Abstract
Purpose
To describe patient-reported outcomes following simple elbow dislocation and to identify the baseline factors that predict outcomes.
Methods
Adult patients treated with a closed reduction for a simple elbow dislocation with or without minor fracture (coronoid avulsion, radial head fracture, or epicondyle avulsion) from 2000 to 2018 completed outcome instruments including Disabilities of the Arm, Shoulder and Hand (QuickDASH) via Research Electronic Data Capture. Descriptive statistics were calculated. Univariate followed by multivariate Tobit regression models were used to determine factors associated with clinical outcomes on QuickDASH. Social deprivation was measured using the Area Deprivation Index. Patients with additional upper-extremity injuries or associated major fractures (Monteggia or terrible triad injuries, distal humerus fractures, etc) were excluded.
Results
At a mean follow-up of 67.5 months, 95% (38/40) of patients reported satisfaction with treatment, and clinical outcomes were good (QuickDASH 9.0 ± 14.8). Univariate analysis showed that higher Area Deprivation Index, older age, female sex, high-energy mechanism of injury, and worker’s compensation (WC) or Medicare insurance status (vs commercial) was associated with significantly worse QuickDASH scores at follow-up. Early therapy, dominant elbow involvement, presence of minor fractures (minimally displaced radial head, coronoid tip, or epicondylar avulsion fractures), race, and treating service did not influence outcomes in univariate analyses. Multivariate analysis demonstrated a significant association between increased social deprivation, WC insurance, and Medicare insurance and worse QuickDASH scores while controlling for new upper-extremity injury, age, sex, and mechanism of injury.
Conclusions
Outcomes and treatment satisfaction following simple elbow dislocation are generally good but are significantly worse for the patients with greater levels of social deprivation and WC or Medicare insurance. Although surgeons should be aware of the possibility that specific subsets of patients may benefit from early therapy, this factor did not appear to influence long-term outcomes in this small cohort.
Type of study/level of evidence
Prognostic III.
Key words: Elbow dislocation, QuickDASH, Range of motion, Social deprivation, Therapy
Elbow dislocations are common injuries, with an estimated incidence of 5.2–6.1 per 100,000 person-years.1, 2, 3 Patient-reported outcomes (PROs) following the dislocation of the elbow with or without associated fractures are frequently quite good, as demonstrated by multiple studies.4, 5, 6, 7 However, this type of injury is not benign as subsets of patients experience a poor functional outcome and many have elbow stiffness even in long-term follow-up.4 Although multiple studies have used PRO instruments to evaluate elbow dislocation outcomes, including the abbreviated version of the Disabilities of the Arm, Shoulder and Hand (QuickDASH), it remains unclear whether specific patient or injury factors are associated with predicting a poor versus good functional outcome for this type of injury.4, 5, 6, 7, 8, 9, 10 Clinically, such information would be helpful to identify which patients may be at risk of a poor outcome at the onset of treatment.
The biopsychosocial model, which captures the interplay between patients’ perceived disability or function and psychological factors such as pain interference, coping skills, resiliency, depression, and social deprivation, is well-established for a wide array of upper-extremity conditions.11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21 Social deprivation is a surrogate for these biopsychosocial factors, in which greater social deprivation has been associated with greater patient-reported disability, anxiety, pain interference, and depression among orthopedic patients, including those recovering from upper-extremity fracture.22, 23, 24, 25, 26, 27 Additionally, biopsychosocial factors have been associated with worse PROs in the early recovery period following distal radius fracture, thumb carpometacarpal arthroplasty, and a variety of elective upper-extremity surgeries.21,28,29 Although possibly related to outcomes, these factors have not been studied in the context of elbow dislocation.
The primary purpose of this study was to describe outcomes following closed reduction of simple elbow dislocations and to compare those outcomes between patients who did and did not have early hand therapy. The QuickDASH was used as the primary measure of upper-extremity function, and biopsychosocial factors were measured using the 2015 Area Deprivation Index (ADI) as an indicator of social deprivation and the Brief Resiliency Scale (BRS).22,30 The secondary purpose was to evaluate whether patient- or injury-specific variables, including social deprivation, were associated with the QuickDASH outcome at final follow-up. We hypothesized that there would be little difference between those who did and did not have early hand therapy and that the outcomes would generally be good, although influenced by injury and patient variables.
Materials and Methods
This retrospective study was approved by the institution institutional review board of University of Utah. Patients treated with closed reduction of simple posterolateral elbow dislocations at a single tertiary level 1 academic institution were retrospectively identified electronically by Current Procedural Terminology codes (24600, 24605). Patients with simple dislocation and those with a dislocation accompanied by minor fracture (type I coronoid avulsion, nondisplaced or minimally displaced radial head fracture, or epicondyle avulsion) were included. Patients with a dislocation and a major fracture (ie, terrible triad or Monteggia injuries, olecranon/ulna fracture, operative radial head/neck fracture, or distal humerus fracture) and those aged <18 years at the time of injury were excluded. Patients who sustained an additional ipsilateral or contralateral upper-extremity injury at the time of their dislocation and those who did not speak English were also excluded. One author (A.V.) reviewed the injury radiographs while they were blinded to the treatment received and outcomes.
All elbow dislocations were reduced in the emergency department with conscious sedation, and then they were immobilized in a posterior slab orthosis. Postreduction radiographs were obtained to verify the adequate reduction. Reduction was performed by an orthopedic consultant or resident. All patients were immobilized following reduction. Postreduction radiographs were reviewed by A.S.vdH. to verify the concentric reduction. The patients were seen in the clinic approximately 2 weeks after the injury by an orthopedic hand surgeon, shoulder and elbow surgeon, or trauma surgeon or by a nonsurgical sports medicine physician. At this visit, immobilization was discontinued, and the treating physician determined whether or not the patient was referred for therapy (based on each provider’s standard protocol). Therapy attendance was confirmed by the presence of therapy notes.
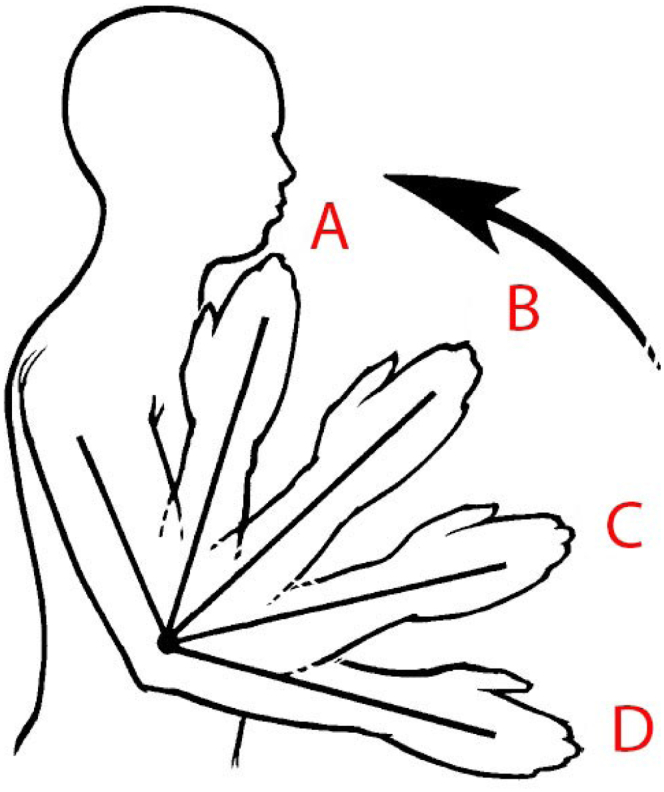
The patients who met the criteria for inclusion in the study were first contacted via a letter that allowed them to opt out of the study. Any patient who did not opt out of the study was then contacted by email with a link for a Research Electronic Data Capture survey. The survey included general questions about their injury and demographics, whether they sustained a subsequent injury to the same extremity after the initial dislocation, QuickDASH, and BRS. The QuickDASH scores ranged from 0 to 100, and higher scores indicated a higher level of perceived disability. The BRS was a 5-question survey designed to measure a patient’s resiliency or ability to cope with difficulties. Higher BRS scores indicated higher resiliency. The patients were also asked to estimate the current elbow range of motion using illustrations of elbow positions (Fig.). Several studies have shown that the visual assessment of elbow range of motion has a high validity compared with clinical goniometer measurements; however, the use of these specific illustrations has not been validated in the current literature.31, 32, 33 Satisfaction with the treatment outcome was queried using a binary Yes/No question asking, “Are you satisfied with your elbow dislocation treatment?” and using a 100-point visual analog scale to measure satisfaction. The patients who did not complete the survey were contacted via telephone. A total of 3 emails and 3 telephone calls were made as needed. If no contact was established after these efforts, the patient was deemed lost to follow-up.
Figure.
Representative illustration from the questionnaire designed to allow patients to estimate their current elbow range of motion. This illustration was used to estimate the degree of flexion. A represents “normal” flexion or 160°. B represents 125° of flexion. C represents 90° of flexion. D represents <90° of flexion.
To measure social deprivation for each patient, we used the ADI for each patient. The ADI was obtained using the 9-digit zip code for each patient.34 The ADI encompasses socioeconomic status identified using geographic deprivation indices obtained from census data, and it has been used in public health studies as a measurement of economic and social characteristics of a neighborhood.34, 35, 36
A power analysis was performed a priori to detect a clinically relevant difference in final QuickDASH scores between a treatment cohort that received early hand therapy within 3 weeks of injury and a control cohort that did not receive early therapy. A minimal clinically important difference of 14 points on the QuickDASH was used for this power calculation, revealing that a total of 27 patients in the treatment cohort and 13 patients in the control cohort were needed.37 These sample sizes were based on a goal of achieving 80% power at a 2-tailed 0.05 level of statistical significance.
Continuous variables were compared using a t test, and categorical variables were compared using chi-square test or Fisher exact test as appropriate. To test associations with the QuickDASH outcome score, we used separate univariate Tobit regression models for each possible factor. The Tobit model was used due to the ceiling effect observed for the QuickDASH outcome.38,39 Our Tobit regression results could be interpreted similarly to a conventional linear regression model, indicating a mean increase in QuickDASH for each unit increase in a continuous predictor. For categorical predictor variables, the Tobit model reported the average increase in QuickDASH for each level of the variable relative to its reference level. The regression coefficients, 95% confidence intervals, and P values were reported for each factor. A multivariate Tobit regression model was used to identify associations between QuickDASH and predictors that were found to be significant in the univariate analysis.
Results
We identified 118 patients who sustained a simple elbow dislocation or dislocation with a minor associated fracture from 2000 to 2018, and who met the inclusion criteria for the study. Thirty-eight patients were unreachable, and 40 patients either declined to participate or submitted incomplete surveys. We received usable surveys from 40 patients, 13 in the control cohort and 27 in the treatment cohort. The average follow-up duration after the reduction was 67.5 months (range, 15.5 months to 14 years). The average age at the time of injury was 36.8 ± 14.1 years, and 55% of the patients were female. There was no statistical difference between cohorts for all patient demographics (Table 1). There was also no statistical difference between cohorts regarding the type of dislocation, mechanism of injury, specialty of the treating physician, history of a subsequent injury to the same extremity, insurance status, or ADI (Table 1).
Table 1.
Demographics and Baseline Patient Characteristics
| Variable | Total (N = 40) | Control (N = 13) | Treatment (N = 27) | P Value |
|---|---|---|---|---|
| Age at injury, mean ± SD | 36.8 ± 14.1 | 41.2 ± 12.8 | 34.7 ± 14.4 | .17 |
| Sex, n (%) | .44 | |||
| Female | 22 (55.0%) | 6 (46.2%) | 16 (59.3%) | |
| Male | 18 (45.0%) | 7 (53.8%) | 11 (40.7%) | |
| Race, n (%) | .68 | |||
| Asian | 1 (2.5%) | 0 (0.0%) | 1 (3.7%) | |
| Caucasian | 37 (92.5%) | 12 (92.3%) | 25 (92.6%) | |
| Other | 2 (5.0%) | 1 (7.7%) | 1 (3.7%) | |
| Hand dominance, n (%) | .52 | |||
| Left | 7 (17.5%) | 3 (23.1%) | 4 (14.8%) | |
| Right | 33 (82.5%) | 10 (76.9%) | 23 (85.2%) | |
| Affected elbow, n (%) | .44 | |||
| Left | 22 (55.0%) | 6 (46.2%) | 16 (59.3%) | |
| Right | 18 (45.0%) | 7 (53.8%) | 11 (40.7%) | |
| Mechanism of injury, n (%) | .22 | |||
| Low energy | 19 (47.5%) | 8 (61.5%) | 11 (40.7%) | |
| High energy | 21 (52.5%) | 5 (38.5%) | 16 (59.3%) | |
| Injury, n (%) | .75 | |||
| Simple | 26 (65.0%) | 8 (61.5%) | 18 (66.7%) | |
| Minor fracture | 14 (35.0%) | 5 (38.5%) | 9 (33.3%) | |
| Specialty of treating physician, n (%) | .81 | |||
| Ortho hand | 19 (47.5%) | 5 (38.5%) | 14 (51.9%) | |
| Ortho shoulder/elbow | 4 (10.0%) | 2 (15.4%) | 2 (7.4%) | |
| Ortho trauma | 8 (20.0%) | 3 (23.1%) | 5 (18.5%) | |
| Nonsurgical | 9 (22.5%) | 3 (23.1%) | 6 (22.2%) | |
| New injuries to same extremity, n (%) | .95 | |||
| No | 31 (77.5%) | 10 (76.9%) | 21 (77.8%) | |
| Yes | 9 (22.5%) | 3 (23.1%) | 6 (22.2%) | |
| Required late therapy, n (%) | .50 | |||
| No | 36 (94.7%) | 10 (90.9%) | 26 (96.3%) | |
| Yes | 2 (5.3%) | 1 (9.1%) | 1 (3.7%) | |
| Insurance status, n (%) | .74 | |||
| Private | 30 (75.0%) | 9 (69.2%) | 21 (77.8%) | |
| Medicare | 1 (2.5%) | 0 (0.0%) | 1 (3.7%) | |
| Medicaid | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| WC | 4 (10.0%) | 2 (15.4%) | 2 (7.4%) | |
| Uninsured | 5 (12.5%) | 2 (15.4%) | 3 (11.1%) | |
| ADI (state), mean ± SD | 4.07 ± 2.68 | 5.15 ± 2.97 | 3.56 ± 2.42 | .08 |
| ADI (national), mean ± SD | 30.7 ± 21.2 | 38.2 ± 24.7 | 27.1 ± 18.7 | .12 |
In general, clinical outcomes were good, with a mean QuickDASH score of 9.0 ± 14.8, and no differences between patients receiving and not receiving early therapy (6.5 ± 11.3 vs 14.1 ± 19.6, respectively; P = .32) were noted. Mean BRS scores were consistent with high levels of resiliency (4.0 ± 0.8). Overall, 95% of patients reported satisfaction with their outcome, and the mean visual analog scale satisfaction score was 85.9 ± 21.0 (Table 2).
Table 2.
Summary of Outcomes
| Variable | Total (N = 40) | Control (N = 13) | Treatment (N = 27) | P Value |
|---|---|---|---|---|
| QuickDASH, mean ± SD | 9.0 ± 14.8 | 14.1 ± 19.6 | 6.5 ± 11.3 | .32 |
| BRS, mean ± SD | 4.0 ± 0.8 | 3.7 ± 1.0 | 4.1 ± 0.7 | .14 |
| Satisfied? N (%) | >.99 | |||
| Yes | 38 (95.0) | 13 (100.0) | 25 (92.6) | |
| No | 2 (5.0) | 0 (0.0) | 2 (7.4) | |
| Satisfaction rating (scale 1–100), mean ± SD | 85.9 ± 21.0 | 82.6 ± 19.4 | 87.4 ± 21.9 | .50 |
| Work with hand therapy again? n (%) | N/A | |||
| Yes | 24 (88.9) | |||
| No | 2 (7.4) | |||
| Undecided | 1 (3.7) | |||
| Preferred to have hand therapy? n (%) | N/A | |||
| Yes | 3 (23.1) | |||
| No | 5 (38.5) | |||
| Undecided | 5 (38.5) | |||
| Early surgery? n (%) | - | |||
| Yes | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| No | 40 (100.0) | 13 (100.0) | 27 (100.0) | |
| Late surgery? n (%) | >.99 | |||
| Yes | 1 (2.5) | 0 (0.0) | 1 (3.7) | |
| No | 39 (97.5) | 13 (100.0) | 26 (96.3) |
N/A, not applicable.
The majority of patients reported equal range of motion to the contralateral uninjured elbow (67.5%), with no differences between those with and without an early therapy (76.9% vs 63%, respectively; P = .38). Moreover, the majority of patients reported full elbow extension (82.4%), elbow flexion (94.1%), pronation (85.7%), and supination (73.5%) (Table 3).
Table 3.
Elbow Range of Motion
| Variable | Total (N = 40) | Control (N = 13) | Treatment (N = 27) | P Value |
|---|---|---|---|---|
| Elbow extension, n (%) | .70 | |||
| 180° (normal) | 28 (82.4) | 7 (77.8) | 21 (84.0) | |
| 150° | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| 120° | 5 (14.7) | 2 (22.2) | 3 (12.0) | |
| 90° | 1 (2.9) | 0 (0.0) | 1 (4.0) | |
| Elbow flexion, n (%) | .47 | |||
| 160° (normal) | 32 (94.1) | 8 (88.9) | 24 (96.0) | |
| 125° | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| 90° | 1 (2.9) | 0 (0.0) | 1 (4.0) | |
| <90° | 1 (2.9) | 1 (11.1) | 0 (0.0) | |
| Elbow pronation, n (%) | .06 | |||
| 90° (normal) | 30 (85.7) | 8 (80.0) | 22 (88.0) | |
| 60° | 1 (2.9) | 1 (10.0) | 0 (0.0) | |
| 30° | 1 (2.9) | 1 (10.0) | 0 (0.0) | |
| 0° (neutral) | 3 (8.6) | 0 (0.0) | 3 (12.0) | |
| Elbow supination, n (%) | .13 | |||
| 90° (normal) | 25 (73.5) | 6 (66.7) | 19 (76.0) | |
| 60° | 1 (2.9) | 1 (11.1) | 0 (0.0) | |
| 30° | 1 (2.9) | 1 (11.1) | 0 (0.0) | |
| 0° (neutral) | 7 (20.6) | 1 (11.1) | 6 (24.0) | |
| Motion same as uninjured elbow? n (%) | .38 | |||
| Yes | 27 (67.5) | 10 (76.9) | 17 (63.0) | |
| No | 13 (32.5) | 3 (23.1) | 10 (37.0) |
Only 1 patient (in the treatment cohort) required late surgery—ligament reconstruction for persistent instability.
In the univariate analysis, there was a significant association between higher QuickDASH scores and higher ADI (greater social deprivation, P = .01), older age at the time of injury (P = .04), female sex (P = .05), high-energy mechanism (P = .04), new upper-extremity injury since the time of elbow closed reduction (P < .01), lower BRS (P = .01), Medicare insurance status (P = .02), and worker’s compensation (WC) insurance status (P < .01). Early therapy, specialty of the treating physician, and the presence of additional minor fractures were not associated with the QuickDASH outcome, per univariate analysis (Table 4).
Table 4.
Univariate Analysis
| Variable | Level |
QuickDASH Coefficient (95% confidence interval) |
P Value |
|---|---|---|---|
| Early therapy | No | Reference | .22 |
| Yes | −9.46 (−24.77, 5.86) | ||
| Age at injury | For each year increasing | 0.52 (0.02, 1.01) | .04 |
| ADI (state) | For each score increasing | 3.45 (1.06, 5.85) | .006 |
| ADI (national) | For each score increasing | 0.53 (0.26, 0.80) | <.001 |
| Sex | Female | Reference | .045 |
| Male | −14.90 (−29.47, −0.33) | ||
| Race | Asian and others | Reference | .67 |
| Caucasian | 5.89 (−22.09, 33.86) | ||
| Mechanism of injury | Low energy | Reference | .039 |
| High energy | −15.28 (−29.74, −0.82) | ||
| Injury | Simple minor fracture | Reference | .27 |
| −8.30 (−23.44, 6.83) | |||
| Specialty of treating physician | Ortho hand | Reference | |
| Ortho shoulder/elbow | −129.74 (−129.74, −129.74) | - | |
| Ortho trauma | −7.93 (−26.44, 10.58) | .39 | |
| Nonortho | 1.45 (−16.56, 19.47) | .87 | |
| New injuries | No | Reference | .003 |
| Yes | 23.85 (8.59, 39.11) | ||
| Required late therapy | Yes | Reference | .23 |
| No | −19.06 (−50.83, 12.71) | ||
| Insurance status | Private | Reference | |
| Medicare | 41.21 (6.58, 75.83) | .02 | |
| WC | 30.77 (12.10, 49.44) | .002 | |
| Uninsured | 813.54 (−3.36, 30.44) | .11 | |
| BRS | −12.84 (−22.24, −3.45) | .009 |
The multivariate model demonstrated a significant association between worse QuickDASH scores and higher ADI (coefficient 0.38; 95% confidence interval 0.91–0.57; P < .01) and Medicare insurance status (30.93; 5.59–56.28; P = .02) or WC insurance status (18.45; 5.91–31.00; P = .01) relative to commercially-insured patients. In other words, for every 10 unit increase in ADI, the QuickDASH score increased by 3.8. Patient insurance status (P = .40), early therapy (P = .36), sex (P = .74), mechanism of injury (P = .88), and BRS score (P = .23) were not significant. These findings were independent of whether a new upper-extremity injury had occurred since the date of the closed reduction (Table 5).
Table 5.
Multivariate Analysis
| Predictor Variable | QuickDASH Coefficient (95% confidence interval) | P Value |
|---|---|---|
| Early therapy | 3.90 (−12.37, 4.58) | .36 |
| Age at injury | 0.07 (−0.27, 0.42) | .68 |
| ADI (national) | 0.38 (0.19, 0.57) | <.001 |
| Female sex | −1.45 (−10.43, 7.52) | .74 |
| High-energy mechanism | −0.61 (−8.87, 7.66) | .88 |
| New injuries | 13.86 (5.20, 22.52) | .003 |
| Medicare insurance | 30.93 (5.59, 56.28) | .018 |
| WC insurance | 18.45 (5.91, 31.00) | .005 |
| Uninsured | 4.71 (−6.47, 15.88) | .40 |
| BRS | −2.56 (−6.80, 1.68) | .23 |
Discussion
Our study demonstrated that the long-term outcomes following closed reduction of simple elbow dislocation are in general good. This correlated with the results from other studies, which also found generally good results in PROs after elbow dislocation.4, 5, 6, 7 As we hypothesized, there was no difference in the outcome scores between the 2 cohorts, suggesting that early therapy does not significantly affect outcomes after an elbow dislocation. In addition, early therapy did not affect patient satisfaction with their injured elbow. To our knowledge, no prior study has evaluated the effect of hand therapy on outcomes after elbow dislocation.
Although the patients did well, we found that social deprivation was associated with worse outcomes. Interestingly, this was independent of injury mechanism, age, sex, early therapy, and all other studied factors. Social deprivation is a nonmodifiable risk factor that has been associated with worse outcomes in prior research.40
Secondary findings of this study are that the insurance status, specifically WC and Medicare, were associated with worse outcomes. However, as there was only 1 patient in the study with Medicare insurance, conclusions as to the effect of Medicare could not be made. Many prior studies have also identified WC as an independent nonmodifiable risk factor for poor outcomes in most orthopedic procedures and conditions.41, 42, 43, 44
Limitations of the study include its retrospective nature that may lead to selection bias and recall bias. Although the providers followed their standard treatment protocol for these patients, the influence of patient or injury factors on the decision to refer to hand therapy was not documented and therefore could lead to selection bias. Furthermore, there was no way to determine compliance with hand therapy. The BRS attempts to measure resiliency, which is a personality trait that would not be expected to change over time. Our analysis uses BRS scores at follow-up rather than at baseline, and it is unclear if that may affect the study findings. Also, the response rate was low (50% of all eligible patients who were able to be contacted and 34% of all eligible patients). However, we still were able to achieve a sufficient sample size to meet that suggested as necessary by our a priori power analysis. Another limitation was that although there was notable variation in social deprivation, the cohort in general demonstrated levels of social deprivation in the lower median of possible scores. Considering that our study found that greater social deprivation is correlated with worse outcomes, it is possible that a similar study including patients with a larger range of social deprivation would only show a stronger correlation.
In conclusion, the PROs following simple elbow dislocation are generally good. Although surgeons should be aware of the possibility that specific subsets of patients may benefit from early therapy, this factor did not appear to influence outcomes, both in terms of PROs and elbow range of motion, in this small cohort. There was an association between worse outcome scores and greater levels of social deprivation or certain insurance types (WC), both nonmodifiable risk factors. These findings identify an opportunity to further investigate health disparities that lead to worse outcomes.
Acknowledgments
The authors acknowledge Jared Potter, BS and Morgan Millar, PhD. This investigation was supported by the University of Utah Population Health Research (PHR) Foundation, with funding in part from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant 5UL1TR001067-05 (formerly 8UL1TR000105 and UL1RR025764).
Footnotes
Declaration of interests: No benefits in any form have been received or will be received related directly or indirectly to the subject of this article.
References
- 1.Stoneback J.W., Owens B.D., Sykes J., Athwal G.S., Pointer L., Wolf J.M. Incidence of elbow dislocations in the United States population. J Bone Joint Surg Am. 2012;94(3):240–245. doi: 10.2106/JBJS.J.01663. [DOI] [PubMed] [Google Scholar]
- 2.Josefsson P.O., Nilsson B.E. Incidence of elbow dislocation. Acta Orthop Scand. 1986;57(6):537–538. doi: 10.3109/17453678609014788. [DOI] [PubMed] [Google Scholar]
- 3.Polinder S., Iordens G.I., Panneman M.J., et al. Trends in incidence and costs of injuries to the shoulder, arm and wrist in the Netherlands between 1986 and 2008. BMC Public Health. 2013;13:531. doi: 10.1186/1471-2458-13-531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anakwe R.E., Middleton S.D., Jenkins P.J., McQueen M.M., Court-Brown C.M. Patient-reported outcomes after simple dislocation of the elbow. J Bone Joint Surg Am. 2011;93(13):1220–1226. doi: 10.2106/JBJS.J.00860. [DOI] [PubMed] [Google Scholar]
- 5.Forthman C., Henket M., Ring D.C. Elbow dislocation with intra-articular fracture: the results of operative treatment without repair of the medial collateral ligament. J Hand Surg Am. 2007;32(8):1200–1209. doi: 10.1016/j.jhsa.2007.06.019. [DOI] [PubMed] [Google Scholar]
- 6.Pugh D.M., Wild L.M., Schemitsch E.H., King G.J., McKee M.D. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. J Bone Joint Surg Am. 2004;86(6):1122–1130. doi: 10.2106/00004623-200406000-00002. [DOI] [PubMed] [Google Scholar]
- 7.de Haan J., Schep N.W., Zengerink I., van Buijtenen J., Tuinebreijer W.E., den Hartog D. Dislocation of the elbow: a retrospective multicentre study of 86 patients. Open Orthop J. 2010;4:76–79. doi: 10.2174/1874325001004020076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gabel C.P., Yelland M., Melloh M., Burkett B. A modified QuickDASH-9 provides a valid outcome instrument for upper limb function. BMC Musculoskelet Disord. 2009;10:161. doi: 10.1186/1471-2474-10-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mintken P.E., Glynn P., Cleland J.A. Psychometric properties of the shortened Disabilities of the Arm, Shoulder, and Hand questionnaire (QuickDASH) and numeric pain rating scale in patients with shoulder pain. J Shoulder Elbow Surg. 2009;18(6):920–926. doi: 10.1016/j.jse.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 10.Stepan J.G., London D.A., Boyer M.I., Calfee R.P. Accuracy of patient recall of hand and elbow disability on the QuickDASH questionnaire over a two-year period. J Bone Joint Surg Am. 2013;95(22):e176. doi: 10.2106/JBJS.L.01485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ayers D.C., Franklin P.D., Ring D.C. The role of emotional health in functional outcomes after orthopaedic surgery: extending the biopsychosocial model to orthopaedics: AOA critical issues. J Bone Joint Surg Am. 2013;95(21):e165. doi: 10.2106/JBJS.L.00799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Das De S., Vranceanu A.M., Ring D.C. Contribution of kinesophobia and catastrophic thinking to upper-extremity-specific disability. J Bone Joint Surg Am. 2013;95(1):76–81. doi: 10.2106/JBJS.L.00064. [DOI] [PubMed] [Google Scholar]
- 13.Kazmers N.H., Hung M., Rane A.A., Bounsanga J., Weng C., Tyser A.R. Association of physical function, anxiety, and pain interference in nonshoulder upper extremity patients using the PROMIS platform. J Hand Surg Am. 2017;42(10):781–787. doi: 10.1016/j.jhsa.2017.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kortlever J.T., Janssen S.J., van Berckel M.M., Ring D., Vranceanu A.M. What is the most useful questionnaire for measurement of coping strategies in response to nociception? Clin Orthop Relat Res. 2015;473(11):3511–3518. doi: 10.1007/s11999-015-4419-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nota S.P., Spit S.A., Oosterhoff T.C., Hageman M.G., Ring D.C., Vranceanu A.M. Is social support associated with upper extremity disability? Clin Orthop Relat Res. 2016;474(8):1830–1836. doi: 10.1007/s11999-016-4892-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oflazoglu K., Mellema J.J., Menendez M.E., Mudgal C.S., Ring D., Chen N.C. Prevalence of and factors associated with major depression in patients with upper extremity conditions. J Hand Surg Am. 2016;41(2):263–269. doi: 10.1016/j.jhsa.2015.11.019. e1–e7. [DOI] [PubMed] [Google Scholar]
- 17.Vranceanu A.M., Jupiter J.B., Mudgal C.S., Ring D. Predictors of pain intensity and disability after minor hand surgery. J Hand Surg Am. 2010;35(6):956–960. doi: 10.1016/j.jhsa.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 18.Ring D., Kadzielski J., Fabian L., Zurakowski D., Malhotra L.R., Jupiter J.B. Self-reported upper extremity health status correlates with depression. J Bone Joint Surg Am. 2006;88(9):1983–1988. doi: 10.2106/JBJS.E.00932. [DOI] [PubMed] [Google Scholar]
- 19.Lozano-Calderon S.A., Souer J.S., Jupiter J.B., Ring D. Psychological differences between patients that elect operative or nonoperative treatment for trapeziometacarpal joint arthrosis. Hand (N Y) 2008;3(3):271–275. doi: 10.1007/s11552-008-9098-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beleckas C.M., Prather H., Guattery J., Wright M., Kelly M., Calfee R.P. Anxiety in the orthopedic patient: using PROMIS to assess mental health. Qual Life Res. 2018;27(9):2275–2282. doi: 10.1007/s11136-018-1867-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Crijns T.J., Bernstein D.N., Ring D., Gonzalez R.M., Wilbur D.M., Hammert W.C. Depression and pain interference correlate with physical function in patients recovering from hand surgery. Hand (N Y) 2019;14(6):830–835. doi: 10.1177/1558944718777814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wright M.A., Adelani M., Dy C., OʼKeefe R., Calfee R.P. What is the impact of social deprivation on physical and mental health in orthopaedic patients? Clin Orthop Relat Res. 2019;477(8):1825–1835. doi: 10.1097/CORR.0000000000000698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Duckworth A.D., Clement N.D., Jenkins P.J., Will E.M., Court-Brown C.M., McQueen M.M. Socioeconomic deprivation predicts outcome following radial head and neck fractures. Injury. 2012;43(7):1102–1106. doi: 10.1016/j.injury.2012.02.017. [DOI] [PubMed] [Google Scholar]
- 24.Jenkins P.J., Perry P.R., Yew Ng C., Ballantyne J.A. Deprivation influences the functional outcome from total hip arthroplasty. Surgeon. 2009;7(6):351–356. doi: 10.1016/s1479-666x(09)80109-1. [DOI] [PubMed] [Google Scholar]
- 25.Jenkins P.J., Watts A.C., Duckworth A.D., McEachan J.E. Socioeconomic deprivation and the epidemiology of carpal tunnel syndrome. J Hand Surg Eur Vol. 2012;37(2):123–129. doi: 10.1177/1753193411419952. [DOI] [PubMed] [Google Scholar]
- 26.Paksima N., Pahk B., Romo S., Egol K.A. The association of education level on outcome after distal radius fracture. Hand (N Y) 2014;9(1):75–79. doi: 10.1007/s11552-013-9557-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Okoroafor U.C., Gerull W., Wright M., Guattery J., Sandvall B., Calfee R.P. The impact of social deprivation on pediatric PROMIS health scores after upper extremity fracture. J Hand Surg Am. 2018;43(10):897–902. doi: 10.1016/j.jhsa.2018.06.119. [DOI] [PubMed] [Google Scholar]
- 28.Jayakumar P., Teunis T., Vranceanu A.M., Lamb S., Ring D., Gwilym S. Early psychological and social factors explain the recovery trajectory after distal radial fracture. J Bone Joint Surg Am. 2020;102(9):788–795. doi: 10.2106/JBJS.19.00100. [DOI] [PubMed] [Google Scholar]
- 29.Kazmers N.H., Grasu B., Presson A.P., Ou Z., Henrie N.B., Tyser A.R. The prognostic value of preoperative patient-reported function and psychological characteristics on early outcomes following trapeziectomy with ligament reconstruction tendon interposition for treatment of thumb carpometacarpal osteoarthritis. J Hand Surg Am. 2020;45(6):469–478. doi: 10.1016/j.jhsa.2019.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.University of Wisconsin School of Medicine Public Health 2015 Area Deprivation Index v2.0. https://www.neighborhoodatlas.medicine.wisc.edu/
- 31.Blonna D., Zarkadas P.C., Fitzsimmons J.S., O’Driscoll S.W. Accuracy and inter-observer reliability of visual estimation compared to clinical goniometry of the elbow. Knee Surg Sports Traumatol Arthrosc. 2012;20(7):1378–1385. doi: 10.1007/s00167-011-1720-9. [DOI] [PubMed] [Google Scholar]
- 32.Beirer M., Friese H., Lenich A., et al. The Elbow Self-Assessment Score (ESAS): development and validation of a new patient-reported outcome measurement tool for elbow disorders. Knee Surg Sports Traumatol Arthrosc. 2017;25(7):2230–2236. doi: 10.1007/s00167-015-3647-z. [DOI] [PubMed] [Google Scholar]
- 33.Schnetzke M., Schüler S., Keil H., et al. Development and validation of a novel questionnaire for self-determination of the range of motion of wrist and elbow. BMC Musculoskelet Disord. 2016;17:312. doi: 10.1186/s12891-016-1171-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Knighton A.J., Savitz L., Belnap T., Stephenson B., VanDerslice J. Introduction of an area deprivation index measuring patient socioeconomic status in an integrated health system: implications for population health. EGEMS (Wash DC) 2016;4(3):1238. doi: 10.13063/2327-9214.1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Butler D.C., Petterson S., Phillips R.L., Bazemore A.W. Measures of social deprivation that predict health care access and need within a rational area of primary care service delivery. Health Serv Res. 2013;48(2 Pt 1):539–559. doi: 10.1111/j.1475-6773.2012.01449.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hofer T.P., Wolfe R.A., Tedeschi P.J., McMahon L.F., Griffith J.R. Use of community versus individual socioeconomic data in predicting variation in hospital use. Health Serv Res. 1998;33(2 Pt 1):243–259. [PMC free article] [PubMed] [Google Scholar]
- 37.Sorensen A.A., Howard D., Tan W.H., Ketchersid J., Calfee R.P. Minimal clinically important differences of 3 patient-rated outcomes instruments. J Hand Surg Am. 2013;38(4):641–649. doi: 10.1016/j.jhsa.2012.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tobin J. Estimation of relationships for limited dependent variables. Econometrica. 1958;26(1):24–36. [Google Scholar]
- 39.McBee M. Modeling outcomes with floor or ceiling effects: an introduction to the Tobit model. Gifted Child Quarterly. 2010;54(4):314–320. [Google Scholar]
- 40.Stephens A.R., Tyser A.R., Kazmers N.H. The impact of social deprivation on orthopaedic outpatient satisfaction using the Press Ganey Outpatient Medical Practice Survey. J Am Acad Orthop Surg. 2020;28(24):e1111–e1120. doi: 10.5435/JAAOS-D-19-00852. [DOI] [PubMed] [Google Scholar]
- 41.Buckley R., Tough S., McCormack R., et al. Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am. 2002;84(10):1733–1744. doi: 10.2106/00004623-200210000-00001. [DOI] [PubMed] [Google Scholar]
- 42.Higgs P.E., Edwards D., Martin D.S., Weeks P.M. Carpal tunnel surgery outcomes in workers: effect of workers’ compensation status. J Hand Surg Am. 1995;20(3):354–360. doi: 10.1016/S0363-5023(05)80086-3. [DOI] [PubMed] [Google Scholar]
- 43.Morris B.J., Haigler R.E., Laughlin M.S., Elkousy H.A., Gartsman G.M., Edwards T.B. Workers’ compensation claims and outcomes after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24(3):453–459. doi: 10.1016/j.jse.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 44.Daniels A.H., Kuris E.O., Kleinhenz D.T., Palumbo M.A. Spine surgery outcomes in workers’ compensation patients. J Am Acad Orthop Surg. 2017;25(10):e225–e234. doi: 10.5435/JAAOS-D-16-00895. [DOI] [PubMed] [Google Scholar]