high-resolution cameras and the fastest communication modules, they can record live images and report abnormal or suspicious situations and notify them to the proper authorities in the shortest possible time. Patrol robots can autonomously navigate to the nearest charging station, recharge themselves and come back to the serving area; thus they can provide 24/7 monitoring services. In this circumstance, patrol robots have been used during the COVID-19 pandemic to run inspections with the law-enforcing authorities. Besides, they monitor body temperature, facial mask-wearing, and social distancing conditions, and alert the relevant authorities to take real-time initiatives with any occurrence of potential threat like high temperature or absence of facial masks. Moreover, integrated with AI, cloud computing, and big data processing functionalities, they can be employed for real-time monitoring of the situation, autonomous decision making, behavioural control, and interaction. Whenever an abnormal or suspicious event such as the absence of facial masks or high body temperature is detected by the robot, an alert is sent to the relevant authorities to take necessary initiatives to handle the event.
The government of Singapore has deployed a four-legged robot named ‘Spot’ [109] developed by Boston Dynamics to patrol in its local parks to enforce social distancing among the visitors. Spot is teleoperated, and it estimates the number of visitors with the installed cameras and broadcasts a prerecorded message about maintaining safe distances among the visitors.
PGuard, a four-wheeled robot has been deployed in the large streets of Tunisia’s capital to monitor the abidance of the imposed coronavirus lockdown. Equipped with a thermal camera and Lider technology, PGuard approaches the pedestrians, asks reasons for disobeying lockdown, and if necessary, scans their identification documents so that the designated authorities can check those [108]. Table 3 accumulates information about some of these deployed robots.
Table 3.
A summary of notable works on surveillance techniques during the COVID-19 pandemic situation.
| Research | Application | Methodology | Performance |
|---|---|---|---|
| [101] | Simulating the spread of COVID-19 | SEIR Model | No metrics provided |
| [106] | Monitoring social distancing regulations from video | Yolo v3 and Deepsort | mAP: 0.846 |
| [107] | Identifying people without face masks | AI | Accuracy: 96.5% |
| [102] | Monitor body temperatures and face mask regulations using patrol robots and alert authorities if absence of mask is detected | 5G patrol robots powered by MIC-770 computers | Able to simultaneously monitor temperatures of 10 people in a 5 m radius |
| [103] | Contact tracing of COVID-19 infected patients using Android and iOS applications and alert traced contacts of potential infection | Bluetooth | No metrics provided |
| [108] | Monitor COVID-19 lockdown situation, question citizens who are outside and record their identification using a patrol robot | Remotely controlled manually, equipped with thermal imaging camera and LiDAR technology | No metrics provided |
3.4. Telehealthcare services during COVID-19
The field of telemedicine has proven valuable during the COVID-19 crisis. Telerobotics has significantly supported in taking the edge off several arduous tasks of the frontline workers. It has aided in curbing the spread by reducing the close interaction between the patients and healthcare workers. Many novel means of remote monitoring of patients were introduced in this pandemic. It not only favoured controlling the spread but also helped to ensure the delivery of healthcare service to non-COVID patients during this pandemic. Fig. 5 demonstrates different telehealthcare instilled services, notably teleconsultation, telesurgery, teleultrasound, telepresence robots, self-checker services, and AI Chatbots, among others.
Fig. 5.
Telehealthcare services during COVID-19 pandemic.
Many hospitals deployed intelligent chatbots [110], [111], [112] to alleviate the pressure in healthcare departments. Some of these chatbots have rendered great service in attending to the general patients. Certain chatbots with advanced design and working algorithms are capable of recommending immediate measures with effective drug and consultation support on demand of the user.
An interactive robot named CRUZR [113] was developed by the Belgian company ZoraBots, which has been used in hospitals and other areas as a first-line controller amid the coronavirus outbreak. The robot can approach visitors, measure their temperature, and interact with them using one of the 53 languages. It can do repetitive works, help the medical staff to concentrate their works and can learn on the duties.
Authors in [114] proposed an intelligent robot that can perform skin-related diagnosis using its vision system. It can also communicate with the patients about the diagnosis results using voice and word-based outputs. It has cloud-based storage capabilities to promote further telemedicine scopes.
Previously developed telemedicine technologies like [115], robot-nurse Tommy in Italy, helping hand for physiotherapist Robert in Denmark, Robotnik in Valencia, Spain have been supporting the telehealthcare facilities during COVID-19. In [115], an intelligent medical agent is developed for the treatment of insomnia which uses a variety of physiological and environmental sensors to collect users’ details. The agent can transfer the results to a cloud platform to facilitate further examination and telemedicine services by a human doctor. It monitors different vital signs from devices in the patient’s room and allows patients to communicate with the doctors by sending messages. A similar technology [116] was developed in Russia for remote health monitoring of cancer patients. This system incorporates a subsystem to provide emergency situations based on the patients’ health statements and presents the necessary data to the doctors. ROBERT, developed by Life Science Robotics (LSR), is a device having an lightweight KUKA robot integrated helps the physiotherapists in Denmark to mobilise the patients while maintaining social distancing.
In [117], authors studied the feasibility of the teleultrasound examination and consultation amid situations like the COVID-19 pandemic. The conventional method increases the risk of infection as it requires a doctor to perform the ultrasound examination being present in the examination room. To mitigate this risk, a 5G network-based telecontrollable robot-assisted technique has been employed for the remote ultrasound diagnosis for COVID-19 patients. Though chest CT examination is a highly recommended standard COVID-19 diagnosis, ultrasound examination can be considered as an alternation due to the unavailability of the CT examination modalities. Robot-assisted teleultrasound eliminates the risk of contamination from close contact with the patients.
The researchers in telehealthcare services during this pandemic have prospected to deliver remote service opportunities with novel technologies like Robotic teleechography [118] for remote diagnosis of organs like lung, heart and thus protect medical staff from unnecessary interaction.
A robotic tabletop device has been developed by the engineers of Rutgers [119] which facilitates accurate steering of catheters and needles into the tiny blood vessels for drawing blood or delivering drugs and other necessary fluids. Automated blood sampling and analysis require complex visual and motion tracking involving the identification of blood vessels from the surrounding tissue, classification, and estimation of their depth. A robotic device is capable of carrying out these tasks combining artificial intelligence and imaging modalities with minimal supervision, which makes it a suitable tool in situations like the COVID-19 pandemic.
A self-checker service for the COVID-19 is developed by the Centers for Disease Control and Prevention and Microsoft which provides self-assessment services and suggests the next course of action for the users.
The adversities during this COVID-19 pandemic have affected the psychological well-being of humans around the globe resulting in mental stress due to the sudden change of normal lives, like being in isolation and lockdown is not an unusual onset. AI-powered mood booster apps ensure the mental well-being of an individual, even detecting whether the individual is in a depression state or not. Table 4 comprises some of the significant AI and Robotics-driven technologies in telehealthcare during this pandemic.
Table 4.
A summary of notable telehealthcare technologies.
| Research | Application | Methodology | Performance |
|---|---|---|---|
| [110] | Providing telehealthcare service using a chatbot | Artificial Intelligence Markup Language (AIML) | 4.8 on a scale of 5 |
| [111] | Collect data on potential COVID-19 cases using a chatbot | AI chatbot | Survey of usefulness: 92% |
| [117] | Performing teleoperated ultrasound examination with assistance of robots | MGIUS-R3 robotic ultrasound system, communication over 5G network | Tele-ultrasound examination performed successfully from 1479 km away |
| [118] | Performing tele-echography using robots to remotely examine lungs, heart and vascular system | MGIUS-R3 robotic tele-echography system, communication over 5G network | Tele-echography was successfully performed on a patient 700 km away and the patient’ lungs, heart, inferior vena cava and blood vessels in both lower extremities were examined |
| [119] | Developing a robotic system that can insert needles into blood vessels in order to draw blood or deliver drugs and other fluids without human intervention | Recurrent fully convolutional networks used to perform vessel segmentation, classification, and depth estimation on near-infrared (NIR) stereo images and duplex ultrasound (US) images to guide a 6-DOF robotic agent with a 3-DOF end effector | Successful cannulation was performed in an in vivo study performed on 20 rats |
3.5. Delivery and supply chain during COVID-19
In hospitals, doctors and other medical staff need to interact in real-time with patients from a safe distance which includes delivering food and medicine to patients, samples to the lab, and reports to doctors. Intelligent and autonomous delivery robots speed up the movement of medicines, samples, and reports and assist the hospitals in managing the overwhelming amount of activities during the coronavirus pandemic. The deployment of autonomous delivery robots can protect patients and medical staff and help reducing health workers’ workload. Autonomous robots can be integrated into the supply and delivery chain as shown in Fig. 6.
Fig. 6.
Autonomous robots in supply chain and delivery.
The autonomous mobile robot Phollower 100 [120] delivery robot, developed by a Slovakian company Phontoneo, is deployed in hospitals and other healthcare centres for distributing medicines, laundry, and other material to different stations. This robot has a responsive web interface and it can take a payload of 100 kg for carrying and 350 kg for pulling.
Drones are also being used as delivery platforms as they provide three-dimensional modality. Drone-based healthcare service implementation have been very common in this pandemic [121], [122], [123]. The system in [124] delivers goods (food, medical supplies, etc.) to required places with a UAV. This app-based system excels in performing delivery operations to a height from the ground, like a certain floor of a building. It navigates outdoor and locates from the base location of the supplier to the desired client address.
Keenon Robotics [125] provided many hospitals in the COVID-19 affected areas of China with delivery robots. The robots assisted in the operations like transportation of medical supplies, delivery of meals to patients and doctors, and accomplishing other necessary tasks [126]. These robots are furnished with Astra Mini S cameras, LIDAR, infrared, and ultrasonic sensors, and they can carry 10 kg of loads. The robot can deliver goods by following a pre-defined route or using SLAM algorithms.
Techmetics [127] designed a delivery robot Techi Butlers for rendering service in hospitals which include distributing lab samples, medication, hospital supplies. This fleet management system equipped with multiple robots has a payload of 250 kg. Hercules from Chinese company UDI [128] is a robot van equipped with LIDAR, stereo vision cameras, fisheye cameras, redundant satellite navigation systems, and deep-learning algorithms to support the self-driving functionality.
A California-based startup, Nuro [130] has built small autonomous delivery robots with Wheels for delivering medical supplies, food, personal protective equipment (PPE), clean linens, and other supplies to health workers in California without human contact. A company from San Francisco has launched Zipline drones [129] to deliver vaccines, medicines, and personal protective equipment with a work area of 22500 square kilometres and a speed of 100 km per hour. These drones were deployed in Ghana to tackle the COVID pandemic and helped the western African country to respond timely in the crisis. Certain applications of Robots in the field of supply chain systems are summarised in Table 5.
Table 5.
A summary of notable delivery and supply chain systems suitable for use during the COVID-19 pandemic.
| Research | Application | Methodology | Performance |
|---|---|---|---|
| [120] | An autonomous, modular mobile robot that can perform delivery and disinfection tasks | 6 wheeled modular robot with centre axle drive, disinfection operation performed using UV-C light | No metrics provided |
| [122] | Perform monitoring, sanitisation, thermal scanning, face recognition and identification, social distance enforcement and other tasks in COVID-19 hot spots using drones | Swarm robotics, Cloud computing, Edge computing, Fog computing, IoT, AI, Thermal imaging | Capable of covering 2KMs in 10 min |
| [124] | Autonomous delivery using an UAV | Delivery request made using an App, UAV path planning using A* | No metrics provided |
| [127] | Robotic system for performing delivery services in hospitals such as distributing lab samples, medication, hospital supplies etc. | Deliveries made by an autonomous robot with multiple compartments and a touch screen for user interaction | Max speed: 1.5 m/s Payload: 130 lbs |
| [129] | Transportation of suspected COVID-19 samples from remote rural areas to testing labs using drones | Test samples are packed in special biological containers with ice and transported in the bellies of Autonomous drones developed by Zipline | Max speed: 128 km/h Payload:1.75 kg Range:160 km. Deliveries made within 30 min |
3.6. Service automation
Robotic process automation (RPA) [131], also referred to as software robotics, is a technology-based on metaphorical software robots which are used to automate business operations while reducing the intervention of human workers. RPA takes over the monotonous, repetitive and tedious tasks usually done by the frontline workers, thus ensures the use of human resources more effectively. During COVID-19, RPA can be used as an efficient tool to empower health care sectors by building software robots capable of undertaking the job of the health workers or medical staff. Further, RPA ensures improved operational efficiency and scalability while decreasing operating costs and error occurrences so as to provide advanced governance services. RPA has been of assistance in numerous fields as shown in Fig. 7.
Fig. 7.
Key application areas of RPA in COVID-19 pandemic.
RPA has been considerably used in testing and diagnosis during this COVID time. With the rapid spread of Coronavirus, the testing sites experience huge demands which result in the long line of the patients waiting for the test [132]. RPA can be used to accelerate COVID-19 testing up to 90% using attended bots to collect patient data, incorporate into the EMR records of the hospital, record the test results, and sends these records to other departments while eliminating the manual errors and reducing waiting time [133]. A mobile survey of the patients is performed by the hospitals for the initial diagnosis purpose. These data are then automatically managed by RPA without involving any data entry specialists, thus reduced the diagnosis time significantly. RPA combined with AI can be used for the efficient and faster testing of COVID-19 from the CT scans or chest X-ray images while reducing the waiting time of the patients up to 70%. RPA bots ensure 24/7 availability of appointment services for the video consultation by automatically scheduling patient requests [134]. RPA bots can be used to increase the speed of the hiring process by automating the background checks, credential verification, and application data upload into the HR system. After completion of the processing, robots notify the competent volunteers to the relevant department and help them to assign volunteers in job areas.
RPA can contribute to accelerating COVID-19 vaccine development and distribution by managing the collaboration and communication of critical clinical data among the multiple teams or processes to reduce the vaccine development period [135].
For recovery and monitoring, developed RPA systems can do wonders to reduce the workloads from the workers. Screening bots monitor the health condition of the employees and flag of their status in case of any suspicious condition such as high body temperatures, thus allows the relevant authorities to initiate proper actions. RPA bots compile COVID-19 related data from multiple data sources from all over the world, analyse those data, generate insightful daily reports, and provides necessary guidelines on risk management [136].
RPA has great potentiality to be employed in back-office operations.RPA facilitates real-time monitoring of pedestrian traffic flow to initiate risk alerts when traffic flow through public areas is too dense [137]. In a pandemic situation like COVID-19, there is an increased volume of medical supply orders such as hand sanitisers, PPEs, etc. which can be handled efficiently by the unattended RPA bots, reducing pressure on procurement teams and avoiding supply delay or stock-out of critical supplies. Accelerating the onboarding of emergency staff: Bots speed up the new recruitment process by 10x automatically performing the police vetting and checking the previous employment status of the healthcare staff. Rapid registration of patients: RPA bots faster the process of new patient registration by checking the status of the existing registration in the database and providing the history and other information of the existing patients. RPA allows faster processing of digital paperwork while eliminating human error by automatically queuing and managing test-related administrative tasks. Automation helps health organisations to make increasing call volumes easier and quicker by accurate tracing and auditing of payments while incorporating constant policy changes.
3.7. Disinfection
COVID-19 spreads from person to person through close contact respiratory droplet transfer and from contaminated surfaces. Disinfecting the surfaces during this time is essential, although manual disinfection task imposes a very high risk of infection.
Disinfecting robot disinfects designated area with ultraviolet-C (UV-C) light or hydrogen peroxide vapour (HPV). It mitigates the chances of hospital-acquired infections and reduces the cleaning labour wages. The UV-C chemicals work by deactivating the DNA and RNA and HPV kills microorganisms through the oxidative process. Two such robots are demonstrated in Fig. 8.
Fig. 8.
Two types of robots used for disinfection applications.
A Danish company, UVD Robots [138], produce UV-C disinfection robots for patient rooms, corridors, and other units in hospitals. This robot disinfects the surface by decomposing DNA structures of viruses, bacteria, and other types of harmful organic microorganisms with UV light. It manoeuvres in the environment by combining LiDAR technology to generate a map and SLAM to navigate through the paths. It operates in the absence of humans and using motion sensors to sense the presence of humans, it shuts the UV lights. The Bucharest Robot and UVD robots collaboratively can disinfect 7500 square metres in a short time. One of the robots provides information to the patients and the other robot work as a waitress to deliver food.
The Nimbus robot [139], developed by the Scottish company Novoa, disinfects surfaces and rooms with hypochlorous acid that destroys the proteins of the bacteria. It atomises the microburst cleaning solution, an EPA-registered hospital-grade disinfectant and eliminates the disinfectant cloud after cleaning.
The Disinfection service robots Xenex [140] does disinfect operations with high-intensity pulse germicidal UV. It possess the most effective form of UV with higher intensity and wide spectrum. Small duration of required exposure for effective doses can remove the harmful bacteria, viruses, and spores with the patented system of pulsed xenon Full Spectrum UV for room disinfection.
Another UV light-oriented disinfecting robot is the autonomous mobile disinfect robot ‘YOUIBOT’ of Servo Dynamics, Singapore. It adaptively navigates through the SLAM algorithm. Other than the cleaning functionality, it can also monitor temperatures of people [143].
In [141], [142], the authors proposed a Type 1 and Type 2 Fuzzy Logic-based disinfecting robot with wall following behaviours that can operate in complex and uncertain environments. Disinfection drones have also been deployed by many companies. XAG converted its ground robots to aerial drones by replacing the agricultural units with disinfectant sprayers. The aerial sprayer provides great advantages in both coverages of the disinfecting substances and in keeping the human operators at a safe distance [144]. Some other drone assisted disinfecting systems were reported in [145], [146], [147]. Some of the notable forefront innovations for disinfection have been summarised in Table 6.
Table 6.
A summary of robotic systems for disinfection purposes in hospitals and other areas.
| Research | Application | Methodology | Performance |
|---|---|---|---|
| [141] | Development of an autonomous multi robot system to perform disinfection, remote body temperature measurements and other tasks in Field hospitals | Environment mapped using SLAM, kinect used as thermal camera to monitor body temperature | No metrics provided |
| [142] | Development of a wall following robot for disinfection in unknown environments | Type-1 and type-2 Fuzzy Logic System (FLS) | Average lateral error: 4.9 cm for type-2 FLS |
| [139] | Autonomous robotic system for disinfecting hospital rooms and kill pathogens that cause healthcare-associated infections (HAIs) including COVID-19 | Atomising system used to spray Hypochlorous acid (HOCl) disinfection solution on surfaces for cleaning and disinfection, filtration and dehumidifying technology used to remove solution from air and other surfaces after cleaning | Capable of cleaning a hospital room in 30 min |
| [143] | Autonomous robotic system for disinfection and remote monitoring body temperature | Robot navigation using SLAM, disinfection using UV light | No metrics provided |
| [144] | Autonomous disinfection operation using drones | Spray disinfectants from drones | No metrics provided |
3.8. Accelerating research and drug development
The COVID-19 catastrophe demands extensive research on viruses to develop faster and effective drug and other remedies to the disease. Researchers and healthcare professionals face difficulties compiling a massive volume of COVID-19 related data to gain necessary insights into the treatment. AI-based solutions speed up the process providing faster access to the relevant research papers and other documents. Moreover, they provide a way to extract medical information from the unstructured text using natural language-based query processing capabilities. A machine learning-enabled search platform is launched by the Amazon web service (AWS) which contributes to easier and quicker access of more than 128,000 research papers and other materials [148].
Machine learning models such as Bayesian ML models and random forest algorithm have already been proven effective in virus molecule scoring process [149], [150]. AI-driven technologies have been brought forth in the formulation of potential drug development for COVID-19 treatment [151], [152], [153]. In [154], the authors reviewed the literature about ML and AI technologies for biomarker discovery, disease characterisation and potential target drug identification in COVID-19. DeepMind [155] has predicted the protein structure of the SARS-CoV-2 virus responsible for causing COVID-19 using deep learning methods.
Machine learning can help to assess the potential candidate drugs in two ways — it can create biomedical knowledge graphs; otherwise, it can build models to predict drug and viral protein interaction [156]. A biomedical knowledge graph that connects biomedical entities inferring their relationship is constructed in [157] using natural language processing techniques. The researchers use a similar graph to identify a potential candidate drug (Baricitinib) for COVID-19 [158]. Scientists also rely on machine learning models to predict drug-target interactions (DTIs). DTI helps to formulate how the candidate drugs interact with the virus protein. Neural networks trained on large DTIs are used to chose a subset of drug candidates that can restrain the virus’s protein most significantly [159]. A neural network-based end-to-end framework named NeoDTI is developed in [160] to predict the DTIs accurately by interpreting the knowledge graph. A potential therapeutic agent for COVID-19 is in its clinical trial which is developed using models learned on similar graph-network [161]. AI and Machine learning techniques have also contributed to the search for potential existing drugs for COVID-19 treatment. Several review works summarised the notable AI applications that have been adopted for drug-repurposing, drug-repositioning and exploring potential drug-target relationship [162], [163], [164].
A wide range of tools for the vaccine research of COVID-19 are being optimised with different AI algorithms [165], [166], [167]. Several applications of AI in accelerating research and drug development to combat the COVID-19 pandemic are summarised in Table 7.
Table 7.
A summary of some notable works in accelerating research and drug development to combat the COVID-19 pandemic.
| Research | Application | Methodology | Performance |
|---|---|---|---|
| [155] | Protein structure prediction of the SARS-CoV-2 virus | AlphaFold | No metrics provided |
| [158] | Identification of a potential drug for treatment of COVID-19 patients | BenevolentAI’s knowledge graph | Baricitinib identified as potential medicine |
| [159] | Screening potential drug candidates for COVID-19 | Deep fully connected neural network (DFCNN) | A number of commercially available drugs were screened |
| [160] | Predicting drug-target interaction (DTI) | Deep learning | 3.5% better performance in terms of AUPR compared to the second best method (DTINet) |
| [161] | Identification of potential drug candidates for treatment of COVID-19 | Combination of machine learning and statistical approach | CVL218 identified as a potential drug with an inhibition rate of 35.16% at 3 M concentration |
4. Future directions
The advent of highly anticipated vaccines has revitalised the pandemic-stricken human race with a fresh breeze of hope. But without ensuring the far and wide distribution and availability of the vaccines, the danger to humankind persists. Involving automation with Robotics and AI-empowered technologies can accelerate the vaccine production, distribution and vaccination process to a large extent. The novel innovations in this field have made it apparent how these technological responses can reinforce the outreach of the vaccine. The emerging field of urban robotics was proven very valuable during the pandemic. So it is quite sure that they will be amply contributing to restructure the linkage of global cities and epidemiology for future crisis response. In many areas, the abrupt rise in the case often exhausts the hospital workforce and attending to the overwhelming number of patients gets more challenging and sometimes infeasible. Service robots with multiple functionalities can be deployed there to aid doctors and healthcare workers. The reformation of biosecurity control measures and their hard and fast implementation should be monitored circumspectly as it was speculated at the beginning of the outbreak that the COVID-19 Coronavirus was evolved from a lab entity. So, supervision of these fields with more intelligent technologies should be explored with more concern.
The Coronavirus strains have mutated in a varied way at different places. Several mutations have been identified as more contagious and deadlier than the others. Kent, UK (B.1.1.7 variant), South Africa (B.1.351 variant), Brazil (B.1.1.28.1 or P.1 variant), and much recently India (B.1.617.2 or Delta variant) are detected as the riskiest variants of Coronavirus. Gene sequencing the samples is the only means to diagnose the new strains. So, novel AI and ML-driven tools should be sought to make the research for identifying risky strains easier. Machine Learning tools can be used to conduct predictive analysis of future virus mutations. In addition to predicting possible mutations, such tools can also be used to analyse the effectiveness of currently available medication on potential future variants and develop medicines and vaccines that are effective against them. This can also facilitate the regulatory management to take proactive measures before the resurgence of crisis situation. Artificial Intelligence can be used to analyse the history and spread of the Coronavirus to predict future outbreaks that may occur. In addition, the existing infrastructure can be analysed using AI tools to estimate the preparedness and response capabilities to such future outbreaks. Moreover, the entire history of the pandemic and previous pandemics can be analysed to prepare guidelines for future pandemics that may occur.
A significant portion of literature has focused on detecting COVID-19 positive cases from chest CT scans, X-rays, and symptoms using artificial intelligence and deep learning-based technologies. These techniques are heavily reliant on huge amounts of data, of which there is a lack of. Thus, it is necessary to facilitate the development of public and open-source datasets consisting of medical images and clinical symptoms. These datasets must be annotated by doctors, researchers, and other experts in the field. This will also allow many researchers, who do not currently have access to such resources, to contribute to this endeavour to develop quick and accurate methods for COVID-19. However, constructing such large-scale corpuscles is a time-consuming process. In the absence of large datasets, state-of-the-art algorithms such as one-shot learning [168], zero-shot learning [169], deep metric learning [170] should also be explored to developed accurate models. These algorithms can develop classification models from very few training examples and even from just one training example. Robotics and AI-based technologies can be implemented to allow automatic checking of body temperature and authorisation/prohibition of entry in many public places such as supermarkets, airports, parks, theatres, and restaurants. Nowadays, most public places include security cameras for surveillance and AI-based technologies that can easily be integrated to monitor and enforce social distancing and face mask regulations. In addition, the behaviour and symptoms of people can also be analysed to identify potential cases. During the design phase, it is necessary to ensure that these systems are designed in a user-friendly and non-threatening way. It is also essential to ensure that privacy issues do not arise. Additionally, many existing robotics systems can be repurposed for assisting healthcare workers and caring for patients. In the field of telehealthcare and telemedicine services, chatbots have seen an influx of applications. State-of-the-art language models like the GPT-3 [171] can be incorporated to develop chatbots with near human-like conversation capabilities. In order to reduce mass human contact, it is necessary to automate more and more industries and introduce robotic systems in more stages of the delivery and supply chain. Although the entire world’s attention is currently on the Coronavirus, it must be ensured that other diseases are not given any less importance. The breakout of another deadly disease amidst the coronavirus pandemic will pose a serious threat to humanity.
5. Conclusion
AI and Robotics are being used in many points of services for COVID-19 to a considerable extent. This paper thoroughly highlights the contributions and probable fields for these technologies during the pandemic. The different norms in the health sector and their task operations are also distinguished in this paper. For COVID-19 detection and diagnosis, the newly found AI-driven methods have been aiding to lessen the pressure on conventional methods. The one concern that persists in the AI-based new solutions is that they are often vulnerable to be less accurate results than conventional methods. In risk assessment and proper triaging of COVID-19 patients, deep learning algorithms are being used to build prediction models to prognosticate patients’ conditions. Similarly, social monitoring, delivery and supply chain, and disinfection operations during this pandemic are being greatly facilitated by many robot-operated applications and technologies. Telehealthcare is another expedient solution for this kind of situation. However, the cost of operations and production limitations are creating a bar in their way to be more widely adopted in underdeveloped areas. Many AI-empowered solutions like telepsychiatry, telemental health services, virtual reality (VR), chatbots, companion bots have addressed the issues that arose in mental health concerns during this pandemic. However, these services still have scopes to improve the serviceable functionalities to a greater extent by standardising the infrastructure.
Although numerous high-performing systems have been developed, many of them failed to go beyond the prototyping phase into public deployment. Widespread testing and isolation of infected patients are crucial for limiting the spread of the virus. While many highly accurate AI-based diagnosis systems have been proposed, they have not seen any real-world usage in most cases. Scepticism and a lack of faith regarding such AI and robotics systems can be observed among healthcare personnel and the general public. Moreover, the lack of mass public trial means that the general performance of these systems is not fully known. The reluctance of people to maintain COVID-19 regulations has been an issue throughout the pandemic. Hence it is also a matter of concern whether people will cater to the imposed restrictions if a robotic system is used in place of a human being. Frequent mutations of the SARS-CoV-2 virus have been a major headache in controlling the pandemic rendering existing medicines and technologies less effective. Therefore it is necessary to update existing technologies, medicines, and vaccines continuously. While developing new systems, it is essential to ensure that these systems are capable of adapting to the ever-changing nature of the Coronavirus. Otherwise, these developments, while being highly potential initially, will become obsolete soon.
From detecting COVID-19 to limiting the spread, reducing the workloads from health workers to streamlining the communicative operations, AI and robotics technologies have adequately catered to public health needs. AI and Robotics technologies have greatly accelerated the research for the development of the COVID vaccine. Several AI-empowered big data analytical tools were used to process the stream of information about the latest findings and investigation results. UAV and RPA platforms have been deployed in vaccine distribution and management and served the purpose very aptly. The responses of technological fields to the recurrent challenges of this pandemic can be a great guiding model for any future catastrophic disaster. The strenuous efforts of the professionals of these fields have lead the outreach of the operations to every domain of the systems. It is expected that the AI and robotics technologies discussed in this paper will significantly assist humankind in combating the COVID-19 pandemic and future disasters that may arise.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors would like to thank Musabbir Ahmed Arrafi from the Department of Robotics and Mechatronics Engineering, University of Dhaka for his contribution to draw the diagrams.
Biographies

Sujan Sarker received the B.S. and M.S. degrees from the Department of Computer Science and Engineering, University of Dhaka, Dhaka, Bangladesh, in 2013 and 2017, respectively. He is currently a Lecturer with the Department of Robotics and Mechatronics Engineering, University of Dhaka. His current research interests include sensor networks, participatory sensing, mobile crowdsourcing, human robot interaction, and swarm robotics. Mr. Sarker is a member of the IEEE Computer Society and the IEEE Robotics and Automation Society.

Lafifa Jamal received her B.Sc. and M.Sc. degrees from the Department of Computer Science, University of Dhaka, Bangladesh. She obtained her Ph.D. degree in Reversible Logic Synthesis from the same university. She is now working as a Professor in the Department of Robotics and Mechatronics Engineering, University of Dhaka, Bangladesh. Her research interest includes Robotics and Intelligent Systems, Internet of Things, Reversible Logic Synthesis, Quantum Computing, Gender and Diversity. She has published a good number of research papers in international conferences and journals. She is a senior member of IEEE. She is a member of IEEE Robotics and Automation Society, IEEE Computer Society, IEEE Women in Engineering, Association for Computing Machinery (ACM), American Association for the Advancement of Science (AAAS), Robotics Society India (RSI), Internet Society (ISOC), Bangladesh Computer Society (BCS) and Bangladesh Women in Technology (BWIT).

Syeda Faiza Ahmed is currently a student of the Department of Robotics and Mechatronics Engineering, University of Dhaka. Her current research interests include Robotics and Intelligent Systems, Internet of Things and Activity Recognition.

Niloy Irtisam is currently a student of the Department of Robotics and Mechatronics Engineering, University of Dhaka. His current research interests include Robotics and Intelligent Systems, Internet of Things, Fog Robotics and Swarm Robotics.
References
- 1.Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Bio Med.: Atenei Parm. 2020;91(1):157. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu Y., Gayle A.A., Wilder-Smith A., Rocklöv J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J. Travel Med. 2020:1–4. doi: 10.1093/jtm/taaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meyerowitz-Katz G., Merone L. A systematic review and meta-analysis of published research data on COVID-19 infection fatality rates. Int. J. Infect. Dis. 2020;101:138–148. doi: 10.1016/j.ijid.2020.09.1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mehra M., Sharma R., Devi D. A brief review on epidemic to pandemic: Novel corona virus (COVID-19) J. Xian Univ. Archit. Technol. 2020;XII(IV):3795–3803. [Google Scholar]
- 5.Worldometer . 2021. Last Accessed: 27 August 2021. [link]. URL https://www.worldometers.info/coronavirus/ [Google Scholar]
- 6.W.H. Organization, et al. World Health Organization; 2020. Laboratory Testing for Coronavirus Disease (COVID-19) in Suspected Human Cases: Interim Guidance, 19 March 2020: Tech. rep. Last Accessed: 20 March 2021. [Google Scholar]
- 7.Sümen A., Adibelli D. The effect of coronavirus (COVID-19) outbreak on the mental well-being and mental health of individuals. Perspect. Psychiatr. Care. 2020;57(3):1041–1051. doi: 10.1111/ppc.12655. [DOI] [PubMed] [Google Scholar]
- 8.Women U. 2021. The shadow pandemic: Violence against women during COVID-19. Last Accessed: 20 March 2021. URL https://www.unwomen.org/en/news/in-focus/in-focus-gender-equality-in-covid-19-response/violence-against-women-during-covid-19. [Google Scholar]
- 9.Tavakoli M., Carriere J., Torabi A. Robotics, smart wearable technologies, and autonomous intelligent systems for healthcare during the COVID-19 pandemic: An analysis of the state of the art and future vision. Adv. Intell. Syst. 2020;2(7) [Google Scholar]
- 10.Albahri O., Zaidan A., Albahri A., Zaidan B., Abdulkareem K.H., Al-qaysi Z., Alamoodi A., Aleesa A., Chyad M., Alesa R., Kem L., Lakulu M.M., Ibrahim A., Rashid N.A. Systematic review of artificial intelligence techniques in the detection and classification of COVID-19 medical images in terms of evaluation and benchmarking: Taxonomy analysis, challenges, future solutions and methodological aspects. J. Infect. Public Health. 2020;13(10):1381–1396. doi: 10.1016/j.jiph.2020.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hashmi H.A.S., Asif H.M. Early detection and assessment of covid-19. Front. Med. 2020;7:311. doi: 10.3389/fmed.2020.00311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gong Z., Jiang S., Meng Q., Ye Y., Li P., Xie F., Zhao H., Lv C., Wang X., Liu X. SHUYU robot: An automatic rapid temperature screening system. Chin. J. Mech. Eng. 2020;33(1):1–4. [Google Scholar]
- 13.Huang H., Chai P., Ehmke C., Merewether G., Dadabhoy F., Feng A., Li C., Thomas A., da Silva M., Raibert M., et al. Agile mobile robotic platform for contactless vital signs monitoring. TechRxiv. 2020;10 doi: 10.34133/2022/9780497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li G., Xiong Z., Zhou H., Xie J., Chen W., Zhou M., Zhu Z., Zhou G., Liu J. Value of CT application in the screening, diagnosis, and treatment of COVID-19. J. Cent. South Univ. (Med. Sci.) 2020;45(3) doi: 10.11817/j.issn.1672-7347.2020.200132. [DOI] [PubMed] [Google Scholar]
- 15.Ozsahin I., Sekeroglu B., Musa M.S., Mustapha M.T., Uzun Ozsahin D. Review on diagnosis of COVID-19 from chest CT images using artificial intelligence. Comput. Math. Methods Med. 2020;2020 doi: 10.1155/2020/9756518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Song J., Wang H., Liu Y., Wu W., Dai G., Wu Z., Zhu P., Zhang W., Yeom K.W., Deng K. End-to-end automatic differentiation of the coronavirus disease 2019 (COVID-19) from viral pneumonia based on chest CT. Eur. J. Nucl. Med. Mol. Imaging. 2020;47(11):2516–2524. doi: 10.1007/s00259-020-04929-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xie J., Wang M., Liu R. Intelligent Systems and Methods to Combat Covid-19. Springer; 2020. Deep learning-based COVID-19 diagnosis and trend predictions; pp. 57–64. [Google Scholar]
- 18.Zhou L., Li Z., Zhou J., Li H., Chen Y., Huang Y., Xie D., Zhao L., Fan M., Hashmi S., et al. A rapid, accurate and machine-agnostic segmentation and quantification method for CT-based COVID-19 diagnosis. IEEE Trans. Med. Imaging. 2020;39(8):2638–2652. doi: 10.1109/TMI.2020.3001810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Loey M., Manogaran G., Khalifa N.E.M. A deep transfer learning model with classical data augmentation and cgan to detect covid-19 from chest ct radiography digital images. Neural Comput. Appl. 2020:1–13. doi: 10.1007/s00521-020-05437-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ardakani A.A., Kanafi A.R., Acharya U.R., Khadem N., Mohammadi A. Application of deep learning technique to manage COVID-19 in routine clinical practice using CT images: Results of 10 convolutional neural networks. Comput. Biol. Med. 2020;121 doi: 10.1016/j.compbiomed.2020.103795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khadidos A., Khadidos A.O., Kannan S., Natarajan Y., Mohanty S.N., Tsaramirsis G. Analysis of COVID-19 infections on a CT image using DeepSense model. Front. Public Health. 2020;8:751. doi: 10.3389/fpubh.2020.599550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pham T.D. A comprehensive study on classification of COVID-19 on computed tomography with pretrained convolutional neural networks. Sci. Rep. 2020;10(1):1–8. doi: 10.1038/s41598-020-74164-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang Z., Liu X., Wang R., Zhang M., Zeng X., Liu J., Yang Y., Liu X., Zheng H., Liang D., et al. FaNet: fast assessment network for the novel coronavirus (COVID-19) pneumonia based on 3D CT imaging and clinical symptoms. Appl. Intell. 2020:1–12. doi: 10.1007/s10489-020-01965-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li L., Qin L., Xu Z., Yin Y., Wang X., Kong B., Bai J., Lu Y., Fang Z., Song Q., et al. Artificial intelligence distinguishes COVID-19 from community acquired pneumonia on chest CT. Radiology. 2020;296(2):E65–-E71. doi: 10.1148/radiol.2020200905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang S.-H., Govindaraj V.V., Górriz J.M., Zhang X., Zhang Y.-D. Covid-19 classification by FGCNet with deep feature fusion from graph convolutional network and convolutional neural network. Inf. Fusion. 2021;67:208–229. doi: 10.1016/j.inffus.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mantas J., et al. The Importance of Health Informatics in Public Health During a Pandemic, Vol. 272. IOS Press; 2020. Setting up an easy-to-use machine learning pipeline for medical decision support: A case study for COVID-19 diagnosis based on deep learning with CT scans; p. 13. [DOI] [PubMed] [Google Scholar]
- 27.Salman F.M., Abu-Naser S.S. Expert system for COVID-19 diagnosis. Int. J. Acad. Inf. Syst. Res. 2020;4(3):1–13. [Google Scholar]
- 28.Mei X., Lee H.-C., Diao K.-y., Huang M., Lin B., Liu C., Xie Z., Ma Y., Robson P., Chung M., Bernheim A., Mani V., Calcagno C., Li K., Li S., Shan H., Lv J., Zhao T., Xia J., Yang Y. Artificial intelligence–enabled rapid diagnosis of patients with COVID-19. Nat. Med. 2020:1–5. doi: 10.1038/s41591-020-0931-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lagos-Ortiz K., Jácome-Murillo E., Aguirre-Munizaga M., Medina-Moreira J. International Conference on Technologies and Innovation. Springer; 2020. Analysis of the services generated through mobile applications for an accurate diagnosis of epidemiological metrics related to Covid-19; pp. 151–165. [Google Scholar]
- 30.Rao A.S.S., Vazquez J.A. Identification of COVID-19 can be quicker through artificial intelligence framework using a mobile phone–based survey when cities and towns are under quarantine. Infect. Control Hosp. Epidemiol. 2020;41(7):826–830. doi: 10.1017/ice.2020.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang Y., Lure F.Y., Miao H., Zhang Z., Jaeger S., Liu J., Guo L. Using artificial intelligence to assist radiologists in distinguishing COVID-19 from other pulmonary infections. J. X-Ray Sci. Technol. 2020;29(1):1–17. doi: 10.3233/XST-200735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sotoudeh H., Tabatabaei M., Tasorian B., Tavakol K., Sotoudeh E., Moini A.L. Artificial intelligence empowers radiologists to differentiate pneumonia induced by COVID-19 versus influenza viruses. Acta Inform. Med. 2020;28(3):190. doi: 10.5455/aim.2020.28.190-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Qjidaa M., Ben-Fares A., Mechbal Y., Amakdouf H., Maaroufi M., Alami B., Qjidaa H. 2020 International Conference on Intelligent Systems and Computer Vision (ISCV) IEEE; 2020. Development of a clinical decision support system for the early detection of COVID-19 using deep learning based on chest radiographic images; pp. 1–6. [Google Scholar]
- 34.Chiu W.H.K., Vardhanabhuti V., Poplavskiy D., Yu P.L.H., Du R., Yap A.Y.H., Zhang S., Fong A.H.-T., Chin T.W.-Y., Lee J.C.Y., et al. Detection of COVID-19 using deep learning algorithms on chest radiographs. J. Thorac. Imaging. 2020;35(6):369–376. doi: 10.1097/RTI.0000000000000559. [DOI] [PubMed] [Google Scholar]
- 35.Buschman H. 2021. Artificial intelligence enables rapid COVID-19 lung imaging analysis at UC San Diego health. Last Accessed: 17 January 2021. URL https://health.ucsd.edu/news/releases/Pages/2020-04-07-artificial-intelligence-enables-rapid-covid-19-lung-imaging-analysis.aspx. [Google Scholar]
- 36.Kongmanee J., Thanapattheerakul T. CSBio’20: Proceedings of the Eleventh International Conference on Computational Systems-Biology and Bioinformatics. 2020. Fine-tuning a lightweight convolutional neural networks for COVID-19 diagnosis; pp. 101–103. [Google Scholar]
- 37.Haritha D., Swaroop N., Mounika M. 2020 5th International Conference on Computing, Communication and Security (ICCCS) IEEE; 2020. Prediction of COVID-19 cases using CNN with X-rays; pp. 1–6. [Google Scholar]
- 38.Gupta A.K., Sharma M., Sharma A., Menon V. A study on SARS-CoV-2 (COVID-19) and machine learning based approach to detect COVID-19 through X-Ray images. Int. J. Image Graph. 2020 [Google Scholar]
- 39.Tiwari M., Tiwari T., Kassab M., Roy A.N., Edeh D.C., Onyema M. Detection of coronavirus disease in human body using convolutional neural network. Int. J. Adv. Sci. Technol. 2020;29(8):2861–2866. [Google Scholar]
- 40.Elgendi M., Nasir M.U., Tang Q., Fletcher R.R., Howard N., Menon C., Ward R., Parker W., Nicolaou S. The performance of deep neural networks in differentiating chest X-rays of COVID-19 patients from other bacterial and viral pneumonias. Front. Med. 2020;7:550. doi: 10.3389/fmed.2020.00550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Al-antari M.A., Hua C.-H., Bang J., Lee S. Fast deep learning computer-aided diagnosis of COVID-19 based on digital chest x-ray images. Appl. Intell. 2020:1–18. doi: 10.1007/s10489-020-02076-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Padma T., Kumari C.U. 2020 International Conference on Smart Electronics and Communication (ICOSEC) IEEE; 2020. Deep learning based chest X-Ray image as a diagnostic tool for COVID-19; pp. 589–592. [Google Scholar]
- 43.Brunese L., Martinelli F., Mercaldo F., Santone A. Machine learning for coronavirus covid-19 detection from chest x-rays. Procedia Comput. Sci. 2020;176:2212–2221. doi: 10.1016/j.procs.2020.09.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shankar K., Perumal E. A novel hand-crafted with deep learning features based fusion model for COVID-19 diagnosis and classification using chest X-ray images. Complex Intell. Syst. 2020:1–17. doi: 10.1007/s40747-020-00216-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pham T.D. Classification of COVID-19 chest X-rays with deep learning: new models or fine tuning? Health Inf. Sci. Syst. 2021;9(1):1–11. doi: 10.1007/s13755-020-00135-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yasar H., Ceylan M. A new deep learning pipeline to detect Covid-19 on chest X-ray images using local binary pattern, dual tree complex wavelet transform and convolutional neural networks. Appl. Intell. 2020:1–24. doi: 10.1007/s10489-020-02019-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gupta A., Gupta S., Katarya R., et al. InstaCovNet-19: A deep learning classification model for the detection of COVID-19 patients using Chest X-ray. Appl. Soft Comput. 2020 doi: 10.1016/j.asoc.2020.106859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Al-Falluji R.A., Katheeth Z.D., Alathari B. Automatic detection of COVID-19 using Chest X-Ray images and modified ResNet18-based convolution neural networks. Comput. Mater. Contin. 2021:1301–1313. [Google Scholar]
- 49.Chowdhury M.E., Rahman T., Khandakar A., Mazhar R., Kadir M.A., Mahbub Z.B., Islam K.R., Khan M.S., Iqbal A., Al Emadi N., et al. Can AI help in screening viral and COVID-19 pneumonia? IEEE Access. 2020;8:132665–132676. [Google Scholar]
- 50.Sharma A., Rani S., Gupta D. Artificial intelligence-based classification of chest X-ray images into COVID-19 and other infectious diseases. Int. J. Biomed. Imaging. 2020;2020:91916–91923. doi: 10.1155/2020/8889023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Alqudah A.M., Qazan S., Alquran H., Qasmieh I.A., Alqudah A. COVID-19 detection from x-ray images using different artificial intelligence hybrid models. Jordan J. Electr. Eng. 2020;6(6):168. [Google Scholar]
- 52.Rajaraman S., Antani S. Weakly labeled data augmentation for deep learning: A study on covid-19 detection in chest x-rays. Diagnostics. 2020;10(6):358. doi: 10.3390/diagnostics10060358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ouchicha C., Ammor O., Meknassi M. CVDNet: A novel deep learning architecture for detection of coronavirus (Covid-19) from chest x-ray images. Chaos Solitons Fractals. 2020;140 doi: 10.1016/j.chaos.2020.110245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wehbe R.M., Sheng J., Dutta S., Chai S., Dravid A., Barutcu S., Wu Y., Cantrell D.R., Xiao N., Allen B.D., et al. DeepCOVID-XR: an artificial intelligence algorithm to detect COVID-19 on chest radiographs trained and tested on a large US clinical data set. Radiology. 2021;299(1):E167–E176. doi: 10.1148/radiol.2020203511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Civit-Masot J., Luna-Perejón F., Domínguez Morales M., Civit A. Deep learning system for COVID-19 diagnosis aid using X-ray pulmonary images. Appl. Sci. 2020;10(13):4640. [Google Scholar]
- 56.Zhang R., Tie X., Qi Z., Bevins N.B., Zhang C., Griner D., Song T.K., Nadig J.D., Schiebler M.L., Garrett J.W., et al. Diagnosis of coronavirus disease 2019 pneumonia by using chest radiography: Value of artificial intelligence. Radiology. 2021;298(2):E88–E97. doi: 10.1148/radiol.2020202944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Toğaçar M., Ergen B., Cömert Z. COVID-19 detection using deep learning models to exploit Social Mimic Optimization and structured chest X-ray images using fuzzy color and stacking approaches. Comput. Biol. Med. 2020;121 doi: 10.1016/j.compbiomed.2020.103805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hassantabar S., Ahmadi M., Sharifi A. Diagnosis and detection of infected tissue of COVID-19 patients based on lung X-ray image using convolutional neural network approaches. Chaos Solitons Fractals. 2020;140 doi: 10.1016/j.chaos.2020.110170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Omoniyi T., Alabere H., Sule E. Journal of Physics: Conference Series, Vol. 1734. IOP Publishing; 2021. Diagnosis of COVID-19 using artificial intelligence based model. [Google Scholar]
- 60.Meng L., Li R. Progress of artificial intelligence diagnosis and prognosis technology for COVID-19 medical imaging. J. Image Graph. 2020:2058–2067. [Google Scholar]
- 61.Chen Y., Jiang G., Li Y., Tang Y., Xu Y., Ding S., Xin Y., Lu Y. A survey on artificial intelligence in chest imaging of COVID-19. BIO Integr. 2020;1(3):137–146. [Google Scholar]
- 62.Kamil M.Y. A deep learning framework to detect Covid-19 disease via chest X-ray and CT scan images. Int. J. Electr. Comput. Eng. 2021;11(1):2088–8708. [Google Scholar]
- 63.Vinod D.N., Prabaharan S. Data science and the role of artificial intelligence in achieving the fast diagnosis of Covid-19. Chaos Solitons Fractals. 2020;140 doi: 10.1016/j.chaos.2020.110182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nath M.K., Kanhe A., Mishra M. 2020 IEEE 5th International Conference on Computing Communication and Automation (ICCCA) IEEE; 2020. A novel deep learning approach for classification of COVID-19 images; pp. 752–757. [Google Scholar]
- 65.Hassan A., Shahin I., Alsabek M.B. 2020 International Conference on Communications, Computing, Cybersecurity, and Informatics (CCCI) IEEE; 2020. Covid-19 detection system using recurrent neural networks; pp. 1–5. [Google Scholar]
- 66.Laguarta J., Hueto F., Subirana B. COVID-19 artificial intelligence diagnosis using only cough recordings. IEEE Open J. Eng. Med. Biol. 2020;1:275–281. doi: 10.1109/OJEMB.2020.3026928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Imran A., Posokhova I., Qureshi H.N., Masood U., Riaz M.S., Ali K., John C.N., Hussain M.I., Nabeel M. AI4COVID-19: AI enabled preliminary diagnosis for COVID-19 from cough samples via an app. Inform. Med. Unlocked. 2020;20 doi: 10.1016/j.imu.2020.100378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Güemes A., Ray S., Aboumerhi K., Desjardins M.R., Kvit A., Corrigan A.E., Fries B., Shields T., Stevens R.D., Curriero F.C., et al. A syndromic surveillance tool to detect anomalous clusters of COVID-19 symptoms in the United States. Sci. Rep. 2021;11(1):1–11. doi: 10.1038/s41598-021-84145-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nguyen T., Zoëga Andreasen S., Wolff A., Duong Bang D. From lab on a chip to point of care devices: The role of open source microcontrollers. Micromachines. 2018;9(8):403. doi: 10.3390/mi9080403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Nguyen T., Duong Bang D., Wolff A. 2019 novel coronavirus disease (COVID-19): paving the road for rapid detection and point-of-care diagnostics. Micromachines. 2020;11(3):306. doi: 10.3390/mi11030306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Taha B.A., Al Mashhadany Y., Hafiz Mokhtar M.H., Dzulkefly Bin Zan M.S., Arsad N. An analysis review of detection coronavirus disease 2019 (COVID-19) based on biosensor application. Sensors. 2020;20(23):6764. doi: 10.3390/s20236764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wong C.K., Ho D.T.Y., Tam A.R., Zhou M., Lau Y.M., Tang M.O.Y., Tong R.C.F., Rajput K.S., Chen G., Chan S.C., et al. Artificial intelligence mobile health platform for early detection of COVID-19 in quarantine subjects using a wearable biosensor: protocol for a randomised controlled trial. BMJ Open. 2020;10(7) doi: 10.1136/bmjopen-2020-038555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Orozco-del Castillo M., Novelo-Cruz R., Hernández-Gómez J., Mena-Zapata P., Brito-Borges E., Álvarez-Pacheco A., García-Gutiérrez A., Yáñez-Casas G. International Congress of Telematics and Computing. Springer; 2020. Fuzzy logic-based COVID-19 and other respiratory conditions pre-clinical diagnosis system; pp. 402–419. [Google Scholar]
- 74.DeCaprio D., Gartner J., McCall C.J., Burgess T., Garcia K., Kothari S., Sayed S. Building a COVID-19 vulnerability index. J. Med. Artif. Intell. 2020;3:1–10. [Google Scholar]
- 75.Harmon S.A., Sanford T.H., Xu S., Turkbey E.B., Roth H., Xu Z., Yang D., Myronenko A., Anderson V., Amalou A., et al. Artificial intelligence for the detection of COVID-19 pneumonia on chest CT using multinational datasets. Nature Commun. 2020;11(1):1–7. doi: 10.1038/s41467-020-17971-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Leventhal R. 2021. Care management for the COVID-19 vulnerable: Medical home network surges forward. Last Accessed: 17 January 2021. URL https://medicalhomenetwork.org/press/care-management-for-the-covid-19-vulnerable-medical-home-network-surges-forward. [Google Scholar]
- 77.Lessmann N., Sánchez C.I., Beenen L., Boulogne L.H., Brink M., Calli E., Charbonnier J.-P., Dofferhoff T., van Everdingen W.M., Gerke P.K., et al. Automated assessment of COVID-19 reporting and data system and chest CT severity scores in patients suspected of having COVID-19 using artificial intelligence. Radiology. 2021;298(1):E18–E28. doi: 10.1148/radiol.2020202439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Xiao L.-s., Li P., Sun F., Zhang Y., Xu C., Zhu H., Cai F.-Q., He Y.-L., Zhang W.-F., Ma S.-C., et al. Development and validation of a deep learning-based model using computed tomography imaging for predicting disease severity of coronavirus disease 2019. Front. Bioeng. Biotechnol. 2020;8:898. doi: 10.3389/fbioe.2020.00898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhu J., Shen B., Abbasi A., Hoshmand-Kochi M., Li H., Duong T.Q. Deep transfer learning artificial intelligence accurately stages COVID-19 lung disease severity on portable chest radiographs. PLoS One. 2020;15(7) doi: 10.1371/journal.pone.0236621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Abdulaal A., Patel A., Charani E., Denny S., Mughal N., Moore L. Prognostic modeling of COVID-19 using artificial intelligence in the United Kingdom: model development and validation. J. Med. Internet Res. 2020;22(8) doi: 10.2196/20259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Meng L., Dong D., Li L., Niu M., Bai Y., Wang M., Qiu X., Zha Y., Tian J. A deep learning prognosis model help alert for COVID-19 patients at high-risk of death: A multi-center study. IEEE J. Biomed. Health Inf. 2020;24(12):3576–3584. doi: 10.1109/JBHI.2020.3034296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ko H., Chung H., Kang W.S., Park C., Kim S.E., Chung C.R., Ko R.E., Lee H., Seo J.H., Choi T.-Y., et al. An artificial intelligence model to predict the mortality of COVID-19 patients at hospital admission time using routine blood samples: Development and validation of an ensemble model. J. Med. Internet Res. 2020;22(12) doi: 10.2196/25442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mushtaq J., Pennella R., Lavalle S., Colarieti A., Steidler S., Martinenghi C.M., Palumbo D., Esposito A., Rovere-Querini P., Tresoldi M., et al. Initial chest radiographs and artificial intelligence (AI) predict clinical outcomes in COVID-19 patients: analysis of 697 Italian patients. Eur. Radiol. 2020:1–10. doi: 10.1007/s00330-020-07269-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Muhammad L., Islam M.M., Usman S.S., Ayon S.I. Predictive data mining models for novel coronavirus (COVID-19) infected patients’ recovery. SN Comput. Sci. 2020;1(4):1–7. doi: 10.1007/s42979-020-00216-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lai L., Wittbold K.A., Dadabhoy F.Z., Sato R., Landman A.B., Schwamm L.H., He S., Patel R., Wei N., Zuccotti G., et al. Healthcare, Vol. 8. Elsevier; 2020. Digital triage: Novel strategies for population health management in response to the COVID-19 pandemic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Jiang X., Coffee M., Bari A., Wang J., Jiang X., Huang J., Shi J., Dai J., Cai J., Zhang T., et al. Towards an artificial intelligence framework for data-driven prediction of coronavirus clinical severity. Comput. Mater. Contin. 2020;63(1):537–551. [Google Scholar]
- 87.Iwendi C., Bashir A.K., Peshkar A., Sujatha R., Chatterjee J.M., Pasupuleti S., Mishra R., Pillai S., Jo O. COVID-19 patient health prediction using boosted random forest algorithm. Front. Public Health. 2020;8:357. doi: 10.3389/fpubh.2020.00357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Assaf D., Gutman Y., Neuman Y., Segal G., Amit S., Gefen-Halevi S., Shilo N., Epstein A., Mor-Cohen R., Biber A., et al. Utilization of machine-learning models to accurately predict the risk for critical COVID-19. Intern. Emerg. Med. 2020;15(8):1435–1443. doi: 10.1007/s11739-020-02475-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zhu J.S., Ge P., Jiang C., Zhang Y., Li X., Zhao Z., Zhang L., Duong T.Q. Deep-learning artificial intelligence analysis of clinical variables predicts mortality in COVID-19 patients. J. Am. Coll. Emerg. Physicians Open. 2020;1(6):1364–1373. doi: 10.1002/emp2.12205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chao H., Fang X., Zhang J., Homayounieh F., Arru C.D., Digumarthy S.R., Babaei R., Mobin H.K., Mohseni I., Saba L., et al. Integrative analysis for COVID-19 patient outcome prediction. Med. Image Anal. 2021;67 doi: 10.1016/j.media.2020.101844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Vítovec M., Baxa J., Mírka H., Flohr T., Schmidt B., Ferda J. The assessment of the lung involvement in COVID-19 pneumonia using automatical analysis employing the artificial intelligence algorithm. Ceska Radiol. 2020;74(3):171–179. [Google Scholar]
- 92.McRae M.P., Dapkins I.P., Sharif I., Anderman J., Fenyo D., Sinokrot O., Kang S.K., Christodoulides N.J., Vurmaz D., Simmons G.W., et al. Managing COVID-19 with a clinical decision support tool in a community health network: Algorithm development and validation. J. Med. Internet Res. 2020;22(8) doi: 10.2196/22033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kwon Y.J., Toussie D., Finkelstein M., Cedillo M.A., Maron S.Z., Manna S., Voutsinas N., Eber C., Jacobi A., Bernheim A., et al. Combining initial radiographs and clinical variables improves deep learning prognostication of patients with COVID-19 from the emergency department. Radiol.: Artif. Intell. 2020 doi: 10.1148/ryai.2020200098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Trebeschi S., Drago S., Birkbak N., Kurilova I., Cǎlin A., Pizzi A.D., Lalezari F., Lambregts D., Rohaan M., Parmar C., et al. Predicting response to cancer immunotherapy using noninvasive radiomic biomarkers. Ann. Oncol. 2019;30(6):998–1004. doi: 10.1093/annonc/mdz108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Shachar C., Gerke S., Adashi E.Y. AI surveillance during pandemics: Ethical implementation imperatives. Hastings Cent. Rep. 2020;50(3):18–21. doi: 10.1002/hast.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hertelendy A.J., Goniewicz K., Khorram-Manesh A. The COVID-19 pandemic: how predictive analysis, artificial intelligence and GIS can be integrated into a clinical command system to improve disaster response and preparedness. Am. J. Emerg. Med. 2020;45:671–672. doi: 10.1016/j.ajem.2020.10.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Devasia J.T., Lakshminarayanan S., Kar S.S. How modern geographical information systems based mapping and tracking can help to combat severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic around the World and India. Int. J. Health Syst. Implement. Res. 2020;4(1):30–54. [Google Scholar]
- 98.Brown N.J. A novel peer-to-peer contact tracking application for COVID-19 and future pandemics. Diabetes Metab. Syndr.: Clin. Res. Rev. 2020;14(5):773–774. doi: 10.1016/j.dsx.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hirose H., Wang L. 2012 Fifth International Symposium on Parallel Architectures, Algorithms and Programming. 2012. Prediction of infectious disease spread using Twitter: A case of influenza; pp. 100–105. [Google Scholar]
- 100.Joshi A., Dey N., Santosh K. Springer; 2020. Intelligent Systems and Methods to Combat Covid-19. [Google Scholar]
- 101.Medrek M., Pastuszak Z. Numerical simulation of the novel coronavirus spreading. Expert Syst. Appl. 2021;166 doi: 10.1016/j.eswa.2020.114109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.2021. How 5G-powered robots are helping China fight coronavirus. last Accessed: 20 March 2021. URL https://www.smartcitiesworld.net/news/news/how-5g-powered-robots-are-helping-china-fight-coronavirus-5154. [Google Scholar]
- 103.Scudellari M. 2021. Covid-19 digital contact tracing: Apple and google work together as mit tests validity. last Accessed: 20 March 2021. URL https://spectrum.ieee.org/the-human-os/biomedical/devices/covid19-digital-contact-tracing-apple-google-mit-tests-validity. [Google Scholar]
- 104.Nguyen C.T., Saputra Y.M., Van Huynh N., Nguyen N.-T., Khoa T.V., Tuan B.M., Nguyen D.N., Hoang D.T., Vu T.X., Dutkiewicz E., et al. A comprehensive survey of enabling and emerging technologies for social distancing—Part I: Fundamentals and enabling technologies. IEEE Access. 2020;8:153479–153507. doi: 10.1109/ACCESS.2020.3018140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hameed B.Z., Patil V., Shetty D.K., Naik N., Nagaraj N., Sharma D. Use of artificial intelligence-based computer vision system to practice social distancing in hospitals to prevent transmission of COVID-19. Indian J. Commun. Med.: Off. Publ. Indian Assoc. Prevent. Soc. Med. 2020;45(3):379. doi: 10.4103/ijcm.IJCM_366_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ahmed I., Ahmad M., Rodrigues J.J., Jeon G., Din S. A deep learning-based social distance monitoring framework for COVID-19. Sustainable Cities Soc. 2021;65 doi: 10.1016/j.scs.2020.102571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.2021. Baidu open sources AI to identify people without face masks. last Accessed: 20 March 2021. URL https://thenextweb.com/neural/2020/02/17/baidu-open-sources-ai-to-identify-people-without-face-masks/ [Google Scholar]
- 108.Jawad R. BBC News; 2020. Coronavirus: Tunisia Deploys Police Robot on Lockdown Patrol. [Google Scholar]
- 109.Vincent J. The Verge; 2021. Spot the Robot is Reminding Parkgoers in Singapore to keep their Distance from one Another. last Accessed: 20 March 2021. URL https://www.theverge.com/2020/5/8/21251788/spot-boston-dynamics-robot-singapore-park-social-distancing. [Google Scholar]
- 110.Battineni G., Chintalapudi N., Amenta F. Healthcare, Vol. 8. Multidisciplinary Digital Publishing Institute; 2020. AI Chatbot design during an epidemic like the novel coronavirus; p. 154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Erazo W.S., Guerrero G.P., Betancourt C.C., Salazar I.S. 2020 11th IEEE Annual Information Technology, Electronics and Mobile Communication Conference (IEMCON) IEEE; 2020. Chatbot implementation to collect data on possible COVID-19 cases and release the pressure on the primary health care system; pp. 0302–0307. [Google Scholar]
- 112.Pranathi B., Nair A., Anushree C., Chandar T. 2020 11th International Conference on Computing, Communication and Networking Technologies (ICCCNT) IEEE; 2020. Sahayantra-A patient assistance robot; pp. 1–6. [Google Scholar]
- 113.Lafranca L., Li J. International Conference on Social Robotics. Springer; 2020. Humans and robots in times of quarantine based on first-hand accounts; pp. 688–707. [Google Scholar]
- 114.Su C.-Y., Samani H., Yang C.-Y., Fernando O.N.N. 2018 International Conference on System Science and Engineering (ICSSE) IEEE; 2018. Doctor robot with physical examination for skin disease diagnosis and telemedicine application; pp. 1–6. [Google Scholar]
- 115.Tsai S.-C., Samani H., Kao Y.-W., Zhu K., Jalaian B. 2018 IEEE International Conference on Artificial Intelligence and Virtual Reality (AIVR) IEEE; 2018. Design and development of interactive intelligent medical agent; pp. 210–215. [Google Scholar]
- 116.Shinkariov S., Zingerman B., Kargalskaya I., Nozik A., Fistul I., Evelson L., Kremenetskaya A., Sun L., Xu J., Kremenetskaya O., et al. International Conference on Health Information Science. Springer; 2020. Telemedicine system with elements of artificial intelligence for health monitoring during COVID-19 pandemic; pp. 103–110. [Google Scholar]
- 117.Wu S., Li K., Ye R., Lu Y., Xu J., Xiong L., Cui A., Li Y., Peng C., Lv F. Robot-assisted teleultrasound assessment of cardiopulmonary function on a patient with confirmed COVID-19 in a Cabin Hospital. Adv. Ultrasound Diagn. Ther. 2020;4(2):128–130. [Google Scholar]
- 118.Wang J., Peng C., Zhao Y., Ye R., Hong J., Huang H., Chen L. Application of a robotic tele-echography system for COVID-19 pneumonia. J. Ultrasound Med. 2021;40(2):385–390. doi: 10.1002/jum.15406. [DOI] [PubMed] [Google Scholar]
- 119.Chen A., Balter M., Maguire T., Yarmush M. Deep learning robotic guidance for autonomous vascular access. Nat. Mach. Intell. 2020;2:104–115. [Google Scholar]
- 120.Bačík J., Tkáč P., Hric L., Alexovič S., Kyslan K., Olexa R., Perduková D. Phollower—The universal autonomous mobile robot for industry and civil environments with COVID-19 germicide addon meeting safety requirements. Appl. Sci. 2020;10(21):7682. [Google Scholar]
- 121.Jat D.S., Singh C. Intelligent Systems and Methods to Combat Covid-19. Springer; 2020. Artificial intelligence-enabled robotic drones for COVID-19 outbreak; pp. 37–46. [Google Scholar]
- 122.Kumar A., Sharma K., Singh H., Naugriya S.G., Gill S.S., Buyya R. A drone-based networked system and methods for combating coronavirus disease (COVID-19) pandemic. Future Gener. Comput. Syst. 2021;115:1–19. doi: 10.1016/j.future.2020.08.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Sarbadhikari S.N., Pradhan K.B. The need for developing technology-enabled, safe, and ethical workforce for healthcare delivery. Saf. Health Work. 2020;11(4):533–536. doi: 10.1016/j.shaw.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Li B.Y., Lin H., Samani H., Sadler L., Gregory T., Jalaian B. 2017 International Conference on Advanced Robotics and Intelligent Systems (ARIS) IEEE; 2017. On 3D autonomous delivery systems: Design and development; pp. 1–6. [Google Scholar]
- 125.2021. Keenon robot. last Accessed: 20 March 2021. URL https://www.keenonrobot.com/ [Google Scholar]
- 126.2021. China’s autonomous delivery vehicles navigate the coronavirus outbreak. last Accessed: 20 March 2021. URL https://syncedreview.com/2020/03/21/chinas-autonomous-delivery-vehicles-navigate-the-coronavirus-outbreak. [Google Scholar]
- 127.2021. Techmetics. last Accessed: 20 March 2021. URL https://www.techmetics-group.com/ [Google Scholar]
- 128.Shen Y., Guo D., Long F., Mateos L.A., Ding H., Xiu Z., Hellman R.B., King A., Chen S., Zhang C., et al. Robots under COVID-19 pandemic: A comprehensive survey. IEEE Access. 2020;9:1590–1615. doi: 10.1109/ACCESS.2020.3045792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Lamptey E., Serwaa D. The use of zipline drones technology for COVID-19 samples transportation in ghana. HighTech Innov. J. 2020;1(2):67–71. [Google Scholar]
- 130.Figliozzi M., Jennings D. Autonomous delivery robots and their potential impacts on urban freight energy consumption and emissions. Transp. Res. Procedia. 2020;46:21–28. [Google Scholar]
- 131.Van der Aalst W.M., Bichler M., Heinzl A. Robotic process automation. Bus. Inform. Syst. Eng. 2018;60:269–272. [Google Scholar]
- 132.Nassir A.A., Baptiste M.J., Mwikarago I., Habimana M.R., Ndinkabandi J., Murangwa A., Nyatanyi T., Muvunyi C.M., Nsanzimana S., Leon M., et al. 2020. Rpa-based method for the detection of SARS-CoV2. MedRxiv. [Google Scholar]
- 133.D.G.S. Inc. 2021. Robotic process automation (RPA) use cases in COVID-19 pandemic situations. last Accessed: 20 March 2021. URL https://trubot.datamatics.com/resources/rpa-use-cases/covid-19. [Google Scholar]
- 134.2021. How RPA can help labs in COVID-19 test reporting automation. last Accessed: 20 March 2021. URL https://www.bigsteptech.com/rpa-helps-labs-in-covid19-test-reporting/ [Google Scholar]
- 135.Wiggers K. 2021. How RPA could help distribute and track COVID-19 vaccines. last Accessed: 20 March 2021. URL https://venturebeat.com/2020/12/27/how-rpa-could-help-distribute-and-track-covid-19-vaccines/ [Google Scholar]
- 136.Neo D. 2021. Rpa and COVID-19 - robots helping put employee health first. last Accessed: 20 March 2021. URL https://www.uipath.com/blog/how-software-robots-help-companies-keep-employees-safe-from-virus. [Google Scholar]
- 137.2021. Social distance monitoring. last Accessed: 20 March 2021. URL https://levelfivesupplies.com/social-distance-monitoring-tools/ [Google Scholar]
- 138.2021. Meet the robots. last Accessed: 20 March 2021. URL https://bucharestrobots.com/ [Google Scholar]
- 139.T.R.R. Staff, T.R.R. Staff . 2021. Nimbus robot uses microburst spray to kill coronavirus, other pathogens. last Accessed: 20 March 2021. URL https://www.therobotreport.com/nimbus-robot-uses-microburst-spray-kill-coronavirus/ [Google Scholar]
- 140.Begić A. International Symposium on Innovative and Interdisciplinary Applications of Advanced Technologies. Springer; 2017. Application of service robots for disinfection in medical institutions; pp. 1056–1065. [Google Scholar]
- 141.Sayed A.S., Ammar H.H., Shalaby R. 2020 2nd Novel Intelligent and Leading Emerging Sciences Conference (NILES) IEEE; 2020. Centralized multi-agent mobile robots SLAM and navigation for COVID-19 field hospitals; pp. 444–449. [Google Scholar]
- 142.Muthugala M., Samarakoon S., Mohan Rayguru M., Ramalingam B., Elara M.R. Wall-following behavior for a disinfection robot using type 1 and type 2 fuzzy logic systems. Sensors. 2020;20(16):4445. doi: 10.3390/s20164445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.2021. Youibot. last Accessed: 20 March 2021. URL https://www.servo.com.sg/youibot. [Google Scholar]
- 144.Brickwood B. 2021. Xag introduces drone disinfection operation to fight coronavirus outbreak. last Accessed: 20 March 2021. URL https://www.healtheuropa.eu/xag-introduces-drone-disinfection-operation-to-fight-the-coronavirus-outbreak/97265/ [Google Scholar]
- 145.Rafaela NajiMiddle East NewsMarch 27, 2020 . 2021. Dubai is using drones to disinfect all the city. last Accessed: 20 March 2021. URL https://www.the961.com/dubai-is-using-drones-to-disinfect-all-the-city/ [Google Scholar]
- 146.2021. Buffalo startup repurposes drones for sanitation to fight COVID-19. last Accessed: 20 March 2021. URL https://spectrumlocalnews.com/nys/buffalo/news/2020/05/05/buffalo-startup-re-purposes-drones-for-sanitation-to-fight-covid-19. [Google Scholar]
- 147.McCandless M.E. 2021. Drone disinfection system kills coronavirus in large indoor spaces. last Accessed: 20 March 2021. URL https://facilityexecutive.com/2020/04/drone-disinfection-system-kills-coronavirus-in-large-indoor-spaces/ [Google Scholar]
- 148.Kass-Hout T.A., MD M.S., Snively B. 2021. Aws launches machine learning enabled search capabilities for COVID-19 dataset. last Accessed: 17 January 2021. URL https://aws.amazon.com/blogs/publicsector/aws-launches-machine-learning-enabled-search-capabilities-covid-19-dataset/ [Google Scholar]
- 149.Ekins S., Freundlich J.S., Clark A.M., Anantpadma M., Davey R.A., Madrid P. Machine learning models identify molecules active against the Ebola virus in vitro. F1000Research. 2015;4:1091. doi: 10.12688/f1000research.7217.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Zhang L., Ai H.-X., Li S.-M., Qi M.-Y., Zhao J., Zhao Q., Liu H.-S. Virtual screening approach to identifying influenza virus neuraminidase inhibitors using molecular docking combined with machine-learning-based scoring function. Oncotarget. 2017;8(47):83142–83154. doi: 10.18632/oncotarget.20915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Ho D. Addressing COVID-19 drug development with artificial intelligence. Adv. Intell. Syst. 2020;2(5) doi: 10.1002/aisy.202000070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Kaushik A.C., Raj U. Ai-driven drug discovery: A boon against COVID-19? AI Open. 2020;1:1–4. [Google Scholar]
- 153.Scudellari M. Researchers are betting that AI and automation can cut drug discovery from five years to six months: Automating antivirals. IEEE Spectr. 2020;57(10):44–49. [Google Scholar]
- 154.Caruso F.P., Scala G., Cerulo L., Ceccarelli M. A review of COVID-19 biomarkers and drug targets: resources and tools. Brief. Bioinform. 2021;22(2):701–713. doi: 10.1093/bib/bbaa328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Jumper J., Tunyasuvunakool K., Kohli P., Hassabis D., Team A. DeepMind website; 2020. Computational Predictions of Protein Structures Associated with COVID-19. [Google Scholar]
- 156.Schmitt M. 2021. How to fight COVID-19 with machine learning. last Accessed: 20 March 2021. URL https://towardsdatascience.com/fight-covid-19-with-machine-learning-1d1106192d84. [Google Scholar]
- 157.Fauqueur J., Thillaisundaram A., Togia T. 2019. Constructing large scale biomedical knowledge bases from scratch with rapid annotation of interpretable patterns. arXiv preprint arXiv:1907.01417. [Google Scholar]
- 158.Richardson P., Griffin I., Tucker C., Smith D., Oechsle O., Phelan A., Rawling M., Savory E., Stebbing J. Baricitinib as potential treatment for 2019-nCoV acute respiratory disease. Lancet. 2020;395(10223):e30–e31. doi: 10.1016/S0140-6736(20)30304-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Zhang H., Saravanan K.M., Yang Y., Hossain M.T., Li J., Ren X., Pan Y., Wei Y. Deep learning based drug screening for novel coronavirus 2019-nCov. Interdiscip. Sci.: Comput. Life Sci. 2020;12:368–376. doi: 10.1007/s12539-020-00376-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Wan F., Hong L., Xiao A., Jiang T., Zeng J. NeoDTI: neural integration of neighbor information from a heterogeneous network for discovering new drug-target interactions. Bioinformatics (Oxford, England) 2019;35:104–111. doi: 10.1093/bioinformatics/bty543. [DOI] [PubMed] [Google Scholar]
- 161.Ge Y., Tian T., Huang S., Wan F., Li J., Li S., Wang X., Yang H., Hong L., Wu N., et al. An integrative drug repositioning framework discovered a potential therapeutic agent targeting COVID-19. Signal Trans. Target. Ther. 2021;6(1):1–16. doi: 10.1038/s41392-021-00568-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Zhou Y., Wang F., Tang J., Nussinov R., Cheng F. Artificial intelligence in COVID-19 drug repurposing. Lancet Digit. Health. 2020;2:E667–E676. doi: 10.1016/S2589-7500(20)30192-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Dotolo S., Marabotti A., Facchiano A., Tagliaferri R. A review on drug repurposing applicable to COVID-19. Brief. Bioinform. 2021;22(2):726–741. doi: 10.1093/bib/bbaa288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Mohanty S., Rashid M.H.A., Mridul M., Mohanty C., Swayamsiddha S. Application of artificial intelligence in COVID-19 drug repurposing. Diabetes Metab. Syndr.: Clin. Res. Rev. 2020;14(5):1027–1031. doi: 10.1016/j.dsx.2020.06.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Bharadwaj K.K., Srivastava A., Panda M.K., Singh Y.D., Maharana R., Mandal K., Singh B.M., Singh D., Das M., Murmu D., et al. Computational Intelligence Methods in COVID-19: Surveillance, Prevention, Prediction and Diagnosis. Springer; 2021. Computational intelligence in vaccine design against COVID-19; pp. 311–329. [Google Scholar]
- 166.Kannan S., Subbaram K., Ali S., Kannan H. The role of artificial intelligence and machine learning techniques: Race for covid-19 vaccine. Arch. Clin. Infect. Dis. 2020;15(2) [Google Scholar]
- 167.Russo G., Reche P., Pennisi M., Pappalardo F. The combination of artificial intelligence and systems biology for intelligent vaccine design. Expert Opin. Drug Discovery. 2020;15(11):1267–1281. doi: 10.1080/17460441.2020.1791076. [DOI] [PubMed] [Google Scholar]
- 168.Vinyals O., Blundell C., Lillicrap T., Wierstra D., et al. Matching networks for one shot learning. Adv. Neural Inf. Process. Syst. 2016;29:3630–3638. [Google Scholar]
- 169.Xian Y., Lampert C.H., Schiele B., Akata Z. Zero-shot learning—a comprehensive evaluation of the good, the bad and the ugly. IEEE Trans. Pattern Anal. Mach. Intell. 2018;41(9):2251–2265. doi: 10.1109/TPAMI.2018.2857768. [DOI] [PubMed] [Google Scholar]
- 170.Kaya M., Bilge H.Ş. Deep metric learning: A survey. Symmetry. 2019;11(9):1066. [Google Scholar]
- 171.Brown T.B., Mann B., Ryder N., Subbiah M., Kaplan J., Dhariwal P., Neelakantan A., Shyam P., Sastry G., Askell A., et al. Language models are few-shot learners. Adv. Neural Inf. Process. Syst. 2020;33:1877–1901. [Google Scholar]