Highlights
-
•
Only 58.2% of the sample were very likely to get the COVID-19 vaccine.
-
•
28.8% of participants were in the pro-vaccine class, and 20.8% had anti-vaccine beliefs.
-
•
27.8% had concerns about vaccine development, and 22.6% were unsure about the vaccines.
-
•
Beliefs about peer vaccine intentions aligned with individual vaccine intentions in each class.
Keywords: COVID-19, Vaccine, Latent class analysis
Abstract
Unprecedented global efforts in vaccine development have resulted in effective vaccines for COVID-19. The pandemic response in the US has been highly politicized, resulting in significant opposition to public health efforts, including vaccines. We aimed to understand patterns of attitudes and beliefs about the COVID-19 vaccine to inform vaccination campaigns.
583 English speaking United States adults were surveyed November 18–29, 2020. Participants answered 11 questions about their attitudes and beliefs about a COVID-19 vaccine, including perceived vaccine effectiveness, likelihood of getting vaccinated, and concerns that vaccine development was rushed/influenced by politics. We conducted a latent class analysis to identify profiles of attitudes/beliefs about a COVID-19 vaccine. We identified four classes of COVID-19 vaccine beliefs. The pro-vaccine class (28.8%) was willing to get vaccinated and had broadly positive beliefs about the vaccine. The development concerns class (27.8%) was willing to get vaccinated but was concerned about the development process. The third class (22.6%) was largely unsure if they would get vaccinated and if their peer groups would be vaccinated. The forth class (anti-vaccine, 20.8%) was dominated by an unwillingness to get vaccinated, vaccine distrust, vaccine development concerns, and peers groups with negative vaccine intentions. Given the large proportion of individuals who were concerned about the COVID-19 vaccine development process, messaging about rigor and approval processes may be critical to securing this group’s commitment to vaccination. Having scientific and cultural leaders endorse vaccination may also be influential.
1. Introduction
The COVID-19 pandemic has taken an enormous toll in the United States. At the time of writing, there have been more than 31 million individuals infected with COVID-19 and more than 560,000 lives lost, representing about 20% of fatalities globally despite the US only representing about 4.25% of the world population (Johns Hopkins University. Coronavirus Resource Center, 2021, United States Census Bureau, 2021). Fortunately, recent breakthroughs in mRNA vaccine science paired with unprecedented global attention and resources have made it possible to rapidly develop highly effective vaccines for COVID-19. For example, the World Health Organization, UNICEF, CEPI, and Gavi came together to establish the COVAX initative for rapid vaccine development and equitable global distribution (World Health Organization, 2021). The US Department of Health and Human Services also organized Operation Warp Speed, which was an unprecedented public–private partnership for rapid vaccine production (Ho, 2021). The COVID-19 vaccine development process further benefitted from advances in using lipid carriers to deliver mRNA vaccines, making the long-researched vaccine modality more viable (Tan and Sun, 2018). Finally, vaccine approval benefitted from accelerated approval pathways available from the Food and Drug Administration (Kesselheim et al., 2021), and importantly this accelerated approval still required the same level of scientific evidence of effectiveness.
Unfortunately, both the COVID-19 pandemic and the development of vaccines have been highly politicized and polarized in the United States (Hart et al., 2020). Some have described this era as a “posttruth pandemic,” as many conservative political leaders, celebrities, and pundits have downplayed the seriousness of the pandemic while also spreading misleading or false information (Parmet and Paul, 2020). At the same time as minimizing the severity of the pandemic, the Trump political regime also pressured vaccine developers to accelerate the process, making public pledges regarding its readiness which were not substantiated by the scientific community (Gonsalves and Yamey, 2020). Vaccine mistrust as well as concerns over vaccine fast-tracking and side effects have been expressed by many Americans and may influence vaccine uptake (Latkin et al., 2021).
Social networks may also impact vaccine uptake. Social network have been found to influence individuals’ health risk perceptions, and the intensity and frequency of interact with a network member is linked to shared beliefs (Scherer and Cho, 2003). This suggests that social network members, especially close ties like family, may represent particularly important influences on vaccine attitudes and behaviors. Social networks can also diffuse information and misinformation about vaccine. For example, social media can serve to diffuse anti-vaccination connections and increase anti-vaccination sentiment momentum, in part because people who share anti-vaccine attitudes tend to cluster together (Hoffman et al., 2019, Yuan et al., 2019). Social processes, including norms, have been previously identified as important influences on vaccination decision making and may be useful leverage points for increasing vaccination (Brewer et al., 2017).
The scale of the pandemic combined with the emergence of variants due to uncontrolled community transmission make rapid mass vaccination and achieving herd immunity much more urgent than other vaccination campaigns. In many ways, mass vaccination efforts must race viral mutation to achieve herd immunity before a new variant becomes dominant and could render existing vaccines less effective. We must understand any attitudes and concerns among the public that may increase vaccine hesitancy and reduce uptake.
To date there have been numerous research studies that begun to explore individual level COVID-19 vaccine hesitancy, highlighting importance differences by race, sex, political alignment, and trust in scientific information sources (Latkin et al., 2021, Aw et al., 2021, Latkin et al., 2021, Troiano and Nardi, 2021). However, it is important to further this research by seeking to identify patterns of beliefs that may be useful in segmenting the broader population and aid in targeting vaccination campaigns. Latent class analysis (LCA) is one tool that can achieve this goal by identifying how vaccine attitudes and beliefs co-occur within individuals. LCA has been used to identify groups across a range of health topics, from climate change (Leiserowitz et al., 2021) to drug use (Schneider et al., 2019) to general vaccine attitudes (Hornsey et al., 2021). In each case, LCA can help elucidate important correlates and differences in service utilization and interest between classes. Understanding the underlying groups within vaccine hesitancy and how these groups differ is essential to moving vaccination campaigns forward.
To address this critical public health challenge, we explore profiles of COVID-19 vaccine attitudes, beliefs, social norms, and acceptance among an online sample of United States adults to inform audience segmentation and targeting of vaccine-related public health campaigns.
2. Methods
2.1. Data source
Data for this study came from an online, longitudinal survey of United States adults conducted via Amazon’s Mechanical Turk survey platform. The data used in this analysis came from the fourth wave of the survey, conducted November 18–29, 2020. MTurk is an optimal platform for quickly collecting high quality data from large groups, while obtaining samples that are typically more representative than those obtained via convenience sampling (Berinsky et al., 2011, Follmer et al., 2017, Huff and Tingley, 2015, Paolacci and Chandler, 2014). Participants were required to be at least 18 years or older, live in the United States, able to speak and read English, and to have had heard of the coronavirus (COVID-19). Attention and validity checks were embedded throughout the survey to increase the reliability of responses (Rouse, 2015). We removed the three transgender individuals from the analytic sample due to the small sample size and sex being a correlate of interest, yielding a final analytic sample size of 583. This study was approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board.
2.2. Measures
Participants responded to 11 statements about their attitudes, beliefs, and concerns about a potential COVID-19 (called coronavirus in questions) vaccine on a 5-point scale (strongly agree, agree, neither, disagree, strongly disagree) (Latkin et al., 2021). The vaccine statements were as follows: (1) a vaccine would prevent me from getting the coronavirus, (2) I would not trust a vaccine for the coronavirus, (3) I am very likely to get a coronavirus vaccine, when available, (4) the majority of my family members will get the coronavirus vaccine, when available, (5) the majority of my friends will get the coronavirus vaccine, when available, (6) I will discourage my friends to get a coronavirus vaccine, (7) I will encourage my family members to get a coronavirus vaccine, (8) I am concerned that the vaccines are being developed too quickly, (9) I am worried about bad side effects if I got a coronavirus vaccine, (10) I am concerned that a coronavirus vaccine will not be effective, and (11) I am concerned that short cuts have been taken with coronavirus vaccine development because of political pressures. For each item, we reduced response categories to agree (strongly agree, agree), neither, or disagree (strongly disagree, disagree). We chose to reduce the response categories in this way to help ensure that there would be sufficient statistical power to estimate stable latent class models and to reduce issues related to sparse data in some cells.
Participants also reported a number of sociodemographic characteristics, including their age, sex (male/female), race (White/Black/other), education level (categorized as less than college/some college or more), whether they live in an urban setting (defined as having a population ≥ 100,000), if they had health insurance, if they were currently required to work outside the home, if their household received assistance from the government (defined as food stamps or checks from the government), and if they had received the flu shot the previous year. We also asked participants to indicate their political alignment on a seven-point scale (very liberal to moderate to very conservative). We combined responses into three categories: liberal, moderate, and conservative.
2.3. Analysis
We conducted a latent class analysis using the 11 indicators of vaccine attitudes, norms, and acceptance to identify groups with homogenous vaccine perceptions. We estimated models with increasing numbers of classes (one through six classes) and then used the Akaike Information Criteria (AIC), Bayesian Information Criteria (BIC), sample size adjusted BIC (saBIC), and Vuong-Lo-Mendell-Rubin Likelihood Ratio Tests (LRT) to select the preferred model (Nylund et al., 2007). We then used the R3STEP approach to assess the associations between latent classes and the sociodemographic characteristics of interest (Asparouhouv and Muthén, 2013). The R3STEP command accounts for potential misclassification in class membership resulting from the class enumeration procedure. Then when associations between class membership and correlates are assessed, the model is weighted for individual probabilitites of belonging to each class. The beta estimates resulting from this procedure can be interpreted in the same way as coefficients from traditional multinomial logisitic regression models. Analyses were conducted using Mplus 8 (Mplus User’s Guide).
3. Results
3.1. Sample characteristics
On average, participants were in their late thirties (M = 39.7, SD = 11.6; Table 1). Slightly more than half the sample was female (57.8%), lived in an urban area (54.6%). The majority of the sample was White (81.0%), had some college education or more (87.5%), and currently had health insurance (83.0%). About one-third (38.8%) were required to work outside the home. Few (13.5%) received government assistance. Forty percent had received their flu shot last year (40.3%). About half (52.9%) were politically liberal, one-fifth (20.5%) were moderate, and about one-quarter (26.6%) were conservative.
Table 1.
Sample characteristics and vaccine attitudes and beliefs.
| N (%) | |
|---|---|
| Age, M(SD) | 39.7 (11.6) |
| Female Sex | 337 (57.8) |
| Race | |
| White | 472 (81.0) |
| Black | 37 (6.4) |
| Other | 74 (12.7) |
| Some College Education or more | 510 (87.5) |
| Lives in urban area | 318 (54.6) |
| Has health insurance | 484 (83.0) |
| Required to work outside the home | 226 (38.8) |
| Receives government assistance | 78 (13.5) |
| Received flu shot last year | 232 (40.3) |
| Political Alignment | |
| Liberal | 307 (52.9) |
| Moderate | 119 (20.5) |
| Conservative | 154 (26.6) |
| A vaccine would prevent me from getting the coronavirus. | |
| Agree | 355 (60.9) |
| Neither | 157 (26.9) |
| Disagree | 71 (12.2) |
| I would not trust a vaccine for the coronavirus. | |
| Agree | 141 (24.2) |
| Neither | 122 (20.9) |
| Disagree | 320 (54.9) |
| I am very likely to get a coronavirus vaccine. | |
| Agree | 339 (58.2) |
| Neither | 97 (16.6) |
| Disagree | 147 (25.2) |
| The majority of my family members will get the coronavirus vaccine. | |
| Agree | 337 (57.8) |
| Neither | 147 (25.2) |
| Disagree | 99 (17.0) |
| The majority of my friends will get the coronavirus vaccine. | |
| Agree | 337 (57.8) |
| Neither | 161 (27.6) |
| Disagree | 85 (14.6) |
| I will discourage my friends to get a coronavirus vaccine. | |
| Agree | 33 (5.7) |
| Neither | 53 (9.1) |
| Disagree | 497 (85.3) |
| I will encourage my family members to get a coronavirus vaccine. | |
| Agree | 347 (59.5) |
| Neither | 124 (21.3) |
| Disagree | 112 (19.2) |
| I am concerned that the vaccines are being developed too quickly. | |
| Agree | 314 (53.9) |
| Neither | 93 (16.0) |
| Disagree | 176 (30.2) |
| I am worried about bad side effects if I got a coronavirus vaccine. | |
| Agree | 372 (63.8) |
| Neither | 79 (13.6) |
| Disagree | 132 (22.6) |
| I am concerned that a coronavirus vaccine will not be effective | |
| Agree | 274 (47.0) |
| Neither | 104 (17.8) |
| Disagree | 205 (35.2) |
| I am concerned that short cuts have been taken with coronavirus vaccine development because of political pressures. | |
| Agree | 330 (56.6) |
| Neither | 84 (14.4) |
| Disagree | 169 (29.0) |
3.2. COVID-19 vaccine beliefs and attitudes
Endorsement of the different vaccine statements varied broadly (Table 1). The least endorsed item was discouraging friends from getting a vaccine (5.7% agree, 9.1% neither, 85.3% disagree). The most endorsed item was worrying about the bad side effects of the vaccine (63.8% agree, 13.6% neither, 22.6% disagree). About sixty percent (60.9%) agree that a vaccine would prevent COVID-19 infection. Over half (58.2%) of participants indicated that they were likely to get a vaccine when available, and a similar percentage believed that their family (57.8%) and friends (57.8%) would get vaccinated. At the same time, more than half (56.6%) of the sample worried that there had been shortcuts taken in vaccine development due to political pressures.
3.3. Latent classes of COVID-19 vaccine beliefs and attitudes
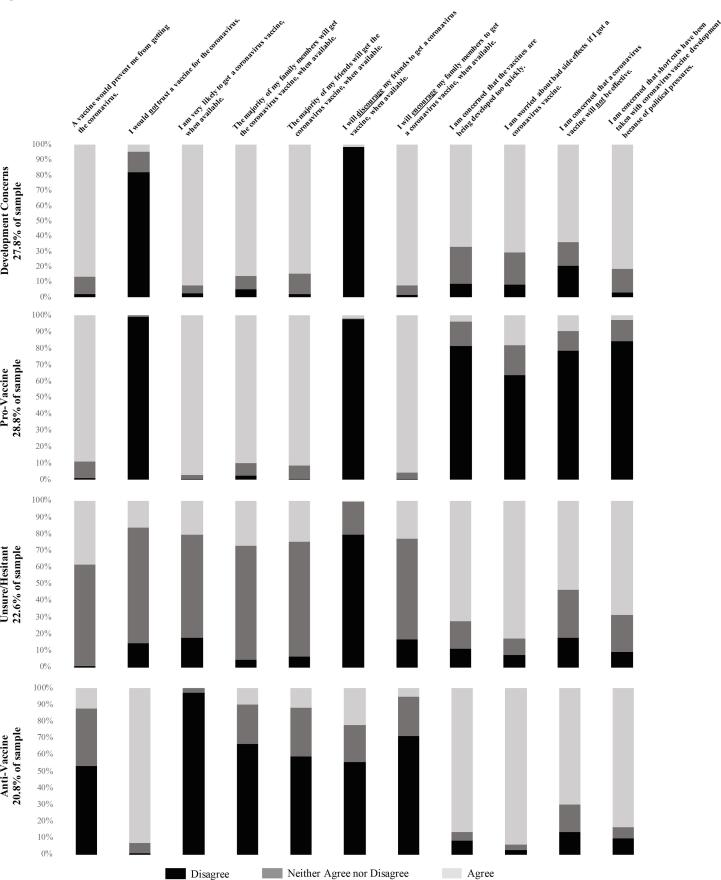
When selecting the latent class model, we favored the BIC for model selection as it is often the best performing fit statistics (Nylund et al., 2007). Therefore, we selected a four-class model (Table 2). The four classes (Fig. 1) were all similarly sized (20.8–28.8% of the sample). The largest class was characterized by positive beliefs about the vaccine, being likely to get the vaccine when available, high social network vaccine acceptance, and few concerns about the development process (28.8% of the sample; called “pro-vaccine” class). The second largest class was characterized by generally positive attitudes towards a COVID-19 vaccine and high social acceptance but had concerns about the vaccine development process (27.8% of the sample; called “development concerns” class). The third class predominantly responded “neither” to the items about their vaccine beliefs and norms and were also unsure if they would get the vaccine (22.6% of the sample; called “unsure” class). The final class had broadly negative attitudes about the vaccine, low perceived social network vaccine acceptance and reported that they were unlikely to get vaccinated (20.8% of the sample; called “anti-vaccine” class).
Table 2.
Latent Class Model Fit Statistics.
| Classes | Smallest Class | Log Likelihood | AIC | BIC | saBIC | Entropy | LRT |
|---|---|---|---|---|---|---|---|
| 1 | – | −5908.195 | 11860.39 | 11956.49 | 11886.648 | – | – |
| 2 | 41.9 | −4818.362 | 9726.725 | 9923.293 | 9780.435 | 0.937 | 0 |
| 3 | 21.8 | −4537.911 | 9211.821 | 9508.858 | 9292.983 | 0.909 | 0 |
| 4 | 20.8 | −4351.672 | 8885.345 | 9282.85 | 8993.958 | 0.895 | 0.634 |
| 5 | 6.0 | −4287.997 | 8803.993 | 9301.966 | 8940.059 | 0.912 | 0.763 |
| 6 | 6.3 | −4236.633 | 8747.265 | 9345.707 | 8910.783 | 0.896 | 0.760 |
Fig. 1.
Latent classes of COVID-19 vaccine attitudes and beliefs.
3.4. Correlates of latent class membership
There were no significant differences between latent classes in terms of age, education, urbanicity, having health insurance, or being required to work outside the home (Table 3). Members of the pro-vaccine class were less likely to be female than those in the development concerns (ß = −0.952, p < 0.001), unsure (ß = −0.694, p = 0.011), and anti-vaccine (ß = −1.178, p < 0.001) classes. Those in the anti-vaccine class were more likely to be Black (ß = 1.823, p = 0.010) or White (ß = 1.118, p = 0.031) than the development concerns class (i.e., development concerns class more likely to be another race). The anti-vaccine class members were also more likely to be Black than the pro-vaccine class members (ß = 2.546, p = 0.004). The anti-vaccine class members were more likely to have received government assistance than members of the pro-vaccine (ß = 1.404, p = 0.001), development concerns (ß = 0.797, p = 0.042) classes, and there was a marginal difference between the anti-vaccine and unsure classes (ß = 0.691, p = 0.073). Members of the anti-vaccine class were less likely to have gotten the flu shot than those in the pro-vaccine (ß = −1.575, p < 0.001) and development concerns (ß = −1.210, p < 0.001) classes. The unsure class members were also less likely to have gotten the flu shot than the pro-vaccine class (ß = −0.699, p = 0.012).
Table 3.
Correlates of Latent Class Membership.
| Development Concerns | Pro-Vaccine | Unsure/Hesitant | Anti-Vaccine | |
|---|---|---|---|---|
| Age, Mean | 38.2 | 41.3 | 39.4 | 40.5 |
| Female Sex, % | 64.8b | 44.1a | 58.5b | 67.6 |
| Race, % | ||||
| White | 76.8a | 84.1 | 81.9 | 83.3 |
| Black | 5.5a | 1.9 | 7.0 | 10.2 |
| Other | 17.7 | 14.0 | 11.1 | 6.5 |
| Some college or more, % | 88.2 | 91.5 | 87.5 | 82.3 |
| Lives in urban area, % | 53.6 | 55.4 | 55.7 | 53.4 |
| Political Alignment, % | ||||
| Liberal | 68.5 | 59.4 | 48.2bc | 29.4 |
| Moderate | 17.6 | 11.6 | 27.6 | 28.3 |
| Conservative | 13.9ab | 29.0a | 24.2b | 42.3 |
| Has health insurance, % | 87.9 | 88.4 | 77.3 | 76.7 |
| Required to work outside the home, % | 38.2 | 42.6 | 37.3 | 37.5 |
| Receives government assistance, % | 13.8a | 7.2a | 14.2 | 21.0 |
| Received flu shot last year, % | 46.5a | 54.5a | 34.0b | 18.7 |
c estimate is significantly (p < 0.05) different from the development concerns class estimate.
estimate is significantly (p < 0.05) different from the anti-vaccine class estimate.
estimate is significantly (p < 0.05) different from the pro-vaccine class estimate.
3.4.1. Political alignment
Members of the pro-vaccine class were more likely to be conservative than those in the development concerns (ß = 0.987, p = 0.032) and unsure (ß = 0.827, p = 0.044) classes and were more likely to be liberal than the unsure class (ß = 1.082, p = 0.004). Members of the development concerns class were more likely to be liberal than the unsure class members (ß = 0.803, p = 0.024). The anti-vaccine class members were more likely to be conservative than the pro-vaccine (ß = −1.630, p < 0.001) and development concerns (ß = −1.351, p < 0.001) class members. The anti-vaccine class members were also marginally more likely to be conservative than those in the development concerns class (ß = 0.793, p = 0.055).
4. Discussion
Using survey data from an online sample of US adults, we identified four profiles of COVID-19 vaccine attitudes that have important implications for vaccine uptake: pro-vaccine, development concerns, unsure, and anti-vaccine. These profiles were relatively evenly distributed in the sample. There were significant differences between classes in terms of political alignment. While more liberal classes had more positive views about the vaccine than conservative classes, the most liberal class was also most likely to worry that the vaccine development process had been compromised due to political pressures (development concerns). This may be due to the distrust in the government after the Trump administration promoted bogus cures for COVID-19, interfered in the CDC’s response to the pandemic, and potentially pressured the FDA to approve the vaccines quickly.
Our results can directly inform public health campaigns to increase vaccine uptake. First, the pro-vaccine group should be encouraged, when they are vaccinated, to share that information with family and friends and post it online. They could also discuss the positive feelings and sense of relief after being vaccinated. Second, media campaigns need to address concerns about the vaccine development process. The development concerns class was 27.8% of the sample and was worried that vaccines had been developed too quickly and that the development was influenced by political pressures. To address concerns about the speed of development, it may be useful to highlight how COVID-19 vaccine development benefitted from unprecedented global attention and resources and decades of previous mRNA vaccine research and recent breakthroughs, which made it possible to develop an effective vaccine rapidly. As the development process is rather complicated and abstract, it may be helpful to develop visual representations about the parallel processes as well as the massive number of people in the phase three trials and current observational studies of vaccine recipients. To address concerns about politics unduly influencing the development process, it will be important to highlight the rigor with which vaccine trial results were evaluated by the FDA, delineating the review process and the independence of the committee that reviews the outcomes. It may also be useful to emphasize that the same vaccines being used in the United States have also been approved in other countries, outside the influence of American political pressures. This information should be combined with liberal leaders vouching for the process, especially as the development concerns group was largely liberal and thus likely skeptical of the failure of the previous US political regime to address the pandemic.
The second type of public health campaign our results suggest is needed to address individuals who are unsure about the efficacy of the COVID-19 vaccines and are undecided about whether they intend to get vaccinated. In our sample, about one-fifth of participants fell into this “unsure” category. To encourage vaccination among members of this group, public health campaigns need to provide clear, accurate, and consistent messages about the safety and effectiveness of the vaccine across a variety of platforms in order to increase the public’s knowledge about and confidence in the vaccine. Additionally, given the high level of concerns about side effects present in this study, messaging should also emphasize that these effects are short term and, in fact, an important part of the vaccine process of ensuring a robust immune response. It will likely be important that these messages are apolitical, focus on scientific facts, and are distributed via credible messengers to combat the misinformation about COVID-19 that has proliferated (Parmet and Paul, 2020). Finally, messaging campaigns should emphasize the importance of getting vaccinated in hastening the return to greater normalcy.
While clear and consistent communication is important, initial research suggests it may be insufficient to change vaccination intentions. One initial experiment found no impact of transparent information campaigns on vaccine intentions (Kerr et al., 2021). This null effect could be due to the fact that the messages were not specifically targeted to groups’ concerns. It is also possible that focusing on information only neglects important emotional elements of COVID-19 decision making, both positive (altruism) and negative (fear and anxiety) (Chou and Budenz, 2020). Incorporating key emotional messages into fact based campaign that address the specific concerns of the target population may be essential for moving the needle on vaccination rates.
Those holding anti-vaccine attitudes will likely be the hardest to influence. Vaccine hesitancy and anti-vaccine attitudes in the United States are largely derived from prolific misinformation and a rise in anti-science beliefs (Hotez et al., 2020, Moran et al., 2016). Further, anti-vaccine groups utilize predatory behavior to target insular and vulnerable communities to raise fears of vaccination (Hotez et al., 2020). As anti-vaccine class in this study was much more likely to be conservative than other classes, conservative leaders and media outlets must use their platforms to correct the misinformation spread about COVID-19 and encourage vaccination among members of their audience. Unfortunately, this group will likely pose the largest barrier to achieving herd immunity to COVID-19 in the United States. While many members of this class perceived that their family and friends would not get vaccinated, this may not be the reality. Interventions which encourage people to talk to their peers about getting vaccinated may help diffuse vaccine uptake intentions within this group. This type of intervention may be especially important given that anti-vaccine communities tend to be insular, especially in their social media presence (Yuan et al., 2019, Hotez et al., 2020). In addition, some preliminary research has suggested that those who are strongly hesitant about vaccination may be more responsive to campaigns that highlight the personal benefits to them, rather than societal goods (Freeman et al., 2021).
While the exact population-level vaccination threshold needed to achieve herd immunity for COVID-19 is not yet known, known thresholds for other diseases can guide estimates. For example, the herd immunity threshold for polio is around 80%, while the more contagious measles has a higher threshold around 95% (Gonçalves, 2008, Rashid et al., 2012). Estimates of the R0 (the metric of how many people a single infected person could spread the disease to) for COVID-19 range from 2.2 to 5.7, suggesting that the herd immunity threshold for this disease is likely somewhere around 82% (Sanche et al., 2020). In our sample, vaccinating the three classes who were not anti-vaccine could approach 80%. While it is unclear if these prevalences of classes translate to the overall population, this does suggest that public health efforts likely should target these groups first in an effort to most rapidly and efficiently approach this hypothetical herd immunity target. Public health efforts can then move to address so-called “anti-vaxxers” with more intensive and targeted interventions.
Our study does have some limitations to consider. First, the data used in this study were collected in November 2020. This was prior to large scale vaccine roll out in the United States, so attitudes may have meaningfully changed in the intervening months as vaccination has become more common. Vaccine attitude monitoring is needed on an ongoing basis, as the pandemic and public health efforts continue to evolve. The sample was not necessarily representative of the United States population. Follow up research is needed to see if these same classes are present in similar proportions with nationally representative data. We also did not ask about messaging strategies that participants would be receptive to, so it is necessary to conduct additional research to evaluate these issues. We also do not know if other types of questions may have modified class membership. Further, racial and ethnic minority individuals represent a relatively small portion of our sample, so further research is needed to understand vaccine attitudes among non-white populations.
5. Conclusions
We identified four classes of COVID-19 vaccine attitudes and beliefs, which can inform public health efforts to increase vaccine uptake. Messaging to specifically address concerns related to the development process and clear and consistent information are two key elements that need to be included in public health campaigns to increase vaccine uptake. Addressing these two concerns and the utilization of social network diffusion intervention approaches may help achieve critical vaccination thresholds in the United States before addressing hard to influence vaccine resistant populations.
Funding
This study was supported by the Alliance for a Healthier World and the National Institute on Drug Abuse (NIDA; R01DA040488). KES was supported by a NIDA training grant (5T32DA007292). The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
CRediT authorship contribution statement
Kristin E. Schneider: Conceptualization, Formal analysis, Writing – original draft. Lauren Dayton: Data curation, Investigation, Writing – review & editing. Saba Rouhani: Writing – review & editing. Carl A. Latkin: Funding acquisition, Investigation, Conceptualization, Supervision, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References:
- Johns Hopkins University. Coronavirus Resource Center. https://coronavirus.jhu.edu/. Published 202Accessed March 12, 2021.
- United States Census Bureau. U.S. and World Population Clock. https://www.census.gov/popclock/. Published 2021. Accessed March 23, 2021.
- World Health Organization. COVAX. https://www.who.int/initiatives/act-accelerator/covax. Published 2021. Accessed March 23, 2021.
- Ho R.J.Y. Warp-speed Covid-19 Vaccine development: beneficiaries of maturation in biopharmaceutical technologies and public-private partnerships. J. Pharm. Sci. 2021;110(2):615–618. doi: 10.1016/j.xphs.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan L.u., Sun X. Recent advances in mRNA vaccine delivery. Nano Res. 2018;11(10):5338–5354. [Google Scholar]
- Kesselheim A.S., Darrow J.J., Kulldorff M., Brown B.L., Mitra-Majumdar M., Lee C.C., Moneer O., Avorn J. An overview of vaccine development, approval, and regulation, with implications For COVID-19: Analysis reviews the Food and Drug Administration’s critical vaccine approval role with implications for COVID-19 vaccines. Health Aff. 2021;40(1):25–32. doi: 10.1377/hlthaff.2020.01620. [DOI] [PubMed] [Google Scholar]
- Hart P.S., Chinn S., Soroka S. Politicization and polarization in COVID-19 news coverage. Sci. Commun. 2020;42(5):679–697. doi: 10.1177/1075547020950735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parmet, W.E., Paul, J. 2020. COVID-19: the first posttruth pandemic. In: American Public Health Association.
- Gonsalves G., Yamey G. Political interference in public health science during covid-19. BMJ. 2020;371 doi: 10.1136/bmj.m3878. [DOI] [PubMed] [Google Scholar]
- Latkin C.A., Dayton L., Yi G., Konstantopoulos A., Boodram B. Trust in a COVID-19 vaccine in the US: A social-ecological perspective. Soc. Sci. Med. 2021;270:113684. doi: 10.1016/j.socscimed.2021.113684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scherer C.W., Cho H. A social network contagion theory of risk perception. Risk Analysis: Int. J. 2003;23(2):261–267. doi: 10.1111/1539-6924.00306. [DOI] [PubMed] [Google Scholar]
- Hoffman B.L., Felter E.M., Chu K.-H., Shensa A., Hermann C., Wolynn T., Williams D., Primack B.A. It’s not all about autism: the emerging landscape of anti-vaccination sentiment on Facebook. Vaccine. 2019;37(16):2216–2223. doi: 10.1016/j.vaccine.2019.03.003. [DOI] [PubMed] [Google Scholar]
- Yuan X., Schuchard R.J., Crooks A.T. Examining emergent communities and social bots within the polarized online vaccination debate in Twitter. Social Media+ Society. 2019;5(3) doi: 10.1177/2056305119865465. [DOI] [Google Scholar]
- Brewer N.T., Chapman G.B., Rothman A.J., Leask J., Kempe A. Increasing vaccination: putting psychological science into action. Psychol. Sci. Public Interest. 2017;18(3):149–207. doi: 10.1177/1529100618760521. [DOI] [PubMed] [Google Scholar]
- Aw J., Seng J.J.B., Seah S.S.Y., Low L.L. COVID-19 vaccine hesitancy—A scoping review of literature in high-income countries. Vaccines. 2021;9(8):900. doi: 10.3390/vaccines9080900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin C., Dayton L.A., Yi G., Konstantopoulos A., Park J.u., Maulsby C., Kong X. COVID-19 vaccine intentions in the United States, a social-ecological framework. Vaccine. 2021;39(16):2288–2294. doi: 10.1016/j.vaccine.2021.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troiano G., Nardi A. Vaccine hesitancy in the era of COVID-19. Public Health. 2021;194:245–251. doi: 10.1016/j.puhe.2021.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leiserowitz A., Roser-Renouf C., Marlon J., Maibach E. Global Warming’s Six Americas: a review and recommendations for climate change communication. Curr. Opin. Behav. Sci. 2021;42:97–103. [Google Scholar]
- Schneider K.E., Park J.N., Allen S.T., Weir B.W., Sherman S.G. Patterns of polysubstance use and overdose among people who inject drugs in Baltimore, Maryland: a latent class analysis. Drug Alcohol Depend. 2019;201:71–77. doi: 10.1016/j.drugalcdep.2019.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornsey M.J., Edwards M., Lobera J., Díaz-Catalán C., Barlow F.K. Resolving the small-pockets problem helps clarify the role of education and political ideology in shaping vaccine scepticism. Br. J. Psychol. 2021 doi: 10.1111/bjop.12500. [DOI] [PubMed] [Google Scholar]
- Berinsky, A.J., Huber, G.A., Lenz, G.S. 2011. Using Mechanical Turk as a subject recruitment tool for experimental research. Submitted for review.
- Follmer D.J., Sperling R.A., Suen H.K. The role of MTurk in education research: advantages, issues, and future directions. Educ. Res. 2017;46(6):329–334. [Google Scholar]
- Huff C., Tingley D. ‘Who are these people?’Evaluating the demographic characteristics and political preferences of MTurk survey respondents. Res. Polit. 2015;2(3):1–11. [Google Scholar]
- Paolacci G., Chandler J. Inside the Turk: understanding mechanical Turk as a participant pool. Curr. Directions Psychol. Sci. 2014;23(3):184–188. [Google Scholar]
- Rouse S.V. A reliability analysis of Mechanical Turk data. Comput. Hum. Behav. 2015;43:304–307. [Google Scholar]
- Nylund K.L., Asparouhov T., Muthén B.O. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct. Eq. Model. Multidisciplinary J. 2007;14(4):535–569. [Google Scholar]
- Asparouhouv T., Muthén B. Appendices for auxiliary variables in mixture modeling: 3-step approaches using Mplus. MPlus user’s guide. 2013 [Google Scholar]
- Mplus User’s Guide [computer program]. Los Angeles, CA: Muthén & Muthén; 1998-2017.
- Kerr J.R., Freeman A.L., Marteau T.M., van der Linden S. Effect of information about COVID-19 vaccine effectiveness and side effects on behavioural intentions: two online experiments. Vaccines. 2021;9(4):379. doi: 10.3390/vaccines9040379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou W.-Y., Budenz A. Considering emotion in COVID-19 vaccine communication: addressing vaccine hesitancy and fostering vaccine confidence. Health Commun. 2020;35(14):1718–1722. doi: 10.1080/10410236.2020.1838096. [DOI] [PubMed] [Google Scholar]
- Hotez P.J., Nuzhath T., Colwell B. Combating vaccine hesitancy and other 21st century social determinants in the global fight against measles. Curr. Opin. Virol. 2020;41:1–7. doi: 10.1016/j.coviro.2020.01.001. [DOI] [PubMed] [Google Scholar]
- Moran M.B., Lucas M., Everhart K., Morgan A., Prickett E. What makes anti-vaccine websites persuasive? A content analysis of techniques used by anti-vaccine websites to engender anti-vaccine sentiment. J. Commun. Healthcare. 2016;9(3):151–163. [Google Scholar]
- Freeman D., Loe B.S., Yu L.-M., Freeman J., Chadwick A., Vaccari C., Shanyinde M., Harris V., Waite F., Rosebrock L., Petit A., Vanderslott S., Lewandowsky S., Larkin M., Innocenti S., Pollard A.J., McShane H., Lambe S. Effects of different types of written vaccination information on COVID-19 vaccine hesitancy in the UK (OCEANS-III): a single-blind, parallel-group, randomised controlled trial. Lancet Public Health. 2021;6(6):e416–e427. doi: 10.1016/S2468-2667(21)00096-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonçalves G. Herd immunity: recent uses in vaccine assessment. Expert Rev. Vaccines. 2008;7(10):1493–1506. doi: 10.1586/14760584.7.10.1493. [DOI] [PubMed] [Google Scholar]
- Rashid H., Khandaker G., Booy R. Vaccination and herd immunity: what more do we know? Curr. Opin. Infect. Dis. 2012;25(3):243–249. doi: 10.1097/QCO.0b013e328352f727. [DOI] [PubMed] [Google Scholar]
- Sanche S., Lin Y.T., Xu C., Romero-Severson E., Hengartner N., Ke R. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg. Infect. Dis. 2020;26(7):1470–1477. doi: 10.3201/eid2607.200282. [DOI] [PMC free article] [PubMed] [Google Scholar]