Abstract
Background
Of the estimated 10 million people affected by (TB) each year, one-third are never diagnosed. Delayed case detection within the private healthcare sector has been identified as a particular problem in some settings, leading to considerable morbidity, mortality and community transmission. Using unannounced standardised patient (SP) visits to the pharmacies, we aimed to evaluate the performance of private pharmacies in the detection and treatment of TB.
Methods
A cross-sectional study was undertaken at randomly selected private pharmacies within 40 districts of Vietnam. Trained actors implemented two standardised clinical scenarios of presumptive TB and presumptive multidrug-resistant TB (MDR-TB). Outcomes were the proportion of SPs referred for medical assessment and the proportion inappropriately receiving broad-spectrum antibiotics. Logistic regression evaluated predictors of SPs’ referral.
Results
In total, 638 SP encounters were conducted, of which only 155 (24.3%) were referred for medical assessment; 511 (80·1%) were inappropriately offered antibiotics. A higher proportion of SPs were referred without having been given antibiotics if they had presumptive MDR-TB (68/320, 21.3%) versus presumptive TB (17/318, 5.3%; adjusted OR=4.8, 95% CI 2.9 to 7.8). Pharmacies offered antibiotics without a prescription to 89.9% of SPs with presumptive TB and 70.3% with presumptive MDR-TB, with no clear follow-up plan.
Conclusions
Few SPs with presumptive TB were appropriately referred for medical assessment by private pharmacies. Interventions to improve appropriate TB referral within the private pharmacy sector are urgently required to reduce the number of undiagnosed TB cases in Vietnam and similar high-prevalence settings.
Keywords: tuberculosis, other study design, health services research, public health
Key questions.
What is already known?
Tuberculosis (TB) is a leading infectious disease killer globally; control efforts are undermined by inadequate case detection and delayed diagnoses, particularly in private settings in countries with a high incidence of TB.
Patients with potential TB frequently approach private pharmacies to access care in these TB high-incidence settings; they are often not referred for TB screening and are supplied a short-term course of broad-spectrum antibiotics, which lead to delayed case detection and enable ongoing community transmission.
There was no geographically representative evidence estimating the magnitude of the problem regarding presumptive TB patient referrals and antibiotic supply within the private pharmacy sector in Vietnam, which responds to two-thirds of the population’s healthcare needs.
What are the new findings?
Our multicentre study, using a standardised patient method, provides estimates of pharmacy referral practices for patients with presumptive TB in the northern and southern regions of Vietnam.
Private pharmacies frequently fail to recognise TB symptoms or to refer patients to TB services, contributing to low rates of case detection; many patients with presumptive TB were inappropriately given antibiotics, including fluoroquinolones.
These findings add to the growing evidence in the literature on limited contribution of private pharmacies to TB case finding and the appropriate use of antibiotics in community settings.
Key questions.
What do the new findings imply?
Our results demonstrate the need to improve the skills of pharmacy staff in the early recognition and appropriate referral of patients with possible TB.
The study highlights the importance of improving antimicrobial stewardship in the community pharmacy setting and supports the WHO’s important recommendations for public–private mix approaches to strengthen TB case finding.
Background
Tuberculosis (TB) is a leading infectious cause of death globally, and TB case numbers are estimated to increase even further due to the disruptions caused by the COVID-19 pandemic.1 An estimated 10 million people developed TB globally in 2019, of whom approximately one-third were never detected or offered appropriate treatment.1 This persistent case-detection gap comprises around 2.9 million cases each year and results in continuing community transmission and undermining national and global TB control efforts.2
Studies from high-incidence settings have shown that patients with TB frequently experience significant delays before obtaining a diagnosis.3 The accessibility and trusted role of pharmacies in local communities4 mean that patients frequently attend private pharmacies soon after developing symptoms of TB.5–7 In India, Vietnam and Uganda, between 40% and 60% of patients who were ultimately diagnosed with TB visited a private pharmacy prior to medical assessment and TB diagnosis.3 8 9 Although private pharmacies should play an important role in case detection and referral, inappropriate management often contributes to delayed diagnosis and TB-specific treatment. Pharmacies may also contribute to the development of antimicrobial resistance (AMR) if they dispense inadequate broad-spectrum antibiotics to patients with TB.10 Hence, private pharmacies have been identified as important stakeholders in both TB and AMR control efforts.6
Private sector engagement is a top priority of the WHO, which encourages national TB control programmes to develop strong public–private partnerships as a part of their End TB Strategy.11 The private sector plays an important role in Vietnam1 and in other middle-income countries in Southeast Asia with a high incidence of TB and drug-resistant TB.1 In Vietnam, private pharmacies account for two-thirds of health service encounters.12 A previous study has shown that a minority of patients in northern Vietnam were referred by private pharmacies to a medical facility capable of establishing a TB diagnosis.13
We aimed to evaluate the referral practices of private pharmacies in Vietnam for standardised patients (SPs) presenting with symptoms of presumptive TB and drug-resistant TB as unannounced ‘mystery shoppers’.
Methods
Study design and setting
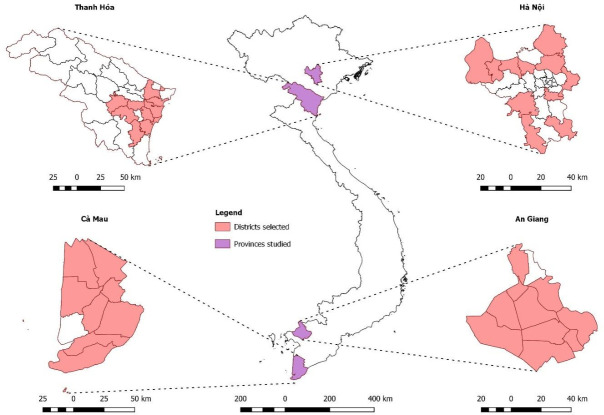
A cross-sectional study was undertaken from April to November 2019 using an SP study method, with SPs visiting randomly selected private pharmacies in 40 districts of Vietnam. This included urban and rural areas in the northern (Hanoi and Thanh Hoa) and southern (Ca Mau and An Giang) provinces (figure 1). Vietnam is a middle-income country in Southeast Asia with a high incidence of TB (176/100 000) and multidrug-resistant TB (MDR-TB) (8.8/100 000) (defined as TB that is resistant to the two most effective first-line antibiotics, rifampicin and isoniazid).1 Tuberculosis diagnosis and treatment in Vietnam are largely provided by a public National Tuberculosis Program. However, the private pharmacy sector has expanded rapidly over the past two decades and is the first point of healthcare contact for the majority of patients.12
Figure 1.
Provinces and districts selected for study participation.
The SP study is regarded as a proven and widely used methodological tool for pharmacy practice research.14 15
Sampling
Districts located within 2 hours’ drive or less than 150 km from the provincial centre were included. Within each district, a geographical area comprising approximately one-quarter of the total population was selected by convenience sampling. The Global Positioning System location of private pharmacies in the selected geographical area was established by the research team physically walking the streets and identifying all pharmacies. Pharmacies were classified as either private pharmacies or drug counters. Vietnamese regulations stipulate that ‘private pharmacies’ in urban areas must be managed by a university graduate pharmacist, and ‘drug counters’ must be led by a pharmacist with college certification.16 Counters selling only traditional medicines, wholesalers and pharmacies located within government health facilities or private hospitals were excluded. Throughout this article, the term pharmacy refers to both drug counters and private pharmacies. Pharmacies were classified as registered (registration identification (ID) displayed on the signboard of the pharmacy) or unregistered (no ID displayed).
A total of 1643 eligible private pharmacies were identified during the mapping process. Details of the study site selection process are included in the online supplemental material.
bmjgh-2021-006475supp001.pdf (60.4KB, pdf)
Development of clinical scenarios
Two clinical scenarios were developed in collaboration with clinicians, pharmacists, public health experts and researchers from Vietnam and Australia:
Presumptive TB: the first scenario involved a male adult with the following symptoms: cough for 3 weeks, fever, loss of appetite and weight loss, as well as reporting a history of using cough medication without any improvement. The patient had not previously sought or received testing for TB.
Presumptive MDR-TB: the second scenario comprised a patient with a cough of 4-week duration and a history of previous TB treatment, with early treatment interruption. The scenarios are summarised in table 1.
Table 1.
Overview of SP scenarios
| Scenario description | Presenting history | Expected outcome |
| 1. Presumptive TB: 2–3 weeks of cough with intermittent fever, along with loss of appetite and weight loss; seeking medical advice for the first time. |
‘I have a cough and fever for the last 2–3 weeks that is not getting better. I have lost my appetite and feel I am losing weight. I have taken cough medicine but there is no improvement. Can I get some medicines?’ | Verbal or written referral to a doctor in a TB centre, hospital or a healthcare provider without dispensing any antibiotics. |
| 2. Presumptive MDR- TB: 4 weeks of cough with history of incomplete TB treatment, seeking medical advice for the first time. | ‘I have been suffering from a bad cough for about 4 weeks. I took some traditional medicines for cough relief, but they are not working. It seems to be similar to the cough I had 2 years ago when I got TB. But I remember that I was already treated for TB for 3 months and the tests were fine. Is it related to my previous condition? What do you suggest?’ The SPs would admit to a loss of appetite, to his clothes becoming a bit loose, fever and feeling fatigued if prompted by the pharmacy staff. If the staff asked about history of TB treatment, the SPs would say ‘I did it for about 3 months, later, when the doctor found my sputum test was fine, I thought it was cured and after 3 months of treatment, I stopped taking the medication’. |
Verbal or written referral to a doctor in a TB centre, hospital or a healthcare provider without dispensing any antibiotics. |
MDR-TB, multidrug-resistant tuberculosis; SP, standardised patient; TB, tuberculosis.
These two scenarios reflect typical clinical presentations with TB. Scenarios used in other settings17 18 were localised to the Vietnamese context, in consultation with clinical pharmacy lecturers, community pharmacists and other clinicians. The scenarios were piloted in 14 pharmacies in northern and southern regions, with further refinement prior to implementation.
For both scenarios, the research design included only middle-aged men as SPs because 75% of prevalent TB cases in Vietnam are male.19 Local actors were trained to present as an SP for one of the two scenarios over a 4-day period by a researcher with experience implementing SP studies in other settings. Training included initial briefing, interactive discussions, role plays and pilot visits to private pharmacies. Actors were evaluated against a checklist to ensure a convincing and standardised performance.
SP visits
A sample of 636 pharmacies were allocated to each of the four provinces according to proportionate to the provincial sample of the eligible mapped pharmacies. A systematic sampling technique was used to select the pharmacies for each scenario. The fifth and sixth pharmacies were selected, starting from a random point of the list of eligible pharmacies in each province for presumptive TB and presumptive MDR-TB scenarios, respectively, until the provincial quota was filled. The same process was continued in all four provinces to randomly allocate pharmacies to both scenarios. The trained SPs were randomly assigned to pharmacies using a predetermined randomisation protocol.
Each selected pharmacy was visited during business hours by one SP and one observer. The observer was identified as a friend and listened to the interaction but did not participate in the clinical encounter. Immediately after leaving the pharmacy, the SP and observer jointly documented the outcome of the visit by completing a structured data collection sheet. They also collected an audio recording of their visit for narrative analysis. The recording mentioned the number of customers present in the shop, the number of staff present, the behaviour of the staff and the layout of the pharmacy.
Stepped antibiotic request
During each encounter, we assessed the pharmacy staff member’s willingness to supply antibiotics at three levels of increasing consumer demand.14 20 During the initial consultation, SPs asked for an unspecified medicine to alleviate their symptoms, without specifying an antibiotic (a ‘level 1’ request). If an antibiotic was not provided during the initial interaction, they asked for a stronger medicine: ‘can you give me any stronger medicine?’ (level 2 request). If the pharmacy staff did not provide an antibiotic, they then explicitly requested an antibiotic: ‘I want an antibiotic’ (level 3 request).
Medicines supplied by the pharmacy were identified by a team of three study pharmacists and were coded according to their therapeutic mode of action. Antibiotics were classified according to their generic name and grouped into three major categories: (1) fluoroquinolones; (2) non-fluoroquinolone broad-spectrum antibiotics (antibiotics that are effective against both Gram-positive and Gram-negative bacteria, including cephalosporins, broad-spectrum penicillins, sulfonamides, macrolides and tetracyclines); and (3) other antibiotics. We classified steroids and non-steroidal anti-inflammatory drugs as anti-inflammatory.
We assessed antibiotic supply in two ways: (1) ‘antibiotic offered’, which was reported in the data collection sheet by the SP and the observer (without medical knowledge) based on the interaction with pharmacy staff; and (2) ‘actual antibiotic supplied’, which was recorded after verification of the received antibiotics by the study pharmacists.
Outcome measures
The primary outcome for both clinical scenarios was the proportion of ‘SPs’ who were referred for medical assessment. This referral includes to TB clinics, public hospitals and private clinics. Secondary outcomes included the proportion of SPs referred without antibiotic supply, the proportion pharmacy staff who asked for additional information about medical history and medicines supplied (online supplemental material describes predesigned list of additional information related questions).
Data collection and analysis
Data collection
Data were documented on paper data collection forms immediately after a pharmacy visit and were later entered into an electronic Research Electronic Data Capture (REDCap) database designed without having any pharmacy identifiable information.21
Sample size
The sample size was based on an expected proportion of inappropriate antibiotic dispensing of 50%, based on studies from comparable settings.17 22 In order to ascertain the proportion of patients referred without supplying an antibiotic, with a precision of ±5% and an alpha of 0.05 (ie, 95% confidence limits), assuming half of the clusters were urban, we estimated that we needed a sample of 318 pharmacies for each scenario. This estimation was derived using sample size formula for proportions.23 Pharmacies were selected for each scenario from the eligible pharmacies using simple random sampling technique (online supplemental material).
Statistical analysis
Descriptive statistics evaluated pharmacy characteristics (classification of pharmacy, registration status, geographical area and gender of the pharmacy staff), duration of interaction, population density, pharmacy density, the medical history taken by pharmacy staff, medications supplied and referral practices. Logistic regression was used to evaluate the relationship between these independent variables and the primary outcome measures. The comparative analysis employed multivariable regression with backward elimination (SPSS V.24). Adjusted ORs (aORs) with 95% CIs were reported. The χ2 likelihood ratio test, pseudo R2 values and the Hosmer-Lemeshow χ2 test were used as model fit statistics to evaluate the multiple logistic regression models.
Patient and public involvement
This SP study was designed to assess presumptive TB patient referrals and medication supply at community pharmacies. Therefore, study participants were pharmacy staff; patients or the public were not involved in the design, conduct, reporting or dissemination plans of our research.
Results
Standardised patients visited 638 pharmacies, including 318 with presumptive TB and 320 presumptive MDR-TB. Characteristics of selected pharmacies are shown in table 2. A greater proportion of pharmacies were classified as drug counters (89.3%) than private pharmacies (10.7%). About 60% of the pharmacies displayed their registration status externally.
Table 2.
Characteristics of participating pharmacies
| Characteristics | SPs with presumptive TB | SPs with presumptive MDR-TB |
| Frequency (%) | Frequency (%) | |
| N=318 | N=320 | |
| Classification of pharmacy | ||
| Pharmacy | 30 (1.6) | 38 (11.9) |
| Drug counter | 288 (90.6) | 282 (88.1) |
| Pharmacy registration status | ||
| Not registered | 129 (40.6) | 128 (40.0) |
| Registered | 189 (59.4) | 192 (60.0) |
| Region | ||
| North | 200 (62.9) | 201 (62.8) |
| South | 118 (37.1) | 119 (37.2) |
| Geographical area | ||
| Rural | 273 (85.8) | 275 (85.9) |
| Urban | 45 (14.2) | 45 (14.1) |
| Gender of pharmacy staff attending the SP | ||
| Male | 73 (23.0) | 65 (20.3) |
| Female | 245 (77.0) | 255 (79.7) |
| Duration of interaction (min) | ||
| Median (IQR) | 4 (3–5) | 5 (4–5) |
| Missing data | 1 | |
| Commune population density (PPH) | ||
| Median (IQR) | 12 (8–16) | 12 (8–17) |
| Number of pharmacies /10 000 population | ||
| Median (IQR) | 11 (7–17) | 11 (7–17) |
MDR-TB, multidrug-resistant tuberculosis; PPH, number of people per hectare; SP, standardised patient; TB, tuberculosis.
Among 318 SPs presenting with presumptive TB, 39 (12.3%, 95% CI 8.9% to 16.4%) encounters resulted in a referral to a healthcare provider (primary outcome). Among 320 SPs with presumptive MDR-TB, 116 (36.3%, 95% CI 31.0% to 41.8%) encounters resulted in a referral to a healthcare provider (primary outcome). Only 17 SPs (5.3%, 95% CI 3.1% to 8.4%) with presumptive TB and 68 (21.1%, 95% CI 16.9% to 26.1%) with presumptive MDR-TB were referred to healthcare providers without the provision of any antibiotics. Antibiotics were mostly offered without pressure (level 1 request) for the presumptive TB scenario by 92.3% of pharmacies, and for presumptive MDR-TB by 96.9% of pharmacies as compared with level 2 and level 3 requests (<8%).
Table 3 presents factors associated with referral for medical assessment. Pharmacies in the south were more likely to refer the SPs to healthcare providers than their northern counterparts for presumptive TB (aOR=8.8, 95% CI: 3.8 to 20.4) and presumptive MDR-TB (aOR=4.8, 95% CI 2.9 to 7.8), respectively. A significantly higher proportion of pharmacy staff inquired about the medical history of patients, during interactions with SPs who had presumptive MDR-TB (n=245, 76.6%), in comparison to those who had presumptive TB (n=195, 61.3%).
Table 3.
Factors associated with referral of SPs with presumptive TB or MDR-TB for medical assessment
| Predictors | Presumptive TB | Presumptive MDR-TB | ||||||
| N=318 | N=320 | |||||||
| Referred to healthcare provider (yes) Frequency (%) |
Referred to healthcare provider (no) Frequency (%) |
Unadjusted OR (95% CI) (referred compared with not referred) | aOR (95% CI) (referred compared with not referred) n=317 (model 1) | Referred to healthcare provider (yes) Frequency (%) |
Referred to healthcare provider (no) Frequency (%) |
OR (95% CI) (referred compared with not referred) | aOR (95% CI) (referred compared with not referred) n=319 (model 2) | |
| Region | ||||||||
| North | 9 (23.1) | 191 (68.5) | 1.0 | 1.0 | 46 (39.7) | 155 (76.0) | 1.0 | 1.0 |
| South | 30 (76.9) | 88 (31.5) | 7.2 (3.3 to 15.9) | 8.78 (3.8 to 20.4) | 70 (60.3) | 49 (24.0) | 4.8 (2.9 to 7.9) | 4.7 (2.9 to 7.8) |
| Geographical location | ||||||||
| Rural | 37 (94.9) | 236 (84.6) | 1.0 | NI | 95 (81.9) | 180 (88.2) | 1.0 | NP |
| Urban | 2 (5.1) | 43 (15.4) | 0.3 (0.1 to 1.3) | 21 (18.1) | 24 (11.8) | 1.7 (0.9 to 3.1) | ||
| Medical history taken by pharmacy staff | ||||||||
| No | 10 (8.1) | 113 (91.9) | 1.0 | 1.0 | 20 (17.2) | 55 (27.0) | 1.0 | 1.0 |
| Yes | 29 (14.9) | 166 (85.1) | 2.0 (0.9 to 4.2) | 3.9 (1.7 to 9.0) | 96 (82.8) | 149 (73.0) | 1.8 (1.0 to 3.1) | 1.8 (1.0 to 3.2) |
| Number of pharmacies/10 000 commune population | ||||||||
| Median (IQR) | 10.7 (5.5–16.6) | 10.7 (6.9–17.7) | 10.6 (5.9–16.1) | 10.8 (6.8–18.3) | NP | |||
| Low (<median) | 1.0 | NP | 1.0 | |||||
| High (≥median) | 0.7 (0.9 to 1.7) | 0.9 (0.6 to 1.5) | ||||||
| Gender of attending staff | ||||||||
| Female | 29 (74.4) | 216 (77.4) | 1.0 | NP | 86 (74.1) | 169 (82.8) | 1.0 | NP |
| Male | 10 (25.6) | 63 (22.6) | 1.2 (0.5 to 2.6) | 30 (25.9) | 35 (17.2) | 1.7 (1.0 to 2.9) | ||
| Registration status | NP | |||||||
| Not registered | 6 (15.4) | 123 (44.1) | 1.0 | 30 (25.9) | 98 (48.0) | 1.0 | NP | |
| Registered | 33 (84.6) | 156 (65.9) | 4.3 (1.8 to 10.7) | 86 (74.1) | 106 (52.0) | 2.6 (1.6 to 4.4) | ||
| Type of facility | NI | |||||||
| Pharmacy | 1 (2.6) | 29 (10.4) | 1.0 | 16 (13.8) | 22 (10.8) | 1.0 | NP | |
| Drug counter | 38 (97.4) | 250 (89.6) | 4.4 (0.6 to 33.3) | 100 (86.2) | 182 (89.2) | 0.8 (0.4 to 1.5) | ||
| Interaction time (min) | NP | NP | ||||||
| Median (IQR) | 4 (4–5) | 4.0 (3–5) | ||||||
| Missing values | 0 | 1 | 4.5 (4–5) | 5.0 (4–5) | ||||
| Low (<median) | 1.0 | 1.0 | ||||||
| High (≥median) | 2.5 (1.1 to 5.9) | 0.9 (0.6 to 1.5) | ||||||
| Commune population density (PPH) | NP | |||||||
| Median (IQR) | 8.4 (4.5–11.6) | 12.2 (8.0–17.1) | 10.6 (6.1–16.2) | 12.6 (8.7–17.1) | ||||
| Low (<median) | 1.0 | 1.0 | 1.0 | |||||
| High (≥median) | 0.3 (0.1 to 0.6) | 0.4 (0.2 to 0.9) | 0.6 (0.4 to 0.9) | |||||
Model accuracy and fit: model 1: PAC=87.7%, omnibus χ2 test for the model <0.001 and Hosmer and Lemeshow χ2 test for the model=0.581.
Model 2: PAC=71.2%, omnibus χ2 test for the model <0.001 and Hosmer and Lemeshow χ2 test for the model=0.840. All of these values indicate that the models fit well.
aOR, adjusted OR; CI, 95% Confidence Interval; MDR-TB, multidrug-resistant tuberculosis; NI, not included in the adjusted model due to few/no observations found in one cell or few cells; NP, not predicted in the dimension of final model produced using backward deletion method; PAC, percentage accuracy in classification; PPH, number of people per hectare; SP, standardised patient.
Pharmacy staff who asked about SPs’ medical history were more likely to refer them to healthcare providers, for both the presumptive TB (aOR=3.9, 95% CI 1.7 to 9.0) and MDR-TB (aOR=1.7, 95% CI 0.9 to 3.3) scenarios. There was no association between the duration of the SPs’ encounter and the proportion of SPs referred for medical assessment.
Table 4 shows the categories of medicines supplied by pharmacy staff. A total of 1475 individual medicines were supplied during the presumptive TB encounters (median five drugs, IQR 4–6 drugs) and 1128 different medicines during the presumptive MDR-TB encounters (median four drugs, IQR 0–5 drugs). Over a quarter of medicines were unlabelled. Antibiotics were the most common category of medicines offered to SPs with presumptive TB (286/318; 89.9%, 95% CI 86.1% to 93.0%) and presumptive MDR-TB (225/320; 70.3%, 95% CI 65.0% to 75.3%).
Table 4.
Pharmacy responses to SPs
| Total SP scenarios | Presumptive TB | MDR-TB |
| Frequency/proportion (%) | Frequency/proportion (%) | |
| N=318 | N=320 | |
| Medical history taken* | ||
| No | 123 (38.7) | 75 (23.4) |
| Yes | 195 (61.3) | 245 (76.6) |
| Referral to medical facility | ||
| Total referrals (any of the following) | 39 (12.3) | 116 (36.3) |
| To TB centre | 07 (2.2) | 57 (17.8) |
| To private clinic | 12 (3.8) | 28 (8.8) |
| To district healthcare centre/hospital | 31 (9.7) | 46 (14.4) |
| Referral without giving antibiotics (subgroup of all aforementioned referrals) | 17 (5.3) | 68 (21.3) |
| Number of ‘all medications’ dispensed | ||
| Median (IQR) | 5 (4–6) | 4 (0–5) |
| 0 (no other medicine dispensed) | 24 (7.5) | 86 (26.9) |
| 1 | 2 (0.6) | 1 (0.3) |
| 2 | 2 (0.6) | 4 (1.3) |
| 3 | 30 (9.4) | 23 (7.2) |
| 4 | 66 (20.8) | 64 (20.0) |
| 5 | 105 (33.0) | 83 (25.9) |
| ≥6 | 89 (27.9) | 59 (18.4) |
| Categories of medicines dispensed | ||
| Number different types of medicines received in total | 1475 (100) | 1127 (100) |
| Unlabelled medicines | 436 (29.6) | 311 (27.6) |
| Antibiotics (general) | 244 (16.5) | 217 (19.3) |
| Antibiotics (with anti-TB activity) | 14 (0.9) | 24 (2.1) |
| Cough medicine | 230 (15.6) | 207 (18.4) |
| Steroids/NSAIDS (anti-inflammatory) | 113 (7.7) | 107 (9.5) |
| Antihistamines | 64 (4.3) | 51 (4.5) |
| Pain/fever relief | 46 (3.1) | 16 (1.4) |
| Vitamin supplementary | 70 (4.7) | 32 (2.8) |
| Other identified medicine (bronchodilators, proton-pump inhibitors, etc) | 106 (7.2) | 81 (7.2) |
| Any combined formulation (combination of cough and cold formulations that included antitussives, antihistamines and/or analgesics) | 152 (10.3) | 81 (7.2) |
| Class of antibiotic dispensed† | N=258 | N=241 |
| Fluoroquinolones | 45 (17.4) | 39 (16.2) |
| Broad-spectrum antibiotics other than fluoroquinolones | 202 (78.3) | 190 (78.8) |
| Other antibiotic (includes lincomycins and unknown) | 11 (4.3) | 12 (5.0) |
| Number of pharmacies sold one antibiotic | 238 (92.2) | 196 (78.7) |
| Number of pharmacies sold two antibiotics | 20 (7.8) | 45 (18.7) |
| Prescription for an antibiotic requested by pharmacy staff | ||
| No | 312 (98.1) | 212 (97.5) |
| Yes | 6 (1.9) | 8 (2.5) |
| Antibiotic offered‡ | ||
| No | 32 (10.1) | 95 (29.7) |
| Yes | 286 (89.9) | 225 (70.3) |
| Level of demand required to obtain antibiotic | N=286 | N=225 |
| Level 1 (Can I get some medicine to alleviate the symptoms?) | ||
| Antibiotic given | 264 (92.3) | 218 (96.9) |
| Antibiotic not given | 13 (7.7) | 7 (3.1) |
| Level 2 (Can I get something stronger?) | ||
| Antibiotic given | 13 (4.5) | 3 (1.3) |
| Antibiotic not given | 9 (3.1) | 4 (1.8) |
| Level 3 (I would like an antibiotic.) | ||
| Antibiotic given | 9 (3.1) | 4 (1.8) |
| Antibiotic not given | 0 | 0 |
*Possible history taken by staff in relation to reported symptoms.
†Actual antibiotics received after being verified by study pharmacists.
‡Reported by standardised patient prior to verification by study pharmacists but not necessarily bought by SP due to several reasons (eg, no change cash notes available, told that antibiotics was dispensed but could not find these and vice versa, etc).
MDR-TB, multidrug-resistant tuberculosis; NSAID, non-steroidal anti-inflammatory drug; SP, standardised patient; TB, tuberculosis.
Antibiotics dispensed
Among the antibiotics verified by study pharmacists (n=258) during the presumptive TB encounters, 202 (78.3%) were broad-spectrum non-fluoroquinolone antibiotics (cephalosporins, broad-spectrum penicillins, macrolides, sulfonamides or tetracyclines) and 45 (17.4%) of antibiotics were fluoroquinolones. Medications used as part of standardised regimens to treat TB, such as levofloxacin or rifampicin, were supplied to 14 (5.4%) SPs with presumptive TB encounters and 33 (13.7%) SPs presenting with presumptive MDR-TB. No SPs were provided with a recommended treatment regimen for TB. More than one antibiotic was supplied in 16 (6.2%) and 39 (16.2%) encounters involving SPs with presumptive TB and presumptive MDR-TB, respectively.
Other common classes of medicines supplied to SPs were antitussives (16.8%), and combination cough and cold formulations (including two or more of antitussives, antihistamines and/or analgesics, 8.9%; table 4).
Discussion
This SP study involving 638 pharmacies across Vietnam is the largest and most geographically representative study of its kind conducted in Vietnam to date. It demonstrated that only a small proportion of SPs with symptoms of presumptive TB and presumptive MDR-TB were referred for medical assessment. Pharmacists taking a medical history were more likely to make a referral than those who did not take a history. Broad-spectrum antibiotics, including fluoroquinolones, were commonly supplied to SPs.
The low proportion of referrals for medical assessment demonstrates the missed opportunities for early case-finding through pharmacies. Delays in accessing testing and treatment for TB undermine control efforts as patients may remain contagious for prolonged periods prior to diagnosis, increasing transmission of Mycobacterium tuberculosis in the community. Delayed diagnosis has been shown to increase TB-related morbidity and mortality.24
Our findings are consistent with studies using SPs in India and a self-reported study among pharmacy staff in Cambodia.17 25 In India, only 13.0% of the patients with presumptive TB symptoms and 62.0% of patients with confirmed TB were referred to a healthcare provider,17 whereas in Cambodia, 29.6% patients were referred for appropriate TB treatment.25 Our study found a lower proportion of referral across Vietnam than a study of 138 private pharmacies in an urban Hanoi province of Vietnam, in which 46.0% of patients were referred.13 In this prior study, 20 pharmacies located within 500 m distance from two TB hospitals were purposely selected and SPs specifically requested TB medications, potentially leading to more referrals. A cross-sectional study among patients with diagnosed TB in southern Vietnam found that those who visited a pharmacy prior to their diagnosis were five times more likely to have delayed access to care (which was defined as more than 4 weeks from first noticed symptom to first health provider contact), compared with those who consulted a national TB programme facility first.26
A higher proportion of referrals in the MDR-TB scenario were expected, as reported previous history of TB refrained from any differential diagnosis and supported by previous studies,13 17 only about one quarters of the pharmacies referred these SPs for screening. This poor referral suggests the pharmacy staff’s confusion or lack of knowledge in identifying presumptive MDR-TB cases. Educating pharmacy staff on TB-related symptoms and importance of presumptive TB case referrals might help to improve the early referrals for patients with presumptive TB.
There was significant regional variation in the referral patterns of pharmacies, with a greater referral rate in southern Vietnam. This shows a heterogeneity in private pharmacy practice between the regions, possibly due to various factors including, but not limited to, extent of pharmacy education and clinical training, business model and the culture that may contribute to this behaviour. This finding highlights the importance of undertaking studies in a wide range of settings in order to characterise differences in local practice and get a more comprehensive overview. Nevertheless, low case referrals were the norm in all settings, which indicates that further effort is required to enhance cooperation between the public and private sectors across the country.
Our study showed a high proportion of encounters which resulted in the supply of broad-spectrum antibiotics to SPs, including antibiotics used in TB treatment, particularly the fluoroquinolones (>16%) used in MDR-TB treatment. This is consistent with studies in other settings.17 27 These findings underpin concerns that unregulated dispensing of antibiotics is likely to amplify the risk of acquired drug resistance, especially against key second-line drugs.28 Inappropriate use of fluoroquinolones may also delay TB diagnosis due to a partial therapeutic effect that may improve patients’ symptoms and reduce the yield of microbiological tests for M. tuberculosis.29 Fluoroquinolones given to patients with undiagnosed MDR-TB compromise one of the most effective second-line TB drugs and will contribute to the emergence and spread of extensively drug-resistant TB.30 Antibiotics were dispensed predominantly at level 1 request. Similar findings were also observed in SP studies conducted at private pharmacies in Sri Lanka14 and Eritrea,31 where most antibiotics were spontaneously dispensed without any pressure exerted by SPs. Therefore, we hypothesise that the current inappropriate antibiotic dispensing practice may be reflect profit motive than external patient pressure. A previous study in Vietnam also found that the revenue of selling antibiotics without a prescription is greater than all sales in both rural and urban pharmacies.32 As we also found that over 95% of the sold antibiotics were broad-spectrum antibiotics, which are generally more expensive than narrow-spectrum antibiotics.
Our study has important public health implications by demonstrating a major opportunity to close persistent case-detection gaps if the private pharmacy sector can be better engaged. Our results demonstrate a need for interventions to improve the early recognition and appropriate referral of patients with presumptive TB (including MDR-TB) to public TB services. Training for pharmacy staff that improves their TB knowledge and emphasises the importance of history taking should improve the rate of referral. Doing this in a sustainable fashion may require inclusion in training curricula and better oversight/monitoring mechanisms. Support for effective public–private mix approaches, which have been advocated by the WHO and other international agencies, promise to make an important contribution to timely TB notification.33
The study also highlights the importance of improving antimicrobial stewardship (AMS) in general, especially in community settings where this is often neglected. AMS programmes promote the responsible use of antimicrobials through the delivery of evidence-based interventions but are often restricted to hospital settings.34 Although the programmes are highly regarded and considered essential to combat inappropriate antimicrobial use and protect human health in the long run,35 they are rarely implemented outside the hospital setting or with involvement of community pharmacies. This remains a major challenge requiring better solutions, especially in settings like Vietnam, where the vast majority of antibiotics are dispensed at the community level.
Our study has a number of strengths. First, the use of standardised patients provides an accurate assessment of the actual behaviour of pharmacy staff. This avoids social desirability bias and observer bias (the Hawthorne effect), which are difficult to avoid with self-reported methods. The selection of actors from local communities increased authenticity and reduced the risk of detection. Second, our study population was broadly representative of the situation in both northern and southern Vietnam. We randomly selected pharmacies for each scenario across 40 districts in the north and south of Vietnam, which adequately captured the diversity of practice across the study region.
Study limitations include the fact that the use of different actors may have introduced some variation in the scenarios. We reduced this by using a rigorous standardised training procedure with ongoing quality assessment through the presence of an observer and external monitoring. SP studies conducted in India found that the personal characteristics of SPs had little effect on the quality of care provided by staff.36 We included populations located within 2 hours of major urban centres in the north and south of the country. These were representative of urban and semirural populations in the most populous northern and southern regions of Vietnam. Remote rural populations were not examined in this study, for practical reasons. Our SPs had a restricted number of responses in order to improve standardisation across the study, although they were trained to communicate as naturally as possible. Responses were scripted using previous experience in conducting similar studies in other settings. While this study explored the practices of pharmacy staff, it did not assess the factors associated with pharmacists’ decisions to refer patients or provide antibiotics. This is an important area for future research, to enable interventions that will improve referral practices in the private pharmacy sector.
In conclusion, this study revealed that a low proportion of private pharmacies in Vietnam appropriately referred patients with presumptive TB for medical assessment. This is important to address, given the considerable TB case-detection gap observed in Vietnam,19 and highlights the importance of strengthening partnerships between the private and public sectors in order to achieve the WHO End TB targets. It also emphasises the need to involve community pharmacies in AMS initiatives in order to reduce the inappropriate use of broad-spectrum antibiotics in Vietnam.
Acknowledgments
The authors thank the provincial Departments of Health in the four participating provinces and the team from Woolcock Institute of Medical Research in Vietnam for their support.
Footnotes
Handling editor: Sanni Yaya
Twitter: @shukryzawahir
Contributors: GF, TAN, JB, ADD, SZ, GBM, JN, SB, KV, TCH, SM, SJ, HTTM, SNT and BJM were responsible for conception and study design. SZ, HL, TAN, TLM, HNV, VNTC, HTTM and TNT were responsible for data curation. SZ, HL, HNV and VNTC accessed and verified the data. HL coordinated study activities across the sites. SZ led the data analysis with supervision from GF. SZ and KaV drafted the manuscript with supervision from GF. All authors contributed to the final version of the manuscript and approved the submission. All authors had full access to all the data in the study, and the corresponding author had final responsibility to submit for publication.
Funding: This study was funded by a grant from the Australian Department of Foreign Affairs and Trade. GF was supported by an National Health and Medical Research Council(NHMRC) Career Development Fellowship (APP1148372). No funding bodies had any role in the study design, data collection, analysis or decision to publish.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein) or of any geographical or locational reference does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information. All deidentified data are included in the article and tables.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Ethical approval was provided by the National Institute of Hygiene and Epidemiology Vietnam (HDDD-41/2018), the University of Sydney Human Research Ethics Committee (2018/2020) and provincial departments of health. A waiver of consent for individual pharmacies was granted by both ethics committees, allowing concealment of the identity of the standardised patients to pharmacy staff to reduce the likelihood of a Hawthorne effect (the inclination of participants who are being monitored as part of the research to change the behaviour being evaluated only because it is being studied).
References
- 1.WHO . Global tuberculosis report 2019, 2020. Available: https://www.who.int/publications/i/item/9789240013131 [Accessed 20 Dec 2020].
- 2.Tiemersma EW, van der Werf MJ, Borgdorff MW, et al. Natural history of tuberculosis: duration and fatality of untreated pulmonary tuberculosis in HIV negative patients: a systematic review. PLoS One 2011;6:e17601. 10.1371/journal.pone.0017601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sreeramareddy CT, Qin ZZ, Satyanarayana S, et al. Delays in diagnosis and treatment of pulmonary tuberculosis in India: a systematic review. Int J Tuberc Lung Dis 2014;18:255–66. 10.5588/ijtld.13.0585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McKinn S, Trinh DH, Drabarek D, et al. Drivers of antibiotic use in Vietnam: implications for designing community interventions. BMJ Glob Health 2021;6:e005875. 10.1136/bmjgh-2021-005875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lönnroth K, Uplekar M, Blanc L. Hard gains through soft contracts: productive engagement of private providers in tuberculosis control. Bull World Health Organ 2006;84:876–83. 10.2471/BLT.06.029983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Daftary A, Jha N, Pai M. Enhancing the role of pharmacists in the cascade of tuberculosis care. J Epidemiol Glob Health 2017;7:1–4. 10.1016/j.jegh.2016.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Surya A, Setyaningsih B, Suryani Nasution H, et al. Quality tuberculosis care in Indonesia: using patient pathway analysis to optimize public-private collaboration. J Infect Dis 2017;216:S724–32. 10.1093/infdis/jix379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kiwuwa MS, Charles K, Harriet MK. Patient and health service delay in pulmonary tuberculosis patients attending a referral Hospital: a cross-sectional study. BMC Public Health 2005;5:122–22. 10.1186/1471-2458-5-122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lönnroth K, et al. Utilization of private and public health-care providers for tuberculosis symptoms in Ho Chi Minh City, Vietnam. Health Policy Plan 2001;16:47–54. 10.1093/heapol/16.1.47 [DOI] [PubMed] [Google Scholar]
- 10.Devasia RA, Blackman A, Gebretsadik T, et al. Fluoroquinolone resistance in Mycobacterium tuberculosis: the effect of duration and timing of fluoroquinolone exposure. Am J Respir Crit Care Med 2009;180:365–70. 10.1164/rccm.200901-0146OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.WHO . Engaging all health care providers in TB control. guidance on implementing public-private mix approaches Geneva, 2006. Available: https://www.who.int/tb/publications/who_htm_tb_2006_360/en/ [Accessed 10 Mar 2021].
- 12.Angelino A, Khanh D, An Ha N, et al. Pharmaceutical industry in Vietnam: sluggish sector in a growing market. Int J Environ Res Public Health 2017;14:976. 10.3390/ijerph14090976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vu DH, van Rein N, Cobelens FGJ, et al. Suspected tuberculosis case detection and referral in private pharmacies in Viet Nam. Int J Tuberc Lung Dis 2012;16:1625–9. 10.5588/ijtld.12.0295 [DOI] [PubMed] [Google Scholar]
- 14.Zawahir S, Lekamwasam S, Aslani P. Community pharmacy staff’s response to symptoms of common infections: a pseudo-patient study. Antimicrob Resist Infect Control 2019;8:1–10. 10.1186/s13756-019-0510-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kwan A, Daniels B, Bergkvist S, et al. Use of standardised patients for healthcare quality research in low- and middle-income countries. BMJ Glob Health 2019;4:e001669. 10.1136/bmjgh-2019-001669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.SOCIALIST REPUBLIC OF VIETNAM . Law on pharmacy: Pursuant to the constitution of socialist Republic of Vietnam. The National Assembly promulgates the Law on Pharmacy, 2016. [Google Scholar]
- 17.Satyanarayana S, Kwan A, Daniels B, et al. Use of standardised patients to assess antibiotic dispensing for tuberculosis by pharmacies in urban India: a cross-sectional study. Lancet Infect Dis 2016;16:1261–8. 10.1016/S1473-3099(16)30215-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Das J, Kwan A, Daniels B, et al. Use of standardised patients to assess quality of tuberculosis care: a pilot, cross-sectional study. Lancet Infect Dis 2015;15:1305–13. 10.1016/S1473-3099(15)00077-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nguyen HV, Tiemersma EW, Nguyen HB, et al. Correction: The second national tuberculosis prevalence survey in Vietnam. PLoS One 2020;15:e0236532–e32. 10.1371/journal.pone.0236532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chang J, Xu S, Zhu S, et al. Assessment of non-prescription antibiotic dispensing at community pharmacies in China with simulated clients: a mixed cross-sectional and longitudinal study. Lancet Infect Dis 2019;19:1345–54. 10.1016/S1473-3099(19)30324-X [DOI] [PubMed] [Google Scholar]
- 21.Harris PA, Taylor R, Minor BL, et al. The REDCap Consortium: building an international community of software platform partners. J Biomed Inform 2019;95:103208. 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zawahir S, Lekamwasam S, Aslani P. Antibiotic dispensing practice in community pharmacies: a simulated client study. Res Social Adm Pharm 2019;15:584–90. 10.1016/j.sapharm.2018.07.019 [DOI] [PubMed] [Google Scholar]
- 23.Schlesselman JJ. Sample size requirements in cohort and case-control studies of disease. Am J Epidemiol 1974;99:381–4. 10.1093/oxfordjournals.aje.a121625 [DOI] [PubMed] [Google Scholar]
- 24.Virenfeldt J, Rudolf F, Camara C, et al. Treatment delay affects clinical severity of tuberculosis: a longitudinal cohort study. BMJ Open 2014;4:e004818. 10.1136/bmjopen-2014-004818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bell CA, Ilomäki J, Pichenda K, et al. Referral of tuberculosis symptomatic clients from private pharmacies to public sector clinics for diagnosis and treatment in Cambodia. J Eval Clin Pract 2015;21:285–91. 10.1111/jep.12306 [DOI] [PubMed] [Google Scholar]
- 26.Lönnroth K, Thuong LM, Linh PD, et al. Delay and discontinuity--a survey of TB patients' search of a diagnosis in a diversified health care system. Int J Tuberc Lung Dis 1999;3:992–1000. [PubMed] [Google Scholar]
- 27.Lönnroth K, Lambregts K, Nhien DT, et al. Private pharmacies and tuberculosis control: a survey of case detection skills and reported anti-tuberculosis drug dispensing in private pharmacies in Ho Chi Minh City, Vietnam. Int J Tuberc Lung Dis 2000;4:1052–9. [PubMed] [Google Scholar]
- 28.Goossens H, Ferech M, Vander Stichele R, et al. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. The Lancet 2005;365:579–87. 10.1016/S0140-6736(05)17907-0 [DOI] [PubMed] [Google Scholar]
- 29.Chen T-C, Lu P-L, Lin C-Y, et al. Fluoroquinolones are associated with delayed treatment and resistance in tuberculosis: a systematic review and meta-analysis. Int J Infect Dis 2011;15:e211–6. 10.1016/j.ijid.2010.11.008 [DOI] [PubMed] [Google Scholar]
- 30.WHO . Meeting report of the who expert consultation on the definition of extensively drug-resistant tuberculosis, 2021. Available: https://www.who.int/publications/i/item/meeting-report-of-the-who-expert-consultation-on-the-definition-of-extensively-drug-resistant-tuberculosis [Accessed 03 Mar 2021].
- 31.Bahta M, Tesfamariam S, Weldemariam DG, et al. Dispensing of antibiotics without prescription and associated factors in drug retail outlets of Eritrea: a simulated client method. PLoS One 2020;15:e0228013. 10.1371/journal.pone.0228013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nga DTT, Chuc NTK, Hoa NP, et al. Antibiotic sales in rural and urban pharmacies in northern Vietnam: an observational study. BMC Pharmacol Toxicol 2014;15:6. 10.1186/2050-6511-15-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Daftary A, Satyanarayana S, Jha N, et al. Can community pharmacists improve tuberculosis case finding? a mixed methods intervention study in India. BMJ Global Health 2019;4:e001417. 10.1136/bmjgh-2019-001417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lam TT, Dang DA, Tran HH, et al. What are the most effective community-based antimicrobial stewardship interventions in low- and middle-income countries? A narrative review. J Antimicrob Chemother 2021;76:1117–29. 10.1093/jac/dkaa556 [DOI] [PubMed] [Google Scholar]
- 35.File TM, Srinivasan A, Bartlett JG. Antimicrobial stewardship: importance for patient and public health. Clin Infect Dis 2014;59 Suppl 3:S93–6. 10.1093/cid/ciu543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kwan A, Daniels B, Saria V, et al. Variations in the quality of tuberculosis care in urban India: a cross-sectional, standardized patient study in two cities. PLoS Med 2018;15:e1002653. 10.1371/journal.pmed.1002653 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2021-006475supp001.pdf (60.4KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information. All deidentified data are included in the article and tables.