Description
A 50-year-old man had bilateral inferior atrophic patches on the iris with visible iris fibrils (shredded-wheat appearance) some of which were floating in the anterior chamber (figure 1).1 There was no previous history of pain, redness, trauma or any ocular procedure. Corneal sensation was normal in both eyes. Anterior segment optical coherence tomography shows disruption of the anterior limiting layer of the iris, shadow due to floating iris tissue in the anterior chamber, intact pigmented epithelium of the iris and splitting of the stroma with moth-eaten appearance (figure 2) suggestive of iridoschisis.2 Iridoschisis is often associated with angle-closure glaucoma, corneal oedema or lens abnormalities.3 4 It is necessary to follow-up with these patients to screen for such changes and treat them accordingly.4
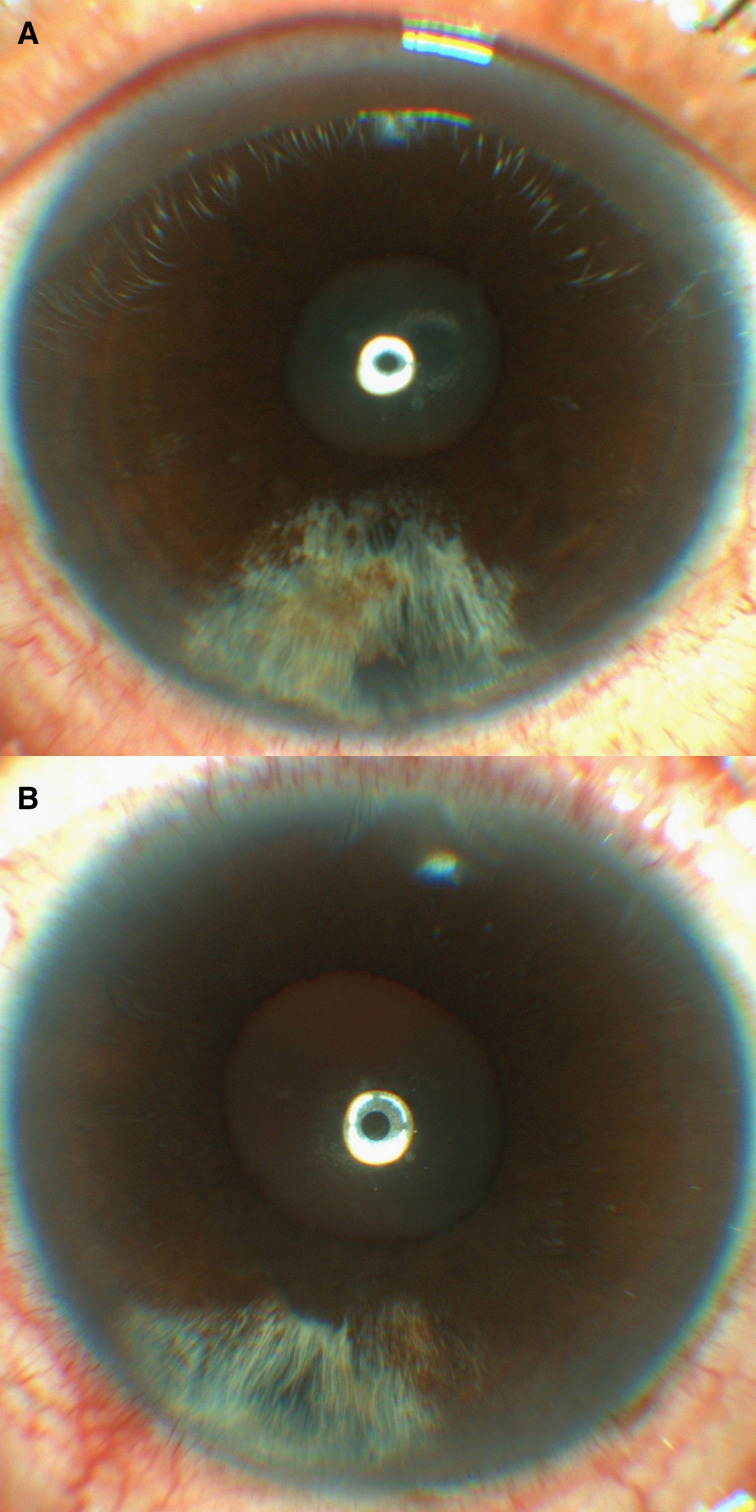
Figure 1.
Slit-lamp photo of the right (A) and the left (B) eye showing an inferior patch of iris atrophy and a shredded-wheat appearance.
Figure 2.
The anterior segment optical coherence tomography of the right eye (A and B) and the left eye (C and D) showing disruption of the anterior limiting layer of the iris, splitting of the stroma with moth-eaten appearance (orange arrow), shadow due to floating iris tissue (yellow arrow) in the anterior chamber and intact pigmented epithelium of the iris (arrowheads) suggestive of iridoschisis.
Learning points.
Iridoschisis usually presents as bilateral inferior atrophic patches of the iris.
Anterior segment optical coherence tomography demonstrates the alterations in the affected iris vividly.
Regular follow-up is required to screen for glaucoma, cornea and lens-related abnormalities.
Acknowledgments
Dr Gopal Bandyopadhyay, Dr Himanshu Shekhar, Dr Kishore Kumar Vatwani, Dr Koushik Basu.
Footnotes
Twitter: @koushiktripathy
Contributors: KT diagnosed the condition, investigated and advised treatment. RA was involved in collection of images with valid consent. KT and RA was involved in drafting the manuscript of the case report. KT, MJ and RA revised the manuscript and maintained the standards of the manuscript as per BMJ protocols. The final manuscript was approved by all the four authors, that is, RA, KT and MJ. All authors are responsible for the integrity and accuracy of the data provided.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
References
- 1.Chen Y, Qian Y, Lu P. Iridoschisis: a case report and literature review. BMC Ophthalmol 2017;17:1–6. 10.1186/s12886-017-0418-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Paniagua L, Bande MF, Rodríguez-Ares MT, et al. A presentation of iridoschisis with plateau iris: an imaging study. Clin Exp Optom 2015;98:290–1. 10.1111/cxo.12250 [DOI] [PubMed] [Google Scholar]
- 3.Omoto T, Agata C, Akiyama R, et al. Iridotrabecular and iridocorneal contact changes after cataract surgery and endothelial keratoplasty in bilateral Iridoschisis. Case Rep Ophthalmol 2021;12:198–203. 10.1159/000513793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pieklarz B, Grochowski ET, Saeed E, et al. Iridoschisis-A systematic review. J Clin Med 2020;9:3324–20. 10.3390/jcm9103324 [DOI] [PMC free article] [PubMed] [Google Scholar]