Abstract
We aimed to do a systematic review and meta-analysis of studies describing suicidal ideation, suicide attempts and suicide and associated risk factors during COVID-19 pandemic. We searched following electronic databases using relevant search terms: Medline, Embase, PsycInfo and CINAHL and systematically reviewed the evidence following PRISMA guidelines. The meta-analysis of prevalence of suicidal ideation was done using random effect model. The search returned 972 records, we examined 106 in full text and included 38 studies describing 120,076 participants. Nineteen studies described suicide or attempted self-harm, mostly in case reports. Out of 19 studies describing suicidal ideations, 12 provided appropriate data for meta-analysis. The pooled prevalence of suicidal ideation in these studies was 12.1% (CI 9.3–15.2). Main risk factors for suicidal ideations were: low social support, high physical and mental exhaustion and poorer self-reported physical health in frontline medical workers, sleep disturbances, quarantine and exhaustion, loneliness, and mental health difficulties. We provide first meta-analytic estimate of suicidal ideation based on large sample from different countries and populations. The rate of suicidal ideations during COVID pandemic is higher than that reported in studies on general population prior to pandemic and may result in higher suicide rates in future.
Keywords: pandemic, isolation, anxiety, depression, lockdown, COVID-19, suicide
1. Introduction
Approximately 86 million cases of COVID-19 have been recorded worldwide (Worldometer, 2021). Suicide and self-harm resulting from direct and indirect effects of the COVID-19 pandemic are a major public health concern. The measures employed by many countries to slow the spread of COVID-19 have ranged from physical/social distancing to full lockdown of cities. These strategies have led to major economic downturn. (International Monetary Fund, 2020). Social, psychological and economic consequences of COVID-19 are likely to affect suicide rates all over the world.
Previous pandemics had significant impact on livelihoods. Reduced food supplies and uncertainty about the future led to increased levels of anxiety in societies (Koh & Goh, 2020; Mak et al., 2009; UNDP, 2015). During the 2003 Severe Acute Respiratory Syndrome (SARS) outbreak, healthcare workers who treated infected patients reported higher levels of burnout, psychological distress, and Post Traumatic Stress Disorder than their peers who did not treat infected patients (Maunder et al., 2006).
Emerging research points to the mental health consequences of COVID-19 as different from previous pandemics, with symptoms of anxiety, depression and stress being common (Kumar & Nayar, 2020) in general population. The magnitude of global involvements, death toll, and imposition of social distancing policies, lockdown measures and isolation had huge social and economic impact. Unemployment alone can lead to up to three fold increased relative-risk of death by suicide, compared with being employed (Milner, 2013). Although the links between economic recessions and suicide are well-established, it is not clear how the relationship plays out in the situation of COVID-19. This relationship may be even more pronounced due to other risk factors such as physical distancing, lock-down, the scaling back of non-essential services and limited access to health care. The physical distancing measures and quarantine can be associated with loneliness (Brodeur et al., 2020) which in turn is a risk factor for suicide across many age groups (Daniel & Goldston, 2012; McClelland et al., 2020).
During this pandemic, self-harm is likely to increase due to limited social interaction and increased feeling of anxiety amongst communities. (Sahoo et al., 2020). Self-harm has been shown to be a risk factor for suicide (Murphy et al., 2012). Combined with the barriers to effective treatment due to several restrictions on face to face treatment, vulnerable individuals (Yao et al., 2020) may experience an increase in suicidal ideation, self-harm or suicide during the COVID-19 pandemic. Modelling studies based on the effect of the COVID-19 pandemic on suicide rates have emerged (Isumi et al, 2020; McIntyre & Lee, 2020). Isumi et al (2020) looked at the impact of COVID-19 on suicide rates during school closure in Japan, whilst McIntyre & Lee (2020) projected the number of excess suicides in Canada as a consequence of the impact of COVID-19 on unemployment. However, there is very little systematic evidence linking COVID-19 to an increased risk of self-harm and/or suicide.
Given that COVID-19 is novel for multitude of reasons discussed above, longitudinal data about its impact on suicide is currently unavailable. The primary aim of this review is to systematically review the evidence about suicide, self-harm and suicidal ideation during the COVID-19 pandemic. The secondary aims were to examine the prevalence of suicide or deliberate self-harm assess the quality of studies in this area, and to evaluate the psychological, social, and clinical risk factors for suicide and self-harm during the COVID-19 pandemic. We also aimed to carry out a Meta – analysis of outcome variables where appropriate.
2. Methods
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement guidelines (Moher et al., 2009). A protocol defining the key methodological parameters was developed prior to the literature search and was registered at the International Prospective Register of Systematic Reviews (PROSPERO) (https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020187255)
2.1. Search strategy
The following electronic databases and platforms were searched from November 2019 to 1st September 2020; Medline, Embase, PsycInfo and CINAHL. A search of the reference lists of the articles included at full text examination phase was carried out.
A search strategy based on following key search terms were used to identify the relevant literature: “Coronavirus” OR Sars-Cov-2" (all variants), “Suicide” OR “suicidal ideation” (all variants), “suicide attempted/ OR suicide” (all variants) "self-injurious behavioural” OR “self-mutilation” self-harm (all variants, "social distance *" OR "stay at home", “quarantine”, "self-isolation" “shield” "shelter-in-place". Truncations and related terms were used as appropriate based on individual database procedures (please see appendix-1 for full search strategy). The search was last updated in September 2020.
We included qualitative, quantitative, mixed methods study designs and case reports. We included all studies that reported individuals in any setting that reported suicidal ideations, suicide or self-harm in relation to the COVID-19 pandemic. We included all studies that described the relationship of suicidal ideations, suicide or self-harm with a COVID-19 related adversity, such as; lockdown, physical distancing, infection with COVID-19, or enduring the COVID-19 pandemic. There were no age restrictions applied. We included individuals of any age who hurt themselves by; cutting, overdoses, gunshot, jumping from height or similar techniques to end their lives. We included studies that; described the measurement of suicidal ideation using a validated measure, explored the prevalence of suicidal ideation in a population of interest, described suicidal attempts or suicide. Studies describing suicidal ideations, suicide or self-harm that was not related to the COVID-19 pandemic were excluded. We included any means of suicide or deliberate self-harm that occurred during the COVID-19 pandemic.
We excluded any studies that were not published in peer-review publications or did not include original data.
2.2. Data extraction and collection
After completing the search process and screening for relevant abstracts, examination of full text articles for inclusion and data extraction was completed by two reviewers (JT & WM) independently, as outlined in the protocol (https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020187255). Disagreements regarding study selection were resolved by consensus or, where appropriate, by a third reviewer (SF). References of articles were also manually searched to identify additional relevant articles.
A data extraction sheet was developed based on the pre- specified outcomes. Relevant data was extracted by three reviewers (JT, WM, MA) and cross checked by another reviewer (SF). Relevant data was extracted; author names, year of publication, country of publication, study design, setting, characteristics of participants, number of participants, inclusion/exclusion criteria, comparison group, method of assessing diagnostic criteria, method of assessing treatment outcomes and factors related to suicidal ideations, suicide or self-harm and COVID-19 (physical distancing, quarantine, lockdown, social isolation or adversities associated with COVID exposure).
2.3. Risk of Bias (quality assessment)
The quality of the studies was assessed independently by two reviewers (JT & WM), and cross checked by a third reviewer (MA) using appropriate checklists. There were no intervention studies included in the review, and therefore observational studies were assessed for quality using the Newcastle-Ottawa Quality Assessment Scale adapted for cross sectional studies (Modesti et al., 2016).
2.4. Meta-analysis
We performed a meta-analysis of prevalence of suicidal ideation. The studies provided percentage of participants reporting suicidal ideation. We meta-analysed the data examining the proportions. We reported the pooled prevalence with a 95% confidence interval (CI). If the same data were reported in more than one publication, we selected the publication that had the most complete data.
We expected many sources of heterogeneity in the studies, including assessment methods, settings, and populations studied. We used a random-effect model for meta-analysis because of heterogeneity. We examined the CIs in the forest plot for variability in the studies and we are reporting an I2 statistic as an indicator of heterogeneity.
We used R packages Meta (version 4.15-1) and metafor (version 2.4-0) for analysis. The analysis was performed in R version 3.6.1. In our meta-analysis we considered individual study weights and utilized the inverse variance method with the Freeman-Tukey double arcsine transformation (Barendregt et al., 2013). As recommended by Schwarzer et al (2019) we performed sensitivity analysis by comparing the results with logit transformations. We used DerSimonian-Laird estimator for tau^2 (DerSimonian and Laird, 1986) and Jackson method for confidence interval of tau^2 and tau.
3. Results
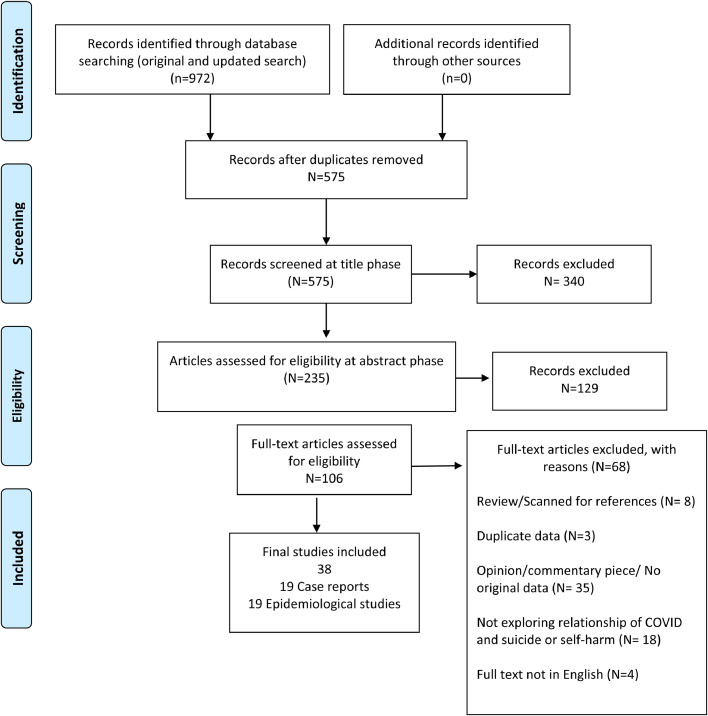
The search returned 972 records. After removing duplicates, 575 titles were screened at title phase. We screen 235 records at abstract phase and excluded 129 records. We selected 106 articles for full text examination, 68 records were excluded and we finally included 38 studies. The reasons for exclusion and details of study selection are given in PRISMA diagram (Fig. 1 )
Fig. 1.
PRISMA 2009 Flow Diagram. Figure legend: Fig. 1 denotes the PRISMA diagram which shows search process that was carried out in selecting texts for final review.
3.1. Characteristics of included studies
Broadly we identified two types of studies. (i) Articles describing suicides and suicidal attempts mostly published as case reports. (ii) Epidemiological studies describing suicidal ideation or self-harm behaviour and associated risk factors. All studies included 120,076 participants. Most studies were published from US (8), India (7), China (7), Bangladesh (3), United Kingdom (2),
The characteristics of included studies are given in table 1 and 2 .
Table 1.
Characteristics of included studies describing attempted suicide and suicide.
| Author/ Year/ Country | Country | Mental health condition | Suicide/ attempted suicide | Relationship with COVID | Comments |
|---|---|---|---|---|---|
|
Goyal et al. (2020) |
India | Not specified | Suicide | Believed he had COVID-19 and was fearful of infecting others |
50-year-old male, Father of three Became preoccupied with media coverage of COVID-19 |
|
Mamun & Ullah (2020) |
Pakistan | Not specified | Attempted suicide and suicide | Economic recession and distress, Fear of COVID-19 infection |
12 suicides, 4 attempted suicides based on media reports |
|
Zhang et al. (2020) |
China | Acute and Transient Psychotic Disorder | Attempted suicide | Fearful of COVID-19 and suspected he was infected despite negative test result. | Male, 20 years old, student. Existing mental health problems |
|
Rani et al. (2020) |
India | Alcohol dependence | Attempted suicide | No access to alcohol due to COVID-19 lockdown withdrawal symptoms | Male, 60 years old, farmer in the community with history of alcohol dependence for 20 years |
|
Epstein et al. (2020) |
Israel | Anxiety and insomnia | Attempted suicide. | Positive for COVID – 19 and on an isolation ward in hospital. During hospital stay, developed anxiety and insomnia symptoms | Male, 34 years old, staying in hospital. medical history of diabetes mellitus and smoking |
|
Aquila et al. (2020a) |
Italy | None described | Suicide | Fear of COVID-19, awaiting test results, forced cohabitation, fear of spreading COVID-19, financial concerns | 10 cases described based on newspaper reports. Cases included 3 nurses and a medical director |
|
Aquila et al. (2020b) |
India | Obsessive thinking and anxiety | Suicide | Obsessive ideas about his health and fear of the global pandemic | Male, 60 years old, retired. Existing mental health problems. Suicide notes detailed his anxiety and obsessive thoughts |
| Rahman et al. (2020) |
Worldwide (Italy, United Kingdom, United States, Mexico, India) | Out of 6 cases, one patient had opioid addiction | Suicide | Awaiting test results, positive COVID-19 result, experiencing COVID-19 symptoms, lack of suitable personal protective equipment, under quarantine restrictions |
6 cases of nurses Based on news reports (49, twenties, 34, 32, age not given, age not given) |
| Lathabhaven et al. (2020) |
India | None stated. ‘Depressive feelings’ |
Suicide | Student concerned about academic performance due to lack of online access for economic reasons. | 15 year old female in the community |
|
Mamun et al. (2020a) |
Bangladesh | None stated | Suicide | Unresolved argument related to online schooling issues caused by COVID-19 quarantine and spatial distancing policies |
‘Suicide pact’ Mother (47) and son (22, university student) dyad in the community. |
|
Mamun et al. (2020b) |
Bangladesh | None mentioned | Suicide | Woman was unable to get treatment for her condition by anyone at the hospital allegedly due to the fear of COVID-19 transmission |
40 year old woman In hospital at time of suicide |
|
Liu et al. (2020) |
China | No history of mental illness ‘Depressive feelings’ |
Attempted suicide | Patient and four of his family members tested positive for COVID-19. Strong sense of guilt of infecting others and worry about being discriminated |
52 year old male admitted to hospital |
| Griffiths et al. (2020) |
India, United States and Bangladesh | None reported | Attempted suicide and suicide | COVID-19 related suicide due to fear of being infected with COVID-19, COVID-19 related ‘tension’, fear of contracting COVID, isolation and quarantine from wife and pressure / discrimination from community, financial consequences of COVID-19 | 6 cases of male female couples based on news reports COVID-19-related Murder-suicide by gunshot. Male shot his partner (who had been suffering from severe breathing problems) before killing himself |
| Mamum & Griffiths (2020) |
Bangladesh | None described | Suicide | Himself and the people in his village believed him to be infected with COVID-19. Prejudice from his community | 36-year-old. Autopsy results showed that he did not have COVID-19 Male, age not specified, from India took his own life, to avoid spreading COVID-19 around his village |
|
Sahoo et al. (2020) |
India | Development of mental health difficulties; excessive worrying, refusal to eat, anxiety. | Attempted suicide | Fear of contracting COVID-19 and excessive worrying about his own death and the death of his family members. Self-isolation worsened his anxiety | 52-year-old male and 40-year-old male in the community |
|
Rana (2020) |
India | Major Depressive Disorder | Suicide | Fear of COVID-19, fear of infecting others | 5 older adultsdied by suicide due to a relapse of major depressive disorder. One couple left a suicide note. Negative COVID-19 test result after suicide. Male & Female couple suicide pact (age not given) 2 Males (75 & 60 years old) 1 Female (65 years old) |
|
Mirza et al. (2020) |
United States | Command auditory Suicidal Hallucinations | Attempted suicide | Tested COVID positive Some general COVID-19 anxiety |
No prior psychiatric or physical medical history 53 year old male |
|
Ahmed et al. (2020) |
India | Alcohol withdrawal symptoms | Suicide | Could not get alcohol due to COVID-19 lockdown restrictions | Evidence from media reports 23 males died by suicide due to the unavailability of alcohol during COVID-19. Age ranged from 28 to 70 years 15 men took their own life within the first 7 days of the lock down. |
|
Buschmann & Tsokos (2020) |
Germany | All eleven cases suffered pre-existing mental difficulties including depression and hypochondriacal delusion |
Suicide | Fear of COVID-19 Effect of COVID-19 lockdown |
11 cases described None proven as being COVID-19 positive |
Table 2.
Characteristics of studies describing suicidal ideation and self-harm behaviours.1
| Author/Year/ Country | Design | Participants | Outcome measure related to suicide or self-harm | Population/ Setting |
|---|---|---|---|---|
|
Smalley et al. (2020) United States |
Retrospective multi centre study Quality improvement project |
Visitors to the emergency department with a ‘behavioural health’ issue | Self-harm and alcohol use were identified as ‘behavioural health’ issue. Data was collected on the occurrence of these at the emergency department. During the one-month study period, the hospital system had 31,387 ED encounters with 2477 (7.9% of visits) |
Emergency department patients |
|
Cai et al. (2020) China |
Case control study | N= 2346 (1173 frontline and 1173 age- and sex-matched non-frontline medical workers) M=702 F= 1644 |
Suicidal ideation Patient Health Questionnaire-9 (PHQ-9) Suicidal ideations were measured by one question: “Over the past two weeks, have you ever had suicidal thoughts?” The responses to this question were “Once/several times” or “Never” |
Community and medical workers |
|
Bryan et al. (2020) United States |
Cross-sectional | Adults N=10, 625 general population survey |
Self-injurious thoughts, suicidal ideation, attempted suicide Self-Injurious Thoughts and Behaviors Interview (SITBI) |
Community general population |
|
Caballero-Domínguez et al. (2020) Colombia |
Cross-sectional | N=700 F=476 M=224 General population survey |
Suicide risk Depression Scale of the Center for Epidemiological Studies (CES-D-IS). |
Online community |
|
Xiaoming et al. (2020) China |
Cross-sectional survey | 8817 hospital workers F= 6874 M= 1943 |
Suicidal and self-harm ideation | Hospital workers |
|
Xin et al. (2020) China |
Cross sectional survey | N= 24,378 M= 7,865 F= 16,513 |
Self-harm or suicidal ideation The item “Over the past 2 weeks, how often have you thought that you would be better off dead, or of hurting yourself” of the Patient Health Questionnaire-9 |
Community – university students |
|
Killgore et al. (2020) United States |
Cross sectional survey | N=3120 18–84 years old; F= 1691 M= 1429 General population |
Suicidal ideation Patient Health Questionnaire – 9 (PHQ-9) |
Community-Online |
|
Gratz et al. (2020) United States |
Cross sectional survey | N= 500 F= 235 M=259 General population |
Suicide risk The Depression Symptom Index-Suicide Subscale (DSI-SS) |
Community – Online |
|
Ahorsu et al. (2020) Iran |
Cross-sectional survey | Total N= 580 Pregnant women (n= 290) Their husbands (n=290) |
Suicidal ideation Patient Health Questionnaire-9 |
Community – Pregnant women and their husbands |
|
Li et al. (2020) Taiwan |
Cross sectional survey | 2031 respondents, data of 1970 analysed. F=1305 M= 650 Transgender=15 |
Suicidal thoughts Suicidal thoughts were assessed with the question on a 5-point Likert scale, with scores ranging from 0 (never) to 4 (extremely severe). |
>20 years old Facebook users |
|
Hao et al. (2020) China |
Cross sectional survey | Total n = 185 Psychiatric Patients (n = 76, M=25, F=51). Healthy controls (n = 109, M=41, F=68). |
Suicidal Ideation | Hospital – dedicated to COVID-19 |
|
Fitzpatrick et al. (2020) United States |
Cross sectional survey | 10,368 adults General population |
Suicidal ideation and attempts Suicide Behavior Questionnaire (SBQ-R) |
Online community |
|
Hou et al. (2020) China |
Cross sectional survey | N= 859 524 students were left-behind children. Males (61.4 %) 16 years and below 79.4% |
Suicidal ideation and attempts Measured with two items “I thought about killing myself” (Yes/no) and “I deliberately tried to kill myself” (Yes/no). |
Senior high school students in rural China |
|
Papadopoulou et al. (2020) Greece |
Cross sectional survey | N= 5116 M=1292 F= 3819 Other = 5 |
Suicide ideation PHQ-9 |
Online community |
|
Czeisler et al. (2020) United States |
Cross sectional survey | N=5412 F= 2784 M= 2676 Other=10 General population |
Suicidal Ideation PHQ-9 |
Online community |
|
Olding et al. (2020) United Kingdom |
Prospective cohort study | 14 participants Data was collected prospectively and reviewed retrospectively on trauma attendances to King's College Hospital |
Self-harm during the lockdown |
Hospital |
| Iob et al. United Kingdom |
Longitudinal survey | N = 44 775 M= 21929 F= 22 846 |
Thoughts and attempts of self-harm suicide, self-harm behaviours Patient Health Questionnaire (PHQ-9) |
Online community |
|
Kim et al. (2020) Korea |
Qualitative | 72 caregivers, M=18 F=54 |
Suicidal ideations Scale not specified |
Caregivers quarantined with young patients after a close contact to a coronavirus disease 2019 case at a children's hospital |
|
Hamm et al. (2020) United States |
Mixed Methods | 73 participants (M= 23,F= 50). Mean age 69.2 (6.0) | Suicidal ideation PHQ-9 item 9, |
Patients with a pre-existing diagnosis of Major depressive disorder |
3.2. Studies on suicide and suicidal attempts
Nineteen studies included 79 cases of suicide and 13 cases of attempted suicide. These were mostly case reports (15 articles) and cases based on news reports (4 articles). These studies included 57 males and 20 females. Suicide cases included members of the community and (n=75) and healthcare and frontline workers (n=10). Eight suicide pacts were described that included a mother- son, and young and elderly couples. The details of suicide and attempted suicide including underlying mental health conditions, means of suicide/ attempted suicide, relationship with COVID-19 and a brief description of cases are given in Table 1.
The main concerns related to COVID-19 in cases of suicide and attempted suicide included: fear of being infected or infecting others, shame and guilt, economic recession and financial hardship, stress due to COVID-19 pandemic and lockdown, self-isolation, being unable to access alcohol, lack of access to educational resources and prejudice from communities. Fear of already being/becoming infected with COVID-19 was prevalent across all cases reported and a significant factor in attempting/completing suicide (n=40). Three patients were awaiting the outcome of their COVID-19 swab result when they took their lives, and the remainder did not know whether they were infected or not, or the information was not given in the studies. Only four cases were actually COVID-19 positive (see table 1 for details).
Two suicides appeared to be due to academic pressures arising from the COVID-19 pandemic. In a suicide pact, a mother and her son ingested poisonous tablets, after an argument with the father/husband related to online schooling issues caused by COVID-19 quarantine and spatial distancing policies (Mamun et al., 2020a). Lathabhavan et al (2020) describes the case of a 15 years old female student who ended her own life due to lack of available resources to complete home schooling. The girl was classed as ‘gifted’ and worried about her academic performance as her family could not afford the equipment to enable her to complete her schooling from home.
Ten cases of suicides and attempted suicides in healthcare workers were described in two articles. Aquila et al. (2020a) reported three Italian nurses working in COVID-19 units who had died by suicide, fearing they had spread the infection, and also reported the suicide of the medical director of an emergency department in Manhattan. In a study based on newspaper reports Rahman and Plummer (2020) describes six cases of suicide in nurses in Italy, England, United States and India. Contributing factors to suicide in these cases were; fear of being infected with COVID-19, critical shortage of personal protective equipment, working with COVID-19 positive environments, and a positive test result for COVID-19.
3.3. Studies describing suicidal ideation or self-harm behaviour and associated risk factors
Nineteen studies including 119,984 participants provided data on suicidal ideations, self-harm thoughts and associated risk factors. Sixteen studies provided data on prevalence of suicidal ideations or examined relationship between a risk factor related to COVID-19. Studies investigated a number of risk factors for suicidal ideation. Out of these, 12 studies had data that was suitable for meta-analysis. Details of risk factors is given in Box 1, while Table 2 describes methodologies used, outcome measures, population characteristics and instruments used.
Box 1. describes the factors associated with suicidal ideations and attempts.
Factors associated with suicidal ideations and attempts
-
•
Fear of COVID-19 or lack of knowledge about COVID-19 (Ahorsu et al., 2020, ; Caballero-Domínguez et al., 2020; Xiaoming et al., 2020)
-
•
COVID-19 diagnosis. (Iob et al., 2020)
-
•
Lower perceived social support and lower COVID-19-specified support (Li et al., 2020)
-
•
High rates of physical and mental exhaustion in frontline medical workers (Cai et al., 2020)
-
•
Sleep disturbances resulting from academic/occupational pressures (Li et al., 2020)
-
•
Poor self-rated health condition among hospital workers (Xiaoming et al., 2020; Li et al., 2020),
-
•
Quarantined during COVID-19 (Hao et al., 2020; Kim et al., 2020; Xin et al., 2020)
-
•
Loneliness during pandemic and thwarted belongingness (Killgore et al., 2020, Gratz et al., 2020)
-
•
Financial strain (Byran et al., 2020)
-
•
Stress related to a life-threatening illness or injury of a close friend or family member (Bryan et al., 2020)
-
•
Being employed and/or being an essential worker (Czeisler et al., 2020)
-
•
Chronic physical illnesses (Iob et al., 2020)
-
•
Psychiatric diagnosis (Iob et al., 2020)
-
•
Belonging to a high risk group for COVID-19 infection (Papadopoulou et al., 2020)
Alt-text: Unlabelled box
Twelve studies (Caballero−Dom'nguez et al., 2020; Li et al., 2020; Iob et al., 2020; Byran et al., 2020; Fitzpatrick et al., 2020; Czeisler et al., 2020; Killgore et al., 2020; Cai et al., 2020; Xin et al., 2020; Xiaoming et al., 2020; Hou et al., 2020; Papadopoulou., 2020) had data that was suitable for meta-analysis which is described below.
3.4. The meta-analysis of prevalence of suicidal ideation
There were 15 datasets from 12 studies that provided suitable data for meta- analysis. Cai et al (2020) had two groups in their study; frontline health workers and non-frontline health workers. Killgore et al (2020) had separate samples for three consecutive months and we treated those as separate datasets. The total sample size in these studies is 113428.
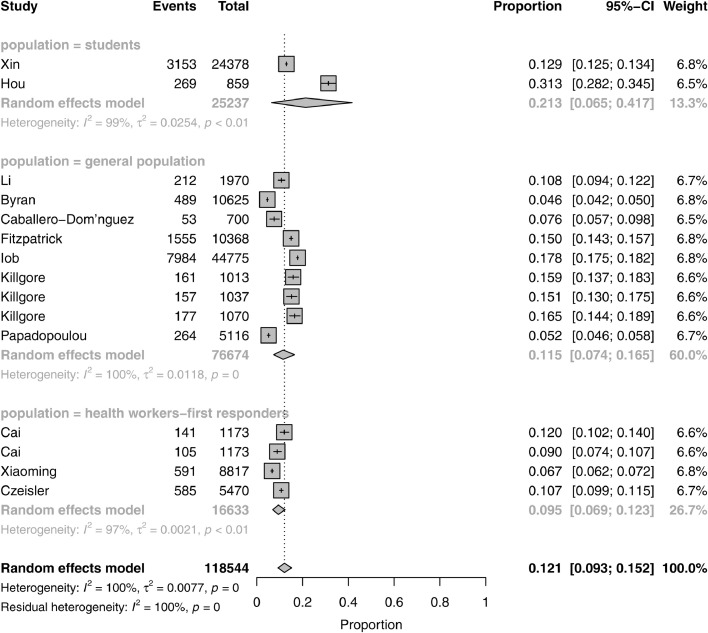
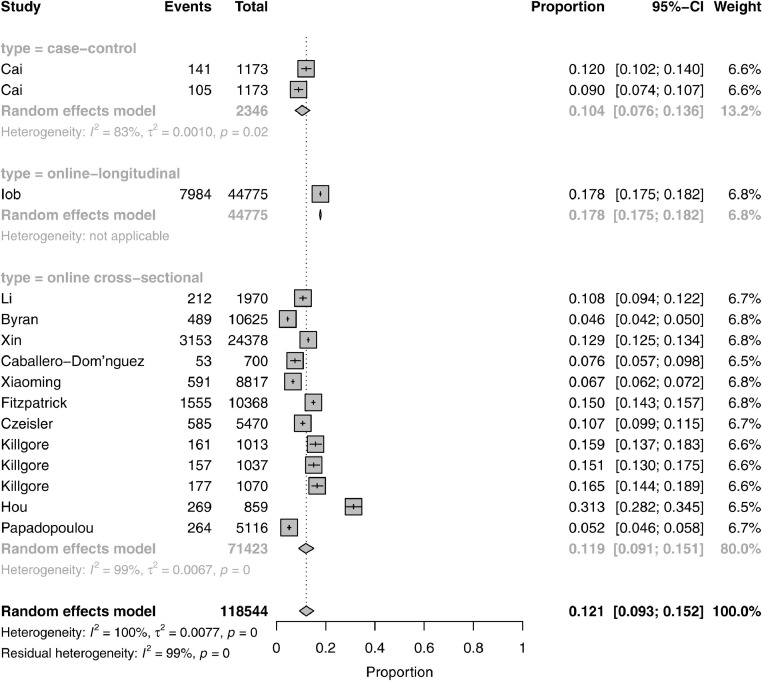
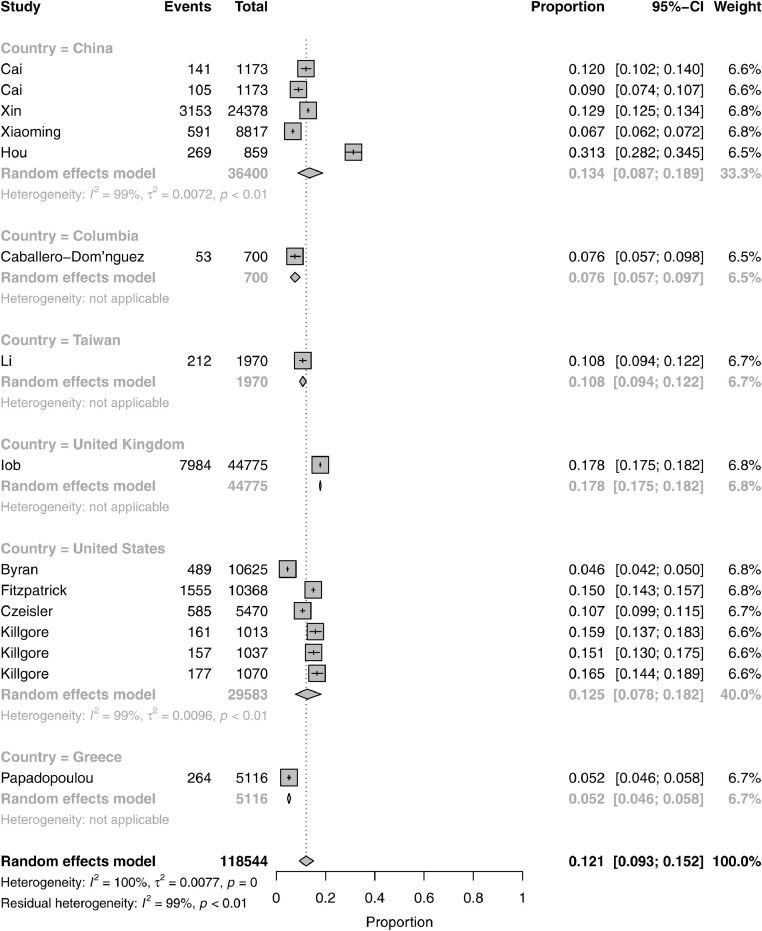
The pooled prevalence of suicidal ideation in these studies was 12.1% (CI 9.3–15.2). The logit transformation resulted in prevalence of 11.5% (CI 9.2–14.3). As the results are close to each other we are only reporting results for Freeman-Tukey double arcsine transformation. The level of heterogeneity was high as expected (I2 = 100%, τ2 = 0.0077, p = 0). We conducted sensitivity analysis based on country of publication, population studied and the study design, the results are summarised in Fig. 2, Fig. 3, Fig. 4 . The pooled prevalence of suicidal ideation for different populations were; general population 11.5% (95CI 7.4–16.5), students 12.3% (95CI 6.5–41.7), health care workers and first responders 9.5% (6.9–12.3) (Fig -2). One longitudinal study by Iob et al (2020) accounted for largest number of participants (= 44775) and suicidal ideation prevalence of 17.8% (95 CI 17.5 - 18.2), while case control study had prevalence of 10.4% (95% CI 7.6–13.6). Rest of studies were cross sectional and had pooled prevalence of 11.9%% (95CI 9.1–15.1) (Fig- 3). The prevalence in different countries was as following: China 13.4% (8.7–18.9), Columbia 7.6% (5.7-9.7), Taiwan 10.8% (9.4–12.2), United Kingdom 17.8% (17.5–18.2), United States 12.5% (7.8–18.2), Greece 5.2 (4.6–5.8) (Fig-4)
Fig. 2.
Fig. 2 shows the pooled prevalence of suicidal ideation for different populations.
Fig. 3.
shows the pooled prevalence of suicidal ideation across the different study designs.
Fig. 4.
shows the pooled prevalence of suicidal ideation across the different countries of publication.
3.5. Relationship between suicidal ideations, suicide or self-harm and the pandemic
In view of high heterogeneity, variety of different variables analysed in included studies and methodologies used in measuring these, we decided against producing a meta-analysis of the association between risk factors and suicidal ideation. A narrative summary of major findings describing relationship between suicidal ideations and the risk factors is given below. Eight studies examined different risk factors prevalent during the pandemic in general, while eight studies examined risks arising from COVID-19 related restrictions such as lockdown and physical distancing measures.
3.5.1. Relationship between suicidal ideations and COVID-19 risk factors
In a cross sectional survey (Czeisler et al., 2020) found that being a carer for adults was associated with higher risk of suicidal ideations (adjusted OR 95% CI 1.20-7.63 p=0.01). Fitzpatrick et al (2020) reported that nearly 15% of respondents in their study were categorized as high risk, scoring 7+ on the SBQ-R (Suicide Behavior Questionnaire); families with children, unmarried, and younger respondents reported higher SBQ-R scores than their counterparts (p < 0.000). Those reporting moderate or high levels of food insecurity were four times more likely to be in the high SBQ-R category compared to those reporting no or low food insecurity (p < 0.000).
Papadopoulou et al (2020) used cross sectional survey to examine suicidal ideation amongst 5116 adults in Greece. Individuals belonging to a high risk group for COVID-19 infection were more likely to have suicidal ideations (p=0.005). Individuals who took part in the survey during the first half (i.e., first 2 weeks) presented significantly lower suicidal ideation (4.31% vs. 7.70%, p < 0.001), anxiety (12.91% vs. 17.75%, p < 0.001), and depression (24.95% vs. 30.94%, p < 0.001), than those who responded during the second half (i.e. latter 2 weeks) of the study period.
Caballero-Domínguez et al (2020) assessed the association between perceived stress related to COVID-19 and suicide risk and found that 7.6% of study participants reported a high suicide risk. High perceived stress related to COVID-19 (Adjusted Odds Ratio 12.69 [6.32–25.68]), depression (adjusted OR= 8.49; CI = 2.58–27.99) and insomnia (adjusted OR= 9.91; CI3.14–15.21) were associated with high suicide risk.
In a cross sectional survey of hospital workers in China, Xiaoming et al (2020) showed that the need of psychological assistance before and during the pandemic, concern about pandemic, and self-rated health condition were risk factors for high level of suicidal and self-harm ideation.
Cai et al (2020) examined suicidal ideation in 1173 frontline medical health workers and in a similar number of age- and sex-matched non-frontline medical workers. Frontline medical workers had higher rates of any mental problem (52.6% vs. 34.0%, adjusted OR=1.88, 95% CI=1.57–2.25) than non-frontline medical workers. No significant difference was observed in terms of suicidal ideation (12.0% vs. 9.0%, adjusted OR=1.25, 95% CI=0.92–1.71).
In a cross sectional online survey Ahorsu et al (2020) examined effect of COVID on mental health in pregnant women and their partners in Iran. In total, 290 pregnant women and their husbands participated in the study. Fear of COVID-19 among pregnant women (β = 0.44, SE = 0.01, p < 0.001) and husbands (β = 0.29, SE = 0.01, p < 0.001) was positively associated with higher suicidal ideation.
Li et al (2020) found that less handwashing, lower perceived social support, lower COVID-19-specified support, poorer self-reported physical health, and younger age were significantly associated with suicidal thoughts.
3.5.2. Relationship between suicidal ideation and COVID-19 related restrictions
Eight studies examined effects of COVID related restrictions and physical distancing measures. Iob et al (2020) used the data from the COVID-19 Social Study, a longitudinal study on the psychological and social experiences of over 50000 adults in the UK during COVID lockdown. In total, 7984 participants (18%) reported experiencing thoughts of suicide or self-harm and 2174 participants (5%) reported harming themselves at least once since the start of the UK's lockdown. Out of the people that reported having thought of self-harm or suicide 43.5% also had a mental health diagnosis.
Bryan et al (2020) found suicidal ideations were generally unrelated to physical distancing measures. General population participants who were subject to large gatherings bans were significantly less likely to report a suicide attempt in the prior month (OR=0.39, 95% CI=0.17–0.88, p=0.024). Smalley et al (2020) examined the effect of ‘stay at home’ orders during the COVID-19 pandemic in data based on 750,000 visits to the emergency department. It was found that suicidal Ideation complaints fell significantly during the “stay at home”. When comparing 2019 to 2020, suicidal ideations encounters decreased by 60.6%.
Hao et al (2020) found that significantly more psychiatric patients reported moderate to severe suicidal ideation than healthy controls (11.8% versus 0.9%, [p < 0.05]) when strict lockdown measures were in place in China. In a study of Chinese students, Xin et al (2020) found that mandatory quarantine status was moderately or strongly associated with self-harm or suicidal ideation (41.2 vs. 12.3%, OR _ 4.98). Killgore et al (2020) examined the effects of COVID restrictions over the first three months (April-June 2020) of the pandemic in the United States. For those participants who were under lockdown, the percentage of individuals reporting any suicidal ideation increased significantly over the three-month period, from 17.6% in April to 30.7% by June (F2,2241=16.13, p<0.00001, partial .2=0.014). Killgore et al., 2020 also found that loneliness scores were positively correlated with suicidal ideation at each observed time point (April. =.42, May. =.40, June. =0.39, all p-values <0.00001), even after controlling for other symptoms of depression. Gratz et al (2020) showed a significant indirect relation of stay-at-home order status to suicide risk through thwarted belongingness.
3.6. Quality assessment of included studies
We used Newcastle-Ottawa Quality Assessment Scale (NOQAS) for the observational studies. The NOQAS provides 1-3 stars for each item such as such as description of cohorts, outcome and ascertainment of exposure, and we converted this to a numerical score. The maximum score for a study is 10. Only two studies (Fitzpatrick et al 2020; Bryan et al (2020) scored 8 on NOQAS. Six studies (Killgore et al, 2020; Iob et al., 2020; Hao et al., 2020; Cai et al., 2020; Caballero – Dominguez et al., 2020; Ahorsu et al., 2020) scored a total of 7, four studies had a score of 6 (Xiaoming et al., 2020; Hamm et al., 2020; Gratz et al., 2020; Czeisler et al., 2020), three studies scored 5 on NOQAS (Xin et al., 2020; Smalley et al., 2020; Hou et al., 2020), three studies scored a total of 4 out of ten (Olding et al., 2020; Li et al., 2020; Papadopoulou et al., 2020) and Kim et al., (2020) only scored two.
4. Discussion
The main findings are that in relation to COVID pandemic (i) literature on suicide is limited to mainly case reports that recorded following reasons for suicide: fear of contamination and the disease, poor care for COVID-19 patients, financial hardship, lockdown, self-isolation, alcohol withdrawal and lack of access to educational resources and stigma (ii) the pooled prevalence of suicidal ideation was 12.1% and (iii) the COVID-19 related factors such as loneliness, physical distancing measures appeared to be important contributory factors to suicidal ideation but evidence was not consistent across studies.
Even a small increase in suicide may affect a large number of people due to the scale of the current pandemic. Literature on suicide during this pandemic is sparse and is almost entirely limited to case reports. This literature can inform clinical practice and can help in identifying research questions for future epidemiological studies. It was clear that majority of cases COVID-19 (or fear of it) precipitated suicide in people who had pre-existing mental health conditions. The role played by media coverage of COVID-19 (Rana et al., 2020), educational pressures on adolescents and economic factors are highlighted by these case reports and need to be investigated in future studies.
Based on these studies it is not possible to comment whether COVID-19 had any effect on suicide rates. A systematic review (Leaune et al., 2020) showed that previous pandemics did not increase the risk of deaths by suicide in people with pre-existing psychiatric disorders but the evidence was limited to only three studies. There is emerging evidence that suicide rates in present pandemic have remained unchanged or declined. Pirkis et al (2021) found that in high-income and upper-middle-income countries, suicide numbers have remained largely unchanged or declined in the early months of the COVID pandemic. Deisenhammer and Kemmler (2021) found a significant decrease in suicide numbers during the first 6 months of the COVID-19 pandemic compared to the respective periods of the preceding year in Austria. Considering that the present pandemic has had a global effect, this evidence is limited to few high and middle income countries, further evidence is needed to understand the impact of present pandemic on rates of suicide.
The estimates of suicidal ideation prevalence vary depending upon population studied, methods used and the location of study (Biswas et al., 2020). The pooled prevalence of suicidal ideation for all participants in our meta-analysis was 12.1%. The pooled prevalence of suicidal ideation for different populations were as following; general population (11.5%), students (12.3%) and health care workers and first responders (9.5%). Sensitivity analysis based on population, country of study and study design showed that only study design accounted for large variation in the prevalence rates. The only longitudinal study by Iob et al (2020) which accounted for 37.7% of the whole sample showed a prevalence of about 17.9%. The findings of Cai et al (2020) and Xiaoming et al (2020) demonstrate that an important consideration is the unique stresses that healthcare professionals have faced during the pandemic, and the impact this has on rates of suicidal ideation. Their findings demonstrate the need for additional support for healthcare staff during a pandemic.
The prevalence of suicidal ideation found in general population was 11.5% which is higher than the prevalence generally reported in literature. A meta-analysis of studies done in mainland China found a pooled lifetime prevalence 3.9% for suicidal ideation in the general population. A cross national study in 17 countries reported lifetime prevalence of suicidal ideation of 9.2% based on a sample of 84,850 adults (Nock et al., 2008). Que et al. (2019) included 73 longitudinal and cross-sectional studies and found a pooled global prevalence estimates of 9•8% for suicidal thoughts in the past 12 months, and 8•0% for recent suicidal thoughts among medical professionals.
Whilst it is important to note that suicidal ideation does not necessarily lead to deliberate self-harm or suicide the psychosocial effects of the COVID-19 pandemic may be the main risk factors for an increase in suicidal ideation. Studies investigated a number of factors as shown in Box-1 that could contribute to high suicidal ideation. Eight studies investigated the effects of COVID-19 related restrictions. With the exception of one study (Bryran et al., 2020), these studies found that COVID-19 lockdown, social distancing measures and stay at home orders were associated with increased suicidal ideation. Studies in previous pandemics (Leaune et al., 2020) and in the infectious diseases such as HIV (Aro et al., 1995) found that fear of being infected by the virus was reported as major reason for suicidal ideations, suicide or self-harm. Social isolation is also considered to be a significant risk factor for deaths by suicide during the 2003 SARS outbreak. Objective social isolation and subjective feelings of loneliness are associated with higher suicidal ideation suicide or self-harm in the general population (Calati et al., 2019). An important finding from the Killgore et al. (2020) study included in this review points to loneliness scores being positively correlated with suicidal ideation, at different time points throughout the pandemic. It is therefore important to consider loneliness when assessing risk in individuals who express suicidal ideations, or who have attempted suicide or carried out self-injurious behaviours. Furthermore, as Calati et al (2019) also recommend, addressing issues around loneliness should be an important part of any interventions that target suicide prevention. However, the long term effects of social isolation are not fully understood yet with regards to the current pandemic. The COVID-19 pandemic has affected populations globally and technologies, such as videoconferencing, are now more widely available to enhance social connectedness. Although, it is important to note that these are not accessible to everyone
4.1. Strengths and limitations
This is a comprehensive systematic review that covers suicidal ideations, acts and suicides. We used a robust methodology following PRISMA guidelines, a pre-specified and comprehensive search strategy that captured 38 studies providing information on 119000 participants. A previous systematic review (John et al., 2020) included 28 studies. To the best of our knowledge, this the first study that provides a meta-analysis of the prevalence of suicidal ideations.
The major limitation of this review is the low quality of included studies and poorly reported mental health outcomes. Studies on suicide during the pandemic are particularly scarce. Almost all included studies had high or unclear risk of bias. Thirteen studies were cross -sectional in design. Almost all were based on online interviews and survey questionnaires completed remotely. All studies relied on self-report measures and with the exception of five (Smalley et al., 2020; Olding et al., 2020; Kim et al., 2020; Hamm et al., 2020; Gratz et al., 2020). Only three studies used a specific, validated measure for suicidal ideation and intention (Bryan et al., 2020; Gratz et al., 2020; Fitzpatrick et al., 2020), the rest relied on suicide or self-harm items of depression scale such as the Patient Health Questionnaire- 9 (PHQ-9) (Kroenke et al., 2001) and the General Anxiety Disorder- 7 (GAD-7) (Spitzer et al., 2006). The long term effects of living through the pandemic, effects of COVID in those who contracted the disease and received highly potent drugs such as steroids or care in Intensive Treatment Units remain largely unknown.
We used a comprehensive search strategy but may have missed some studies from low and middle income (LAMI) countries. It is well known that the major databases such as Medline or EMBASE cover less than 50% of research from LAMI countries, as most journals published in LAMI countries are not indexed in these databases. For example, Pakistan is an LAMI country with over 100 medical journals, however only six of these journals are indexed in PubMed (PakMediNet, 2021). This may be important considering large population affected by COVID in countries such as India and Brazil. The prevalence of suicidal ideation estimates are based on heterogeneous populations. High risk groups such as clinicians and frontline staff in health care facilities may be more prone to mental health consequences of COVID but there were only two studies from this group. Despite these limitations, we believe we have estimated the prevalence of suicidal ideations and factors that underlie suicidal ideations, suicide or self-harm in a pandemic. We highlight the diagnostic and screening measures that were used in the included studies, which could possibly be used to help design future studies. This information will help to design better epidemiological and intervention studies in future.
4.2. Implications
Our results highlight the need to perform high quality research on suicide risk and prevention in the current pandemic context. In view of the high prevalence of suicidal ideation, it is important that practitioners should routinely assess for fear of infection during the COVID-19 pandemic to detect people with higher suicide risk. This is important in case of high risk people such as those in nursing homes, the elderly and those in quarantine measures.
Social connection plays a key role in suicide prevention. The prevention of loneliness induced by quarantine measures should be included in public health interventions during the COVID-19 pandemic. Brief contact interventions such as post-discharge telephone contacts; emergency or crisis cards; and postcard or letter contacts may be useful in providing social support and promoting distance-based access to mental health care and have been used to reduce suicide risk (Milner et al., 2016). It would be important to evaluate these interventions in people facing quarantine and social isolation.
Future studies need to use reliable and valid measures for identification of suicide risk, include a proper control group and adequate follow up for identification of risk factors for suicide and self-harm during the COVID-19 pandemic. Studies in people who have experienced COVID-19 infections are practically non-existent. In view of the fact that there are now millions of people who have been COVID-19 positive and have experienced the trauma associated with COVID treatment, future studies need to examine the psychological effects and, suicidal ideation, self-harm and suicide in this population. The included studies were performed in a small number of countries. Suicidal ideations, suicide or self-harm are known to be shaped by cultural and social contexts. Across the globe, a COVID-19 diagnosis and its implications will be different, and this needs to be handled with a degree of skill and expertise. It is important to conduct properly designed studies in different countries, especially in low and middle income countries who are facing a large prevalence of COVID-19 infection.
Declaration of Competing Interest
We have no conflict of interest to declare.
Acknowledgments
We would like to acknowledge our information specialist Fiona Rees, who along with the library team, supported us with conducting the search, and providing advice.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2021.114228.
Smalley et al. (2020) does not give number of participants, only gives emergency department 'encounters' which are episodes of care
Appendix. Supplementary materials
References
- Ahmed S., Khaium M.O., Tazmeem F. COVID-19 lockdown in India triggers a rapid rise in suicides due to the alcohol withdrawal symptoms: evidence from media reports. Int. J. Soc. Psychiatry. 2020;66(8):827–829. doi: 10.1177/0020764020938809. [DOI] [PubMed] [Google Scholar]
- Ahorsu D.K., Imani V., Lin C.Y., Timpka T., Broström A., Updegraff J.A., Årestedt K., Griffiths M.D., Pakpour A.H. Associations between fear of COVID-19, mental health, and preventive behaviours across pregnant women and husbands: an actor-partner interdependence modelling. Int. J. Mental Health Addict. 2020:1–15. doi: 10.1007/s11469-020-00340-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aquila I., Sacco M.A., Ricci C., Gratteri S., Montebianco Abenavoli L., Oliva A., Ricci P. The role of the COVID-19 pandemic as a risk factor for suicide: What is its impact on the public mental health state today? Psychol. Trauma: Theory Res. Pract. Policy. 2020 doi: 10.1037/tra0000616. [DOI] [PubMed] [Google Scholar]
- Aquila I., Sacco M.A., Ricci C., Gratteri S., Ricci P. Quarantine of the Covid-19 pandemic in suicide: a psychological autopsy. Med. Leg. J. 2020 doi: 10.1177/0025817220923691. p.0025817220923691. [DOI] [PubMed] [Google Scholar]
- Aro A.R., Henriksson M., Leinikki P., Lönnqvist J. Fear of AIDS and suicide in Finland: a review. AIDS Care. 1995;7:5187–5197. [PubMed] [Google Scholar]
- Barendregt J.J., Doi S.A., Lee Y.Y., Norman R.E., Vos T. Meta-analysis of prevalence. J. Epidemiol. Commun. Health. 2013;67(11):974–978. doi: 10.1136/jech-2013-203104. [DOI] [PubMed] [Google Scholar]
- Biswas T., Scott J.G., Munir K., Renzaho A.M., Rawal L.B., Baxter J., Mamun A.A. Global variation in the prevalence of suicidal ideation, anxiety and their correlates among adolescents: a population based study of 82 countries. EClinicalMedicine. 2020;24 doi: 10.1016/j.eclinm.2020.100395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodeur A., Clark A.E., Fleche S., Powdthavee N. Assessing the impact of the coronavirus lockdown on unhappiness, loneliness, and boredom using Google Trends. arXiv preprint. 2020 arXiv:2004.12129. [Google Scholar]
- Bryan C.J., Bryan A.O., Baker J.C. Associations among state‐level physical distancing measures and suicidal thoughts and behaviors among US adults during the early COVID‐19 pandemic. Suicide and Life‐Threatening Behavior. 2020;50(6):1223–1229. doi: 10.1111/sltb.12653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buschmann C., Tsokos M. Corona-associated suicide–Observations made in the autopsy room. Leg. Med. (Tokyo) 2020 doi: 10.1016/j.legalmed.2020.101723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caballero-Domínguez C.C., Jiménez-Villamizar M.P., Campo-Arias A. Suicide risk during the lockdown due to coronavirus disease (COVID-19) in Colombia. Death Stud. 2020:1–6. doi: 10.1080/07481187.2020.1784312. [DOI] [PubMed] [Google Scholar]
- Cai Q., Feng H., Huang J., Wang M., Wang Q., Lu X., Xie Y., Wang X., Liu Z., Hou B., Ouyang K. The mental health of frontline and non-frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: a case-control study. J. Affect. Disord. 2020;275:210–215. doi: 10.1016/j.jad.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calati R., Ferrari C., Brittner M., Oasi O., Olié E., Carvalho A.F., Courtet P. Suicidal thoughts and behaviors and social isolation: a narrative review of the literature. J. Affect. Disord. 2019;245:653–667. doi: 10.1016/j.jad.2018.11.022. [DOI] [PubMed] [Google Scholar]
- Czeisler M.É., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R., Weaver M.D., Robbins R., Facer-Childs E.R., Barger L.K., Czeisler C.A. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. Morbid. Mortal. Week. Rep. 2020;69(32):p.1049. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniel S.S., Goldston D.B. Hopelessness and lack of connectedness to others as risk factors for suicidal behavior across the lifespan: implications for cognitive-behavioral treatment. Cogn. Behav. Pract. 2012;19(2):288–300. [Google Scholar]
- DerSimonian R., Laird N. Meta-analysis in clinical trials. Control. Clin. Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Epstein D., Andrawis W., Lipsky A.M., Ziad H.A., Matan M. Anxiety and suicidality in a hospitalized patient with COVID-19 infection. Eur. J. Case Rep. Internal Med. 2020;7(5) doi: 10.12890/2020_001651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick K.M., Harris C., Drawve G. How bad is it? Suicidality in the middle of the COVID-19 pandemic. Suicide Life Threat. Behav. 2020;50(6):1241–1249. doi: 10.1111/sltb.12655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal K., Chauhan P., Chhikara K., Gupta P., Singh M.P. Fear of COVID 2019: first suicidal case in India! Asian J. Psychiatry. 2020;49 doi: 10.1016/j.ajp.2020.101989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths M.D., Mamun M.A. COVID-19 suicidal behavior among couples and suicide pacts: case study evidence from press reports. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.113105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz K.L., Tull M.T., Richmond J.R., Edmonds K.A., Scamaldo K.M., Rose J.P. Thwarted belongingness and perceived burdensomeness explain the associations of COVID-19 social and economic consequences to suicide risk. Suicide Life Threat. Behav. 2020;50(6):1140–1148. doi: 10.1111/sltb.12654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamm M.E., Brown P.J., Karp J.F., Lenard E., Cameron F., Dawdani A., Lavretsky H., Miller J.P., Mulsant B.H., Pham V.T., Reynolds C.F. Experiences of American older adults with pre-existing depression during the beginnings of the COVID-19 pandemic: a multicity, mixed-methods study. Am. J. Geriatr. Psychiatry. 2020;28(9):924–932. doi: 10.1016/j.jagp.2020.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao F., Tan W., Jiang L., Zhang L., Zhao X., Zou Y., Hu Y., Luo X., Jiang X., McIntyre R.S., Tran B. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou T.Y., Mao X.F., Dong W., Cai W.P., Deng G.H. Prevalence of and factors associated with mental health problems and suicidality among senior high school students in rural China during the COVID-19 outbreak. Asian J. Psychiatry. 2020;54 doi: 10.1016/j.ajp.2020.102305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Monetary Fund. 2020. World Economic Outlook: The Great Lockdown. https://www.imf.org/en/Publications/WEO/Issues/2020/04/14/weo-april-2020. (Accessed 27th January 2021).
- Iob E., Steptoe A., Fancourt D. Abuse, self-harm and suicidal ideation in the UK during the COVID-19 pandemic. Br. J. Psychiatry. 2020;217(4):543–546. doi: 10.1192/bjp.2020.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isumi A., Doi S., Yamaoka Y., Takahashi K., Fujiwara T. Do suicide rates in children and adolescents change during school closure in Japan? The acute effect of the first wave of COVID-19 pandemic on child and adolescent mental health. Child Abuse Negl. 2020;110 doi: 10.1016/j.chiabu.2020.104680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John A., Okolie C., Eyles E., Webb R.T., Schmidt L., McGuiness L.A., Olorisade B.K., Arensman E., Hawton K., Kapur N., Moran P. The impact of the COVID-19 pandemic on self-harm and suicidal behaviour: a living systematic review. F1000Research. 2020;9(1097):p.1097. doi: 10.12688/f1000research.25522.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder R.G., Lancee W.J., Balderson K.E., Bennett J.P., Borgundvaag B., Evans S., Fernandes C.M., Goldbloom D.S., Gupta M., Hunter J.J., Hall L.M. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg. Infect. Dis. 2006;12(12):p.1924. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modesti P.A., Reboldi G., Cappuccio F.P., Agyemang C., Remuzzi G., Rapi S., Perruolo E., Parati G., ESH Working Group on CV Risk in Low Resource Settings Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PLoS One. 2016;11(1) doi: 10.1371/journal.pone.0147601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore W.D., Cloonan S.A., Taylor E.C., Allbright M.C., Dailey N.S. Trends in suicidal ideation over the first three months of COVID-19 lockdowns. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H., Park K.J., Shin Y.W., Lee J.S., Chung S., Lee T., Kim M.J., Jung J., Lee J., Yum M.S., Lee B.H. Psychological Impact of Quarantine on Caregivers at a Children's Hospital for Contact with Case of COVID-19. J. Korean Med. Sci. 2020;(28):35. doi: 10.3346/jkms.2020.35.e255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh D., Goh H.P. Occupational health responses to COVID-19: what lessons can we learn from SARS? J. Occup. Health. 2020;62(1):12128. doi: 10.1002/1348-9585.12128. p.e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar A., Nayar K.R. COVID 19 and its mental health consequences. J. Mental Health. 2020;180(6):817–818. doi: 10.1080/09638237.2020.1757052. [DOI] [PubMed] [Google Scholar]
- Lathabhavan R., Griffiths M. First case of student suicide in India due to the COVID-19 education crisis: a brief report and preventive measures. Asian J. Psychiatry. 2020 doi: 10.1016/j.ajp.2020.102202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leaune E., Samuel M., Oh H., Poulet E., Brunelin J. Suicidal behaviors and ideation during emerging viral disease outbreaks before the COVID-19 pandemic: A systematic rapid review. Prev. Med. 2020 doi: 10.1016/j.ypmed.2020.106264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li D.J., Ko N.Y., Chen Y.L., Wang P.W., Chang Y.P., Yen C.F., Lu W.H. COVID-19-related factors associated with sleep disturbance and suicidal thoughts among the Taiwanese public: a Facebook survey. Int. J. Environ. Res. Public Health. 2020;17(12):p.4479. doi: 10.3390/ijerph17124479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Cao L., Li X., Jia Y., Xia H. Awareness of mental health problems in patients with coronavirus disease 19 (COVID-19): A lesson from an adult man attempting suicide. Asian J. Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak I.W.C., Chu C.M., Pan P.C., Yiu M.G.C., Chan V.L. Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatry. 2009;31(4):318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamun M.A., Ullah I. COVID-19 suicides in Pakistan, dying off not COVID-19 fear but poverty?–The forthcoming economic challenges for a developing country. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamun M.A., Chandrima R.M., Griffiths M.D. Mother and son suicide pact due to COVID-19-related online learning issues in Bangladesh: an unusual case report. Int. J. Mental Health Addict. 2020:1–4. doi: 10.1007/s11469-020-00362-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamun M.A., Bodrud-Doza M., Griffiths M.D. Hospital suicide due to non-treatment by healthcare staff fearing COVID-19 infection in Bangladesh? Asian J. Psychiatry. 2020;54 doi: 10.1016/j.ajp.2020.102295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milner A., Spittal M.J., Kapur N., Witt K., Pirkis J., Carter G. Mechanisms of brief contact interventions in clinical populations: a systematic review. BMC Psychiatry. 2016;16(1):1–10. doi: 10.1186/s12888-016-0896-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirza J., Ganguly A., Ostrovskaya A., Tusher A., Viswanathan R. Command suicidal hallucination as initial presentation of coronavirus disease 2019 (COVID-19): a case report. Psychosomatics. 2020;106 doi: 10.1016/j.psym.2020.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClelland H., Evans J.J., Nowland R., Ferguson E., O'Connor R.C. Loneliness as a predictor of suicidal ideation and behaviour: a systematic review and meta-analysis of prospective studies. J. Affect. Disord. 2020;274:880–896. doi: 10.1016/j.jad.2020.05.004. [DOI] [PubMed] [Google Scholar]
- McIntyre R.S., Lee Y. Projected increases in suicide in Canada as a consequence of COVID-19. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milner A., Page A., LaMontagne A.D. Long-term unemployment and suicide: a systematic review and meta-analysis. PLoS One. 2013;8(1):51333. doi: 10.1371/journal.pone.0051333. p.e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy E., Kapur N., Webb R., Purandare N., Hawton K., Bergen H., Waters K., Cooper J. Risk factors for repetition and suicide following self-harm in older adults: multicentre cohort study. Br. J. Psychiatry. 2012;200(5):399–404. doi: 10.1192/bjp.bp.111.094177. [DOI] [PubMed] [Google Scholar]
- Nock M.K., Borges G., Bromet E.J., Alonso J., Angermeyer M., Beautrais A., Bruffaerts R., Chiu W.T., De Girolamo G., Gluzman S., De Graaf R. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br. J. Psychiatry. 2008;192(2):98–105. doi: 10.1192/bjp.bp.107.040113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olding J., Zisman S., Olding C., Fan K. Penetrating trauma during a global pandemic: changing patterns in interpersonal violence, self-harm and domestic violence in the Covid-19 outbreak. The Surgeon. 2020 doi: 10.1016/j.surge.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PakMediNet. (2021). Medical Journals of Pakistan. Available at https://www.pakmedinet.com/journal.php. (Accessed 01 June 2021).
- Papadopoulou A., Efstathiou V., Yotsidi V., Pomini V., Michopoulos I., Markopoulou E., Gournellis R. Suicidal ideation during COVID-19 lockdown in Greece: prevalence in the community, risk and protective factors. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2021.113713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirkis J., John A., Shin S., DelPozo-Banos M., Arya V., Analuisa-Aguilar P., Appleby L., Arensman E., Bantjes J., Baran A., Bertolote J.M. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. The Lancet Psychiatry. 2021 doi: 10.1016/S2215-0366(21)00091-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Que J., Shi L., Liu J., Gong Y., Sun Y., Mi W., Lin X., Bao Y., Sun H., Shi J., Lu L. Prevalence of suicidal thoughts and behaviours among medical professionals: a meta-analysis and systematic review. Lancet North Am. Ed. 2019;394:11. p.S. [Google Scholar]
- Rahman A., Plummer V. COVID-19 related suicide among hospital nurses; case study evidence from worldwide media reports. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rana U. Elderly suicides in India: an emerging concern during COVID-19 pandemic. Int. Psychogeriatr. 2020;10(32):1–7. doi: 10.1017/S1041610220001052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rani S., Sahoo S., Parveen S., Mehra A., Subodh B.N., Grover S. Alcohol-related self-harm due to COVID-19 pandemic: might be an emerging crisis in the near future: A case report. Indian Journal of Psychiatry. 2020;62(3):p.333. doi: 10.4103/psychiatry.IndianJPsychiatry_356_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahoo S., Bharadwaj S., Parveen S., Singh A.P., Tandup C., Mehra A., Chakrabarti S., Grover S. Self-harm and COVID-19 pandemic: an emerging concern–A report of 2 cases from India. Asian J. Psychiatry. 2020 doi: 10.1016/j.ajp.2020.102104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarzer G., Chemaitelly H., Abu-Raddad L.J., Rücker G. Seriously misleading results using inverse of Freeman-Tukey double arcsine transformation in meta-analysis of single proportions. Res. Synth. Methods. 2019;10(3):476–483. doi: 10.1002/jrsm.1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smalley C.M., Malone D.A., Meldon S.W., Borden B.L., Simon E.L., Muir M.R., Fertel B.S. The impact of COVID-19 on suicidal ideation and alcohol presentations to emergency departments in a large healthcare system. Am. J. Emerg. Med. 2020;41:237. doi: 10.1016/j.ajem.2020.05.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- UNDG (United Nations Development Group)-Western and Central Africa, 2015. Socio-economic impact of Ebola virus disease in West African countries: A call for national and regional containment, recovery and prevention. Available at https://www.undp.org › Reports › ebola-west-africa. (Accessed 28 May 2021).
- Worldometer, 2021. Coronavirus Update (Live): 100,388,749 Cases And 2,152,444 Deaths From COVID-19 Virus Pandemic – Worldometer. https://www.worldometers.info/coronavirus (Accessed 26 January 2021).
- Xiaoming X., Ming A., Su H., Wo W., Jianmei C., Qi Z., Hua H., Xuemei L., Lixia W., Jun C., Lei S. The psychological status of 8817 hospital workers during COVID-19 epidemic: a cross-sectional study in Chongqing. J. Affect. Disord. 2020;276:555–561. doi: 10.1016/j.jad.2020.07.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xin M., Luo S., She R., Yu Y., Li L., Wang S., Ma L., Tao F., Zhang J., Zhao J., Li L. Negative cognitive and psychological correlates of mandatory quarantine during the initial COVID-19 outbreak in China. Am. Psychol. 2020;75(5):p.607. doi: 10.1037/amp0000692. [DOI] [PubMed] [Google Scholar]
- Yao H., Chen J.H., Xu Y.F. Patients with mental health disorders in the COVID-19 epidemic. The Lancet Psychiatry. 2020;7(4) doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang K., Shi Y., Liu H., Hashimoto K. A case report of suicide attempt caused by acute and transient psychotic disorder during the COVID-19 outbreak. Case Rep. Psychiatry. 2020;2020 doi: 10.1155/2020/4320647. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.