Abstract
Background
Controlling blood pressure (BP) is an international health concern, and high BP is a major contributor to cardiovascular disease mortality. Evidence has shown that educational interventions directed at patients potentially improve BP control and adherence to medications and lifestyle modifications. In addition, a text messaging intervention has a potential effect on BP control; however, the dosage of a text messaging intervention has not been determined in previous reviews, resulting in difficult application in practice.
Objective
This review aimed to identify the effectiveness of a text messaging intervention on hypertension management with a specific focus on the dosage of text messaging and the type of additional interventions with text messaging.
Methods
A systematic review was conducted and reported on in accordance with PRISMA guideline. Participants were aged 18 years and older and diagnosed with primary hypertension. The included studies used text messaging as a component of the intervention. We searched for randomized controlled trials published until June 30, 2020, from the following health-related electronic databases: Embase, Medline, CINAHL Complete, PsycINFO, and Scopus. Data were extracted for qualitative synthesis and meta-analysis. The Physiotherapy Evidence Database Scale was used to assess the methodological quality of each study, and the quality of the included studies was assessed independently by two authors.
Results
Twelve studies met the inclusion criteria. The overall methodological quality was fair (mean score 5.75). The frequency of text message delivery varied from daily to biweekly. Health education was identified in 4 studies as an additional intervention with text messaging. The overall results showed that the text messaging intervention significantly reduced systolic BP (SBP) but not diastolic BP (DBP). There was no significant difference in BP reduction between studies that lasted 6 months or less and those that lasted more than 7 months. Seven studies that lasted 6 months or less involving 1428 patients with hypertension were pooled for further meta-analysis. Text messages delivered at a lower frequency (once per week or less) had a small effect on SBP reduction (effect size 0.35, P<.01) and DBP reduction (effect size 0.28, P=.01). In addition, the use of a text messaging intervention halved the odds of uncontrolled BP among patients with hypertension in 6 months (odds ratio 0.46, P=.02).
Conclusions
This review found that a text messaging intervention was effective in BP control. One-way text messaging delivered in a weekly manner was suggested to be effective and required fewer resources. Future studies should use different forms of text message and be integrated into other interventions to improve adherence behaviors and BP control among patients with hypertension.
Keywords: text messaging, hypertension, blood pressure, mHealth, meta-analysis
Introduction
Background
For a decade, hypertension (HTN) has been the leading risk factor for global disease burden [1]. Over 1 billion people are estimated to have HTN worldwide [2], which necessitates the development of national and international guidelines that provide scientific evidence for the control of blood pressure (BP) [3-8]. Persistent adherence to medications and lifestyle modifications is emphasized in the guidelines to control BP effectively; however, a low adherence rate has been noted in reviews and studies. Two systematic reviews have revealed that medication adherence among patients with HTN is 55% [9,10]. Regarding adherence to lifestyle modifications, studies have shown that adherence to one component of lifestyle modifications ranges from 14% to 85% [11-14], while only 1.7% to 23.6% of patients with HTN adhered to all components of lifestyle modifications: smoking cessation, limited alcohol consumption, regular exercise, maintenance of optimal body weight, and healthy diet [14,15].
Different interventions have been developed such as self BP monitoring, educational interventions, and health professional–led care to improve adherence to HTN management. Reviews suggested that educational interventions directed at patients not only improved BP significantly [16] but also had a significant effect on adherence to medications and lifestyle modifications [17,18]. The reviews further indicated that adding digital components such as text messaging potentially enhances the effect of educational interventions, resulting in improved BP control.
Text Messaging Intervention
Systematic reviews of the effect of text messaging intervention on HTN management were not lacking; nonetheless, the results were inconclusive. Vargas and colleagues [19] included both quasi-experimental and randomized controlled trials (RCTs) in the review. They searched for articles published until July 2015, and 6 studies were included in the meta-analysis. Although the review revealed that the use of 2-month to 12-month text messaging interventions potentially decreases both systolic blood pressure (SBP) and diastolic blood pressure (DBP), the effect size was not determined because of insufficient data and high heterogeneity was noted because of different study designs [19]. In another systematic review, Islam et al [20] included RCTs published between January 1990 and July 2016, and the interventions lasted at least 6 months, with 70% of participants with cardiovascular diseases completing the study. Nine studies were included in the meta-analysis, and the results showed that interventions using a 6-month to 12-month text messaging intervention significantly reduced SBP and DBP among patients with cardiovascular diseases; however, high heterogeneity was observed as different dosages of text messaging intervention were pooled for meta-analysis [20]. Kassavou and Sutton [21] reviewed the use of voice messaging and text messaging interventions on medication adherence among patients with cardiometabolic diseases. They searched for RCTs published between January 1992 and April 2016. Of the 17 included studies, 9 used text messaging. The results of the meta-analysis indicated that the 25-day to 12-month interventions could improve medication adherence significantly; however, high heterogeneity was noted again because of wide variety of interventions used with text messaging. In addition, the authors did not differentiate the effects of text messaging from those of voice messaging on medication adherence [21]. Although the use of a text messaging intervention potentially improves BP control and medication adherence, the frequency of using a text messaging intervention varies from multiple messages per day to fewer than one message per week [19-21]. A review suggested that the use of 2-way text messaging, which required the participants to reply to the received text message, could improve BP control [19]. However, this suggestion was not based on the effect of pooled data. Thus, the directionality of effective text messaging remains inconclusive.
Other than a text messaging intervention, the use of smartphone apps and websites was reviewed and found to have a significant effect on BP control [22]. The interventions required participants to download a HTN smartphone app or access specific websites for HTN management. The ownership of a smartphone is the basic requirement for smartphone apps, and internet access is a prerequisite for both the apps and websites. However, concerns regarding the required technological competency and data protection have been raised [23]. Alternatively, a text messaging intervention can be delivered to recipients via a telecommunication network without any specific apps or internet access. Text message is compatible with being delivered and received between mobile phones and smartphones. Thus, the use of a test messaging intervention potentially covers more people than that of smartphone apps or websites.
Research Gap
In summary, a text messaging intervention may improve HTN management; however, effective additional interventions with text messages have not been identified in previous reviews. A significant effect on BP reduction and medication adherence on HTN-related diseases could be noted if the intervention lasted more than 6 months, but the effectiveness of text messaging interventions lasting 6 months or less was unclear. Also, the dosage of text messaging in terms of frequency and directionality was inconclusive in previous reviews. Regarding the inclusion and exclusion criteria of previous reviews, the included studies were published until July 2016, which might not have reflected the increased use of mobile phones in recent years. As a text messaging intervention is simple to use and widely accepted by both mobile phone and smartphone users, it is worth including recent evidence to review the use of text messaging in HTN management.
Aims
This review aimed to identify the effectiveness of a text messaging intervention in HTN management, with a specific focus on the dosage of text messaging interventions lasting 6 months or less in terms of frequency and directionality and the type of additional interventions with text messages.
Methods
Study Design
A systematic review and meta-analysis were conducted and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement [24], and the search was guided by the PRISMA framework:
Participants: adults with HTN
Interventions: text messaging
Comparisons: standard care or usual care
Outcomes: BP
Study design: RCT
Search Strategy
Keywords used in the search included hypertension, high blood pressure, adult, text messaging, text message, sms, short message service, and texting. The electronic databases related to health sciences used were Embase, Medline, CINAHL Complete (via EbscoHost), PsycINFO, and Scopus. Since the number of included studies in the previous review of the use of text messaging interventions was small [19-21], we searched for articles available in the databases until June 30, 2020 for screening. A manual search was conducted to identify potentially eligible studies from the reference lists of previous reviews [19-21].
Selection Criteria
Participants
Adults aged 18 years and over who had been diagnosed with primary HTN were included. Patients diagnosed with secondary HTN or pregnancy-related HTN were excluded as they required different management strategies [3,8].
Interventions
Studies that used text messaging as a single or combined intervention were included. Studies using any specific HTN smartphone apps were excluded.
Comparisons and Design
Standard care or usual care provided to the control group was set as a comparator. For the 3-arm RCTs, a comparison was made between the control group and the text messaging intervention group. The comparison between the text messaging intervention group and other active intervention group was not conducted. The study design was limited to RCT to yield reliable evidence on the effectiveness of the interventions. All unpublished theses, conference papers, and non-English articles were excluded.
Outcome
The mean and standard deviation of both SBP and DBP were used as continuous data for the meta-analysis. The number of participants with uncontrolled BP in each group was used as dichotomous data for the meta-analysis.
Quality Assessment
The methodological quality of the RCTs was assessed using the Physiotherapy Evidence Database (PEDro) scale. The scale was designed to assess the quality of an RCT and assesses 11 items including randomization, allocation concealment, blinding, treatment of data, and dropout rate [25]. Among the items, 1 point was awarded to each item if the criteria were fulfilled; 10 of the items were rated, resulting in a total score range of 0-10. The total score <4 was considered low quality, which affected the applicability of the evidence [26]. A cutoff of 4 was used to determine the selection of each study. The quality of the RCTs was assessed independently by the first and fourth authors, and the disagreements were discussed and resolved by the second author.
Data Synthesis and Meta-analysis
Data from eligible studies were extracted into a form containing the following information: authors, year of publication, type of RCT (2-arm or 3-arm), guiding theory, age of participants, setting, dosage of text messaging intervention, and outcomes.
Review Manager 5.4 (Cochrane Collaboration) was used in the meta-analysis to extract data regarding changes in SBP and DBP between baseline and final assessment. In accordance with the aim of this review, 3 subgroup analyses were conducted according to directionality, frequency, and combined interventions. Standardized mean difference (SMD) with a 95% confidence interval was used for the pooled effect of continuous data, SBP, and DBP. The I2 statistic was used to detect heterogeneity. A random effects model was used as it allows for different true effect sizes across studies [27]. SMDs equal to 0.2, 0.5, and 0.8 represented small, moderate, and large effects, respectively [28]. Regarding the dichotomous data on BP control, the number of participants with uncontrolled BP and total sample size in each of the intervention and comparator groups were used to determine the effect size and reported as odds ratio (OR). A sensitivity analysis was conducted to explore possible differences between the intention-to-treat analysis and others.
Results
Search Results
A total of 1731 articles were initially identified from database searches, and 2 additional articles were identified in the manual search, as shown in Figure 1. A web-based application for systematic reviews, Rayyan, was used to remove duplicates and screen titles and abstracts [29]. Among the 56 articles assessed in full text, 2 were excluded due to low quality (PEDro score <4). The reasons for excluding those studies were that they did not conceal the group allocation process from the participants, therapists, and assessors; furthermore, only the participants from the intervention group withdrew from the study, and the data management and analysis methods were not stated clearly. Finally, 12 studies met the selection criteria. The characteristics of the studies and dosage of the text messaging intervention are described below.
Figure 1.
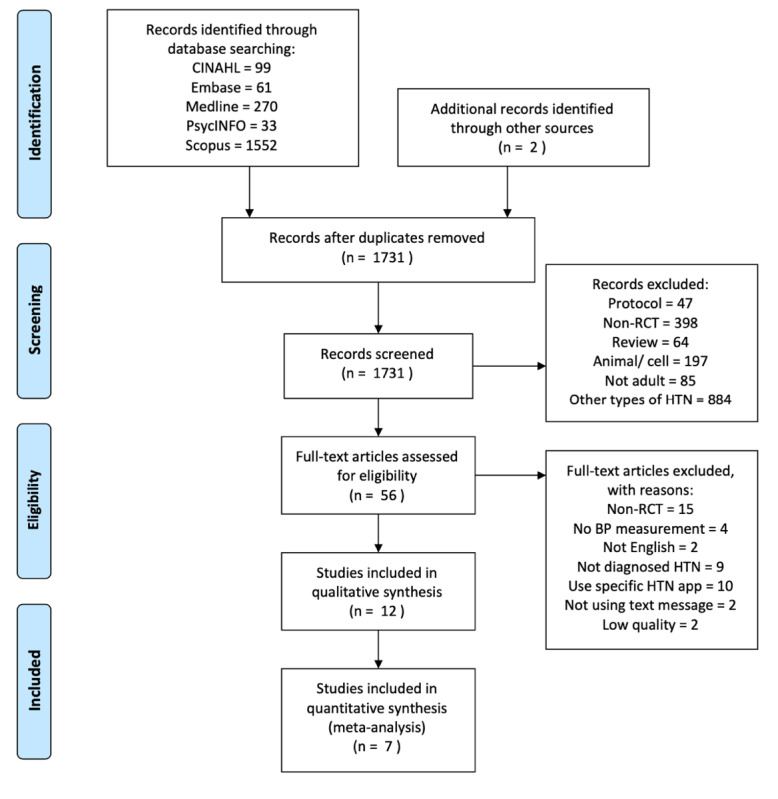
Flow diagram of literature selection process. BP: blood pressure; HTN: hypertension; RCT: randomized controlled trial.
Quality of Studies
Of the 12 included studies, the overall methodological quality was fair, and the PEDro score ranged from 4 to 8, with a mean score of 5.75 (Table 1). None of the studies was able to fulfill the participant-blinding criterion due to the nature of the text messaging intervention (Figure 2). Participants automatically knew their group allocation because no text messages were delivered to the control group. In addition, blinding of therapists was lacking in most studies in that the therapists knew the participant group allocation when providing care. The assessors in some studies knew the group allocation during follow-up data collection. Regarding the treatment of data, intention-to-treat was not followed in some studies, and clinical significance in each group was not assessed.
Table 1.
Characteristics of included studies.
| Author | Duration of intervention (study design) | Frequency (directionality) | Theory | Additional intervention | PEDroa score |
| Márquez Contreras et al [41] | 6 mb (2-arm) | 2/wc (1-way) | No | Health education, print materials | 5 |
| Carrasco et al [40] | 6 m (2-arm) | 4/w (1-way) | No | No | 6 |
| Bobrow et al [39] | 12 m (3-arm) | 1/w (1-way & 2-way) | No | No | 8 |
| Buis et al [30] | 1 m (2-arm) | 1/dd (1-way) | Health belief model | No | 4 |
| He et al [31] | 18 m (2-arm) | 1/w (1-way) | No | Health education | 6 |
| Varleta et al [32] | 6 m (2-arm) | 1/14 days (1-way) | Social cognitive theory | No | 5 |
| Wan et al [33] | 3 m (2-arm) | 1/w (1-way) | Health belief model | Health education, phone call, booklet | 7 |
| Mehta et al [34] | 4 m (3-arm) | 1/d (2-way) | No | No | 7 |
| Zahr et al [35] | 6 m (2-arm) | 2/d (2-way) | No | No | 4 |
| Schroeder et al [36] | 12 m (2-arm) | 1/w (1-way) | No | No | 7 |
| Tahkola et al [37] | 12 m (2-arm) | Varied (1-way) | Information-motivation-behavioral skills model | No | 5 |
| Zhai et al [38] | 3 m (2-arm) | 1/3 d (1-way) | No | Health education | 5 |
aPEDro: Physiotherapy Evidence Database.
bm: month.
cw: week.
dd: day.
Figure 2.
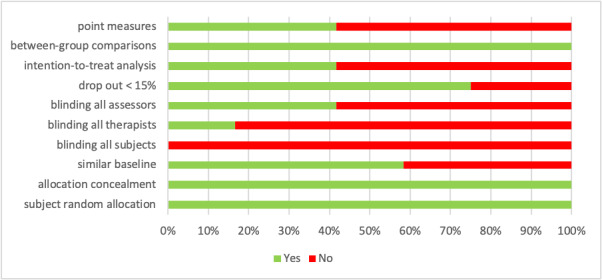
Methodological quality as percentage across all included studies.
Characteristics of Studies
The included studies were published between 2004 and 2020; 9 were published after 2016 [30-38]. The characteristics of the included studies are summarized in Table 1. Of the 12 included studies, 2 were 3-arm RCTs [34,39], and 4 studies provided the interventions lasted more than 7 months [31,36,37,39]. The number of participants in each study varied from 67 to 1432, with a mean age of 58.97 years. Participants mean age was over 60 years in 3 studies [32,38,40]. Four studies were conducted in the United States; 2 each in China and Spain; and one each in Argentina, South Africa, Chile, and Finland.
Regarding the additional interventions with text messaging, 4 studies integrated face-to-face health education with text messaging intervention to reinforce the effect on HTN management [31,33,38,41]. Only 4 studies were guided by theory, 2 of which used the health belief model [30,33], with the social cognitive theory and information-motivation-behavioral skills model used in 2 other studies [32,37].
Dosage of Text Messaging Interventions
The frequency of delivering text messages to patients with HTN varied from daily to biweekly among the included studies. Only one study used an individualized frequency to deliver text messages to the participants [37]. Text messages were delivered every day for the first 2 weeks, after which the frequency decreased from the third week onward. The first telephone follow-up was conducted in the fourth week to evaluate the participants’ BP levels. The frequency of text messages would increase thereafter if BP was not controlled at the follow-up. In addition, He et al [31] and Tahkola et al [37] tailored the content of text messages in accordance with the barriers identified in the assessment and follow-up.
Regarding the directionality, 2-way text messaging was seldom used in the studies. Zahr et al [35] required the participants to report SBP and DBP via the text messages. In the Mehta et al [34] 3-arm RCT, one intervention arm received an electronic pill box that was connected to an internet platform to monitor the use of medication, while another intervention arm required the participants to respond to text messages if they had taken the medication. The Bobrow et al [39] study was a 3-arm RCT that compared the effects of 1-way and 2-way text messaging on HTN management with the control group. Participants replied to text messages to change the medical appointments, delivery times, and language of the text message delivery. In comparison with the control group, the results of the study by Bobrow et al [39] showed that the use of 1-way text messaging decreased SBP significantly, whereas the decrease in SBP in the 2-way text messaging arm failed to achieve statistical significance. Bobrow et al [39] suggested that the nonsignificant findings might have been related to the older age of the participants or their experience in using technology.
Other Outcomes
In addition to BP measurement, medication adherence was commonly assessed (Table 2). However, the methods of assessment differed among the studies. Six studies used self-reported measures to assess the medication adherence [30-33,36,38]. One study compared medication adherence between electronic pill boxes and text message responses [34] and another used the pill count [39]. Among the studies using self-reported measures, the Morisky Medication Adherence Scale was used in 3 studies. Most studies demonstrated an improvement in medication adherence after the use of text messaging. However, the diverse assessment methods resulted in difficulty in comparing medication adherence between studies. It is noteworthy that only one study used a self-reported approach to assess the adherence to lifestyle modifications among the patients with HTN [33].
Table 2.
Outcome measures of included studies.
| Author | Blood pressure | Medication adherence | Adherence to lifestyle modifications | Appointment adherence |
| Márquez Contreras et al [41] | +a | Nb | N | –c |
| Carrasco et al [40] | – | N | N | N |
| Bobrow et al [39] | + | – | N | N |
| Buis et al [30] | – | – | N | N |
| He et al [31] | + | + | N | N |
| Varleta et al [32] | – | + | N | N |
| Wan et al [33] | + | + | + | N |
| Mehta et al [34] | – | – | N | N |
| Zahr et al [35] | – | N | N | N |
| Schroeder et al [36] | – | – | N | – |
| Tahkola et al [37] | – | N | N | N |
| Zhai et al [38] | + | + | N | N |
a+: significant differences between intervention group (text messaging alone or with additional interventions) and control group (standard care or usual care; P<.05).
bN: not measured.
c–: nonsignificant differences between intervention and control groups.
Meta-analysis
Four studies used interventions that lasted 12 months or more, while the interventions in 8 studies lasted 6 months or less. The corresponding authors of 2 studies were contacted via email to obtain unreported data, but only 1 of them provided the requested data [32]. The study from which unreported data could not be obtained was excluded from the meta-analysis. In the Bobrow et al [39] 3-arm RCT, text messaging was used in 2 intervention groups, and 2 comparisons with control group were extracted for meta-analysis. In the Mehta et al [34] 3-arm RCT, text messaging was used in one intervention group, while an electronic pill box was used in another intervention group. Thus, only one comparison was performed. Although some long-term studies, such as those by Bobrow et al [39] and He et al [31], provided midprocess data at 6 months, the interventions were not delivered to completion, and the 6-month data failed to reflect the holistic effect of the interventions. The midprocess data at 6 months was not extracted for meta-analysis. Figures 3 and 4 illustrate the durations of intervention lasting 6 months or less and those lasting more than 7 months made no statistical differences in SBP and DBP reduction (subgroup differences, P>.05). The overall results revealed that the text messaging intervention significantly reduced SBP (Figure 3, SMD=.13, P=.01) but not DBP (Figure 4, SMD=.06, P=.56). To explore the effectiveness of text messaging interventions lasting 6 months or less, we excluded all studies with interventions lasted more than 7 months. Also, the study without obtaining unreported data was excluded. As a result, 7 studies lasting 6 months or less were pooled for meta-analysis in terms of directionality, frequency, and type of intervention.
Figure 3.
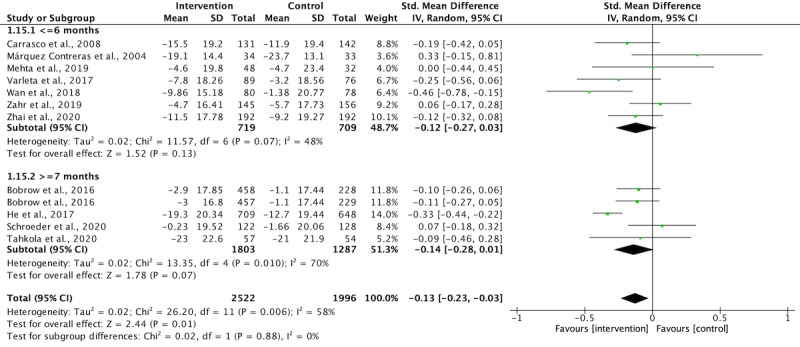
The effect of study duration on systolic blood pressure reduction.
Figure 4.
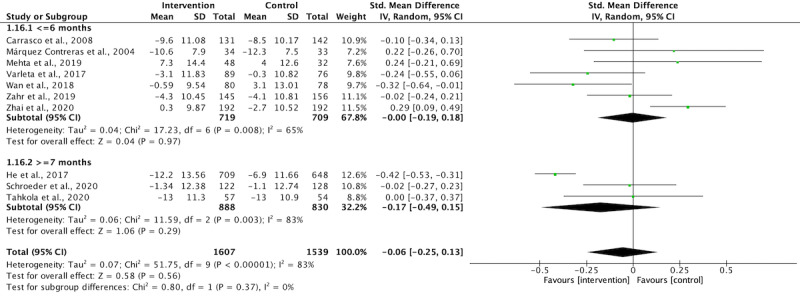
The effect of study duration on diastolic blood pressure reduction.
Tables 3 and 4 show the effectiveness of a text messaging intervention on SBP and DBP reduction with interventions lasted 6 months or less. Regarding the directionality of text messaging, neither 1-way nor 2-way text messaging had a significant effect on SBP or DBP reduction. However, a small effect on SBP and DBP reduction was noted when text messages were delivered in a weekly manner (ie, 1 text message per week). However, the use of a text messaging intervention alone or in combination with health education did not significantly affect SBP or DBP reduction. Six studies reported the number of participants with uncontrolled BP (SBP ≥140 mm Hg or DBP ≥90 mm Hg) at the end of the study. The data were pooled as shown in Figure 5, and the use of a text messaging intervention helped patients with HTN achieve a controlled BP with SBP <140 mm Hg and DBP <90 mm Hg (OR 0.46, P=.02).
Table 3.
Effectiveness of text messaging on systolic blood pressure reduction with interventions lasting 6 months or less.
| Subgroup analysis | Number of studies | Effect size (95% CI) | Heterogeneity I2 (%) | P value | Significance of subgroup differences (P value) | |||||||
| Directionality of text messaging | .10 | |||||||||||
|
|
1-way | 5 | 0.18 (0.00, 0.36) | 49 | .05 | —a | ||||||
|
|
2-way | 2 | –0.05 (–0.25, 0.15) | 0 | .65 | — | ||||||
| Frequency of text messaging | .02 | |||||||||||
|
|
>1 per week | 5 | 0.04 (–0.09, 0.18) | 22 | .53 | — | ||||||
|
|
≤1 per week | 2 | 0.35 (0.13, 0.57) | 0 | .002 | — | ||||||
| Type of intervention | .87 | |||||||||||
|
|
With health education | 3 | 0.13 (–0.23, 0.48) | 74 | .49 | — | ||||||
|
|
Text messaging only | 4 | 0.09 (–0.06, 0.24) | 14 | .23 | — | ||||||
aNot applicable.
Table 4.
Effectiveness of text messaging on diastolic blood pressure reduction with interventions lasting 6 months or less.
| Subgroup analysis | Number of studies | Effect size (95% CI) | Heterogeneity I2 (%) | P value | Significance of subgroup differences (P value) | ||
| Directionality of text messaging | .58 | ||||||
|
|
1-way | 5 | 0.03 (–0.22, 0.29) | 75 | .79 | —a | |
|
|
2-way | 2 | –0.03 (–0.24, 0.17) | 0 | .75 | — | |
| Frequency of text messaging | .01 | ||||||
|
|
>1 per week | 5 | –0.10 (–0.28, 0.08) | 50 | .27 | — | |
|
|
≤1 per week | 2 | 0.28 (0.06, 0.50) | 0 | .01 | — | |
| Type of intervention | .97 | ||||||
|
|
With health education | 3 | –0.06 (–0.48, 0.36) | 81 | .77 | — | |
|
|
Text messaging only | 4 | 0.07 (–0.08, 0.21) | 10 | .37 | — | |
aNot applicable.
Figure 5.
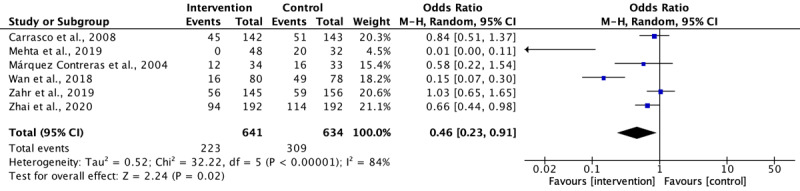
Odds ratio of text messaging on blood pressure control.
Sensitivity Analysis
Among the 11 studies with sufficient data pooled in the meta-analysis, 5 used intention-to-treat analysis and the rest did not clearly state their method of analysis. No significant subgroup difference in SBP and DBP reduction was noted between the intention-to-treat analysis and others (Multimedia Appendix 1). Seven studies with text messaging interventions lasted 6 months or less, 2 of which used intention-to-treat analysis. Figure S4 showed a significant subgroup difference in DBP reduction (Multimedia Appendix 1). The pooled results of studies using intention-to-treat analysis showed a favorable effect in the control group, in which usual care reduced DBP more effectively than the text messaging intervention [34,38]. No significant subgroup difference in SBP reduction was noted among interventions that lasted 6 months or less (Multimedia Appendix 1).
Discussion
Summary
This review identified 12 RCTs from 5 electronic databases. The study duration varied from 1 to 18 months. Five studies were published between January 2019 and June 2020, showing that the interest in using text messaging has increased in HTN research. In the meta-analysis, the use of a text messaging intervention significantly reduced SBP but not DBP. Seven studies with a text messaging intervention lasting 6 months or less, involving 1428 patients with HTN, were pooled for further analysis. The results showed that the delivery of weekly text messages significantly improved both SBP and DBP. In addition, the use of a text messaging intervention halved the odds of uncontrolled BP in patients with HTN in 6 months. This review provided information regarding the dosage of a text messaging intervention and type of additional interventions in HTN research using text messages.
Directionality and Frequency
A systematic review of patients with HTN claimed that the use of 2-way text messaging potentially reduces SBP and DBP [19]; however, our findings did not reveal any significant effect relating to the directionality of text messaging on SBP and DBP reduction with an intervention lasting 6 months or less. Noteworthily, participants were required to respond when 2-way text messaging was used. In terms of simple yes/no responses, a session on how to reply to text messages was necessary if specific information, such as BP level, was required. The use of 2-way text messaging may potentially require additional resources. Head et al [42] found that the use of 1-way text messaging significantly increased the likelihood of healthy behaviors. The Bobrow et al [39] 3-arm RCT also showed that the use of 1-way text messaging decreased SBP significantly. Having the same tendency, our findings revealed that 1-way text messaging might potentially reduce SBP (Table 3, SMD=.18, P=.05). Therefore, 1-way text messaging might be more feasible and effective for patients with HTN.
Regarding frequency, a decreasing frequency was found to have a moderate effect on health promotion in a review [42]. Since only 1 included study used a decreasing frequency of text messaging on HTN management [37], the effect was not examined in this review. Accordingly, a previous review revealed that the daily or weekly delivery of text messages had a minute effect on promoting health behaviors [42]. Our findings revealed that text messaging could reduce SBP as well as the odds of uncontrolled BP given a target population of patients with HTN and the weekly delivery of text messages.
Types of Intervention
Health education was a commonly used intervention in combination with text messages among the included studies. In this review, a text messaging intervention alone and the combined use of health education had no significant effect on SBP and DBP reduction. The findings contradicted those of a recent review, in which the use of supportive methods, such as text messages and take-home reading materials, with health education yielded a moderately significant effect in improving both SBP and DBP among patients with HTN [18]. In addition, a review by Head et al [42] found that a text messaging intervention alone and the combination of text messages with other interventions could have a significantly small effect on health promotion; however, the duration of their included studies was not limited, and a wide variety of combined interventions was noted such as websites, health education, print materials, pedometers, and daily records of health behavior. Hence, the effectiveness of a text messaging intervention alone or in combination with other interventions to manage HTN remains inconclusive.
On the other hand, tailored content of text messages showed a significant effect on health promotion and medication adherence in previous reviews [21,42]. Two studies in this review were found to tailor their text messages to the participants [31,37], but the interventions lasted 12 to 18 months, resulting in an effect that was not analyzed in the meta-analysis. He et al [31] recruited 1432 patients with HTN in their study and revealed that the tailored content reduced SBP and DBP significantly; however, a significant reduction in SBP and DBP was not noted in the study by Tahkola et al [37]. Another study recruiting people with uncontrolled BP showed that tailored content did not make a significant difference in the reduction of SBP and DBP [43]. The effect of tailored content of text messages on SBP and DBP in patients with HTN was inconclusive. In addition, tailored content requires additional resources, as He et al [31] estimated that the use of tailored content would cost an extra US $6.36 per patient per month. Therefore, tailored content of text messages may not be beneficial to patients with HTN, especially in health care systems with limited resources.
Assessment of Adherence to HTN Management
Medication adherence was assessed in most of the included studies. However, adherence to lifestyle modifications is the core element in HTN management guidelines for patients with HTN and those at risk of HTN [3-8]. The only included study that assessed adherence to lifestyle modifications was conducted by Wan et al [33] in 2018. They revealed that the use of standardized content of text messages combined with health education and leaflet intervention could improve adherence behaviors in 3 months [33]. Another 2-arm RCT recruited 710 patients with coronary heart diseases and showed that adherence to lifestyle modifications improved significantly when tailored content of text messages was delivered 4 times a week for 6 months [44]. These studies suggest that a text messaging intervention may be an effective method to improve adherence to lifestyle modifications. Future studies should examine the effect of text messaging on adherence to both medications and lifestyle modifications among patients with HTN. Regarding the choice of adherence scale, the Treatment Adherence Questionnaire for Patients with Hypertension [45] was suggested in 2 systematic reviews, as it is a comprehensive measure that covers adherence to both medication and lifestyle modifications and is designated for patients with HTN [46,47].
Intention-to-Treat Analysis
A significant difference of DBP reduction in control group was found in the sensitivity analysis (Multimedia Appendix 1). The significant result was from studies that delivered text messages more frequently (more than once per week) [34,38]. The significant DBP reduction in the control group may indicate information overload by means of high frequency of text messaging [48].
Limitations
Several limitations were noted in this review. We searched for and included only English articles, thus reducing the diversity of the analyzed studies. Only 7 studies were included in the subgroup analysis. Hence, the findings should be interpreted with caution, since the subgroup analyses consisted of a very small number of studies and the variations in dosage of text messaging and combination with health education caused high heterogeneity in the meta-analysis. The decision to only include RCTs in the meta-analysis increased the internal validity of the findings; nonetheless, the external validity might have decreased. The scope of the review was limited to the text messaging, and advanced features added to today’s mobile phones or smartwatches to enhance HTN management were not explored.
Implications
We have provided advice for the use of text messaging in HTN management in practice and research. The use of text messaging could help patients with HTN return to controlled BP levels in 6 months or less, and 1-way text messaging could be useful if delivered weekly to patients with HTN. The standardized content of text messages can be stored in a preprogrammed database. Once clients agree to receive text messages, their mobile phone numbers can be entered into the program, thus facilitating the regular delivery of text messages to the clients.
The rapid growth of smartphone ownership and advancing technologies in recent decades has evolved a new mode of delivering text messages. Data from the Pew Research Center showed that smartphone ownership in advanced economies increased from 68% to 76% between 2015 and 2018 [49,50]. Instead of using a traditional short message service, text messages can now be delivered in the form of voice, images, and videos via general smartphone communication apps such as Telegram and WhatsApp. The advanced features of text messaging may enhance adherence behaviors, resulting in an improvement in BP control [51,52]. Hence, future studies should examine the effect of informative images and videos on HTN management, including BP regulation, medication adherence, and adherence to lifestyle modifications. The integration of text messaging with advanced technology should be explored in future studies.
Conclusions
This review updates the information from previous reviews with a focus on patients with HTN. The meta-analysis provides evidence for the use of a text messaging intervention in BP control. As indicated in the meta-analysis, the use of a text messaging intervention lowers the odds of uncontrolled BP. Text messages delivered at a lower frequency had a small effect on the reduction of SBP and DBP. Although the effect of a text messaging intervention on medication adherence was not examined, most included studies showed improvement after the intervention. Thus, text messaging is a potentially useful intervention for HTN management. Regarding the implications of this review, weekly 1-way text messaging is recommended in practice and research. The use of text messages should be incorporated into different interventions in future studies to further improve adherence behaviors and BP control among patients with HTN. There is great potential for professional development in the area of using advanced features of text messages and the more feasible use of these features in delivering messages to clients effectively.
Abbreviations
- BP
blood pressure
- DBP
diastolic blood pressure
- HTN
hypertension
- OR
odds ratio
- PEDro
Physiotherapy Evidence Database
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-analyses
- RCT
randomized controlled trial
- SBP
systolic blood pressure
- SMD
standardized mean difference
Sensitivity analysis.
Footnotes
Authors' Contributions: HLT contributed to data search, extraction, and analysis and then drafted and revised this paper. EMLW advised on data analysis, revised the paper, and approved the final manuscript. KC revised the paper and approved the final manuscript. SFC contributed to data search and extraction and approved the final manuscript.
Conflicts of Interest: None declared.
References
- 1.GBD 2019 Diseases and Injuries Collaborators Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020 Oct 17;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. https://linkinghub.elsevier.com/retrieve/pii/S0140-6736(20)30925-9 .S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . Hypertension. Geneva: World Health Organization; https://www.who.int/news-room/fact-sheets/detail/hypertension . [Google Scholar]
- 3.Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA, Williamson JD, Wright JT. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018 May 15;71(19):e127–e248. doi: 10.1016/j.jacc.2017.11.006. https://linkinghub.elsevier.com/retrieve/pii/S0735-1097(17)41519-1 .S0735-1097(17)41519-1 [DOI] [PubMed] [Google Scholar]
- 4.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I, ESC Scientific Document Group 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018 Sep 01;39(33):3021–3104. doi: 10.1093/eurheartj/ehy339.5079119 [DOI] [PubMed] [Google Scholar]
- 5.Joint Committee for Guideline Revision 2018 Chinese Guidelines for Prevention and Treatment of Hypertension: a report of the Revision Committee of Chinese Guidelines for Prevention and Treatment of Hypertension. J Geriatr Cardiol. 2019 Mar;16(3):182–241. doi: 10.11909/j.issn.1671-5411.2019.03.014. http://europepmc.org/abstract/MED/31080465 .jgc-16-03-182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, Horio T, Hoshide S, Ikeda S, Ishimitsu T, Ito M, Ito S, Iwashima Y, Kai H, Kamide K, Kanno Y, Kashihara N, Kawano Y, Kikuchi T, Kitamura K, Kitazono T, Kohara K, Kudo M, Kumagai H, Matsumura K, Matsuura H, Miura K, Mukoyama M, Nakamura S, Ohkubo T, Ohya Y, Okura T, Rakugi H, Saitoh S, Shibata H, Shimosawa T, Suzuki H, Takahashi S, Tamura K, Tomiyama H, Tsuchihashi T, Ueda S, Uehara Y, Urata H, Hirawa N. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019) Hypertens Res. 2019 Sep;42(9):1235–1481. doi: 10.1038/s41440-019-0284-9.10.1038/s41440-019-0284-9 [DOI] [PubMed] [Google Scholar]
- 7.Lee H, Shin J, Kim G, Park S, Ihm S, Kim HC, Kim K, Kim JH, Lee JH, Park J, Pyun WB, Chae SC. 2018 Korean Society of Hypertension Guidelines for the management of hypertension: part II-diagnosis and treatment of hypertension. Clin Hypertens. 2019;25:20. doi: 10.1186/s40885-019-0124-x. https://clinicalhypertension.biomedcentral.com/articles/10.1186/s40885-019-0124-x .124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, Ramirez A, Schlaich M, Stergiou GS, Tomaszewski M, Wainford RD, Williams B, Schutte AE. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension. 2020 Jun;75(6):1334–1357. doi: 10.1161/HYPERTENSIONAHA.120.15026. [DOI] [PubMed] [Google Scholar]
- 9.Abegaz TM, Shehab A, Gebreyohannes EA, Bhagavathula AS, Elnour AA. Nonadherence to antihypertensive drugs: a systematic review and meta-analysis. Medicine (Baltimore) 2017 Jan;96(4):e5641. doi: 10.1097/MD.0000000000005641. doi: 10.1097/MD.0000000000005641.00005792-201701270-00009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carvalho AS, Santos P. Medication adherence in patients with arterial hypertension: the relationship with healthcare systems' organizational factors. Patient Prefer Adherence. 2019;13:1761–1774. doi: 10.2147/PPA.S216091. doi: 10.2147/PPA.S216091.216091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alefan Q, Huwari D, Alshogran O, Jarrah MI. Factors affecting hypertensive patients' compliance with healthy lifestyle. Patient Prefer Adherence. 2019;13:577–585. doi: 10.2147/PPA.S198446. doi: 10.2147/PPA.S198446.198446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Selçuk KT, Çevik C, Mercan Y, Koca H. Hypertensive patients’ adherence to pharmacological and non-pharmacological treatment methods, in Turkey. Int J Community Med Public Health. 2017 Jul 22;4(8):2648–2657. doi: 10.18203/2394-6040.ijcmph20173308. [DOI] [Google Scholar]
- 13.Tibebu A, Bekele DM, Negesa L. Adherence to recommended lifestyle modifications and factors associated for hypertensive patients attending chronic follow-up units of selected public hospitals in Addis Ababa, Ethiopia. Patient Prefer Adherence. 2017 Feb;11:323–330. doi: 10.2147/ppa.s126382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fang J, Moore L, Loustalot F, Yang Q, Ayala C. Reporting of adherence to healthy lifestyle behaviors among hypertensive adults in the 50 states and the District of Columbia, 2013. J Am Soc Hypertens. 2016 Mar;10(3):252–262.e3. doi: 10.1016/j.jash.2016.01.008. http://europepmc.org/abstract/MED/26851000 .S1933-1711(16)00009-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Andualem A, Gelaye H, Damtie Y. Adherence to lifestyle modifications and associated factors among adult hypertensive patients attending chronic follow-up units of Dessie Referral Hospital, North East Ethiopia, 2020. Integr Blood Press Control. 2020;13:145–156. doi: 10.2147/IBPC.S275575. doi: 10.2147/IBPC.S275575.275575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Glynn L, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2010 Mar 17;(3):CD005182. doi: 10.1002/14651858.CD005182.pub4. [DOI] [PubMed] [Google Scholar]
- 17.Conn VS, Ruppar TM, Chase JD, Enriquez M, Cooper PS. Interventions to improve medication adherence in hypertensive patients: systematic review and meta-analysis. Curr Hypertens Rep. 2015 Dec 11;17(12):94. doi: 10.1007/s11906-015-0606-5. http://europepmc.org/abstract/MED/26560139 .10.1007/s11906-015-0606-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tam HL, Wong EML, Cheung K. Effectiveness of educational interventions on adherence to lifestyle modifications among hypertensive patients: an integrative review. Int J Environ Res Public Health. 2020 Apr 07;17(7):2513. doi: 10.3390/ijerph17072513. https://www.mdpi.com/resolver?pii=ijerph17072513 .ijerph17072513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vargas G, Cajita MI, Whitehouse E, Han H. Use of short messaging service for hypertension management: a systematic review. J Cardiovasc Nurs. 2017;32(3):260–270. doi: 10.1097/JCN.0000000000000336. http://europepmc.org/abstract/MED/27111819 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shariful Islam SM, Farmer AJ, Bobrow K, Maddison R, Whittaker R, Pfaeffli Dale LA, Lechner A, Lear S, Eapen Z, Niessen LW, Santo K, Stepien S, Redfern J, Rodgers A, Chow CK. Mobile phone text-messaging interventions aimed to prevent cardiovascular diseases (Text2PreventCVD): systematic review and individual patient data meta-analysis. Open Heart. 2019;6(2):e001017. doi: 10.1136/openhrt-2019-001017. https://openheart.bmj.com/lookup/pmidlookup?view=long&pmid=31673381 .openhrt-2019-001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kassavou A, Sutton S. Automated telecommunication interventions to promote adherence to cardio-metabolic medications: meta-analysis of effectiveness and meta-regression of behaviour change techniques. Health Psychol Rev. 2017 Sep 12;:1–18. doi: 10.1080/17437199.2017.1365617. [DOI] [PubMed] [Google Scholar]
- 22.Ma Y, Cheng HY, Cheng L, Sit JW. The effectiveness of electronic health interventions on blood pressure control, self-care behavioural outcomes and psychosocial well-being in patients with hypertension: a systematic review and meta-analysis. Int J Nurs Stud. 2019 Apr;92:27–46. doi: 10.1016/j.ijnurstu.2018.11.007.S0020-7489(18)30267-0 [DOI] [PubMed] [Google Scholar]
- 23.Morrissey EC, Casey M, Glynn LG, Walsh JC, Molloy GJ. Smartphone apps for improving medication adherence in hypertension: patients' perspectives. Patient Prefer Adherence. 2018;12:813–822. doi: 10.2147/PPA.S145647. doi: 10.2147/PPA.S145647.ppa-12-813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009 Jul 21;339(1):b2535. doi: 10.1136/bmj.b2535. http://www.bmj.com/lookup/pmidlookup?view=long&pmid=19622551 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maher C, Sherrington C, Herbert R, Moseley A, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003 Aug;83(8):713–721. [PubMed] [Google Scholar]
- 26.Cashin AG, McAuley JH. Clinimetrics: Physiotherapy Evidence Database (PEDro) Scale. J Physiother. 2020 Jan;66(1):59. doi: 10.1016/j.jphys.2019.08.005. https://linkinghub.elsevier.com/retrieve/pii/S1836-9553(19)30092-X .S1836-9553(19)30092-X [DOI] [PubMed] [Google Scholar]
- 27.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002 Jun 15;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 28.Faraone SV. Interpreting estimates of treatment effects: implications for managed care. Pharma Therapeutics. 2008 Dec;33(12):700–711. http://europepmc.org/abstract/MED/19750051 . [PMC free article] [PubMed] [Google Scholar]
- 29.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016 Dec 05;5(1):210. doi: 10.1186/s13643-016-0384-4. https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-016-0384-4 .10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Buis L, Hirzel L, Dawood RM, Dawood KL, Nichols LP, Artinian NT, Schwiebert L, Yarandi HN, Roberson DN, Plegue MA, Mango LC, Levy PD. Text messaging to improve hypertension medication adherence in African Americans from primary care and emergency department settings: results from two randomized feasibility studies. JMIR Mhealth Uhealth. 2017 Feb 01;5(2):e9. doi: 10.2196/mhealth.6630. https://mhealth.jmir.org/2017/2/e9/ v5i2e9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.He J, Irazola V, Mills KT, Poggio R, Beratarrechea A, Dolan J, Chen C, Gibbons L, Krousel-Wood M, Bazzano LA, Nejamis A, Gulayin P, Santero M, Augustovski F, Chen J, Rubinstein A, HCPIA Investigators Effect of a community health worker-led multicomponent intervention on blood pressure control in low-income patients in Argentina: a randomized clinical trial. JAMA. 2017 Sep 19;318(11):1016–1025. doi: 10.1001/jama.2017.11358. http://europepmc.org/abstract/MED/28975305 .2654383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Varleta P, Acevedo M, Akel C, Salinas C, Navarrete C, García A, Echegoyen C, Rodriguez D, Gramusset L, Leon S, Cofré P, Retamal R, Romero K. Mobile phone text messaging improves antihypertensive drug adherence in the community. J Clin Hypertens (Greenwich) 2017 Dec 21;19(12):1276–1284. doi: 10.1111/jch.13098. doi: 10.1111/jch.13098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wan LH, Zhang XP, You LM, Ruan HF, Chen SX. The efficacy of a comprehensive reminder system to improve health behaviors and blood pressure control in hypertensive ischemic stroke patients: a randomized controlled trial. J Cardiovasc Nurs. 2018;33(6):509–517. doi: 10.1097/JCN.0000000000000496. [DOI] [PubMed] [Google Scholar]
- 34.Mehta SJ, Volpp KG, Troxel AB, Day SC, Lim R, Marcus N, Norton L, Anderson S, Asch DA. Electronic pill bottles or bidirectional text messaging to improve hypertension medication adherence (Way 2 Text): a randomized clinical trial. J Gen Intern Med. 2019 Nov 08;34(11):2397–2404. doi: 10.1007/s11606-019-05241-x. http://europepmc.org/abstract/MED/31396815 .10.1007/s11606-019-05241-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zahr RS, Anthony CA, Polgreen PM, Simmering JE, Goerdt CJ, Hoth AB, Miller ML, Suneja M, Segre AM, Carter BL, Cavanaugh JE, Polgreen LA. A texting-based blood pressure surveillance intervention. J Clin Hypertens (Greenwich) 2019 Oct 10;21(10):1463–1470. doi: 10.1111/jch.13674. doi: 10.1111/jch.13674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schroeder EB, Moore KR, Manson SM, Baldwin MA, Goodrich GK, Malone AS, Pieper LE, Xu S, Fort MP, Son-Stone L, Johnson D, Steiner JF. A randomized clinical trial of an interactive voice response and text message intervention for individuals with hypertension. J Clin Hypertens (Greenwich) 2020 Jul 09;22(7):1228–1238. doi: 10.1111/jch.13909. doi: 10.1111/jch.13909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tahkola A, Korhonen P, Kautiainen H, Niiranen T, Mäntyselkä P. Personalized text message and checklist support for initiation of antihypertensive medication: the cluster randomized, controlled check and support trial. Scand J Prim Health Care. 2020 Jun 02;38(2):201–209. doi: 10.1080/02813432.2020.1753380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhai P, Hayat K, Ji W, Li Q, Shi L, Atif N, Xu S, Li P, Du Q, Fang Y. Efficacy of text messaging and personal consultation by pharmacy students among adults with hypertension: randomized controlled trial. J Med Internet Res. 2020 May 20;22(5):e16019. doi: 10.2196/16019. https://www.jmir.org/2020/5/e16019/ v22i5e16019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bobrow K, Farmer AJ, Springer D, Shanyinde M, Yu L, Brennan T, Rayner B, Namane M, Steyn K, Tarassenko L, Levitt N. Mobile phone text messages to support treatment adherence in adults with high blood pressure (SMS-Text Adherence Support [StAR]): a single-blind, randomized trial. Circulation. 2016 Feb 09;133(6):592–600. doi: 10.1161/CIRCULATIONAHA.115.017530. http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=26769742 .CIRCULATIONAHA.115.017530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Carrasco MP, Salvador CH, Sagredo PG, Márquez-Montes J, González DMMA, Fragua JA, Rodríguez MC, García-Olmos LM, García-López F, Carrero AM, Monteagudo JL. Impact of patient-general practitioner short-messages-based interaction on the control of hypertension in a follow-up service for low-to-medium risk hypertensive patients: a randomized controlled trial. IEEE Trans Inf Technol Biomed. 2008 Nov;12(6):780–791. doi: 10.1109/TITB.2008.926429. http://paperpile.com/b/vf5PfU/XjR5 . [DOI] [PubMed] [Google Scholar]
- 41.Márquez Contreras E, de la Figuera von Wichmann M, Gil Guillén V, Ylla-Catalá A, Figueras M, Balaña M, Naval J. [Effectiveness of an intervention to provide information to patients with hypertension as short text messages and reminders sent to their mobile phone (HTA-Alert)] Aten Primaria. 2004 Nov 15;34(8):399–405. doi: 10.1016/s0212-6567(04)78922-2. https://linkinghub.elsevier.com/retrieve/pii/13068215 .13068215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Head KJ, Noar SM, Iannarino NT, Grant HN. Efficacy of text messaging-based interventions for health promotion: a meta-analysis. Soc Sci Med. 2013 Nov;97:41–48. doi: 10.1016/j.socscimed.2013.08.003.S0277-9536(13)00447-4 [DOI] [PubMed] [Google Scholar]
- 43.Tobe SW, Yeates K, Campbell NRC, Maar MA, Perkins N, Liu PP, Sleeth J, McAllister C, Hua-Stewart D, Wells G, Bernick J. Diagnosing hypertension in Indigenous Canadians (DREAM-GLOBAL): a randomized controlled trial to compare the effectiveness of short message service messaging for management of hypertension: Main results. J Clin Hypertens (Greenwich) 2019 Jan 26;21(1):29–36. doi: 10.1111/jch.13434. doi: 10.1111/jch.13434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chow CK, Ariyarathna N, Islam SMS, Thiagalingam A, Redfern J. mHealth in cardiovascular health care. Heart Lung Circ. 2016 Aug;25(8):802–807. doi: 10.1016/j.hlc.2016.04.009.S1443-9506(16)30091-9 [DOI] [PubMed] [Google Scholar]
- 45.Ma C, Chen S, You L, Luo Z, Xing C. Development and psychometric evaluation of the Treatment Adherence Questionnaire for Patients with Hypertension. J Adv Nurs. 2012 Jun;68(6):1402–1413. doi: 10.1111/j.1365-2648.2011.05835.x. [DOI] [PubMed] [Google Scholar]
- 46.Pérez-Escamilla B, Franco-Trigo L, Moullin JC, Martinez-Martinez F, Garcia-Corpas JP. Identification of validated questionnaires to measure adherence to pharmacological antihypertensive treatments. Patient Prefer Adherence. 2015 Apr;:569. doi: 10.2147/ppa.s76139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pareja-Martínez E, Esquivel-Prados E, Martínez-Martínez F, García-Corpas JP. Questionnaires on adherence to antihypertensive treatment: a systematic review of published questionnaires and their psychometric properties. Int J Clin Pharm. 2020 Apr 05;42(2):355–365. doi: 10.1007/s11096-020-00981-x.10.1007/s11096-020-00981-x [DOI] [PubMed] [Google Scholar]
- 48.Liu C, Kuo K. Does information overload prevent chronic patients from reading self-management educational materials? Int J Med Inform. 2016 May;89:1–8. doi: 10.1016/j.ijmedinf.2016.01.012.S1386-5056(16)30012-0 [DOI] [PubMed] [Google Scholar]
- 49.Poushter J. Smartphone ownership and internet usage continues to climb in emerging economies. Washington: Pew Internet and American Life Profect; 2016. Feb 22, [2021-01-31]. https://www.pewresearch.org/global/wp-content/uploads/sites/2/2016/02/pew_research_center_global_technology_report_final_february_22__2016.pdf . [Google Scholar]
- 50.Taylor K, Silver L. Smartphone ownership is growing rapidly around the world, but not always equally. Washington: Pew Internet and American Life Project; 2019. Feb 05, [2021-01-31]. https://www.pewresearch.org/global/wp-content/uploads/sites/2/2019/02/Pew-Research-Center_Global-Technology-Use-2018_2019-02-05.pdf . [Google Scholar]
- 51.Ng WWM, Wong ASW, Cheung K. A cluster randomized controlled trial feasibility study of a WhatsApp-delivered intervention to promote healthy eating habits in male firefighters. Int J Environ Res Public Health. 2021 Jun 20;18(12):6633. doi: 10.3390/ijerph18126633. https://www.mdpi.com/resolver?pii=ijerph18126633 .ijerph18126633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Xiong S, Berkhouse H, Schooler M, Pu W, Sun A, Gong E, Yan LL. Effectiveness of mHealth interventions in improving medication adherence among people with hypertension: a systematic review. Curr Hypertens Rep. 2018 Aug 07;20(10):86. doi: 10.1007/s11906-018-0886-7.10.1007/s11906-018-0886-7 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Sensitivity analysis.


