Summary
This report describes a challenging obstetric case in which septic emboli from Streptococcus oralis endocarditis subsequently led to central nervous system infection. There were delays in diagnosis as the patient presented with non‐specific symptoms of fever, diarrhoea and vomiting, initially suspected to be due to viral gastroenteritis and later SARS‐CoV‐2 infection. Antibiotics were commenced once gram positive cocci were isolated from a blood culture. The patient made no significant improvement despite antimicrobial therapy and subsequently developed a worsening headache and delirium. This deterioration was not rapidly recognised despite the use of a routine obstetric early warning score. However, a diagnosis of meningitis was made once the potential severity of the patient’s condition was recognised and Streptococcus oralis was identified in cerebrospinal fluid and blood cultures. Bacterial endocarditis was diagnosed following transthoracic echocardiography. The patient improved with optimised antimicrobial therapy and delivered a healthy baby. This example highlights how non‐specific symptoms can be caused by rare and life‐threatening illnesses, and emphasises that early warning scores might not easily identify neurological deterioration in obstetric patients.
Keywords: endocarditis, meningitis, pregnancy, sepsis
Introduction
Endocarditis is rare in pregnancy with a reported incidence of 1 per 100,000 per year [1]. A systematic review of endocarditis during pregnancy and postpartum found a 10–15% risk of maternal mortality. The review identified intravenous drug use, congenital heart disease and rheumatic heart disease as the three most common risk factors for endocarditis in pregnancy. However, it concluded that maternal risk factors have altered over recent decades due to a reduced prevalence of rheumatic heart disease [2].
Bacterial meningitis is less common in pregnancy than endocarditis and has a higher mortality and morbidity for both mother and fetus. The incidence of bacterial meningitis in the general adult population in the United Kingdom is 1 per 100,000 per year and its incidence in pregnancy is rarer, though difficult to quantify precisely due to its infrequent diagnosis [3]. A literature review of papers written in English, French or German identified 42 instances of bacterial meningitis in pregnancy; Streptococcus pneumoniae was identified as the causative organism in 60% [4]. The average age of patients was 33, all were multigravida and 57% presented in the third trimester. The most common risk factors for bacterial meningitis in pregnancy were otitis and sinusitis, which were seen in 60% of cases. Maternal mortality was 28%, and 37% of cases resulted in loss of the pregnancy.
This report describes the diagnostic challenges encountered in a case in which these two rare pathologies occurred together in pregnancy.
Report
A 33‐year‐old woman presented to hospital with fever, diarrhoea and vomiting 33 weeks into her second pregnancy. The pregnancy was complicated only by obstetric cholestasis, for which the patient was taking ursodeoxycholic acid. Physical examination and blood tests were normal, other than a mildly elevated alkaline phosphatase level. High vaginal swabs and SARS‐CoV‐2 polymerase chain reaction were negative. The patient was diagnosed with viral gastroenteritis and discharged home.
Two days later, the patient re‐presented to hospital with a fever and feeling generally unwell. Her vital signs comprised: blood pressure 125/88 mmHg; heart rate 113 beats.min‐1; temperature 38.9°C; respiratory rate 22 breaths.min‐1; and peripheral oxygen saturations of 99% on room air. An arterial blood gas was normal with a lactate of 1.3 mmol.l‐1. Routine blood tests were normal except for a modest increase in alkaline phosphatase level from 190 to 255 IU.l‐1 and a C‐reactive protein of 74 mg.l‐1. Blood was sent for culture and the patient was admitted with a differential diagnosis of COVID‐19 or viral gastroenteritis. The following day, gram positive cocci were isolated from the blood culture and intravenous vancomycin was commenced. An urgent transthoracic echocardiogram was performed which identified no pathology. Following initial fluid resuscitation, the heart rate reduced to 100 beats.min‐1 and remained static over the next four days. However, the patient made no significant clinical improvement during this time.
A mild headache was reported on day four of admission. The Modified Early Obstetric Warning Score (MEOWS) was 0 as vital signs were within the normal range [5]. The patient had a routine review by an obstetrician and simple analgesia was prescribed. However, six hours later, the patient developed hyperactive delirium and her partner reported that her behaviour was similar to that encountered several years previously during a gastrointestinal infection requiring antibiotics and fluid resuscitation. The MEOWS did not trigger the need for urgent anaesthetic and obstetric reviews for a further four hours at which point the patient’s headache had become severe and her heart rate had increased to 120 beats.min‐1 [5]. On review, the patient was encephalopathic with neck stiffness and photophobia. A clinical diagnosis of central nervous system (CNS) infection was made, empiric ceftriaxone and acyclovir were commenced and vancomycin was continued. A diagnostic lumbar puncture showed purulent cerebrospinal fluid and biochemical analysis confirmed bacterial meningitis. Streptococcus oralis viridians ribonucleic acid was detected in the cerebrospinal fluid and also isolated from two sets of blood cultures taken 12 hours apart.
A multidisciplinary meeting with anaesthetic, obstetric, critical care and microbiology teams was convened. The acuity of the illness, gestational age and absence of fetal compromise were considered; it was decided the patient would be transferred to the high dependency unit on the labour ward. Expedited delivery would only be deemed necessary in the event of a pathological cardiotocograph or patient deterioration. The images obtained on transthoracic echocardiography were re‐examined. An echogenic mass in the aortic root was identified and a diagnosis of endocarditis was made. Magnetic resonance imaging (MRI) of the brain confirmed generalised meningitis with pyogenic ventriculitis of the lateral ventricles (Fig. 1).
Figure 1.
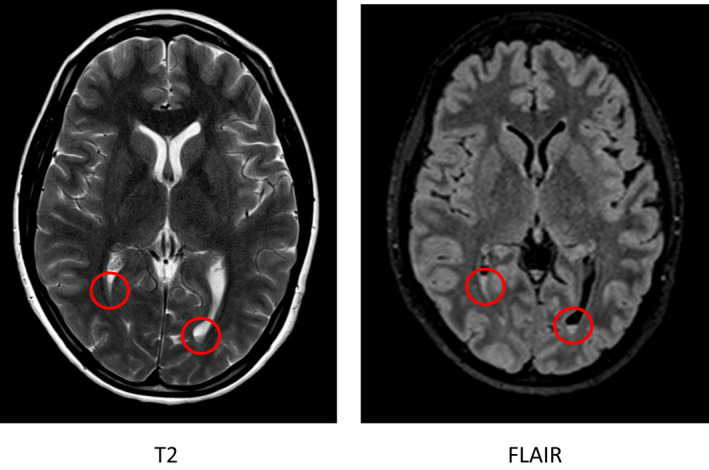
Magnetic resonance images demonstrating dependent fluid levels in the occipital horns of the lateral ventricles (red circles).
Over the next 48 hours, the patient’s delirium improved and their tachycardia and pyrexia resolved. Eight days following their initial presentation, the patient went into spontaneous labour. Patient‐controlled analgesia was provided using fentanyl, and she had an uncomplicated vaginal delivery. Five days post‐delivery, the patient was discharged home with a peripherally inserted central venous catheter and arrangements were made for outpatient antibiotic therapy. Repeat MRI of the brain one month after discharge demonstrated significant improvement, with some residual matter remaining in the left lateral ventricle. Her baby suffered intermediate weight loss and neonatal jaundice but recovered and remains healthy.
Discussion
This clinical episode demonstrates two rare and concurrent complications of pregnancy – infective endocarditis and bacterial meningitis. We believe this is the first example in the literature which describes Streptococcus oralis as the causative microorganism for both processes in the context of pregnancy. Furthermore, the events demonstrate how protocolised care can lead to delayed diagnosis of life‐threatening pathologies. We identified five learning opportunities which we feel could have either reduced time to diagnosis or prevented deterioration:
When the patient re‐presented with deteriorating symptoms and signs of sepsis, a repeat diagnosis of viral infection was made with atypical SARS‐CoV‐2 as the primary diagnosis and viral gastroenteritis as a differential. Bacterial infection was considered, and blood cultures were taken. However, vancomycin was not commenced until organisms were isolated. We believe suspicion of a COVID‐19 illness contributed to the delay in the administration of antibiotics for the management of sepsis. Of note, our tertiary obstetric unit benefits from the presence of obstetric medicine physicians who are present during working hours. The patient was initially reviewed by the physicians, but deteriorated during the weekend. We wonder if the presence of medical diagnosticians on weekdays can paradoxically reduce the willingness of obstetricians and anaesthetists to question working diagnoses and alter medical management plans out of hours.
The transthoracic echocardiogram was initially reported as ‘normal’. This demoted endocarditis as a diagnostic consideration. A repeat echocardiogram may have been warranted within the four day period where a lack of clinical improvement was observed. Furthermore, we suspect that caring for patients with SARS‐CoV‐2 had made clinicians less suspicious of alternative causes of intermittent pyrexia in this case. Two further subtle diagnostic clues to endocarditis were missed despite multidisciplinary input: after the diagnosis, Janeway lesions were identified, and careful questioning revealed a recent visit to a dental hygienist. Clinically, the patient was intermittently pyrexial, had evidence of septic emboli and, upon review of the echocardiogram images, was found to have a left‐sided lesion.
The diagnosis of endocarditis was made after the identification of the central nervous system infection by reconsidering the unifying diagnosis and a repeat review of the echocardiogram. The Modified Duke Criteria for the diagnosis of endocarditis were met in this patient [6]. However, the non‐specific symptoms on initial presentation and the missed lesion on the echocardiogram highlight the difficulty of this diagnosis. We wish to highlight this specific learning point to anaesthetists responsible for obstetric care, given the significant mortality of endocarditis in pregnancy.
Initially, this patient’s symptoms were attributed to COVID‐19. The patient was therefore managed in a side room, geographically distant from the main hub of the labour ward. Overnight, the patient exhibited worsening confusion. This symptom was not identified as requiring escalation by midwifery staff following the MEOWS algorithm. Several hours later, the presence of a headache triggered the MEOWS escalation pathway. This symptom was classified as ‘pain not caused by labour’, prompting escalation. Due to midwives’ familiarity with post‐dural puncture headaches, the anaesthetic team was contacted for clinical review, and identified symptoms and signs of CNS infection.
The only neurological parameter that MEOWS records is the Alert, Voice, Pain and Unconscious (AVPU) scale for assessing conscious level. However, this scale is not equipped to detect abnormalities of cognition. In the context of the infrequent incidence of neurological deterioration on the labour ward, we believe that the absence of this feature caused a significant delay in recognising the importance of this patient’s developing delirium. Based on this example, we wonder if future iterations of the MEOWS score would benefit from including an assessment of cognition, though we recognise that in the obstetric setting this can be challenging to assess, for example during labour. Perhaps more importantly, we believe that multidisciplinary teaching on evolving sepsis in the obstetric setting should emphasise that significant changes in mental status should trigger a prompt review by a senior clinician.
In conclusion, endocarditis, meningitis and ventriculitis are rare in pregnancy and to encounter them in the same presentation is extremely unusual. A crucial learning point is the non‐specific nature of the initial presentation and the difficulty and time taken to arrive at the correct diagnosis. Early recognition of deterioration and prompt multidisciplinary re‐evaluation in the absence of response to treatment can result in excellent outcomes even when the diagnosis is rare and potentially life‐threatening.
Acknowledgements
Published with the written consent of the patient. No external funding or competing interests declared.
References
- 1. Montoya ME, Karnath BM, Ahmad M. Endocarditis during pregnancy. Southern Medical Journal 2003; 96: 1156–7. [DOI] [PubMed] [Google Scholar]
- 2. Kebed KY, Bishu K, Al Adham RI, et al. Pregnancy and postpartum infective endocarditis: a systematic review. Mayo Clinic Proceedings 2014; 89: 1143–52. [DOI] [PubMed] [Google Scholar]
- 3. National Institute for Health and Care Excellence . Meningitis ‐ Bacterial Meningitis and Meningococcal Disease, 2020. www.cks.nice.org.uk/topics/meningitis‐bacterial‐meningitis‐meningococcal‐disease (accessed 23/04/2021).
- 4. Adriani KS, Brouwer MC, van der Ende A, van de Beek D. Bacterial meningitis in pregnancy: report of six cases and review of the literature. Clinical Microbiology and Infection 2012; 18: 345–51. [DOI] [PubMed] [Google Scholar]
- 5. Cole M. A modified early obstetric warning system. Journal of Midwifery 2014; 22: 862. [Google Scholar]
- 6. European Society of Cardiology . IE Summary Card, 2016. www.escardio.org/static‐file/Escardio/Guidelines/Publications/Summary%20card/IE_2016‐_Summary_Card.pdf (accessed 23/04/2021).


