Abstract
Introduction
Studies have indicated that youth who use e-cigarettes are more likely to progress to cigarette smoking; however, the likelihood that these youth would have used tobacco products in the pre-vaping era is unclear.
Aims and Methods
This study sought to determine whether youth who used e-cigarettes in 2014–2018 would have likely been smokers in the period preceding e-cigarette availability. Analyzing Monitoring the Future 12th grade data (United States, 2009–2018), we forecasted the prevalence of current smoking with logistic regression-derived propensity scores. Models predicted smoking for all subsequent years, incorporating sociodemographic, family, alcohol, and school-related variables, and a linear time trend. We compared forecasted to observed smoking prevalence annually, and prevalence of current e-cigarette use among nonsmokers across smoking propensity tertiles.
Results
Until 2014, observed smoking prevalence mirrored forecasted prevalence. Afterward, forecasted rates consistently overestimated prevalence. Among nonsmoking youth, e-cigarette use was lowest among those with lowest predicted probability of cigarette smoking (3.8%; 95% confidence interval [CI]: 3.3, 4.4) and highest among those with highest probability (23.5%; 95% CI: 22.2, 24.9).
Conclusions
Youth e-cigarette use has increased rapidly, with high prevalence among nonsmoking youth. However, the decline in current smoking among 12th graders has accelerated since e-cigarettes have become available. E-cigarette use is largely concentrated among youth who share characteristics with smokers of the pre-vaping era, suggesting e-cigarettes may have replaced cigarette smoking.
Implications
Among nonsmoking youth, vaping is largely concentrated among those who would have likely smoked prior to the introduction of e-cigarettes, and the introduction of e-cigarettes has coincided with an acceleration in the decline in youth smoking rates. E-cigarettes may be an important tool for population-level harm reduction, even considering their impact on youth.
Introduction
E-cigarettes were introduced to the United States in 2009, becoming widely available around 2014.1 Their potential public health implications have been hotly debated.2 While recent clinical trials have indicated the promise of e-cigarettes in smoking cessation,3 and a special committee review by the National Academy of Sciences found “conclusive evidence” that complete switching to e-cigarettes from cigarettes reduces toxicant and carcinogen exposure,4 there is considerable concern e-cigarettes may initiate youth into nicotine dependence. Studies have indicated that youth who use e-cigarettes are more likely to progress to cigarette smoking.4 However, it is unclear whether nonsmoking youth who use e-cigarettes would have been smokers prior to the widespread availability of e-cigarettes, or if e-cigarette use is occurring among youth who would not have otherwise used any nicotine or tobacco product. This is a critical gap in the research informing the debate over e-cigarettes’ role in population-level harm reduction.
Prior studies have sought to address this question using various methods and populations with mixed results. Studies conducted in the earlier years of e-cigarettes’ widespread availability in Scotland, England, and Hawaii have found that e-cigarette use may predict smoking onset among youth with fewer risk factors for and more protective factors against smoking initiation.5–7 However, in the United States, one recent study of nationally representative group-level data showed that the rapid increase in youth e-cigarette uptake temporally coincided with a faster decline in youth smoking prevalence.8 Another recent study used propensity score matching in another nationally representative dataset showing that <1% of adolescents who used e-cigarettes first were established cigarette smokers, and that adolescents who used e-cigarettes first were less likely to become cigarette smokers compared with adolescents who tried other tobacco products first, or to matched adolescents who did not initially use any tobacco product.9 These conflicting findings suggest that more research is necessary to clarify the nature of the relationship between youth e-cigarette use and smoking initiation.
While it is difficult to draw a causal relationship between e-cigarette availability and decreased smoking behavior within the United States without a control group (e-cigarettes became widely available throughout the country at once), two pieces of evidence would further support this hypothesis. First, a forecasting model incorporating individual-level covariates that accurately predicts smoking prevalence prior to the introduction of e-cigarettes, but overestimates smoking prevalence after their introduction, would suggest e-cigarettes displaced smoking. Second, the prevalence of e-cigarette use among nonsmoking youth would be concentrated among those with a high forecasted probability of current smoking based on their sociodemographic and other characteristics. The current study used data from Monitoring the Future, a nationally representative school-based survey, to predict current smoking prevalence among 12th graders in the United States using regression-derived propensity scores. We compared forecasted to observed smoking prevalence annually, both prior to and following the widespread availability of e-cigarettes, and examined the prevalence of current e-cigarette use among nonsmoking youth across smoking propensity tertiles.
Methods
We analyzed publicly available data from 12th graders in the 2009–2018 Monitoring the Future study (N = 139 142), a repeated cross-sectional survey conducted in a nationally representative school-based sample. Beginning in 2004–2008, and ending in 2009–2013 (the period preceding widespread e-cigarette availability), we used rolling 5-year periods to fit survey-weighted logistic models for the odds of current (past 30-day) cigarette smoking, then predicted smoking probability for all subsequent years not included in each model. In addition to a linear time trend, models included students’ age, gender, race/ethnicity, geographic region of residence, urbanicity of current residence, urbanicity of childhood residence, school type, grade point average, alcohol consumption, presence of father in the household, parents’ educational attainment, and number of siblings. Models excluded any variable related to youth smoking that could have been changed by the introduction or availability of e-cigarettes (eg, close friends’ approval of smoking may decrease as a result of introducing e-cigarettes), as these were considered potential mediators of the effect of e-cigarette availability on adolescent smoking. We compared observed smoking prevalence each year to prevalence forecasts among all youth in the sample. For 2016–2018 (the years for which data on e-cigarette use were available) we compared the prevalence of current e-cigarette use among nonsmokers across tertiles of smoking propensity scores (tertiles were assigned within years, and propensity scores were estimated based on a model fit to 2009–2013 data).
Results
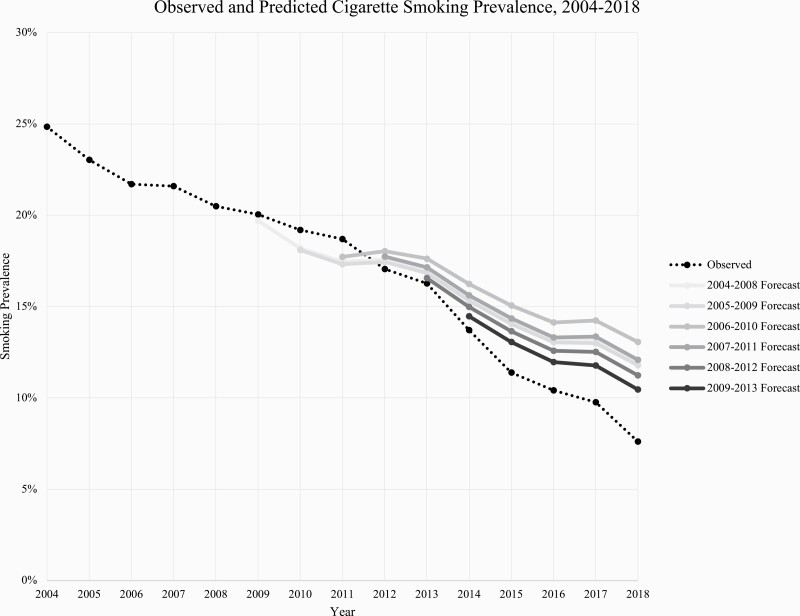
Prior to 2014, there were negligible differences between the forecasted and observed smoking prevalence (mean difference: <−0.1%, range: −1.4%, 1.4%). In contrast, for the period 2014–2018, forecasted rates consistently overestimated observed smoking prevalence (mean difference: −2.9%, range: −5.5%, −0.8%). Forecasted prevalence diverged from observed prevalence increasingly over time as vaping prevalence increased. By 2018, forecasting based on 2009–2013 observations, current 12th grade smoking prevalence was 7.6% (95% confidence interval [CI]: 7.1, 8.1) compared with a predicted 9.7% (95% CI: 9.4, 10.0) (Figure 1). Among nonsmokers in 2016–2018, e-cigarette use was lowest among those with the lowest predicted probability of smoking (3.8%; 95% CI: 3.3, 4.4), and highest among those with the highest predicted probability of smoking (23.5%; 95% CI: 22.2, 24.9).
Figure 1.
Observed versus predicted cigarette smoking prevalence.
Discussion
Our study provides further evidence in support of earlier findings that, although youth e-cigarette use has increased rapidly, the decline in current smoking among 12th graders has accelerated since the availability of e-cigarettes.8 Our findings also supported work showing that adolescents who tried e-cigarettes as their first tobacco product were less likely to have ever smoked or currently smoke cigarettes compared with adolescents who used another non-cigarette tobacco product first, or matched controls.9
We also identified novel evidence that declining smoking is likely not due to changing compositions of high school students. Our forecasting approach showed that smoking prevalence declined even compared with a counterfactual population for which sociodemographic and other factors predictive of smoking remained constant. Additionally, among nonsmokers, e-cigarette use was most common among youth who would have had the highest likelihood of becoming smokers prior to e-cigarettes’ popularization, and is extremely uncommon among youth with a low probability of smoking, with that probability conditional on individual-level smoking predictors and determined by extrapolating data from the pre-vaping period. There may be unknown factors unrelated to the availability of e-cigarettes that changed the rate of decline in youth smoking rates beginning in 2014. However, these findings contribute to a body of evidence suggesting that the availability of e-cigarettes may reduce population-level harm from nicotine products, and provide evidence against the hypothesis that e-cigarette availability promotes nicotine dependence in youth who would not have otherwise used nicotine products.
These findings should be interpreted in the context of previous research. One study conducted in four Scottish schools in 2015–2016 found that never smokers aged 11–18 who had never tried an e-cigarette at baseline were more likely to have experimented with cigarettes at follow-up one year later.5 Analyses controlled for whether youth self-reported at baseline that they would smoke if a friend offered a cigarette or any time in the next year. Another study conducted in 2014–2015 among students (aged 13–14 at baseline) in English schools had similar findings: students that had never smoked but had tried e-cigarettes at baseline had four times the odds of initiating smoking by follow-up.6 This study controlled for friend and family smoking behavior, plans to smoke, smoking norms and beliefs, perceived behavioral control, and self-efficacy about saying no to smoking. A school-based study conducted among 9th–11th graders in Hawaii in 2013–2014 found that the relationship between baseline e-cigarette use and smoking onset at follow-up was stronger for adolescents with lower levels of rebelliousness and willingness to smoke and higher levels of parental support.7
These differences may be attributable to several factors. First, two of these studies were conducted in the United Kingdom, where e-cigarette use has not increased at the same rate or become as widespread as in the United States, and where e-cigarette regulations are more comprehensive.10 The third study took place in Hawaii prior to and in the first year of e-cigarettes’ widespread availability, and may represent an entirely different social context than the current one. Further, these studies accounted for preexisting risk for smoking initiation using factors chosen through theory and empirical evidence. Our study extends these methods by accounting for a large number of factors contributing to smoking propensity, and verifying the predictive validity of our models by comparing smoking prevalence predicted by our models to observed prevalence in the same data, finding negligible differences prior to the widespread availability of e-cigarettes (indicating that our model was well calibrated to predict smoking prevalence in the absence of e-cigarettes), and increasing divergence each year afterward. These studies also may not all be directly comparable to the current study because of differences in outcome measures (eg, experimentation vs. current smoking).
Youth who have not initiated smoking by 12th grade may still go on to become smokers, particularly as the average age of smoking initiation increases.11 However, at least half of smokers initiate before age 18, and initiating prior to age 18 (compared with between 18 and 21) is associated with a greater likelihood of regular smoking and nicotine dependence.12 However, future research should use other samples to extend these methods beyond age 18, into early adulthood. Additionally, our models extrapolate pre-2014 linear time trends to predict smoking rates in later years, which requires stronger assumptions than study designs that are able to incorporate control groups. Future research should consider leveraging time differences in the introduction of e-cigarettes between jurisdictions to further these methods.
This study adds to a growing body of literature indicating that e-cigarettes’ potential benefits for smoking cessation may not be outweighed by their contribution to youth tobacco initiation, in terms of their overall public health impact. Reducing demand for and use of all nicotine products is an important public health goal. However, it is also critical to weigh the potential for e-cigarettes to reduce nicotine-related harm on a population level when evaluating specific public health policies that may reduce their availability.
Supplementary Material
A Contributorship Form detailing each author’s specific involvement with this content, as well as any supplementary data, are available online at https://academic.oup.com/ntr.
Funding
This work was supported by National Institute on Alcohol Abuse and Alcoholism T32 AA007459 to NAS.
Declaration of Interests
None declared.
References
- 1. U.S. Department of Health and Human Services. E-cigarette Use Among Youth and Young Adults. A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2016. [Google Scholar]
- 2. Fairchild AL, Bayer R, Lee JS. The e-cigarette debate: what counts as evidence? Am J Public Health. 2019;109(7):1000–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hajek P, Phillips-Waller A, Przulj D, et al. A randomized trial of e-cigarettes versus nicotine-replacement therapy. N Engl J Med. 2019;380(7):629–637. [DOI] [PubMed] [Google Scholar]
- 4. Committee on the Review of the Health Effects of Electronic Nicotine Delivery Systems. Harm reduction. In: Stratton K, Kwan LY, Eaton DL, eds. Public Health Consequences of E-Cigarettes. Washington, DC: National Academies Press; 2018. [PubMed] [Google Scholar]
- 5. Best C, Haseen F, Currie D, et al. Relationship between trying an electronic cigarette and subsequent cigarette experimentation in Scottish adolescents: a cohort study. Tob Control. 2018;27(4):373–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Conner M, Grogan S, Simms-Ellis R, et al. Do electronic cigarettes increase cigarette smoking in UK adolescents? Evidence from a 12-month prospective study. Tob Control. 2018;27(4):365–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wills TA, Sargent JD, Gibbons FX, Pagano I, Schweitzer R. E-cigarette use is differentially related to smoking onset among lower risk adolescents. Tob Control. 2016;26(5):534–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Levy DT, Warner KE, Cummings KM, et al. Examining the relationship of vaping to smoking initiation among US youth and young adults: a reality check. Tob Control. 2019;28(6):629–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shahab L, Beard E, Brown J. Association of initial e-cigarette and other tobacco product use with subsequent cigarette smoking in adolescents: a cross-sectional, matched control study. Tob Control. 2021;30(2):212–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hammond D, Rynard VL, Reid JL. Changes in prevalence of vaping among youths in the United States, Canada, and England from 2017 to 2019. JAMA Pediatr. 2020;174(8):797–799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Barrington-Trimis JL, Braymiller JL, Unger JB, et al. Trends in the age of cigarette smoking initiation among young adults in the US from 2002 to 2018. JAMA Netw Open. 2020;3(10):e2019022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ali FRM, Agaku IT, Sharapova SR, Reimels EA, Homa DM. Onset of regular smoking before age 21 and subsequent nicotine dependence and cessation behavior among US adult smokers. Prev Chronic Dis. 2020;17:E06. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.