Abstract
Objectives. To examine age and temporal trends in the proportion of COVID-19 deaths occurring out of hospital or in the emergency department and the proportion of all noninjury deaths assigned ill-defined causes in 2020.
Methods. We analyzed newly released (March 2021) provisional COVID-19 death tabulations for the entire United States.
Results. Children (younger than 18 years) were most likely (30.5%) and elders aged 64 to 74 years were least likely (10.4%) to die out of hospital or in the emergency department. In parallel, among all noninjury deaths, younger people had the highest proportions coded to symptoms, signs, and ill-defined conditions, and percentage symptoms, signs, and ill-defined conditions increased from 2019 to 2020 in all age–race/ethnicity groups. The majority of young COVID-19 decedents were racial/ethnic minorities.
Conclusions. The high proportions of all noninjury deaths among children, adolescents, and young adults that were coded to ill-defined causes in 2020 suggest that some COVID-19 deaths were missed because of systemic failures in timely access to medical care for vulnerable young people.
Public Health Implications. Increasing both availability of and access to the best hospital care for young people severely ill with COVID-19 will save lives and improve case fatality rates.
Deaths from “natural” causes (i.e., noninjury causes) that occur outside the hospital (OH) inpatient setting often represent lost opportunities for life-saving critical care. COVID-19 deaths that occur in the emergency department (ED) should be grouped with OH deaths, not with inpatient deaths as was done in 2 previous studies. 1 , 2 In the United States, most hospitals are permitted to treat and house patients in the ED for no more than 24 hours. After that time, patients must be either admitted as full inpatients or discharged, typically to home or a long-term care facility. Consequently, noninjury ED deaths are deaths for which critical care (i.e., rescue) was accessed too late.
During a pandemic, all deaths from the pandemic disease should be considered avoidable deaths, even deaths among the very elderly. Nonetheless, in public health it is common to describe deaths among patients who are younger than 65 years as “premature.” Premature OH and ED (OH/ED) deaths often are the result of longstanding and systematic barriers in access to high-quality medical care. Although elders aged 65 years and older experience the same barriers to high-quality hospital care as do younger patients, OH/ED deaths in this age group, particularly among those aged 85 years and older, may occur in a planned manner after a known illness and reflect the patient’s wishes for end of life care. 2
During the first pandemic year, COVID-19 fatalities were skewed very sharply toward elders. Nevertheless, there were more than 103 000 “premature” COVID-19 deaths that occurred among persons younger than 65 years in the United States during 2020. We examined age differences and temporal trends in OH/ED COVID-19 mortality, using death certificate tabulations released on a provisional basis by the National Center for Health Statistics (NCHS).
METHODS
We obtained 3 separate tabulations of deaths involving COVID-19 from NCHS in March 2021, each covering the 2020–2021 pandemic period for the entire United States. The place of death tabulation included all COVID-19 deaths, stratified by age group, month, year, and place of death. 3 The race/ethnicity tabulation included all COVID-19 deaths, stratified by age group and 7 combined categories of Hispanic ethnicity and race. 4 The cause of death tabulation included all deaths, stratified by year, age group, race/ethnicity, and selected underlying causes of death. 5 This file included data for both 2019 and 2020. We used CDC WONDER (Centers for Disease Control and Prevention Wide-ranging ONline Data for Epidemiologic Research) to access data on place of death for all noninjury decedents by age for calendar year 2019.
We analyzed 3 categories of place of death, defined as follows:
-
•
OH/ED deaths included the following places of death listed on the death certificate: ED, dead on arrival, decedent’s home, other, and place of death unknown.
-
•
Long-term care and hospice deaths included deaths that occurred in a hospice facility or nursing home or long-term care facility. Note that patients receiving hospice care at home would have place of death listed as decedent’s home.
-
•
Hospital inpatient deaths had medical facility–inpatient listed as the place of death.
RESULTS
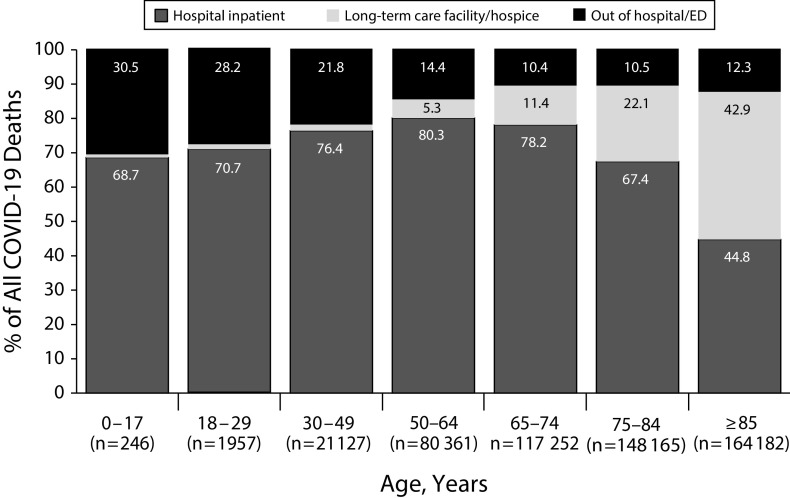
OH/ED deaths included all decedents who died in a hospital ED, en route to an ED, at home, or at another location outside a health care facility (e.g., workplace). Figure 1 shows the proportion of COVID-19 decedents who died OH/ED through March 2021 by age. Children were most likely to die OH/ED (30.5%), followed by young adults aged 18 to 29 years (28.2%). Elders were least likely to die OH/ED (10.4% to 12.3%).
FIGURE 1.
Place of COVID-19 Death, by Decedent Age: United States, January 2020–March 2021
Note. ED = emergency department.
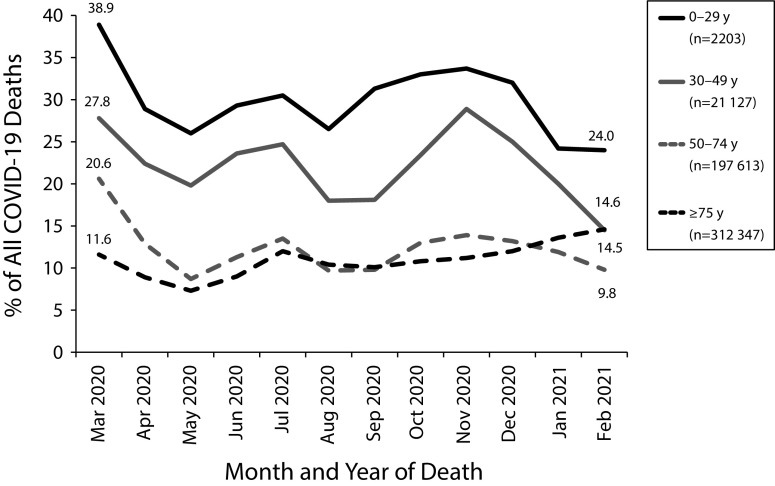
Temporal trends in OH/ED COVID-19 deaths by age are shown in Figure 2. The highest OH/ED proportions occurred in March 2020, when the pandemic was largely constrained to the greater New York City metropolitan area. After the first month, the age disparity in OH/ED deaths diminished little over time, and in February 2021, COVID-19 decedents aged 0 to 29 years were still 65% more likely to die OH than were older decedents.
FIGURE 2.
Percentage of COVID-19 Deaths Occurring out of Hospital or in the Emergency Department, by Decedent Age: United States, March 2020–February 2021
Comparison by age of OH/ED mortality for all “natural” causes in 2019 with the COVID-19 results for 2020–2021 revealed several interesting patterns (Figure A, available as a supplement to this article at https://www.ajph.org). First, the association of age with OH/ED mortality was very different in 2019. In contrast to findings for COVID-19, children had the lowest proportion of OH/ED deaths for all noninjury causes. Second, the proportion of children who died OH/ED from COVID-19 in 2020 was much higher than was the proportion of those who died OH/ED from noninjury deaths in 2019 (30.5% vs 19.1%). Finally, among adults, OH/ED death was proportionately more frequent in 2019 than it was in 2020.
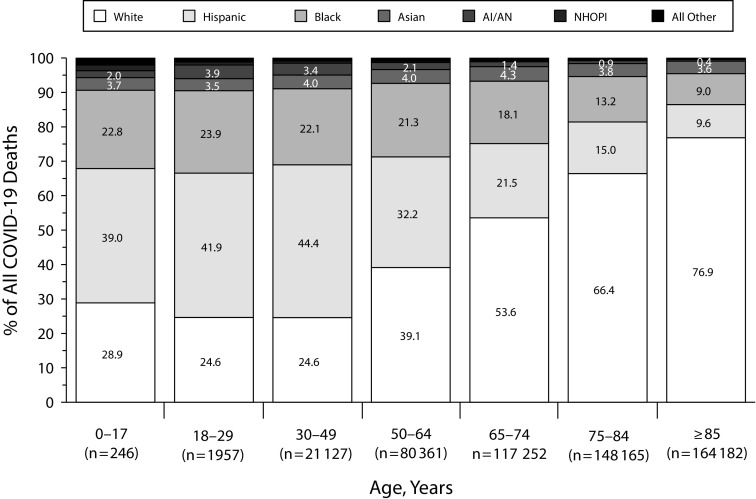
Place of death tabulations for COVID-19 decedents stratified by race and ethnicity have not yet been released, so we were unable to directly examine race/ethnicity disparities in OH/ED death. Figure 3 shows that among all COVID-19 decedents, race and ethnicity varied markedly by age: the majority of child decedents were non-White (39.0% Hispanic, 22.8% Black, 3.7% Asian, 2.0% American Indian/Alaska Native, 1.6% Native Hawaiian/other Pacific Islander, 0.8% more than one race). Similarly, only one quarter (24.6%) of young adult decedents (aged 18–29 years and 30–49 years) were non-Hispanic White. By contrast, the majority of elderly COVID-19 decedents were White.
FIGURE 3.
Race and Ethnicity of COVID-19 Decedents, by Age: United States, January 2020–March 2021
Note. AI/AN = American Indian/Alaska Native; NHOPI = Native Hawaiian or Pacific Islander.
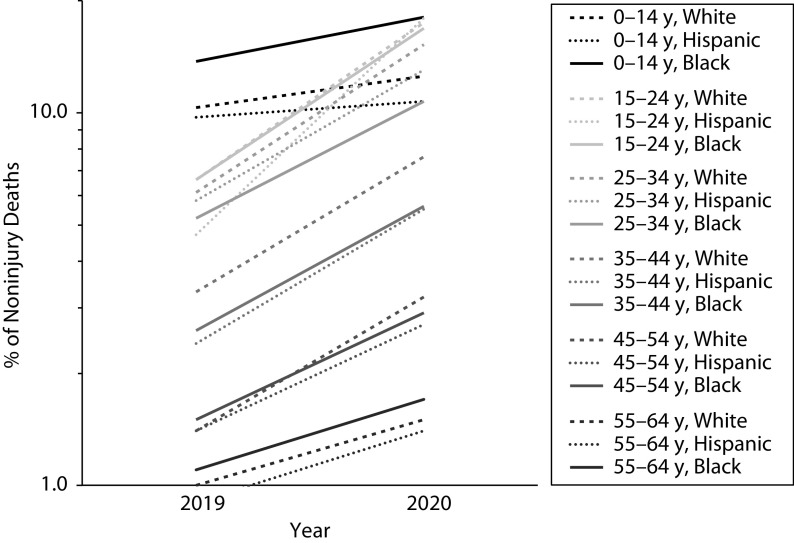
Symptoms, signs, and ill-defined conditions (SSID) are a group of nonspecific International Classification of Diseases, 10th Revision (ICD-10; Geneva, Switzerland: World Health Organization; 1992) codes used on death certificates when medical history is absent or is insufficient to confidently ascribe a specific disease as cause of death. 6 SSID is most frequently used for OH/ED deaths. Figure 4 depicts the level of SSID mortality by age and race/ethnicity and the change from 2019 to 2020 in the proportion of all noninjury deaths coded to SSID. Note that the logarithmic scale on the y-axis means that parallel trend lines result when the percentage change from 2019 to 2020 is the same for different groups. Children aged 0 to 14 years had the highest percentage of deaths coded to SSID in 2019, likely because of sudden infant death syndrome, which falls in the SSID ICD-10 codes. Percentage SSID increased from 2019 to 2020 in children of all racial/ethnic groups, with the strongest increase (from 13.7% to 18.0%) in Black children (Figure 4).
FIGURE 4.
Percentage of All Noninjury Deaths Coded to Symptoms, Signs, and Ill-Defined Conditions, by Age and Race/Ethnicity: United States, 2019 and 2020
The greatest increase in percentage SSID deaths among all age–race/ethnicity groups was among Hispanic adolescents and young adults aged 15 to 24 years, from 4.7% in 2019 to 17.9% in 2020 (Figure 4). Similarly, percentage SSID in Whites aged 15 to 24 years increased from 6.6% to 17.4% and in Blacks from 6.6% to 16.8%. Among adults of older age groups, percentage SSID increased similarly from 2019 to 2020 for all racial/ethnic groups, but absolute levels declined with age.
DISCUSSION
Taken together, the unlinked provisional data sources we analyzed reveal that child, adolescent, and young adult COVID-19 decedents were much more likely than were older decedents to die OH/ED and overall were predominantly racial and ethnic minorities. Although current data limitations preclude a definitive conclusion that racial and ethnic minorities are more likely than non-Hispanic Whites to die from COVID-19 OH/ED, our results support the need for priority investigation of this hypothesis.
In parallel, the relatively high proportions of all noninjury deaths among children, adolescents, and young adults that were coded to SSID in 2020 suggest that some COVID-19–involved deaths were missed because of systemic failures in timely access to medical care for vulnerable young people.
Premature, OH/ED COVID-19 deaths represent a failure of the medical care system to reach all critically ill patients with life-saving measures. 7 Barriers to accessing high-quality hospital medical care operate at multiple scales 8 , 9 : the individual person (e.g., lack of health insurance), the household level (e.g., lack of transportation, job and family responsibilities), and the community level (e.g., inadequate or geographically distant hospital facilities). Even in the absence of interpersonal discrimination, structural racism negatively affects non-White patients and families seeking hospital care through multiple mechanisms, including residential segregation. 10 , 11
Secondary to the consequences of barriers to quality care, OH/ED deaths also negatively affect the accuracy of cause of death coding on the death certificate. 12 When deaths are unattended or are witnessed only by laypeople, it can be very difficult for physicians to confidently ascribe a specific disease as the underlying cause of death. This is particularly true for decedents who had not received regular health care. SSID cause of death codes are not “garbage” codes, as some investigators have labeled them. 13 They are better thought of as “canary” codes—indications that the health care system has failed to provide adequate medical care at the end of life. 6 , 14 For example, a 120% increase in the incidence of OH cardiac arrest during the pandemic has been reported, 15 but the prevalence of SARS-CoV-2 infection in those individuals was unknown. One investigation in France found that 22% of those who died at home of cardiac arrest probably or definitely had COVID-19. 16
Limitations
The very recent death tabulations we analyzed in this study were generated by the NCHS from provisional death certificate files that have not been finalized. Additional deaths may be added for the study period, and individual death records may be modified if additional information becomes available, particularly about causes of death. NCHS has published a full discussion of data limitations online. 17 In addition, the NCHS definition of “COVID-19–involved deaths” includes only deaths for which COVID-19 is listed as an underlying or contributing cause of death. We did not include decedents who were known to have COVID-19 (i.e., had tested positive) but whose death certificate did not mention COVID-19. Currently, there is no centralized and complete data system that would permit the counting of these deaths.
Public Health Implications
Place of death data from the death certificate do not provide any information about the progression of episodes of care (in outpatient, ED, and inpatient settings) in the weeks and days immediately preceding death. Particularly for children, adolescents, and young adults, who have the greatest likelihood of surviving COVID-19 if they receive timely high-quality hospital care, we need further focused research and ongoing surveillance. Several priority research questions emerge from our findings. Had young people who eventually died OH/ER from COVID-19 been previously hospitalized and discharged with a positive prognosis? Had these patients visited an ED previously and been sent home? Are these decedents disproportionately located in geographic areas with fewer acute care hospital beds? To what degree have COVID-19 fatalities been miscoded to SSID?
In the second year of the pandemic, the United States still suffers from inadequate epidemiologic surveillance of COVID-19 incidence, severity, and fatality. The disparate effects of the pandemic on young people, racial and ethnic minorities, rural residents, and other vulnerable groups cannot be adequately understood or effectively ameliorated without rapid improvements in our surveillance systems and improved data transparency and availability. In particular, the timely release to nongovernmental researchers of full death certificate datafiles would broaden the scientific expertise and capacity available to investigate high-priority research questions.
More importantly, the case fatality rate for COVID-19 (regardless of which genetic viral variants are predominant at any given time and place) will always depend on the availability of both accurate medical evaluation and high-quality hospital medical care for severely ill patients. This is true despite the fact that no robust cure for COVID-19 has been identified yet. Multiple organ system pathologies engendered by the virus, still not well understood, often require life-saving rescue in the form of assisted ventilation, temporary renal dialysis, and resuscitation. Increasing both availability of and access to the best hospital care for young people severely ill with COVID-19 will save lives and could possibly reduce racial and ethnic disparities in mortality as well.
ACKNOWLEDGMENTS
The authors would like to thank Vickie Mays for helpful editorial suggestions.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to report.
HUMAN PARTICIPANT PROTECTION
This study used only publicly available, de-identified data sets and was therefore exempt from institutional review board review.
REFERENCES
- 1.Chuzi S, Molsberry R, McCabe ME, et al. Distribution in place of death for COVID-19–related mortality in the United States. J Am Geriatr Soc. 2020;68(9):1917–1918. doi: 10.1111/jgs.16721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chua IS, Shi SM, Levine DM. Place of death and end-of-life care utilization among COVID-19 decedents in a Massachusetts health care system. J Palliat Med. 2021;24(3):322–323. doi: 10.1089/jpm.2020.0674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. 2021. https://data.cdc.gov/NCHS/NVSS-Provisional-COVID-19-Deaths-by-Place-of-Death/4va6-ph5s
- 4.Centers for Disease Control and Prevention. 2021. https://data.cdc.gov/NCHS/Deaths-involving-coronavirus-disease-2019-COVID-19/ks3g-spdg
- 5.Centers for Disease Control and Prevention. 2021. https://data.cdc.gov/NCHS/AH-Monthly-provisional-counts-of-deaths-by-age-gro/r5pw-bk5t
- 6.Becker TM, Wiggins CL, Key CR, Samet JM. Symptoms, signs, and ill-defined conditions: a leading cause of death among minorities. Am J Epidemiol. 1990;131(4):664–668. doi: 10.1093/oxfordjournals.aje.a115550. [DOI] [PubMed] [Google Scholar]
- 7.Friedman J, Calderón-Villarreal A, Bojorquez I, Vera Hernández C, Schriger DL, Tovar Hirashima E. Excess out-of-hospital mortality and declining oxygen saturation: the sentinel role of emergency medical services data in the COVID-19 crisis in Tijuana, Mexico. Ann Emerg Med. 2020;76(4):413–426. doi: 10.1016/j.annemergmed.2020.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marco CA, Weiner M, Ream SL, Lumbrezer D, Karanovic D. Access to care among emergency department patients. Emerg Med J. 2012;29(1):28–31. doi: 10.1136/emj.2010.103077. [DOI] [PubMed] [Google Scholar]
- 9.Hill A, Schimmel Hyde J. Insurance coverage and access to care for workers with disabilities, 2001–2017. Disabil Health J. 2020;13(1):100843. doi: 10.1016/j.dhjo.2019.100843. [DOI] [PubMed] [Google Scholar]
- 10.Haider AH, Scott VK, Rehman KA, et al. Racial disparities in surgical care and outcomes in the United States: a comprehensive review of patient, provider, and systemic factors. J Am Coll Surg. 2013;216(3):482–492. doi: 10.1016/j.jamcollsurg.2012.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fiscella K, Sanders MR. Racial and ethnic disparities in the quality of health care. Annu Rev Public Health. 2016;37:375–394. doi: 10.1146/annurev-publhealth-032315-021439. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/data/nvss/vsrg/vsrg03-508.pdf
- 13.GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151–1210. doi: 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kulhánová I, Menvielle G, Bopp M, et al. Socioeconomic differences in the use of ill-defined causes of death in 16 European countries. BMC Public Health. 2014;14:1295. doi: 10.1186/1471-2458-14-1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lim ZJ, Ponnapa Reddy M, Afroz A, Billah B, Shekar K, Subramaniam A. Incidence and outcome of out-of-hospital cardiac arrests in the COVID-19 era: a systematic review and meta-analysis. Resuscitation. 2020;157:248–258. doi: 10.1016/j.resuscitation.2020.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hubert H, Baert V, Beuscart JB, Chazard E. Use of out-of-hospital cardiac arrest registries to assess COVID-19 home mortality. BMC Med Res Methodol. 2020;20(1):305. doi: 10.1186/s12874-020-01189-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/nvss/vsrr/covid19/tech_notes.htm