Abstract
Background
There is limited evidence for use of the Research Capacity and Culture tool across multidisciplinary health professionals. We explored using the Research Capacity and Culture tool among multidisciplinary health professionals at an Australian secondary hospital.
Methods
A cross-sectional observational study where online and paper-based surveys of the Research Capacity and Culture tool were disseminated between November 2020 and January 2021. Descriptive analyses of demographic variables and Likert scale items were summarized using median and inter-quartile ranges. Differences between organization, team and individual domains were checked using a Friedman test. Post-hoc Wilcoxon signed rank tests determined specific differences between domains.
Results
Seventy-six multidisciplinary health professionals (female, 89.3%) reported overall perceptions of research success/skills highest in the organization (median 6), followed by the team (median 5) and individual domains (median 3.5). Only 21.3% agreed that research activities were a part of their role description. Mean scores across professions were highest for Medicine (5.47), Midwifery (4.52), Nursing (4.47) and Allied Health (3.56), respectively, for the team domain. Individual domain scores across all professions were below 50%. Commonly reported barriers to research were “lack of time for research,” “other work roles taking priority” and “a lack of skill.” “Developing skills” was the most common personal motivator.
Conclusion
Multidisciplinary health professionals reported the highest overall perception of research success/skills in the organization domain. Medical health professionals perceived research success/skills highest compared to nursing, midwifery and allied health professionals.
Keywords: research capacity, research culture, workforce, nursing, midwifery, allied health, medicine, organizational planning
Background
Research culture is described as an environment within an organization that supports the growth of new scientific knowledge and provides opportunities for staff to translate research into practice.1 It is well known that evidence-based practice is essential for the delivery of effective and efficient services within the healthcare sector.2,3 An enabling research culture promotes integration of the best available evidence to inform health policy and service planning to ensure optimal consumer and health system outcomes.4 Research capacity, alternatively, refers to the ability to produce research.1 Building research capacity is fundamental to enabling research culture growth within any health service and is reliant on the continual development of individual skills and organizational infrastructure and processes in research.5 The benefits of increasing research capacity include increased workforce retention, job satisfaction, workforce research skills, patient satisfaction and integration of evidence-based practice.6,7
A strategic and methodological approach to building research capacity is required, given the evolving nature of health policies, constant changes in healthcare leadership and research champion positions; and the multidisciplinary nature of health professionals and clinical services within a hospital and health service.8,9 The research capacity and culture (RCC) tool is a validated measure of research capacity and culture at the individual, team and organization levels within an Australian healthcare context.10 The RCC tool is a well-established tool to measure research capacity and culture and has excellent internal consistencies (α = 0.95, 0.96 and 0.96 respectively) and strong test–retest reliability (ICC = 0.77, 0.83 and 0.82 respectively) across organisation, team and individual domains.10
Past studies using the RCC tool to measure research culture and capacity have either focused on allied health professionals within Australian tertiary and regional facilities; or on single allied health disciplines.1,11–18
While other tools to measure research capacity are validated and used in the literature, the RCC is reported to be a good example of a comprehensive tool and is widely used.19 There is a need for the development of a tailored RCC tool which is contextualised to multidisciplinary healthcare professionals that includes medical, nursing and midwifery staff alongside allied health professionals. Validating the RCC tool on multidisciplinary healthcare professionals is vital due to: a) the multidisciplinary nature of the delivery of clinical services across an organisation; and b) generalisability of the RCC tool in healthcare contexts of varying sectors. Friesen and colleagues reported on RCC among nursing, allied health and health management staff in a community health services context and found that community health staff had limited capacity to generate research with current levels of skill, funding and time.13 However, no medical health professionals were surveyed in this study which is a limitation because medical health professionals’ clinical practice is strongly informed by available evidence when compared to allied health, nursing and midwifery health professions.20,21 Thus, the evaluation of RCC within a healthcare context would benefit from the inclusion of multidisciplinary health professions with varying levels of research skills and practice.
The delivery of women, children and family services within a healthcare environment is multidisciplinary in nature and includes medical, allied health, nursing and midwifery health professionals. Understanding perceptions on RCC across all professions is vital in developing research infrastructure, systems and initiatives which are appropriate and tailored to current workforce composition. A formal assessment of research skill gaps and training needs at the individual and organizational levels is fundamental to inform the development of individualized research capacity and capability strategies and initiatives. However, no studies were identified that use the RCC tool across multidisciplinary allied health, nursing, midwifery and medical health professionals specifically working in women, children and family services. Thus, this study aimed to explore the current research capacity and culture among health professionals working with women, children and family services at an Australian 265-bed (Level 4, Clinical Services Capability Framework)22 secondary hospital using the RCC tool; and identify motivators and barriers to research participation. This study provides practical contributions to researchers and policy makers by providing insights on how the Research Capacity and Culture (RCC) tool could be applied across multidisciplinary health professionals within a healthcare facility.
Methods
We conducted a cross-sectional observational study an Australian secondary 265-bed facility (Level 4, Clinical Services Capability Framework) Hospital22 within the largest hospital and health service in Australia. Women, Children and Family services are provided within acute and ambulatory care settings across metropolitan, regional and rural areas of Queensland, Australia.
Ethics Approval and Consent to Participate
Caboolture Hospital is a part of Metro North Hospital & Health Service (MNHHS) in Queensland, Australia. MNHHS is the largest hospital and health service in Australia and consists of a number of hospitals and facilities including:
Royal Brisbane & Women’s Hospital
The Prince Charles Hospital
Redcliffe Hospital
Caboolture Hospital
Surgical Treatment and Rehabilitative Services
Community & Oral Health Services
All ethical review of studies are completed at either at Royal Brisbane & Women’s Hospital or The Prince Charles Hospital Human Research Ethics Committees (HREC). This study was approved by The Prince Charles Hospital HREC (Project ID: 65960) as a low-risk research project. Staff provided implied consent through voluntary completion of the survey. The study was conducted according to Good Clinical Practice (GCP), the declaration of Helsinki and the National Health and Medical Research Council (NHMRC) criteria for the ethical conduct of research in humans.
Participants and Recruitment
All health professionals working with women, children and/or families, as part of their employment were eligible to participate in this study. Health professionals (eg, nursing, midwifery, medical, allied health) employed on a casual, temporary or permanent basis at any full-time equivalent met inclusion criteria. During the study period, there were a total of 35.2 medical, 9.2 allied health, 23 paediatric nurses and 90 midwifery full-time equivalent staff working within women, children and family services at our facility. Administrative staff and health professional students on placement were excluded.
Convenience sampling was used and the RCC survey was promoted across health professional streams and services using multiple communication strategies including: targeted phone calls and/or emails to directors, bulk staff emails from unit managers to eligible staff, facility newsletters; physical survey return boxes were left on the maternity and children’s wards for return of completed paper surveys; and in person attendance at clinical (eg, daily ward rounds) and non-clinical (eg, departmental meetings, special interest groups) meetings across nursing, midwifery, medical and allied health.
Research Capacity and Culture (RCC) Tool
An online [via Research Electronic Data Capture (RedCAP®) software] and paper-based survey were disseminated between November 2020 to January 2021. This survey included study information at the beginning for potential participants to read and provide informed voluntary consent to participate. The remainder of the survey consisted of demographic questions and the full RCC tool.10 Demographic questions from the original RCC tool included: work role title, professional qualifications and enrolment in a research higher degree. Additional demographics were collated to enable further exploration of any relationship between demographic characteristic and RCC outcomes to assist in the development of a research capacity and capability plan individualized to our workforce. Additional demographic information collected included: age, work role level/grading, number of years in professional service, employment status, predominant workplace setting and discipline. The full RCC tool consisted of a total of 52 questions across the domains of organization, team and individual levels. A copy of the RCC tool for this study can be found in the article by Holden et al.10
Outcome Measures
Primary outcomes included overall responses for the organization, team and individual components of the RCC tool. Secondary outcomes included categorical variables for barriers (n=18) and facilitators (n=18) to research capacity and culture on the RCC tool.
Statistical Analysis
Descriptive analysis of each demographic variable and Likert scale item on the RCC tool were summarized using median and inter-quartile ranges (IQR). The RCC results for the organizational, team and individual domains were analyzed as ordinal data (scale 1–10) and a domain mean for each Professional group recorded. “Unsure” responses were scored 0 and not included in the calculation of descriptive statistics but reported separately.
Differences between organization, team and individual domains were checked using a Friedman test. Where a difference was found between domains, post hoc Wilcoxon signed rank tests was used to determine specifically which parameters in the domains differed. The level of statistical significance was set at p<0.05. Data were analyzed using IBM SPSS Statistics software version 27.
Results
A total of 76 predominantly female (89.3%) health professional staff participated in this study with one survey incomplete and removed from the analysis resulting in an estimated completion rate of 47.6%. Higher proportions of medical and allied health professionals returned surveys than midwives and nurses. Demographics for participants are detailed in Table 1.
Table 1.
Demographics of Participants
| Nursing F(%) | Midwifery F(%) | Medical F(%) | Allied Health F(%) | |
|---|---|---|---|---|
| Health Profession | 22 (28.9%) | 25 (32.9%) | 20 (27.6%) | 8 (10.5%) |
| Sex | ||||
| Male | 0 | 0 | 7 (40%) | 0 |
| Female | 22 (100%) | 25 (100%) | 12 (60%) | 8 (100%) |
| Mainly working in: (could select more than one) | ||||
| Paediatrics | 17 (77%) | 0 | 10 (50%) | 5 (62%) |
| Obstetrics/ Gynaecology | 2 (9%) | 3 (12%) | 8 (40%) | 2 (25%) |
| Maternity | 6 (27%) | 25 (100%) | 5 (25%) | 7 (87%) |
| Neonatal | 4 (18%) | 1 (4%) | 1 (5%) | 3 (38%) |
| Years employed as HP | ||||
| <2 | 0 | 6 (24%) | 7 (37%) | 0 |
| 2–5 | 2 (9%) | 1 (4%) | 5 (26%) | 3 (38%) |
| 6–10 | 2 (9%) | 0 | 1 (6%) | 2 (25%) |
| 11–15 | 2 (9%) | 0 | 2 (10%) | 0 |
| 16–20 | 1 (5%) | 2 (8%) | 0 | 1 (12%) |
| >20 | 15 (68%) | 16 (64%) | 4 (21%) | 2 (25%) |
| Years employed at this site | ||||
| <2 | 1 (4%) | 6 (24%) | 10 (53%) | 3 (38%) |
| 2–5 | 5 (23%) | 1 (4%) | 5 (26%) | 2 (25%) |
| 6–10 | 5 (23%) | 4 (16%) | 1 (5%) | 2 (25%) |
| 11–15 | 2 (9%) | 4 (16%) | 2 (10%) | 0 |
| 16–20 | 2 (9%) | 3 (12%) | 1 (5%) | 0 |
| >20 | 7 (32%) | 7 (28%) | 0 | 1 (12%) |
| Location(s) of employment (astaff work across multiple settings) | ||||
| Inpatients | 18 (82%) | 24a (96%) | 18a (90%) | 6a (75%) |
| Outpatients | 4 (18%) | 3a (12%) | 12a (60%) | 4a (50%) |
| Home visiting | 0 | 2a (8%) | 0 | 0 |
| Community based | 0 | 2a (8%) | 0 | 0 |
| Employment status | ||||
| Full-Time | 2 (9%) | 5 (20%) | 9 (47%) | 4 (50%) |
| Full-Time temporary | 0 | 0 | 5 (26%) | 1 (13%) |
| Part-Time | 18 (91%) | 16 (64%) | 2 (11%) | 3 (27%) |
| Part-Time temporary | 2 (9%) | 2 (8%) | 2 (11%) | 0 |
| Casual | 0 | 2 (8%) | 1 (5%) | 0 |
| Qualifications | ||||
| Undergraduate Certificate/ Diploma | 2 (9%) | 1 (4%) | 0 | 0 |
| Undergraduate Degree | 7 (32%) | 11 (44%) | 5 (26%) | 5 (62%) |
| Honours/Post-Graduate Degree | 3 (14%) | 4 (16%) | 5 (26%) | 1 (13%) |
| Post-Graduate coursework | 9 (41%) | 7 (28%) | 8 (42%) | 2 (25%) |
| Masters/PhD by research | 1 (5%) | 0 | 1 (5%) | 0 |
| Currently undertaking Post-Graduate study | 0 | 2 (8%) | 1 (5%) | 0 |
Overall Perceptions of Organization, Team and Individual Level Perceptions of Research Culture and Capacity
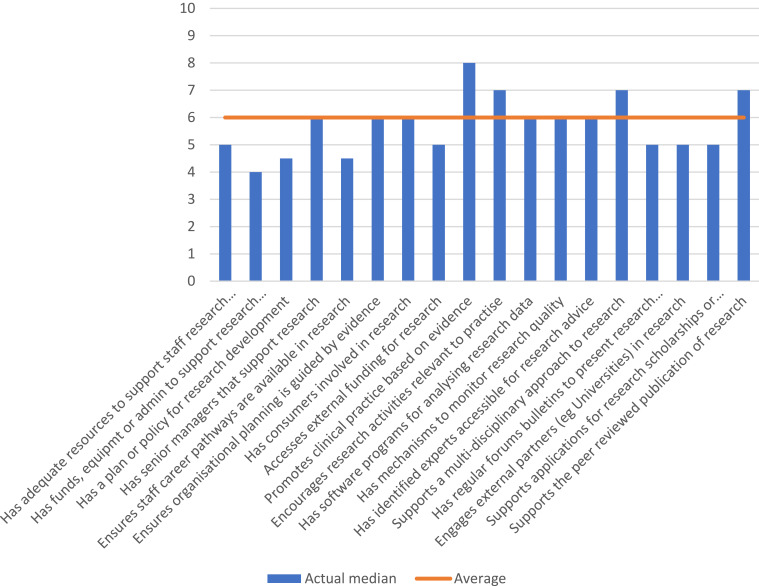
Across multidisciplinary health professionals working with women, children and family services, the median scores, on the scale of 1 to 10, for the organization domain (median 6) were highest followed by the team domain (median 5), with the individual domain lowest (median 3.5). See –figure3. For the organization domain, the highest median response was for “Promoted clinical practice based on evidence” (median 8) and lowest for “Has funds, equipment or admin to support research activities” (median 4). See Table 2.
Figure 1.
Overall participant perceptions of organisational-level research culture and capacity.
Notes:  Actual median.
Actual median.  Average.
Average.
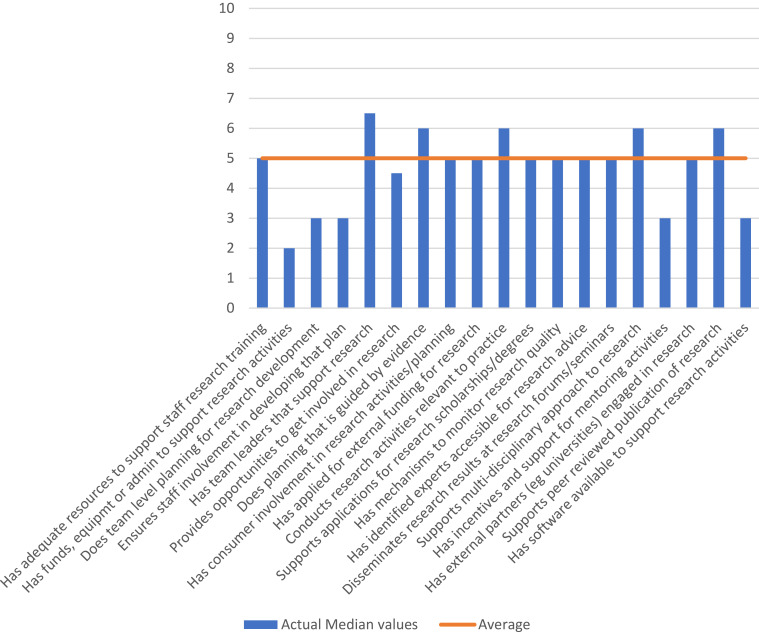
Figure 2.
Overall participant ranking of their perceptions of team-level research culture and capacity. Scale: 1, no skill or success; to 10, high skill or success.
Notes:  Actual median values.
Actual median values.  Average.
Average.
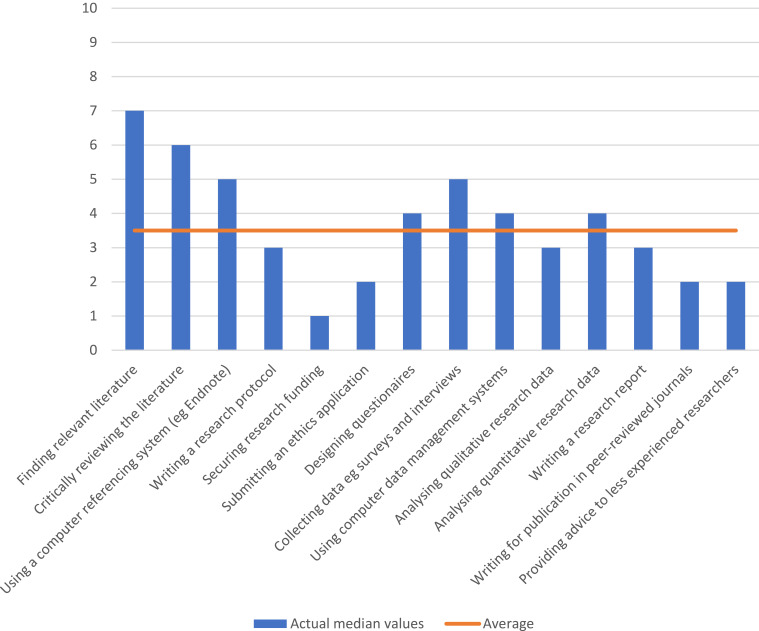
Figure 3.
Overall participants ranking of their own perceptions of their individual research culture and capacity. Scale: 1, no skill or success; to 10, high skill or success.
Notes:  Actual median values.
Actual median values.  Average.
Average.
Table 2.
Organizational Success/Skill Levels Across All Professions in Women’s Children’s Families Stream (N=75)
| Description | Median | IQR | % Unsure |
|---|---|---|---|
| Has adequate resources to support staff research training | 4 | 3–7 | 32 |
| Has funds, equipment, or admin to support research activities | 5 | 2–5 | 39 |
| Has a plan or policy for research development | 4.5 | 2–7 | 55 |
| Has senior managers who support research | 6 | 5–8 | 29 |
| Ensures staff career pathways are available in research | 4.5 | 2–6 | 39 |
| Ensures organization planning is guided by evidence | 6 | 5–8 | 35 |
| Has consumers involved in research | 6 | 4–7 | 45 |
| Accesses external funding for research | 5 | 2–7 | 55 |
| Promotes clinical practice based on evidence | 8 | 6–9 | 5 |
| Encourages research activities relevant to practice | 8 | 5–11 | 0 |
| Has software programs for analyzing research data | 6 | 4–8 | 71 |
| Has mechanisms to monitor research quality | 6 | 3–7 | 65 |
| Has identified experts accessible for research advice | 6 | 4–8 | 53 |
| Supports a multidisciplinary approach to research | 7 | 5–8 | 36 |
| Has regular forums/bulletins to present research findings | 5 | 2–7 | 29 |
| Engages external partners (eg, universities) in research | 5 | 3–7 | 45 |
| Supports applications for research scholarships/degrees | 5 | 4–7 | 44 |
| Supports the peer-reviewed publication of research | 7 | 4–7 | 44 |
Notes: 1=no success/skill and 10=highest possible success/skill.
Median responses to the team domain were highest for “Has team leaders that support research” (median 6.5); “Does planning that is guided by evidence” (median 6); “Conducts research activities relevant to practice” (median 6); and “Supports Multi-disciplinary approach to research” (median 6). The lowest scoring median response for the team domain was for “Has funds, equipment or admin to support research activities” (median 2). See Table 3.
Table 3.
Team Success/Skill Levels Across All Professions in Women’s Children’s Families Stream (N=75)
| Description | Median | IQR | % Unsure |
|---|---|---|---|
| Has adequate resources to support staff research training | 5 | 2–6 | 32 |
| Has funds, equipment, or admin to support research activities | 4 | 2–6 | 27 |
| Does team-level planning for research development | 3 | 2–6 | 32 |
| Ensures staff involvement in developing that plan | 3 | 2–5 | 32 |
| Has team leaders who support research | 6.5 | 4–8 | 25 |
| Provides opportunities to get involved in research | 4.5 | 3–6 | 20 |
| Does planning that is guided by evidence | 6 | 4–8 | 29 |
| Has consumer involvement in research activities/planning | 5 | 2–6 | 39 |
| Has applied for external funding for research | 5 | 2–6 | 55 |
| Conducts research activities relevant to practice | 6 | 3–7 | 25 |
| Supports applications for research scholarships/degrees | 5 | 4–7 | 43 |
| Has mechanisms to monitor research quality | 5 | 2–7 | 49 |
| Has identified experts accessible for research advice | 5 | 3–7 | 44 |
| Disseminates research results at research forums/seminars | 5 | 3–7 | 37 |
| Supports a multidisciplinary approach to research | 6 | 4–8 | 36 |
| Has incentives and support for mentoring activities | 3 | 2–6 | 44 |
| Has external partners (eg, universities) engaged in research | 5 | 2–7 | 48 |
| Supports peer-reviewed publication of research | 6 | 3–8 | 39 |
| Has software available to support research activities | 3 | 2–5 | 47 |
Notes: 1=no success/skill and 10=highest possible success/skill.
Individual median responses were much lower than for team and organization domains and below average (median 3.5). “Securing research funding” was lowest scoping across the WCF line (median 1). While “Finding relevant literature” scored highest (median 7). See Table 4.
Table 4.
Individual Success/Skill Levels Across All Professions in Women’s Children’s Families Stream (N=75)
| Description | Median | IQR | % Unsure |
|---|---|---|---|
| Finding relevant literature | 7 | 5–8 | 8 |
| Critically reviewing the literature | 6 | 3–8 | 8 |
| Using a computer referencing system (eg, Endnote) | 5 | 2–7 | 11 |
| Writing a research protocol | 3 | 1–6 | 12 |
| Securing research funding | 1 | 1–3 | 19 |
| Submitting an ethics application | 2 | 1–3 | 20 |
| Designing questionnaires | 4 | 1–7 | 15 |
| Collecting data, eg, surveys and interviews | 5 | 3–7 | 13 |
| Using computer data management systems | 4 | 2–6 | 15 |
| Analyzing qualitative research data | 3 | 1–6 | 16 |
| Analyzing quantitative research data | 4 | 1–7 | 16 |
| Writing a research report | 3 | 1–6 | 15 |
| Writing for publication in peer-reviewed journals | 2 | 1–3 | 17 |
| Providing advice to less experienced researchers | 2 | 1–3 | 17 |
Notes: 1=no success/skill and 10=highest possible success/skill.
The mean number of participants selecting “unsure” for a majority of items in the organization and team domains were high (41.4% and 38.0% respectively), but much lower at 16% for the individual domain.
Only Item 9 in organization domain (“Promoted clinical practice based on evidence”) had a low rate of “unsure” response (5.3%). Sub analysis of these unsure responses for the organization domain showed no significant differences in mostly unsure responses (>50%) for health professions (Pearson χ2 = 3.637 DF=3 p=0.303), total years employed (Pearson χ2 = 3.888 DF=5 p=0.566), or professional qualifications (Pearson χ2 = 5.767 DF=4 p=0.217). However, there were significant differences in mostly unsure responses for those working in paediatrics (Pearson χ2 = 5.418 DF=1 p=0.020), but not obstetrics, maternity or neonatal areas.
Sub analysis of the unsure responses for the team domain showed no significant differences in mostly unsure responses for sex (Pearson χ2 = 0.285 DF=1 p=0.594), location of work, and total years employed (Pearson χ2 = 3.059 DF=5 p=0.691). However, there were significant differences in mostly unsure responses for health professions (Pearson χ2 = 12.862 DF=3 p=0.006), professional qualifications (Pearson χ2 = 10.746 DF=4 p=0.030), and for those working in paediatrics (Pearson χ2 = 4.606 DF=1 p=0.032), but not obstetrics, maternity or neonatal areas.
Sub analysis of these unsure responses for the individual domain showed no significant differences in mostly unsure responses for sex (Pearson χ2 = 0.021 DF=1 p=0.884), health profession (Pearson χ2 = 2.279 DF=3 p=0.516), location of work, stream/area of work, professional qualifications, and total years employed (Pearson χ2 = 1.838 DF = 5 p = 0.871).
There was a significant difference in the overall median scores for the organization, team, and individual domains of the RCC (Friedman χ2(2) = 27.434, p < 0.001). Post hoc analysis with Wilcoxon signed-rank tests demonstrated that the organization domain had a significantly higher median (IQR) score of 6 (4–8) than the team domain 5 (3–6) (Z = −4.409, p < 0.001) and that both the organization and team domains’ median scores were significantly higher than that of the individual domain, 4 (2–6) (organization versus individual domain Z = −4.858, p < 0.001; team versus individual domain Z = −2.155, p = 0.031). The data were not sufficient to perform exploratory factor analysis.
The majority of respondents were not currently involved in research [n = 57 (77%]. Collecting data was the highest ranked research activity [n = 11 (14.9%)], while no respondents reported any activity relating to submitting an ethics application or writing a literature review. In the past 12 months 6.8% had co-authored a paper for publication or presented research findings at a conference (4.1%). Only 21.3% of respondents agreed that research activities were part of their role description.
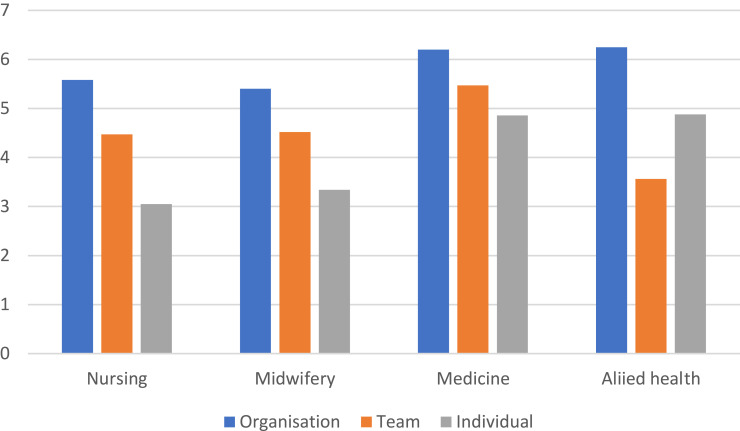
Perceptions of Organization Research Culture and Capacity by Health Profession
Across the organization domain, mean scores across professions were highest for Allied Health (6.25), then Medicine (6.2) Nursing (5.58), and lowest for Midwifery (5.4) respondents. Mean scores across professions were highest for Medicine (5.47), then Midwifery (4.52), Nursing (4.47) and lowest for Allied Health (3.56) respondents for the team domain. For the individual domain, mean scores across professions were below 50% for all professions. See Figure 4 for full details.
Figure 4.
Median perceptions of organisation research culture and capacity by health profession.
Notes:  Organisation.
Organisation.  Team.
Team.  Individual.
Individual.
Motivators and Barriers to Research
The most commonly reported barriers to research were “lack of time for research,” “other work roles taking priority” and “a lack of skill.” Almost one-third of respondents (31%) reported that they were “not interested in research.” “Developing skills” was the most common personal motivator to do research with “career advancement,” “identified problem needing changing” and “to keep brain stimulated” the next most common motivators. Other barriers reported in comments included having been “put off by complexity of research”; “a previous bad experience with a university supervisor” and missed opportunity when “outcomes of research (were) presented by other team members”.
Discussion
This article reports on the research capacity and culture for the multidisciplinary team providing care for women, children, and families of an Australian secondary hospital. Overall responses were highest for the organization domain, followed by the team domain and lowest for the individual domain. This was similarly reflected in responses for each professional stream (medicine, midwifery and nursing) with allied health the exception, who responded highest overall for organization, then individual and lowest for the team domain. However, despite a high proportional response, there were, comparatively, very small numbers of allied health respondents to the other professional groups. A large percentage of all respondents were unsure on a majority of items in relation to the organization and team domains similar to other studies using this tool.1,12,13,23
In our study, health professionals working in women, children and family services within our facility reported the highest scores for research skills and success in the organization domain and the lowest scores in the individual domain. This is consistent with previous studies which have reported RCC among multidisciplinary health professionals in a community health setting;13 and among multidisciplinary allied health professionals in tertiary,1 regional,11 and statewide public health care sectors.10,24 However, when directly comparing our study with RCC results reported among multidisciplinary health professionals in an Australian community health setting,13 notable differences exist across organization and team domains. Within the organization domain, our participants reported higher levels of “promoting clinical practice based on evidence” [median 8 (6–9) compared to mean 7.5 (2.0)],13 “encourages research activity relevant to practice” [median 8 (5–11) compared to mean 6.2 (2.4)],13 “supports multidisciplinary approach to research” [median 7 (5–8) compared to mean 5.9 (2.6)],13 “supports the peer-reviewed publication of research” [median 7 (4–7) compared to mean 5.8 (2.5)].13 Within the team domain, our participants reported lower levels of having “does team-level planning for research development” [median 3 (2–6) compared to mean 4.2 (2.3)] and “ensures staff involvement in developing that plan” [median 3 (2–5) compared to 4.4 (2.5)] and “has incentives and support for mentoring activities” [median 3 (2–6) compared to mean 4.3 (2.4)].13 The inclusion of non-clinical staff in Friesen’s study may provide an explanation for the differences in RCC at the team domain.13 In contrast, our RCC results were based on responses from frontline clinical staff within a hospital setting where dedicated time to attend team meetings related to research is scarce and is continuously competing with clinical demands.
Compared to RCC in a community health setting, health professional staff in our study reported higher research success/skills at the organizational level but lower perceptions of research success/skills at the team level. This suggests that overall, our current organization supports and values evidence-based practice; however, more work is required within the organization to improve our team leaders and managers on research receptivity, advocacy, and literacy. This is an important next step as healthcare leaders and managers are vital to the success of facilitating research culture.9
There were significant differences in mostly unsure responses across all domains for professionals working in paediatrics (Pearson χ2 = 5.418 DF=1 p=0.020), but not in obstetrics, maternity or neonatal areas. This was an unexpected result and why paediatric multidisciplinary staff perceive less capacity and below average supporting culture for research is unknown and is suggested as an area for further investigation. Other research highlights the fundamental nature of the organizational context in which professionals work remains central to the development of a research culture.25
The lowest proportion of unsure responses seen in the individual level domains suggests professionals were most confident in their knowledge of their own capability and capacity in research. However, the low median scores (median scores <50% across all professions) reflect a profession that has limited capacity for research. This may be further explained by large numbers who do not think research is part of their professional role and who do not want to be involved in research. Higher proportions of medical and allied health professionals returned surveys than midwives and nurses. In the face of the extensive distribution strategies and efforts to engage nursing and midwifery professionals, this finding further supports a disinterest in research by these groups. Other literature varied in the proportion of unsure responses with a study in primary health setting13 reporting similar high proportions to ours; whilst a study of allied health professionals in a local health district reported much lower unsure responses.1
Contrary to studies of RCC with allied health professionals, only 21.3% of all respondents in our study agreed that research activities were part of their role description.1,12,13,23 Both registered Nurse and Midwifery standards (1.7 and 6.1 respectively) state that “The Registered Nurse contributes to quality improvement and relevant research” and that “The Midwife actively contributes to quality improvement and research activities.” The lack of understanding of the requisite nature of the standards of practice for nurses and midwives has been identified. Barriers to achieving standards of practice such as research due to a lack of resources as well as a lack of evidence of nurses involvement in research, policy or guideline development has also been reported in other research.26 A lack of time and resources for research was consistently reported across the cohort in our study similar to other studies of multidisciplinary healthcare groups using this tool.27
To improve individual research success/skills, consideration for research internships aimed at providing staff with experience and opportunities to engage in research and/or quality improvement projects to learn and develop their research skills is recommended. Successful nursing and allied health research internship programs have been implemented with positive benefits reported from the perspective of graduates and organizations in relation to increased RCC and workforce retention.28–30 To improve team research success/skills, embedded researchers within clinical teams and a focus on developing team leaders and managers who are research literate is critical, including support to modify rosters to include non-clinical hours dedicated for quality improvement and/or research. Embedded researchers can facilitate increased networking, engage with and build research capacity of clinicians within their teams.31 The development of research leaders, on the other hand, has the potential to increase the clinical area or team’s research profile.32
The effectiveness of implemented initiatives to improve RCC among multidisciplinary healthcare professionals should be evaluated based on a combination of tangible traditional metrics (ie, publications, funding grants) and non-tangible metrics which take into consideration contextual influences (eg, attitudes, identity, expectations,)33 and changes on relational structures (eg, partnerships and networks, communications) essential for research success/skills.34
Strengths and Limitations
The use of a validated tool in understanding healthcare professional perceptions of research culture and capacity was a strength of our study design. However, there were some limitations to our study. These may include self-selection bias in participation. It is likely healthcare professionals who completed the RCC were the most interested and/or engaged in research. While enormous efforts were made to engage clinicians in participating in this survey, it is acknowledged that the response rates were low, particularly in the largest professional groups of nursing and midwifery. Future studies could consider completion of the RCC via mandatory training programs to ensure that results obtained are reflective of staff perceptions across health professional groups. Finally, it is acknowledged that the RCC tool does not provide established cut-off values. As a result, this limited our ability to meaningfully interpret the results as descriptive statistics was used in the absence of established cut-off values.
Conclusions
This study examined the research capacity and culture across multidisciplinary health professionals in a regional hospital setting. The highest perception of research success/skills across professions was in the organization domain. Medical health professionals perceived research success/skills highest compared to nursing, midwifery and allied health professionals. The consistent reporting of lack of resources such as time and competing clinical demands as barriers to research highlight a need for change on how support is provided for clinicians to engage in research. Recommendations including embedded clinical researchers and improving team leaders and managers research receptivity, advocacy, and literacy to lead by example. The study provides practical contributions to researchers and policy makers by providing insights on how the Research Capacity and Culture (RCC) tool could be applied across multidisciplinary health professionals within a healthcare facility.
Acknowledgments
Thank you to our nursing, midwifery, allied health and medicine colleagues who volunteered to participate in the study. We appreciate your honesty and truly value the opportunity to use the information you provided to help build on our research culture and capacity.
Funding Statement
No funding was received to complete this study.
Data Sharing Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
- 1.Alison JA, Zafiropoulos B, Heard R. Key factors influencing allied health research capacity in a large Australian metropolitan health district. J Multidiscip Healthc. 2017;10:277. doi: 10.2147/JMDH.S142009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sackett DL, Rosenberg WMC, Gray JAM, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. (it’s about integrating individual clinical expertise and the best external evidence)(Editorial). Br Med J. 1996;312(7023):71. doi: 10.1136/bmj.312.7023.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hanney S, Boaz A, Jones T, Soper B. Engagement in research: an innovative three-stage review of the benefits for health-care performance. Health Serv Deliv Res. 2013;1(8):1–152. doi: 10.3310/hsdr01080 [DOI] [PubMed] [Google Scholar]
- 4.Dimond EP, Germain D, Nacpil LM, et al. Creating a “culture of research” in a community hospital: strategies and tools from the national cancer institute community cancer centers program. Clin Trials. 2015;12(3):246–256. doi: 10.1177/1740774515571141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harding K, Lynch L, Porter J, Taylor NF. Organisational benefits of a strong research culture in a health service: a systematic review. Aust Health Rev 2017;41(1):45–53. doi: 10.1071/AH15180 [DOI] [PubMed] [Google Scholar]
- 6.Wenke R, Mickan S. The role and impact of research positions within health care settings in allied health: a systematic review. BMC Health Serv Res. 2016;16(a). doi: 10.1186/s12913-016-1606-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Misso ML, Ilic D, Haines TP, Hutchinson AM, East CE, Teede HJ. Development, implementation and evaluation of a clinical research engagement and leadership capacity building program in a large Australian health care service. (Report). BMC Med Educ. 2016;16(13). doi: 10.1186/s12909-016-0525-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whitworth A, Haining S, Stringer H. Enhancing research capacity across healthcare and higher education sectors: development and evaluation of an integrated model. BMC Health Serv Res. 2012;12:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Slade SC, Philip K, Morris ME. Frameworks for embedding a research culture in allied health practice: a rapid review. Health Res Pol Syst. 2018;16(1):29. doi: 10.1186/s12961-018-0304-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holden L, Pager S, Golenko X, Ware RS. Validation of the research capacity and culture (RCC) tool: measuring RCC at individual, team and organisation levels. Aust J Prim Health. 2012;18(1):62–67. doi: 10.1071/PY10081 [DOI] [PubMed] [Google Scholar]
- 11.Borkowski D, McKinstry C, Cotchett M. Research culture in a regional allied health setting. Aust J Prim Health. 2017;23(3):300–306. doi: 10.1071/PY16085 [DOI] [PubMed] [Google Scholar]
- 12.Elphinston RA, Pager S. Untapped potential: psychologists leading research in clinical practice. Aust Psychol. 2015;50(2):115–121. doi: 10.1111/ap.12102 [DOI] [Google Scholar]
- 13.Friesen EL, Comino EJ. Research culture and capacity in community health services: results of a structured survey of staff. Aust J Prim Health. 2016;23(2):123–131. doi: 10.1071/PY15131 [DOI] [PubMed] [Google Scholar]
- 14.Howard AJ, Ferguson M, Wilkinson P, Campbell KL. Involvement in research activities and factors influencing research capacity among dietitians. J Hum Nutr Diet. 2013;26(1):180–187. doi: 10.1111/jhn.12053 [DOI] [PubMed] [Google Scholar]
- 15.Lazzarini P, Geraghty J, Kinnear E, Butterworth M, Ward D. Research capacity and culture in podiatry: early observations within Queensland Health. J Foot Ankle Res. 2013;6(1):1. doi: 10.1186/1757-1146-6-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pager S, Holden L, Golenko X. Motivators, enablers, and barriers to building allied health research capacity. J Multidiscip Healthc. 2012;5(53):53–59. doi: 10.2147/JMDH.S27638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wenke RJ, Mickan S, Bisset L. A cross sectional observational study of research activity of allied health teams: is there a link with self-reported success, motivators and barriers to undertaking research?(Report). BMC Health Serv Res. 2017;17(1). doi: 10.1186/s12913-017-1996-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williams CM, Lazzarini PA. The research capacity and culture of Australian podiatrists. J Foot Ankle Res. 2015;8(1):11. doi: 10.1186/s13047-015-0066-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bilardi D, Rapa E, Bernays S, Lang T. Measuring research capacity development in healthcare workers: a systematic review. BMJ Open. 2021;11(7):e046796–e046796. doi: 10.1136/bmjopen-2020-046796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ahmed R, Farooq A, Storie D, Hartling L, Oswald A. Building capacity for education research among clinical educators in the health professions: a BEME (best evidence medical education) systematic review of the outcomes of interventions: BEME guide no. 34. Med Teach. 2016;38(2):123–136. doi: 10.3109/0142159X.2015.1112893 [DOI] [PubMed] [Google Scholar]
- 21.Friesen EL, Comino EJ, Reath J, et al. Building research capacity in south-west Sydney through a primary and community health research unit. Aust J Prim Health. 2014;20(1):4–8. doi: 10.1071/PY12081 [DOI] [PubMed] [Google Scholar]
- 22.Clinical Services Capability Framework Self-Assessment. Available from: https://www.health.qld.gov.au/_data/assets/pdf_file/0025/634903/cscf-selfassess-sum-metro-north.pdf. Accessed August 21, 2017.
- 23.Matus J, Wenke R, Hughes I, Mickan S. Evaluation of the research capacity and culture of allied health professionals in a large regional public health service. J Multidiscip Healthc. 2019;12:83–96. doi: 10.2147/JMDH.S178696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Williams C, Miyazaki K, Borkowski D, McKinstry C, Cotchet M, Haines T. Research capacity and culture of the Victorian public health allied health workforce is influenced by key research support staff and location. Aust Health Rev. 2015;39(3):303–311. doi: 10.1071/AH14209 [DOI] [PubMed] [Google Scholar]
- 25.Wilkes L, Jackson D. Enabling research cultures in nursing: insights from a multidisciplinary group of experienced researchers. Nurse Res. 2013;20(4):28–34. doi: 10.7748/nr2013.03.20.4.28.e310 [DOI] [PubMed] [Google Scholar]
- 26.Cashin A, Heartfield M, Bryce J, et al. Standards for practice for registered nurses in Australia. Collegian. 2017;24(3):255–266. doi: 10.1016/j.colegn.2016.03.002 [DOI] [Google Scholar]
- 27.Gill SD, Gwini SM, Otmar R, Lane SE, Quirk F, Fuscaldo G. Assessing research capacity in Victoria’s south‐west health service providers. Aust J Rural Health. 2019;27(6):505–513. doi: 10.1111/ajr.12558 [DOI] [PubMed] [Google Scholar]
- 28.Olive P, Maxton F, Bell CA, et al. Clinical academic research internships: what works for nurses and the wider nursing, midwifery and allied health professional workforce. J Clin Nurs. 2020. doi: 10.1111/jocn.15611 [DOI] [PubMed] [Google Scholar]
- 29.Hauck YL, Lewis L, Bayes S, Keyes L. Research capacity building in midwifery: case study of an Australian graduate midwifery research intern programme. Women Birth. 2015;28(3):259–263. doi: 10.1016/j.wombi.2015.02.005 [DOI] [PubMed] [Google Scholar]
- 30.Nightingale J, Fowler-Davis S, Grafton K, et al. The role of allied health professions and nursing research internships in developing a research culture: a mixed-methods exploration of stakeholder perspectives. Health Res Pol Syst. 2020;18(1):1–122. doi: 10.1186/s12961-020-00638-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mickan S, Coates D. Embedded researchers in Australia: survey of profile and experience across medical, nursing and midwifery and allied health disciplines. J Clin Nurs. 2020. doi: 10.1111/jocn.15593 [DOI] [PubMed] [Google Scholar]
- 32.Henshall C, Greenfield DM, Jarman H, Rostron H, Jones H, Barrett S. A nationwide initiative to increase nursing and midwifery research leadership: overview of year one programme development, implementation and evaluation. J Clin Nurs. 2020. doi: 10.1111/jocn.15558 [DOI] [PubMed] [Google Scholar]
- 33.Edelman A, Brown A, Pain T, Larkins S, Harvey G. Evaluating research investment and impact at a regional Australian hospital and health service: a programme theory and conceptual framework. Health Res Policy Syst. 2020;18(1):30. doi: 10.1186/s12961-020-0542-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Coen SE, Bottorff JL, Johnson JL, Ratner PA. A relational conceptual framework for multidisciplinary health research centre infrastructure. Health Res Policy Syst. 2010;8(1):29. doi: 10.1186/1478-4505-8-29 [DOI] [PMC free article] [PubMed] [Google Scholar]