Abstract
Objectives
Prevalence estimates for specific chronic conditions and multimorbidity (MM) in eastern Europe are scarce. This national study estimates the prevalence of MM by age group and sex in Estonia.
Design
A population-based cross-sectional study, using administrative data.
Setting
Data were collected on 55 chronic conditions from the Estonian Health Insurance Fund from 2015 to 2017. MM was defined as the coexistence of two or more conditions.
Participants
The Estonian Health Insurance Fund includes data for approximately 95% of the Estonian population receiving public health insurance.
Primary and secondary outcome measures
Prevalence and 95% CIs for MM stratified by age group and sex.
Results
Nearly half (49.1%) of the individuals (95% CI 49.0 to 49.3) had at least 1 chronic condition, and 30.1% (95% CI 30.0 to 30.2) had MM (2 or more chronic conditions). The number of conditions and the prevalence of MM increased with age, ranging from an MM prevalence of 3.5% (3.5%–3.6%) in the youngest (0–24 years) to as high as 80.4% (79.4%–81.3%) in the oldest (≥85 years) age group. Half of all individuals had MM by 60 years of age, and 75% of the population had MM by 75 years of age. Women had a higher prevalence of MM (34.9%, 95% CI 34.7 to 35.0) than men (24.4%, 95% CI 24.3 to 24.5). Hypertension was the most frequent chronic condition (24.5%), followed by chronic pain (12.4%) and arthritis (7.7%).
Conclusions
Hypertension is an important chronic condition amenable to treatment with lifestyle and therapeutic interventions. Given the established correlation between uncontrolled hypertension and exacerbation of other cardiovascular conditions as well as acute illnesses, this most common condition within the context of MM may be suitable for targeted public health interventions.
Keywords: epidemiology, general medicine (see internal medicine), public health, internal medicine
Strengths and limitations of this study.
One of the strengths of our study is the methodological comparability with previous research.
The second strength is the nearly 95% nationwide coverage of our dataset, the validity of which has been tested and proven.
A limitation of our study is the definition of a chronic condition and multimorbidity (MM) used in our study, which is contestable in all studies of MM.
Background
The management of patients with multimorbidity (MM) has become a challenge for healthcare systems as most individuals with long-term conditions are living with multiple long-term conditions.1 The prevalence of MM is increasing along with population ageing,2 but ageing is not the only factor predisposing the population increase in MM3 and healthcare utilisation has experienced a concomitant increase in response to managing these complex patients.4–6 In addition to ageing, MM is associated with other sociodemographic factors, such as female sex, lower education, lower household income, living alone, social deprivation and ethnicity,7–10 as well as health conditions, such as obesity,11 hypertension and having one chronic condition at baseline. Behavioural factors like smoking and physical inactivity are also influential.12 Having multiple chronic conditions is associated with poor outcomes: patients have a decreased quality of life, psychological distress, longer hospital stays, more postoperative complications, a higher cost of care and higher mortality.13
The management of patients with MM is a formidable challenge for healthcare systems. Research in this area is perhaps most urgently needed in low-income and middle-income countries, where the burden of MM is high, the specific distributions and determinants of the disease may differ and access to care may be impeded by a fragmented healthcare system, which is continuing to modernise and restructure.14 Although research is beginning to elucidate the distribution of co-occurring conditions in these countries, the comparability of findings is limited by methodological differences. This work demonstrates the utility of administrative data for constructing prevalence estimates, an approach that is particularly helpful for middle and high-to-middle-income countries, where resource limitations make administrative data not only immediately useful but also scalable, allowing for rate comparisons with other countries. In addition, the transition from a hospital-centric system in Estonia following independence from the Soviet Union was motivated by a desire to strengthen primary healthcare and thereby improve population health.15 Having a set of prevalence estimates for MM is essential for measuring the ongoing success of this transition, adjusted by the prevalence of various conditions amenable to outpatient treatment. Finally, and perhaps most importantly, the SARS-CoV-2 pandemic drew attention to the important contribution of MM to the need for sound public health measures and rapid identification of effective medical interventions based on risk stratification. Frailty has been linked to infection,16 severity,16 17 geographic differences in severity and mortality by MM,18 prompting a renewed focus on improving global health and access to care, probabilistic modelling,19 the triage of care and shielding of the most vulnerable.20 This study presents an important contribution to this developing literature with a comprehensive set of prevalence estimates for MM in eastern Europe.
MM is a growing global health problem affecting all nations regardless of wealth.21 A better understanding of the national or regional epidemiology of MM is necessary to allocate healthcare resources and develop treatment strategies that allow clinicians to deliver patient-centred care that appreciates the potential for competing priorities.1 21 Furthermore, in the context of the coronavirus pandemic, the clinician is faced with the challenge of reconciling competing priorities: maintain stable health among those with MM via telemedicine and other access interventions while preventing the exacerbation of acute SARS-CoV-2 if the patient becomes infected. Certainly, the time has come for all nations to better support individuals in preventing or modifying MM in the interest of improved overall health as well as optimising patient outcomes following infection. The prevalence of MM has been extensively studied in western European countries. For example, in a recent MM prevalence study using a medical practice database in Scotland, 23.2% of patients were living with MM.1 A recent systematic review and meta-analysis of observational studies22 found an overall pooled 33.1% prevalence of MM. There was a considerable difference in the pooled estimates of MM between high-income and low-income countries, with a prevalence of 37.9% and 29.7%, respectively. Still, data are scarce regarding the prevalence of MM in eastern Europe, where life expectancy is shorter than in western Europe, particularly among men. The recent Survey of Health, Ageing and Retirement in Europe (SHARE) study found that among all European countries, eastern and central Europe had the highest MM prevalence, revealing a remarkable health inequality across European regions.7 To illustrate the gap, 70–79-year-old central and eastern Europeans suffer from about the same level of MM as ≥80-year-old northern Europeans.7 However, the SHARE study is limited to self-reported data among individuals aged 50 years or more. Given the limited population-based research in eastern Europe, the use of administrative health data is necessary to develop more accurate regional MM prevalence estimates.
Estonia belongs to the group of eastern European high-to-middle-income countries with relatively low life expectancy and a large sex health gap. The life expectancy among Estonian men is 73.8 years (compared with that of 82.1 years in Estonian women) and is comparable to male life expectancy in China (74.5 years), Argentina (73.6 years) and Mexico (72.6 years). Estonian male life expectancy is markedly shorter than that of regional neighbouring countries, such as Finland (78.6 years), Sweden (80.8 years) or France (79.8 years).23 Disability-free life expectancy in Estonia is also low, being 52.8 years for men and 55.6 years for women in 2018.24 The burden of co-occurring chronic disease, leading to disability and premature death, is an important contributor to this reduced life expectancy in Estonia.
In Estonia, national public health insurance covers approximately 95% of the population. Family physicians are responsible for providing a core package of health services to the individuals registering with the practice for care.25 Following Estonian independence in 1992, important steps were implemented to modernise the health system and improve coordination and access to primary care. In particular, access to family physicians was expanded before streamlining the hospital network, centralising specialty care and establishing a pharmaceutical formulary and treatment guidelines.26 One of the stated goals of restructuring was to provide better chronic disease management, coordinated by the general practitioner, for whom a bonus system was implemented in 2005 to take on these duties. Although management guidelines and quality standards have been implemented for specific chronic conditions, this process has been slow to consider MM.26 Family physicians in Estonia lack clear evidence-based standards for the management of patients with multiple chronic diseases, and the applicability of a single evidence-based guideline to MM is limited and can be problematic.27
A definitive, population-based assessment of MM prevalence by age and between males and females is needed to inform the continued restructuring of the healthcare system to accommodate the growing proportion of these patients.
Methods
For this population-based cross-sectional study, we obtained data from the Estonian Health Insurance Fund (EHIF), which is essentially the sole health insurance provider in Estonia covering approximately 95% of the population.28 We included all subjects from the EHIF database from 1 January 2015 through 31 December 2017. The data abstraction from the EHIF database included year and month of birth, sex assigned at birth, dates for health claims, type of care (inpatient and outpatient care, rehabilitation, nursing care, etc), services provided, all diagnosis codes on claims and the date and diagnosis code on prescriptions. Study subjects were assigned a unique identifier decoupled from personal identification information to enable longitudinal tracking of care while maintaining patient privacy.
To identify all patients with chronic physical and mental conditions, the International Classification of Diseases, Tenth Revision (ICD-10) diagnosis codes for main and other (accompanying) diagnoses were used. For the chronic physical and mental conditions analysis, we selected 55 conditions (online supplemental appendix, table 1). The list of conditions was based on previous MM research to enable comparability1 29 30 and adjusted by the authors (MJ, RK, AU, MO and HP) for use in Estonia. According to Barnett et al,1 we included morbidities that were likely to be chronic, defined as having a significant impact on patients over at least the most recent year, defined in terms of the need for chronic treatment, reduced function, reduced quality of life and risk of future morbidity and mortality.
bmjopen-2021-049045supp001.pdf (57.9KB, pdf)
We constructed the case definition for a chronic condition as follows: the presence of at least two diagnosis codes at least 6 weeks apart for the same condition (ie, matching ICD-10 category) during the study period 1 January 2015 through 31 December 2017 (online supplemental appendix, table 1). This definition enabled us to include chronic conditions while excluding patients with previously diagnosed but improved conditions (eg, conditions where remission is possible, such as epilepsy, asthma, pain or depression). The 6-week interval between the diagnoses reduced over-ascertainment of cases. The inclusion of prescriptions in the data query allowed us to identify patients whose claims profile included diagnosis codes for only one condition, whereas their prescription history identified treatment for multiple conditions.
The ascertainment period was extended to 3 years because some patients visit their physician infrequently. For instance, 17% of publicly insured individuals had no evidence of a visit to a family physician and 37% had no evidence of a visit to a specialist in 2017.28 If we had elected a shorter study period, we might have inadvertently excluded the MM profile of nearly 20% of the population. Any correlation between lower healthcare utilisation and sociodemographic characteristics that impede access (such as lack of paid time off from work for illness, lack of transportation in rural areas, etc) would bias our claims-driven prevalence estimates to undercount MM among individuals facing these access challenges. The prevalence of chronic conditions among all publicly insured individuals was estimated on 31 December 2017 among all persons who were publicly insured at that time.
The study procedures were conducted according to local data protection regulations.
Patient and public involvement
This was an administrative claims study, and as such there were no patients enrolled in this study.
Statistical analysis
The outcomes were the prevalence of chronic conditions, MM and the mean number of conditions by age and sex, estimated as a proportion of individuals with the current characteristics and among the total number of people insured. All results are presented with 95% CIs. Adjustment by age and sex was done using univariate and multivariate Poisson regression. Prevalence ratios and 95% CIs are presented. The analysis was performed using STATA V.14.
Results
We analysed the data of all publicly insured individuals (n=1 240 927, 94.1% of the total population as of 31 December 2017).28 31 Half of the individuals (49.1%, 95% CI 49.0 to 49.3) had one or more chronic conditions, and 30.1% (95% CI 30.0 to 30.2) had MM. The mean number of conditions was 1.33 (95% CI 1.21 to 1.33) (table 1).
Table 1.
Study population, the prevalence of chronic conditions, the mean number of chronic conditions and MM by age group and sex
| Population (%) | Prevalence of chronic conditions (95% CI) | Mean number of conditions (95% CI) | Prevalence of MM (95% CI) | ||
| Total | 1 240 927 (100.0) | 49.1 (49.0 to 49.3) | 1.33 (1.32 to 1.33) | 30.1 (30.0 to 30.2) | |
| Age group (years) | 0–24 | 331 450 (26.7) | 18.2 (18.0 to 18.3) | 0.23 (0.22 to 0.23) | 3.5 (3.5 to 3.6) |
| 25–44 | 326 460 (26.3) | 34.8 (34.6 to 35.0) | 0.56 (0.55 to 0.56) | 12.6 (12.5 to 12.7) | |
| 45–64 | 323 256 (26.0) | 65.6 (65.3 to 65.8) | 1.64 (1.63 to 1.64) | 41.0 (40.7 to 41.2) | |
| 65–84 | 225 705 (18.2) | 85.6 (85.2 to 85.9) | 3.22 (3.21 to 3.22) | 71.1 (70.8 to 71.5) | |
| ≥85 | 34 056 (2.7) | 90.4 (89.4 to 91.4) | 3.92 (3.90 to 3.94) | 80.4 (79.4 to 81.3) | |
| Sex | Men | 569 087 (45.9) | 43.6 (43.4 to 43.7) | 1.06 (1.06 to 1.07) | 24.4 (24.3 to 24.5) |
| Women | 671 840 (54.1) | 53.8 (53.7 to 54.0) | 1.55 (1.54 to 1.55) | 34.9 (34.7 to 35.0) | |
| Number of conditions | 0 | 631 299 (50.9) | – | – | – |
| 1 | 236 547 (19.1) | – | – | – | |
| 2 | 128 263 (10.3) | – | – | – | |
| 3 | 83 751 (6.7) | – | – | – | |
| 4 | 57 501 (4.6) | – | – | – | |
| 5 | 39 159 (3.2) | – | – | – | |
| 6 | 25 567 (2.1) | – | – | – | |
| 7 | 16 259 (1.3) | – | – | – | |
| ≥8 | 22 581 (1.8) | – | – | – |
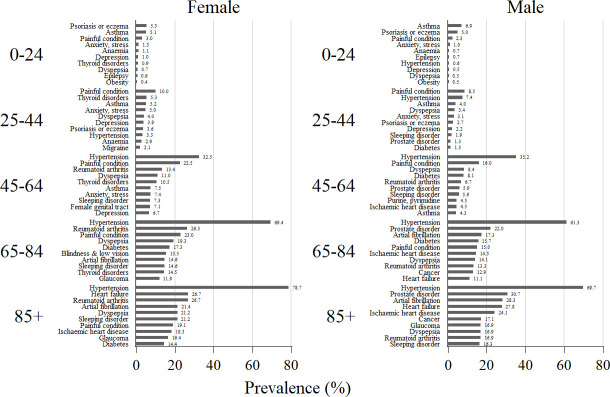
The prevalence of any chronic condition increased with age, from 18.2% (95% CI 18.0 to 18.3) in the youngest age group (0–24 years) to as high as 65.6% (95% CI 65.3 to 65.8) in the group of 45–64 years, and 90.4% (95% CI 89.4 to 91.4) among the oldest (85+ years) (table 1). In the youngest age group, 0–24 years, the mean number of conditions was 0.23 (0.22–0.23), and it increased with age, reaching 3.22 (3.21–3.22) in age 65–84 years and 3.92 (3.90–3.94) among those aged ≥85 years. The prevalence and number of chronic conditions in 5-year age groups are presented in figure 1.
Figure 1.
Prevalence of chronic conditions and multimorbidity (in numbers) by 5-year age groups.
The prevalence of MM also increased with age, from 3.5% (95% CI 3.5 to 3.6) among those younger than 25 years to as high as 80.4% (95% CI 79.4 to 81.3) among those aged ≥85 years. MM prevalence was higher among women than men, with about every third woman and every fourth man having MM. At a younger age, the prevalence of MM among women was comparable to that in men: the prevalence ratio (PR women/men) was 1.00 (95% CI 0.99 to 1.02) in the age group of 0–24 years. It increased gradually from 1.10 (95% CI 1.09 to 1.10) among those aged 25–29 years to 1.27 (95% CI 1.24 to 1.29) in 65–69 years, and declined again to be more similar between women and men among those aged ≥85 years (1.09, 95% CI 1.05 to 1.13).
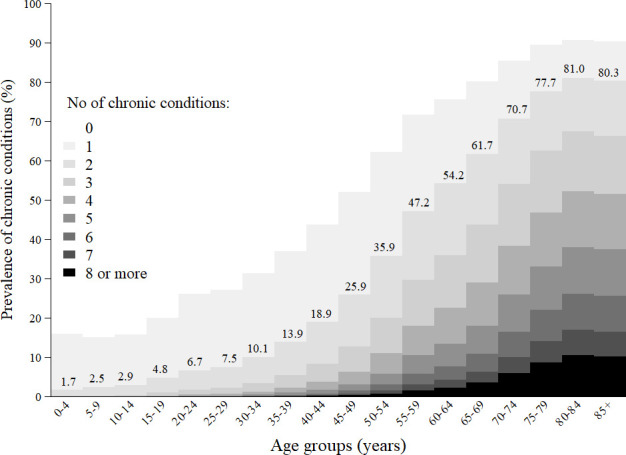
The prevalence of the 10 most common chronic conditions in men and women by age group is shown in figure 2, and the prevalence of all chronic conditions in the study (in the total population and among patients with MM) in the online supplemental appendix 1, table 1. Hypertension was the most frequent chronic condition in the three oldest age groups for both men and women. Hypertension affects one in four individuals (24.5 %) in the total population and about two-thirds (67.4%) among patients with MM.
Figure 2.
The prevalence of the 10 most common chronic conditions in men and women by age group.
Chronic pain ranked second with a prevalence of 12.4% in the total population and 32.3% among patients with MM. Chronic pain was defined according to Barnett et al1 as chronic pain associated with selected physical conditions such as osteoarthritis and low back pain (online supplemental appendix, table 1). The prevalence of painful conditions increases in older age as does the prevalence of cardiovascular diseases and conditions (eg, atrial fibrillation, ischaemic heart disease and heart failure).
Rheumatoid arthritis and other inflammatory arthropathies ranked third in the total population and patients with MM, with the respective prevalences of 7.6% and 23.6%. This condition was closely followed by dyspepsia, with 7.4% of the total population and 22.12% of patients with MM. The conditions with prevalence over 10% among patients with MM included diabetes, sleep disorders, atrial fibrillation, asthma, thyroid disorders, blindness and low vision, ischaemic heart diseases, anxiety and heart failure. In older men (65+ years), prostate disorders were frequent (22.8%), while in older women (65+ years) arthritis was quite prevalent (26.4%). Diseases such as asthma, diabetes and dyspepsia were common across all age groups. In younger age groups, asthma, chronic pain, psoriasis or eczema, and mental health conditions were most frequent.
Discussion
The disease burden from chronic conditions is high in Estonia. Half of the individuals had at least one chronic disorder, and one-third had MM. The burden is increasing with age, being high already among middle-aged population groups (aged 45–64 years), where 66% of individuals have a prevalent condition. Among those with MM, hypertension was the most prominent chronic condition, followed by chronic pain and arthritis.
Our results were overall very similar to the results of global and regional studies. A recent systematic review and meta-analysis of observational studies22 calculated an overall 33.1% pooled prevalence of MM. Still, their estimate of MM for the high-income countries in that review was 37.9%, whereas our estimate of 30.1% is a bit lower, apparently due to the methodological differences discussed above. As described earlier in the background, disability-free life expectancy is low for Estonia, perhaps owing to the relatively high burden of MM. Comparing our results to the Scottish primary care research, MM was higher in our study (30.1% compared with 23.2% in Scotland).1 Age group comparisons reveal that MM is more prevalent in Estonia in all age groups, especially in 45–64 years (41.0% in Estonia vs 30.4% in Scotland) and 65–84 years (71.1% vs 64.9%), except for the ≥85 years age group, where it is very similar (80.4% vs 81.5%).
As for the types of prevalent chronic conditions, our findings converge with several other studies that identified hypertension, diabetes, asthma and arthritis as the most prevalent conditions. In a recent Canadian study, the top five chronic conditions of the 17 examined among those with MM were mood disorders, hypertensive disorders, asthma, arthritis and diabetes.32 Lenzi et al found that hypertension, diabetes and depression were highly prevalent among Italians.33 Our national data also concur that morbidity increases with age, an association that has been demonstrated in other studies as well.1 3 32–34 In a Canadian study of self-reported chronic conditions, the prevalence of more than 3 conditions increased with age from 30% in the 45–49-year-old age group to 52% in individuals aged 60–64 years.34 In Lithuania, the risk of acquiring an additional chronic condition was found to increase exponentially from the age of 29 years and stabilise between the age of 51 years and 57 years.35 36
Acknowledging the sex gap in health that is characteristic of Eastern Europe, we aimed to assess the sex-specific differences in MM. We found that in women aged 25+ years, the prevalence of MM is higher than men, with the largest difference among those aged 65–69 years. This elevated prevalence of MM among women has been confirmed in some studies3 34 but not in others.32
Some limitations of our study may affect generalisability. First, the definition of a chronic condition used in our study is contestable. However, we sought to ensure conformance with the methodologies used in prior research and establish the chronicity of the disease. Thus, the healthcare claim or prescription with a specific condition had to be identified at least two times during the period of observation. The second limitation is the heterogeneous MM prevalence estimates due to methodological differences, including the MM definition, the list and grouping of conditions accounted for, the age range, data source and collection of data.37 38 A universal definition and list of conditions used for MM research do not exist.38 We attempted to optimise generalisability by adopting the list from previous research. To allow accurate estimations of disease burden, and effective disease management and resource distribution, a standardised operationalisation of MM are needed.1 22 Third, it is possible that some people with chronic conditions did not visit a physician or made only one visit over the study period, thus the under-ascertainment of conditions cannot be ruled out. Fourth, the EHIF database covers approximately 95% of the population but lacks the data for approximately 5% of uninsured individuals.31 However, given that all individuals aged 64 years and older are covered by health insurance, we acknowledge that a minor ascertainment bias may exist in younger age groups, as the health data for the uninsured individuals were not available. Fifth, not all individuals who were insured at the date of observation (31 December 2017) were insured during the entire 3-year study period, which might result in minor under-ascertainment among those newly enrolled.
One of the strengths of our study is the effort expended to enable comparability with the results of other studies. We used the list of conditions from previous research1 29 30 36 with only minor adjustments to reflect the regional diagnostic practices. Another strength of our analysis lies in the use of a data source with 95% nationwide coverage and complete follow-up, free of recall and social desirability biases. Furthermore, the validity of EHIF data, although established for financial and not health research purposes, has been tested recently39 and the study concluded that these data can be used for monitoring changes in chronic condition prevalence with a precision sufficient for informing healthcare policy. Our study thus provides high validity and generalisability of results allowing inferences to other eastern European populations.
Conclusions
The prevalence of MM in Estonia is relatively high compared with other European countries, and higher among women than men. The prevalence of MM increases with age, with hypertension the most frequent chronic condition, followed by chronic pain and arthritis. As the public health infrastructure continues to modernise, efforts must be placed on primary prevention of the conditions, which lead to hypertension, such as obesity. The development of patient-centred, evidence-based treatment recommendations will help align patient and physician with respect to health goals and the means to achieve these outcomes.
Supplementary Material
Footnotes
Contributors: MJ, RK, HP, AU and MO conceptualised and designed the study. MJ and HP collected, managed and analysed the data. All co-authors contributed to the interpretation of the findings and drafting of the manuscript. MJ wrote the original draft, and MJ and KL wrote the final version. HP provided visualisations. All co-authors approved the final version for submission.
Funding: This work was supported by the Estonian Ministry of Education and Research (grant number: IUT34-17).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository. Data are available upon reasonable request. The authors confirm that all data associated with the study are fully available without restriction from the Estonian Health Insurance Fund at https://www.haigekassa.ee/en. The data can be requested by completing the application at the following address: https://ankeet.haigekassa.ee/surveys/?s=4KXEPFDEKF or sending a written request to info@haigekassa.ee.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The study was conducted in accordance with local data protection regulations. The study was approved by the Tartu University Research Ethics Committee (280/T-7, 19.2018). The ethics committee waived the requirement for informed consent for the analysis presented in the manuscript.
References
- 1.Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. The Lancet 2012;380:37–43. 10.1016/S0140-6736(12)60240-2 [DOI] [PubMed] [Google Scholar]
- 2.Kingston A, Robinson L, Booth H, et al. Projections of multi-morbidity in the older population in England to 2035: estimates from the population ageing and care simulation (PACSim) model. Age Ageing 2018;47:374–80. 10.1093/ageing/afx201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van Oostrom SH, Gijsen R, Stirbu I, et al. Time trends in prevalence of chronic diseases and multimorbidity not only due to aging: data from general practices and health surveys. PLoS One 2016;11:e0160264. 10.1371/journal.pone.0160264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bähler C, Huber CA, Brüngger B, et al. Multimorbidity, health care utilization and costs in an elderly community-dwelling population: a claims data based observational study. BMC Health Serv Res 2015;15:23. 10.1186/s12913-015-0698-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Oostrom SH, Picavet HSJ, de Bruin SR, et al. Multimorbidity of chronic diseases and health care utilization in general practice. BMC Fam Pract 2014;15:1–9. 10.1186/1471-2296-15-61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Quinaz Romana G, Kislaya I, Cunha Gonçalves S, et al. Healthcare use in patients with multimorbidity. Eur J Public Health 2020;30:16–22. 10.1093/eurpub/ckz118 [DOI] [PubMed] [Google Scholar]
- 7.Nielsen CR, Halling A, Andersen-Ranberg K. Disparities in multimorbidity across Europe – Findings from the SHARE Survey. Eur Geriatr Med 2017;8:16–21. 10.1016/j.eurger.2016.11.010 [DOI] [Google Scholar]
- 8.Aminisani N, Stephens C, Allen J, et al. Socio-Demographic and lifestyle factors associated with multimorbidity in New Zealand. Epidemiol Health 2020;42:e2020001. 10.4178/epih.e2020001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ashworth M, Durbaba S, Whitney D, et al. Journey to multimorbidity: longitudinal analysis exploring cardiovascular risk factors and sociodemographic determinants in an urban setting. BMJ Open 2019;9:e031649. 10.1136/bmjopen-2019-031649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nunes BP, Batista SRR, de AFB. Multimorbidity: the Brazilian longitudinal study of aging (ELSI-Brazil). Rev Saude Publica 2018;52 Suppl 2:10s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flores T, Rodrigues AP, Neves R. The risk of multimorbidity associated with overweight and obesity: data from the Brazilian National health survey 2013. J Obes Metab Syndr 2021;30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wikström K, Lindström J, Harald K, et al. Clinical and lifestyle-related risk factors for incident multimorbidity: 10-year follow-up of Finnish population-based cohorts 1982–2012. Eur J Intern Med 2015;26:211–6. 10.1016/j.ejim.2015.02.012 [DOI] [PubMed] [Google Scholar]
- 13.Fortin M, Soubhi H, Hudon C, et al. Multimorbidity’s many challenges. BMJ 2007;334:1016–7. 10.1136/bmj.39201.463819.2C [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hurst JR, Agarwal G, van Boven JFM, et al. Critical review of multimorbidity outcome measures suitable for low-income and middle-income country settings: perspectives from the global alliance for chronic diseases (GACD) researchers. BMJ Open 2020;10:e037079. 10.1136/bmjopen-2020-037079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Atun R, Gurol–Urganci I, Hone T, et al. Shifting chronic disease management from hospitals to primary care in Estonian health system: analysis of national panel data. J Glob Health 2016;6. 10.7189/jogh.06.020701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chudasama YV, Gillies CL, Appiah K, et al. Multimorbidity and SARS-CoV-2 infection in UK Biobank. Diabetes Metab Syndr 2020;14:775–6. 10.1016/j.dsx.2020.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Honardoost M, Janani L, Aghili R, et al. The association between presence of comorbidities and COVID-19 severity: a systematic review and meta-analysis. Cerebrovasc Dis 2021;50:132–40. 10.1159/000513288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thakur B, Dubey P, Benitez J. A systematic review and meta-analysis of geographic differences in comorbidities and associated severity and mortality among individuals with COVID-19. Sci Reports 2021;111:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clark A, Jit M, Warren-Gash C, et al. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Glob Health 2020;8:e1003–17. 10.1016/S2214-109X(20)30264-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fernández-Niño JA, Guerra-Gómez JA, Idrovo AJ. Multimorbidity patterns among COVID-19 deaths: proposal for the construction of etiological models. Rev Panam Salud Publica 2020;44:e166. 10.26633/RPSP.2020.166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sathanapally H, Sidhu M, Fahami R, et al. Priorities of patients with multimorbidity and of clinicians regarding treatment and health outcomes: a systematic mixed studies review. BMJ Open 2020;10:e033445. 10.1136/bmjopen-2019-033445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nguyen H, Manolova G, Daskalopoulou C, et al. Prevalence of multimorbidity in community settings: a systematic review and meta-analysis of observational studies. J Comorb 2019;9:2235042X1987093. 10.1177/2235042X19870934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dicker D, Nguyen G, Abate D, et al. Global, regional, and national age-sex-specific mortality and life expectancy, 1950–2017: a systematic analysis for the global burden of disease study 2017. The Lancet 2018;392:1684–735. 10.1016/S0140-6736(18)31891-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.TE75: Disability Free Life Expectancy by Sex and Age Group . Health Statistics and Health Research Database, National Institute of Health Development, Tallinn, Estonia, 2020. Available: https://statistika.tai.ee/index_en.html
- 25.Estonian Health Insurance Fund . Estonian health care system, 2021. Available: https://www.haigekassa.ee/en/people/health-care-services/estonian-health-care-system
- 26.Lai T, Knai C. Assessing chronic disease management in European health systems: Country reports: Estonia. In: Nolte E, Knai C, eds. Assessing chronic disease management in European health systems: Country reports. Copenhagen: World Health Organization, 2015: 37–42. [PubMed] [Google Scholar]
- 27.Silina V, Kalda R. Challenges for clinical practice and research in family medicine in reducing the risk of chronic diseases. notes on the EGPRN spring conference 2017 in Riga. Eur J Gen Pract 2018;24:112–7. 10.1080/13814788.2018.1429594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eesti Haigekassa . Estonian health insurance fund. Annu. Rep, 2017. Available: https://www.haigekassa.ee/
- 29.van den Bussche H, Koller D, Kolonko T, et al. Which chronic diseases and disease combinations are specific to multimorbidity in the elderly? results of a claims data based cross-sectional study in Germany. BMC Public Health 2011;11:101. 10.1186/1471-2458-11-101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schäfer I, von Leitner E-C, Schön G, et al. Multimorbidity patterns in the elderly: a new approach of disease clustering identifies complex interrelations between chronic conditions. PLoS One 2010;5:e15941. 10.1371/journal.pone.0015941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Statistics Estonia . PO021: population, 1 January by sex, year and age group, 2017. Available: https://www.stat.ee/database
- 32.Ryan BL, Bray Jenkyn K, Shariff SZ, et al. Beyond the grey tsunami: a cross-sectional population-based study of multimorbidity in Ontario. Can J Public Health 2018;109:845–54. 10.17269/s41997-018-0103-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lenzi J, Avaldi VM, Rucci P, et al. Burden of multimorbidity in relation to age, gender and immigrant status: a cross-sectional study based on administrative data. BMJ Open 2016;6:e012812. 10.1136/bmjopen-2016-012812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sakib MN, Shooshtari S, St. John P, et al. The prevalence of multimorbidity and associations with lifestyle factors among middle-aged Canadians: an analysis of Canadian longitudinal study on aging data. BMC Public Health 2019;19:1–13. 10.1186/s12889-019-6567-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jurevicienė E, Onder G, Visockienė Ž, et al. Does multimorbidity still remain a matter of the elderly: Lithuanian national data analysis. Health Policy 2018;122:681–6. 10.1016/j.healthpol.2018.03.003 [DOI] [PubMed] [Google Scholar]
- 36.Navickas R, Visockienė Ž., Puronaitė R, et al. Prevalence and structure of multiple chronic conditions in Lithuanian population and the distribution of the associated healthcare resources. Eur J Intern Med 2015;26:160–8. 10.1016/j.ejim.2015.02.015 [DOI] [PubMed] [Google Scholar]
- 37.Diederichs C, Berger K, Bartels DB. The measurement of multiple chronic diseases-a systematic review on existing multimorbidity indices. J Gerontol A Biol Sci Med Sci 2011;66A:301–11. 10.1093/gerona/glq208 [DOI] [PubMed] [Google Scholar]
- 38.Fortin M, Stewart M, Poitras M-E, et al. A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. The Annals of Family Medicine 2012;10:142–51. 10.1370/afm.1337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Otsa K, Talli S, Harding P, et al. Administrative database as a source for assessment of systemic lupus erythematosus prevalence: Estonian experience. BMC Rheumatol 2019;3:1–6. 10.1186/s41927-019-0074-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-049045supp001.pdf (57.9KB, pdf)
Data Availability Statement
Data are available in a public, open access repository. Data are available upon reasonable request. The authors confirm that all data associated with the study are fully available without restriction from the Estonian Health Insurance Fund at https://www.haigekassa.ee/en. The data can be requested by completing the application at the following address: https://ankeet.haigekassa.ee/surveys/?s=4KXEPFDEKF or sending a written request to info@haigekassa.ee.