Abstract
Objective
Mental health emergencies among young people are increasing. There is growing pressure for emergency departments to screen patients for mental health needs even when it is not their chief complaint. We hypothesized that young people with an initial non‐specific condition and emergency department (ED) revisits have increased mental health needs.
Methods
Retrospective, observational study of the California Office of Statewide Health Planning and Development Emergency Department Discharge Dataset (2010–2014) of young people (11–24 years) with an index visit for International Classification of Diseases, Ninth Revision diagnostic codes of “Symptoms, signs, and ill‐defined conditions” (Non‐Specific); “Diseases of the respiratory system” (Respiratory) and “Unintentional injury” (Trauma) who were discharged from a California ED. Patients were excluded if they had a prior mental health visit, chronic disease, or were pregnant. ED visit frequency was counted over 12 months. Regression models were created to analyze characteristics associated with a mental health visit.
Results
Patients in the Non‐Specific category compared to the Respiratory category had 1.2 times the odds of a future mental health visit (OR 1.20; 95% CI 1.17–1.24). Patients with ≥1 ED revisit, regardless of diagnostic category, had 1.3 times the odds of a future mental health visit. Patients with both a Non‐Specific index visit and 1, 2, and 3 or more revisits with non‐specific diagnoses had increasing odds of a mental health visit (OR 1.38; 95% CI 1.29–1.47; OR 1.70; 95% CI 1.46–1.98; OR 2.20; 95% CI 1.70–2.87, respectively.)
Conclusions
Young people who go to the ED for non‐specific conditions and revisits may benefit from targeted ED mental health screening.
Keywords: Young people ED mental health visits, young people mental health needs, young people mental health screening, young people repeat ED visits
1. INTRODUCTION
1.1. Background
Throughout the last decade, mental health emergencies among young people in the United States have increased. Suicide is now the second leading cause of death in young people, 1 defined by the World Health Organization (WHO) as individuals between 10 and 24 years of age. 2 , 3 , 4 Visits to emergency departments in this population for mental health disorders, suicidal ideation, suicide attempts, self‐harm, and substance use are also increasing. 5 , 6 , 7 , 8 , 9 , 10 , 11 Some note that the advent of social media has been tied with increasing rates of self‐harm and suicidal ideation among young people. 12 Similarly, high rates of cyberbullying have contributed to the growing mental health burden among adolescents, with a meta‐analysis showing the median prevalence was 23% among teenagers. 13 Even among college‐aged people depression, anxiety, and suicide have increased significantly in the United States in the last decade. 14 In addition, during the COVID‐19 pandemic young people between 11 and 24 years of age were more likely to have moderate to severe signs of anxiety and depression compared to older age groups. 15
This landscape of increasing mental health needs and increasing emergency department (ED) mental health visits of young people is concurrent with a change in primary care and ED use. Decreased access to primary care, lower caregiver health literacy, public insurance, Hispanic ethnicity, and certain non‐White races, have all been linked to higher rates of pediatric ED visits. 16 , 17
1.2. Importance
Given the higher risk of mental health symptoms in young people along with the increased use of ED in the pediatric population it has been suggested that EDs should screen pediatric patients for mental health needs. 18 , 19 Although there are validated screening tools for patients in the pediatric ED setting, most EDs, however, have not routinely adopted these, citing multiple barriers including the time required for universal mental health screening in a busy ED. 20 , 21 , 22 We seek to identify a population who would benefit from targeted ED mental health screening, thus encouraging healthcare practitioners to take advantage of this currently missed opportunity to identify patients with mental health needs.
1.3. Objectives of this investigation
Our study objective was to identify the characteristics of a population that would benefit from targeted ED mental health screening. We hypothesized that young people, 11 to 24 years of age, who visited the ED for non‐specific conditions and who made frequent ED visits, would present to the ED with a subsequent mental health diagnosis at higher rates when compared to control populations. We have selected this age group given the Affordable Care Act allowed young adults access to the health insurance through their parents, the high needs of mental health resources in this population, and the classification of young people up to 24 years of age by certain organizations including the WHO and United Nations. 23
The Bottom Line.
An analysis of more than 7 million emergency department visits by young people 11–24 years of age in California showed that patients with non‐specific symptoms and frequent ED visits had greater odds of a future mental health visit, up to 2.2 times greater risk with 3 or more revisits in a 12‐month period. These results suggest that young people who go to the ED for non‐specific conditions and revisits may benefit from targeted ED mental health screening.
2. METHODS
2.1. Study design and data source
This was a retrospective, observational study of a non‐public version of the California Office of Statewide Health Planning and Development (OSHPD) Emergency Department Discharge Dataset (2010–2014), to which all California licensed hospitals are required to submit administrative data semiannually for every patient visit. Reported data include patient demographic information such as age, gender, county of residence, and race and ethnicity; principal diagnosis and 24 other diagnoses, as well as external cause of injury codes (E‐codes); treatment information such as principal and other procedures; disposition, total charges; and expected source of payment. 24 The OSHPD datasets are used standardly in population‐wide health care use studies in California in areas of trauma, pediatric regionalization, and mental health use. 25 , 26 , 27 Our university institutional review board and the California human subjects panel approved this protocol. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for observational studies were utilized in preparing this manuscript.
2.2. Definition of visit categories
We used International Classification of Diseases, Ninth Revision (ICD‐9), Clinical Modification discharge diagnosis codes to define 3 categories: (1) “Non‐Specific” Category: Patients with ED visits with sole ICD‐9 diagnostic codes “Symptoms, signs, and ill‐defined conditions” (780.5‐781.1; 782, 784.0‐784.61, 784.9, 786.2,786.5‐787.91, 789.0‐789.6); (2) “Respiratory” Category: Patients with ED visits with sole ICD‐9 Diagnostic codes of “Diseases of the respiratory system” (460‐519); and (3) “Trauma” Category: Patients with ED visits with ICD‐9 diagnostic codes of “injury” 800–957 specified as “accidental” (E880‐E928).
The Non‐Specific category of patients served as our primary study category as we sought to study a clinically meaningful group of young people who might be using the ED as a proxy for primary health care, where mental health screening is more routinely carried out. The Respiratory and Trauma Categories were the comparator groups. These 2 groups were chosen because they represented the 2 most common pediatric ED diagnostic groupings. 28
While a patient could have more than one discharge diagnosis, all discharge diagnostic codes had to be in the same category. For example, a patient with a discharge diagnosis of abdominal pain (ICD‐9 Code 789.00) and nausea with vomiting (ICD‐9 Code 787.01) would be included in the Non‐Specific category. However, a patient with discharge diagnosis of abdominal pain (ICD‐9 Code 789.00) and a urinary tract infection (ICD‐9 Code 599.0) would be excluded from the study.
2.3. Exclusion criteria
We excluded patients with chronic conditions; patients who were admitted, transferred, or expired; patients who were pregnant in the last year; or patients with a prior mental health diagnosis. Patients with no patient identifier or an out‐of‐state address were also excluded.
2.4. Patient population
We identified 7,158,164 visits by young people 11–24 years of age to California EDs during the study years (Figure 1). We then identified patients who had sole discharge diagnoses that in the Non‐Specific, Respiratory, or Trauma category and classified the earliest visit as the index visit. Patients who had any of the exclusion criteria defined previously were then excluded. In addition, we then looked back 365 days from the patient's first index visit and excluded patients with a previous mental health diagnosis, chronic condition, or pregnancy because all likely have medical care or access to appropriate resources. 29
FIGURE 1.
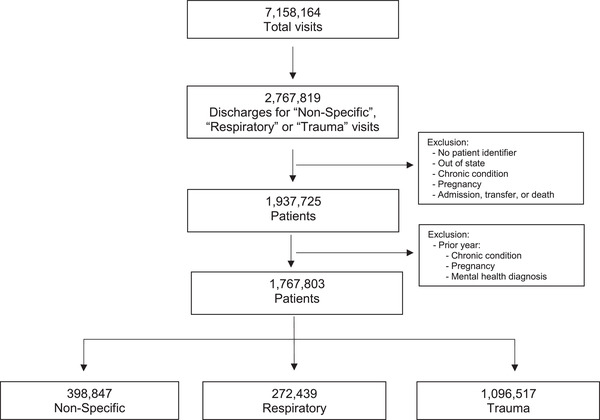
Flow chart depicting derivation of final study sample from patients aged 11–24 years with index visits between January 1, 2011 to September 30, 2014
2.5. Index visits
We then studied patients based on their index visit category using an iterative process beginning with discharge diagnoses between January 1, 2011, and September 30, 2014. All Non‐Specific index visits within the dataset were identified and associated patients were placed in the Non‐Specific category. Patients with index visits with Respiratory and Trauma diagnoses were then identified and categorized via the same method. The patients associated with each category's index visit then had their data reviewed to look for subsequent ED revisits within the next 365 days. An ED revisit was defined as the number of ED visits a patient had within 365 days of the index visit or until the patient had an ED visit with a mental health discharge diagnosis (ICD‐9 290–316), whichever was sooner. The mental health ED visit within 365 days did not count as a revisit.
2.6. Independent variables
We stratified patient age groups: 11–14, 15–17, 18–20, and 21–24 years of age. Race and ethnicity were categorized as a single variable with the following categories: White Non‐Hispanic (White), Black Non‐Hispanic (Black), Hispanic, Native American, Asian/Pacific Islander, and Other. Insurance status was categorized as public or government, private, or uninsured. Urban and rural status was designated by the metropolitan statistical area of the county of the patient's residence. 30 ED revisit frequency was categorized as 0 (the patient had only an index visit with no revisits) to 3 or more revisits.
2.7. Outcome variables
Our outcome variable was an ED mental health visit within 365 days after the index visit for 1 of the 3 study categories: Non‐Specific, Respiratory, or Trauma.
2.8. Statistical methods and analysis
We first tabulated index visit category by demographic characteristics, with or without a new mental health visit and by ED visit frequency. Subsequently, using the previously defined independent and outcome variables, multivariate regression models were created to analyze characteristics associated with an ED mental health visit. Our main model included patient demographics, as well as index visit category and ED visit frequency, adjusting for the study year. We conducted prespecified subgroup analyses for patients in the Non‐Specific index visit category. A second prespecified subgroup analysis was performed with the Non‐Specific population with revisits for non‐specific complaints only. We assessed multicollinearity by checking the variance inflation factor, which demonstrated minimal multicollinearity. P values less than 0.05 were a priori designated as statistically significant. Statistical analysis was performed using SAS 9.4.
3. RESULTS
3.1. Characteristics of study subjects
Of 7,158,164 youth (11–24 years) visits, 1,767,803 patients with Non‐Specific, Respiratory, and Trauma diagnoses were identified that fit the inclusion criteria (Figure 1). Of these patients, 398,847 (22.5%) were categorized with a Non‐Specific index visit, 272,439 (15.4%) had a Respiratory index visit, and 1,096,517 (62.0%) had a Trauma index visit.
Table 1 shows the characteristics of the study population in regard to demographics, insurance, and region. For patients in the Non‐Specific category, 11–14 year‐olds made up the largest proportion (29.4%) of patients. Females represented the majority of Non‐Specific patients (59.7%). Regarding race and ethnicity, Hispanics (49.5%) and Whites (30.0%) represented the largest proportion of patients. Although most patients had some form of insurance, 14.6% were uninsured. The majority of Non‐Specific patients (91.0%) were treated in urban areas.
TABLE 1.
Characteristics of patients who were discharged from a California ED in 2011 to 2014 with an index visit category of non‐specific, respiratory or trauma
| Category | Non‐Specific | Respiratory | Trauma | Total |
|---|---|---|---|---|
| Total Patients | 398,847 | 272,439 | 1,096,517 | 1,767,803 |
| Age (years) | ||||
| 11–14 | 117,416 (29.4%) | 90,716 (33.3%) | 396,194 (36.1%) | 604,326 (34.2%) |
| 15–17 | 104,304 (26.2%) | 71,682 (26.3%) | 315,774 (28.8%) | 491,760 (27.8%) |
| 18–20 | 75,543 (18.9%) | 48,619 (17.8%) | 164,365 (15.0%) | 288,527 (16.3%) |
| 21‐24 | 101,584 (25.5%) | 61,422 (22.5%) | 220,184 (20.1%) | 383,190 (21.7%) |
| Insurance Type | ||||
| Public | 161,501 (40.5%) | 123,196 (45.2%) | 347,058 (31.7%) | 631,755 (35.7%) |
| Private | 177,101 (44.4%) | 105,774 (38.8%) | 549,291 (50.1%) | 832,166 (47.1%) |
| Uninsured | 58,284 (14.6%) | 42,283 (15.5%) | 170,795 (15.6%) | 271,362 (15.4%) |
| Other | 1,961 (0.5%) | 1,186 (0.4%) | 29,373 (2.7%) | 32,520 (1.8%) |
| Gender | ||||
| Female | 238,281 (59.7%) | 150,399 (55.2%) | 407,271 (37.1%) | 795,951 (45.0%) |
| Male | 160,557 (40.3%) | 122,036 (44.8%) | 689,213 (62.9%) | 971,806 (55.0%) |
| Missing | 9 (0.0%) | 4 (0.0%) | 33 (0.0%) | 46 (0.0%) |
| Race | ||||
| White | 119,469 (30.0%) | 85,551 (31.4%) | 428,154 (39.0%) | 633,174 (35.8%) |
| Black | 36,464 (9.1%) | 30,122 (11.1%) | 96,045 (8.8%) | 162,631 (9.2%) |
| Hispanic | 197,429 (49.5%) | 129,291 (47.5%) | 441,416 (40.3%) | 768,136 (43.5%) |
| Asian/Pacific Islander | 19,393 (4.9%) | 10,673 (3.9%) | 56,525 (5.2%) | 86,591 (4.9%) |
| Native American | 1,121 (0.3%) | 757 (0.3%) | 3,588 (0.3%) | 5,466 (0.3%) |
| Other | 17,189 (4.3%) | 11,905 (4.4%) | 49,852 (4.5%) | 78,946 (4.5%) |
| Not Available | 7,782 (2.0%) | 4,140 (1.5%) | 20,937 (1.9%) | 32,859 (1.9%) |
| Region | ||||
| Rural | 29,665 (7.4%) | 23,902 (8.8%) | 92,872 (8.5%) | 146,439 (8.5%) |
| Urban | 362,876 (91.0%) | 243,211 (89.3%) | 980,451 (89.4%) | 1,586,538 (89.7%) |
| Not Available | 6,306 (1.6%) | 5,326 (2.0%) | 23,194 (2.1%) | 34,826 (2.0%) |
3.2. Main results
The vast majority of patients in all categories (97.7%) did not have a new mental health ED visit within a year of their index visit (Table 2). However, Non‐Specific patients had the highest percentage of patients who returned with a new mental health ED visit (3.2%), compared to Respiratory (2.7%) and Trauma (1.9%) patients. Likewise, the majority of patients did not have any revisits (86.0%); while 10.0% had 1 revisit; 2.6% had 2 revisits and 1.3% had 3+ revisits. Patients with a new mental health ED visit compared to those without, had a larger proportion of revisits. Of patients with a new mental health visit, 73.9% had an index visit only, while 18.1% had 1 revisit; 5.1% had 2 revisits and 2.9% had 3+ revisits. Proportions of revisits in patients without a new mental health ED visit reflected the overall population proportions.
TABLE 2.
Association between frequency of visits with new mental health diagnosis compared to no mental health diagnosis by index visit category (n = 1,767,803)
| Total for All Categories | Non‐Specific | Respiratory | Trauma | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Total Patient Pop. | No Mental Health ED Visit | New Mental Health ED Visit | No Mental Health ED Visit | New Mental Health ED Visit | No Mental Health ED Visit | New Mental Health ED Visit | No Mental Health ED Visit | New Mental Health ED Visit | |
| ED Revisits* | |||||||||
| 0 | 1,515,794 | 1,485,809 (86.0%) | 29,985 (73.9%) | 307,936 (79.8%) | 8,794 (68.1%) | 217,305 (81.9%) | 5,208 (71.9%) | 960,568 (89.3%) | 15,983 (78.2%) |
| 1 | 180,787 | 173,422 (10.0%) | 7,365 (18.1%) | 50,580 (13.1%) | 2,576 (19.9%) | 32,978 (12.4%) | 1,416 (19.5%) | 89,864 (8.4%) | 3,373 (16.5%) |
| 2 | 47,760 | 45,704 (2.6%) | 2,056 (5.1%) | 16,697 (4.3%) | 890 (6.9%) | 9,943 (3.7%) | 408 (5.6%) | 19,064 (1.8%) | 758 (3.7%) |
| 3+ | 23,462 | 22,267 (1.3%) | 1,195 (2.9%) | 10,715 (2.8%) | 659 (5.1%) | 4,967 (1.9%) | 214 (3.0%) | 6,585 (0.6%) | 322 (1.6%) |
| Total | 1,767,803 | 1,727,202 (97.7%) | 40,601 (2.3%) | 385,928 (96.8%) | 12,919 (3.2%) | 265,193 (97.3%) | 7,246 (2.7%) | 1,076,081 (98.1%) | 20,436 (1.9%) |
ED revisits under “No Mental Health ED Visit” equates to the number of visits 365 days after the index visit (because the patient had no subsequent mental health revisit); ED revisits under “New Mental ED Health Visit” equates to the number of visits between the index visit and the new mental health ED visit that occurred within 365 days of the index visit.
We used a multivariate regression analysis to identify characteristics associated with presenting with a new mental health ED visit (Table 3). Odds ratios were adjusted to account for other patient characteristics. Patients in the Non‐Specific category compared to Respiratory category had 1.2 times the odds of a new mental health ED visit (odds ratio [OR] 1.20; 95% confidence interval [CI] 1.17–1.24). In contrast, patients in the Trauma category compared to Respiratory category had a 20% decrease in odds of a new mental health ED visit (OR 0.80; 95% CI 0.78–0.83).
TABLE 3.
Characteristics associated with a mental health visit after an index visit categorized as Non‐Specific, Respiratory, or Trauma via multivariate regression analysis. (n = 1,701,062) [c = 0.756]
| Characteristic | Adjusted Odds Ratio (95% Confidence Interval) |
|---|---|
| Index Visit Diagnosis | |
| Respiratory | Reference |
| Non‐Specific | 1.20 (1.17–1.24) |
| Trauma | 0.80 (0.78–0.83) |
| Age, years | |
| 11–14 | Reference |
| 15–17 | 1.77 (1.70–1.85) |
| 18–20 | 7.51 (7.23–7.79) |
| 21–24 | 7.19 (6.93–7.46) |
| Payer | |
| Private | Reference |
| Public | 1.88 (1.83–1.92) |
| Uninsured | 1.49 (1.45–1.54) |
| Other | 0.90 (0.84–0.97) |
| Female Sex | 0.80 (0.77–0.83) |
| Race | |
| White Non‐Hispanic | Reference |
| Black | 0.93 (0.90–0.96) |
| Hispanic | 0.67 (0.65–0.68) |
| Asian | 0.46 (0.43–0.49) |
| Native American | 1.28 (1.11–1.47) |
| Other | 0.70 (0.66–0.73) |
| Rural Hospital | 1.43 (1.39–1.48) |
| ED Revisits | |
| 0 | Reference |
| 1 | 1.31 (1.28–1.35) |
| 2 | 1.26 (1.20–1.32) |
| 3+ | 1.31 (1.23–1.39) |
Age, sex, race/ethnicity, insurance, and hospital setting also affected an individual's odds for a new mental health ED visit. Older patients had increased odds of having a new mental health ED visit. Specifically, patients 21–24 years of age had over 7 times increased odds (OR 7.19; 95% CI 6.93–7.46) of having a new mental health ED visit when compared to 11–14 year‐olds.
Females had a 20% decrease in odds (OR 0.80; 95% CI 0.77–0.83) of presenting with a new mental health ED visit than males. In regard to race and ethnicity, when compared to White patients, Native Americans had the highest odds of a new mental health ED visit (OR 1.28; 95% CI 1.11–1.47).
Individuals with public insurance had almost twice the odds (OR 1.88; 95% CI 1.83–1.92) of having a subsequent mental health visit compared to those with private insurance. Uninsured patients had 1.5 times the odds (OR 1.49; 95% CI 1.45–1.54) of having a new mental health ED visit compared to patients with private insurance. Individuals from rural areas had 1.4 times the odds (OR 1.43; 95% CI 1.39–1.48) of having a new mental health ED visit when compared to those treated from urban areas.
Regarding ED revisits, patients with ≥1 ED revisit, regardless of diagnostic category, had approximately 1.3 times the odds of a new mental health ED visit. Patient ORs for a new mental health ED visit did not significantly rise with subsequent visits and stayed approximately the same at 1.3 times the odds whether there were 1, 2, or 3+ ED revisits.
3.3. Subgroup analysis
We subsequently performed a prespecified subgroup analyses with just the Non‐Specific population (n = 384,928) to identify characteristics associated with presenting with a new mental health ED visit (Table 4). In Non‐Specific patients with any type of ED revisit, there was approximately a 1.3 odds increase between the number of repeat visits and a new mental health ED visit. There was no statistically significant difference between the number of revisits (1, 2, 3, or more). A second prespecified subgroup analysis was performed with the Non‐Specific population with revisits for non‐specific complaints only. This analysis identified a significant association between the number of revisits for non‐specific needs and the odds of a future mental health visit. Non‐Specific patients with 1 (OR 1.38; 95% CI 1.29–1.47), 2 (OR 1.70; 95% CI 1.46–1.98), and 3 or more (OR 2.20; 95% CI 1.70–2.87) non‐specific ED revisits had increasing odds of a new mental health ED visit with each subsequent revisit.
TABLE 4.
Subgroup analysis of characteristics associated with a future mental health visit in the non‐specific population for patients with (a) any ED revisit and (b) non‐specific ED revisits. (n = 384,928); [c = 0.722]
| Adjusted Odds Ratio (95% Confidence Interval) | ||
|---|---|---|
| Non‐Specific Population | ||
| Characteristic | Any ED Revisit* | Non‐Specific ED Revisit** |
| Age, years | ||
| 11–14 | Reference | Reference |
| 15–17 | 1.69 (1.56–1.82) | 1.68 (1.56–1.81) |
| 18–20 | 6.01 (5.63–6.43) | 6.16 (5.77–6.58) |
| 21–24 | 5.65 (5.29–6.03) | 5.76 (5.40–6.16) |
| Payer | ||
| Private | Reference | Reference |
| Public | 1.73 (1.66–1.80) | 1.76 (1.69–1.84) |
| Uninsured | 1.42 (1.35–1.49) | 1.43 (1.36–1.50) |
| Other | 1.15 (0.90–1.46) | 1.15 (0.90–1.47) |
| Female Sex | 0.80 (0.77–0.83) | 0.80 (0.77–0.83) |
| Race | ||
| White Non‐Hispanic | Reference | Reference |
| Black | 0.94 (0.89–1.00) | 0.95 (0.90–1.01) |
| Hispanic | 0.66 (0.63–0.69) | 0.66 (0.63–0.69) |
| Asian | 0.48 (0.43–0.54) | 0.47 (0.42–0.53) |
| Native American | 1.01 (0.75–1.35) | 1.01 (0.76–1.36) |
| Other | 0.67 (0.61–0.74) | 0.67 (0.61–0.74) |
| Rural | 1.36 (1.28–1.44) | 1.37 (1.29–1.45) |
| ED Revisits | ||
| 0 | Reference | Reference |
| 1 | 1.28 (1.22–1.34) | 1.38 (1.29–1.47) |
| 2 | 1.27 (1.18–1.36) | 1.70 (1.46–1.98) |
| 3+ | 1.37 (1.26–1.49) | 2.20 (1.70–2.87) |
ED revisit defined as any revisit for any condition, including respiratory, trauma, and other medical diagnoses
ED revisit defined as any revisit for a non‐specific condition as defined in the methods.
3.4. Limitations
This study has several limitations. Although our study was limited to one state, California is racially and ethnically diverse and accounts for approximately 12% of the total US population. Thus, we believe that findings from this population‐wide study are relevant to many US populations. We use an administrative dataset, which is subject to the inherent shortcomings of these datasets. Clinical information is lacking and diagnoses are subject to coding errors. However, OSHPD has been used for large population‐wide studies with success and are the only readily available data that allow for initial understanding of the association of ED use for non‐specific diagnoses and mental health visits in an entire population of youth. In addition, patients were excluded if they had a previous mental health diagnosis but only during an ED visit in the prior 365 days. This likely excludes those with significant decompensated mental health issues but likely underestimates those with actual mental health diagnoses.
4. DISCUSSION
In our population‐wide study of California young people with ambulatory ED visits, we find that overall, subsequent ED visits for a mental health condition are uncommon. However, among a significant minority of young people, we identify demographic and visit characteristics that are associated with a new mental health ED visit. ED visits for non‐specific complaints were associated with increased odds of a subsequent mental health visit. Similarly, multiple revisits, especially revisits to the ED for non‐specific conditions within twelve months, increase the odds of a new mental health visit. Our analyses have thus identified a population of young people at risk for a future mental health ED visit, and presumptively higher risk for mental health needs, who should be targeted for ED mental health screening.
We found that increased age is associated with higher odds of a new ED mental health visit. In particular, the OR was significantly higher for patients 18 years of age and above. This could be secondary to multiple etiologies, including an increased incidence of mental health problems in young adulthood, increased ability to use alcohol legally, and a culture of using other substances. 31 Young adults also experience the transition of primary medical care away from the pediatric to the adult setting, transitions in insurance, and transitions away from home where the burden of decision making is on them rather than their childhood caregivers. In these settings, the ED might be an easier location to seek care than with a primary care physician. Given the results, it could be argued to prioritize targeting screening for the young adult population in particular.
Strikingly, we find that being male has a greater association with a future mental health visit than being female. We also found that Native Americans had the highest odds of a new mental health ED visit compared to Whites. This is notable given the low overall prevalence of Native Americans in our sample but consistent with the current literature, which shows that Native American communities suffer from historical trauma, higher rates of substance use, and Native American youth have high rates of depression. 32 We find Hispanics and Asians have decreased mental health visits. There have been studies showing underuse of mental health resources, possibly related to cultural stigma. 33
Interestingly, patients whose index visit was in the Trauma category had decreased odds of a future mental health visit compared to patients in the Respiratory category and even more so for those in the Non‐Specific category. This could be because these patients are more likely to have an identifiable reason for coming to the ED (eg, a major or minor traumatic event). Thus, these patients may not be using the ED for reasons that have greater associations with mental health needs.
Notably, patients with public insurance or who are uninsured have increased odds of a new mental health ED visit. This could be because of decreased access to primary care in public insurance (and subsequent screening) and a decrease in mental health resources in the public system. 34 Even if those seeking care for mental health needs in the ED may be owing to lack of outpatient resources, the purpose of this study suggests these patients may still benefit from screening in order to get them more mental resources than they are finding in the outpatient setting.
Rural young people, although they comprise a minority of our study population, had consistently increased odds of a subsequent mental health visit. This could be secondary to lack of access to and/or resources in either primary care or mental health care. 35 Additionally, studies have shown that rural populations have lower access to substance use treatment, including for adolescents. 36 As telemedicine capabilities expand, the difference in access to care between rural and urban adolescents may decrease. 37
We demonstrate that using the ED for non‐specific complaints and for more than one visit has a strong association with a subsequent ED mental health visit. This could be secondary to lack of primary care and the resulting lack of routine mental health screening and referral that would take place in the physician's office. These ED visits for non‐specific conditions come from the most vulnerable populations: uninsured people, adolescents, and young adults. Additionally, some have hypothesized that some individuals with somatic symptoms may instead have an underlying mental health condition. 38
The ED is an important intervention point for young people whose mental health may be suffering to the point of considering death by suicide. In 1 study in England and Wales, Gairin et al found that among adolescents and adults who died by suicide, 39% had visited an ED in the preceding 12 months. 39 These findings were replicated in Northwest England a decade later, when 43% adolescents and adults who died by suicide, were found to have visited an ED in the year before their death. 40 These studies underscore the urgency of identifying and intervening in at‐risk populations in the ED.
As early as 1999, the US Surgeon General recognized that screening played a key role in early identification of mental health problems. 41 Mental health screening tools exist and have been validated for ED use. One example is the Ask Suicide Screening Questionnaire (ASQ), which consists of only 4 questions where a positive response to only 1 of the questions is 97% sensitivity in capturing at‐risk patients. 20 Another example is the HEADS‐ED, which is designed to capture multiple mental health concerns efficiently. 21 In addition, the Health Resources and Services Administration provides a valuable public toolkit that references several other screening tools and resources to help EDs manage and coordinate care for pediatric patients with a mental health crisis. 42 Suicide screening has been shown to be supported by adolescent patients and does not necessarily increase ED lengths of stay. 43 In addition, mental health screening can lead to effective interventions in patients. For example, King et al. found adolescents presenting to the ED for nonpsychiatric complaints who screened positive for suicide risk but did not warrant hospitalization could receive a targeted feedback and interview intervention that decreased depression and suicidality on follow‐up compared to a control group. 44 Another study found that having an intervention plan in adults who screened positive during the ED universal suicide risk screen resulted in 30% fewer total suicide attempts. 45
Unfortunately, these tools remain poorly and inconsistently used, possibly because the extent of the problem has not been well quantified nor publicized. There is also inertia because of the belief that it would be too burdensome to screen all patients and possibly there is a lack of a referral system for a positive screen. Lastly, mental health screeners have not been made part of a standard workflow; however, the available literature suggests it would benefit patients. We contribute to the field and the urgency by identifying characteristics associated with a high‐risk population of young people vulnerable to a future mental health visit. As an area of future study, it would be enlightening to see if Emergency Severity Index (ESI) triage level 4 and 5 patients may yield similar results. In addition, further analysis to see if these non‐specific and frequent ED visits are associated with more specific outcomes, such as suicidal ideation and suicide attempt, could be relevant given some of the screening tools mentioned assess for suicidality. Because all the patients in this study were discharged, one could presume their conditions were low acuity or not urgent and ESI level may be easier to screen for in electronic health systems.
After identification of this specific population of young people at increased association of an ED mental health visit, we believe the next step would be to develop a protocol and workflow for identifying this population in the ED to implement an appropriate screening process and to identify adequate referrals and resources for those who screen positive. Most important, the next step would be to validate the efficiency, efficacy, and outcomes of these processes.
In summary, young people who come to the ED for non‐specific conditions, and those who make frequent subsequent visits, are a vulnerable population and at potentially increased risk than previously known of a future ED mental health visit. Performing targeted mental health screening on this population is a first and imperative step in alleviating need.
CONFLICTS OF INTEREST
All authors have no conflicts to disclose
AUTHOR CONTRIBUTIONS
AF, MH, OS, and NEW conceived the study and designed the trial. NEW and OS supervised the data collection; managed the data, including quality control, and statistical advice on study design. AF, MH, OS, and NEW analyzed the data. AF, MH, NB, and NEW drafted the manuscript, and all authors contributed substantially to its revision. AF takes responsibility for the paper as a whole.
Biography
Andrea Fang, MD, is a Clinical Assistant Professor of Emergency Medicine and Pediatrics and the Pediatric Emergency Medicine Fellowship Director at Stanford University School of Medicine in Stanford, California.

Fang A, Hersh M, Birgisson N, Saynina O, Wang NE. “Could We Have Predicted This?” The Association of a Future Mental Health Need in Young People with a Non‐Specific Complaint and Frequent Emergency Department Visits. JACEP Open. 2021;2:e12556. 10.1002/emp2.12556
Supervising Editor: Chadd Kraus, DO, DrPH
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org ). The authors have stated that no such relationships exist.
Meetings
“‘Could We Have Predicted This?’ Association of Youth Low‐Acuity Emergency Department Visits with Mental Health” Society of Academic Emergency Medicine Annual Meeting, Denver, CO; May 2020 (Oral Presentation – Accepted. Presentation cancelled due to COVID‐19)
“Asking for Help? The Association of Frequent Youth Emergency Department Visits with a Future Mental Health Visit”, Pediatric Academic Societies Meeting, Philadelphia, PA; May 2020 (Poster Presentation – Accepted. Conference cancelled due to COVID‐19)
REFERENCES
- 1. National Institute of Mental Health. Health information statistics, suicide. https://www.nimh.nih.gov/health/statistics/suicide.shtml 2021.
- 2. World Health Organization . Adolescent health. https://www.who.int/southeastasia/health‐topics/adolescent‐health. 2021. [Google Scholar]
- 3. World Health Organization . Sixty‐fourth world health assembly: youth and health risks, Report by the Secretariat. https://apps.who.int/gb/ebwha/pdf_files/WHA64/A64_25‐en.pdf. 2021. [Google Scholar]
- 4. World Health Organization . Adolescence: a period needing special attention ‐ recognizing‐adolescence. https://apps.who.int/adolescent/second‐decade/section2/page1/recognizing‐adolescence.html. 2021.
- 5. Burstein B, Agostino H, Greenfield B. Suicidal attempts and ideation among children and adolescents in US emergency departments, 2007–2015. JAMA Pediatr. 2019;173(6):598‐600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pittsenbarger ZE, Mannix R. Trends in pediatric visits to the emergency department for psychiatric illnesses. Acad Emerg Med. 2014;21(1):25‐30. [DOI] [PubMed] [Google Scholar]
- 7. Lo CB, Bridge JA, Shi J, Ludwig L, Stanley RM. Children's mental health emergency department visits: 2007–2016. Pediatrics. 2020;145(6). [DOI] [PubMed] [Google Scholar]
- 8. Plemmons G, Hall M, Doupnik S, et al. Hospitalization for suicide ideation or attempt: 2008–2015. Pediatrics. 2018;141(6). [DOI] [PubMed] [Google Scholar]
- 9. Kalb LG, Stapp EK, Ballard ED, et al. Trends in psychiatric emergency department visits among youth and young adults in the US. Pediatrics. 2019;143(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cutler GJ, Rodean J, Zima BT, et al. Trends in pediatric emergency department visits for mental health conditions and disposition by presence of a psychiatric unit. Acad Pediatr. 2019;19(8):948‐955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hoffmann JA, Stack AM, Samnaliev M, Monuteaux MC, Lee LK. Trends in visits and costs for mental health emergencies in a pediatric emergency department, 2010–2016. Acad Pediatr. 2019;19(4):386‐393. [DOI] [PubMed] [Google Scholar]
- 12. Sedgwick R, Epstein S, Dutta R, Ougrin D. Social media, internet use and suicide attempts in adolescents. Curr Opin Psychiatry. 2019;32(6):534‐541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hamm MP, Newton AS, Chisholm A, et al. Prevalence and effect of cyberbullying on children and young people: a scoping review of social media studies. JAMA Pediatr. 2015;169(8):770‐777. [DOI] [PubMed] [Google Scholar]
- 14. Duffy ME, Twenge JM, Joiner TE. Trends in mood and anxiety symptoms and suicide‐related outcomes among u.s. undergraduates, 2007–2018: evidence from two national surveys. J Adolesc Health. 2019;65(5):590‐598. [DOI] [PubMed] [Google Scholar]
- 15. Mental Health America . COVID‐19 and Mental Health: a Growing Crisis. Mental Health America. https://mhanational.org/research‐reports/covid‐19‐and‐mental‐health‐growing‐crisis. 2021. [Google Scholar]
- 16. Alpern ER, Clark AE, Alessandrini EA, et al. Recurrent and high‐frequency use of the emergency department by pediatric patients. Acad Emerg Med. 2014;21(4):365‐373. [DOI] [PubMed] [Google Scholar]
- 17. Hong M, Thind A, Zaric GS, Sarma S, The impact of improved access to after‐hours primary care on emergency department and primary care utilization: a systematic review. Health Policy. 2020;124(8):812‐818. [DOI] [PubMed] [Google Scholar]
- 18. Hooker EA, Mallow PJ, Oglesby MM. Characteristics and trends of emergency department visits in the United States (2010‐2014). J Emerg Med. 2019;56(3):344‐351. [DOI] [PubMed] [Google Scholar]
- 19. Bernstein J, Dorfman D, Lunstead J, et al. Reaching Adolescents for prevention: the role of pediatric emergency department health promotion advocates. Pediatr Emerg Care. 2017;33(4):223‐229. [DOI] [PubMed] [Google Scholar]
- 20. Horowitz LM, Bridge JA, Teach SJ, et al. Ask suicide‐screening questions (ASQ): a brief instrument for the pediatric emergency department. Arch Pediatr Adolesc Med. 2012;166(12):1170‐1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cappelli M, Gray C, Zemek R, et al. The HEADS‐ED: a rapid mental health screening tool for pediatric patients in the emergency department. Pediatrics. 2012;130(2):e321‐327. [DOI] [PubMed] [Google Scholar]
- 22. Nager AL, Pham PK, Grajower DN, Gold JI. Mental health screening among adolescents and young adults in the emergency department. Pediatr Emerg Care. 2017;33(1):5‐9. [DOI] [PubMed] [Google Scholar]
- 23. United Nations Department of Economic and Social Affairs . Definition of Youth. https://www.un.org/esa/socdev/documents/youth/fact‐sheets/youth‐definition.pdf. 2021.
- 24. Office of Statewide Health Planning and Development. Data Resources . https://oshpd.ca.gov/data‐and‐reports/data‐resources/ 2021.
- 25. Zocchi MS, Hsia RY, Carr BG, Sarani B, Pines JM. Comparison of mortality and costs at trauma and nontrauma centers for minor and moderately severe injuries in California. Ann Emerg Med. 2016;67(1):56‐67. [DOI] [PubMed] [Google Scholar]
- 26. Supat B, Brennan JJ, Vilke GM, Ishimine P, Hsia RY, Castillo EM. Characterizing pediatric high frequency users of California emergency departments. Am J Emerg Med. 2019;37(9):1699‐1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Niedzwiecki MJ, Sharma PJ, Kanzaria HK, McConville S, Hsia RY. Factors associated with emergency department use by patients with and without mental health diagnoses. JAMA Netw Open. 2018;1(6).. e183528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Burns C, Wang NE, Goldstein BA, Hernandez‐Boussard T. Characterization of young adult emergency department users: evidence to guide policy. J Adolesc Health. 2016;59(6):654‐661. 10.1016/j.jadohealth.2016.07.011. [DOI] [PubMed] [Google Scholar]
- 29. Agency for Healthcare Research and Quality . Chronic condition indicator (CCI) for ICD‐9‐CM . https://www.hcup‐us.ahrq.gov/toolssoftware/chronic/chronic.jsp. 2021.
- 30. Rural County Representatives of California. Rural Counties . https://www.rcrcnet.org/. 2020.
- 31. Park MJ, Paul Mulye T, Adams SH, Brindis CD, Irwin CE. The health status of young adults in the United States. J Adolesc Health. 2006;39(3):305‐317. [DOI] [PubMed] [Google Scholar]
- 32. Garcia JL, Historical trauma and American Indian/Alaska Native youth mental health development and delinquency. New Directions for Child and Adolescent Development. 2020;2020(169):41‐58. [DOI] [PubMed] [Google Scholar]
- 33. Brenes F. Hispanics, mental health, and suicide: brief report. Hisp Health Care Int Off J Natl Assoc Hisp Nurses. 2019;17(3):133‐136. [DOI] [PubMed] [Google Scholar]
- 34. Hodgkinson S, Godoy L, Beers LS, Lewin A. Improving mental health access for low‐income children and families in the primary care setting. Pediatrics. 2017;139(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Baldwin L‐M, Patanian MM, Larson EH, et al. Modeling the mental health workforce in Washington State: using state licensing data to examine provider supply in rural and urban areas. J Rural Health. 2006;22(1):50‐58. [DOI] [PubMed] [Google Scholar]
- 36. Borders TF, Booth BM. Research on rural residence and access to drug abuse services: where are we and where do we go?. J Rural Health. 2007;23:79‐83.. Suppl. [DOI] [PubMed] [Google Scholar]
- 37. Marcin JP, Shaikh U, Steinhorn RH. Addressing health disparities in rural communities using telehealth. Pediatr Res. 2016;79(1‐2):169‐176. [DOI] [PubMed] [Google Scholar]
- 38. Baren JM, Mace SE, Hendry PL, Dietrich AM, Grupp‐Phelan J, Mullin J. Children's mental health emergencies‐part 1: challenges in care: definition of the problem, barriers to care, screening, advocacy, and resources. Pediatr Emerg Care. 2008;24(6):399‐408. [DOI] [PubMed] [Google Scholar]
- 39. Gairin I, House A, Owens D. Attendance at the accident and emergency department in the year before suicide: retrospective study. Br J Psychiatry. 2003;183:28‐33. [DOI] [PubMed] [Google Scholar]
- 40. Da Cruz D, Pearson A, Saini P, et al. Emergency department contact prior to suicide in mental health patients. Emerg Med J. 2011;28(6):467‐471. [DOI] [PubMed] [Google Scholar]
- 41. US Department of Health and Human Services, US Department of Education, US Department of Justice. Report of the Surgeon General's Conference on Children's Mental Health: A National Action Agenda . Washington (DC): US Department of Health and Human Services;. http://www.ncbi.nlm.nih.gov/books/NBK44233/ 19, 2020. [Google Scholar]
- 42. Human Resources and Services Administration . Critical Crossroads: Pediatric Mental Health Care in the Emergency Department. https://www.hrsa.gov/sites/default/files/hrsa/critical‐crossroads/critical‐crossroads‐tool.pdf. 2021.
- 43. Horowitz L, Ballard E, Teach SJ, et al. Feasibility of screening patients with nonpsychiatric complaints for suicide risk in a pediatric emergency department: a good time to talk?. Pediatr Emerg Care. 2010;26(11):787‐792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. King CA, Gipson PY, Horwitz AG, Opperman KJ. Teen options for change: an intervention for young emergency patients who screen positive for suicide risk. PS. 2014;66(1):97‐100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Miller IW, Camargo CA, Arias SA, et al. Suicide prevention in an emergency department population: the ED‐SAFE study. JAMA Psychiatry. 2017;74(6):563‐570. [DOI] [PMC free article] [PubMed] [Google Scholar]


