Abstract
Objectives
This study sought to determine whether the increased use of telehealth was associated with a difference in outcomes for outpatients with heart failure.
Background
The COVID-19 pandemic led to dramatic changes in the delivery of outpatient care. It is unclear whether increased use of telehealth affected outcomes for outpatients with heart failure.
Methods
In March 2020, a large Midwestern health care system, encompassing 16 cardiology clinics, 16 emergency departments, and 12 hospitals, initiated a telehealth-based model for outpatient care in the setting of the COVID-19 pandemic. A propensity-matched analysis was performed to compare outcomes between outpatients seen in-person in 2018 and 2019 and via telemedicine in 2020.
Results
Among 8,263 unique patients with heart failure with 15,421 clinic visits seen from March 15 to June 15, telehealth was employed in 88.5% of 2020 visits but in none in 2018 or 2019. Despite the pandemic, more outpatients were seen in 2020 (n = 5,224) versus 2018 and 2019 (n = 5,099 per year). Using propensity matching, 4,541 telehealth visits in 2020 were compared with 4,541 in-person visits in 2018 and 2019, and groups were well matched. Mortality was similar for telehealth and in-person visits at both 30 days (0.8% vs 0.7%) and 90 days (2.9% vs 2.4%). Likewise, there was no excess in hospital encounters or need for intensive care with telehealth visits.
Conclusions
A telehealth model for outpatients with heart failure allowed for distanced encounters without increases in subsequent acute care or mortality. As the pressures of the COVID-19 pandemic abate, these data suggest that telehealth outpatient visits in patients with heart failure can be safely incorporated into clinical practice.
Key Words: cardiomyopathy, electronic medical record, telehealth visits, video visits
Abbreviations and Acronyms: APP, advanced practice practitioner; ED, emergency department; HF, heart failure; ICU, intensive care unit; IQR, interquartile range
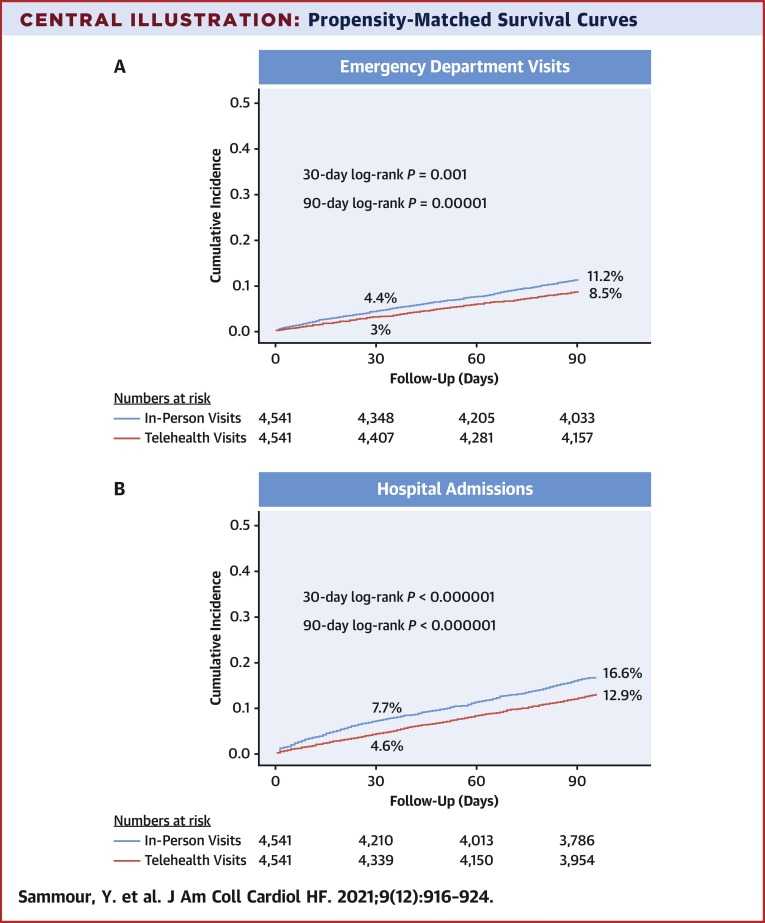
Central Illustration
The COVID-19 crisis created unprecedented challenges to health care delivery, leading to a dramatic transformation in the processes of outpatient care (1). Furthermore, excess mortality has been reported in 2020 compared with in previous years, with only about two-thirds related to COVID-19 infections (2). The remaining excess mortality may be attributable to several factors, including a delay in patients seeking medical attention for non-COVID-19 illnesses. Given the imposition of stay-at-home orders and the hesitancy of patients to leave home in the initial stages of the pandemic, there was a need for an abrupt transition to outpatient telehealth visits that involve distanced real-time interaction between patients and providers using audio and/or video capabilities without direct physical interaction (3,4). This was encouraged by professional societies (5) and facilitated by Centers for Medicare and Medicaid Services and private payers by reimbursing telehealth visits at equal rates to in-person visits (3). The rapid need to transition to telehealth services mandates an understanding of potential adverse outcomes associated with this transition (6) to help inform future telemedicine use in the heart failure (HF) population.
HF is a particularly important disease for which to examine the impact of telehealth, as it is a chronic condition necessitating continual assessment of symptoms, health status, and medication adjustment (7). Moreover, patients with HF are a particularly vulnerable population for complications related to COVID-19 infection, including critical illness and mortality (8). At the start of the pandemic, our large Midwestern health care system transitioned to a predominantly telehealth-based model. This report describes the changes in delivering outpatient care for patients with HF during 2020 and compares outcomes to similar periods in 2018 and 2019.
Methods
The Saint Luke’s Health System is a large Midwestern health care system that comprises 16 different cardiology clinics, 16 emergency department (ED) locations, and 12 hospitals across the greater Kansas City metro area and surrounding suburbs in both Missouri and Kansas. Our cardiology medical team consists of 113 different providers including 66 attending cardiologists and 47 advanced practice providers (APPs) (Supplemental Figure 1). We conducted a retrospective study of patients who were seen at Saint Luke’s Health System cardiology clinics from March 15 to June 15, 2020, and compared them with patients seen during the same time period in 2018 and 2019. The exposure variable was the type of outpatient visit, defined as either in-person or telehealth (video or telephone virtual visit). Outpatient encounter characteristics, demographics, comorbidities, and outcomes were extracted from the electronic medical record (Epic) by including patients with International Classification of Diseases-Tenth Revision codes of primary or secondary HF diagnoses in their problem list at the outpatient encounter (Supplemental Table 1). Other comorbid diagnoses were also extracted from the electronic medical record problem list. We excluded patients with a heart transplant or left ventricular assist device. The study was approved by our Institutional Review Board and ethics committee, and informed consent was waived.
Continuous variables were expressed as mean ± SD and compared using Student’s t-test. Categorical variables were expressed as percentages and compared using chi-square tests. The main study outcomes included all-cause death, ED visits, hospital admissions, and need for intensive care unit (ICU) at 30 and 90 days after the index in-person visit. ED visits referred to patients who presented to the ED and were discharged without hospital admission. For patients with multiple ED visits or hospital admissions after the index clinic visit, the first occurrence was used. For unadjusted analyses, time to the various outcomes were assessed using Kaplan-Meier curves and the log-rank test.
To address differences in telehealth versus in-person visits, we matched patients on the likelihood of having a telehealth visit by creating a propensity score with telehealth visits as the dependent variable and the following variables as independent variables: age; sex; White race; Hispanic ethnicity; acute HF; HF with reduced ejection fraction; hypertension; diabetes; chronic kidney disease stage ≥3; coronary artery disease; prior myocardial infarction, percutaneous coronary intervention, and/or coronary artery bypass grafting; prior stroke; atrial fibrillation; prior ventricular tachycardia; implantable cardioverter-defibrillator; COVID-19 infection; and appointment scheduled within 48 hours. In-person visits in 2018 and 2019 were matched 1:1 with telehealth visits in 2020. We used a caliper width of 0.2× the SD of the logit of the propensity score and used a standardized difference of 10 to be the marker of balance. Survival curves were then constructed based on the propensity-matched analysis. A 2-tailed P value of 0.05 was used for significance testing throughout the study. Statistical analyses were conducted using SPSS version 27.0 (SPSS Inc) and SAS version 9.4 (SAS Institute).
Results
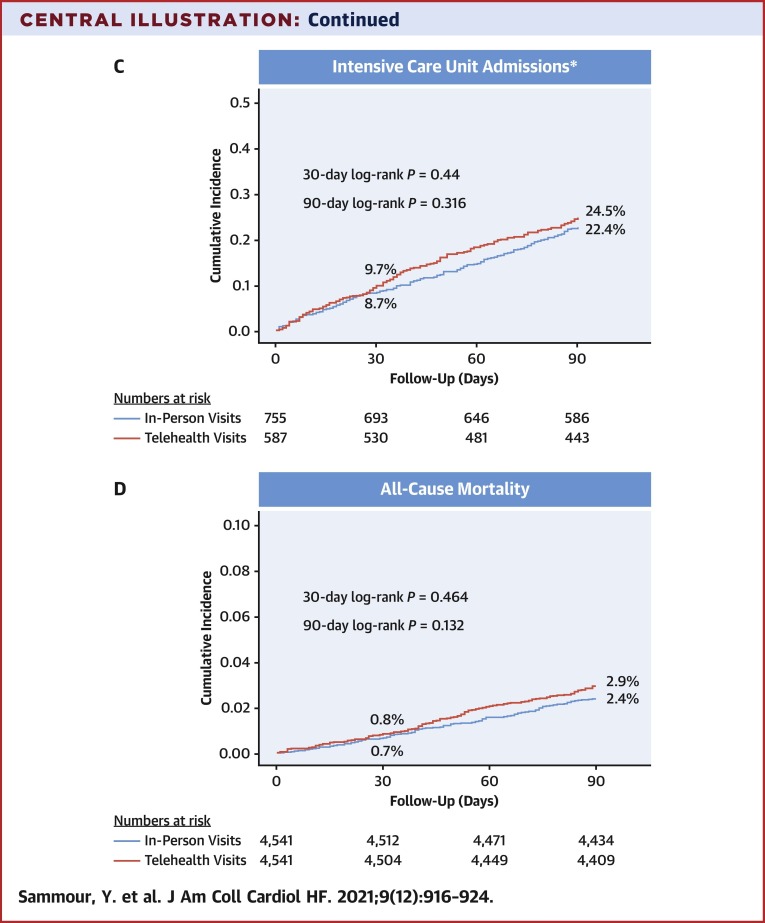
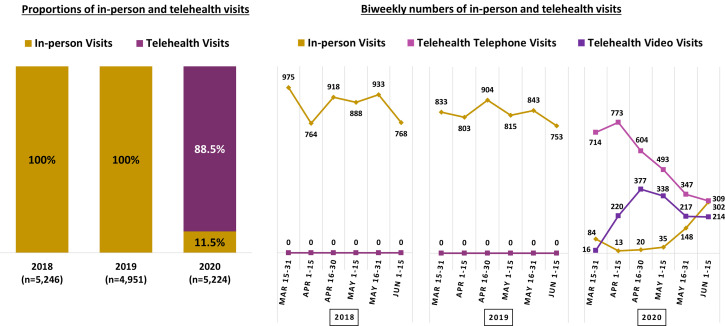
We identified 8,263 unique patients with HF with 15,421 clinic visits that included 5,246 visits in 2018, 4,951 visits in 2019, and 5,224 visits in 2020. Telehealth was not used in either 2018 or 2019, yet the vast majority of encounters were telehealth during the study period in 2020 (88.5% of visits with 70% telephone and 30% video) beginning March 16, 2020 (Figure 1 ). In fact, more unique patients were seen in 2020 (n = 4,063) than in 2018 and 2019 (n = 3,675 and n = 3,619, respectively) (Supplemental Figure 2). Across years, there was no difference in the proportion of patients seen by physicians versus APPs, nor in patients seen by HF specialists versus nonspecialists (Figure 2 ). Of the total 2020 visits, more video visits were conducted by physicians than by APPs (29% vs 22%; P < 0.001) and by HF providers than by other cardiology providers (30% vs 25%; P < 0.001) (Figure 2).
Figure 1.
Trends in In-Person Versus Telehealth Visits
Proportions and biweekly numbers of clinic encounters according to the mode of visit.
Figure 2.
In-Person Versus Telehealth Visits by Provider Type
Distribution of clinic visits according to provider type and mode of visit (all visits in 2018 and 2019 were in-person). APP = advanced practice provider; HF = heart failure.
Baseline characteristics of the entire cohort before matching are found in Supplemental Table 2. The mean age was slightly lower in 2020 than in 2018 and 2019 (70.5 years vs 71.4 years; P < 0.001). Visits in patients with systolic HF were similar across the 3 years, although acute HF diagnoses were significantly lower in 2020 than in 2018 and 2019 (6.8% vs 10.2%; P < 0.001), and lower for telehealth visits than for in-person visits performed during 2020 (5.8% vs 14%; P < 0.001). Visits scheduled within the prior 48 hours were more common in 2020 than in prior years (15.9% vs 8.1%; P < 0.001) and were also more common in 2020 for in-person visits versus telehealth visits (18.4% vs 15.6%; P < 0.001). Known COVID-19 infections were rare and occurred before or within 90 days of outpatient visit in 0.4% of patients.
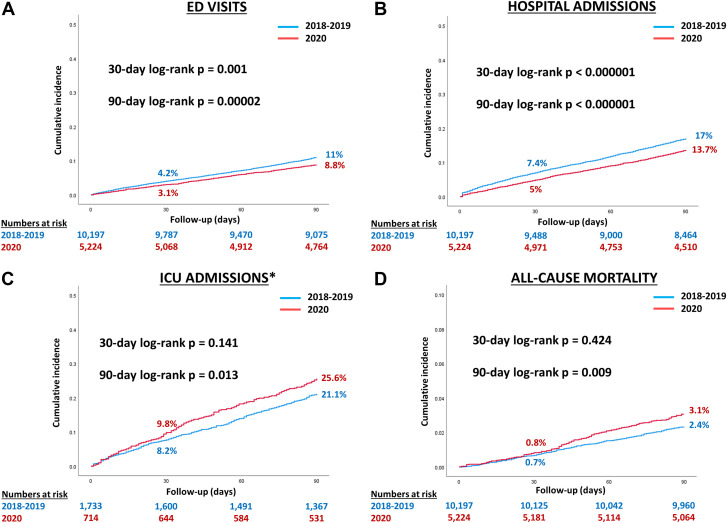
At 90 days following the index outpatient visit, there were 1,582 ED visits, 2,447 hospitalizations, 549 ICU admissions, and 400 deaths. Unadjusted outcomes were first compared for 2020 versus 2018 and 2019 and demonstrated fewer ED visits and hospital admissions in 2020 at both 30 and 90 days (Figure 3 ). Among patients who were hospitalized, there was higher acuity of care indicated by increased need for ICU stays within 90 days in 2020 despite no differences at 30 days. All-cause death was similar at 30 days but higher at 90 days in 2020 compared with in 2018 and 2019. In 2020 versus 2018 and 2019, there were no differences in the length of hospital stay (median: 3.9 days [interquartile range (IQR): 2.2-6.6 days] vs 3.7 days [IQR: 2.1-6.4 days]; P = 0.402), the rates of hospice (3.5% vs 2.4%; P = 0.115), or rates of home discharges (77.0% vs 78.8%; P = 0.344). Comparing telehealth to in-person visits among all years, there was no difference in the rates of all-cause mortality or need for intensive care. However, there were lower rates of ED visits and hospital admissions with telehealth visits compared with in-person visits, as all telehealth visits were performed in 2020 (Supplemental Table 2). Rates of ED visits and hospitalizations after in-person office visits in 2020 were similar to the rates seen in prior years both at 30 days (3.5% vs 4.2% for ED visits, 7.3% vs 7.4% for hospitalizations) and 90 days (11.3% vs 11.0% for ED visits, 18.4% vs 17.0% for hospitalizations).
Figure 3.
Unadjusted Survival Curves by Year
Unadjusted outcomes according to year, demonstrating fewer emergency department (ED) visits and hospital admissions (A and B) and more intensive care unit (ICU) admissions and all-cause mortality (C and D) in 2020 versus prior years. ∗ICU admissions as a percentage of patients hospitalized.
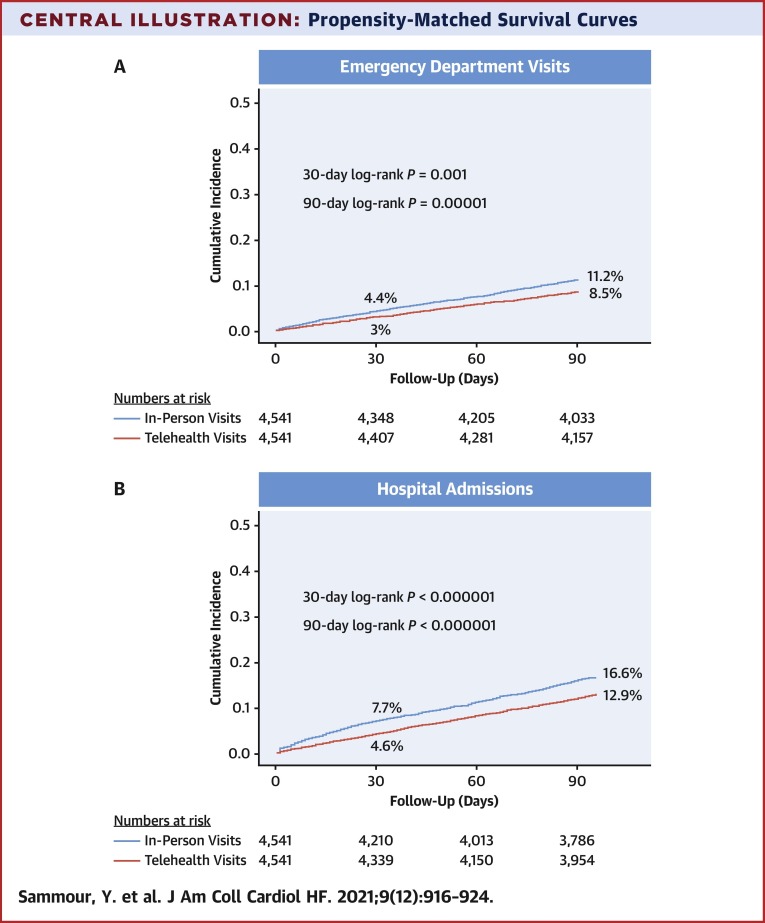
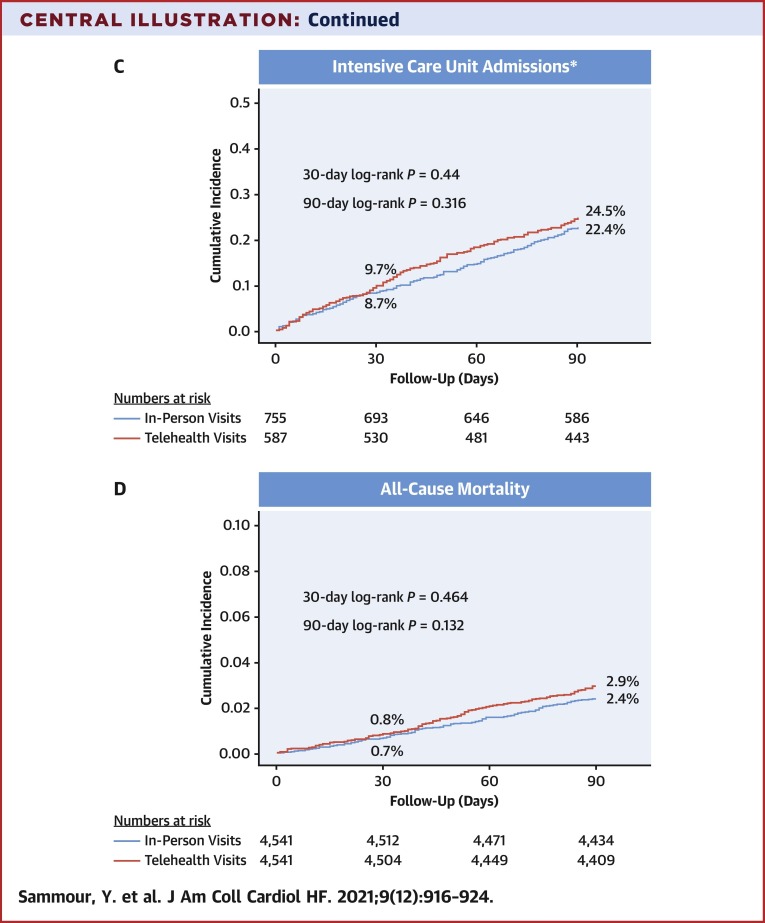
Propensity-matched analysis
The propensity-matched cohort included 4,541 patients with in-person visits in 2018 and 2019 and 4,541 patients with telehealth visits in 2020. There were no significant differences in baseline characteristics between the matched cohorts (Table 1 , standard difference plot in Supplemental Figure 3). Admissions to the ED or hospital were lower after the telehealth visits than after in-person visits at both 30 days (6.8% vs 10.4%) and 90 days (17.9% vs 23.3%; P < 0.001 for both) (Central Illustration ). Among hospitalized patients, there was no difference in ICU admissions between telehealth and in-person visits at either 30 or 90 days. Similarly, there was no difference in mortality at either 30 (0.8% vs 0.7%; P = 0.465) or 90 days (2.9% vs 2.4%; P = 0.133).
Table 1.
Baseline Characteristics After Matching
| In-Person Visits (n = 4,541) | Telehealth Visits (n = 4,541) | P Value | |
|---|---|---|---|
| Year of visit | <0.001 | ||
| 2018 | 2,325 (51.2) | 0 (0.0) | |
| 2019 | 2,216 (48.8) | 0 (0.0) | |
| 2020 | 0 (0.0) | 4,541 (100.0) | |
| Provider type | 0.316 | ||
| Physician | 2,891 (63.7) | 2,845 (62.7) | |
| Advanced practice provider | 1,650 (36.3) | 1,696 (37.3) | |
| Heart failure provider | 1,287 (28.3) | 1,365 (30.1) | 0.071 |
| Scheduled within 48 h of visit date | 667 (14.7) | 651 (14.3) | 0.633 |
| Age, y | 71.1 ± 13.8 | 70.8 ± 14.0 | 0.311 |
| Male | 2,495 (54.9) | 2,474 (54.5) | 0.657 |
| Race | 0.807 | ||
| White | 3,742 (82.4) | 3,712 (81.7) | |
| Black | 682 (15.0) | 700 (15.4) | |
| Asian | 21 (0.5) | 22 (0.5) | |
| Other | 96 (2.1) | 107 (2.4) | |
| Hispanic ethnicity | 94 (2.1) | 102 (2.3) | 0.549 |
| Payer source | 0.039 | ||
| Medicare | 2,195 (48.6) | 2,113 (46.9) | |
| Commercial | 2,049 (45.4) | 2,048 (45.5) | |
| Medicaid | 194 (4.3) | 251 (5.6) | |
| Other government | 24 (0.5) | 31 (0.7) | |
| Self-pay | 54 (1.2) | 60 (1.3) | |
| Acute heart failure | 262 (5.8) | 269 (5.9) | 0.754 |
| Systolic heart failure | 1,982 (43.6) | 2,032 (44.7) | 0.290 |
| Hypertension | 3,821 (84.1) | 3,836 (84.5) | 0.665 |
| Diabetes | 2,039 (44.9) | 2,089 (46.0) | 0.292 |
| Hyperlipidemia | 3,005 (66.2) | 2,973 (65.5) | 0.478 |
| Chronic kidney disease stage ≥3 | 1,459 (32.1) | 1,511 (33.3) | 0.244 |
| Coronary artery disease | 2,437 (53.7) | 2,367 (52.1) | 0.141 |
| Prior MI, PCI, or CABG | 1,652 (36.4) | 1,643 (36.2) | 0.844 |
| Prior stroke | 456 (10.0) | 468 (10.3) | 0.677 |
| Atrial fibrillation | 2,036 (44.8) | 2,019 (44.5) | 0.719 |
| Prior ventricular tachycardia | 897 (19.8) | 891 (19.6) | 0.874 |
| Implantable cardioverter defibrillator | 1,079 (23.8) | 1,043 (23.0) | 0.372 |
Values are n (%) or mean ± SD.
CABG = coronary artery bypass graft; MI = myocardial infarction, PCI = percutaneous coronary intervention.
Central Illustration.
Propensity-Matched Survival Curves
Outcomes according to mode of visit, demonstrating fewer emergency department (ED) visits and hospital visits in patients after a telehealth visit (A and B) and similar subsequent rates of intensive care unit (ICU) admission (C) and all-cause mortality (D). ∗ICU admissions as a percentage of patients hospitalized.
Discussion
The COVID-19 pandemic mandated a rapid change in the modes of health care delivery, and understanding the safety of this transformation is critical to rethinking the optimal design of care after the pandemic abates. Telehealth was rapidly adopted in our health system during the early phase of the pandemic in 2020. Among outpatients with a history of HF, telehealth visits were not associated with an increase in subsequent ED visits, hospital admissions, intensive care use, or all-cause mortality at either 30 or 90 days. Collectively, these data suggest that telehealth visits could be safely implemented.
In response to the pandemic, there was a remarkable transformation in the processes of outpatient care delivery (1). Many health care systems were forced to reduce their in-person outpatient visit capacity and instead pursue innovative solutions such as telehealth. The Heart Failure Society of America strongly recommended the outpatient use of telehealth for management of patients with HF during the COVID-19 era because telehealth offers multiple potential benefits including feasibility, increased access to care, ability to save time and costs, and patient satisfaction (5). Our health system effectively transitioned on March 16, 2020, to an almost entirely telehealth platform for outpatient visits; over a short period of time, we were able to conduct 4,622 telehealth visits for patients with HF, comprising 88.5% of the total visits during the study period, including 30% done by video and 70% by telephone. As our technical infrastructure had time to adapt and telehealth became more facile in our practice, an increasing percentage of outpatient telehealth visits were conducted as video visits. To decrease in-person patient and provider contacts, several physician and APP providers were transitioned from hospital service to outpatient telehealth clinic, enabling us to leverage our providers to reach a greater number of outpatients in 2020 compared with in prior years.
While limiting in-person patient/provider contact during the COVID-19 pandemic may have helped stem the tide of COVID-19 infections (9), there were concerns that this may potentially come at the cost of delaying care for other medical conditions, resulting in decreased hospitalizations among patients with HF compared with similar time periods in prior years (10). Furthermore, excess all-cause mortality (up to 20%) has been reported in the United States between March and the end of July 2020, with only two-thirds of that increase related to COVID-19, suggesting that a considerable number of patients died because of avoidance of care and late presentation to hospitals among other causes (2). More specifically, cardiovascular deaths increased by 8% during the pandemic including a 23% rise in deaths related to HF. This also included a 35% increase in deaths at home, and 32% at care homes and hospices (11). Our results confirm this unadjusted overall increase in all-cause mortality and increased acuity of illness in 2020 versus in prior years.
Our results are similar to limited comparative data regarding the outcomes of telehealth versus in-person encounters among outpatients with HF. Gorodeski et al (12) performed a randomized clinical trial among 108 postdischarge patients with HF seen between October 2018 and July 2019. The use of telehealth visits was not associated with changes in mortality, ED visits, or hospital admissions at 45 days in comparison with in-person visits, suggesting the safety of telehealth visits (12). Furthermore, Salzano et al (13) assessed the utility of telemedicine among 103 patients with HF in Italy seen during the early pandemic between March 11 and May 4, 2020, who received different telemedicine services including telephone visits (64%), online chats (34%), and video visits (2%). The use of telemedicine was associated with lower rates of hospitalizations for HF (2.9% vs 17.3%; P = 0.001), but similar rates of mortality (1.9% vs 2.9%; P > 0.05) in comparison with a cohort of 104 patients seen in-person during 2019 (13). The lower rates of ED visits and hospitalizations in the Salzano cohort and our cohort following telehealth visits in 2020 is likely related to the overall global climate where patients were less likely to seek in-person acute care because of the pandemic. It is also possible that patients who preferred telehealth visits were more likely to adhere to social distancing and more likely to avoid hospital care even when feeling sick. However, after adjustment, telehealth visits were not associated with increased mortality in our analysis. Due to the low rate of identified COVID-19 infections in our cohort, COVID-19 infection did not significantly drive outcomes including need for ICU or mortality.
After the first wave of the pandemic, we used a hybrid model of in-person and telehealth visits. Patients were seen in-person either by request or because they were acutely ill. In fact, patients who had in-person visits in 2020 had comparable rates of subsequent acute care visits as those who had in-person visits in 2018 and 2019. Underlying any hybrid telehealth model is the importance of careful selection of the mode of visit for the appropriate types of patients depending on the acuity of their conditions among other factors. Standardized quality of life assessments such as the Kansas City Cardiomyopathy Questionnaire can be employed prior to the outpatient visit to help triage patients to telehealth or in-person visits. This is an area for further research. Patient preference should also be considered, as many patients with HF are frail or may live a long distance from the clinic, making telehealth visits more attractive, particularly in the setting of stable symptomatology.
Study Limitations
This is a retrospective study from a single system. Limitations to propensity matching including the loss of participants related to matching and the inability to adjust for unmeasured confounders, specifically those related to the COVID-19 pandemic. Moreover, diagnoses were based on International Classification of Diseases-Tenth Revision codes in the medical record, and our data set lacked information regarding the rates of HF guideline-directed medical therapy used in our cohort, which may affect outcomes. Additionally, it is possible that subsequent ED visits or hospitalizations outside our health system were under-reported; although, we captured results from 16 ED locations and 12 hospitals in our health system. Finally, in this analysis, we did not identify the causes of death or the reasons for the hospital encounters. Further data are needed to confirm the relative safety of a telehealth strategy in the HF population over a more sustained period of time. Although, we hypothesize that greater risks would be observed early after telehealth visits, where patients’ acuity might be misjudged.
Conclusions
Rapid adoption of a telehealth model during the COVID-19 pandemic in patients with a diagnosis of HF facilitated continuity of care without increases in subsequent hospital encounters or mortality. Longer term multicenter cohorts are needed to better understand the methods to triage patients to telehealth visits and implications on outcomes in patients with HF.
Perspectives.
COMPETENCY IN MEDICAL KNOWLEDGE: Telehealth encounters for outpatients with HF are not associated with an increase in subsequent acute care or mortality compared to in-person visits. As the pressures of the COVID-19 pandemic abate, our data suggest that telehealth outpatient visits can be safely incorporated into clinical practice.
TRANSLATIONAL OUTLOOK: Future studies should evaluate methods to help triage patients to telehealth or in-person visits, which may include previsit patient-centered quality of life assessment.
Funding Support and Author Disclosures
Dr Spertus is the principal investigator of grants from National Institutes of Health, Abbott Vascular, and the American College of Cardiology Foundation; is a consultant to Janssen, Novartis, Amgen, Myokardia, AstraZeneca, Bayer, and Merck; serves on the Scientific Advisory Board of United Healthcare and the Board of Directors for Blue Cross Blue Shield of Kansas City; owns the copyright to the Kansas City Cardiomyopathy Questionnaire, Seattle Angina Questionnaire, and Peripheral Artery Questionnaire; and has an equity interest in Health Outcomes Sciences. Dr Sperry is a consultant to Pfizer and Alnylam. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Acknowledgment
The authors acknowledge Lynn Miller from Saint Luke’s Health System for his work on behalf of this manuscript.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental figures and tables, please see the online version of this paper.
Appendix
References
- 1.Mann D.M., Chen J., Chunara R., Testa P.A., Nov O. COVID-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc. 2020;27(7):1132–1135. doi: 10.1093/jamia/ocaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Woolf S.H., Chapman D.A., Sabo R.T., Weinberger D.M., Hill L., Taylor D.D.H. Excess deaths from COVID-19 and other causes, March-July 2020. JAMA. 2020;324(15):1562–1564. doi: 10.1001/jama.2020.19545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Medicare and Medicaid Services . Department of Health and Human Services; 2020. Medicare Telemedicine Health Care Provider Fact Sheet. Accessed June 10, 2021. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. [Google Scholar]
- 4.Kichloo A., Albosta M., Dettloff K., et al. Telemedicine, the current COVID-19 pandemic and the future: a narrative review and perspectives moving forward in the USA. Fam Med Community Health. 2020;8(3) doi: 10.1136/fmch-2020-000530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gorodeski E.Z., Goyal P., Cox Z.L., et al. Virtual visits for care of patients with heart failure in the era of COVID-19: a statement from the Heart Failure Society of America. J Card Fail. 2020;26(6):448–456. doi: 10.1016/j.cardfail.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bokolo A., Jr. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst. 2020;44(7):132. doi: 10.1007/s10916-020-01596-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mosterd A., Hoes A.W. Clinical epidemiology of heart failure. Heart. 2007;93(9):1137–1146. doi: 10.1136/hrt.2003.025270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alvarez-Garcia J., Lee S., Gupta A., et al. Prognostic impact of prior heart failure in patients hospitalized with COVID-19. J Am Coll Cardiol. 2020;76(20):2334–2348. doi: 10.1016/j.jacc.2020.09.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lyu W., Wehby G.L. Comparison of estimated rates of coronavirus disease 2019 (COVID-19) in border counties in Iowa without a stay-at-home order and border counties in Illinois with a stay-at-home order. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.11102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hall M.E., Vaduganathan M., Khan M.S., et al. Reductions in heart failure hospitalizations during the COVID-19 pandemic. J Card Fail. 2020;26(6):462–463. doi: 10.1016/j.cardfail.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu J., Mamas M.A., Mohamed M.O., et al. Place and causes of acute cardiovascular mortality during the COVID-19 pandemic. Heart. 2021;107(2):113–119. doi: 10.1136/heartjnl-2020-317912. [DOI] [PubMed] [Google Scholar]
- 12.Gorodeski E.Z., Moennich L.A., Riaz H., Jehi L., Young J.B., Tang W.H.W. Virtual versus in-person visits and appointment no-show rates in heart failure care transitions. Circ Heart Fail. 2020;13 doi: 10.1161/CIRCHEARTFAILURE.120.007119. [DOI] [PubMed] [Google Scholar]
- 13.Salzano A., D'Assante R., Stagnaro F.M., et al. Heart failure management during the COVID-19 outbreak in Italy: a telemedicine experience from a heart failure university tertiary referral centre. Eur J Heart Fail. 2020;22(6):1048–1050. doi: 10.1002/ejhf.1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.