Abstract
Objective:
To determine and evaluate the accuracy of methods physicians use to detect diagnostic criteria for pediatric hypertension (hypertensive BPs on ≥3 occasions) in electronic health records (EHRs).
Methods:
Methods used by pediatric-trained physicians (n=12) to detect diagnostic criteria for hypertension in a simulation using a child’s EHR data were directly observed, timed, and evaluated for accuracy. All physicians were given the same information regarding diagnostic criteria to eliminate knowledge gaps. Then, computer modeling and EHR data from 41,654 3–18-year-olds were used to simulate and compare the accuracy of detecting hypertension criteria using an observed-shorthand method vs. the guideline-recommended/gold-standard method.
Results:
No physician used the guideline-recommended method of determining multiple time-of-care hypertension thresholds for child age/height at the time of each BP measure. One physician estimated the child’s BP diagnosis without computing thresholds; 11/12 physicians determined the child’s hypertension threshold from age/height data at the time of a current visit and applied/imputed this threshold to BP measured at all visits (current-visit threshold used to assess historical-visit BPs) to detect three separate BP elevations. Physicians took 2.3 minutes (95% CI, 1.5–3.0) to declare a diagnosis. Sensitivity was 83.1% when applying the current-visit threshold to detect the guideline-recommended-BP-threshold diagnosis using EHR data. Specificity and positive-/negative-predictive values ranged from 98.5–99.9%.
Conclusions:
Physicians applied a shorthand method to evaluate pediatric BPs. Computer-simulated comparison of the shorthand and guideline methods using clinical data suggests the shorthand method could yield an inaccurate impression of a child’s BP history in 17% of pediatric ambulatory visits.
Condensed Abstract
Complex computation of blood-pressure thresholds during outpatient visits has been cited as an impediment to diagnosing pediatric hypertension. Guidelines recommend clinicians recognize blood pressures exceeding hypertension thresholds at ≥3 separate visits. It was unclear if physicians use this method.
Observation of physicians identified use of a single hypertension threshold indexed to a child’s age and height at an active visit, not the threshold for age/height at the time of previous visits to detect if a child meets diagnostic criteria for hypertension. Comparison of this practical-though-imperfect method with the guideline-recommended method revealed physicians may miss many children meeting guideline-recommended hypertension criteria.
Keywords: clinical decision support, diagnostic validity, electronic health record
Pediatric providers fail to recognize high blood pressure (BP) in 46–90% of children with elevated BPs.1–3 Diagnostic errors – failures to establish the correct diagnosis given the opportunity – cause patient harm.4–7 By the time pediatric hypertension is finally diagnosed, 20–40% of children already have developed left ventricular hypertrophy.8,9 A potential barrier to diagnosing pediatric hypertension is the complex computation of BP thresholds10,11; clinicians must confirm a child has hypertension by identifying hypertensive BPs – an average systolic or diastolic BP (SBP/DBP) ≥95th percentile – on three or more occasions.10,11
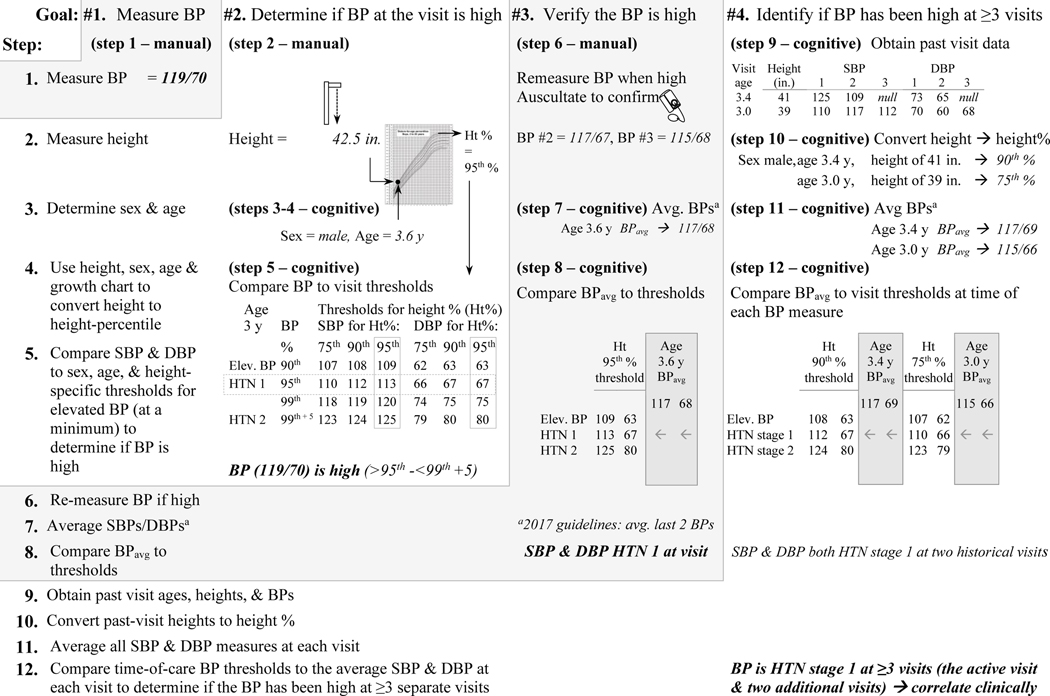
Electronic health records (EHRs) may improve pediatric hypertension detection.10 The EHR can be customized to transform height to height-percentile using age and sex, average BP measures obtained at a visit, and reference active guideline-based thresholds to evaluate if a child’s BP is hypertensive (Figure 1).10,11 In trials of EHR alerts, these customized functions have increased re-measuring high BPs and alerted clinicians to BP elevations at a single visit.12–15
Fig. 1.
Tasks and task steps to determine hypertension criteria in children using guideline-based criteria without computation/automation: three steps are manual/physical (cannot be automated) and nine are cognitive/mental steps (amenable to automation and use for clinical confirmation)a
aNote that the 2017 updated guideline recommends averaging the last two BP measures which ideally should be obtained using the auscultatory method (using a sphygmomanometer). The Fourth Report states ’If the [first measured] BP is >90th, the BP should be repeated twice at the same office visit, and an average SBP and DBP should be used (e.g., the Fourth Report does not specify whether to average all BP measures or only the last two).10,11
A remaining challenge is identifying ≥3 incident BP elevations to prompt a clinician to consider if a child meets criteria for hypertension diagnosis.10,11 To date, only one clinical decision support (CDS) system has aided hypertension diagnosis upon a child having a confirmed third BP elevation, but the system calculates past BP% thresholds using the most recent height percentile.14,16 Guidelines recommend using BP% thresholds calculated at each visit using contemporaneous measures of BP, height, and age.10,11
Use of a child’s most recent height and BP% threshold (vs. using height at each visit to compute separate thresholds) might result in a diagnostic error (under/over-diagnosis).17 We observed physicians evaluate if a child met diagnostic criteria for hypertension. Then, we performed a study to determine the accuracy of detecting BP% elevations using the observed method of applying a single BP% threshold calculated using height and age at one visit vs. three discrete BP% thresholds calculated using contemporaneous measures of BP, height, and age.
METHODS
Workflow observation.
To inform the design of a pediatric hypertension CDS system, we used workflow observations to identify tasks that were manual (and could not be automated) vs. cognitive and amenable to computation using CDS.18 Cognitive tasks include referencing information, performing calculations, or having to commit information to memory.19 Pediatric-trained physicians who were participating as stakeholders and volunteers (and care for children at clinics within a large pediatric health system where the CDS was to be piloted) were asked to talk out loud while identifying criteria for pediatric hypertension during a simulated outpatient visit. The simulated case was an 11-year-old with three past visits, 2–3 recorded BPs at each visit, and average SBPs at three visits that each exceeded the threshold for hypertension. No identifiable information about the physicians was collected.
Physicians were observed and stopwatch-timed while completing the following: “Determine if this [simulated] patient [in an EHR test environment] has a hypertensive BP at the visit or meets criteria for a hypertension diagnosis defined as hypertensive BPs at three separate visits.” All physicians were given the same definitions and diagnostic criteria to eliminate any knowledge gaps about diagnosis. For example, thresholds for elevated (termed “prehypertensive” per Fourth-Report guidelines) and hypertensive BPs, and the need for three separate visits with hypertensive BPs to diagnose hypertension were defined verbally in advance. Three diagnostic options were given: BP elevated at the visit (but not hypertensive), hypertensive at the visit but <3 visits with hypertensive BPs, hypertensive at ≥3 separate visits (meets criteria for hypertension diagnosis), or normal. Volunteers started with the EHR opened to the test patient’s visit.
The observer (C.T.) started the stopwatch when the physician stated he/she was ready, manually recorded each screen navigated by the physician, physician comments, and whether the physician determined thresholds for hypertension at the active visit and for each of the past visits. When the physician stated the BP diagnosis, the observer recorded the time and documented the diagnosis. Workflow elements that were recorded included number of computer screens navigated (for example, vital-sign flowsheet to progress note equals two screens), and methods used to view BP information and calculate BP thresholds. We observed additional physician volunteers until no novel workflows for determining BP diagnosis were observed in three consecutive observations.
Computer-Modeling Study.
Based on observations from the workflow-observation project that suggested most physicians were calculating a single hypertension threshold using the height and age at the time of care, we conducted a computer-modeling study using retrospective, longitudinal EHR data from 3–18-year-olds followed in 54 primary-care clinics (in academic, community, and private-practice settings in Dallas, Texas from May 2009 to July 2016). BP data that are stored in the EHR are collected by trained nurses or medical assistants using automated oscillometric devices to measure BP after a patient sits at rest 3–5 minutes. Measurements are repeated if the initial BP exceeds the 95th percentile. Clinicians are encouraged to use auscultation to confirm a high BP. The EHR data were used to determine the diagnostic accuracy (true positives and negatives) of detecting three discrete BP% elevations using a single BP% threshold calculated using the most current measure of BP, height, and age obtained at the point of care, compared to the guideline-recommended method of using three separate hypertension thresholds each calculated using contemporary measures of BP, height, and age. The study was approved by the UTSW IRB.
The computer-modeling study aimed to compare the accuracy of detecting three discrete BP% elevations using a single/point-of-care BP% threshold compared to three time-of-care hypertension thresholds. Inclusion criteria were: child followed in one of the primary-care clinics that stored data in a single common EHR; BP, age, sex, and height data at ≥3 visits to calculate BP%; and child age 3–18 years at a visit with ≥2 preceding visits with data to calculate BP% (age, height, BP). Extracted EHR data included primary-care visits with associated dates and measures of age, height, and the lowest recorded BP measure. For simplicity, the study excluded data regarding BP re-measurement, prior hypertension diagnosis, or BP medications. Cohort data were de-identified with an identifiable link (through a HIPAA waiver) to patient charts to probe for reasons for discrepant diagnoses between the single-threshold and guideline-based methods.
Algorithms.
We developed two computational algorithms to simulate use of a single BP% threshold vs. the guideline-recommended method of using three discrete BP% thresholds.11 Each algorithm computed thresholds for BP categories. For simplicity, we focused on detecting criteria for hypertension stage 1, BP ≥95th percentile, in accordance with the Fourth Report guidelines active at the time the BPs were collected (primary outcome).11 Recognizing new guidelines and thresholds were published in 2017, we also simulated use of a single BP% threshold vs. BP% thresholds at the time of each BP measure according to 2017 AAP-guideline-recommended thresholds.10
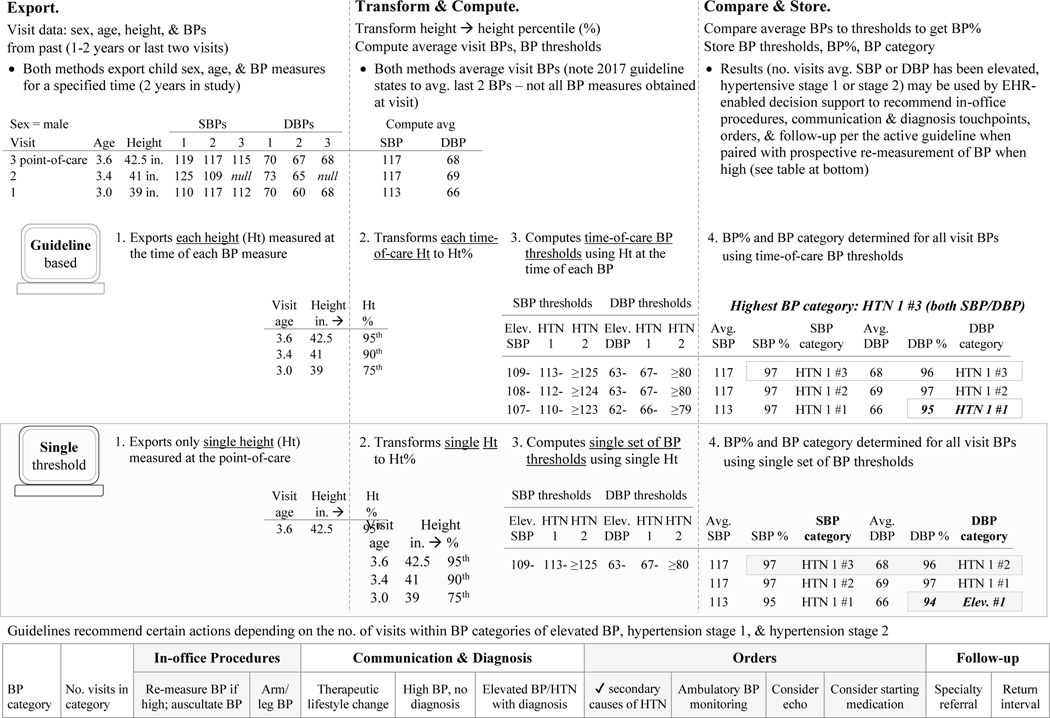
The single-threshold algorithm (modeled on observed physician behavior) determined BP elevations exceeding the hypertension threshold at past visits using the threshold calculated from the most recent visit’s height/age (Figure 2). The time-of-care-threshold algorithm calculated individual hypertension thresholds for each visit using contemporaneous BP, age, and height measures. Time-of-care thresholds were calculated by harnessing height/age from historical visits (stored in EHRs) to calculate historical BP-percentile thresholds (not stored in EHRs).
Fig. 2.
Steps to determine hypertension criteria in children with computation using the single-threshold method and the guideline-based method
Both algorithms used a BP measured at a primary-care visit as the point of reference and determined hypertension criteria by looking at BPs measured at primary-care visits within the past two years. The rationale for using BPs at visits within two years of the reference BP was that the TeenBP hypertension CDS trial defined participants as meeting diagnostic criteria for hypertension based on hypertensive BPs at three visits within a two-year period.16
Diagnostic Performance.
The primary outcome was diagnostic accuracy of the single-threshold algorithm to detect three time-of-care (guideline-recommended) hypertensive BP elevations. Diagnostic accuracy of the single-threshold algorithm was compared to the guideline-based algorithm for determining hypertension from the perspective of the (1) clinician seeing a patient at a clinic visit (BP exceeding hypertension threshold at the visit plus at ≥2 preceding historical visits within two years of the visit) and (2) health system considering possible missed diagnoses of hypertension among a population of unique children (defined using all of each patient’s visits and looking for any two-year period in which hypertension criteria were met).
Analysis.
Sociodemographic characteristics of children in the retrospective cohort were extracted for the third visit, which would be the first opportunity to determine if hypertension diagnostic criteria were met.10,11 Diagnostic accuracy for detecting hypertension using the single-threshold approach compared to the guideline-based approach was calculated as sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) using standard definitions and methods.20 SAS PROC GENMOD (version 9.4, Cary, NC) with a compound symmetry correlation structure was used to construct 95% confidence intervals (CIs) that accounted for intra-individual correlation between visits. The reason for a discrepancy in diagnosis between algorithms was investigated by computing test characteristics stratified by child age (<13 years vs. 13+ years) and the presence of a height outlier (defined as a height 2 standard deviations above or below the mean).
RESULTS
Twelve pediatric physicians completed the exercise with the simulated patient who met criteria for hypertension diagnosis. None used the guideline-recommended time-of-care-threshold method to determine the BP diagnosis. All physicians stated that they use the lowest recorded BP measure at a visit (vs. the average of all BPs recorded) to evaluate a child’s BP. On average, it took physicians 2.3 minutes (SD 65) to declare the BP diagnosis. Observed workflow patterns each started with review of BPs in a visit-encounter flowsheet (that included measured BPs at the current and historical visits) and ended with the physician stating the diagnosis. There were four observed workflow patterns:
Approximation (n=1 physician, 1 EHR/computer screen, 3 task-steps, and 30 seconds to determine diagnosis): in the vital-sign flowsheet, the physician reviewed the child’s BPs at the visit and historical visits and stated that the child appeared to have an elevated BP reading, but probably not hypertension (no threshold computed).
Use of one automated smart phrase (n=6 physicians, 7 task-steps, 3 EHR screens, and 96–120 seconds to diagnosis): from the visit flowsheet/BP review, the physician opened a progress note, navigated to the physical-exam section of the note, typed a smart phrase to calculate the current visit threshold for hypertension, compared the threshold to the visit BP, returned to the visit flowsheet, then evaluated whether BPs from historical visits shown in the visit flowsheet exceeded the visit threshold for hypertension.
Use of two automated smart phrases (n=4 physicians, 9 task-steps, 3 screens, and 138–180 seconds): the workflow described above with one additional smart phrase that pulled in BP measures from the child’s last three visits. The physician used the calculated hypertension threshold for the visit to evaluate the current visit BP and the past visit BPs, then returned to the visit flowsheet to compare the current visit threshold to all historical BPs shown in the visit flowsheet; and,
Manual (n=1 physician, 17 task-steps, 8 screens, and 300 seconds): after viewing the BPs in the visit flowsheet, the physician went online, opened a search engine, typed in pediatric BP lookup tables, and selected a link that opened the tables. The physician returned to the chart, verified age and sex, opened the growth chart, clicked on the height curve, and identified the child’s height percentile. Returning to the online BP lookup tables, the sex, age, and height percentile were used to determine a single BP threshold for SBP and another for DBP which the physician wrote on a piece of paper. The physician returned to the chart, selected a navigation pane to open a “review flowsheets” screen that contained all ambulatory BPs measured within the health system (whereas the visit flowsheet only presents BP measures collected at the visit location), then evaluated the visit threshold for hypertension to BPs from historical visits in the flowsheet.
Only the provider using the complete approximation approach stated an inaccurate diagnosis. The physician stated that the child appeared to have an elevated BP, but not hypertension.
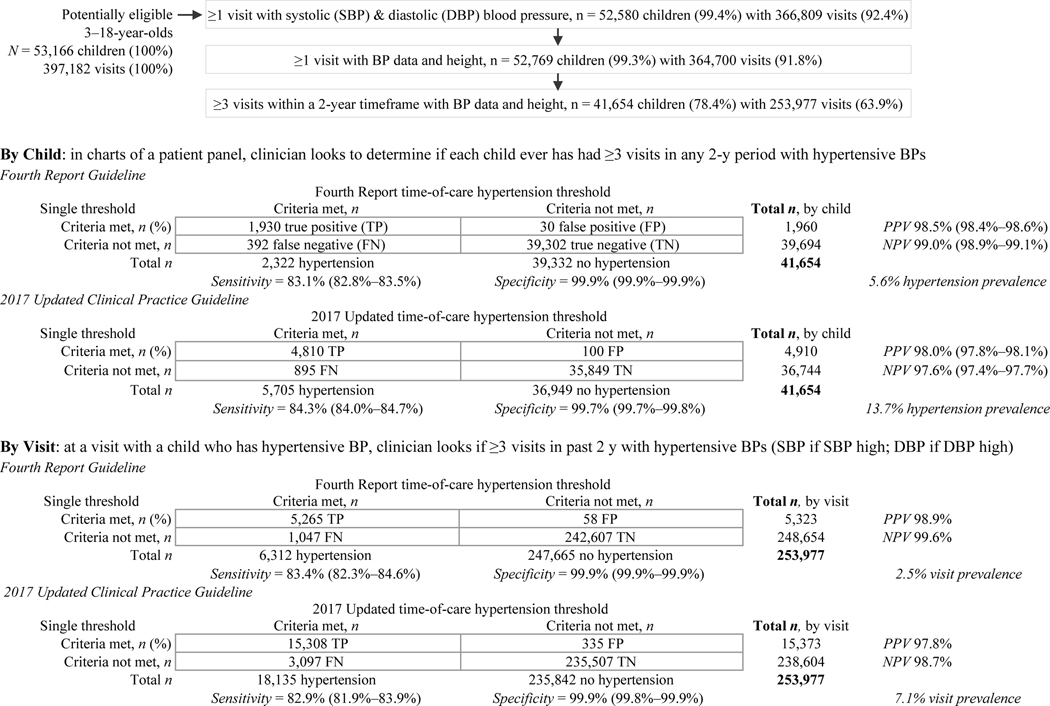
The cohort for the computer-modeling study included 41,654 unique patients with ≥3 primary-care visits and sufficient data at each visit to compute time-of-care BP-percentile thresholds (Figure 3). Most children (82.4%) were younger than 13 years old; just over half were female; nearly one-quarter were African American, almost half were Latino; 38.7% had a BMI ≥85th percentile; and 54% were followed at community and private-practice clinics, with the remainder at academic clinics (Table 1).
Fig. 3.
Participant flow witxh comparison of the performance of the single-threshold algorithm vs. the reference standard - the guideline-based time-of-care algorithm - for detecting pediatric hypertension criteria using the Fourth Report and (separately) the 2017 Updated Clinical Practice Guideline
Table 1.
Cohort characteristics (N = 41,654)
| Characteristic | Category | Sample No. | Proportion |
|---|---|---|---|
|
| |||
| Age category | |||
| 3 – 12 years | 34,321 | 82.4% | |
| 13 years and older | 7,333 | 17.6% | |
|
| |||
| Sex | |||
| Male | 20,391 | 49.0% | |
| Female | 21,263 | 51.0% | |
|
| |||
| Race/ethnicity | |||
| African American | 9,872 | 23.7% | |
| Latino, white | 18,717 | 44.9% | |
| Non-Latino, white | 6,455 | 15.5% | |
| Other/unknown | 6,610 | 15.9% | |
|
| |||
| BMI category | |||
| Below 85th percentile | 25,436 | 61.1% | |
| Overweight | 6,940 | 16.7% | |
| Obesity | 9,180 | 22.0% | |
| Missing | 98 | 0.2% | |
|
| |||
| Clinic site | |||
| Academic practices | 19,148 | 46.0% | |
| Community & private practices | 22,506 | 54.0% | |
At third visit in cohort – the first opportunity that a child had three separate visits with a blood pressure measurement at which diagnostic criteria for hypertension could potentially be fulfilled.
Using the Fourth Report guideline-based algorithm, diagnostic criteria for hypertension were fulfilled in 5.6% of unique children and at 2.5% of patient encounters (Figure 3). In other words, at 2.5% of visits, a child had a hypertensive BP at the time of care and at two separate visits in the preceding two years; 5.6% of unique children had a hypertensive BP at a reference visit plus two additional separate visits within any contiguous two-year period. Using the updated 2017 guideline, diagnostic criteria for hypertension were fulfilled in 13.7% of unique children and at 7.1% of patient encounters.
Accuracy of Single-Threshold Algorithm.
Using the Fourth-Report guideline, the sensitivity of the single-threshold approach to detect hypertension criteria in a unique child was 83.1% and at a patient encounter was 83.4%; the specificity was 99.9% for both a unique child and visit (Figure 3). The PPV (proportion of patients/visits that test positive and had three hypertensive BPs) was 98.5% for a child and 98.9% for a visit. NPV (proportion of patients/visits that test negative) was 99.0% for a child and 98.9% for a visit. Using the 2017 guideline, the sensitivity of the single-threshold approach to detect hypertension criteria was 84.3% for a child and 82.9% for a patient encounter; the specificity was 99.7% for a unique child and 99.9% for a visit. The PPVs for a child (98%) and visit (97.8%) were comparable. The NPV was 97.6% for a unique child and 98.7% for a visit.
In a unique child, using either the 2004 or 2017 guideline, the single-threshold approach’s sensitivity to detect hypertension criteria was higher for children ages 13 years and older (vs. 3–12 years, Table 2a); for example, the sensitivity was 100% for age 13+ years vs. 83% for ages 3–12 years when using the 2017 guideline. Sensitivity was higher in the presence of a height outlier for the Fourth Report guideline and in the absence of a height outlier for the 2017 guideline. Specificity varied by age (0.3% higher for age 13+ y) and height (0.4% higher in the absence of a height outlier) for the 2017 guideline but not the 2004 guideline.
Table 2a.
For unique child, association of age category & height outliers and the sensitivity/specificity of the single-threshold approach vs. the guideline-recommended approach (reference standard) for determining hypertension (HTN)
| Threshold | Ref. | Threshold | Ref. | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sub- | 2004 guideline | Sensitivity | Specificity | 2017 guideline | Sensitivity | Specificity | |||||
|
|
|
||||||||||
| group | Category | Single | HTN | No HTN | 95% CI | 95% CI | Single | HTN | No HTN | 95% CI | 95% CI |
| Age | <13 y | HTN | 1,735 | 25 | 82.3% | 99.9% | HTN | 4,360 | 100 | 83.0% | 99.7% |
| No HTN | 372 | 32,105 | 82.0%–%82.7 | 99.9%–99.9% | No HTN | 895 | 28,882 | 82.6%–83.3% | 99.6%–99.7% | ||
|
|
|||||||||||
| 13+ y | HTN | 195 | 5 | 90.7% | 99.9% | HTN | 450 | 0 | 100% | 100% | |
| No HTN | 20 | 7,197 | 90.4%–91.0% | 99.9%–99.9% | No HTN | 0 | 6,967 | %–% | %–% | ||
|
| |||||||||||
| Height | No outlier | HTN | 1,665 | 27 | 82.7% | 99.9% | HTN | 4,208 | 81 | 85.6% | 99.8% |
| outlier a | No HTN | 349 | 35,469 | 82.3%–83.0% | 99.9%–99.9% | No HTN | 709 | 32,512 | 85.3%–85.9% | 99.7%–99.8% | |
|
|
|||||||||||
| Any outlier | HTN | 265 | 3 | 86.0% | 99.9% | HTN | 602 | 0 | 76.4% | 99.4% | |
| No HTN | 43 | 3,833 | 85.7%–%86.4 | 99.9%–99.9% | No HTN | 186 | 3,337 | 76.0%–76.8% | 99.4%–99.5% | ||
Height outlier present at visit or at a visit with blood pressure within the 730 days before the visit.
For a unique visit, the single-threshold approach had a higher sensitivity to detect hypertension among older children (13+ years vs. 3–12 years) for both guidelines, and when height outliers were absent for the 2017 guideline (Table 2b). At the visit level using the Fourth Report guideline, the sensitivity of the single-threshold approach did not differ when a height outlier was present, and specificity was not affected by age or height outliers. Using the 2017 guideline, specificity did not differ by age, but was 0.3% higher when height outliers were absent.
Table 2b.
For unique visit, association of age category & height outliers and the sensitivity/specificity of the single-threshold approach vs. the guideline-recommended approach (reference standard) for determining hypertension (HTN)
| Threshold | Ref. | Threshold | Ref. | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sub- | 2004 guideline | Sensitivity | Specificity | 2017 guideline | Sensitivity | Specificity | |||||
|
|
|
||||||||||
| group | Category | Single | HTN | No HTN | 95% CI | 95% CI | Single | HTN | No HTN | 95% CI | 95% CI |
| Age | <13 y | HTN | 4,332 | 46 | 82.7% | 99.9% | HTN | 13,174 | 335 | 81.6% | 99.8% |
| No HTN | 908 | 202,251 | 81.4%–84% | 99.9%–99.9% | No HTN | 2,967 | 191,061 | 80.5%–82.7% | 99.8%–99.8% | ||
|
|
|||||||||||
| 13+ y | HTN | 933 | 12 | 87% | 99.9% | HTN | 1,864 | 0 | 93.5% | 100% | |
| No HTN | 139 | 45,356 | 84.6%–89.5% | 99.9%–99.9% | No HTN | 130 | 44,446 | 92.2%–94.8% | NA | ||
|
| |||||||||||
| Height | No outlier | HTN | 4,201 | 35 | 83.1% | 99.9% | HTN | 12,255 | 227 | 86.1% | 99.9% |
| outlier a | No HTN | 853 | 217,043 | 81.8%–84.4% | 99.9%–99.9% | No HTN | 1,977 | 207,673 | 85.4%–86.8% | 99.9%–99.9% | |
|
|
|||||||||||
| Any outlier | HTN | 1,064 | 23 | 84.6% | 99.9% | HTN | 2,783 | 108 | 71.3% | 99.6% | |
| No HTN | 194 | 30,564 | 82%–87.1% | 99.9%–99.9% | No HTN | 1,120 | 27,834 | 68.0%–74.7% | 99.5%–99.7% | ||
Height outlier present at visit or at a visit with blood pressure within the 730 days before the visit.
DISCUSSION
Workflow observations suggest that determining whether a child meets criteria for diagnosis of hypertension takes >2 minutes/patient, and when physicians compute a threshold, they may incorrectly apply the BP% threshold at the visit to BPs at historical visits. Most tasks to identify ≥3 BP elevations are cognitive and therefore amenable to computation using EHRs. In a test patient, the single-threshold approach led 11 out of 12 providers to state the correct diagnosis. Indeed, computer-modeling results indicate the single-threshold approach has a high PPV and NPV (~98%–99%); yet the sensitivity of the approach suggests its use may result in missing potential hypertension diagnoses in 17% of real patient encounters and children. Findings from simulation of the two approaches suggest the potential improvement that use of a guideline-based (vs. single-threshold) approach could have in accurately identifying children with ≥3 BP elevations (per EHR data). This information is critical for ensuring these children receive guideline-based clinical confirmation and evaluation for hypertension diagnosis.
Use of a single-threshold (abbreviated) approach still required a substantial amount of clinician time per our direct observations. Given the average visit length for primary care visits is 15.7 minutes, it is apparent that using the guideline-based method with historical heights and BP%s is too time-consuming for use in clinical practice.21 This finding demonstrates the great potential of automating the cognitively complex task of finding three separate hypertensive BP%s.22 Lowering the cognitive load for clinicians may increase clinician efficiency and improve accuracy of pediatric hypertension diagnosis, particularly if coupled with adherence to guideline-recommended re-measurement of high BPs, averaging of all visit BP measures, and computation of the visit BP% for the average SBP and DBP. Alternatively, simply storing the time-of-care SBP% and DBP% thresholds in conjunction with visit BP data (for example, in flowsheets preferably with flagging of BP values exceeding the time-of-care thresholds) could allow clinicians to identify historical BP elevations more effectively with significantly less effort. Diagnosis of hypertension is critical to trigger appropriate actions, including evaluation of secondary causes of hypertension or initiation of BP medication.10,11,23
Our study findings suggest that we can more accurately identify cases of hypertension (that might otherwise be missed) by reconstituting contemporary/time-of-care BP percentiles rather than estimating if historical BP measures exceed the single point-of-care-visit threshold for hypertension alone. This finding has important implications for EHR-enabled CDS because prior CDS tools did not incorporate time-of-care (guideline-based) hypertension thresholds. The first EHR-enabled tools to address pediatric hypertension have either alerted clinicians with a single point-of-care BP-percentile elevation (without time-of-care BP-percentile information) or presented historical BP-percentiles calculated by imputing height (using the most recent height percentile).14,15 Our findings demonstrate that prompting clinicians to consider whether to diagnose hypertension using only the point-of-care threshold for hypertension – the workflow we observed clinicians use – could result in missed diagnostic opportunities.
Study limitations include observation of a small number of physicians (no non-physicians) in a simulation environment; however, this setting allowed careful documentation and timing of a workflow that had not previously been observed directly. Algorithms applied in computer models assumed reasonable data accuracy to generate a reference standard, yet the study relied on retrospective data that were subject to data-entry error and other factors that potentially influence BP accuracy. Another potential limitation is the use of the lowest BP measure recorded at each visit. Physicians we observed reported using the lowest BP measure; Kharbanda et al. have reported that clinicians enrolled in their trials customarily relied on the lowest recorded oscillometric BP for decision making (despite extensive guideline-based trainings).16 Results may have been impacted by use of the two-year lookback period for determining hypertensive BPs. We acknowledge these limitations but do not believe they nullify the study’s evidence that identifying ≥3 BP elevations is time-consuming, and the accuracy appears to differ with use of a single threshold vs. time-of-care/guideline-based thresholds for determining criteria for hypertension diagnosis.
Strengths of our study include direct observation of clinician workflow, evaluation of the workflow’s potential impact on diagnostic accuracy using computer modeling, and workflow-observation data that provide evidence of the time and steps used to determine if a child meets criteria for pediatric hypertension diagnosis. Results from observing and diagramming clinical workflow revealed cognitively complex tasks that could be automated through EHR-enabled CDS. The use of a large sample of children with EHR data to simulate the observed provider behavior in a modeling study is novel. Computer simulation allowed quantification of the potential extent of inaccuracy in identifying children with ≥3 hypertensive BP elevations.
Conclusion.
We observed physicians use a single-threshold method to determine if a child should be considered for hypertension diagnosis. Our modeling experiment suggests that the single-threshold method may miss 17% of patient encounters and children at which a child has ≥3 separate occasions with hypertensive BP elevations in a two-year period when compared to the guideline-based method. In the absence of the EHR storing a child’s calculated BP% (or visit-specific BP% thresholds for the active guideline) for historical visits, EHR-based CDS that accurately identifies three discrete historical elevations in BP% holds great promise for supporting providers in identifying children who may have pediatric hypertension. EHR-user demand is needed to accelerate EHR vendor implementation of either solution – prospective calculation/storage of BP% in EHRs or integration of automatic hypertension detection using guideline-recommended algorithms.24–26
ACKNOWLEDGEMENTS
The authors would like to acknowledge Jenny Park for her work building and running the guideline-based computer-modeling simulations used in this study.
Sources of funding: Supported in part by the Children’s Clinical Research Advisory Committee (to Dr. Turer), Awards #K23HL118152 and #R03HL144811 from the NHLBI (to Dr. Turer), #R21DK114764 from the NIDDK (to Dr. Turer), #K23DK104065 from NIDDK (to Dr. Bowen), and the UTSW summer medical student research program (to Ms. Doney). The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH.
All abbreviations are standard, and include:
- BMI
body mass index
- BP
blood pressure
- CDS
clinical decision support
- EHR
electronic health record
- IRB
institutional review board
Footnotes
Disclosures: The authors have no financial relationships or conflicts of interest relevant to this article to disclose.
REFERENCES
- 1.Daley MF, Sinaiko AR, Reifler LM, Tavel HM, Glanz JM, Margolis KL, et al. Patterns of care and persistence after incident elevated blood pressure. Pediatrics 2013;132:e349–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hansen ML, Gunn PW, Kaelber DC. Underdiagnosis of hypertension in children and adolescents. JAMA 2007;298:874–9. [DOI] [PubMed] [Google Scholar]
- 3.Lo JC, Sinaiko A, Chandra M, Daley MF, Greenspan LC, Parker ED, et al. Prehypertension and hypertension in community-based pediatric practice. Pediatrics 2013;131:e415–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berner ES, Miller RA, Graber ML. Missed and delayed diagnoses in the ambulatory setting. Ann Intern Med 2007;146:470; author reply 70–1. [DOI] [PubMed] [Google Scholar]
- 5.Carroll AE, Buddenbaum JL. Malpractice claims involving pediatricians: epidemiology and etiology. Pediatrics 2007;120:10–7. [DOI] [PubMed] [Google Scholar]
- 6.Rinke ML, Singh H, Heo M, Adelman JS, O’Donnell HC, Choi SJ, et al. Diagnostic errors in primary care pediatrics: Project RedDE. Acad Pediatr 2018;18:220–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh H, Thomas EJ, Wilson L, Kelly A, Pietz K, Elkeeb D, et al. Errors of diagnosis in pediatric practice: A multisite survey. Pediatrics 2010;126:70–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ingelfinger JR. Clinical practice. The child or adolescent with elevated blood pressure. N Engl J Med 2014;370:2316–25. [DOI] [PubMed] [Google Scholar]
- 9.Brady TM, Appel LJ, Holmes KW, Fivush B, Miller ER 3rd., Association between adiposity and left ventricular mass in children with hypertension. J Clin Hypertens (Greenwich) 2016;18:625–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 2017;140. [DOI] [PubMed] [Google Scholar]
- 11.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The Fourth Report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 2004;114:555–76. [PubMed] [Google Scholar]
- 12.Brady TM, Neu AM, Miller ER 3rd, Appel LJ, Siberry GK, Solomon BS. Real-time electronic medical record alerts increase high blood pressure recognition in children. Clin Pediatr (Phila) 2015;54:667–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kharbanda EO, Asche SE, Sinaiko A, Nordin JD, Ekstrom HL, Fontaine P, et al. Evaluation of an electronic clinical decision support tool for incident elevated BP in adolescents. Acad Pediatr 2018;18:43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kharbanda EO, Nordin JD, Sinaiko AR, Ekstrom HL, Stultz JM, Sherwood NE, et al. TeenBP: Development and piloting of an EHR-linked clinical decision support system to improve recognition of hypertension in adolescents. EGEMS (Wash DC) 2015;3:1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Twichell SA, Rea CJ, Melvin P, Capraro AJ, Mandel JC, Ferguson MA, et al. The effect of an electronic health record-based tool on abnormal pediatric blood pressure recognition. Congenit Heart Dis 2017;12:484–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kharbanda EO, Asche SE, Sinaiko AR, Ekstrom HL, Nordin JD, Sherwood NE, et al. Clinical decision support for recognition and management of hypertension: A randomized trial. Pediatrics 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parker ED, Sinaiko AR, O’Connor PJ, Ekstrom H, Appana D, Amundson J, et al. Potential misclassification of blood pressure status in children and adolescents with short or tall stature. Am J Epidemiol 2016;183:79–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Militello LG, Arbuckle NB, Saleem JJ, Patterson E, Flanagan M, Haggstrom D, et al. Sources of variation in primary care clinical workflow: implications for the design of cognitive support. Health Informatics J 2014;20:35–49. [DOI] [PubMed] [Google Scholar]
- 19.Furniss SK, Burton MM, Grando A, Larson DW, Kaufman DR. Integrating process mining and cognitive analysis to study EHR workflow. AMIA Annu Symp Proc 2016;2016:580–89. [PMC free article] [PubMed] [Google Scholar]
- 20.Jaeschke R, Guyatt GH, Sackett DL. Users’ guides to the medical literature. III. How to use an article about a diagnostic test. The Evidence-Based Medicine Working Group. JAMA 1994;271:703–7. [DOI] [PubMed] [Google Scholar]
- 21.Tai-Seale M, McGuire TG, Zhang W. Time allocation in primary care office visits. Health Serv Res 2007;42:1871–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bates DW, Kuperman GJ, Wang S, Gandhi T, Kittler A, Volk L, et al. Ten commandments for effective clinical decision support: Making the practice of evidence-based medicine a reality. J Am Med Inform Assoc 2003;10:523–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Flynn J. The changing face of pediatric hypertension in the era of the childhood obesity epidemic. Pediatr Nephrol 2013;28:1059–66. [DOI] [PubMed] [Google Scholar]
- 24.Dufendach KR, Eichenberger JA, McPheeters ML, Temple MW, Bhatia HL, Alrifai MW, et al. Core functionality in pediatric electronic health records. AHRQ comparative effectiveness technical briefs. Rockville (MD): Agency for Healthcare Research and Quality (US); 2015. [PubMed] [Google Scholar]
- 25.Wald JS, Haque SN, Rizk S, Webb JR, Brown S, Ebron S, et al. Enhancing health IT functionality for children: The 2015 children’s EHR format. Pediatrics 2018;141. [DOI] [PubMed] [Google Scholar]
- 26.Temple MW, Sisk B, Krams LA, Schneider JH, Kirkendall ES, Lehmann CU. Trends in use of electronic health records in pediatric office settings. J Pediatr 2019;206:164–71 e2. [DOI] [PubMed] [Google Scholar]