Introduction
The COVID-19 pandemic has created changes to the epidemiology of individuals accessing healthcare services, specifically those who are marginalized in society. High rates of anxiety, stress, and depression have been observed. 1 Some policy-makers have postulated that COVID-related lockdown measures may increase suicide rates, yet potentially increased rates of suicide may be related to many other factors during the pandemic. 2 The objective of this study was to measure the impact of public health measures on rates of suicide during the first wave of the COVID-19 pandemic.
Methods
In this cohort study, we assembled suicide death data for all residents of the Canadian province of British Columbia (BC) from the BC Coroners Service from January 2010 through August 2020. The population of BC was 5.1 million at the beginning of 2020. 3
In BC, consistent with the Supreme Court of Canada’s decision in F.H. v. Hugh McDougall, a finding of suicide is now made on a balance of probabilities, in that it is more likely than not, that the death was a result of intentional self-harm. This study was not subject to institutional review board approval or the requirement for informed consent because it used public data.
We used autoregressive integrated moving average (ARIMA) models to analyze suicide deaths in BC, controlling for monthly population as a covariate. 4 We also controlled for seasonal variation. We plotted suicide deaths during each month of 2020 for which complete data exist (January to August). Incident rates and ratios for the first wave of the COVID-19 pandemic (March to August) and the previous 10-year period (2010 to 2019) were determined. Statistical significance was set at P < 0.05, and all tests were 2-tailed. Analysis was conducted with Stata (version 16, College Station, TX).
Results
During the first wave of the COVID-19 pandemic (March to August, 2020), 237 suicide deaths were observed in BC (incident rate 0.93 [95% CI, 0.87 to 0.99] per 100,000 person-months). From 2010 to 2019, 5758 suicide deaths were observed in BC (incident rate 1.01 [95% CI, 0.95 to 1.07] per 100,000 person-months) resulting in an incident rate ratio of 0.92 (95% CI, 0.86 to 0.98).
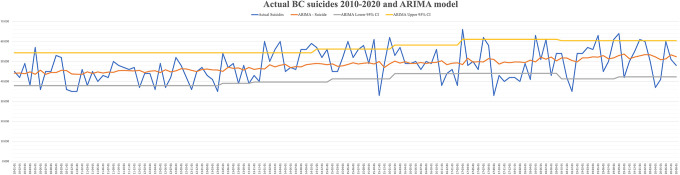
Using ARIMA models controlling for monthly population changes and seasonal variation, the number of suicide deaths during the first wave of the pandemic did not deviate from projected expectations (Figure 1).
Figure 1.
Autoregressive integrated moving average model of expected suicide deaths versus observed suicide deaths for British Columbia for the study period.
Discussion
The initial phase of the COVID-19 pandemic in Canada was met with an unparalleled degree of government spending and support programs to support those citizens impacted economically. These measures may have mitigated some of the mental health consequences during the initial phase of the pandemic including the risk of suicide. Notably, the stable rates of suicide observed in BC parallel those observed with ecological disasters. 5 Our findings are also similar to recent observations from the United States and Australia showing no increase in suicide rates in the initial phase of the pandemic. 4,6 The effect of prolonged economic hardship, increased substance use, and social isolation on suicide rates with the continuation of the pandemic has yet to be determined.
A potential limitation of our study is that in some Canadian jurisdictions, it can take up to 2 years for coroners to make the final determination regarding suicide. It is unclear the effect this may have on our study findings, but we attempted to control for this variability by using the 10-year period prior to the pandemic as a control.
Future research is warranted to explore the impact of the COVID-19 pandemic on the mental health and rates of suicide among at-risk groups in the population including youth, indigenous persons, and economically disadvantaged persons.
Footnotes
Authors’ Note: Data are publicly accessible at https://www2.gov.bc.ca/assets/gov/birth-adoption-death-marriage-and-divorce/deaths/coroners-service/statistical/suicide_knowledge_update.pdf.
Author Contributions: David Barbic, Frank X. Scheuermeyer, Skye P. Barbic, and William G. Honer conceived and developed this study. David Barbic obtained the data, verified the underlying data, and analyzed the data. All authors were involved in the interpretation of the results and preparation of the article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: David Barbic, MD, MSc https://orcid.org/0000-0002-6998-3151
References
- 1. Hawke LD, Barbic SP, Voineskos A, et al. Impacts of COVID-19 on youth mental health, substance use, and well-being: a rapid survey of clinical and community samples: répercussions de la COVID-19 sur la santé mentale, l’utilisation de substances et le bien-être des adolescents : un sondage rapide d’échantillons cliniques et communautaires. Can J Psychiatry. 2020;65(10):701–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gunnell D, Appleby L, Arensman E, et al. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7(6):468–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Services M of C. Population estimates—province of British Columbia [Internet]. Province of British Columbia, Canada; 2021. [accessed 2021 Jan 29]. https://www2.gov.bc.ca/gov/content/data/statistics/people-population-community/population/population-estimates [Google Scholar]
- 4. Faust JS, Shah SB, Du C, Li SX, Lin Z, Krumholz HM. Suicide deaths during the COVID-19 stay-at-home advisory in Massachusetts, March to May 2020. JAMA Netw Open. 2021;4(1):e2034273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Morganstein JC, Ursano RJ. Ecological disasters and mental health: causes, consequences, and interventions. Front Psychiatry. 2020;11:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Leske S, Kõlves K, Crompton D, Arensman E, de Leo D. Real-time suicide mortality data from police reports in Queensland, Australia, during the COVID-19 pandemic: an interrupted time-series analysis. Lancet Psychiatry. 2021;8(1):58–63. [DOI] [PMC free article] [PubMed] [Google Scholar]