Abstract
A case of testicular metastasis of colon cancer, which clinically mimicked a hydrocele of the testis, is presented. Imaging study suggested a scrotal hydrocele, but slow yet gradual enlargement of the hydrocele and the past history of colon cancer prompted an orchiectomy for the pathologic diagnosis and treatment. The pathologic diagnosis was testicular metastasis of colon cancer. Testicular metastasis presenting as a hydrocele is unusual, and imaging and macroscopic findings useful for the differential diagnoses are discussed. A brief review of pertinent literature is also included.
Keywords: Colon cancer, Hydrocele, Metastasis, Testis
1. Introduction
Testicular metastasis of cancer is uncommon, which is confusing with primary neoplasm of the testis.1,2 Pathologic diagnosis is challenging if the pathologists are unaware of the presence of primary malignancies. Unless properly informed of the primary tumour, testicular metastases may be misdiagnosed. However, testicular metastases usually have solid tumour, so the diagnosis of testicular tumour, whether primary or secondary, is clinically obvious. Testicular metastasis mimicking a hydrocele is exceedingly rare, with several reported cases to date in the English literature.3, 4, 5 We experienced a case, which had a past history of colon cancer, was clinically suspected of a scrotal hydrocele, but was pathologically diagnosed as metastasis from colon cancer. Helpful clues in imaging surveys to reach the correct diagnosis are discussed with a brief review of relevant literature.
2. Case presentation
A 76 year-old man with a past history of colon cancer noticed painless swelling of his right scrotum. Sixteen months before, the patients underwent colectomy for sigmoid colon cancer. The pathologic diagnosis was moderately differentiated adenocarcinoma with peritoneal/omentum dissemination, retroperitoneum invasion, and metastases to the regional lymph nodes and the liver. Left ureter was spared from tumour invasion, but testicular artery and vein were involved by the tumour. Adjuvant therapy consisting of 5-fluorouracil/irinotecan + panitumumab failed to achieve response. With the emergence and subsequent progression of the scrotal hydrocele, orchiectomy was performed for the pathologic diagnosis of the hydrocele and the remedy of right inguinal hernia. Macroscopically, the orchiectomy specimen consisted of multi-locular thin-walled cysts, which was apparently resembled with testicular hydrocele. However, with close observation, small polyp-like tubercles were occasionally observed on the cyst walls (Fig. 1A and B). Histologically, these polypoid lesions were composed of nests of moderately differentiated tubular adenocarcinoma filled with luminal eosinophilic necrosis (Fig. 2A). Within the cyst walls, which were thin and smooth to the naked eye, moderately differentiated adenocarcinoma was seen together with seminiferous tubules (Fig. 2B). Immunohistochemically, these tubular adenocarcinomas were positive for CDX-2 (not shown). These findings confirmed that this testicular ‘hydrocele’ was a testicular metastasis of colon cancer.
Fig. 1.
A,B. Macroscopic appearance of the excised ‘hydrocele’ of the testis. Note that the testis is consisted of multi-locular this-walled cysts. The cysts wall is smooth, but small papillary protrusions (arrowhead) were noted. (bar = 2 cm).
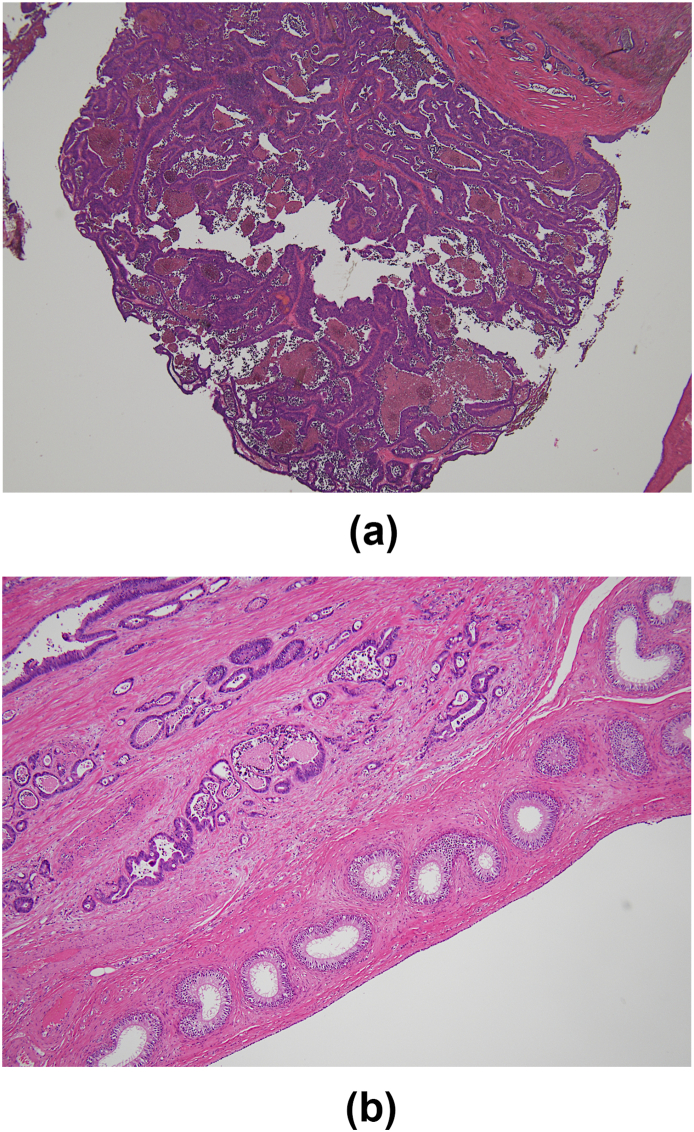
Fig. 2.
Histology of the resected ‘hydrocele’ of the testis. A Moderately differentiated adenocarcinoma seen in the papillary lesion. The lumen is filled with eosinophilic necrosis. (corresponding to one of the arrowhead in Fig. 1). B Moderately differentiated adenocarcinoma (left upper) and vestigial seminiferous tubules (right lower) observed in the wall of the thin cyst. Right lower is the inner side of the cyst. Note that the seminiferous tubules are arranged as a thin layered manner, and tubular adenocarcinomas proliferated in the stroma behind. (A,B Haematoxylin and eosin stain, × 200).
3. Discussion
Cancer metastasis to the testis is uncommon. It is occasionally detected as an incidental finding in the autopsy cases of advanced cancer. Testicular metastases from various primary cancers during the course of cancers have been reported as case reports and summarized in reviews.1, 2, 3, 4, 5 Testicular metastases of cancer mimicking as hydrocele are exceptionally rare. Only several cases have been described in English literature so far.3, 4, 5 Of these, some of the hydrocele-like metastases were an epididymal cyst3 or were located adjacent to the epididymis.5 In one case, a solid tumour within the testis was also detected.3 Our case was unusual in that whole right testis became multi-cystic. As seen in Fig. 1, macroscopically no solid tumour was present within the lesion. Because no tumour was depicted by imaging studies before the operation, we were not confident whether this ‘hydrocele’ was malignant.
Histologically, both moderately differentiated tubular adenocarcinoma and seminiferous tubules were recognized within the cyst wall (Fig. 2B). This meant that the ‘hydrocele’ seen in our case was really a testicular metastasis. This form of testicular metastasis was deceptively confusing with a hydrocele. However, small papillary tubercles on the cyst wall may be a useful finding for suspecting a neoplastic lesion. These small polypoid lesions might be visualized by meticulous manoeuvring of the ultrasound probe or with thin-slice CT. The cyst walls were thin and smooth in our case. However, if the walls were irregularly thickened, the possibility of a malignant cystic tumour should be reminded. These findings, when clearly depicted by imaging, may be a valuable guide for the diagnosis.
The route of testicular metastasis is considered as propagation with arterial blood flow, retrograde venous spread, lymphatic invasion, via vas deferens to the epididymis, or through patent tunica vaginalis.4 In our case, the route of spread to the testis was not determined. As lymphatic invasion was recognized in the surgical specimens, testicular artery/vein was involved, and peritoneal dissemination were present at the time of colectomy, it is possible that the cancer cells might be seeded to the testis either route mentioned above. However, it is unclear why the metastasis did not form solid tumour in the testis and develop hydrocele-like cysts in our case. The testicular metastasis might somehow cause fluid retention, which transformed testicular parenchyma into multi-cystic lesion, and displaced seminiferous tubules in the thin wall of the cysts arranged as a rim-like manner.
Interestingly, scrotal metastases that developed as a ‘hydrocele’ were all right-sided,3, 4, 5 as well as our case. However, it is unclear whether this right-side preference is just a coincidence or determined by yet unknown anatomical factor(s).
The tumours reported to metastasize to the testis are prostate, melanoma, kidney, colon, urinary tract, lung, oesophagus, stomach, etc.1,2 Of these, colon cancer is the third1 and fourth2 frequent. Thus the possibility of testicular metastasis from colon cancer should be raised as a differential diagnosis when a tumour in the scrotum is clinically suspected especially when there is the past history of colon carcinoma.
In summary, a case of testicular metastasis from colon cancer that was clinically confusing with hydrocele of the testis is described. Macroscopically, the metastatic lesion simulated hydrocele of the testis. However, small polypoid tubercles were observed on the cyst walls, which were pathologically diagnosed as moderately differentiated adenocarcinoma. When encountered a testicular hydrocele in a case with past history of malignancy, scrupulous imaging studies is mandatory.
Statement of ethics
Written informed consent to publish case report was obtained from the patient.
Funding sources
None to be declared.
Author contributions
Takahiko Sakuma was responsible for the pathologic investigation and gross/histological diagnosis.
Koutarou Aoki, Masanori Ando, Kenichi Inaoka, Takeshi Ito and Katsuya Yamashitawere involved in the clinical diagnosis, operation and procurement of the surgical material, and patient care.
All the authors have contributed to the preparation of the manuscript.
Declaration of competing interest
The authors have no conflicts of interest to declare.
References
- 1.Haupt H.M., Mann R.B., Trump D.L., Abeloff M.D. Metastatic carcinoma involving the testis. Clinical and pathologic distinction from primary testicular neoplasms. Cancer. 1984;54(4):709–714. doi: 10.1002/1097-0142(1984)54:4<709::aid-cncr2820540419>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 2.Ulbright T.M., Young R.H. Metastatic carcinoma to the testis: a clinicopathologic analysis of 26 nonincidental cases with emphasis on deceptive features. Am J Surg Pathol. 2008;32(11):1683–1693. doi: 10.1097/PAS.0b013e3181788516. [DOI] [PubMed] [Google Scholar]
- 3.Charles W., Joseph G., Hunis B., Rankin L. Metastatic colon cancer to the testicle presenting as testicular hydrocele. J Clin Oncol. 2005;23(22):5256–5257. doi: 10.1200/JCO.2005.06.109. [DOI] [PubMed] [Google Scholar]
- 4.Hanash K.A., Carney J.A., Kelalis P.P. Metastatic tumors to testicles: routes of metastasis. J Urol. 1969;102(4):465–468. doi: 10.1016/s0022-5347(17)62174-8. [DOI] [PubMed] [Google Scholar]
- 5.Højgaard Rasmussen H., Schrøder P. Testicular hydrocele: an initial sign of colon carcinoma. Case report. Acta Chir Scand. 1988;154(1):65–66. [PubMed] [Google Scholar]