Individuals with chronic liver disease without cirrhosis rarely develop hepatocellular carcinoma (HCC). However, few chronic liver disease endotypes have been known to cause HCC formation in the absence of cirrhosis, namely, hepatitis B. In North America, the development of de novo HCC in the absence of cirrhosis in autoimmune hepatitis (AIH) is an atypical presentation. We describe a case of a Caucasian man born in the United States developing multifocal HCC in the setting of AIH.
A72-year-old Caucasian male with AIH presented with complaints of abdominal discomfort. His AIH was diagnosed in 1986 and was managed solely on prednisone monotherapy with normal laboratory values after failing a course of steroid sparing therapy and azathioprine because of intractable headaches. At the time, he discontinued alcohol ingestion. Currently, he reported no jaundice, icterus, abdominal distention, palmar erythema, rashes, or pruritis. His physical examination was unrevealing without edema, abdominal distention, caput medusa, or spider angiomas. His complete blood count, comprehensive metabolic panel, and international normalizing ratio were normal. Viral hepatitis and iron panels, ceruloplasmin, and alpha-1 antitrypsin were also normal, whereas his alpha-fetoprotein was 1,089 ng/mL. He underwent an abdominal ultrasound revealing a liver mass in the absence of liver nodularity, echotexture coarseness, or reversal of portal vein flow. An MRI was then performed which demonstrated 2 adjacent masses that lacked contrast washout (Figure 1) and were not present on previous imaging 3 years ago. He subsequently underwent resection with 3 distinct tumors found (Figure 1) and pathology consistent with multifocal HCC. In addition, the resected portion of the liver was noncirrhotic with focal residual bridging fibrosis, Ishak 3, and histological activity index of 3/18 (Figure 2). The patient tolerated the surgery with a full recovery.
Figure 1.
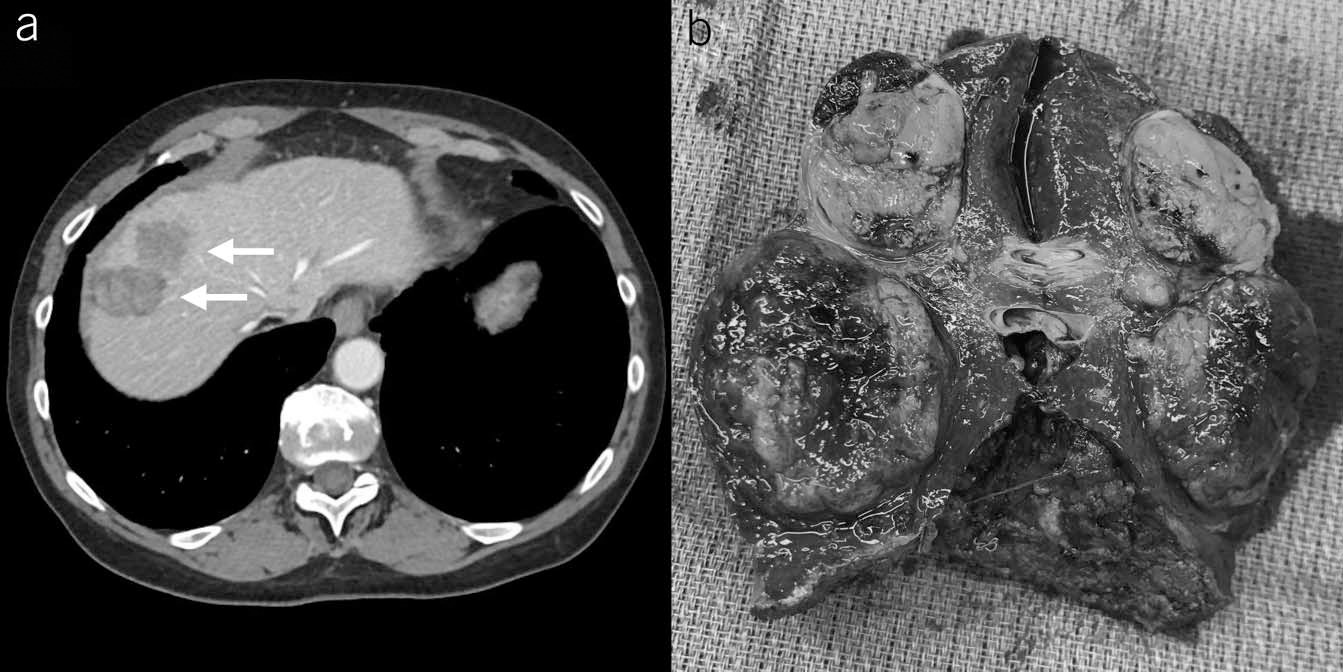
(a) Two masses (arrows) measuring 3.2 by 2.4 cm and 2.3 by 2.1 cm with a heterogeneous signal and washout of contrast. (b) Gross liver specimen including segments 4 and 8 measuring 9×9× 4 cm. A reddish-brown soft round mass measuring 3 × 3 × 2.5 cm and yellowish-gray oval firm mass measuring 2×2×1.5cm are visualized. An additional nodule measuring 1×0.8×30.8cm was identified by dissection (not visualized on gross specimen).
Figure 2.
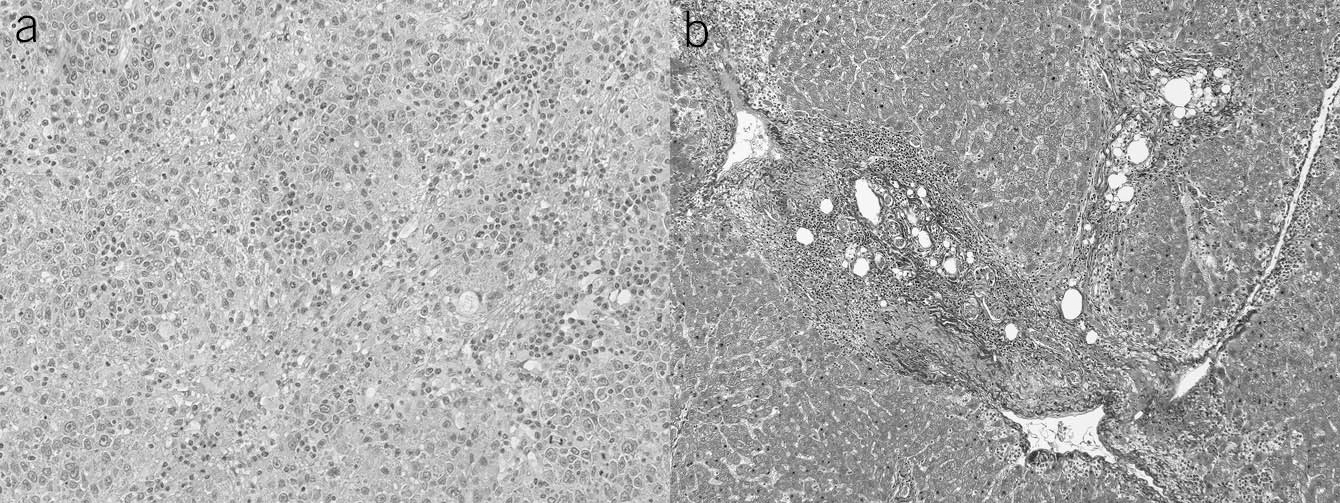
Histological analysis. (a) Hematoxylin and eosin stain (×200) of the tumor. Histologic type and grade: hepatocellular carcinoma, grade 4 undifferentiated. (b) Masson stain (×100) of a section of hepatic parenchyma taken away from the tumor shows bridging fibrosis, Ishak 3.
We describe a case of multifocal HCC in a noncirrhotic patient with long-standing AIH. Although he had normal routine laboratory testing, the patient’s inability to tolerate steroid sparing therapy may have contributed to the development of HCC. Although HCC is the most common primary liver cancer seen in adults, aside from chronic hepatitis B infection, it is rarely seen in chronic liver diseases. The development of HCC in noncirrhotic patients with AIH, although described, is rare. A recent meta-analysis of 6,528 patients with AIH reported that, at diagnosis, the pooled incidence of HCC was approximately 10 per 1,000 patient years, but only one patient did not have cirrhosis (1). This rare occurrence has only been described in 2 small Japanese cohorts where patients with AIH developed HCC in the absence of cirrhosis (2,3).
Generally, professional guidelines have recommended formal screening for HCC every 6 months in all patients who develop cirrhosis (4,5). Only certain patient populations such as chronic hepatitis B infection have been recommended for HCC screening outside of the presence of cirrhosis (4). The low incidence of HCC in patients with AIH lacking cirrhosis makes effective screening difficult with these patients more likely to present with a malignant mass with lymphovascular invasion. Therefore, we propose considering ordering alpha-fetoprotein and liver ultrasound in select patients with AIH who are on long-term steroid monotherapy.
Acknowledgments
Financial support: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. Grant Z99-DK999999.
Footnotes
CONFLICTS OF INTEREST
Potential competing interests: J.N.R.: None declared. C.A.L.G.: None declared. B.G.: None declared. W.R.S.: None declared. J.M.H.: None declared. C.K.: None declared.
Guarantor of the article: Christopher Koh, MD, MHSc.
Informed consent: Informed consent was obtained for this case report.
REFERENCES
- 1.Tansel A, Katz LH, El-Serag HB, et al. Incidence and determinants of hepatocellular carcinoma in autoimmune hepatitis: A systematic review and meta-analysis. Clin Gastroenterol Hepatol 2017;15(8):1207–17.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Watanabe T, Soga K, Hirono H, et al. Features of hepatocellular carcinoma in cases with autoimmune hepatitis and primary biliary cirrhosis. World J Gastroenterol 2009;15(2): 231–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ohira H, Abe K, Takahashi A, et al. Clinical features of hepatocellular carcinoma in patients with autoimmune hepatitis in Japan. J Gastroenterol 2013;48(1):109–14. [DOI] [PubMed] [Google Scholar]
- 4.Marrero JA, Kulik LM, Sirlin CB, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 Practice guidance by the American Association for the Study of Liver Diseases. Hepatology 2018; 68(2):723–50. [DOI] [PubMed] [Google Scholar]
- 5.Manns MP, Czaja AJ, Gorham JD, et al. Diagnosis and management of autoimmune hepatitis. Hepatology 2010;51(6):2193–213. [DOI] [PubMed] [Google Scholar]


