Abstract
Background:
Soft tissue laxity around the knee joint has been recognized as a crucial factor affecting correction error during medial open-wedge proximal tibial osteotomy (MOWPTO). Medial laxity in particular, which represents the changes in joint-line convergence angle (JLCA), affects soft tissue correction.
Purpose:
The purpose of this study was to quantify medial laxity and develop a preoperative planning method that considers medial laxity.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
This study retrospectively reviewed 139 knees in 117 patients who underwent navigation-assisted MOWPTO from January 2014 to July 2019 for symptomatic medial compartment osteoarthritis with varus alignment >5°. We compared the results of 2 preoperative planning methods: conventional Miniaci (n = 47) and latent medial laxity reduction (LMLR) (n = 92). We evaluated the incidence of undercorrection, acceptable correction, and overcorrection. The radiologic parameters were analyzed using multiple linear regression with a stepwise selection model to establish an equation for the optimal preoperative planning method. The intraclass correlation coefficients (ICCs) of intraobserver, interobserver, and intermethod reliability were calculated.
Results:
The Miniaci method showed a higher incidence of overcorrection (55.3%) than the LMLR method (22.8%) at postoperative 6 months (P = .0006). Multiple linear regression with a stepwise selection model revealed a high correlation coefficient (R 2 = 0.888) for the following equation: Adjusted planned correction angle = 0.596 + 0.891 × Target correction angle – 0.255 × ΔJLCA valgus . Upon simplification, the following equation showed the highest intermethod ICC value (0.991): Target correction angle – ⅓ΔJLCA valgus , while the Miniaci method showed a relatively low ICC value of 0.875.
Conclusion:
There was a risk of overcorrection after MOWPTO using the conventional Miniaci method. An equation that considers medial laxity may help during preoperative planning for optimal correction during MOWPTO.
Keywords: medial laxity, proximal tibial osteotomy, preoperative planning, correction error
Medial open-wedge proximal tibial osteotomy (MOWPTO) is an established surgical procedure for early medial compartment osteoarthritis in relatively active patients. 7,21,27 Clinical outcomes depend on the accurate correction of postoperative lower limb alignment. 3,42 Undercorrection could lead to deformity recurrence, whereas overcorrection could cause lateral compartment osteoarthritis, poor cosmetic outcomes, and poor functional outcomes including gait problems. 5,18,27,39,41 Although several techniques for preoperative correction planning have been introduced to obtain accurate alignment, 1,6,26,30,34,45 unexpected correction errors remain unresolved. 4,9,22,24
The factors associated with coronal correction errors in MOWPTO are still unclear. The extent of bony correction does not correlate with the correction error. 22 Coronal alignment correction errors may be due to the low reproducibility of intraoperative assessment tools, including navigation and fluoroscopy-based methods. 27,30 Soft tissue laxity around the knee joint has recently been recognized as a crucial factor affecting correction error. 17,25,27,28,37 –39 Some previous studies have noted that medial and lateral soft tissue laxity could affect coronal correction error. 37,39 While medial soft tissue laxity is widely accepted as having a crucial effect on soft tissue correction during MOWPTO, controversial findings have been reported for the effect of lateral laxity. 25,37,43
The most common method for quantifying soft tissue laxity is to measure the changes in the joint-line convergence angle (JLCA). 11,25,27 Lee et al 27 indicated that changes in JLCA correlated with correction errors and that a large JLCA change correlated with overcorrection. Heijens et al 11 also reported that the bony correction in MOWPTO is accompanied by additional JLCA changes by stretching the medial soft tissue. Park et al 37 noted that overcorrection was more likely to occur in cases presenting a ≥4° JLCA and a ≥1.5° valgus stress angle. However, the amount of reduction of the correction angle required during preoperative planning, in terms of medial soft tissue laxity, remains unknown. 19,37
The purpose of this study was to (1) quantify medial laxity and develop a preoperative planning method that considers medial laxity and (2) develop an equation to reduce coronal correction error in terms of preoperative medial soft tissue laxity. The hypothesis of this study was that the conventional Miniaci preoperative planning method has a risk of overcorrection for MOWPTO as compared with a method for medial soft tissue laxity reduction planning.
Methods
Study Sample
This study was a retrospective review of 154 knees in 131 patients who underwent navigation-assisted MOWPTO from January 2014 to July 2019 for symptomatic medial compartment osteoarthritis with varus alignment >5°. Among these consecutive patients, we excluded those with a history of knee ligament injury (6 knees), revision operations attributed to revarization after MOWPTO (3 knees), cosmetic surgeries (2 knees), and those lost to follow-up within 6 months after surgery (2 knees). Additionally, 2 knees subjected to conventional MOWPTO (using fluoroscopy and rod method) were excluded because of unstable navigation transmitter sensing.
Ultimately, 139 knees (117 patients) were included in this study (Figure 1). The study protocol was approved by the institutional review board at Samsung Medical Center.
Figure 1.
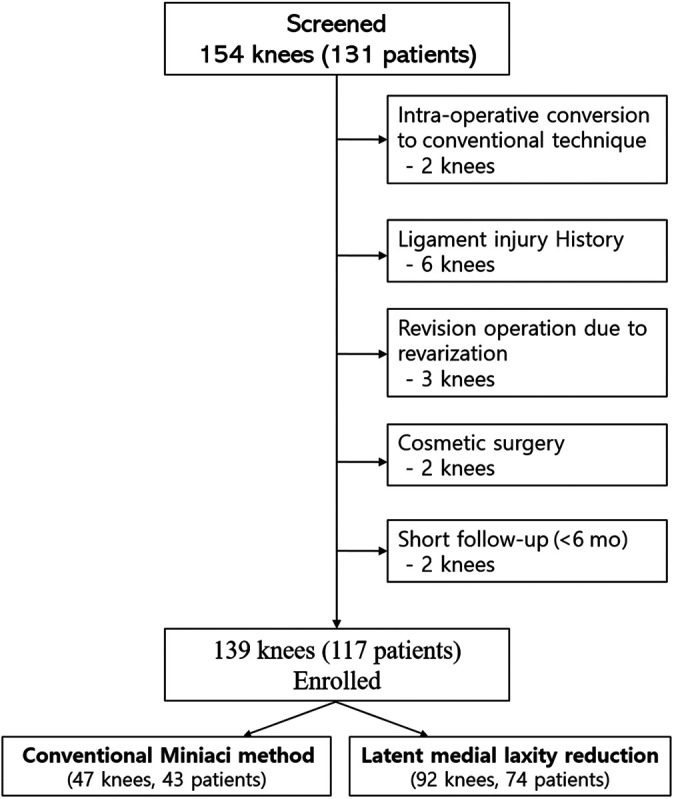
Flowchart showing exclusion of the study participants.
Surgical Procedure and Postoperative Protocols
The surgical procedures were performed as previously described by Kyung et al. 22 The OrthoPilot Navigation System HTO Version 2.1 (Aesculap) was used to confirm intraoperative coronal alignment. All MOWPTO procedures were performed by a single senior knee surgeon (J.H.W.). The targeted postoperative mechanical axis (MA) was 3° valgus of the absolute value of the preoperative mechanical axis (MA); the amount of coronal correction was determined preoperatively by standing whole-leg, varus stress, and valgus stress radiographs 23 (Figure 2).
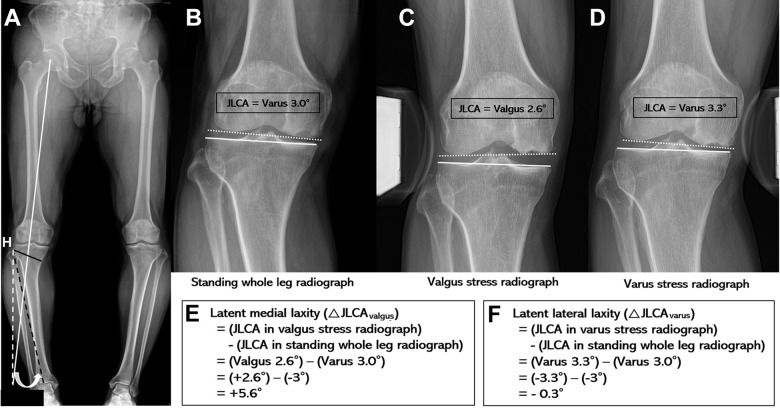
Figure 2.
(A) Preoperative planning using the Miniaci method. H, hinge point. White line: an extension line connecting the hip center and the calculated point of expected weightbearing line after osteotomy. Black dashed line: a line connecting the lateral tibial hinge site, H, and the center of the ankle joint. White dashed line: a line connecting the lateral tibial hinge site, H, and white line. White arrow: the angle formed by black dashed line and white dashed line, determined to be the predicted correction angle. Black line: planned osteotomy site. (B-F) Calculation of latent medial laxity and lateral laxity. White dotted line: a line tangential to the distal femoral condyle. White line: a line tangential to the tibial plateau. JLCA, joint-line convergence angle (angle formed between white dotted line and white line). If the apex of the JLCA was medial, it was recorded as negative (–, varus); if it was lateral, it was recorded as positive (+, valgus).
The MA was defined as the angle subtended by a line drawn from the center of the femoral head to the center of the knee and a line drawn from the center of the knee to the center of the talus. To evaluate soft tissue laxity on the coronal plane, the JLCA was measured as the angle between the line connecting the distal femur and the proximal tibial articular surfaces on standing whole-leg radiographs (Figure 2, B-D). 10,27,40
If the apex of the JLCA was medial, it was recorded as negative and denoted as varus; if it was lateral, it was recorded as positive and denoted as valgus. Latent medial laxity was calculated by subtracting the JLCA on weightbearing standing radiographs from the JLCA on valgus stress radiographs and was denoted as ΔJLCAvalgus (Figure 2E). 25 Latent lateral laxity was calculated by subtracting the JLCA on weightbearing standing radiographs from the JLCA on varus stress radiographs and was denoted as ΔJLCAvarus (Figure 2F).
From January 2014 to November 2015, we used the Miniaci method for preoperative planning. The preoperative Miniaci method correction angle was determined using the target point with the weightbearing line passing through 62.5% of the tibial plateau. 32 The predicted correction angle was determined as the angle formed by a line connecting the lateral tibial hinge site and the center of the ankle joint and an extended line from the lateral tibial hinge site to the expected weightbearing line after osteotomy (Figure 2A).
After November 2015, we used an alternate formula that considered latent medial laxity 25,27 :
where the targeted correction angle (TCA) was 3° valgus of the absolute value of the preoperative MA. This was named the latent medial laxity reduction (LMLR) method.
The navigational MA was obtained and recorded after registration of the navigation (Figure 3A). The navigational MA was measured as the operator held the patient’s second toe to lift the whole limb slightly from the operating table, without any valgus or varus force applied to knee joint. 40
Figure 3.
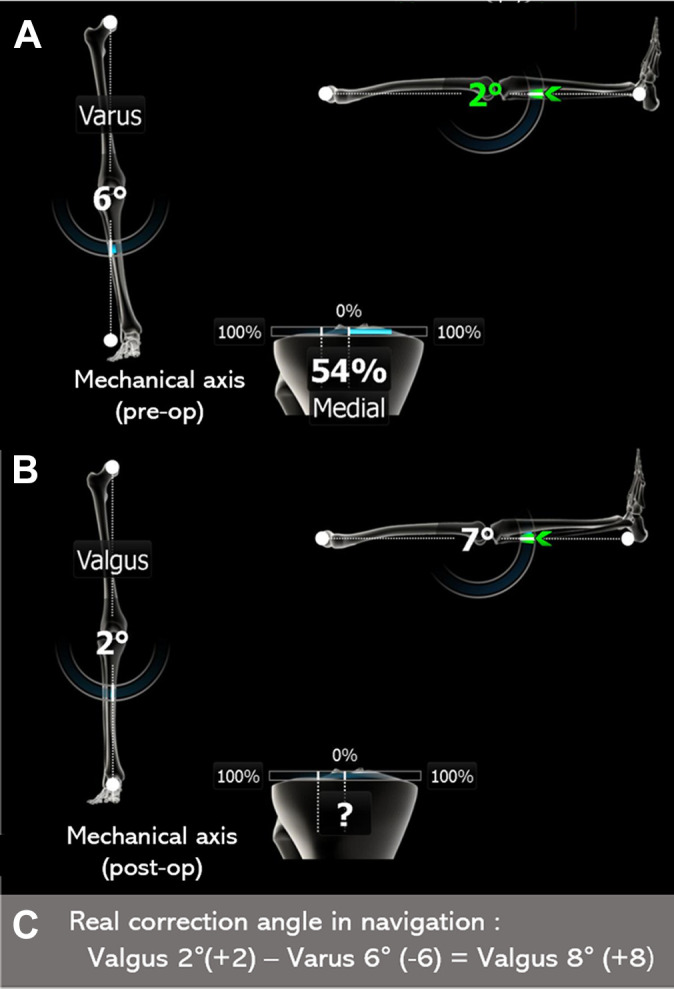
Measurement of the real correction angle in the navigation system. The real correction angle was confirmed as the difference between the (A) pre- and (B) postoperative hip-knee-ankle angles in the navigation system, as calculated in panel C.
The distal portion of the superficial medial collateral ligament was transected at the tibia along the planned osteotomy line. All MOWPTOs were performed in a biplanar fashion. Using real-time information from the navigation system, a planned coronal correction was made, and the proximal tibia was fixed using a locking plate (TomoFix; DePuy Synthes). The postoperative navigational MA was obtained and recorded after completion of the plate fixation (Figure 3B). We filled the osteotomy gap with an allograft cancellous chip bone (Korea Bone Bank). The difference between the pre- and postoperative navigational MA was defined as the real correction angle (RCA) (Figure 3C). Although we believed in the accuracy of intraoperative navigation, we rely more on the “degree of change” than the navigational MA itself. Thus, in situations where the preoperative MA showed 6° varus and the postoperative limb axis showed 2° valgus in navigation, the RCA was 8° valgus regardless of the preoperative navigational MA. 25,40
The age, weight, preoperative MA angle and JLCA on radiographs, latent medial and lateral laxity, and RCA in the navigation system were analyzed to determine their effect on the postoperative change in the MA.
The patients were allowed to walk with clutch and toe-touch weightbearing on the operated limb immediately after the operation. Exercise with full range of motion was started on the second postoperative day. From the second postoperative week, the patients were instructed to increase the amount of weightbearing on the operated limb gradually through the next 4 weeks. The patients visited the outpatient clinic at 6 weeks, 3 months, and 6 months postoperatively.
Radiographic Measurements
Standing whole-leg anteroposterior radiographs of both legs were obtained preoperatively and at 3 and 6 months postoperatively (Figure 4). Preoperatively, the Telos stress device (Metax GmbH) was used to evaluate soft tissue laxity. The preoperative varus stress and valgus stress views of the knee joint were obtained in full extension and the supine position, respectively, with a varus and valgus force of 15 kgf at the joint-line level. 25
Figure 4.
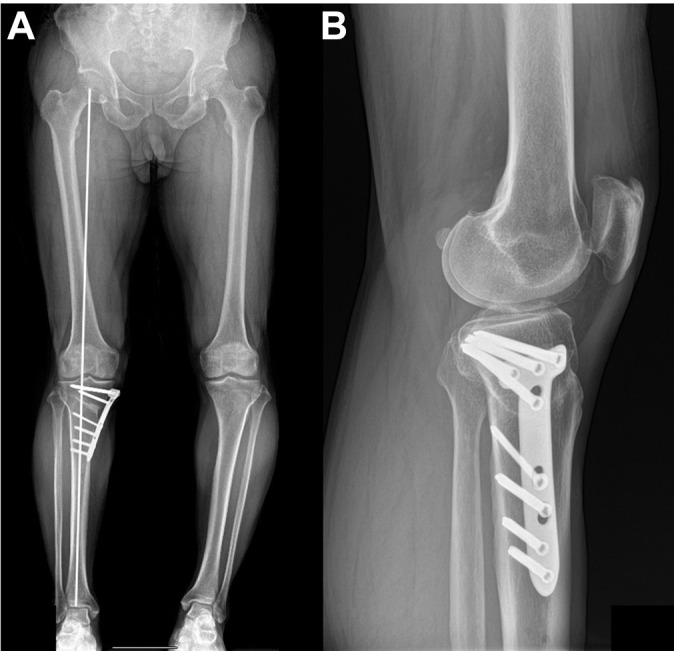
Representative postoperative (A) standing whole-leg and (B) lateral radiographs using latent medial laxity reduction planning method at 6 months. The white line in panel A indicates the weightbearing axis.
Varus and valgus alignments were recorded as negative and positive values, respectively. The final surgical target was 3° valgus of MA. The coronal correction discrepancy of the MA within a valgus range of 1.5° to 4.5° (valgus 3° ± 1.5°) was defined as an acceptable correction, whereas corrections <1.5° and >4.5° were defined as undercorrection and overcorrection, respectively.
These factors were measured using a digitized picture archiving and communication system (Centricity 6.0 SP9; GE Healthcare), and the magnification was automatically corrected in the program.
Statistical Analysis
We used a 2 × 3 chi-square test to evaluate the incidence of undercorrection, acceptable correction, and overcorrection between the Miniaci and LMLR planning methods. We selected the acceptable correction cases from the total cases, regardless of the planning method. Pearson correlation analysis was performed to confirm correlation between (1) the JLCA, latent medial laxity (ΔJLCAvalgus), latent lateral laxity (ΔJLCAvarus), and TCA and (2) acceptable correction. Statistical significance was defined as P < .05.
Multiple linear regression with a stepwise selection was performed on the selected statistically significant factors. The eligibility criterion for the predictive model was P < .05. If the P value of the variable was >.05, the variable was considered an explicative variable, and it was excluded from the model. In multiple linear regression analysis, α is a constant, and the β coefficient denotes the affecting power of each variable. 29 The selected final model was presented with β coefficients, P values, and adjusted coefficients of determination (R 2). The discrepancy between the expected value and the observed value was evaluated using standardized residuals. Statistical analysis was performed using SPSS Version 25.0 (IBM Corp).
Finally, we compared the selected final regression model with the Miniaci and LMLR methods using intermethod reliability. 2,16 LMLR equations were as follows, with the value subtracted from the TCA determined according to the degree of ΔJLCAvalgus:
The intermethod intraclass correlation coefficient (ICC) was used to evaluate the correction values calculated by the final regression model, Miniaci method, and each LMLR model. The intermethod ICC is a kind of interobserver ICC; however, the subject of the observer is each planning method.
Two trained orthopaedic surgeons (D.J.R and J.H.K.) independently measured radiographic parameters at intervals of 3 weeks between the measurements. The ICC was used to determine intra- and interobserver reliability, with values >0.75 considered good. 20 The average value of the measurements was used in the analysis. An ICC value >0.8 was adopted for the reliability of the statistical analysis. The results of the intra- and interobserver reliabilities of each measurement are described in Appendix Table A1. All of the parameters showed good correlation.
A post hoc test was performed to determine the sample size by G power (Version 3.1; Institut für Experimentelle Psychologie, Heinrich Heine Universität) by a multiple linear regression test with an α error of 0.05 and power of 0.8. 8,29 The calculations, based on a sample size of 84 knees showing acceptable correction, indicated this study had adequate power (0.89) to detect a significant difference in the measurement outcomes.
Results
The mean pre- and postoperative MAs were –8.46° (range, –5.0° to –18.8°) and 3.97° (range, –1.5° to 10.4°), respectively. The mean 6-month postoperative MA of the Miniaci group was 4.87°, which was significantly different from that of the LMLR group (3.51°) (P = .001). The mean ΔJLCAvalgus was 4.66°, with no significant difference between the Miniaci and LMLR groups. The detailed radiographic parameter results are summarized in Table 1.
Table 1.
Characteristics and Radiographic Parameters a
| Knees, Mean (Range) | ||||
|---|---|---|---|---|
| Total (N = 139) | Miniaci Method (n = 47) | LMLR Method (n = 92) | P Value | |
| Age, y | 54.4 (33 to 65) | 53.66 (33 to 64) | 54.78 (36 to 65) | .378 |
| Male:female b | 48:91 | 13:34 | 35:57 | .223 |
| MA on standing XR, deg c | ||||
| Preoperative | –8.46 (–5.0 to –18.8) | –7.83 (–5.1 to –12.7) | –8.78 (–5.0 to –18.8) | .071 |
| 6-mo postoperative | 3.97 (–1.5 to 10.4) | 4.87 (–1.5 to 9.8) | 3.51 (–1.1 to 10.4) | .001 |
| JLCA, deg c | ||||
| On standing-leg XR | –3.52 (–12.8 to 1.1) | –3.24 (–8.4 to –0.2) | –3.67 (–12.8 to 1.1) | .255 |
| On valgus stress XR | 1.13 (–2.2 to 7.6) | 1.19 (–1.5 to 5.7) | 1.10 (–2.2 to 7.6) | .768 |
| On varus stress XR | –5.18 (–12.1 to –0.9) | –4.88 (–8.7 to –0.9) | –5.34 (–12.1 to –1.0) | .162 |
| ΔJLCAvalgus, deg c | 4.66 (0.8 to 16.8) | 4.44 (0.8 to 10.1) | 4.78 (1.2 to 16.8) | .428 |
| ΔJLCAvarus, deg c | –1.67 (–4.4 to 0.7) | –1.63 (–3.3 to –0.3) | –1.68 (–4.4 to 0.7) | .809 |
| RCA, deg | 9.94 (6.0 to 20.0) | 10.23 (6.0 to 16.0) | 9.79 (6.0 to 20.0) | .338 |
| TCA, deg | 11.46 (8.0 to 21.80) | 10.83 (8.1 to 15.7) | 11.78 (8.0 to 21.8) | .071 |
a Bold P value indicates statistically significant difference between methods (P < .05). JLCA, joint-line convergence angle; ΔJLCA, difference in JLCA between standing and valgus stress radiograph; LMLR, latent medial laxity reduction; MA, mechanical axis; RCA, real correction angle; TCA target correction angle; XR, radiograph.
b No. of knees.
c Positive values denote valgus alignment, and negative values denote varus alignment.
Overall, 19 of 47 knees (39.6%) subjected to the Miniaci method and 65 of 92 knees (69.9%) subjected to the LMLR method achieved acceptable correction. This difference was statistically significant (χ2[3, N = 139] = 14.69; P = .0006) (Table 2). The Miniaci method showed a higher incidence of over-correction (55.3%) than the latent medial laxity reduction method (22.8%). There was a significant difference in the acceptable:overcorrected ratio between the planning methods (χ2[2, n = 131] = 14.29; P = .00015). However, there was no significant difference for the acceptable:undercorrected ratio (χ2[2, n = 55] = 2.514; P = .112) (Figure 5).
Table 2.
Postoperative Mechanical Axis Outcomes After Each Planning Method a
| Total | Miniaci Method | LMLR Method | P Value | |
|---|---|---|---|---|
| Acceptable b | 84 | 19 | 65 | .0006 |
| Overcorrection | 47 | 26 | 21 | |
| Undercorrection | 8 | 2 | 6 |
a Bold P value indicates statistically significant difference between methods (P < .05). LMLR, latent medial laxity reduction.
b Defined as mechanical axis within a valgus range of 1.5° to 4.5°.
Figure 5.
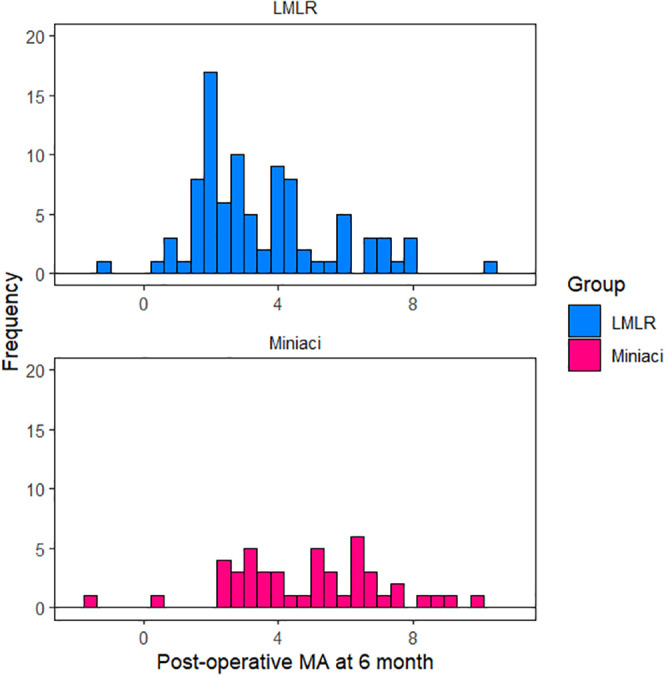
Distribution of mechanical axis (MA) values in each preoperative planning method at 6 months postoperatively. LMLR, latent medial laxity reduction.
In a subgroup analysis of high-grade latent medial laxity (ΔJLCAvalgus >5.5°), the 2 planning methods demonstrated a significant difference for acceptable correction (χ2[2, n = 48] = 11.07; P = .0008). Additionally, a significant difference occurred between the correction methods at middle- or low-grade latent medial laxity (ΔJLCAvalgus <5.5°) (χ2[2, n = 83] = 5.67; P = .017) (Table 3).
Table 3.
Subgroup Analysis According to ΔJLCAvalgus a
| Method, n (%) | |||
|---|---|---|---|
| ΔJLCAvalgus | Miniaci | LMLR | P Value |
| >5.5° | .0008 | ||
| Acceptable correction | 3 (21.4) | 25 (73.5) | |
| Overcorrection | 11 (78.6) | 9 (26.5) | |
| <5.5° | .017 | ||
| Acceptable correction | 16 (51.6) | 40 (76.9) | |
| Overcorrection | 15 (48.4) | 12 (23.1) | |
a Bold P values indicate statistically significant difference between methods (P < .05). JLCA, joint-line convergence angle; ΔJLCA, difference in JLCA between standing-leg and valgus stress radiographs; LMLR, latent medial laxity reduction.
Among all cases, 84 knees within the acceptable range after MOWPTO were analyzed using Pearson correlation analysis. The standing JLCA (P < .0001), latent medial laxity (ΔJLCAvalgus; P = .001), and TCA (P < .0001) were all significantly correlated with the RCA. The latent lateral laxity (ΔJLCAvarus) was not significantly correlated with RCA (P = .091). Using multiple linear regression with a stepwise selection model, we set a prediction model for the accurate postoperative MA of the lower limb. The adjusted planning correction angle equation that was established with statistically correlated factors using the multiple regression test was as follows:
The observed data were highly correlated with the expected data for TCA and ΔJLCAvalgus in the standardized residuals (R = 0.942, R 2 = 0.888, adjusted R 2 = 0.885; P < .05) (Table 4).
Table 4.
Multiple Linear Regression Analysis of the Real Correction Angle a
| Unstandardized Coefficients | Standardized Coefficients | |||
|---|---|---|---|---|
| DV: Explicative Variable | B | SE (B) | ß | P Value |
| RCA | ||||
| Constant | 0.596 | 0.376 | .117 | |
| TCA | 0.891 | 0.036 | 1.005 | <.0001 |
| ΔJLCAvalgus | –0.255 | 0.046 | –0.221 | <.0001 |
aR = 0.942, R 2 = 0.888, adjusted R 2 = 0.885; P < .05. Bold P values indicate statistical significance (P < .05). DV, dependent variable; JLCA, joint-line convergence angle; ΔJLCA, difference in JLCA between standing-leg and valgus stress radiographs; RCA, real correction angle; TCA, target correction angle.
The intermethod ICC was calculated for each method and evaluated accordingly (Table 5). Results indicated that the simplified equation, TCA – ⅓ΔJLCA valgus , showed the highest ICC value (0.991 [95% CI, 0.987-0.994]; P < .0001). The Miniaci method had a lower ICC value (0.875 [95% CI, 0.814-0.917]; P < .0001).
Table 5.
Intermethod ICC Values of Each Simplified Formula Versus Ideal Correction Angle Method a
| DV: Explicative Variable | Intermethod ICC (95% CI) b |
|---|---|
| Regression value | |
| Miniaci | 0.881 (0.822-0.921) |
| TCA – ΔJLCAvalgus | 0.819 (0.733-0.879) |
| TCA – ½ΔJLCAvalgus | 0.976 (0.964-0.985) |
| TCA – ⅓ΔJLCAvalgus | 0.992 (0.988-0.995) |
a DV, dependent variable; ICC, intraclass correlation coefficient; JLCA, joint-line convergence angle; ΔJLCAvalgus difference in JLCA between standing-leg and valgus stress radiographs; TCA, target correction angle.
b Each ICC value, P < .0001.
Discussion
The most important finding of this study was that the Miniaci method has a tendency for coronal overcorrection during MOWPTO, especially for those with high-grade latent medial laxity (ΔJLCAvalgus >5.5°). Preoperative correction planning that considers latent medial laxity should be used. We suggest the following equation:
Through adjusted planning, we can reduce the risk of overcorrection in case of postoperative targeting Fujisawa point (weight-bearing line to 62–66% of the width of the plateau) or a valgus of 3°.
The effects of soft tissue laxity on coronal correction error after MOWPTO have been reported in previous studies. 19,25,27,37,40 Ogawa et al 35 stated that the JLCA could be changed by shifting the weightbearing axis from medial to lateral and by stretching the medial soft tissue. Lee et al 27 also found that a large change in JLCA from before and after MOWPTO may suggest alignment overcorrection. The change in JLCA value between pre- and postoperative alignment correlated with overcorrection; however, this value could not be used preoperatively to plan for MOWPTO. 19 Through this study, we tried to quantify medial laxity using the concept of latent medial laxity 25 and developed a preoperative planning method that considered medial laxity. Therefore, this study has important implications for improving the accuracy of postoperative coronal alignment after MOWPTO.
In normal knees, the JLCA ranges from 0° to 2°. 13 However, the parallel JLCA differs in patients with medial osteoarthritis because of varus alignment, with pseudolaxity of the lateral side resulting from substantial amounts of intra-articular cartilage loss in the medial compartment. 27,36 In medial laxity knees with varus alignment, the difference in values between JLCA while standing and on application of valgus force could be significantly large. Preoperative valgus stress can mimic the postoperative valgization status of the proximal tibia. Thus, we can assume that the difference in values between JLCA while standing and on application of valgus stress is similar to latent medial laxity.
There is consensus on the effect of medial laxity and varus angular deformity 6 (JLCA in this study) on overcorrection, but the relevance of latent lateral laxity is still controversial. 25,37 Based on our previous study 25 and this study, the concept of latent medial laxity, which is reflected in medial soft tissue laxity and adduction moment, is a crucial factor in correction error. Latent lateral laxity was found to be a confounding factor. In this study, we developed a preoperative planning method that considers medial laxity while excluding the controversial factors. Although there is no clear study on the quantifying effect of medial laxity, Kim et al 19 reported that 1° of valgus overcorrection was related to every 2.5° of JLCA. Park et al 37 also noted that an MA value of 1.3° is almost equal to a mean JLCA change of 1.2°. Considering these values, we developed a simple formula of subtracting one-half or one-third of the JLCA from the TCA. This simplified formula had an excellent ICC with the ideal formula according to multiple linear regression analysis, and it is easy to apply in preoperative planning in case of postoperative targeting Fujisawa point (weight-bearing line to 62–66% of the width of the plateau)or a valgus of 3°.
Our study had several limitations. First, there is a risk of selection bias owing to the retrospective design. Second, this study reviewed patients from a single institution and by a single surgeon (J.H.W.). Additional studies are required to apply the formula for different TCAs, according to each patient’s medial compartment status. 18 Third, all parameters except navigation were measured on plain radiographs. The accuracy of the parameters is strongly affected by patient position, especially in patients with flexion contractures; that is, errors deriving from the rotation error remain. Fourth, surgical procedures including medial soft tissue release and differences in soft tissue laxity may have affected the results. Fifth, although navigation is known to be reliable, 22,40 it could lead to errors if some of the references are not adequate.
A sixth limitation is that the postoperative target of 3° valgus of the MA is debatable. For a long time, the widely accepted concept was that correction of 3° to 5° valgus of the MA was essential to achieve satisfactory outcomes. 12,14 Recently, there has been concern about lateral compartment osteoarthritis, poor cosmetics, and poor functional outcomes, including gait problems, attributed to overcorrection. 5,18,39,41 Jakob et al 15 suggested that correction of the MA should depend on the thickness of the remaining medial compartment cartilage. A recent biomechanical study showed that overcorrection of >3° valgus of the MA presents no advantage in unloading the medial compartment peak pressure. 31,44 Kim et al 18 also reported that correction to neutral or <3° valgus could be effective and safe in MOWPTO with concomitant cartilage procedures. We did not look at patient outcomes or functional reports after our surgical procedures. Although this is very important to demonstrate the clinical significance, it was not a part of the purpose of our study. Another limitation was that the valgus JLCA was measured on anteroposterior radiographs instead of standing whole-leg radiographs, as there was no definite protocol to reproduce constant valgus force with the standing position. Thus, there is a risk of error for measuring the valgus JLCA. 10 Finally, we did not evaluate the changes in tibial slope, which is another important alignment factor. 34,33
Conclusion
The conventional Miniaci method has the risk of coronal overcorrection after MOWPTO. An equation that considers medial laxity can facilitate a preoperative plan for optimal correction during MOWPTO.
Appendix
Table A1.
Results of ICC Values of Each Measurement of Radiological Parameters a
| ICC (95% CI) b | ||
|---|---|---|
| Interobserver | Intraobserver | |
| Mechanical axis | ||
| Preoperative | 0.979 (0.970-0.985) | 0.989 (0.985-0.992) |
| 6 mo postoperative | 0.976 (0.966-0.983) | 0.986 (0.980-0.991) |
| JLCA radiograph | ||
| Standing leg | 0.961 (0.946-0.972) | 0.980 (0.972-0.986) |
| Valgus stress | 0.954 (0.936-0.967) | 0.975 (0.967-0.983) |
| Varus stress | 0.956 (0.940-0.968) | 0.965 (0.958-0.971) |
| ΔJLCA | ||
| Valgus: latent medial laxity | 0.945 (0.923-0.960) | 0.972 (0.960-0.980) |
| Varus: latent lateral laxity | 0.949 (0.933-0.961) | 0.953 (0.941-0.963) |
a A measurement was considered reliable if the ICC was >0.80. ICC, intraclass correlation coefficient; JLCA, joint-line convergence angle.
b Each ICC value, P < .001.
Footnotes
Final revision submitted March 21, 2021; accepted April 14, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: This research was supported by the Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Science and ICT (NRF-2017R1A2B3007362 and 2015R1A2A1A15054779 to J.H.W.). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Samsung Medical Center (2020-05-004-001).
References
- 1. Akamatsu Y, Mitsugi N, Mochida Y, et al. Navigated opening wedge high tibial osteotomy improves intraoperative correction angle compared with conventional method. Knee Surg Sports Traumatol Arthrosc. 2012;20(3):586–593. doi:10.1007/s00167-011-1616-8 [DOI] [PubMed] [Google Scholar]
- 2. Allen S, Parent E, Khorasani M, Hill DL, Lou E, Raso JV. Validity and reliability of active shape models for the estimation of Cobb angle in patients with adolescent idiopathic scoliosis. J Digit Imaging. 2008;21(2):208–218. doi:10.1007/s10278-007-9026-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bito H, Takeuchi R, Kumagai K, et al. A predictive factor for acquiring an ideal lower limb realignment after opening-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2009;17(4):382–389. doi:10.1007/s00167-008-0706-8 [DOI] [PubMed] [Google Scholar]
- 4. Brouwer RW, Bierma-Zeinstra SMA, van Raaij TM, Verhaar JAN. Osteotomy for medial compartment arthritis of the knee using a closing wedge or an opening wedge controlled by a Puddu plate: a one-year randomised, controlled study. J Bone Joint Surg Br. 2006;88(11):1454–1459. doi:10.1302/0301-620X.88B11.17743 [DOI] [PubMed] [Google Scholar]
- 5. Dowd GSE, Somayaji HS, Uthukuri M. High tibial osteotomy for medial compartment osteoarthritis. Knee. 2006;13(2):87–92. doi:10.1016/j.knee.2005.08.002 [DOI] [PubMed] [Google Scholar]
- 6. Dugdale TW, Noyes FR, Styer D. Preoperative planning for high tibial osteotomy: the effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop Relat Res. 1992;274:248–264. [PubMed] [Google Scholar]
- 7. El-Azab HM, Morgenstern M, Ahrens P, Schuster T, Imhoff AB, Lorenz SGF. Limb alignment after open-wedge high tibial osteotomy and its effect on the clinical outcome. Orthopedics. 2011;34(10):e622–e628. doi:10.3928/01477447-20110826-02 [DOI] [PubMed] [Google Scholar]
- 8. Faul F, Erdfelder E, Buchner A, Lang A-G. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–1160. doi:10.3758/BRM.41.4.1149 [DOI] [PubMed] [Google Scholar]
- 9. Gaasbeek RDA, Nicolaas L, Rijnberg WJ, van Loon CJM, van Kampen A. Correction accuracy and collateral laxity in open versus closed wedge high tibial osteotomy: a one-year randomised controlled study. Int Orthop. 2010;34(2):201–207. doi:10.1007/s00264-009-0861-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Graden NR, Dean RS, Kahat DH, DePhillipo NN, LaPrade RF. True mechanical alignment is found only on full-limb and not on standard anteroposterior radiographs. Arthrosc Sports Med Rehabil. 2020;2(6):e753–e759. doi:10.1016/j.asmr.2020.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Heijens E, Kornherr P, Meister C. The coronal hypomochlion: a tipping point of clinical relevance when planning valgus producing high tibial osteotomies. Bone Joint J. 2016;98(5):628–633. doi:10.1302/0301-620X.98B5.33394 [DOI] [PubMed] [Google Scholar]
- 12. Hernigou P, Medevielle D, Debeyre J, Goutallier D. Proximal tibial osteotomy for osteoarthritis with varus deformity: a ten to thirteen-year follow-up study. J Bone Joint Surg Am. 1987;69(3):332–354. [PubMed] [Google Scholar]
- 13. Higuchi T, Koseki H, Yonekura A, et al. Comparison of radiological features of high tibial osteotomy and tibial condylar valgus osteotomy. BMC Musculoskelet Disord. 2019;20(1):409. doi:10.1186/s12891-019-2764-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ivarsson I, Myrnerts R, Gillquist J. High tibial osteotomy for medial osteoarthritis of the knee: a 5 to 7 and 11 year follow-up. J Bone Joint Surg Br. 1990;72(2):238–244. [DOI] [PubMed] [Google Scholar]
- 15. Jakob RP, Jacobi M. Closing wedge osteotomy of the tibial head in treatment of single compartment arthrosis. Article in German. Orthopade. 2004;33(2):143–152. doi:10.1007/s00132-003-0600-5 [DOI] [PubMed] [Google Scholar]
- 16. Kenawey M, Hasan NMA, Saleh S, El-Deen MA, Abdel Aziz AH, Shiha A. Intraobserver and intermethod reliability for using two different computer programs in preoperative lower limb alignment analysis. The Egyptian Journal of Radiology and Nuclear Medicine. 2016;47(4):1515–1519. doi:10.1016/j.ejrnm.2016.09.005 [Google Scholar]
- 17. Kim H-J, Lee H-J, Shin J-Y, Park K-H, Min S-G, Kyung H-S. Preoperative planning using the picture archiving and communication system technique in high tibial osteotomy. J Orthop Surg (Hong Kong). 2017;25(1):23094 99016684701. doi:10.1177/2309499016684701 [DOI] [PubMed] [Google Scholar]
- 18. Kim MK, Ko BS, Park JH. The proper correction of the mechanical axis in high tibial osteotomy with concomitant cartilage procedures—a retrospective comparative study. J Orthop Surg Res. 2019;14(1):281. doi:10.1186/s13018-019-1333-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kim SH, Ro D-H, Lee Y-M, Cho Y, Lee S, Lee M-C. Factors associated with discrepancies between preoperatively planned and postoperative alignments in patients undergoing closed-wedge high tibial osteotomy. Knee. 2017;24(5):1129–1137. doi:10.1016/j.knee.2017.05.013 [DOI] [PubMed] [Google Scholar]
- 20. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163. doi:10.1016/j.jcm.2016.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Koshino T, Yoshida T, Ara Y, Saito I, Saito T. Fifteen to twenty-eight years’ follow-up results of high tibial valgus osteotomy for osteoarthritic knee. Knee. 2004;11(6):439–444. doi:10.1016/j.knee.2004.03.005 [DOI] [PubMed] [Google Scholar]
- 22. Kyung BS, Kim JG, Jang K-M, et al. Are navigation systems accurate enough to predict the correction angle during high tibial osteotomy? Comparison of navigation systems with 3-dimensional computed tomography and standing radiographs. Am J Sports Med. 2013;41(10):2368–2374. doi:10.1177/0363546513498062 [DOI] [PubMed] [Google Scholar]
- 23. Laprade RF, Bernhardson AS, Griffith CJ, Macalena JA, Wijdicks CA. Correlation of valgus stress radiographs with medial knee ligament injuries: an in vitro biomechanical study. Am J Sports Med. 2010;38(2):330–338. doi:10.1177/0363546509349347 [DOI] [PubMed] [Google Scholar]
- 24. Laprade RF, Spiridonov SI, Nystrom LM, Jansson KS. Prospective outcomes of young and middle-aged adults with medial compartment osteoarthritis treated with a proximal tibial opening wedge osteotomy. Arthroscopy. 2012;28(3):354–364. doi:10.1016/j.arthro.2011.08.310 [DOI] [PubMed] [Google Scholar]
- 25. Lee D kyung, Wang JH, Won Y, et al. Preoperative latent medial laxity and correction angle are crucial factors for overcorrection in medial open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2020;28(5):1411–1418. doi:10.1007/s00167-019-05502-6 [DOI] [PubMed] [Google Scholar]
- 26. Lee D-H, Han S-B, Oh K-J, et al. The weight-bearing scanogram technique provides better coronal limb alignment than the navigation technique in open high tibial osteotomy. Knee. 2014;21(2):451–455. doi:10.1016/j.knee.2012.09.003 [DOI] [PubMed] [Google Scholar]
- 27. Lee D-H, Park S-C, Park H-J, Han S-B. Effect of soft tissue laxity of the knee joint on limb alignment correction in open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2016;24(12):3704–3712. doi:10.1007/s00167-015-3682-9 [DOI] [PubMed] [Google Scholar]
- 28. Lee O-S, Lee ES, Lee YS. Disparity between preoperative target correction amount and postoperative correction amount in open wedge high tibial osteotomy. Knee Surg Relat Res. 2019;31(2):126–131. doi:10.5792/ksrr.18.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Marill KA. Advanced statistics: linear regression. Part II: multiple linear regression. Acad Emerg Med. 2004;11(1):94–102. doi:10.1197/j.aem.2003.09.006 [DOI] [PubMed] [Google Scholar]
- 30. Marti CB, Gautier E, Wachtl SW, Jakob RP. Accuracy of frontal and sagittal plane correction in open-wedge high tibial osteotomy. Arthroscopy. 2004;20(4):366–372. doi:10.1016/j.arthro.2004.01.024 [DOI] [PubMed] [Google Scholar]
- 31. Mina C, Garrett WE, Pietrobon R, Glisson R, Higgins L. High tibial osteotomy for unloading osteochondral defects in the medial compartment of the knee. Am J Sports Med. 2008;36(5):949–955. doi:10.1177/0363546508315471 [DOI] [PubMed] [Google Scholar]
- 32. Miniaci A, Ballmer FT, Ballmer PM, Jakob RP. Proximal tibial osteotomy: a new fixation device. Clin Orthop Relat Res. 1989;246:250–259. [PubMed] [Google Scholar]
- 33. Nha K-W, Kim H-J, Ahn H-S, Lee D-H. Change in posterior tibial slope after open-wedge and closed-wedge high tibial osteotomy: a meta-analysis. Am J Sports Med. 2016;44(11):3006–3013. doi:10.1177/0363546515626172 [DOI] [PubMed] [Google Scholar]
- 34. Noyes FR, Goebel SX, West J. Opening wedge tibial osteotomy: the 3-triangle method to correct axial alignment and tibial slope. Am J Sports Med. 2005;33(3):378–387. doi:10.1177/0363546504269034 [DOI] [PubMed] [Google Scholar]
- 35. Ogawa H, Matsumoto K, Ogawa T, Takeuchi K, Akiyama H. Preoperative varus laxity correlates with overcorrection in medial opening wedge high tibial osteotomy. Arch Orthop Trauma Surg. 2016;136(10):1337–1342. doi:10.1007/s00402-016-2521-x [DOI] [PubMed] [Google Scholar]
- 36. Pape D, Duchow J, Rupp S, Seil R, Kohn D. Partial release of the superficial medial collateral ligament for open-wedge high tibial osteotomy: a human cadaver study evaluating medial joint opening by stress radiography. Knee Surg Sports Traumatol Arthrosc. 2006;14(2):141–148. doi:10.1007/s00167-005-0649-2 [DOI] [PubMed] [Google Scholar]
- 37. Park J-G, Kim J-M, Lee B-S, Lee S-M, Kwon O-J, Bin S-I. Increased preoperative medial and lateral laxity is a predictor of overcorrection in open wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2020;28(10):3164–3172. doi:10.1007/s00167-019-05805-8 [DOI] [PubMed] [Google Scholar]
- 38. Park J-Y, Chang CB, Kang D-W, Oh S, Kang S-B, Lee MC. Development and validation of a prediction model for knee joint line orientation after high tibial osteotomy. BMC Musculoskelet Disord. 2019;20(1):434. doi:10.1186/s12891-019-2820-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sabzevari S, Ebrahimpour A, Roudi MK, Kachooei AR. High tibial osteotomy: a systematic review and current concept. Arch Bone Jt Surg. 2016;4(3):204–212. [PMC free article] [PubMed] [Google Scholar]
- 40. So S-Y, Lee S-S, Jung EY, Kim JH, Wang JH. Difference in joint line convergence angle between the supine and standing positions is the most important predictive factor of coronal correction error after medial opening wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2020;28(5):1516–1525. doi:10.1007/s00167-019-05555-7 [DOI] [PubMed] [Google Scholar]
- 41. Song SJ, Bae DK, Kim KI, Lee CH. Conversion total knee arthroplasty after failed high tibial osteotomy. Knee Surg Relat Res. 2016;28(2):89–98. doi:10.5792/ksrr.2016.28.2.89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Sprenger TR, Doerzbacher JF. Tibial osteotomy for the treatment of varus gonarthrosis: survival and failure analysis to twenty-two years. J Bone Joint Surg Am. 2003;85(3):469–474. [PubMed] [Google Scholar]
- 43. Takagawa S, Kobayashi N, Yukizawa Y, Oishi T, Tsuji M, Inaba Y. Preoperative soft tissue laxity around knee was associated with less accurate alignment correction after hybrid closed-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2020;28(9):3022–3030. doi:10.1007/s00167-019-05762-2 [DOI] [PubMed] [Google Scholar]
- 44. Van Thiel GS, Frank RM, Gupta A, et al. Biomechanical evaluation of a high tibial osteotomy with a meniscal transplant. J Knee Surg. 2011;24(1):45–53. doi:10.1055/s-0031-1275401 [DOI] [PubMed] [Google Scholar]
- 45. Yoon S-D, Zhang G, Kim H-J, Lee B-J, Kyung H-S. Comparison of cable method and miniaci method using picture archiving and communication system in preoperative planning for open wedge high tibial osteotomy. Knee Surg Relat Res. 2016;28(4):283–288. doi:10.5792/ksrr.16.052 [DOI] [PMC free article] [PubMed] [Google Scholar]