Abstract
Objective:
Insomnia is a significant concern among African-American breast cancer survivors (BCS). Social constraints (SC)- receiving unsupportive or critical responses when expressing trauma-related emotions- and fear of recurrence (FOR) have been associated with insomnia. We examined FOR as a mediator in the relationship between SC and insomnia in African-American BCS. We hypothesized a direct effect of SC on insomnia, and an indirect effect of SC on insomnia through FOR.
Methods:
64 African-American BCS completed a questionnaire assessing demographics, clinical characteristics, SC, FOR, and insomnia. Participants were an average of M= 8.41 (SD= 5.8) year survivors. The mediation was tested using PROCESS for SPSS.
Results:
The direct effect of SC on insomnia was significant (direct effect= .17, SE= .08, p= .04). Also, the indirect effect of SC on insomnia through FOR was significant (indirect effect= .19, SE= .10, 95% CI= .05, .41).
Conclusions:
Experiencing SC from family and friends could produce cognitions that impact sleep for BCS and FOR could be one of those cognitions. Family-based models of care that emphasize the emotional needs of survivors and families could be a relevant strategy to address the SC that impact sleep.
Keywords: Breast Neoplasms, Cancer Survivors, African Americans, Women, Sleep Initiation and Maintenance Disorders
BACKGROUND
Insomnia is a major concern among breast cancer survivors (BCS)1,2. A significant proportion of BCS experience problems with sleep years after diagnosis2,3. Insomnia is defined as feeling dissatisfied with the amount and quality of sleep including experiencing problems falling asleep, maintaining sleep, or having early morning awakenings that cause distress or impaired functioning during the day4,5. Sleep problems are associated with functional impairment, reduced quality of life6, increased mortality risk7 and adverse cardiovascular8 and metabolic consequences9.
Limited data exists on this issue among African-American women, a group known to have high breast cancer (BC) rates10 and a high prevalence of suboptimal sleep10,11. In a study of African-American BCS1, 43% of participants reported clinically significant sleep disturbances1. The prevalent symptoms of insomnia were: difficulty maintaining sleep, dissatisfaction with sleep, difficulty falling asleep, and early morning awakenings1. While Taylor et al (2012) examined insomnia in African-American BCS, most studies have focused primarily on Caucasian BCS.
Several factors contribute to insomnia in BCS including demographic (e.g. older age) and psychological factors (e.g. higher anxiety, more intrusive thoughts about cancer)1,12. Social factors (e.g. inner-city residence, low emotional/social support, care-giving to family/friends) are associated with sleep among older African-Americans11. Few studies, however, have examined how social factors influence sleep in BCS.
While limited, data show16–18 that social constraints (SC) are associated with insomnia in cancer survivors. SC are situations in which trauma survivors feel hindered in their attempts to express trauma-related emotions by people close to them (e.g. family and friends responding in negative ways when the survivor attempts to share emotions related to the traumatic event, or making the survivor feel misunderstood or alienated)19. Some data suggests that BC diagnosis and treatment are considered traumatic experiences36. According to the Social Cognitive Processing Theory of Emotional Adjustment to Cancer, BCS who are unable to express trauma-related emotions with important individuals have difficultly experiencing the psychological benefits of discussing the emotions (e.g. healthy cognitive processing, healthy psychological adaptation to the trauma, and better psychological outcomes)19.
Delays in healthy psychological adaptation to a traumatic event can create lingering and elevated psychological distress19 that can deleteriously impact physiological functioning such as sleep1. Of the few studies16–18 that have explored how SC impacts insomnia in BCS, one study- in Chinese American BCS- reported that SC from a spouse was associated with poorer sleep quality18. Additional studies conducted in cancer survivors (various cancer sites) reported that SC from individuals in one’s social network, romantic partners, and healthcare providers was associated with fatigue and sleep disturbance16,17. Minimal work has examined how SC affects African-Americans’ management of cancer20. The current study is the first to examine the role of SC on insomnia in African-American BCS.
Understanding what mediates the relationship between SC and insomnia is equally important. Previous studies have identified certain mediators (e.g. self-efficacy, avoidant coping, and perceived stress) linking SC with insomnia16–18. Fear of recurrence (FOR) is a commonly reported BC symptom, a noted consequence of SC, and a precursor of insomnia- making it another potential mediator16–18,21,22. FOR is defined as having unrelenting thoughts of a cancer recurrence in the same organ or different part of the body23. A previous study reported low/moderate levels of FOR in African-American BCS24.
According to Leventhal’s Common-Sense Self-Regulation Model of Illness21,25, external cues from the social environment serve as antecedents of FOR. One source of these cues is socially constrained environments partly composed of family members whose avoidance of health-related discussions with the cancer survivor21 may trigger FOR. As previously mentioned, if a BCS is unable to express trauma-related emotions with important close individuals, it could result in lingering elevated distress (e.g. FOR)19. In fact, a study found that SC from the spouses of BCS was associated with increased FOR22.
FOR is also a likely mechanism linking SC to insomnia because there is evidence pointing to FOR as a precursor of insomnia26,27. Harvey’s Cognitive Model of the Maintenance of Insomnia 26 suggests that individuals with insomnia have excessive negatively toned thoughts throughout the day including worrying about the future27. Thus, FOR might be a commonly experienced source of negatively toned thoughts for BCS with insomnia. This reasoning is supported by studies that have reported positive relationships between FOR and insomnia in the cancer population28,29. The relationship between FOR and insomnia requires further investigation in African-American BCS. Because African-American BCS experience poorer sleep quality than the general population10,11 and report moderate levels of FOR, building our understanding of the potential role of FOR in insomnia among African-American BCS is important.
Leventhal’s Common-Sense Model of Self-Regulation supports SC as an antecedent of FOR while Harvey’s Model of the Maintenance of Insomnia supports insomnia as a consequence of FOR. No study, to our knowledge, has examined FOR as a mediator in the relationship between SC and insomnia. Examining this association among African-American BCS is especially important since this group demonstrates sub-optimal sleep patterns10,11 and moderate FOR 24. The current study examined the direct effect of SC on insomnia and the indirect effect of SC on insomnia through FOR in African-American BCS. We hypothesized that higher SC would be associated with greater insomnia and that FOR would mediate the relationship.
METHODS
Participants
64 African-Americans were extracted from a larger community sample of BCS. Participant eligibility requirements included: self-identified as female with a history of BC (no other cancer site), free from recurrence, completed all BC treatment (except hormonal therapy), and no history of bipolar disorder, schizoaffective disorder, or schizophrenia.
Recruitment
Participants were recruited from hospitals, community centers, non-profit organizations, and BCS support groups in the greater Washington, DC area from July 2017 to July 2018. The study was advertised by distributing a flyer onsite and through the social media pages and listservs of the recruitment partners. Participation was open to BCS of all races.
Procedures
Study approval was obtained from the Howard University Institutional Review Board (IRB-17-CAS-27). Participants completed a 30-minute survey assessing study variables with the option to anonymously complete the questionnaire online, by mail, or in-person (no participants selected this option). Offering multiple forms of questionnaire administration provided more convenience to participants. All participants were provided a preamble describing the study requirements and participant rights. Signed informed consent was obtained.
Instruments
Background Questionnaire:
Demographic and clinical variables were assessed in a background questionnaire including: age, education, household income, marital status, time since diagnosis (years), stage at diagnosis, surgery type (lumpectomy or mastectomy), treatment type (chemotherapy, no chemotherapy), and menopausal status (pre-menopause, peri-menopause, and post-menopause).
Social Constraints:
The SC Scale (SCS) is a 15-item measure of an individual’s perception of hampered attempts to disclose emotions related to an experienced traumatic event19. SC were examined using the Family and Friends domain of the SCS (e.g. “How often do you feel as though you had to keep your feelings about [breast cancer] to yourself because they made your [family and friends] feel uncomfortable?”). Responses are recorded on a four-point scale (1- “never” to 4- “often”). A total score on the SCS is computed by summing the 15 responses (possible score range: 15 – 60) - higher scores indicate greater SC. Adequate internal consistency for the SCS was reported in 210 BCS (α= .95)30. The SCS demonstrated internal consistency in the present sample (α= .94). To our knowledge, this is the first study to use the full SCS among African-American BCS.
Fear of Recurrence:
The Concerns About Recurrence Scale- Overall Concerns Index (CARS-OC) measures the frequency and intensity of BCS’s worries about having a cancer recurrence and the potential for the worries to be upsetting. CARS-OC has four items (e.g. “How afraid are you that your breast cancer could recur?”) measured on a six-point scale (1- lowest level of worry to 6- highest level of worry)24. Items are summed to produce an average score for overall FOR24. CARS-OC demonstrated internal consistency (α= .87) and concurrent validity when compared to related constructs (e.g. intrusive thoughts and avoidance subscales of the Impact of Events Scale, and the Distress and Well-being subscales of the Mental Health Inventory) in a primarily Caucasian sample of BCS24 and internal consistency in African-American BCS25. In the present study, the internal consistency of CARS-OC was adequate (α= .94).
Insomnia:
The Insomnia Severity Index (ISI) is a seven-item measure evaluating the perceived severity of clinically significant insomnia symptoms experienced within the past two weeks (e.g. “Please rate the severity of your insomnia problems (last 2 weeks): 1) Difficulty falling asleep”)31. Items are scored on a 5-point scale (0 = “not at all” to 4 = “very much”). Total scores are obtained by summing the items (possible score range: 0 – 28). For an oncology sample, scores ≥8 indicate clinically significant sleep difficulties associated with insomnia32. The ISI demonstrated internal consistency (α= .74) and concurrent validity when compared to sleep diaries in a general clinical setting31 and demonstrated internal consistency in an African-American BCS sample (α= .90)1. The internal consistency of the ISI for the current study was adequate, (α= .92).
Data Analysis
Analyses were performed using Version 24.0 of SPSS. Descriptive statistics were used to describe sample characteristics and main study measures (Table 1). Total scores were computed for the SCS and the ISI, and an average score was computed for the CARS-OC. If participants inadvertently skipped items, study team members requested that participants complete the missing data if willing. To examine the indirect relationship between SC and insomnia through FOR, a simple mediation model was employed using Model 4 in Version 3.0 of the PROCESS macro for SPSS34, 35. The PROCESS macro calculates the following four effects: i) the effect that SC (X) has on FOR (M) (a pathway), ii) the effect that FOR has on insomnia (Y) (b pathway), iii) the direct effect that SC has on insomnia (c’), the indirect effect that SC has on insomnia through FOR (ab), and the total effect of SC on insomnia (c)34. A 95% bias-corrected bootstrap confidence interval was computed for the indirect effect of SC on insomnia through FOR34. A power analysis determined that a minimum of 55 participants was needed to obtain high power (α= .80) and effect sizes of .15 with α= .05.
Table 1.
Participant Characteristics (N= 64)
| Characteristic | n % | M (SD) |
|---|---|---|
|
| ||
| Age (years) (range= 22– 75) | 57.8 (10.5) | |
|
| ||
| Age (years) | ||
| - Under 34 | 2 (3.1%) | |
| - 35– 49 | 9 (14.1%) | |
| - 50– 64 | 33 (51.6%) | |
| - 65 and above | 20 (31.3%) | |
|
| ||
| Marital Status | ||
| - Married/Partner | 31 (48.4%) | |
| - Single/Divorced/Separated/Widowed | 33 (51.6%) | |
|
| ||
| Education | ||
| - At least a High School Diploma | 9 (14.1%) | |
| - Vocational Training/ Some College | 30 (46.9%) | |
| - College | 9 (14.1%) | |
| - Some Professional School After College | 2 (3.1%) | |
| - Professional Degree | 14 (21.9%) | |
|
| ||
| Annual Household Income | ||
| - < $50,000 | 19 (29.7%) | |
| - $50,000– $99,999 | 21 (32.8%) | |
| - $100,000– $149,999 | 9 (14.1%) | |
| - > $150,000 | 8 (12.5%) | |
| - Refused/Don’t know | 7 (10.9%) | |
|
| ||
| Cancer Stage | ||
| - Stage 1 | 33 (51.6%) | |
| - Stage 2 | 18 (28.1%) | |
| - Stage 3 | 12 (18.8%) | |
| - Stage 4 | 1 (1.6%) | |
|
| ||
| Surgery Type | ||
| - Lumpectomy | 31 (48.4%) | |
| - Mastectomy | 33 (51.6%) | |
|
| ||
| Time Since Diagnosis (years) (range: 0.25– 25) | 8.41 (5.8) | |
|
| ||
| Treatment Type | ||
| - Chemotherapy | 38 (59.4%) | |
| - No chemotherapy | 26 (40.6%) | |
|
| ||
| Menopausal Status | ||
| - Pre-menopause | 5 (7.8%) | |
| - Peri-menopause | 11 (17.2%) | |
| - Post-menopause | 48 (75.0%) | |
Descriptive statistics of sample characteristics.
RESULTS
Participant Characteristics
168 individuals were screened for eligibility. Of the individuals screened, 29 were ineligible (still in active treatment (n= 3), history of recurrence and/or other cancer (n= 25), severe psychological disorder (n= 1)). Of the remaining 139 eligible individuals, 41 declined to participate and 96 completed the study requirements: African-American (n= 64), Caucasian (n= 27), Hispanic (n= 3), and Asian/Pacific Islander (n= 2).
Demographic and clinical characteristics for African-American participants are summarized in Table 1. The average age was M= 57.8 years (SD= 10.5; range= 22–75). Thirty-one participants were married or with a partner (48.4%), 9 (14.1%) had at least a high school diploma, and 38 (59.4%) earned at least $50k annually.
Most of the sample presented with stage 1 (51.6%) or stage 2 (28.1%). Thirty-one participants (48.4%) reported receiving a lumpectomy and 33 (51.6%) a mastectomy. Participants were M= 8.41 (SD= 5.8) years past receiving a BC diagnosis. Five participants (7.8%) were pre-menopausal, 11 (17.2%) were peri-menopausal, and 48 (75%) were postmenopausal. Thirty-eight participants (59.4%) received chemotherapy while 26 (40.6%) did not.
Descriptive Statistics for Main Study Measures
Descriptive statistics for the main study measures (SC, FOR, and insomnia) were also calculated. The mean total score on the SCS was M= 24.2 (SD= 11.4) (range 15 – 60). The average score on the CARS-OC was M= 2.6 (SD= 1.6) (range 1 – 6) and 60.9% of the sample reported FOR ≥ 2 on the CARS-OC. The mean ISI score was M= 9.8 (SD= 7.6) (range 0 – 28) and 57.8% of participants experienced clinically significant insomnia (ISI scores ≥8). The most prevalent sleep concerns were: sleep dissatisfaction (60.9%), difficulty staying asleep (50%), problems waking up too early (42.2%), and difficulty falling asleep (40.6%).
Mediation of FOR Between SC and Insomnia
Demographic and treatment-related characteristics previously related to insomnia were tested as covariates: age, income, marital status, education, surgery type, menopausal status, treatment type, stage at diagnosis, and time since diagnosis 1,5,17,18,33. Although none of the tested variables were associated with insomnia (p> 0.05), age was selected as a covariate because it is most frequently predictive of insomnia in the literature 1,5,17,18,33.
Figure 1 presents the results of the mediation analysis. We examined FOR (M) as a mediator between SC (X) and insomnia (Y) controlling for age. The model explained 34.14% of the variance in insomnia (p< .001). The direct effect of SC on insomnia (direct effect= .17, SE= .08, p= .04, 95% CI: .01, .33), the effect of SC on FOR (effect= .07, SE= .02, p<.001, 95% CI: .04, .10), and the effect of FOR on insomnia (effect= 1.94, SE= .60, p= .002, 95% CI: .74, 3.14) were significant. The indirect effect indicated that FOR mediated the relationship between SC and insomnia (completely standardized indirect effect= .19, SE= .10, 95% CI: .05, .41).
Figure 1.
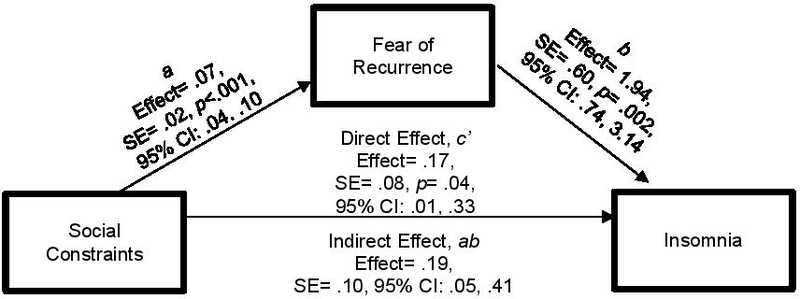
The Indirect Effect of Social Constraints on Insomnia Through Fear of Recurrence
FOR (M) as a mediator between SC (X) and insomnia (Y) controlling for age.
DISCUSSION
We examined the link between SC and insomnia and examined FOR as a mediator among African-American BCS. Over half the sample reported clinically significant insomnia. SC were positively associated with insomnia and FOR mediated the relationship. The following discussion outlines ways in which our results align with previous studies.
Insomnia
In our sample, 57.8% of participants had clinically significant insomnia (ISI scores ≥ 8) - slightly higher than the prevalence of insomnia reported in a previous, similarly sized sample (N= 51) of African-American BCS (43.12%)1. This highlights that insomnia continues to be a problem among African-American BCS.
The most prevalent sleep complaints in the present sample included: sleep dissatisfaction (60.9%), difficulty staying asleep (50%), early morning awakenings (42.2%), and difficulty falling asleep (40.6%). These were also the top four concerns in a previous study of African-American BCS1. These sleep problems have emerged as the most prevalent complaints across two samples of African-American BCS which underscores the need for effective supportive care to address insomnia in this population.
Social Constraints
Regarding the presence of SC, this sample reported low/moderate SC indicating that, to a moderate extent, family and friends may hinder attempts to disclose cancer-related emotions (M= 24.2, SD= 11.4, range 15 to 60). A previous study of BCS reported a mean of M= 26.6 (SD= 11) for SCS scores36. Few studies have examined SC in African-American BCS20. Our data adds to the growing body of literature on SC in cancer survivors showing that SC is a phenomenon that is also experienced among African-American BCS.
Fear of Recurrence
The present sample reported low/moderate CARS-OC scores (M= 2.6, SD= 1.6, range 1 – 6). This was similar to the average CARS-OC score in a previous sample of African-American BCS (M= 2.65, SD= 1.44)24, and a primarily Caucasian sample of BCS (M= 2.91, SD= 1.29)23. The combined findings from these studies show that FOR is a persistent issue among BCS. Furthermore, Taylor et al.’s (2012) study of FOR in African-American BCS reported that participants reporting low/moderate FOR showed increased psychological distress and decreased quality of life24. Thus, implications for the current study suggest that even low to moderate levels of FOR warrant assessment and support during follow-up clinical care.
Social Constraints and Insomnia
The direct effect of SC on insomnia was significant – the more a participant perceived that family and friends hindered attempts to express cancer-related emotions, the greater symptoms of insomnia. This was consistent with the results of previous studies reporting a positive relationship between SC and insomnia16–18.
Fear of Recurrence as a Mediator Between Social Constraints and Insomnia
As expected, FOR served as a mediator in the relationship between SC and insomnia. Based on the present results and Leventhal’s Common-Sense Self-Regulation Model of Illness21,25, family members who avoid health-related discussions with the survivor may trigger FOR. When BCS are not given the opportunity to express their cancer-related emotions, they are left to deal with ruminating thoughts without receiving objective or reassuring feedback from others, which can create anxiety, stress, worry, and FOR 19,21. According to Harvey’s Cognitive Model of the Maintenance of Insomnia, these psychological consequences impact sleep26,27. The present findings extend the Taylor et al (2012) study by showing that SC and FOR contribute to insomnia in African-American BCS. It is also notable that SC remained significantly associated with insomnia after considering age and FOR. Sleep is largely influenced by the external social environment (e.g. sleep patterns of family members, technology screen-time, relationships with family members). These findings support that unpleasant social interactions with family could add more complexity in understanding sleep experiences for African-American BCS.
We examined the effects that SC from family and friends had on FOR and insomnia. Our sample did not report high levels of SC from family and friends. The experience of SC from family and friends in this sample was relatively infrequent, but impactful when it occurred. A future study might examine SC from a spouse or partner, which has previously been associated with both FOR and insomnia 16,18,22. Also, examining African-centered communication styles that facilitate well-being among African-Americans, and examining SC from the broader social environment (e.g. healthcare providers) could be useful in understanding the many layers of SC experienced by African-American BCS. African-Americans often experience discrimination from the healthcare system39. Discriminatory social interactions with healthcare providers could make African-Americans feel constrained in discussing their experiences and feel that they must deal with emotional trauma from BC in isolation39. These experiences could have an impact on their sleep, as one study reported that SC from healthcare providers was associated with fatigue and sleep disturbances in BCS16. More research is needed to identify protective factors that could improve sleep among this population. Also, a future study could examine whether the SC expressed in African-Americans are different from other ethnic groups.
It would be worthwhile to explore these relationships in other socio-demographic groups, survivors of other cancer sites, and various genders. For example, BCS who are sexual and gender minorities (e.g. lesbian, gay, bisexual, same-gender loving, transgender, queer, questioning, genderqueer, and other sexual/gender minorities who eschew labelling) face unique social struggles including lack of support from BCS organizations and clinicians36, a higher prevalence of post-cancer relationship difficulties, fatigue, and energy problems37. These social issues make psychological adjustment to cancer survivorship and possibly SC particularly challenging for this group.
Study Limitations
Although this study makes a meaningful contribution, it has its limitations. First, this cross-sectional data does not allow temporal relationships between study variables to be examined. Secondly, we only used the CARS-OC to assess FOR. A future study should incorporate all CARS subscales23. Thirdly, although a power analysis supports the sufficiency of this sample size, the sample is smaller than other similar studies. Finally, this sample was highly educated, thus the results might not be reflective of the experiences of a broad range of BCS. The recruitment method is open to bias and representativeness is not guaranteed. There was no attempt to provide comparisons on the ISI in relation to a non-cancer age-matched control group.
Clinical Implications
Our results support the importance of preparing survivors and families for the emotional burden that accompanies survivorship. A family-based model of care focused on building survivors’ and families’ capacity to manage emotional needs after cancer is a relevant strategy to improve psychological and functional adjustment to survivorship38. Interventions might target family members interested in learning how to engage in empathic communication with relatives with a history of BC. Also, cognitive-behavioural therapy is effective in reducing insomnia in the cancer population and in ethnic minorities. Mindfulness-based interventions and relaxation training improves overall psychological adjustment to cancer survivorship and is relevant for African-Americans.
Conclusions
Mediators linking SC to insomnia in cancer survivors have been identified previously (self-efficacy, avoidant coping, perceived stress)16–18. We have expanded the literature by highlighting FOR as a cognitive mediator linking SC to insomnia. We also extend the generalizability of prior studies by showing that SC is linked to insomnia in African-American BCS - a group with prevalent sleep problems1.
Table 2.
Intercorrelations Between Major Study Variables
| Social Constraints | Fear of Recurrence | Insomnia | |
|---|---|---|---|
| Social Constraints | - | .51*** | .46*** |
| Fear of Recurrence | - | - | .54*** |
Pearson’s r Correlations
p<.05
p<.01
p<.001.
Acknowledgements
The Thelma D. Jones Breast Cancer Fund, Howard University Frederick Douglass Doctoral Scholars Fellowship, Health Careers Opportunity Program (HCOP Grant # D18HP29035), and NCI (P.I.: Jamie Ostroff; CA009461; R01 CA207442-03S1; P.I.: Craig Thompson; P30CA008748) supported manuscript preparation.
Footnotes
Conflicts of Interest
The authors have no conflicts of interest.
Data Availability Statement
Research data are not shared.
References
- 1.Taylor TR, Huntley ED, Makambi K, et al. Understanding sleep disturbances in African-American breast cancer survivors: A pilot study. Psychooncology. 2012. doi: 10.1002/pon.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lindley C, Vasa S, Sawyer WT, Winer EP. Quality of life and preferences for treatment following systemic adjuvant therapy for early-stage breast cancer. J Clin Oncol. 1998. doi: 10.1200/JCO.1998.16.4.1380 [DOI] [PubMed] [Google Scholar]
- 3.Couzi RJ, Helzlsouer KJ, Fetting JH. Prevalence of menopausal symptoms among women with a history of breast cancer and attitudes toward estrogen replacement therapy. J Clin Oncol. 1995. doi: 10.1200/JCO.1995.13.11.2737 [DOI] [PubMed] [Google Scholar]
- 4.Association AP. Diagnostic an Statistical Manual of Mental Disorders; 2016. doi: 10.1176/appi.books.9780890425596.744053 [DOI]
- 5.S.N. G, J.A. J, J. S, P. G, M. P, L. C Sleeping well with cancer: A systematic review of cognitive behavioral therapy for insomnia in cancer patients. Neuropsychiatr Dis Treat. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Simon GE, Vonkorff M. Prevalence, burden, and treatment of insomnia in primary care. Am J Psychiatry. 1997. doi: 10.1176/ajp.154.10.1417 [DOI] [PubMed] [Google Scholar]
- 7.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002. doi: 10.1001/archpsyc.59.2.131 [DOI] [PubMed] [Google Scholar]
- 8.Chien KL, Chen PC, Hsu HC, et al. Habitual sleep duration and insomnia and the risk of cardiovascular events and all-cause death: Report from a community-based cohort. Sleep. 2010. doi: 10.1093/sleep/33.2.177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patel SR, Malhotra A, White DP, Gottlieb DJ, Hu FB. Association between reduced sleep and weight gain in women. Am J Epidemiol. 2006. doi: 10.1093/aje/kwj280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.American Cancer Society. Cancer Facts & Figures 2016, Atlanta: American Cancer Society; 2016. Cancer Facts & Figures 2016. Atlanta. [Google Scholar]
- 11.Williams NJ, Grandner MA, Wallace DM, Cuffee Y, Airhihenbuwa C, Okuyemi K, … & Jean-Louis G (2016). Social and behavioral predictors of insufficient sleep among African Americans and Caucasians. Sleep medicine, 18, 103–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morin CM, Ware JC. Sleep and psychopathology. Appl Prev Psychol. 1996. doi: 10.1016/S0962-1849(96)80013-8 [DOI] [Google Scholar]
- 13.Ford DE, Kamerow DB. Epidemiologic Study of Sleep Disturbances and Psychiatric Disorders: An Opportunity for Prevention? JAMA J Am Med Assoc. 1989. doi: 10.1001/jama.1989.03430110069030 [DOI] [PubMed] [Google Scholar]
- 14.Mellinger GD, Balter MB, Uhlenhuth EH. Insomnia and Its Treatment: Prevalence and Correlates. Arch Gen Psychiatry. 1985. doi: 10.1001/archpsyc.1985.01790260019002 [DOI] [PubMed] [Google Scholar]
- 15.Ohayon MM, Caulet M, Priest RG, Guilleminault C. DSM-IV and ICSD-90 insomnia symptoms and sleep dissatisfaction. Br J Psychiatry. 1997. doi: 10.1192/bjp.171.4.382 [DOI] [PubMed] [Google Scholar]
- 16.Adams RN, Mosher CE, Cohee AA, et al. Avoidant coping and self-efficacy mediate relationships between perceived social constraints and symptoms among long-term breast cancer survivors. Psychooncology. 2017. doi: 10.1002/pon.4119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adams RN, Mosher CE, Winger JG, Abonour R, Kroenke K. Cancer-related loneliness mediates the relationships between social constraints and symptoms among cancer patients. J Behav Med. 2018. doi: 10.1007/s10865-017-9892-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yeung NCY, Ramirez J, Lu Q. Perceived stress as a mediator between social constraints and sleep quality among Chinese American breast cancer survivors. Support Care Cancer. 2017. doi: 10.1007/s00520-017-3632-9 [DOI] [PubMed] [Google Scholar]
- 19.Lepore SJ, Revenson TA. Social Constraints on Disclosure and Adjustment to Cancer. Soc Personal Psychol Compass. 2007. doi: 10.1111/j.1751-9004.2007.00013.x [DOI] [Google Scholar]
- 20.Halbert CH, Wrenn G, Weathers B, Delmoor E, Ten Have T, Coyne JC. Sociocultural determinants of men’s reactions to prostate cancer diagnosis. Psychooncology. 2010. doi: 10.1002/pon.1574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee-Jones C, Humphris G, Dixon R, Hatcher MB. Fear of cancer recurrence - A literature review and proposed cognitive formulation to explain exacerbation of recurrence fears. Psychooncology. 1997. doi: [DOI] [PubMed] [Google Scholar]
- 22.Cohee AA, Adams RN, Johns SA, et al. Long-term fear of recurrence in young breast cancer survivors and partners. Psychooncology. 2017. doi: 10.1002/pon.4008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vickberg SMJ. The concerns about recurrence scale (CARS): A systematic measure of women’s fears about the possibility of breast cancer recurrence. Ann Behav Med. 2003. doi: 10.1207/S15324796ABM2501_03 [DOI] [PubMed] [Google Scholar]
- 24.Taylor TR, Huntley ED, Sween J, et al. An exploratory analysis of fear of recurrence among African-American breast cancer survivors. Int J Behav Med. 2012. doi: 10.1007/s12529-011-9183-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Leventhal H, Diefenbach M, Leventhal EA. Illness cognition: Using common sense to understand treatment adherence and affect cognition interactions. Cognit Ther Res. 1992. doi: 10.1007/BF01173486 [DOI] [Google Scholar]
- 26.Harvey AG. A cognitive model of insomnia. Behav Res Ther. 2002. doi: 10.1016/S0005-7967(01)00061-4 [DOI] [PubMed] [Google Scholar]
- 27.Hiller RM, Johnston A, Dohnt H, Lovato N, Gradisar M. Assessing cognitive processes related to insomnia: A review and measurement guide for Harvey’s cognitive model for the maintenance of insomnia. Sleep Med Rev. 2015. doi: 10.1016/j.smrv.2014.11.006 [DOI] [PubMed] [Google Scholar]
- 28.J.M. P, R. J, J. R, et al. Prevalence and predicators of insomnia among cancer survivors. J Clin Oncol. 2017. [Google Scholar]
- 29.Berrett-Abebe J, Cadet T, Pirl W, Lennes I. Exploring the relationship between fear of cancer recurrence and sleep quality in cancer survivors. J Psychosoc Oncol. 2015. doi: 10.1080/07347332.2015.1020586 [DOI] [PubMed] [Google Scholar]
- 30.Schmidt JE, Andrykowski MA. The Role of Social and Dispositional Variables Associated With Emotional Processing in Adjustment to Breast Cancer : An Internet-Based Study. 2004;23(3):259–266. doi: 10.1037/0278-6133.23.3.259 [DOI] [PubMed] [Google Scholar]
- 31.Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001. doi: 10.1016/S1389-9457(00)00065-4 [DOI] [PubMed] [Google Scholar]
- 32.Savard MH, Savard J, Simard S, Ivers H. Empirical validation of the insomnia severity index in cancer patients. Psychooncology. 2005. doi: 10.1002/pon.860 [DOI] [PubMed] [Google Scholar]
- 33.Vargas S, Wohlgemuth WK, Antoni MH, Lechner SC, Holley HA, Carver CS. Sleep dysfunction and psychosocial adaptation among women undergoing treatment for non-metastatic breast cancer. Psychooncology. 2010. doi: 10.1002/pon.1603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford Publications; 2017. [Google Scholar]
- 35.Williamson TJ, Ostroff JS, Haque N, Martin CM, Hamann HA, Banerjee SC, & Shen MJ (2020). Dispositional Shame and Guilt as Predictors of Depressive Symptoms and Anxiety Among Adults With Lung Cancer: The Mediational Role of Internalized Stigma. Stigma and Health. Advance online publication. 10.1037/sah0000214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cordova MJ, Cunningham LLC, Carlson CR, Andrykowski MA. Social constraints, cognitive processing, and adjustment to breast cancer. J Consult Clin Psychol. 2001. doi: 10.1037/0022-006X.69.4.706 [DOI] [PubMed] [Google Scholar]
- 37.Brown MT, McElroy JA. Unmet support needs of sexual and gender minority breast cancer survivors. Support Care Cancer. 2018. doi: 10.1007/s00520-017-3941-z [DOI] [PubMed] [Google Scholar]
- 38.Kamen C, Mustian KM, Dozier A, Bowen DJ, Li Y. Disparities in psychological distress impacting lesbian, gay, bisexual and transgender cancer survivors. Psychooncology. 2015. doi: 10.1002/pon.3746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cuevas AG, O’Brien K, & Saha S (2016). African American experiences in healthcare:“I always feel like I’m getting skipped over”. Health Psychology, 35(9), 987. [DOI] [PubMed] [Google Scholar]
- 40.Ryan P, Sawin KJ. The Individual and Family Self-Management Theory: Background and perspectives on context, process, and outcomes. Nurs Outlook 2009. doi: 10.1016/j.outlook.2008.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.[dataset] Martin CM, Greene D, Taylor TR; 2018; Breast Cancer Survivor Study; Data repository: Statistical Package for Social Sciences
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Research data are not shared.


