Abstract
Background
The Pacific Islands have some of the highest rates of suicide in the Western Pacific region. The purpose of this study was to systematically review the literature on suicidal behaviour in the Pacific Islands.
Methods
A comprehensive search of Web of Science, PubMed, PsycINFO, Cochrane, CINAHL and Embase databases was conducted for all articles published until 1st February 2021. Inclusion criteria included papers that referred to a pre-specified list of Pacific Islands. Papers referring exclusively to other countries were excluded. Other exclusion criteria included not being about suicide or suicide attempts or not presenting original research. Narrative synthesis was applied without meta-analysis. The review followed PRISMA guidelines.
Findings
A total of 36 papers were included for review. Of the Pacific Islands, Kiribati has the highest age-standardised rate of suicide mortality. Key risk groups across the Islands included youth, people of Indian ethnicity in Fiji (a prominent ethnic group in Fiji), and Indigenous peoples across other Islands. Prominent methods were self-poisoning and hanging. A distinct lack of intervention studies was found.
Interpretation
Overall, the Pacific Islands appear to have relatively high rates of suicide and suicide attempts compared to other countries in the region. This was particularly striking among youth. This review provides important directions for future suicide prevention activities, including means restriction, sensitive media/community coverage, enhanced surveillance, and the development and evaluation of interventions tailored to the needs of young people and other cultural groups.
Funding
None.
Keywords: Pacific Islands, suicide, suicide attempts, systematic literature review, suicide prevention
Panel: Research in context.
Evidence before this study
The Pacific Islands are a culturally and geographically diverse group of countries and territories in the Southern Pacific Ocean. The literature indicates that these islands are experiencing rapid social change due to external forces such as climate change and Westernisation. Unfortunately, according to global estimates, the Pacific Islands have some of the highest age-standardised suicide rates in the entire Western Pacific Region, and young people appear particularly vulnerable. There is an urgent need for a greater understanding of suicidal behaviours across the Pacific Islands to inform prevention for the region.
Added value of this study
To our knowledge, this is the first systematic literature review of suicide and suicide attempts across the Pacific Islands. The review specifically focuses on mortality rates, prevalence of suicide attempts, main methods, key risk factors/groups, and prevention/intervention activities across the region. Thereby this review provides targets for enhanced and tailored suicide prevention throughout this diverse and understudied region in terms of identifying vulnerable groups and prominent methods relevant to the Pacific Islands.
Implications of all the available evidence
Findings confirm the high burden of suicide and suicide attempts across the Pacific Islands, particularly for young people, people of Indian ethnicity in Fiji (who comprise a key ethnic group there), and Indigenous peoples. There was a lack of intervention studies or evaluations of prevention programs. Nevertheless, findings are in line with public health recommendations which can be tailored to the context of the Pacific Islands. For instance, access to common means such as pesticide use in rural areas should be restricted. Pacific Island countries should be supported in establishing and maintaining regional surveillance systems and implementing and evaluating evidence-based and culturally appropriate suicide prevention strategies.
Alt-text: Unlabelled box
1. Introduction
The Pacific Islands include the regional areas of Melanesia (Fiji, New Caledonia, Papua New Guinea, Solomon Islands, and Vanuatu), Micronesia (Federated States of Micronesia, Guam, Kiribati, Marshall Islands, Nauru, Northern Marianas Islands, Palau), and Polynesia (American Samoa, Cook Islands, French Polynesia, Hawaiian Islands, Niue, Pitcairn Islands, Samoa, Tokelau, Tonga, Tuvalu, Wallis and Futuna) [1]. While many Islands are independent countries, some remain states or territories of countries like France (French Polynesia and New Caledonia), the United Kingdom (Pitcairn Islands), or the United States of America (American Samoa, Guam, Hawaii, Northern Marianas), which hints at the more recent history and influence of Western colonisation and global wars that have spread across the vast Pacific Ocean.
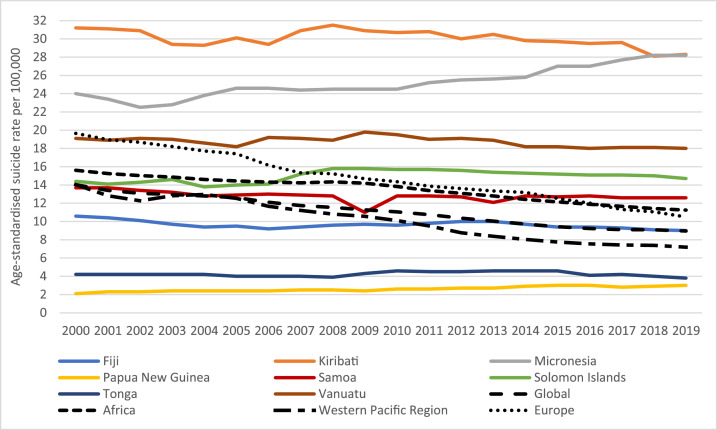
Despite their tranquil beauty and reputation as popular holiday destinations for foreign tourists, the Pacific Islands are experiencing complex and rapid societal change, including loss of culture and spiritual connectedness due to the impacts of climate change [2] and Westernisation. [3], [4], [5], [6], [7] These external factors have been linked to helplessness, poor wellbeing, and suicidal behaviours, particularly for Indigenous peoples and those living in the Pacific Islands. [8], [9], [10], [11], [12], [13] Indeed, the Pacific Islands have some of the highest rates of suicide in the broader Western Pacific Region (WPR). [14] The World Health Organization's (WHO) recent global health estimates for 2000-2019 include age-standardised suicide rates for eight Pacific Islands, with Kiribati, Federated States of Micronesia and Vanuatu having the highest rates, and several exceeding the current global age-standardised rate of 9.0 per 100,000 (Figure 1 provides some comparisons). [15,16]
Figure 1.
Age-standardised rates of suicide (per 100,000) across the Pacific Islands based on WHO Global Health Estimates (2000-2019) [15], with the Global, European, African and Western Pacific Regional rates included for comparison. Data source: World Health Organization, Global Health Estimates.
However, within the WPR, there are differences in age patterns, whereby suicides in the Pacific Islands peak in younger years. [17] These youth suicides appear to be driving the higher rates. For example, a recent study provided crude suicide rates per 100,000 people for youth aged 10-19 years, which were only 4.4 in the Republic of Korea but 16 in Kiribati, 10.8 in the Federated States of Micronesia, 5.2 in Papua New Guinea, 4.7 in the Solomon Islands, and 4.4 in Vanuatu. [14] Furthermore, the prevalence of self-reported youth suicidal ideation and suicide attempts within the previous year is also highest globally in the Pacific Islands. [18], [19], [20] Given suicide attempts are important risk factors for suicide, [21] and the years of life lost due to youth suicide across the islands, an important need exists for enhanced suicide and suicide attempt prevention throughout the region. [22] However, as typically smaller countries in terms of size, population, and economies, these countries face particular challenges. For instance, the need to overcome remoteness and limited access to culturally safe health care and resources, societal or cultural barriers such as suicide-related stigma, [21] and a lack of integrated suicide prevention strategies including accurate and responsive surveillance systems to address suicidal behaviours effectively. [17, [21], [22], [23], [24], [25]
This study aims to be the first to systematically review the literature on suicide and suicide attempts in the Pacific Islands to determine mortality, prevalence, main methods, and risk groups/factors to inform future suicide prevention activities in the WPR.
2. Methods
This review was reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Guidelines [26] (PRISMA checklist supplied in Supplementary Table 1). There was no funding agency to have any role in study design, data collection, data analysis, data interpretation, or report writing. The review protocol was not prospectively registered.
2.1. Inclusion and exclusion criteria
Given the geographical vastness and cultural diversity of the Pacific Islands as a region, a decision was made based upon the Pacific Industrial Classification [1] to include only those studies which referred to American Samoa, Cook Islands, Fiji, French Polynesia, Guam, Kiribati, Marshall Islands, (Federated States of) Micronesia, Nauru, New Caledonia, Niue, Northern Marianas, Palau, Papua New Guinea, Pitcairn Islands, Samoa, Solomon Islands, Tokelau, Tonga, Tuvalu, Vanuatu, and/or Wallis and Futuna (for further demographic information on each see Supplementary Table 2). Papers referring exclusively to other Western Pacific countries such as Australia, New Zealand, Japan or China were excluded, as were papers referring exclusively to countries outside the WPR, including the Pacific islands of Hawaii (USA). Other exclusion criteria included not being about suicide or suicide attempts (e.g., suicidal ideation), or not presenting any original empirical research (e.g., personal communication).
2.2. Search strategy
A search of Web of Science, PubMed, PsycINFO, Cochrane, CINAHL and Embase databases was conducted without date restriction until 13th October 2020. A final update to the search was completed before the final extraction and synthesis of results (1st February 2021). Reference lists of included articles were also screened for any publication that met eligibility criteria. Database specific Boolean operators (AND, OR, NOT) and truncation symbols (* and “ ”) were used. There were no language restrictions during the search; however only five non English titles were identified (and subsequently excluded based upon the preceding inclusion/exclusion criteria). Search terms included were:
-
1.
(“American Samoa” OR “Cook Islands” OR Fiji OR “French Polynesia” OR Guam OR Kiribati OR “Marshall Islands” OR Micronesia OR Nauru OR “New Caledonia” OR Niue OR “Northern Marianas” OR Palau OR “Papua New Guinea” OR Pitcairn OR Samoa OR “Solomon Islands” OR Tokelau OR Tonga OR Tuvalu OR Vanuatu OR “Wallis and Futuna” OR “Pacific Islands” OR “Western Pacific”)
AND
-
2.
(suicide* OR drowning OR “self poisoning” OR overdose OR “self injury” OR “self harm” OR “self immolation”)
NOT
-
3.
(“suicide gene” OR “suicide genes” OR “suicidal gene” or “suicidal genes”)
2.3. Data extraction
Descriptive data were exported from the databases into a pre-extraction file to record author(s), title, year of publication, journal/volume/issue, and article abstract. Duplicate records were deleted. Two reviewers (SM, YWK) independently checked each title/abstract against the inclusion and exclusion criteria. This process was cross-checked by the senior reviewer (KK), with discussions to clarify any discrepancies. Ineligible articles at this stage were marked for removal. The full texts of the remaining articles were then read against the eligibility criteria. Ineligible articles were discussed for consensus and removed. Data from the selected articles were further extracted into tables to include author(s), publication year, country/countries, data collection period, study design, data sources, rates of suicide or suicide attempts, risk groups/factors, suicide or suicide attempt methods, other information, and major limitations. Extracted information was independently cross-checked by multiple co-authors (SM, YWK, SL, KK).
2.4. Quality assessment
Two reviewers (SM & KK) independently assessed the quality of included articles using a quality assessment checklist, [27] with discrepancies in scoring discussed for consensus (as applied in previous reviews [28, 29]).
2.5. Data analysis/synthesis
Suicidal behaviours have multiple and interconnected causal determinants. [30] Given the variety of studies identified in this review, the ability to conduct meta-analyses was deemed not appropriate. Such variety related to differences in the measurement and completeness of suicide and suicide attempt surveillance across the Pacific Islands, differences in risk factors explored across studies, as well as the rich diversity of the Pacific Islands themselves where information on suicidal behaviours was drawn. For example, prevalence and cultural/ethnic risk groups of Fiji (from which the majority of studies were identified) may not translate into meaningful targets for suicide prevention in other smaller or culturally different Pacific Island nations with different healthcare systems. Furthermore, a lack of randomised controlled trials or nonrandomised case control studies, as well as some overlap in samples of cross-sectional studies made meta-analysis more difficult. Instead, the Synthesis Without Meta-analysis (SWiM) [31] extension to the PRISMA guidelines and narrative synthesis guidelines for systematic reviews [32] were consulted (Supplementary Table 3). In this review, narrative synthesis was applied in order to directly address the aims of the review where meta-analysis was not applicable. Namely, to address the following questions: what is the mortality/prevalence of suicidal behaviours, the main methods used, key risk groups/factors, and any prevention/interventions across the Pacific Islands.
3. Results
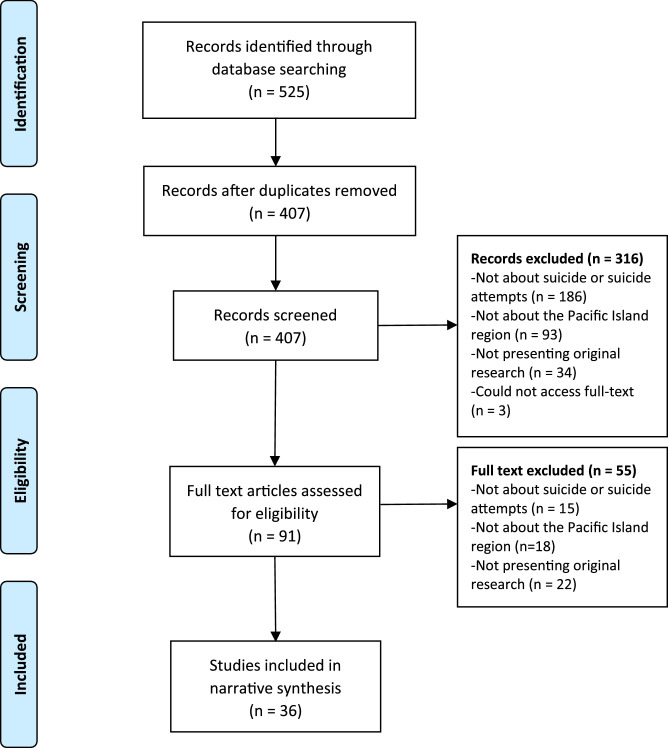
Once all final searches had been completed, a total of 525 articles were retrieved. A total of 117 duplicate titles were removed, leaving 408 articles for screening against the eligibility criteria. Following the exclusion of 316 articles based upon their title/abstract, the full text of 92 articles were read, with a final 36 papers included in the narrative synthesis (Figure 2[33]).
Figure 2.
Study selection flow-diagram based on PRISMA guidelines.
3.1. Study details
Table 1 provides an overview of study designs and data collection periods, with most being retrospective case-series (n=16) or cross-sectional prevalence studies (n=11). The remaining designs were ecological monitoring studies (n=6), case-control (n=2), and only one study [34] was a randomised controlled trial.
Table 1.
Study characteristics of included studies.
| Author(s), year | Country(ies) & Data period | Outcome | Sample/population and/or number of cases | Study design | Data collection & sources |
|---|---|---|---|---|---|
| Aghanwa, 2000 [35] | Fiji, Suva (15th January, 1999 – 14th January, 2000) | Suicide attempts (SA) | N=39 suicide attempts & N=67 other patients as controls | Case-control study | Consecutive cases of attempted suicide from the Colonial War Memorial Hospital, Suva, Fiji were evaluated within 24h of the receipt of the referrals by the consultant psychiatrist; controls - other psychiatric patients |
| Aghanwa, 2001 [36] | Fiji, Suva (January 1999 - December 2000) | SA | N=58 deliberate self-poisoning (of 68 SA) | Case series | Patients with Deliberate self-poisoning (DSP) from the Colonial War Memorial Hospital, Suva, Fiji. |
| Aghanwa, 2004 [5] | Fiji, Suva (1st January, 1999-30th June, 2002) | SA | N=128 suicide attempts | Case series | People who attempted suicide seen by the consultation-liaison psychiatric service in Colonial War Memorial Hospital in Suva, Central/Eastern of Fiji |
| Amadeo et al., 2015 [34] | French Polynesia (2008-2010) | SA | N=200 (of 515 hospital presentations): 100 in the intervention and 100 in treatment as usual | RCT | Testing brief intervention contact (BIC) in reducing NFSB. Of 515 persons admitted for presentations of NSFB to the ED of the Hospitalier de Polynésie Française |
| Amadeo et al., 2016 [23] | French Polynesia (2008-2010) | SA | N=556 hospital presentations (by 515 people) | Case series | Surveillance of admitted NFSB cases to the Emergency Department of the French Polynesia Hospital (Centre Hospitalier de Polynésie Française); 2012 Census data were used to calculate rates by specific socio-demographic groups. |
| Booth, 1999a [3] | Fiji (1982-83, 86, 89-90), Vanuatu (1990-1992), Micronesia (1960-1987), Federated States of Micronesia (1988-92), Marshall Islands (1988-1992 and 1992-1993), Tonga (1971-1982), Western Samoa (1981-83, 1988-92), American Samoa (1990-1991), Papua New Guinea (1990), Guam (1988-1992) | Suicide | Population of respective countries | Ecological study | Monitoring of published and unpublished official records obtained from health, police and vital registration authorities. Secondary sources comprise data reported in existing studies, which are re-analysed (Deoki 1987, Hezel 1987, 1989, Bowles 1985, Finau & Lasalo 1985). Age standardisation using World population (WHO 1995). |
| Booth, 1999b [55] | Western Samoa (1981, 1988-1991), Fiji (1982-83, 1989-1990) | Suicide | Population of respective countries | Ecological study | Monitoring of published (Deoki 1987, Bowles 1985) and unpublished health, coroners' and police records. |
| Booth, 2010 [6] | Guam (1971, 1974-2006) | Suicide | Population of respective country | Ecological study | Monitoring of published mortality data from Department of Public Health and Social services by cause of death for 1971, 1974-2003. |
| Bridges, 2008 [4] | The Cook Islands, Federated States of Micronesia, Fiji Islands, Marshall Islands, Nauru, Niue, Palau, Papua New Guinea, Samoa, Solomon Islands, Tonga, Tuvalu, Vanuatu (2002 or closest year) | Suicide | Population of respective countries | Ecological study | The age-standardised rates of suicide from the WHO mortality database. |
| De Leo et al., 2013 [24] | Fiji (2004-2009), Tonga (1979-2009), Vanuatu (2010), French Polynesia (1999, 2003, 2005-2007) | Suicide & SA | Suicide: N=455 (Fiji); N=120 (Tonga); N=2 (Vanuatu); N=155 (French Polynesia) SA: N=646 (Fiji); N=19 (Tonga); N=10 (Vanuatu); N=557 (French Polynesia) |
Case series | SA surveillance in Fiji (St Giles Hospital - a psychiatric hospital), French Polynesia (Taaone Hospital Tahiti), Tonga (Tongatapu Main Hospital) and Vanuatu (Vila Central Hospital) Suicide surveillance from Fiji (Central Police Department); French Polynesia (National Police Department); Guam (Office of the Chief Medical Examiner), Tonga (Police Department, Tongatapu) and Vanuatu (Ministry of Health). |
| Devries et al., 2011 [56] | Samoa (2000-2003) | SA | N=1438 (Samoa) | Cross-sectional study | Secondary analysis of a WHO multi-country prevalence study investigating women's health and domestic violence using a national sample from Samoa of women aged 15-49 years. Participants were asked about lifetime suicide attempts. |
| Goodfellow et al., 2020 [49] | New Caledonia (2014-2015) | Suicide | N=52 suicides (out of 75 identified cases) | Case series | Psychological autopsies with family members of decedents identified via the Justice Department of New Caledonia |
| Haynes, 1984 [37] | Macuata - one of Fiji's provinces (1979-1982) and all Fiji (1981-1982) | Suicide | N=79 suicides | Case series | Surveillance of all suicide verdict in Macuata province specifically from the Police Register of Unnatural Deaths (1979-1982) (main data source). Supplementary data were obtained from medical records at Labasa Hospital. Police headquarters provided data for the whole of Fiji for 1981-82 (used only for rate comparisons). |
| Henson et al., 2012 [38] | Fiji (January 2010-December 2010) | SA | N=153 counselling referrals for suicide attempts & N=5,438other counselling referrals as controls | Case-control study | Secondary analysis of archived de-identified data collected for clinical and program evaluation purposes by Pacific Counselling & Social Services of Fiji. As this data were archival, the nature of the specific interventions is not known. Data from 4 regional hospitals in Fiji. Controls - other hospitalised patients. |
| Herman et al., 2016 [46] | Fiji, Vitu Levu (12 months concluding 30th September, 2006) | Suicide & SA | N=35 suicides (of 63 fatal injuries) N=60 non-fatal self-harm (of 452 non-fatal injuries) |
Case series | Surveillance of fatal and non-fatal intentional self-injury using The Fiji Injury Surveillance in Hospitals system (established at all hospitals in Viti Levu as part of the Traffic-Related Injury in the Pacific project). Cases were identified from hospital accident and emergency registers, admission and post-mortem records. TRIP-15. |
| Kushal et al., 2021 [20] | Cook Islands (2015), Fiji (2016), French Polynesia (2015), Kiribati (2011), Niue (2010), Samoa (2011), Solomon Islands (2011), Tokelau (2014), Tuvalu (2013), Vanuatu (2011), Wallis Futuna (2015) | SA | N=350 of 366 (Cook Islands); N=1303 of 1537 (Fiji); N=1732 of 1902 (French Polynesia); N=1253 of 1340 (Kiribati); N=73 of 82 (Niue); N=1259 of 2200 (Samoa); N=799 of 925 (Solomon Islands); N=75 of 85 (Tokelau); N=598 of 679 (Tuvalu); N=798 of 852 (Vanuatu); N=604 of 718 (Wallis Futuna) All aged 12-18 years |
Cross-sectional study | Secondary analysis of the Global School-Based Health Survey (GSHS) which uses a two-stage cluster sample design of school going adolescents, self-completed questionnaire, countries that included a question ‘During the past 12 months, did you actually attempt suicide?’ were analysed. |
| Liu et al., 2018 [19] | Kiribati (2011), Niue (2010), Samoa (2011), Solomon Islands (2011), Tuvalu (2013), Vanuatu (2011) | SA | N=1555 (Kiribati); N=134 (Niue); N=2303 (Samoa); N=1293 (Solomon Islands); N=899 (Tuvalu); N=1014 (Vanuatu) Reported response rate varied from 93.7% Samoa – 100% Niue All aged 12-18 years |
Cross-sectional study | Secondary analysis of the GSHS (see above). |
| Lowe, 2019 [7] | Federated States of Micronesia (1990-1999) | Suicide | N=74 suicides | Ecological study | Monitoring suicide reports in each village or municipality based on the Micronesian Seminar to calculate the 10-year average (1990-99) suicide rates per 100,000 on municipality level. |
| Peiris-John et al., 2013 [39] | Fiji, Viti Levu (12 months commencing 1st October 2005) | Suicide & SA | N=16 suicides by poisoning N=82 non-fatal intentional self poisonings |
Case series | Surveillance of fatal and non-fatal intentional self-injury by poisoning using The Fiji Injury Surveillance in Hospitals system (established at all hospitals in Viti Levu as part of the Traffic-Related Injury in the Pacific project). Cases were identified from hospital accident and emergency registers, admission and post-mortem records. TRIP-11. |
| Peltzer & Pengpid, 2015 [58] | Kiribati, Samoa, Solomon Islands, Vanuatu (2011) | SA | N=6540 school-going adolescents “predominantly” aged 13-16 years old (summed across all Pacific Island) | Cross-sectional study | Secondary analysis of the GSHS (see above). |
| Pengpid & Peltzer, 2020 [59] | Tonga (2017) | SA | N=3333 school-going adolescents (Mean age 14 years, IQR=3) | Cross-sectional study | Secondary analysis of the GSHS (see above). |
| Pengpid & Peltzer, 2020 [60] | Kiribati (2015-2016) | SA | N=2156 adults aged 18-69 years | Cross-sectional study | Secondary analysis of 2015-2016 Kiribati STEPS survey. The survey utilised a 3-stage cluster sampling strategy and was targeted at community-based adults. |
| Pinhey & Millman, 2004 [47] | Guam (2001) | SA | N=1381 (response rate of 96.6%) | Cross-sectional study | Secondary analysis of Guam's Youth Risk Behaviour Survey, sampling frame consisted of 4 public high schools and 3 Catholic high schools in Guam where youth were asked, “During the past 12 months did you actually attempt suicide?” |
| Price & Karim, 1975 [40] | Fiji (1971-1972) | Suicide | N=90 suicides | Case series | Surveillance of death certificates and post mortem records of the Fiji Medical Statistics Department and the perusal of mental hospital case sheets. Additional data were collected by detailed survey of the circumstances of suicides in two defined localities in Fiji by interviewing next of kin. |
| Pridmore et al., 1995 [42] | Fiji (1969-79, 1980-89) | Suicide & SA | Population of respective country | Ecological study | Monitoring of annual reports of the Ministry of Health (and equivalent authorities), which is based on individual hospital reports. |
| Pridmore et al., 1996 [41] | Fiji (1st July 1985-30th June 1993) - eight years | Suicide | N=304 suicides (hanging or poisoning) | Case series | Autopsies held at two hospitals. Cases were accepted where all details of residence, race, sex and age were given and where the pathologist found that poisoning or hanging had caused death. |
| Pridmore, 1997 [52] | Solomon Islands (Jan 1989-Jul 1993) | Suicide & SA | N=13 suicides N=123 further instances of suicidal behaviours |
Case series | Surveillance from the "suicide book" maintained by the Casualty Department of Central Hospital (the date, name, sex, method of self-injury, and, in the case of ingestion, the name and amount of drugs consumed). |
| Ran et al., 2015 [48] | Guam (2009) | SA | N=207 (response rate 82.1%) | Cross-sectional study | Self-report survey of students at the University of Guam (all students were invited to participate) where young people were asked about lifetime suicide attempts |
| Ree, 1971 [43] | Macuata province in Fiji (1962-1968) | Suicide | N=73 suicides | Case series | Surveillance from police records in Macuata Province. |
| Roberts et al., 2007 [44] | Fiji, Western Viti Levu (January 2004-December 2005) | SA | N=132 suicide attempts | Case series | People referred to Family Support and Education Group after attempted suicide |
| Rubinstein, 1983 [51] | Micronesia (widely) (more specifically covered Federated State of Micronesia (Yap, Truk, Ponape), Republic of Palau and the Marshall Islands (Kwajalein and Majuro)) 1960-1980 | Suicide | A case file of “over 300” suicides (as well as “over 300 suicide attempts” although analyses did not investigate these further) | Case series | All available official reports were examined for data relevant to Micronesian suicides during the post-war period. These sources included hospital and medical records, all death certificates from each District Clerk of Courts Office, police records and statistics where compiled and pertinent church records. Supplemented with 250 psychological autopsy interviews. |
| Sakamoto et al., 2020 [54] | Commonwealth of the Northern Marianas Islands (2017) | SA | N=1943 (response rate of 64%) | Cross-sectional study | Youth Risk Behavior Survey for the CNMI. Survey used two-stage cluster sampling strategy and was for grades 9-12, where students were asked “During the past 12 months, how many times did you actually attempt suicide?” |
| Sharma et al., 2017 [57] | Kiribati, Solomon Islands, Vanuatu (2011) | SA | N=1582 (Kiribati); N=1421 (Solomon Islands); N=1119 (Vanuatu) Response rate varied from 72% (Vanuatu) to 85% (Kiribati & Solomon Islands) |
Cross-sectional study | Secondary analysis of the GSHS (see above). |
| Tavite & Tavite, 2009 [53] | Tokelau (1980-2004) | Suicide & SA | N=142 completed a cross-sectional survey (aged 15-45); N=6 suicides; N=40 suicide attempts | Case series | Surveillance of all available records on suicidal cases (1980-2004), interviews with relatives of those who died by suicide, or those who attempted suicide (1998-2004); cross-sectional study of all people in Tokelau in 2004. |
| Vignier et al., 2011 [50] | New Caledonia (2007) | SA | N=1400 youth aged 16 to 25 years (response rate 88.1%) | Cross-sectional study | A survey of young people using a stratified sample based on 2004 census data were constructed for each of the four geographic regions; the stratifying factors were sex, age group, and school enrolment status. Young people were asked “Have you ever tried to commit suicide?” |
| Wainiqolo et al., 2012 [45] | Fiji; Viti Levu (1st October 2005 – 30th September 2006) | Suicide & SA | N=78 suicides; N=144 suicide attempts | Case series | Surveillance of all injury-related deaths and primary admissions to hospitals using the Fiji Injury Surveillance in Hospital database (used an adapted version of the WHO Injury Surveillance Guideline). TRIP-10 |
Note: TAU = treatment as usual; BIC = brief intervention contact; NFSB = non-fatal suicidal behaviour; SA = suicide attempt; WHO = World Health Organization; CNMI = Commonwealth of Northern Marianas Islands; GSHS = Global School Based Health Survey; TRIP = Traffic-Related Injury in the Pacific Project.
The included studies were further separated into those discussing suicide (n=12; Table 2) and those that discussed self-harm/suicide attempts (n=17; Table 3). An additional seven articles discussed both fatal and non-fatal self-harm (n=7), and relevant information was spread across both tables. In terms of coverage of the Pacific Islands, most articles focused on a single country, of which most (n=13) were about Fiji. [5,[35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46] The remaining studies identified in the review covered Guam (n=3), [6,47,48] New Caledonia (n=2), [49,50] (Federated States of) Micronesia (n=2), [7,51] French Polynesia (n=2), [23,34] and one each on the Solomon Islands, [52] Tokelau, [53] and The Commonwealth of the Northern Marianas Islands. [54] A further four articles contained information from multiple Pacific Island countries, [3,4,24,55] and six analysed data from globally distributed surveys. [19,20,[56], [57], [58], [59] Data for these latter studies came from the Global School-Based Student Health Survey (GSHS), [19,20,[57], [58], [59] and the WHO multi-country study on women's health and domestic violence. [56] For these studies, only specific findings related to the Pacific Islands were extracted. It is noted that four of the GSHS studies analysed the prevalence of self-reported suicide attempts and shared some temporal overlap (see Table 1). [19,20,57,58] The Pitcairn Islands were not represented in any of the identified studies, although it is noted that this is the smallest of the Pacific Islands (total population of approximately 60 people [1]).
Table 2.
Important findings and information regarding suicide in the Pacific Islands.
| Author(s), year | Suicide rates | Risk groups/ risk factors | Suicide methods | Other important information | Limitations | Quality |
|---|---|---|---|---|---|---|
| Booth, 1999a [3] | Rates per 100,000: Fiji (ASR P: 19 M: 22 F: 15; CR P: 17 M: 19 F: 14), Vanuatu (CR: P: 3 M: 3 F: 3), 'Micronesia(1960-87)' (ASR T: 20 M: 36 F: 3; CR T: 18 M: 33 F: 3), Federated States of Micronesia (CR P: 31), Marshall Islands (1988-1992 CR T: 26; 1992-1993 CR T: 16 M: 29 F: 2), Tonga (CR T: 1 M: 2 F: <1), Western Samoa (ASR T: 34 M: 49 F: 18; CR T: 31 M: 41 F: 21), American Samoa (CR T: 18 M: 34 F: 0), New Caledonia (CR P:10, M: 17, F: 2), Papua New Guinea (1990: CR: <1, unreliable data), French Polynesia (1988-1992, ASR T: 9, M: 12, F: 5, CR T: 9 M: 12, F: 5), Guam (1988-1992 ASR P: 15, M: 24, F: 4, CR P:16, M:27, F: 4); Northern Marianna Islands 1990-1992 CR P: 13, M: 22, F: 3; Palau 1988-92 C P: 29. | Male youth in all countries, female youth in Indian-Fijians and Western Samoa. | The predominant method was hanging (60% and 73% in Indian-Fijians, >80% in Micronesia, 79% in French Polynesia), except for Western Samoa where paraquat (pesticide) predominates (74-82%) | For Fiji, Tonga and Western Samoa suicide attempt information were available, however, data was used only to calculate the fatality rate. | Pacific data on suicide vary in completeness and quality (see further details/reasons p 434), ASRs only for selected countries. | 13 (Medium) |
| Booth, 1999b [55] | Female youth suicide rate: 70 per 100,000 in 1981. Indian-Fijians: 60 per 100,000. For males, youth rates of 64 among Western Samoans and 57 among Indian-Fijians. | Higher in females in these two populations. Female youth account for a greater number of suicides than male youth in both populations. | Predominant method hanging (60% % 73%) for Indian-Fijians. Predominant method paraquat (pesiticide) (82% and 73%) for Western Samoans. | Crude rates reported in graph: Indian-Fijians and Western Samoans, female age pattern peaks at younger age than males. For Western Samoans, the female rate exceeds the male rate at age 20-24. For Indian-Fijians, the female suicide rate was slightly higher than the male rate at 15-24. | Relative suicide rates used for internal comparison. The sum of male and female rates is 100 and are not comparable between populations. Data from drowning were omitted due to uncertainty of intent. The data for 1989-1990 are unpublished and also omit some months are thus incomplete. Data from 1988-1991 cover only deaths in hospital (including dead on arrival) and are also incomplete. The incomplete data are only used for internal comparison. | 8 (Low) |
| Booth, 2010 [6] | Suicide rates increased rapidly in 1990s. ASR: Males - 1978-1982: 35; 1988-1992 - 75; 1998-2002 - 100; 2002-2006: 70; Females: 1978-1982: 32; 1988-1992 - 58; 1998-2002 - 100; 2002-2006: 62. | Youth - 19% of male suicides aged <20 (mode) and 59% aged <30. In females, 25% of suicides occurring in aged <20 (mode) and 54% aged <30. | NR | Several potential factors increasing suicide were hypothesised, including militarisation, loss of land, threats to loss of language and culture, migration, urbanisation, rapid economic growth, tourism and suicide contagion. | Different ICD classification used over years. Population data for rates were available for limited years. | 14 (Medium) |
| Bridges, 2008 [4] | ASRs per 100,000: Cook Islands 4.6, Federated States of Micronesia 5.0, Fiji Islands 4.1, Marshall Islands 7.4, Nauru 4.1, Niue 4.4, Palau 5.6, Papua New Guinea 12.4, Western Samoa 5.4, Solomon Islands 4.7, Tonga 4.6, Tuvalu 7.9, Vanuatu 5.1. | NR | NR | A positive correlation between suicide rates and population growth was reported. No association between suicide rates and population size or population density. | WHO data with varying quality | 11 (Low) |
| De Leo et al., 2013 [24] | NR as differing years. | Males (e.g., 19:1 in Tonga and 8:1 in Guam) and youth (e.g., a median age of 22 in Tonga, 27 in Guam). | The predominant method is hanging (over 70% in males and females, except females in Guam and Tongan - 57.1% and 50%) | Several other areas could contribute data only for either fatal or NFSB, rather than both. | Very small numbers for Vanuatu (n=2), likely to underreport. | 16 (Medium) |
| Goodfellow et al., 2020 [49] | NA | Indigenous Kanak were over-represented in suicide deaths, suicide ratio by gender was 1.7 men to women, 62% had at least one mental disorder (major depression and alcohol/other substance use disorders being the most common), and serious relationship difficulties were common preceding death. | NR | Recall bias, emotional and interviewer bias. | Small sample | 18 (High) |
| Haynes, 1984 [37] | Annual rates per 100,000 in Fiji (total): Indian-Fijian males - n = 78, rate = 45.2; Fijian males - n = 14, rate= 9.2; Indian-Fijian females - n = 57, rate = 33.1; Fijian females n = 14, rate = 9.3. In Macuata, 1979-1982: Indian-Fijian males n = 29, rate = 61.0; Fijian males n = 2, rate= 11.6; Indian-Fijian females n = 34, 71.9; Fijian females - 0. | Indian-Fijian women under 30 (vs Indian-Fijian men under 30); Indian-Fijian men over 30 (vs women over 30). Higher rates among Indian-Fijians in Macuata vs. Indian-Fijians in Fiji. Indian-Fijians account for 90% of all suicides - 100% of females and 91% of males. Suicides rarely recorded in Bua and Cakaudrove populations. 69% of cases in Fiji aged < 30. Hindus (vs. Muslims): ratios of 14:1 in males and 8:1 in females. | Predominant method hanging - 60% of male cases and 77% of female cases. | NA | Small area analysis mainly, police data | 16 (High) |
| Herman et al., 2016 [46] | Fatal self-harm was present in 35 cases of hospitalisation (55.6% of all cases in the year), of which 6 were Indigenous Fijians, and 26 were Indian-Fijians | Men and women of Indian ethnicity | NR | NA | Unclear what methods were used for self-harm, specifically | 15 (Medium) |
| Lowe, 2019 [7] | The Ten-year average suicide rate was 18.8 per 100,000 - 32.8 in urban municipalities, 23.2 in near urban, and 13.2 in outer atolls (these differences were significant). | Urbanisation, disintegration, and incongruity between modern economic resources and achieved modern material lifestyle were linked to increase the risk of suicide in the community level. | NR | NA | Ecological study - subject to ecological fallacy. Overall models only accounted for a small amount of the variance, and models did not include other important variables (e.g., mental health). | 17 (High) |
| Peiris-John et al., 2013 [39] | The annual crude rate of fatal intentional poisonings was 2.3 per 100,000. | Indian ethnicity and those aged 15-29. | Out of 1/3 of documented substances, 41.2% were chemicals (e.g., kerosene), 35.3% drugs and 23.5% pesticides | Out of all poisoning fatalities, 76% were of Indian ethnicity, 53% were male, and 70% were aged 15-29 years old | Only poisoning cases over one year, substances involved recorded only in 1/3 of cases, of the 17 fatalities, one was deemed unintentional, and rates should be interpreted accordingly. | 17 (High) |
| Price & Karim, 1975 [40] | An annual crude rate of 8.4 per 100,000 (M: 8.7 F: 8.2) (90 suicides over the study period). | Of the 90 cases reported, 82 (91.1%) occurred in Indian-Fijians. Indian-Fijian females were slightly higher than Indian-Fijian males. Rural residence and Hinduism faith. | Predominant method hanging (100% in females, 91.6% in males) | Only 7.8% (n=7) received psychiatric treatment, with the next of kin information revealing that 40% had a diagnosed or suspected mental illness. Suicide rates for the Indian-Fijian subpopulation are higher for females in younger age groups (15-44) and males in older age groups (45 and over). | The crude rate for two years. It is likely an underestimate as it includes only those in which the ascertainment of suicide seemed to be in no doubt (e.g., excluding drowning). | 9 (Low) |
| Pridmore, 1997 [52] | An annual crude suicide rate of 3.9 per 100,000 in a population of 75,000 (13 suicides over the study period). | Females accounted for 62% of suicides. | Chloroquine (n=9), M: 33%, F: 67% Hanging (n=4), M: 50%, F: 50% |
The Central Hospital serves the 75,000 people living in Honiara and to the east and west, along the northern coast. | Possibility of missing cases (those not hospitalised), particularly in more isolated areas; crude rate. | 12 (Low) |
| Pridmore et al., 1996 [41] | An annual crude rate 8.87 per 100,000 (304 autopsies over the study period). | Indian Fijians - 19.5 per 100,000 compared to 1.53 per 100,000 for Indigenous Fijians. The Difference rate of autopsies between regions and sexes not significant. | The predominant method was hanging (6.09 autopsies per 100,000), followed by poisoning (2.78 per 100,000). | NA | Coverage of 2 out of 3 pathology departments in Fiji (exact population of their coverage not provided). Crude rates only. It did not include burning, drowning and motor vehicle accidents. The Eastern Division is the most traditional; it has a small population (46 652) and no pathology department and cannot be examined separately. | 12 (Low) |
| Pridmore et al., 1995 [42] | An annual crude rate 1.5 (1.3- 1.7); the suicide rate rose from 0.2 (0.1-0.4) in 1969-1979 to 2.6 (2.2-2.9) in 1980-1989. The two epoch ratio (%) was 1100 (630-1800): a 1000% increase, which was statistically significant. | Indian Fijians (> 6 times the rate of Indigenous Fijians); females (1.7 times the rate of males). | NA | Subgroup data by ethnicity and sex provided for violence by self (AKA suicide and self-inflicted injury - includes fatal and non-fatal). | Crude rate - no data by age groups. Authors assumed that sex distribution in the population was 50:50. | 12 (Low) |
| Ree, 1971 [43] | An annual crude rate 25.8 per 100,000 (73 recorded suicides over the study period), the majority were hanging (70, 95.9%); two shootings and one drowning. The Indian-Fijian suicide rate was 33.4, and the Fijian suicide rate was 5.7. | Indian-Fijians (vs Fijians), and rates higher overall in Indian-Fijian females than males, particularly in young Indian-Fijian females. | The predominant method was hanging (70 of 73, 95.9%). | No deaths in the urban area of Macuata. | Crude rate over eight years. | 9 (Low) |
| Rubinstein, 1983 [51] | Suicide rates were calculated in 4 year sequences (the population figure from the midpoint of the sequence was used). Annual suicide rates per 100,000 for males had 8-fold rise: 1960-63 - 6.4 (n=9); 1964-1967 - 10.25 (n=16); 1968-1971 - 22.2 (n=39); 1972-1975 - 42.4 (n=84); 1976-1979 - 49.5 (n=110); for females: 1960-63 - 0; 1964-1967 - 1.2 (n=2); 1968-1971 - 1.2 (n=2); 1972-1975 - 2.0 (n=4); 1976-1979 - 4.5 (n=10). | Adolescent males aged 15-24 years old (altogether accounting for >50%). Overall, male: female ratio is 16:1. | NA | Independence after the study: the Republic of Palau in 1981; The Federated States of Micronesia in 1986; the Marshall Islands formal in 1990. Includes extra information from about 250 semi-structured interviews modelled on the ‘psychological autopsy’ protocol conducted with friends and relatives of suicide victims throughout Micronesia. Indication to contagion. | Annual rates, over 20 years, age-specific rates over five years. Likely to have severe recall bias as going back over 20 years with psychological autopsy. | 16 (Medium) |
| Tavite & Tavite, 2009 [53] | Six suicides in a small population of 1,500 from 1980-2004 (as per official records). | Youths (14-25 years old), accounted for 83% of fatalities. No gender difference (1:1). Most (67%) fatal cases occurred in Fakaofo and none in Nukunonu. | The predominant method was hanging (83%). | NA | Very little information available from hospital records and only accounted for suicidal cases that needed medical attention. Members of the public were aware of several other cases that were not recorded. | 12 (Low) |
| Wainiqolo et al., 2012 [45] | An annual crude rate 12.0 per 100,000 (95% CI = 9.3-14.6) (78 cases over the study period, 32% of all admissions). | The indian-Fijians self-inflicted injury death rate was almost ten times higher than Indigenous Fijians. | NR | The study does focus more widely on injuries, not specific to suicidal behaviour. | The crude rate for one year based on small numbers. | 15 (Medium) |
Note: ASR = age standardised rate; CR = crude rate; NA = not applicable; NR = not reported; WHO = World Health Organization; 95%CI = 95% confidence interval; F = female; M = male
Table 3.
Important findings and information regarding suicide attempts and non-fatal suicidal behaviour in the Pacific Islands
| Author(s), year | NFSB rates and/or prevalence | Risk groups/ risk factors | NFSB methods | Other important information | Limitations | Quality |
|---|---|---|---|---|---|---|
| Aghanwa, 2000 [35] | An annual suicide attempt rate 34.8 per 100,000 in 1999 (39 SA cases over the study period). | Adolescent and young adults, mostly students, not being married. | The predominant method was medical drug overdose (46.2%). | There were significant differences by marital status (suicide attempters were most frequently never married). There were significant differences by employment status (most suicide attempters were students, while most of the other patients were unemployed persons). | Over one year, a small number of consecutive patients, control/comparison group was "other psychiatric patients." | 13 (Medium) |
| Aghanwa, 2001 [36] | An annual rate of deliberate self-poisoning (DSP) 25.9 per 100,000 (68 suicide attempts; the subjects of the specific study were 58 DSP cases over the study period). | NR | Drug overdose (n=31), poison-ingestion (n=27). | Younger age, female gender, higher rate of psychopathology and low rate of recent alcohol abuse are associated more with drug overdose than poison ingestion in suicidal attempts. | Consecutive patients with DSP and small numbers, no control/comparison group. | 15 (Medium) |
| Aghanwa, 2004 [5] | NR | NR | Although males used violent methods such as hanging and wounding, more females used poisoning methods, the difference in methods was not significant. | The mean age of female (M=22.99) suicide attempters was significantly lower than that of their male counterparts (M=25.15). Alcohol misuse was significantly higher in males (42.5%) than females (10.2%). The motive for the act being a ‘desire to die’ was significantly higher in males (90%) than females (54.6%). |
Did not report prevalence or rates, no control/comparison group. In total 134 patients, six were excluded due to leaving the hospital before psychiatric intervention or dying as a result of complications arising from the index attempts. | 16 (Medium) |
| Amadeo et al., 2015 [34] | n = 21, 21% in TAU, n = 24, 26.7% in BIC. | NR | NR | There was no statistical difference in the frequency of suicidal behaviour (suicides or repeated NFSB). | The limited sample size and timeframe of the investigation made it difficult to obtain a statistically detectable difference in suicidal behaviours. Due to limited funding, only 200 people participated. | 14 (Medium) |
| Amadeo et al., 2016 [23] | The mean rate of non-fatal suicidal behaviour (NFSB) presenting at ED is 79.4 per 100,000 in 2008-2010. | Females (2.13:1), those aged 25-34 years, followed by 15-24 years (however, the prevalence of NFSB by age groups was highest for 15-24, followed by 25-34); divorced/separated; single; unemployed (highest rates). | The predominant method was drug intoxication (X60-X64, 63.8%). | The most frequent precipitating factor to the episode was relationship problems (68.6%). A more correct estimate of the annual number of NFSB for all French Polynesia would be a crude rate of 98 per 100,000. | Records suicide method (first method up to three methods) and triggers/events related to episode. Some cases were not monitored due to the temporary unavailability of staff. No control group and population census data were available only for a limited number of variables. | 18 (High) |
| De Leo et al., 2013 [24] | NR as differing years. | Youth (median age of NFSB <28 in all 4 PI countries); females (gender ratios of 0.7 in Fiji and 0.5 in French Polynesia). | Most frequent method of NFSB - Fiji: chemicals/poisons M: 71.4% F: 58.4%; Tonga: hanging M: 100% F: 50% (only 19 persons); Vanuatu: analgesics M: 80% F: 40% (only 10 persons); French Polynesia: psychotropic drugs M:31.7%, F:38.6%. | Only the first presentation to the healthcare facility was included. The description was specific to persons, not events. | Low numbers for Tonga (19) and Vanuatu (10); likely to be underestimated also in Fiji as information from a psychiatric hospital. | 16 (Medium) |
| Devries et al., 2011 [56] | 3.3% of the Samoan national sample of women (n=1,640; aged 15-49 years) reported ever attempting suicide. | Childhood sexual abuse, probable mental illness, non-partner physical violence, non-partner sexual violence, intimate partner violence. | NR | A survey was completed interview-style, and authors acknowledged that country or site-specific (vs global) models might have allowed for a more nuanced understanding of culturally specific risk/protective factors. | Cross-sectional, question about suicide attempts was asked from those who reported lifetime suicidal ideation. | 17 (High) |
| Henson et al., 2012 [38] | 153 (2.7%) out of 5581 cases were referred for a suicide attempt. | Indo-Fijian, male, younger age, single or de facto, and secondary or tertiary education (compared to other hospitalised patients). | The most common method of attempted suicide was intentional self-poisoning (78.4%). An additional 10.5% of the total group attempted suicide by hanging, strangulation and suffocation. |
NA | The comparison/control group was limited to other hospitalised patients who were referred for services. | 17 (High) |
| Herman et al., 2016 [46] | Non-fatal self-harm was present in 60 hospitalisations (13.3% for the year), of which 13 (4.4%) were Indigenous Fijians, and 45 (28.1%) were Indian-Fijians. | Men and women of Indian ethnicity. | NR | The majority of non-fatal injuries were from poisoning in Fijians of Indian ethnicity (however not clear whether these were intentional self-poisoning). | Case series with one year of data. | 15 (Medium) |
| Kushal et al., 2021 [20] | SA prevalence split by gender for each Pacific Island. The highest for boys was Samoa at 58.9%, and the lowest was French Polynesia at 5.3%. The highest for girls was Samoa at 47.9%, and the lowest was Niue at 6.7%. For most Islands, the prevalence of SA between boys and girls was reasonably equivocal however, there was some country-level variation. | NA; further analyses were reported in aggregate. | NR | Analyses restricted to adolescents aged 12-15 years. | Cross-sectional, reliance on self-report, could not control for important variables such as previous SA, depression etc. | 18 (High) |
| Liu et al., 2018 [19] | Prevalence of SA in Islands combined: 31.2% for boys, 26.8% for girls, and 28.6% total (the difference between genders was significant, and the total prevalence was highest for this region compared to other global regions). The prevalence of SA for each Island was only provided for Samoa 61.2%, the Solomon Islands 33.6%, and Kiribati 31.5%, which incidentally were the top three highest out of all 40 countries reported on this study. | NR; further analyses were for combined sample rather than Pacific Islands specifically however, food insecurity, bullying and loneliness were risk factors for the total sample. | NR | Total sample size n=146460 (GSHS) and n=8820 Chinese young adolescents survey; aged 12 - 18 years. | Reliance on self-reported SA, differing years of data collection compared, the GSHS only targets adolescents in school which may be low in LMICs. | 18 (High) |
| Peiris-John et al., 2013 [39] | The annual crude rate of non-fatal intentional poisoning hospitalisation was 12.9 per 100,000. | Indians, females and those aged 15-29. | Out of 1/3 of documented substances, 41.2% were chemicals, 35.3% drugs and 23.5% pesticides. | Out of all poisoning hospitalisations, the proportion of intentional poisoning was higher in Fijian Indians than Fijians (66.4% vs 23.4%). | Only poisoning cases over one year, substances involved recorded only in 1/3 of cases. | 17 (High) |
| Peltzer & Pengpid, 2015 [58] | Prevalence of SA in last 12 months: Kiribati - 31.5%; Samoa - 62%; Solomon Islands - 35%, Vanuatu - 23.5% in total sample (overall % in 34.9%, N = 6540). | Preadolescent and adolescent (<12 years vs non-initiators) initiation of cigarette smoking. Initiation of alcohol and drug use at ages <12 and ≥12 were both associated with suicide attempts. Substance use initiation <12 years for two or more substances. Association between adolescent alcohol initiation and suicide attempts in girls but not in boys. | NR | NA | Cross-sectional, self-report. | 18 (High) |
| Pengpid & Peltzer, 2020 [59] | SA in previous 12-months 16.5% at least once, 7.6% twice or more. | SA was associated with several factors, including female sex, loneliness, frequently bullied, not having close friends, frequent fights, frequent school truancy, amphetamine use. For girls specifically, there was the addition of anxiety. | NR | NA | Cross-sectional, self-report. | 14 (Medium) |
| Pengpid & Peltzer, 2020 [60] | 5.1 % (n= 101) reported a lifetime history of SA. | In adjusted analyses, a lifetime history of SA was associated with psychological distress, cohabiting, and physical problems (e.g., heart attack, stroke). In unadjusted analyses, alcohol problems (family and self), a family member having attempted suicide, and sedentary behaviour was also associated. | The main methods of SA were hanging (67%) and overdose of medication (11%). | Lifetime suicide attempt was analysed separately whereas suicide attempt in the previous 12-months was grouped with suicidal ideation and planning during the last 12-months. | Cross-sectional, relatively low response rate of 55%, reliance on self-report. | 16 (Medium) |
| Pinhey & Millman, 2004 [47] | 28.2% of girls and 14.5% of boys reported suicide attempt in the past 12 months. | Same-sex orientation, especially for boys. SA was also associated with increased alcohol abuse and hopelessness. | NA | Independent variables included measures of hopelessness, relationship, physical abuse, and binge alcohol use. | All suicide attempt data reported in the survey were incomplete owing to the self-reported nature of data. A response rate of 96.6%. | 14 (Medium) |
| Pridmore, 1997 [52] | An annual suicide attempt rate 36 per 100,000 (123 cases over the study period). | Females | Majority by chloroquine ingestion, except for one case. | NA | Possibility of missing cases, particularly from more isolated areas. | 12 (Low) |
| Pridmore et al., 1995 [42] | An annual non-fatal injury by self rate 12.0 (11.4- 13.8) per 100,000 in 1969-89; the rate rose from 7.1 (6.5-7.8) to 16.4 (15.5-17.4) (increase statistically significant). | Indians and females (although the authors grouped suicide and self-inflicted injury together). | NA | Male and female violence by self increased at a parallel rate over the 20 year period. | Subgroup data by ethnicity and sex provided for violence by self in total (authors do not indicate but seem to include fatal and non-fatal). | 12 (Low) |
| Ran et al., 2015 [48] | 8.2% of students with lifetime suicide attempts (n = 17). | NR for attempts, only for ideation. | NR | Survey captured demographics, information on suicide ideation and suicide attempts. | The analysis focused more on suicide ideation rather than a suicide attempt. The response rate was 82.1%. | 16 (Medium) |
| Roberts et al., 2007 [44] | NA | Mainly females, Indians, young, single or married (those who married, mainly arranged marriage), main triggers: family, marital or relationship problems. | NA | NA | Descriptive study, with no comparison group. Did not include prevalence. | 13 (Medium) |
| Sakamoto et al., 2020 [54] | 13.6% of youth reported suicide attempt in the previous year | SA was associated with the experience of violence and substance use for both girls and boys; girls were more likely to have attempted suicide than boys. | NA | NA | Cross-sectional, self-reported data. | 18 (High) |
| Sharma et al., 2017 [57] | Prevalence of SA was 31% in Kiribati, 37% in the Solomon Islands, and 23% in Vanuatu (30.9% overall) | SA was associated with being bullied and experiencing violence, and suicide attempts increased with increased length of exposure. | NA | NA | Cross-sectional, self-reported data. | 17 (High) |
| Tavite & Tavite, 2009 [53] | 40/1500 as per official records, attempted suicide in 1980-2004 (3% of the population). As per a cross-sectional survey in 2004 - 14% reported a lifetime suicide attempt, and 63% reported having relatives who have attempted suicide. | Mainly males by the official records, but females by the survey; the main triggers were different relationship problems. | The predominant method of attempt was hanging (40%). | Increasing trend of suicide attempts between 1980-2004 as per official records. | Very little information available from hospital records, and only recorded those who needed medical attention. Members of the public were aware of several other cases that were not recorded. The cross-sectional study had a low response rate (38%). | 12 (Low) |
| Vignier et al., 2011 [50] | 12% of the total sample reported lifetime suicide attempt. | Higher self-reported SA in female youth, associated with early substance use, possibly associated with Kava use in the Kanak peoples of New Caledonia. | NA | Paper focused on kava use among youth in Kanak and other ethnic communities. | Cross-sectional, self-reported data. | 13 (Medium) |
| Wainiqolo et al., 2012 [45] | An annual self-inflicted injury rate 22.1 per 100 000 (18.5-25.7) (144 cases over the study period). | The Indian-Fijians self-inflicted injury rate was almost five times higher than Indigenous Fijians. | NR | The study does focus more widely on injuries, not specific to suicidal behaviour. | Potential misclassification of some variables was noted. | 15 (Medium) |
Note: SA = suicide attempt; NFSB = non-fatal suicidal behaviour; NA = not applicable; NR = not reported; DSP = deliberate self-poisoning; TAU = treatment as usual; BIC = brief intervention component; ED = emergency department.
3.2. Suicide mortality and prevalence of suicide attempts across the region
Papers providing mortality information for the Islands were often over ten years old (Table 2). Therefore, Figure 1 provides the most recent figures for age-standardised suicide mortality for Kiribati (highest), Federated States of Micronesia, Vanuatu, Solomon Islands, Samoa, Fiji, Tonga and Papua New Guinea. [15] Regarding suicide attempts, prevalence varied across the Islands (Table 3). Based upon the GSHS, the rates for self-reported youth suicide attempts in the previous 12-months were highest globally in Samoa, the Solomon Islands and Kiribati. [19,57] Across the Islands, the prevalence was broadly comparable across genders; however, for Islands such as Samoa, Tuvalu and Vanuatu, boys reported attempting suicide more frequently than girls, which is different to predominant trends in Western countries. [19,20]
3.3. Suicide and suicide attempt methods
Across studies, the most common methods of suicide were hanging/suffocation or poisoning (e.g., pesticides, chemicals, medications), with minimal variation by gender and age (Table 2). For suicide attempts (Table 3), this information was limited mainly to data monitoring and surveillance records at hospitals and health services. Overall, poisoning by pesticides, chemicals, or medications were again the most common methods, followed by hanging/suffocation. In one of the few studies reporting on suicide attempt methods with data from multiple countries, outcomes from the WHO/START (‘Suicide Trends in At-Risk Territories’) Study [25] upheld this pattern, with a higher prevalence of poisonings in Fiji, Vanuatu and French Polynesia, and a higher prevalence of hanging in Tonga. [24]
3.4. Risk groups and risk factors
Regarding suicide in the Pacific Islands, it was clear from the included studies that a particularly vulnerable group were young people. Young men, in particular, were overrepresented in suicides in Tonga and Guam, [24] and Micronesia. [51] For Tokelau [53], the gender ratio appeared relatively equal. In contrast, for the Solomon Islands [52] and Fiji, the gender ratio in youth was often reversed. This finding was particularly striking when examining the rates of young Fijian women of Indian heritage (compared to Indigenous Fijians), [3,37,39,40,43,45,46,55] a pattern that appears to have remained consistent since the 1970s [43] until the present day. [39,45,46] In older ages, men of Indian heritage were more likely to die by suicide in Fiji. [37] Therefore, regardless of age or gender, Fijians of Indian heritage had higher rates of suicide, particularly those living in rural areas, and where young women were experiencing family issues. [37]
In New Caledonia, Indigenous Kanak peoples were overrepresented in suicides and, based on psychological autopsies, approximately 60% were likely to have symptoms consistent with a mental health diagnosis such as depression or substance use problems before death (the authors note this is less than other more developed countries). [49] The association between mental health and suicide was less clear for other Islands. In one older study of Micronesian suicides in youth, suicide was framed by relatives as related more so to anger and a somewhat spontaneous act carried out as an appeal for support in line with local cultural views as opposed to ideas of Western/medical definitions of ‘depression’. [51] Considering and acknowledging differences in cultural perspectives in relation to suicide prevention and research is essential. For instance, stigma and shame may be a barrier to seeking help and self-disclosure, thus inhibiting accurate portrayals of suicide and subsequent prevention strategies. [24,53]
Similarly, when examining suicide attempts/self-harm, young people emerged as a key risk group. For specific countries and associated factors, self-reported repeated suicide attempts in young people in Tonga (twice or more in one year) was associated with female gender, feelings of loneliness, experiences of bullying, and substance use. [59] In Guam, young boys who self-reported same-sex attraction were more likely to report a prior suicide attempt. [47] Feelings of loneliness or alcohol abuse were associated in both genders, whereas being of White ethnicity appeared protective in young girls. [47] The use of traditional psychoactive substances such as Kava was also associated with suicidal behaviours. [50]
For adults in Kiribati, psychological distress and physical health issues were associated with the lifetime prevalence of suicide attempts. For the previous 12-months, identifying as female and younger age was also important. [60] Again, Fijians of Indian heritage, particularly young women, were more likely to present to hospitals with an episode of self-harm or suicide attempt. [5,35,36,38,39,45,46] Factors associated with suicide attempts in these Fijians included loss, financial issues, family problems, feelings of hopelessness or being ‘trapped’, or feeling a lack of purpose. [38] For young women of Indian heritage, it appeared family issues may be particularly relevant (e.g., conflict with spouse's parents [37]), while a history of substance use, such as alcohol, may be more relevant for men. [5] The predominance of suicide deaths and attempts in Indian-Fijians was also described in relation to their minority status and history of being colonised and indentured. [38] A few studies also discussed the role of abuse and maltreatment in relation to increased suicide attempts in adolescents in Guam [47] and Samoan women [56]. In French Polynesia, psychological and physical abuse was a precipitant of suicidal behaviour in both men and women in nearly a third of instances. [23]
3.5. Suicide prevention and intervention
There were limited studies meeting our inclusion criteria that evaluated interventions or prevention strategies, with only a few older studies in Fiji incidentally describing the process of admission and psychiatric assessment available in one hospital. [5,35,36] A more recent study [34] from French Polynesia used a randomised controlled trial (as part of the WHO/START study) to test a brief intervention targeted at suicide and repeated non-fatal suicidal behaviours (NFSBs). From 2008 to 2010, 200 persons who had presented to hospitals for repeated NFSBs were randomised to either treatment-as-usual (TAU) or a TAU plus brief intervention and contact (TAU+). [34] Following the study follow-up period (18-months), there were no statistical differences between either group in terms of suicides (n=2 TAU; n=0 TAU+) and self-harm instances (n=21 TAU; n=24 TAU+). However, funding limitations meant that only French Polynesia could participate, limiting the sample size. Even then, challenges with geography and varying access to hospitals/health care meant participants were restricted to the more populated Island of Tahiti. The authors described these challenges of remoteness and access as key barriers to successful awareness-raising, help-seeking, and implementation of interventions across the Pacific Islands. Yet, the telephone intervention trialled in this study may help to overcome some of these barriers. [34]
3.6. Quality assessment
Quality ratings ranged from 9 (Low) to 18 (High), with most (47%) being deemed ‘medium’ quality (Tables 2 and 3; Supplementary Table 4). Areas limiting the quality overall tended to be insufficient description or quality of data sources or sample characteristics and unclear definitions of suicide cases (or suicide attempt/self-harm). Despite the use of two independent observers and consensus discussions, the use of a published tool, and the majority of studies being classified as medium in quality it is important to note that the overall designs of studies (e.g., case series, ecological studies) represent some of the lower tiers of evidence [61] and there was a distinct lack of higher quality designs (e.g., randomised controlled trials). Results of the narrative synthesis should be interpreted in light of these considerations.
4. Discussion
This systematic review synthesised literature on suicide and suicide attempts across the Pacific Islands. The review identified 36 papers per inclusion/exclusion criteria. Across included studies, suicide rates varied across the islands. However, the majority of these studies were relatively old and limited in their data coverage. However, based on recent WHO estimates, Kiribati has the highest age-standardised rates of suicide across the entire WPR (including other lower middle income countries). [16] Furthermore, Samoa, Solomon Islands and Kiribati had the highest prevalence of self-reported suicide attempts in young people. [19]
A further and important objective of the current review was to characterise key methods, risk groups, and interventions within the literature to inform future suicide prevention in the region. Overall, the most common methods for both suicide and suicide attempts were self-poisoning and suffocation/hanging. Despite minor variations with countries in the broader WPR, [17,24] these findings are broadly consistent with other large-scale studies on suicide methods across Europe [62] and among young people globally. [63] The higher prevalence of self-poisoning in suicides and suicide attempts in the Pacific Islands has been linked to access. Specifically, limited access to other means such as firearms may influence higher rates of hanging, and easy access to lethal pesticides in rural areas of the islands or prescription medications may influence the selection of these methods. [24,38] Therefore, based upon these findings, an important direction for future suicide prevention strategies across the islands will be restricting access to lethal pesticides/chemicals and appropriate media/community reporting of such incidences to avoid sensationalising suicidal behaviours and inadvertently influencing the use of certain means. [17,24,30,38] Given the small geography and population, such practices may also prevent any clustering of suicidal behaviours. [6] A further challenge will be ensuring that people living in rural/remote areas have timely access to hospitals and healthcare that can treat the outcomes of non-fatal poisonings with hazardous substances.
Given their higher rates and prevalence of suicidal behaviours, young people are a vulnerable group across the Islands. Early studies attributed this to the role of social change, whereby as the Pacific Islands rapidly became more urbanised and Westernised, there may have been a corresponding rise in social disintegration. This disintegration may have forced young people to navigate the complex divide between traditional roles and social structures. [6,7] While other countries have higher suicide rates in older ages, the current findings are comparable with Indigenous peoples worldwide. [64] There were no differences in methods for young people, and findings are consistent with previous work investigating the global trends in methods of suicide in young people. [63] Another key risk group were minority groups such as Indigenous Kanak peoples in New Caledonia [49] and Fijians of Indian ethnicity. [3,35,37,39,41,42,44,45,55,65] Therefore, future suicide prevention strategies should focus on interventions and awareness campaigns that are sensitive to the needs and cultural preferences of youth and minority cultural groups. [34,49,53] For example, the gender roles and expectations placed upon young women in Indian-Fijian households, [5,37] the unique challenges of young people, [5,7,19] and the cultural preferences of Indigenous peoples. [66] For young people, these strategies could include further means restriction, awareness and skills training, and gatekeeper training programs with schools. [14] Interestingly, gender associations with suicidal behaviours were not as clear as in other Western Pacific countries such as Australia or New Zealand whereby there is a clear preponderance of suicide in men and suicide attempts in women. [24] Instead, there were often no differences for either gender or the pattern was reversed in some islands such as Vanuatu or when examining specific sub-groups such as Indian-Fijians. [24] This was also true for suicide attempts, whereby in Islands such as Tonga or Vanuatu, young men were just as likely to attempt suicide as young women. [24] These differences highlight the importance of further surveillance throughout the Pacific Islands that builds upon the earlier work of the WHO/START study. [17,[23], [24], [25],49] The association between mental health conditions and suicidal behaviours did not appear to be a focus of many articles. Nevertheless, there was some indication that aspects of mental health such as depression [49,54] and substance use [5,49,54,57,58] may be relevant. It is important that the various unique health systems across Pacific Island countries can adequately address mental health or psychiatric conditions and that help-seeking is encouraged across the lifespan and different cultural or ethnic groups. However, those who have attempted suicide or engaged in non-fatal self-harm should be identified and assertively followed up in the community as recommended by the WHO [67] and trialled in French Polynesia. [34] However, we acknowledge certain geographical and financial constraints may serve as barriers to establishing wide reaching mental health facilities across smaller or less populated Islands.
Despite the earliest included paper in this review being nearly 50 years old, [43] we did not identify many papers meeting our inclusion criteria that focused on describing or evaluating suicide prevention interventions/strategies. Some studies described the process and challenges of psychiatric evaluation in certain areas of Fiji, [5,35,36] others presented information on injury surveillance systems in Fiji which were not focused on suicidal behaviours but could identify them, [39,45,46] and only one presented the outcomes of an RCT in Tahiti, French Polynesia as part of the WHO/START study. [34] However, a recent review of suicide prevention activities in the broader WPR does provide a more detailed description of suicide prevention in French Polynesia whereby implementing the WHO/START study was crucial in supporting suicide and self-harm surveillance infrastructure, as well as further awareness-raising campaigns and the creation of crisis helplines. [22] Furthermore, there are more recent examples in the literature of developing online, mobile screening tools to support identifying suicidal behaviours and depression by health professionals in Fiji, which may prove promising for suicide prevention across the Pacific Islands in the future. [68] However, overall, a crucial finding of this review was that there was limited research and evidence for suicide prevention interventions across the Pacific Islands (despite high rates of suicide and suicide attempts). This is likely due in part to the difficulties in establishing and maintaining adequate surveillance systems of suicide and suicide attempts providing direction for suicide prevention activities, as well as limited research infrastructure across the countires. Nevertheless, recent WHO guidelines describe public health initiatives for suicide prevention that can be applied and tailored to each of the Pacific Islands in line with findings on key risk factors/groups identified in our review, such as the restriction of access to common means, sensitive media coverage, and supporting young people. [67]
4.1. Methodological considerations
While most studies were case series or cross-sectional, these studies provide crucial information as to mortality, prevalence and potential risk groups/factors key to informing prevention strategies. [21] Over time, the timeliness, comprehensiveness and completeness of surveillance records may be improving. For example, early studies investigating suicide across the Pacific Islands [3,55] were limited by the ‘incompleteness’ of data records. More recently, developing and using prospective injury surveillance systems in hospitals [39,45,46] has enabled more complete analyses of fatal and importantly non-fatal intentional self-harm. However, databases were still restricted to major trauma hospitals on the largest island in Fiji. Furthermore, relying on information from hospitals and health services misses those who did not seek/receive medical help for their suicide attempt.
The studies relying on global health survey data provide important and comparable information as to the prevalence of self-reported suicide attempts in representative samples of young people across several Pacific Islands. [19,20,[57], [58], [59] However, there was substantial overlap in samples across the studies (albeit analysing different age ranges and research questions). The identified studies in this review suggest that these surveys are irregular. Nevertheless, these surveys allow cross-country comparisons and may identify people who may have attempted suicide or engaged in self-harm without seeking help and are thus missed from hospital-based registries. There is a need for periodical completions for up-to-date figures and more comprehensive monitoring over time. It is recommended that countries continue with implementing the GSHS for young people and introduce the optional mental health/suicide module of the WHO STEPS Surveillance Survey for adults. [69]
Combined, these considerations further serve to highlight some of the complexities of researching suicidal behaviours, not least of which includes the consistent measurement and surveillance of such behaviours around the world. Notably, however, the eligible studies based on the WHO/START study [23,24,34,49] demonstrate the capacity and feasibility of developing and maintaining a sentinel suicide and self-harm surveillance system throughout the region. Maintaining or extending this should be the focus of future work.
4.2. Limitations and future directions
The review used widely accepted guidelines to ensure adequate reporting of procedures and findings. Nevertheless, there exist some challenges that limit the current findings. First, most studies were case-series surveillance, data monitoring, or cross-sectional surveys instead of other more rigorous methodologies that would better facilitate meta-analyses. Second, the field of suicide prevention research and practice is constrained by the use of inconsistent terminology. [70] This was evident across the papers, particularly those related to suicide attempts that used other terminology like non-fatal suicidal behaviours or self-harm. While every effort was made to include only papers referring to suicide attempts (i.e., not non-suicidal self-injury/harm), given the difficulties in determining intention, some papers may have included instances of non-suicidal self-harm. It is recommended that future research follow expert consensus in the use of terminology for suicide and self-harm. [70] Future research should support the Pacific Islands to enhance or reinstate suicide and self-harm sentinel surveillance systems across the region, and develop and evaluate suicide prevention interventions for key risk groups. Given the impact of climate change on the wellbeing of those living in the Pacific Islands [2] and links made between climate change and suicidal behaviours, [8], [9], [10], [11], [12], [13] future research would also benefit from investigating this as a potential risk factor in relation to suicidal behaviour across the Pacific Islands, particularly for young people. Results of the narrative synthesis are also constrained by the varied quality of included articles. Furthermore, there was a lack of suitable quality assessment tool for ecological and case-series designs, and also for appraising the quality of identified articles from a tailored and culturally sensitive perspective (e.g., the new Aboriginal and Torres Strait Islander quality appraisal tool [71]) that was responsive to the diversity of the Pacific Islands.
4.3. Conclusion
Overall, the Pacific Islands appear to have relatively high rates of suicide and suicide attempts compared to other countries. By identifying common methods like self-poisoning with pesticides and key risk groups such as young people, this review provides important directions for future suicidal behaviour prevention activities across the Islands. These include restricting access to means, sensitive media/community coverage, enhanced surveillance across the Islands, and the development and evaluation of interventions tailored to the needs and preferences of young people and other cultural groups.
Contributors
SM: Investigation, formal analysis, Data curation, visualisation, writing – original draft, writing – review & editing; DDL: Conceptualisation, writing – review & editing, Supervision; YWK: Investigation, formal analysis, data curation, writing – review & editing; SL: data Curation, writing – review & editing; BG: conceptualisation, writing – review & editing; KK: Conceptualisation, supervision, data curation, formal analysis, writing – review & editing.
Data sharing
Search results can be made available upon request to the corresponding author.
Declaration of Competing Interest
The authors declare no competing interests.
Acknowledgements
None.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lanwpc.2021.100283.
Appendix. Supplementary materials
References
- 1.Lal N. Pacific Standard Industrial Classification of All Economic Activities 2014. In: Devision SfD, ed. Noumea: Secretariat of the Pacific Community; 2014.
- 2.McNamara KE, Westoby R, Chandra A. Exploring climate-driven non-economic loss and damage in the Pacific Islands. Current Opinion in Environmental Sustainability. 2021;50:1–11. doi: 10.1016/j.cosust.2020.07.004. [DOI] [Google Scholar]
- 3.Booth H. Pacific Island suicide in comparative perspective. Journal of Biosocial Science. 1999;31(4):433–448. doi: 10.1017/S0021932099004332. [DOI] [PubMed] [Google Scholar]
- 4.Bridges FS. Social integration and suicide in the Western Pacific Islands. Psychological Reports. 2008;102(3):683–686. doi: 10.2466/pr0.102.3.683-686. [DOI] [PubMed] [Google Scholar]
- 5.Aghanwa H. The determinants of attempted suicide in a general hospital setting in Fiji Islands: a gender-specific study. General Hospital Psychiatry. 2004;26(1):63–69. doi: 10.1016/j.genhosppsych.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 6.Booth H. The Evolution of Epidemic Suicide on Guam: Context and Contagion. Suicide and Life-Threatening Behavior. 2010;40(1):1–13. doi: 10.1521/suli.2010.40.1.1. [DOI] [PubMed] [Google Scholar]
- 7.Lowe ED. Social Change and Micronesian Suicide Mortality: A Test of Competing Hypotheses. Cross-Cultural Research. 2019;53(1):3–32. doi: 10.1177/1069397118759004. [DOI] [Google Scholar]
- 8.Clayton S. Climate anxiety: Psychological responses to climate change. Journal of Anxiety Disorders. 2020;74 doi: 10.1016/j.janxdis.2020.102263. [DOI] [PubMed] [Google Scholar]
- 9.Dumont C, Haase E, Dolber T, Lewis J, Coverdale J. Climate change and risk of completed suicide. The Journal of nervous and mental disease. 2020;208(7):559–565. doi: 10.1097/NMD.0000000000001162. [DOI] [PubMed] [Google Scholar]
- 10.Tiatia-Seath J, Tupou T, Fookes I. Climate Change, Mental Health, and Well-Being for Pacific Peoples: A Literature Review. The Contemporary Pacific. 2020;32(2):399–430. doi: 10.1353/cp.2020.0035. [DOI] [Google Scholar]
- 11.Cianconi P, Betrò S, Janiri L. The impact of climate change on mental health: a systematic descriptive review. Frontiers in psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.00074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Middleton J, Cunsolo A, Jones-Bitton A, Wright CJ, Harper SL. Indigenous mental health in a changing climate: A systematic scoping review of the global literature. Environmental Research Letters. 2020;15(5) doi: 10.1088/1748-9326/ab68a9. [DOI] [Google Scholar]
- 13.Gibson K, Barnett J, Haslam N, Kaplan I. The mental health impacts of climate change: Findings from a Pacific Island atoll nation. Journal of Anxiety Disorders. 2020;73 doi: 10.1016/j.janxdis.2020.102237. [DOI] [PubMed] [Google Scholar]
- 14.Wasserman D, Carli V, Iosue M, Javed A, Herrman H. Suicide prevention in childhood and adolescence: a narrative review of current knowledge on risk and protective factors and effectiveness of interventions. Asia-Pacific Psychiatry. 2021:e12452. doi: 10.1111/appy.12452. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. Global Health Estimates (2000-2019). https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates. Accessed 8th June 2021.
- 16.World Health Organization . World Health Organization; Geneva: 2021. Suicide worldwide in 2019: Global Health Estimates. [Google Scholar]
- 17.De Leo D, Milner A, Wang X. Suicidal Behavior in the Western Pacific Region: Characteristics and Trends. Suicide and Life-Threatening Behavior. 2009;39(1):72–81. doi: 10.1521/suli.2009.39.1.72. [DOI] [PubMed] [Google Scholar]
- 18.Uddin R, Burton NW, Maple M, Khan SR, Khan A. Suicidal ideation, suicide planning, and suicide attempts among adolescents in 59 low-income and middle-income countries: a population-based study. Lancet Child & Adolescent Health. 2019;3(4):223–233. doi: 10.1016/S2352-4642(18)30403-6. [DOI] [PubMed] [Google Scholar]
- 19.Liu X, Huang Y, Liu Y. Prevalence, distribution, and associated factors of suicide attempts in young adolescents: School-based data from 40 low-income and middle-income countries. PLoS One. 2018;13(12) doi: 10.1371/journal.pone.0207823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kushal SA, Amin YM, Reza S, Shawon MSR. Parent-adolescent relationships and their associations with adolescent suicidal behaviours: Secondary analysis of data from 52 countries using the Global School-based Health Survey. EClinicalMedicine. 2021;31 doi: 10.1016/j.eclinm.2020.100691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization . World Health Organization; 2014. Preventing suicide: A global imperative. [Google Scholar]
- 22.Pirkis J, Amadeo S, Beautrais A, Phillips M, Yip PSF. Suicide Prevention in the Western Pacific Region. Crisis. 2020;41(Suppl 1):S80–s98. doi: 10.1027/0227-5910/a000670. [DOI] [PubMed] [Google Scholar]
- 23.Amadéo S, Kõlves K, Malogne A. Non-fatal suicidal behaviours in French Polynesia: Results of the WHO/START study and its implications for prevention. J Affect Disord. 2016;189:351–356. doi: 10.1016/j.jad.2015.09.042. [DOI] [PubMed] [Google Scholar]
- 24.De Leo D, Milner A, Fleischmann A. The WHO START study: suicidal behaviors across different areas of the world. Crisis. 2013;34(3):156–163. doi: 10.1027/0227-5910/a000193. [DOI] [PubMed] [Google Scholar]
- 25.De Leo D, Milner A. The WHO/START Study: Promoting suicide prevention for a diverse range of cultural contexts. Suicide and Life-Threatening Behavior. 2010;40(2):99–106. doi: 10.1521/suli.2010.40.2.99. [DOI] [PubMed] [Google Scholar]
- 26.Page MJ, McKenzie JE, Bossuyt PM. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1016/j.jclinepi.2021.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kmet LM, Cook LS, Lee RC. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. 2004. doi:10.7939/R37M04F16
- 28.Mathieu SL, Uddin R, Brady M. Systematic Review: The State of Research Into Youth Helplines. Journal of the American Academy of Child & Adolescent Psychiatry. 2020 doi: 10.1016/j.jaac.2020.12.028. [DOI] [PubMed] [Google Scholar]
- 29.Radez J, Reardon T, Creswell C, Lawrence PJ, Evdoka-Burton G, Waite P. Why do children and adolescents (not) seek and access professional help for their mental health problems? A systematic review of quantitative and qualitative studies. European child & adolescent psychiatry. 2020:1–29. doi: 10.1007/s00787-019-01469-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Turecki G, Brent DA, Gunnell D. Suicide and suicide risk. Nature reviews Disease primers. 2019;5(1):1–22. doi: 10.1038/s41572-019-0121-0. [DOI] [PubMed] [Google Scholar]
- 31.Campbell M, McKenzie JE, Sowden A. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368 doi: 10.1136/bmj.l6890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Popay J, Roberts H, Sowden A. Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme Version. 2006;1:b92. [Google Scholar]
- 33.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine. 2009;6(7) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Amadeo S, Rereao M, Malogne A. Testing brief intervention and phone contact among subjects with suicidal behavior: a randomized controlled trial in French Polynesia in the frames of the World Health Organization/Suicide Trends in At-Risk Territories study. Mental Illness. 2015;7(2):48–53. doi: 10.1108/mi.2015.5818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Aghanwa HS. The characteristics of suicide attempters admitted to the main general hospital in Fiji Islands. Journal of Psychosomatic Research. 2000;49(6):439–445. doi: 10.1016/S0022-3999(00)00193-8. [DOI] [PubMed] [Google Scholar]
- 36.Aghanwa HS. Attempted suicide by drug overdose and by poison-ingestion methods seen at the main general hospital in the Fiji islands: a comparative study. General Hospital Psychiatry. 2001;23(5):266–271. doi: 10.1016/S0163-8343(01)00156-6. [DOI] [PubMed] [Google Scholar]
- 37.Haynes RH. Suicide in Fiji: a preliminary study. Br J Psychiatry. 1984;145:433–438. doi: 10.1192/bjp.145.4.433. [DOI] [PubMed] [Google Scholar]
- 38.Henson C, Taylor A, Cohen J, Waqabaca AQ, Chand S. Attempted suicide in Fiji. Religion. 2012;5(1.94):3.63–68.33. [Google Scholar]
- 39.Peiris-John R, Kafoa B, Wainiqolo I, Reddy RK, McCaig E, Ameratunga SN. Population-based characteristics of fatal and hospital admissions for poisoning in Fiji: TRIP Project-11. Injury Prevention. 2013;19(5):355–357. doi: 10.1136/injuryprev-2012-040651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Price J, Karim I. Suicide in Fiji - 2-Year Survey. Acta Psychiatrica Scandinavica. 1975;52(3):153–159. doi: 10.1111/j.1600-0447.1975.tb00032.x. [DOI] [PubMed] [Google Scholar]
- 41.Pridmore S, Lawler A, Couper D. Hanging and poisoning autopsies in Fiji. Australian and New Zealand Journal of Psychiatry. 1996;30(5):685–687. doi: 10.3109/00048679609062666. [DOI] [PubMed] [Google Scholar]
- 42.Pridmore S, Ryan K, Blizzard L. Victims of violence in Fiji. Australian and New Zealand Journal of Psychiatry. 1995;29(4):666–670. doi: 10.3109/00048679509064983. [DOI] [PubMed] [Google Scholar]
- 43.Ree GH. Suicide in Macuata Province, Fiji - Review of 73 Cases. Practitioner. 1971;207(1241):669. -+ [PubMed] [Google Scholar]
- 44.Roberts G, Cohen J, Khan N, Irava W. Attempted suicide in Western Viti Levu, Fiji. Pac Health Dialog. 2007;14(2):29–33. [PubMed] [Google Scholar]
- 45.Wainiqolo I, Kafoa B, Kool B, Herman J, McCaig E, Ameratunga S. A profile of Injury in Fiji: findings from a population-based injury surveillance system (TRIP-10) BMC Public Health. 2012;12 doi: 10.1186/1471-2458-12-1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Herman J, Peiris-John R, Wainiqolo I. Epidemiology of fatal and hospitalised injuries among youth in Fiji (TRIP 15) Journal of paediatrics and child health. 2016;52(11):1026–1031. doi: 10.1111/jpc.13250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pinhey TK, Millman SR. Asian/Pacific islander adolescent sexual orientation and suicide risk in Guam. American Journal of Public Health. 2004;94(7):1204–1206. doi: 10.2105/ajph.94.7.1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ran M-S, Chen S, Salomon MI. Factors related to suicidal ideation among college students in Guam. Illness, Crisis, & Loss. 2015;23(1):21–32. doi: 10.2190/IL.23.1.c. [DOI] [Google Scholar]
- 49.Goodfellow B, Kolves K, Selefen AC, Massain T, Amadeo S, De Leo D. The WHO/START study in New Caledonia: A psychological autopsy case series. Journal of Affective Disorders. 2020;262:366–372. doi: 10.1016/j.jad.2019.11.020. [DOI] [PubMed] [Google Scholar]
- 50.Vignier N, Lert F, Salomon C, Hamelin C. Kava drinking associated with suicidal behaviour among young Kanaks using kava in New Caledonia. Australian and New Zealand Journal of Public Health. 2011;35(5):427–433. doi: 10.1111/j.1753-6405.2011.00737.x. [DOI] [PubMed] [Google Scholar]
- 51.Rubinstein DH. Epidemic suicide among Micronesian adolescents. Social Science & Medicine. 1983;17(10):657–665. doi: 10.1016/0277-9536(83)90372-6. [DOI] [PubMed] [Google Scholar]
- 52.Pridmore S. Suicidal behavior in the Honiara area of the Solomon Islands. International Journal of Mental Health. 1997;25(4):33–38. doi: 10.1080/00207411.1996.11449376. [DOI] [Google Scholar]
- 53.Tavite A, Tavite S. Suicide in the Tokelau islands. Pac Health Dialog. 2009;15(2):67–83. [PubMed] [Google Scholar]
- 54.Sakamoto JL, Shibanuma A, Jimba M. Depressed mood, suicidal behaviors, and health risk behaviors among youths in the Commonwealth of the Northern Mariana Islands: the 2017 CNMI Youth Risk Behavior Survey. BMC Public Health. 2020;20(1):489. doi: 10.1186/s12889-020-08663-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Booth H. Gender, power and social change: Youth suicide among Fiji Indians and Western Samoans. Journal of the Polynesian Society. 1999;108(1):39–68. [Google Scholar]
- 56.Devries K, Watts C, Yoshihama M. Violence against women is strongly associated with suicide attempts: evidence from the WHO multi-country study on women's health and domestic violence against women. Soc Sci Med. 2011;73(1):79–86. doi: 10.1016/j.socscimed.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 57.Sharma B, Lee TH, Nam EW. Loneliness, Insomnia and Suicidal Behavior among School-Going Adolescents in Western Pacific Island Countries: Role of Violence and Injury. International Journal of Environmental Research and Public Health. 2017;14(7) doi: 10.3390/ijerph14070791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Peltzer K, Pengpid S. Early Substance Use Initiation and Suicide Ideation and Attempts among School-Aged Adolescents in Four Pacific Island Countries in Oceania. International Journal of Environmental Research and Public Health. 2015;12(10):12291–12303. doi: 10.3390/ijerph121012291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pengpid S, Peltzer K. Past 12-month history of single and multiple suicide attempts among a national sample of school-going adolescents in Tonga. Asia-Pacific Psychiatry. 2021;13:e12425. doi: 10.1111/appy.12425. [DOI] [PubMed] [Google Scholar]
- 60.Pengpid S, Peltzer K. Prevalence and correlates of suicidal behavior among a national population-based sample of adults in Kiribati. Asia-Pacific Psychiatry. 2020:e12444. doi: 10.1111/appy.12444. [DOI] [PubMed] [Google Scholar]
- 61.Oxford Centre for Evidence Based Medicine. Oxford Centre for Evidence Based Medicine: Levels of Evidence (March 2009). https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009. Published 2009. Accessed 21/02/2021.
- 62.Värnik A, Kõlves K, van der Feltz-Cornelis CM. Suicide methods in Europe: a gender-specific analysis of countries participating in the “European Alliance Against Depression. Journal of Epidemiology & Community Health. 2008;62(6):545–551. doi: 10.1136/jech.2007.065391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kõlves K, De Leo D. Suicide methods in children and adolescents. European child & adolescent psychiatry. 2017;26(2):155–164. doi: 10.1007/s00787-016-0865-y. [DOI] [PubMed] [Google Scholar]
- 64.Pollock NJ, Naicker K, Loro A, Mulay S, Colman I. Global incidence of suicide among Indigenous peoples: a systematic review. BMC Medicine. 2018;16(1):145. doi: 10.1186/s12916-018-1115-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lester D. Suicide in emigrants from the Indian subcontinent. Transcultural psychiatry. 2000;37(2):243–254. doi: 10.1177/136346150003700206. [DOI] [Google Scholar]
- 66.Leske S, Paul E, Gibson M, Little B, Wenitong M, Kolves K. Global systematic review of the effects of suicide prevention interventions in Indigenous peoples. J Epidemiol Community Health. 2020;74(12):1050–1055. doi: 10.1136/jech-2019-212368. [DOI] [PubMed] [Google Scholar]
- 67.World Health Organization; Geneva: 2021. Live Life: An implementation guide for suicide prevention in countries. [Google Scholar]
- 68.Chang O, Patel VL, Iyengar S, May W. Impact of a mobile-based (mHealth) tool to support community health nurses in early identification of depression and suicide risk in Pacific Island Countries. Australasian Psychiatry. 2021;29(2):200–203. doi: 10.1177/1039856220956458. [DOI] [PubMed] [Google Scholar]
- 69.World Health Organization. The WHO STEPwise approach to noncommunicable disease risk factor surveillance: WHO STEPS Surveillance Manual. https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/steps. Published 2020. Accessed 1st June 2021.
- 70.De Leo D, Goodfellow B, Silverman M. International study of definitions of English-language terms for suicidal behaviours: a survey exploring preferred terminology. BMJ open. 2021;11(2) doi: 10.1136/bmjopen-2020-043409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Harfield S, Pearson O, Morey K. Assessing the quality of health research from an Indigenous perspective: the Aboriginal and Torres Strait Islander quality appraisal tool. BMC medical research methodology. 2020;20(1):1–9. doi: 10.1186/s12874-020-00959-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.