Abstract
Nepal is a country in south Asia with a high burden of cardiometabolic diseases (CMDs). Strengthening primary healthcare (PHC) is a key strategy to mitigate this increasing burden and achieve universal health coverage. While previous studies in Nepal have assessed PHC use among the elderly, none have specifically explored PHC use among people with CMDs. Therefore, this mixed-methods study aimed to assess the use and perception of PHC services in Nepal among people living with CMDs for primary and secondary prevention of cardiovascular disease. We used a quantitative survey followed-up by semi-structured qualitative interviews. The sampling frame comprised five PHC facilities in Sindhuli district (rural; eastern Nepal) and five in Kailali district (urban; western Nepal), with participants selected from each facility via convenience sampling. 114 people (mean age: 54.5 ± 14.7, sex ratio 1.04) with CMDs participated in the survey. Survey data showed general dissatisfaction with PHC services. Medicine cost was rated “too expensive” by 52 and 63% of rural and urban participants, respectively. Interview data showed that perceived poor bedside manner was tied to negative perceptions of PHC quality, and vice versa. Lack of resources and excessive barriers to care was mentioned by every interviewee. In conclusion, PHC use was high but overall satisfaction relatively low. Our results suggest that bedside manner is a practical target for future research. Additionally, we identified several barriers to care, and, based on existing literature, we suggest electronic-health interventions may have potential to mitigate these challenges.
Keywords: primary healthcare (PHC), cardiovascular disease, hypertension, stroke, diabetes, Nepal
Introduction
Control of cardiometabolic diseases (CMDs), which encompasses cardiovascular disease (CVD, primarily heart disease and stroke) and related conditions such as hypertension and diabetes, is an urgent global health priority (1–5). Primary healthcare (PHC) is on the frontline of CMD control because it targets modifiable risk factors, promotes healthy lifestyle habits, and provides continuity of care across the lifespan (6–10). PHC utilization is a key indicator of PHC accessibility, affordability, and perceived effectiveness (11–14). Since prevention and control of CMDs depends heavily on mobilizing health systems to serve large populations, PHC utilization can also be viewed as one indicator for the potential of PHC to combat CMDs (15, 16). Likewise, understanding patient perception of PHC use elucidates factors which may influence overall utilization, thereby providing meaningful targets for future research and intervention (13, 17–19). Despite its strategic position to combat CMDs, however, primary healthcare is often the weakest link in already underdeveloped health systems in many low- and middle-income countries (LMICs) (20–26).
This study examines the use and perception of PHC services for the prevention and management of CMDs in Nepal, a small, landlocked country in south Asia. Nepal is a low-income country with about 80% of the population living in rural areas. It is considered to be one of the least developed countries globally, with ~15% of the population below the international income poverty line (27). Non-communicable diseases (NCDs) account for more than 44 % of deaths and 80 % of outpatient contacts in Nepal (28). Tertiary care is limited, expensive, and disproportionately concentrated in urban areas (29). In contrast, by law, basic health services must be provided free of charge within PHCs (30). Though Nepal is well-positioned to benefit from strong PHC services for CMD control, literature on the perception and use of these services in Nepal is sparse. Studies have examined PHC utilization among aging Nepalese populations (29, 31, 32), but not specifically people with CMDs. Therefore, a better understanding of these factors in Nepal may illuminate the potential of PHC in both prevention and management of CMDs in a challenging setting.
Our primary study objectives are to assess the use and perception of PHC services for prevention and management of CMDs among people living with CMDs in Nepal. We explore PHC facilities in both an urban and a rural setting and capture data on patient utilization of PHC services for both primary and secondary prevention of cardiovascular disease.
Methods
Overview and Study Setting
This study was conducted as part of the four-country “FAITH” (feasibility assessment of invigorating grassroots primary healthcare) study, whose protocol is published elsewhere (15). We used a mixed-method study design, conducting structured quantitative surveys followed up by a smaller number of qualitative in-depth interviews with select participants. Our sampling frame was ten PHC facilities across two regions of Nepal: five in Kailali district and five in Sindhuli district. Sindhuli is a rural, mountainous area in eastern Nepal which was severely affected by the 2015 earthquake. Kailali, in contrast, is a comparatively more urbanized district in the far Western development region. Topographically it is a flat plain with some hilly areas, and it shares a border with India. Facilities were selected by cluster convenience sampling.
Participants
For the quantitative survey, we used convenience cluster sampling to recruit at least ten participants with CMD from each PHC facility according to the following inclusion criteria: (1) over 18 years of age; (2) have ever been diagnosed with at least one of the following conditions: heart disease, stroke, hypertension, and/or diabetes; (3) willing to participate and able to reach the sampled PHC facility to be interviewed. Exclusion criteria included: (1) people who were seriously ill, and (2) people with communication difficulties who are unable to answer the questionnaires or participate in the interviews. To compensate for the inherent weaknesses in cluster convenience sampling, we applied additional selection strategies to each facility to achieve the most balanced and representative sample possible: (1) an equal ratio of male and female participants; (2) a balance of patients across age groups, including at least two participants younger than 45 at each facility; (3) when possible, two participants who had not obtained care from this facility in the previous 12 months; and (4) those who had been diagnosed by a healthcare professional as having heart disease and/or having experienced a stroke were prioritized over those with other conditions. Strategy 3 compensates for using the PHC facility as our sampling frame, where we are more likely to enroll active PHC patients. Strategy 4 corrects for the higher proportion of hypertension/diabetes cases which would otherwise comprise most of the sample.
For the qualitative component, we followed up a smaller number of participants from the quantitative survey for inclusion in the in-depth semi-structured interview. Data collectors selected two participants at each facility to be interviewed, based on willingness to participate and ability to communicate. Our target was 10 interviews from each study district and 20 overall, as this number is usually enough to reach information saturation.
Data Collection
Our quantitative questionnaire was modeled after the WHO STEPS survey (33) and included four sections: demographics, cardiovascular disease history, access to PHC services, and medication history. We measured “PHC use” as a function of visits within the past 12 months and “time needed to see a provider” as the combination of travel time and wait time. We measured “perception” by using Likert-scale ratings of travel time, wait time, medicine cost, and overall treatment cost (the full sum paid by the patient to the PHC for their visit). For the qualitative component, we developed a standardized interview guide of five questions for the semi-structured in-depth interviews. Questions covered disease management, satisfaction with PHC services and treatments, and emergency preparedness. Interviews were conducted in Nepali language, audio-recorded, and translated to English.
Data Analysis
Quantitative data analysis was completed via R Studio (34). Descriptive analysis of sociodemographic factors included age, gender, education status, health status, occupation, and marital status. For subgroup analysis, we dichotomized participants by location (rural/urban) and disease status (hypertension/diabetes vs. CVD), using Kruskal-Wallis tests for continuous variables (number of PHC visits, travel time, and wait time) and Pearson's Chi-Squared for categorical variables (Likert-scale ratings of travel time, wait time, medicine cost, and treatment cost).
Qualitative data analysis was completed using NVIVO 11 (QSR International). A team of three trained coders, using a thematic analysis approach, created the codebook and systematically coded all 20 in-depth interviews to identify relevant themes and sub-themes. The codebook was drafted and finalized based on discussion and mutual agreement of all three coders, and an inter-rater reliability of >80% was achieved prior to the start of coding. Theme frequencies and key themes mentioned by interviewees from each district were tabulated (Table 3). Finally, representative quotes from the major thematic areas were selected to illustrate participants' attitudes and perceptions of receiving care at their local PHC facility.
Ethical Approval
We received ethical approval from the Duke University Institutional Review Board (IRB) (Protocol Number: Pro00082962) and the Nepal Health Research Council (NHRC) (Reg. No. 158/2017). We obtained written informed consent from all participants prior to starting data collection.
Results
Quantitative Data
Table 1 shows the sociodemographic profile of our participants. We completed 114 valid questionnaires and 20 in-depth semi-structured interviews in August 2017. Of those, 63 surveys and 10 interviews came from urban areas (Kailali district) and 51 surveys and 10 interviews came from rural areas (Sindhuli district). The mean age (±standard deviation) was 54.5 ± 14.7 years and the sex ratio was 1.04. In both study locations, sociodemographic variables indicated low socioeconomic status among participants. In Sindhuli, 70% of participants were illiterate or educated below a primary school level; the most common form of employment was agriculture (45%); unemployment was 6%; and the most common self-reported health status was “bad/very bad” (45%). In Kailali, 56% of participants were illiterate or educated below a primary school level; the most common form of employment was agriculture (37%); unemployment was 16%; and the most common self-reported health status was “average” (37%).
Table 1.
Participant sociodemographic profile.
| Urban (n = 63) | Rural (n = 51) | ||||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Age (years) | |||||
| <45 | 20 | 32 | 13 | 26 | |
| 45-65 | 24 | 38 | 23 | 45 | |
| >65 | 19 | 30 | 15 | 29 | |
| Sex | |||||
| Female | 31 | 49 | 25 | 49 | |
| Male | 32 | 51 | 26 | 51 | |
| Education Status | |||||
| Illiterate | 15 | 24 | 20 | 39 | |
| Literate | 20 | 32 | 16 | 31 | |
| Primary Level | 8 | 13 | 3 | 6 | |
| Secondary Level | 10 | 16 | 9 | 18 | |
| Higher Secondary | 9 | 14 | 1 | 2 | |
| Undergraduate | 1 | 2 | 2 | 4 | |
| Post-Graduate | 0 | 0 | 0 | 0 | |
| Marital Status | |||||
| Currently married | 58 | 92 | 45 | 88 | |
| Never married | 1 | 2 | 1 | 2 | |
| Widowed | 4 | 6 | 4 | 7 | |
| Divorced/separated | 0 | 0 | 1 | 2 | |
| Self-Reported Health | |||||
| Very good/good | 19 | 31 | 13 | 25 | |
| Average | 23 | 37 | 25 | 29 | |
| Very bad/bad | 20 | 32 | 23 | 45 | |
| Occupation | |||||
| Government | 5 | 8 | 2 | 4 | |
| Agriculture | 23 | 37 | 23 | 45 | |
| Business | 10 | 16 | 7 | 14 | |
| Student | 0 | 0 | 1 | 2 | |
| Housewife | 13 | 21 | 4 | 8 | |
| Retired | 2 | 3 | 3 | 6 | |
| Unemployed | 10 | 16 | 3 | 6 | |
| Other | 0 | 0 | 8 | 16 | |
Table 2 describes annual PHC use, travel time, and wait time, and compares differences between two subgroups: location and disease type. PHC use was frequent to semi-frequent, with the mean number of PHC visits in the past year being 7.5 ± 6.6 in urban areas and 8.7 ± 9.5 in rural areas. This is an average of one PHC visit per every 1.4 to 1.6 months. There were no significant differences between subgroups except for travel time by disease status, with the CVD group reporting longer travel times to reach their local PHC facility.
Table 2.
PHC Utilization and Time Needed to See a Provider.
| Location | Disease Type | |||||
|---|---|---|---|---|---|---|
| Urban | Rural | p | CVD | Hypertension/Diabetes | p | |
| n = 63 | n = 51 | n = 50 | n = 62 | |||
| PHC Visits Past Year | ||||||
| Mean | 7.5 | 8.7 | 0.500 | 8.1 | 8.2 | 0.468 |
| SD | 6.6 | 9.5 | 8.9 | 7.4 | ||
| Travel Time (min) | ||||||
| Mean | 14.5 | 21.8 | 0.106 | 22.1 | 13.1 | 0.002 |
| SD | 14.7 | 24.6 | 22.0 | 13.8 | ||
| Wait Time (min) | ||||||
| Mean | 11.3 | 15.4 | 0.180 | 13.1 | 12.7 | 0.383 |
| SD | 9.2 | 24.5 | 9.5 | 12.4 | ||
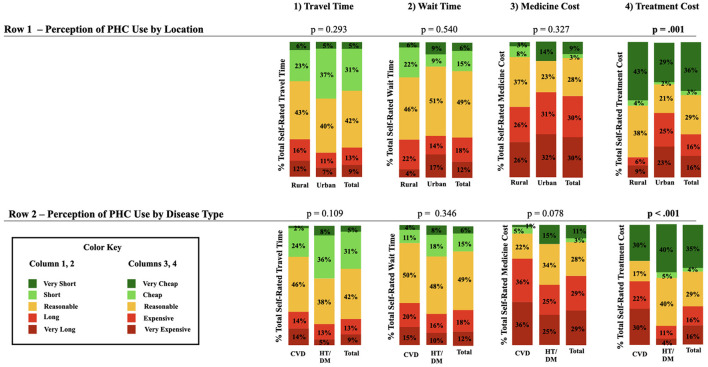
Figure 1 describes perception of travel time, wait time, medicine cost, and treatment cost, with subgroup analysis by location (urban vs. rural) and disease type (CVD vs. hypertension/diabetes). Treatment cost was found to be significant (p ≤.001) in both subgroups, with a higher proportion of both urban participants and participants with CVD reporting treatment cost as “too expensive” compared to rural and hypertension/diabetes participants. The difference in treatment cost can be visualized in column 4. Additionally, column 3 shows that the highest amount of dissatisfaction was with respect to the cost of medicine. Medicine cost was rated “too expensive” by 72% of participants with CVD, 50% of those with hypertension/diabetes, 52% of rural residents, and 63% of urban residents.
Figure 1.
Perception of PHC use.
Qualitative Data
Table 3 shows the results of the thematic analysis for the 20 in-depth interviews. We identified three major themes: barriers to PHC utilization, perception of PHC services, and participant recommendations. We further identified five to eight sub-themes within each major theme. Within the following text, numbers within brackets signify the proportion of respondents who mentioned the respective topic (e.g., 100% = all participants mentioned / said this). A sociodemographic profile of interview participants is included in Appendix.
Table 3.
Summary of Thematic Analysis.
| Themes and Subthemes | Times Mentioned |
Participants Discussing Theme |
Key Points | ||
|---|---|---|---|---|---|
| Urban | Rural | n = 20 | % | ||
| A) Barriers to PHC Utilization | |||||
| Financial | 18 | 34 | 14 | 70 | Patients use PHC centers because they are the closest point of contact with the health system, and hospitals / tertiary care is too far away. However, despite visiting a PHC center, patients cited lack of machines, doctors, medicine, and cost of treatment as barriers to receiving proper care or returning to the PHC center. |
| Lack of Resources | 44 | 54 | 20 | 100 | |
| Geographic / Travel-related | 12 | 11 | 14 | 70 | |
| Education | 1 | 2 | 3 | 15 | |
| Medicine Not Effective | 2 | 4 | 5 | 25 | |
| Distrust Health Workers | 0 | 3 | 2 | 10 | |
| Poor Administration / Leadership | 0 | 3 | 3 | 15 | |
| Insufficient Open Hours | 2 | 0 | 1 | 5 | |
| B) Perception of PHC services | |||||
| Wait Time | 2 | 1 | 3 | 15 | High emphasis placed on physician behavior/competency over other areas. Perceived quality of medical care was strongly tied to perceptions of staff behavior / bedside manner as gentle and caring or not. |
| Cleanliness | 0 | 1 | 1 | 5 | |
| Staff Behavior | 10 | 9 | 9 | 45 | |
| Health Worker Competency | 8 | 7 | 15 | 75 | |
| Treatment Satisfaction | 2 | 6 | 8 | 40 | |
| C) Patient Recommendations | |||||
| Medicine / Equipment Availability | 25 | 27 | 20 | 100 | Participant recommendations were consistent: availability of essential resources and financial assistance / reduced costs were the major suggestions to improve PHC quality. |
| Lower Physician Turnover /Absence | 1 | 4 | 5 | 25 | |
| Access to Specialist Care | 18 | 9 | 10 | 50 | |
| Free Medicine / Financial Assistance | 12 | 35 | 17 | 85 | |
| Health Education / Awareness | 0 | 5 | 4 | 20 | |
When asked about barriers to PHC utilization, all participants expressed frustration with the lack of resources at their local PHC (100%), but most also noted that traveling elsewhere for healthcare was not feasible due to distance, cost of travel, and difficulties associated with travel such as heavy seasonal rain and landslides (70%).
“For a heart patient like me, if there were services like ECHO, ECG, medicine, and a doctor available here at the PHC itself, we needn't go elsewhere…It would be easier if all things were available here itself.” (Participant SS, Sindhuli District)
Despite a national policy that all PHC centers should have a doctor, many participants reported this was not the case. (When a physician is not present, health assistants and auxillary healthcare workers generally provide care).
“I hope doctors will be available soon. The worst thing is, we don't have MBBS doctor here. He comes once in a while, stays for 1–2 days and leaves. This the main problem: patients have to bear it. Doctors don't stay here.” (Participant HS, Kailali District)
When asked about perception of the PHC center, participants emphasized staff behavior (45%) and their competency (75%). While assessments of provider competency were mixed, these appraisals (either positive or negative) were strongly tied to perceptions of the physician's attitude and bedside manner.
“The most recent place I went for check-up, I really liked the service and attitudes of the (female staff) there. And the doctor. his way of talking and checking the patients was really very good. The place I went before there was horrible. The doctor was rude and I felt that they would certainly kill most patients just by talking to them” (Participant DN, Kailali District).
One common point of dissatisfaction, mentioned by both urban and rural residents, was young doctors (either recently graduated or still in training) staffing PHC facilities. They were perceived as being both less competent and less likely to stay and practice at the PHC facility than other physicians.
“We don't have good doctors here. Only the learners come here. They come here for internship and for practical. Good doctors don't come here and I don't like it” (Participant MS, Kailali district).
Conversely, having staff from the community was perceived more favorably.
Finally, recommendations for improved PHC services were consistent. Every interviewee suggested improving the availability of equipment and essential medicines. One participant concisely summarized the dilemma between close but low-quality PHC care and distant, higher quality tertiary care:
“As per my knowledge, it will be better if we take the patient to the Belghari PHC first as this PHC is very close and in our community. But for us to be able to choose the Belghari PHC first, we need equipment and facilities in here” (Participant JR, Sindhuli District).
Health education and counseling, an area where PHC is uniquely positioned to excel, was also noted as being substandard:
“Most of the people are unaware and don't have any idea how to manage these kind of disease. As the awareness about the proper care of the heart is absent in our community, priority should be given to these things…There was one member of our community who died when he took two pills at once that was meant for 2 days as he had forgot to take the pills the day before. He was immediately taken to Kathmandu but he died anyway.” (Participant JR, Sindhuli District).
Discussion
Interpretation of Data
This study examined PHC use and perceptions among people with cardiometabolic disease in Nepal. Global literature has described PHC use and patient satisfaction in many contexts, and previous studies in Nepal have focused on PHC use among aging populations (29, 31, 32). As the first study (to the best of our knowledge) to specifically describe use and perception of PHC services for CMDs in Nepal, this manuscript serves as a call to action for contributing new knowledge to this important space in the literature.
In our study, though PHC use was high, satisfaction was relatively low. Moreover, our result for mean PHC use may be an underestimate among PHC users given that our sample comprises both current PHC users (n = 101, 91.4%) and participants who had not sought care a their PHC in the past 12 months (n = 11, 9.6%). At face value, this may seem paradoxical since other studies have found that perception of low quality and unavailability of needed services is associated with lower PHC use (13–15). The difference in our study may be explained in the following way: we specifically studied PHC use among people with CMDs, a group that requires regular checkups and longitudinal management of their health condition(s), while other studies examined PHC use among whole communities for a broad variety of conditions. Due to the chronic nature of their illness, people with CMD may be more likely to consistently use local PHC facilities. This is in contrast to those with acute problems or other medical issues where a once-off visit to a more distant tertiary care facility may be judged the better option. This indicates that even though PHC facilities are not functioning at a level to meet patient expectations, they are still the first choice treatment center and on the frontline of CMD management for this group. Strengthening CMD prevention and management in local PHC centers therefore still offers strong potential to mitigate the burden of CMDs within their respective communities.
Medicine cost received the highest dissatisfaction ratings from both rural and urban residents. This represents a serious challenge, as many drugs for the prevention and management of CMDs are classified as “essential medicines” which the WHO recommends should be available “at a price the individual and community can afford” (35). In Nepal, the essential medicines policy goes even further: the essential drugs list for PHC contains 60 medications which are required to be available free of charge at governmental health facilities (36). Despite this, medication costs are the highest household health expense and a major driver of impoverishment in most low-income countries like Nepal (35). As 60% of participants rated medication cost “too expensive” and 85% recommended decreasing medication cost, disparity between policy and practice likely persists. Moreover, despite that WHO PEN (package of essential NCD interventions) recommends that essential medicines should be available at PHC facilities (37), 100% of our interview participants recommended increasing medicine availability, implying at least some needed medicines were not available. While resource constraints are an expected issue, it is also estimated <10% of PHC facilities in Nepal are in compliance with required drug storage practices for the essential medicines they did receive (36). This contributes to drug degradation and further perpetuates the scarcity of essential medicines. Therefore, our results suggest more attention should be given to closing the gap between policy and practice, ensuring that qualifying essential medicines are both available and free of charge at PHCs in Nepal and confirming the essential drugs list adequately covers CMDs.
The interview data adds nuance to the discrepancy between high PHC use and lower satisfaction ratings. In large part, participants attributed the higher use of local PHC services to financial, logistic, and geographic barriers to travel elsewhere for care. This helps explain our survey finding of high PHC use among our sample of people with CMDs in tandem with low satisfaction ratings. Negative perception of PHC services was most strongly driven by perceived lack of needed medicines, equipment, and health personnel. These negative perceptions were mitigated, in part, when participants believed their healthcare providers had good bedside manner. This mediating effect of provider behavior has been documented elsewhere, for example in a similar study on patient perception of PHC in India (19). That study observed that patients placed high emphasis on physician behavior and the patient-physician relationship as strong indicators of satisfaction. Our study results are congruent with these findings, and indicate that bedside manner and the provider-patient relationship are key factors for PHC use among patients with CMDs. A tool has been developed in Nepal for observed rating of communication skills and therapeutic relationships between patient and provider (38, 39), as well as patient-rated version of interactions with providers, which is correlated with mental health outcomes in PHCs (40). In addition, the WHO Foundational Helping Skills training, which focuses on provider communication skills, is currently being piloted in Nepal (41). The findings here support the need for structured evaluation and training in provider communication skills, such as combining WHO Foundational Helping Skills training with WHO PEN training.
Strengths and Limitations
This study is the first to examine perception and use of PHC services for CMDs in Nepal. The use of mixed-methods bolstered the overall quality and breadth of data, and we explored utilization of PHC services for both primary and secondary prevention of cardiovascular diseases. Additionally, sampling facilities from urban and rural areas adds to the strength of our study.
The main limitations are the use of only two districts of Nepal as study sites, the use of cluster convenience sampling, and the limited sample size. With respect to study sites, Nepal is an extremely diverse country, both ethnically and geographically. Within the limitations of being only two study sites, Sindhuli and Kailali do portray characteristic regions of the country and serve for our purposes as an exploratory study. Second, cluster convenience sampling was used out of necessity given budget and timing restraints. This method can potentially bias results via sampling bias. To mitigate this, we introduced additional inclusion/exclusion criteria such as gender parity, age parity, parity between CMD type, and people with CMDs who had not used the PHC facility within the past year, to reduce the inherent limitation of cluster convenience sampling. Finally, while our sample size of 114 participants is too small to act as a regionally or nationally generalizable sample, the number was large enough to permit statistical subgroup comparisons. In the qualitative component, our interviewees reached information saturation before completion of the 20th interview, evidencing sufficiency of the sample size for our purposes. Taken together, these limitations do not invalidate our data. We are therefore able to draw conclusions appropriate to the level of an exploratory study, using our results to highlight evidence gaps and important areas of investigation.
Recommendations and Future Research
Given the exploratory nature of this study, our recommendations focus on identifying the highest priority problems. From our mixed-methods approach, we found that PHC use was relatively high, while overall satisfaction relatively low. What can be done to improve satisfaction? Increase in the availability of essential medicines, diagnostic and therapeutic equipment, and essential personnel were clear themes that emerged from the data. Notably, the most discussed aspect of PHC satisfaction was not satisfaction of the medical treatment but behavior of the staff. Many participants reported feeling greater levels of trust in and satisfaction with PHC services when they believed their caretakers had good bedside manner. As a corollary, participants reported stronger feelings of distrust and lower perceived treatment quality when they perceived their caretaker's attitudes as poor. Therefore, in addition to increasing resources and investment in PHC, we recommend more research into the influence of bedside manner and the patient-physician relationship in PHC prevention and management of CMDs in Nepal, and how this can be improved
All participants reported their PHC lacked needed resources to provide them with appropriate care. This drove interest in seeking care at distant tertiary facilities and from specialists in cardiovascular medicine. Based on existing evidence, we suggest one potential solution to the challenges identified in our study is electronic health (“e-health”) innovations such as mobile health and telemedicine interventions. E-health provides a platform to deliver some critical aspects of CMD care directly to people in their own hometowns, even in the most isolated and rural areas (42–44). Over 3/4 of Nepali households use a mobile phone (45) and previous studies have reported encouraging results with e-health interventions in the control of CMDs both in Nepal (46–48) and other countries (49, 50). While the potential of these interventions is clear, implementation is a challenge in resource-limited settings. A recent review of e-health interventions in Nepal found that many were not adequately integrated into the existing healthcare system nor scaled beyond a local level (51). Therefore, we suggest this may also be a worthwhile target for future research aimed at improving CMD control in Nepal.
Conclusion
This study used mixed-methods to investigate use and perception PHC services for CMDs in two low-resource settings in Nepal. PHC use was high but overall satisfaction was low. Medication cost was the strongest point of dissatisfaction, with 100% of interview participants recommending increasing medicine availability and 85% suggesting to decrease medicine cost. Perceptions of provider competency were tied to the perceived quality of their bedside manner. Therefore, we suggest bedside manner and the patient-physician relationship are important and practical targets for future studies aimed at improving PHC-level CMD control in this setting. Finally, we identified several key barriers to PHC use, including: financial challenges, lack of equipment/essential medications, and geographic barriers. While we did not directly investigate e-health, based on existing evidence, we suggest e-health interventions may be a complementary, potentially effective strategy to mitigate the barriers to PHC services identified in our study. Therefore, we propose this is an additional area for further research.
As stated in 2019 by (21) “Primary care is more than a first point of care; it is the core process of a health system”. We strongly recommend further efforts aimed at enhancing the prevention and management of CMDs at the PHC level in Nepal, which will contribute to overall health system strengthening.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Duke University Institutional Review Board (Protocol Number: Pro00082962) Nepal Health Research Council (NHRC) (Reg. No. 158/2017). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
NP, EG, KG, SNK, BAK, SK, AA, and LY conceived the study design and contributed substantially to data acquisition, analysis, and interpretation, and production and approval of the final manuscript. SX, TØ, JM, and QL contributed substantively to data analysis and interpretation, critical revision, and final approval of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by the World Health Organization Asia Pacific Observatory on Health System and Policies (supporting the overall activities of the four country FAITH study, of which this study is a part): WHO Registration: 2016/622444-0; grant number: 2014/77862. Duke University and Duke Kunshan University provided financial support to graduate students who conducted fieldwork in Nepal for data collection.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We acknowledge our collaboration with and the contributions of the Transcultural Psychosocial Organization Nepal in Kathmandu, Nepal. We further acknowledge the contributions of Joshila Rai for her strong intellectual and logistic support during the fieldwork. We would also like to thank the Institute of Medicine of Tribhuvan University and the Nepal Health Research Council for their indispensable support.
Appendix
Table A1.
Sociodemographic Profile of In-Depth Interview Participants.
| Participant ID | Location | Gender | Age | Occupation | CVD Condition |
|---|---|---|---|---|---|
| MS | Urban | Male | 61 | Yoga Trainer | Heart Disease |
| KC | Urban | Male | 67 | Agriculture | Heart Disease, HTN |
| MJ | Urban | Male | 49 | Unemployed | Stroke, HTN |
| BD | Urban | Female | 52 | Agriculture | Stroke, HTN, Heart Disease |
| DV | Urban | Male | 39 | Agriculture | Stroke, HTN |
| JF | Urban | Female | 54 | Retired | HTN |
| AL | Urban | Female | 58 | Housewife | Heart Disease |
| HS | Urban | Male | 52 | NGO | HTN, Diabetes |
| TR | Urban | Male | 43 | Business | Stroke |
| DN | Urban | Female | 41 | Government | Heart Disease, Diabetes |
| BK | Rural | Male | 75 | Unemployed | HTN, Diabetes |
| MD | Rural | Female | 64 | Agriculture | HTN |
| SK | Rural | Female | 26 | Agriculture | Stroke, Heart Disease, HTN |
| KG | Rural | Male | 37 | Business | HTN, Diabetes |
| JR | Rural | Male | 53 | Government | HTN |
| ST | Rural | Female | 35 | Housewife | HTN |
| NP | Rural | Male | 63 | Unemployed | Heart Disease, HTN, Diabetes |
| LJ | Rural | Male | 65 | Retired | Stroke, HTN, Diabetes |
| SS | Rural | Female | 71 | NGO | Heart Disease |
| AT | Rural | Male | 40 | Tailor | HTN, Diabetes |
References
- 1.World Health OrganizationCardiovascular diseases (CVDs) . World Health Organization. (2017). Available online at: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed Jul 07, 2020).
- 2.Lou N. Hypertension, related mortality rising globally. Medical News and Free CME Online. MedpageToday. (2017). Available online at: https://www.medpagetoday.com/Cardiology/Hypertension/62429 (accessed Jul 07, 2020)
- 3.World Health Organization . Hypertension. World Health Organization. (2019). Available online at: https://www.who.int/news-room/fact-sheets/detail/hypertension (accessed Jul 07, 2020).
- 4.World Health Organization . The top 10 causes of death. World Health Organization (2017). Available online at: http://www.who.int/mediacentre/factsheets/fs310/en/ (accessed Jul 07, 2020).
- 5.Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. lancet. (2016) 388:1545–602. 10.1016/S0140-6736(16)31678-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Demaio AR, Nielsen KK, Tersbøl BP, Kallestrup P, Meyrowitsch DW. Primary Health Care: a strategic framework for the prevention and control of chronic non-communicable disease. Glob Health Action. (2014) 7:24504. 10.3402/gha.v7.24504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mahipala P, Dorji G, Tisocki K, Rani M. A critical review of addressing cardiovascular and other non-communicable diseases through a primary health care approach in the South-East Asia Region. Cardiovasc Diagn Ther. (2019) 9:150–57. 10.21037/cdt.2018.09.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lall D, Prabhakaran D. Organization of primary health care for diabetes and hypertension in high, low and middle income countries. Expert Rev Cardiovasc Ther. (2014) 12:987–95. 10.1586/14779072.2014.928591 [DOI] [PubMed] [Google Scholar]
- 9.Mendis S, Johnston SC, Fan W, Oladapo O, Cameron A, Faramawi MF. Cardiovascular risk management and its impact on hypertension control in primary care in low-resource settings: a cluster-randomized trial. Bull World Health Organ. (2010) 88:412–9. 10.2471/BLT.08.062364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frenk J. Reinventing primary health care: the need for systems integration. Lancet. (2009) 374:170–3. 10.1016/S0140-6736(09)60693-0 [DOI] [PubMed] [Google Scholar]
- 11.Gage AD, Leslie HH, Bitton A, Jerome JG, Joseph JP, Thermidor R, et al. Does quality influence utilization of primary health care? evidence from haiti. Glob Health. (2018) 14:1–9. 10.1186/s12992-018-0379-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sule SS, Ijadunola KT, Onayade AA, Fatusi AO, Soetan RO, Connell FA. Utilization of primary health care facilities: lessons from a rural community in southwest Nigeria. Niger J Med. (2008) 17:98–106. 10.4314/njm.v17i1.37366 [DOI] [PubMed] [Google Scholar]
- 13.Muhammed KA, Umeh KN, Nasir SM, Suleiman IH. Understanding the barriers to the utilization of primary health care in a low-income setting: implications for health policy and planning. J Public Health Afr. (2013) 4:e13. 10.4081/jphia.2013.e13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adar T, Levkovich I, Castel OC, Karkabi K. Patient's utilization of primary care: a profile of clinical and administrative reasons for visits in Israel. J Prim Care Community Health. (2017) 8:221–7. 10.1177/2150131917734473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gong E, Lu H, Shao S, Tao X, Peoples N, Kohrt BA, et al. Feasibility assessment of invigorating grassrooTs primary healthcare for prevention and management of cardiometabolic diseases in resource-limited settings in China, Kenya, Nepal, Vietnam (the FAITH study): rationale and design. Glob Health Res Policy. (2019) 4:1–9. 10.1186/s41256-019-0124-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yan LL, Xiong S, Lu H, Gong E, Peoples N, Tang S. Strengthening Primary Healthcare For Prevention And Management Of Cardio-Metabolic Disease In Low- And Middle-Income Countries. New Delhi: World Health Organization Regional Office for South-East Asia; (2019). Available online at: https://apps.who.int/iris/handle/10665/329402 [Google Scholar]
- 17.Papp R, Borbas I, Dobos E, Bredehorst M, Jaruseviciene L, Vehko T, et al. Perceptions of quality in primary health care: perspectives of patients and professionals based on focus group discussions. BMC Fam Pract. (2014) 15:1–3. 10.1186/1471-2296-15-128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Doubova SV, Guanais FC, Pérez-Cuevas R, Canning D, Macinko J, Reich MR. Attributes of patient-centered primary care associated with the public perception of good healthcare quality in Brazil, Colombia, Mexico and El Salvador. Health Policy Plan. (2016) 31:834–43. 10.1093/heapol/czv139 [DOI] [PubMed] [Google Scholar]
- 19.Ardey R, Ardey R. Patient perceptions and expectations from primary health-care providers in India. J Family Med Prim Care. (2015) 4:53. 10.4103/2249-4863.152254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization . NCDs Assessing national capacity for the prevention and control of NCDs. World Health Organization. (2020). Available online at: http://www.who.int/ncds/surveillance/ncd-capacity/en/ (accessed Jul 7, 2020).
- 21.Varghese C, Nongkynrih B, Onakpoya I, McCall M, Barkley S, Collins TE. Better health and wellbeing for billion more people: integrating non-communicable diseases in primary care. BMJ. (2019) 364:l327. 10.1136/bmj.l327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Detollenaere J, Hanssens L, Vyncke V, De Maeseneer J, Willems S. Do we reap what we sow? exploring the association between the strength of european primary healthcare systems and inequity in unmet need. PLoS ONE. (2017) 12:e0169274. 10.1371/journal.pone.0169274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mutale W, Bosomprah S, Shankalala P, Mweemba O, Chilengi R, Kapambwe S, et al. Assessing capacity and readiness to manage NCDs in primary care setting: Gaps and opportunities based on adapted WHO PEN tool in Zambia. PLoS ONE. (2018) 13:e0200994. 10.1371/journal.pone.0200994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mendis S, Al Bashir I, Dissanayake L, Varghese C, Fadhil I, Marhe E, et al. Gaps in capacity in primary care in low-resource settings for implementation of essential noncommunicable disease interventions. Int J Hypertens. (2012) 29:2012. 10.1155/2012/584041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pakhare A, Kumar S, Goyal S, Joshi R. Assessment of primary care facilities for cardiovascular disease preparedness in Madhya Pradesh, India. BMC Health Serv Res. (2015) 15:1–8. 10.1186/s12913-015-1075-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Picon RV, Dias-da-Costa JS, Fuchs FD, Olinto MT, Choudhry NK, Fuchs SC. Hypertension management in Brazil: usual practice in primary care—a meta-analysis. Int J Hypertension. (2017) 2:2017. 10.1155/2017/1274168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.United Nations Development Programme. Human Development Indicators-Nepal: Poverty. (2018). Available online at: https://hdr.undp.org/en/count ries/profi les/NPL (accessed Dec 23, 2020).
- 28.Mishra SR, Neupane D, Bhandari PM, Khanal V, Kallestrup P. Burgeoning burden of non-communicable diseases in Nepal: a scoping review. Global Health. (2015) 11:1–0. 10.1186/s12992-015-0119-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Acharya S, Ghimire S, Jeffers EM, Shrestha N. Health care utilization and health care expenditure of Nepali older adults. Front Public Health. (2019) 7:24. 10.3389/fpubh.2019.00024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chand PB, Kharelc R. Politics of primary health care in Nepal. In: Medcalf A, Bhattacharya S, Momen H. editors. Health For All: The Journey Of Universal Health Coverage. Hyderabad (IN): Orient Blackswan; (2015). Chapter 11. Available online at: https://www.ncbi.nlm.nih.gov/books/NBK316266/ [PubMed] [Google Scholar]
- 31.Sanjel S, Mudbhari N, Risal A, Khanal K. The utilization of health care services and their determinants among the elderly population of dhulikhel municipality. Kathmandu Univ Med J. (2012) 10:24–9. 10.3126/kumj.v10i1.6911 [DOI] [PubMed] [Google Scholar]
- 32.Gurung LB, Paudel G, Yadav UN. Health service utilization by elderly population in urban nepal: a cross-sectional study. J Manmohan Mem Inst Health Sci. (2016) 2:27–36. 10.3126/jmmihs.v2i0.15794 [DOI] [Google Scholar]
- 33.NCDs . The STEPS Instrument And Support Materials. (2017). Available online at: https://www.who.int/ncds/surveillance/steps/instrument/en/ (accessed July 07, 2020).
- 34.R Core Team. R: A Language And Environment For Statistical Computing. R Foundation For Statistical Computing. Vienna, Austria: (2013). Availale online at: http://www.R-project.org/. [Google Scholar]
- 35.World Health Organization . Essential medicines. World Health Organization. (2016). Available online at: https://www.who.int/medicines/services/essmedicines_def/en/ (accessed Jul 7, 2020).
- 36.Jha AK, Dhakal N, Gyanwali P, Humagain B, Jha N, BC R, et al. Quality of essential medicines in public health care facilities of Nepal−2019. Nepal Health Res Counc. (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.World Health Organization . NCDS Tools For Implementing Who Pen (Package Of Essential Noncommunicable Disease Interventions). World Health Organization (2020). Available online at: https://www.who.int/ncds/management/pen_tools/en/ (accessed Jul 07, 2020).
- 38.Kohrt BA, Jordans MJ, Rai S, Shrestha P, Luitel NP, Ramaiya MK, et al. Therapist competence in global mental health: development of the ENhancing Assessment of Common Therapeutic factors (ENACT) rating scale. Behav Res Ther. (2015) 69:11–21. 10.1016/j.brat.2015.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kohrt BA, Mutamba BB, Luitel NP, Gwaikolo W, Onyango Mangen P, Nakku J, et al. How competent are non-specialists trained to integrate mental health services in primary care? global health perspectives from Uganda, Liberia, and Nepal. Int Rev Psychiatry. (2018) 30:182–98. 10.1080/09540261.2019.1566116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jordans MJ, Garman EC, Luitel NP, Kohrt BA, Lund C, Patel V, et al. Impact of integrated district level mental health care on clinical and functioning outcomes of people with depression and alcohol use disorder in Nepal: a non-randomised controlled study. BMC Psychiatry. (2020) 20:1–3. 10.1186/s12888-020-02832-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kohrt BA, Schafer A, Willhoite A, Van't Hof E, Pedersen GA, Watts S, et al. Ensuring quality in psychological support (who equip): developing a competent global workforce. World Psychiatry. (2020) 19:115. 10.1002/wps.20704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tomlinson M, Rotheram-Borus MJ, Swartz L. Tsai AC. Scaling up mhealth: where is the evidence? PLoS Med. (2013) 10:e1001382. 10.1371/journal.pmed.1001382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yasmin F, Banu B, Zakir SM, Sauerborn R, Ali L, Souares A. Positive influence of short message service and voice call interventions on adherence and health outcomes in case of chronic disease care: a systematic review. BMC Med Inform Decis Mak. (2016) 16:1–4. 10.1186/s12911-016-0286-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Agarwal S, LeFevre AE, Lee J, L'engle K, Mehl G, Sinha C, et al. Guidelines for reporting of health interventions using mobile phones: mobile health (mHealth) evidence reporting and assessment (mERA) checklist. BMJ. (2016) 17:352. 10.1136/bmj.i1174 [DOI] [PubMed] [Google Scholar]
- 45.Wilson R, zu Erbach-Schoenberg E, Albert M, Power D, Tudge S, Gonzalez M, et al. Rapid and near real-time assessments of population displacement using mobile phone data following disasters: the 2015 Nepal earthquake. PLoS currents. (2016) 24:8. 10.1371/currents.dis.d073fbece328e4c39087bc086d694b5c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ni Z, Atluri N, Shaw RJ, Tan J, Khan K, Merk H, et al. Evaluating the feasibility and acceptability of a mobile health–based female community health volunteer program for hypertension control in rural Nepal: cross-sectional study. JMIR Mhealth Uhealth. (2020) 8:e15419. 10.2196/15419 10.2196/15419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Morrison JL, Shrestha NR, Hayes B, Zimmerman M. Mobile phone support for rural health workers in Nepal through 'Celemedicine'. J Nepal Med Assoc. (2013) 52:538–42. 10.31729/jnma.2287 [DOI] [PubMed] [Google Scholar]
- 48.Mars M. Telemedicine and advances in urban and rural healthcare delivery in Africa. Prog Cardiovasc Dis. (2013) 56:326–35. 10.1016/j.pcad.2013.10.006 [DOI] [PubMed] [Google Scholar]
- 49.Sharma SB. Telenursing-a potential resource in the eHealth agenda of India. J Int Soc Telemed eHealth. (2014) 2:19–28. [Google Scholar]
- 50.Government of Nepal . National e-Health Strategy (2017). [Google Scholar]
- 51.Ashish KC, Sunny AK, Poudel RP, Basnet O. A review of ehealth initiatives: implications for improving health service delivery in Nepal. J Nepal Health Res Counc. (2019) 17:269–77. 10.33314/jnhrc.v17i3.1787 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.