Abstract
Face masks are necessary for fighting against the coronavirus disease 2019 around the world. As the face mask is usually made from polymers and phthalates are widely-used additives into the polymers, the face mask could be a potential source of phthalate exposure to humans. However, limited knowledge is available on the occurrence and risks of the phthalates from the face mask. In this study, twelve phthalates were determined in 56 mask samples collected from different countries. The phthalates were detected in all the samples with total levels ranging from 115 ng/g to 37,700 ng/g. Estimated daily intakes (EDIs) of the phthalates from the masks ranged from 3.71 to 639 ng/kg-bw/day, and the EDIs of the phthalates from masks for toddlers were approximately 4–5 times higher than those for adults. Non-carcinogenic risks in relation to the phthalates in masks were found to be within safe levels, yet 89.3% of the mask samples exhibited potential carcinogenic effects to humans. The extent of the risks for wearing masks located at a moderate level comparing with other skin-contacted products. This study unveiled a potential source of phthalate exposure to human, and indicated necessity of managing types and levels of additives in the face masks.
Keywords: Face mask, Phthalate exposure, Estimated daily intake, Risk assessment
Graphical Abstract
1. Introduction
Since the outbreak of the coronavirus disease 2019 (COVID-19) which was claimed to be a pandemic by the World Health Organization (WHO), more than 114 million (by March 3, 2021) people have been infected by this virus (WHO Coronavirus Disease, 2021). The COVID-19 is highly contagious and it attacks not only lung but also heart, kidney, brain and many other organs (Lukiw et al., 2020, Vasquez-Bonilla et al., 2020). According to the WHO, the impact of the COVID-19 may last for decades. Fortunately, it has been convinced that protective face masks can be applied to prevent the spread of the coronavirus and the masks can reduce the spray of droplets when worn over the nose and mouth (Zhang et al., 2020, Cheng et al., 2020, Prather et al., 2020). Therefore wearing a mask has gradually become a habit of people.
Millions of masks can be consumed within 1 d, protecting millions of people from infection (Li et al., 2020). However, the numerous masks have simultaneously brought some adverse effects on the environment and human health. For instance, the rising consumption and production of the face masks globally can increase the plastic waste and plastic particle pollution (Aragaw, 2020, Fadare and Okoffo, 2020, Patricio Silva et al., 2021). Furthermore, recent studies reported that long-term use of plastic mask could lead to various of skin problems (Aerts et al., 2020, Bhatia et al., 2020, Xie et al., 2020). It was speculated that these skin problems were mainly caused by the chemicals released from the mask. The mask is usually made of polymers (mostly polypropylene) and the polymers can involve lots of additives (Jung et al., 2021, Camargo et al., 2020). Among the additives, phthalate is a group of high production volume (HPV) chemicals that needs to be concerned.
Phthalates are usually used as plasticizers to reduce shear in the polymer producing process and to improve flexibility and versatility of the polymers (Guo and Kannan, 2013, Rahman and Brazel, 2004, Vieira et al., 2011). Although the use of phthalates has been partly regulated in some countries, their annual usage amount is still up to several million tons (Net et al., 2015). The phthalates are usually applied as additives and they are not chemically bonded to the materials, therefore they can be easily released into the environment and enter human body, and further exert a series of adverse effects (Gong et al., 2016). For instance, the phthalate exposure was reported to affect fetal growth and had reproductive toxicity (Martino‐Andrade and Chahoud, 2010, Yost et al., 2019, Kay et al., 2013). Butyl benzyl phthalate (BBP) and diisononyl phthalate (DINP) were proved to affect testosterone and semen parameters (Radke et al., 2018). Bis(2-ethylhexyl)phthalate (DEHP) was also found to be associated with penile birth defects and other effects related to androgen disruption (Bornehag et al., 2015).
Previous studies reported that the phthalates were widely determined in textiles and skin contacted products, including cotton clothing (Li et al., 2019), sanitary napkin (Tang et al., 2019, Gao et al., 2019), paper diaper and toys (Negev et al., 2018) et al. The phthalates from these products can enter human body through dermal absorption, as well as ingestion. It is reported that these phthalate exposures might lead to contact allergy and even pose carcinogenic risks to humans (Li et al., 2019, Rovira and Domingo, 2019). Compared with the mentioned textiles and skin contacted products, the face mask can directly contact people’s nose and mouth, then the phthalates can be taken up through dermal absorption, ingestion and inhalation. These joint exposure pathways may increase the phthalates intakes comparing with other products. However, there is no regulation or standard on the use of phthalates in mask products around the world. The phthalate occurrence and exposure from the mask and its potential risk to human health are still knowledge gaps.
Under this circumstance, in the present study, 56 mask samples were collected and 12 phthalates in the masks were analyzed. The phthalate contents in the masks among different countries and different production standards were investigated. In addition, the daily intakes of the phthalates from the masks were estimated, and the phthalate exposures for adults and toddlers were compared. Finally, the health risks of the phthalate exposure were assessed, including carcinogenic risk and non-carcinogenic risk. We hope the results can be employed to fill the knowledge gap for the mask production standards as well as phthalate management policies.
2. Materials and methods
2.1. Chemicals
Twelve phthalates were analyzed in this study, including dimethyl phthalate (DMP), diethyl phthalate (DEP), diisobutyl phthalate (DiBP), di-n-butyl phthalate (DBP), bis(2-methoxyethyl)phthalate (DMEP), diamyl phthalate (DPP), dihexyl phthalate (DHXP), dicyclohexyl phthalate (DCHP), bis(2-Ethylhexyl)phthalate (DEHP), diphenyl phthalate (DPhP), di-n-octyl phthalate (DNOP) and dinonyl phthalate (DNP). Three deuterated compounds were used as surrogates, including diisobutyl phthalate-d4 (DiBP-d4), dimethyl phthalate-d4 (DMP-d4) and diethyl phthalate-d4 (DEP-d4). All of the targets and surrogates were purchased from AccuStandard Inc. (New Haven, USA). Hexamethylbenzene was acted as an international standard and it was obtained by J&K Scientific Ltd. (China).
2.2. Sample collection and preparation
Fifty-six brands of masks from different countries and regions were collected through online or local shops in May of 2020, including 44 Chinese brands, 6 European brands, 3 American brands, 2 Japanese brands and 1 South Korean brand. All of these masks were manufactured locally and widely used in daily life. The 44 Chinese brands contained 28 masks for adults and 16 masks for toddlers, and the masks from other countries were all for adults. The 28 Chinese adult mask brands contained 11 KN95 masks and 17 disposable masks. Detailed information on the masks is shown in Table S1 in supporting information.
In order to avoid potential contamination during storage, the mask samples were prepared immediately after collection. Elastic band and metal nose strip in the mask were removed, and then the net weight of the masks was determined (listed in Table S1). The mask samples were cut into small pieces through stainless steel scissors within 2 mm × 2 mm. Three masks from each brand were cut together and mixed as a representative sample, and then placed in a pre-cleaned glass bottle. 0.5 g sample was accurately weighed, then 50 ng of each surrogate standard was added. After equilibration for 4 h, the samples were extracted twice with 10 mL of dichloromethane/ethyl acetate (1:1, V/V) for 30 min in an ultrasonic bath. The eluent was separated with the sample through a glass syringe. Then the combined eluent was blown down to approximately 0.5 mL with N2. Finally, 50 ng of internal standard was spiked.
2.3. Instrumental analysis
The phthalates were analyzed through an Agilent gas chromatography mass spectrometry (GC-MS, 6890N-5975) in selected ion monitoring mode, operating with EI source. Separation was performed by a HP-5MS capillary column (30 m × 0.25 mm × 0.25 µm), and high purity helium was used as carrier gas at a flow rate of 1 mL/min. Temperatures of GC injection port and transfer line were both kept at 290 °C. The GC oven temperature was performed with a thermal gradient as following: 60 °C for 1 min, 20 °C /min to 220 °C, held for 1 min, 5 °C /min to 250 °C held for 1 min, 20 °C /min to 290 °C, held for 6 min, and finally programmed to 300 °C at 10 °C /min, held for 6 min. Temperatures for the ion source and quadrupole region were set at 230 °C and 150 °C, respectively. The retention time and precursor ion/product ions of the 12 phthalates are provided in the Supporting Information and Table S2.
2.4. Quality assurance and quality control
Only glass and stainless steel containers and tools were used during the whole procedures. All the containers and tools were rinsed with hexane and ethyl acetate prior to use. A procedural blank, as well as a duplicated sample, was processed in every ten samples as a batch. The relative standard deviations measured from duplicate samples were proved to be within 20%. DEHP, DBP, DEP, DMP, and DiBP were detected with low levels in the blank samples. The contamination of the phthalates during the pretreatment procedures seems inevitable. Similar results for the contamination were also found in lots of previous studies on phthalate analyzation (Guo and Kannan, 2013, Li et al., 2019, Gao et al., 2019, Tang et al., 2020). The recoveries of the phthalates ranged from 79.3% to 113.2%, indicating the matrix effect did not affect the analyzing results based on the internal standard method. The surrogate recoveries for DiBP-d4, DMP-d4 and DEP-d4 in all samples were 91.1 ± 10.9%, 87.2 ± 8.1% and 89.2 ± 8.8%, respectively. All phthalate concentrations in the samples were corrected with the blank and the surrogate recoveries. Method detection limits (MDLs) of the 12 phthalates fluctuated between 4.8 ng/g and 26.5 ng/g (listed in Table S2). Levels below the MDLs were set as of zero for statistical analysis.
2.5. Estimation of phthalate exposure
Estimated daily intakes (EDIs) for phthalates in the masks were estimated with the following equations according to previous studies (Tang et al., 2019):
| (1) |
where C i is the measured phthalate concentration in the mask (ng/g); M is the weight (g) of the mask measured in this study (Table S1); N is the number of masks used per day, in this study the N value was set as 1; A is the absorption rate of phthalate in mask by human body. In previous studies, the skin absorption rates of the phthalates were set as 5% for cosmetics and personal care products, 5–10% for paper diapers and 15% for sanitary napkins when estimating phthalates intake (Tang et al., 2019). Here, for the masks, the phthalate exposure can take place in two forms: through the direct contact with human skin, and through inhalation of the air gap between mask and skin surface. The respiration can lead to increase of temperature and moisture content, this might further increase the release rate of phthalates from mask as well as the intake rate into human body. Therefore, the absorption rate was selected as a higher value than the other products, i.e., 20%; BW represents body weight, assumed as 60 kg for adult and 8 kg for toddler according to the European Union Risk Assessment Report. In this model, the product of C, M and A was regarded as the intake of the phthalates from one mask in one day. Usage duration of a single masks was considered as 3–4 h, which was similar to that of a single paper diaper or sanitary napkin. The usage period of the masks within one day was distinguished with the paper diaper or sanitary napkin by adjusting the N values.
2.6. Risk assessment
The non-carcinogenic risks to adults and toddlers associated with the phthalates in the masks were estimated using hazard quotient (HQ) and the cumulative non-carcinogenic risks were estimated by the hazard index (HI), which is a sum of the HQ of individual phthalate. The calculation of the cumulative risks was based on assumption that the phthalates had similar mode of toxic action (Martino‐Andrade and Chahoud, 2010). The HQ can be calculated using Eq. (2) (Li et al., 2019):
| (2) |
where RfD is the reference dose of the individual phthalate. In this study, the RfD values were assumed to be equal to their corresponding oral RfD. The oral RfD values were obtained from the database of the United State Environmental Protection Agency (U.S. EPA) and listed in Table S3 in the supporting information. Carcinogenic risks (CRs) of the phthalates for adults and toddlers from the masks were conducted with the following equation:
| (3) |
where CFS is a slope factor of exposure to the individual phthalate. The CFS values of the phthalates were also assumed to be equal to their corresponding oral CFS (listed in Table S3).
2.7. Data analysis
SPSS version 21 was applied to analyze the data acquired (IBM SPSS, Armonk, NY, USA). The Kolmogorov-Smirnov test was employed to examine the normal distribution of the data. A nonparametric test was performed to compare various groups in the case that the data was not consistent with the assumption of normality. The Mann-Whitney test was applied for the comparison between two groups, while the Kruskal Wallis test was applied to compare multiple sets of measured data. This study set the statistical significance at less than 0.05.
3. Results and discussion
3.1. Phthalate concentrations
The phthalates contents in the 56 mask samples were listed in Table S4 and summarized in Table 1. Eleven phthalates were detected among the 12 targets. DEHP was detected in all samples, and DMP, DEP, DiBP, DBP, DPP, DPhP and DNP were detected with detection frequencies of > 50%, indicating that multiple phthalates were generally present in the face masks. DCHP was not found in any of the mask samples. The Kolmogorov-Smirnov test indicated that concentrations of most phthalates exhibited non-normal distribution (p < 0.05). The total concentrations of the phthalates ranged from 115 ng/g to 37,700 ng/g, with a median level of 1950 ng/g. DEHP, DBP and DiBP were found to be predominant phthalates with median levels of 590 ng/g, 322 ng/g and 321 ng/g. The maximum concentration was found for DEHP (36,700 ng/g), followed by DBP (4780 ng/g). The mask is mainly made of hot melt adhesive and non-woven fabric, and DEHP was reported to be a major plasticizer in these two materials (Wang et al., 2011, Lee et al., 2014). Thus the DEHP showed the highest detection level and detection frequency. Similar results were also found in other products, such as preschool children’s clothing (Tang et al., 2020) and feminine hygiene products (Gao et al., 2019).
Table 1.
Detection frequencies (DF, %) and concentrations (ng/g) of phthalates in mask samples (n = 56).
| Compound | Mean | Median | IQRa | Range | DF |
|---|---|---|---|---|---|
| DMP | 22.8 | 17.3 | 18.8 | < MDLb-126 | 76.8 |
| DEP | 76.2 | 12.0 | 61.4 | < MDL-1780 | 53.6 |
| DiBP | 401 | 321 | 347 | < MDL-1450 | 98.2 |
| DBP | 523 | 322 | 246 | < MDL-4780 | 98.2 |
| DMEP | 9.4 | < MDL | < MDL | < MDL-252 | 10.7 |
| DPP | 47.4 | 36.8 | 50.3 | < MDL-149 | 80.4 |
| DHXP | 131 | < MDL | 41.6 | < MDL-1530 | 44.6 |
| DEHP | 1590 | 590 | 789 | 37.4–36,700 | 100 |
| DPhP | 93.3 | 85.2 | 77.6 | < MDL-290 | 94.6 |
| DNOP | 93.8 | 7.1 | 43.4 | < MDL-1960 | 50.0 |
| DNP | 158 | 37.0 | 226 | < MDL-1500 | 57.1 |
| Total | 3150 | 1950 | 2620 | 115–37,700 |
IQR represents interquartile range.
MDL represents method detection limit.
Although the occurrence of the phthalates in masks was rarely reported in previous studies, some investigations on the phthalates in textiles and clothes can be used to compare with the results of this work. Previous studies reported that phthalates in crib mattress, nylon sheets and diaper-changing mats were above 0.1% by mass (Negev et al., 2018), which were much higher than those detected in the masks here. In addition, the concentrations of the phthalates in masks were 2–3 times lower than those in cotton clothing (Li et al., 2019), and 10–20 times lower than those in jeans (Gong et al., 2016). These can be mainly caused by adsorption of phthalates from surrounding air and environment during production and storage for the clothes (Li et al., 2019). While the environment for mask producing can be relatively clean and the masks were usually independently packaged, therefore the contamination of phthalates for the masks can be less.
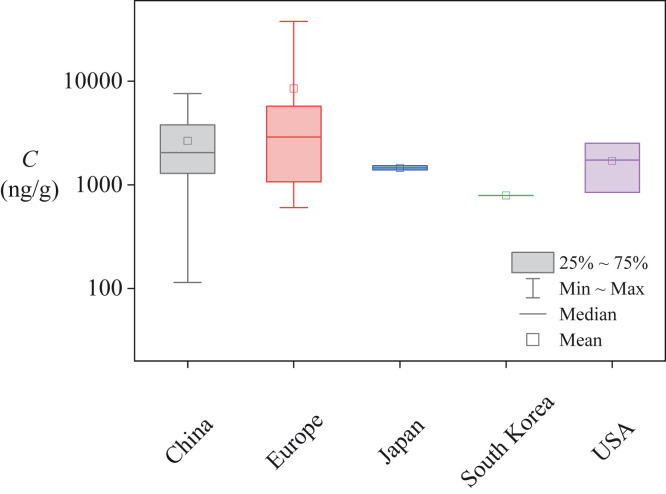
3.2. Phthalate contamination profile
Masks from 5 countries and regions were analyzed to examine whether the phthalate content depend on the geographical origin. As the samples collected from South Korea and Japanese were too few, they were not considered in the statistical analysis. According to the statistical test results, the total concentrations of the 11 detected phthalates did not differ significantly among the masks from different countries (p = 0.423, Fig. 1). The median values of the total phthalate concentrations ranged from 1730 ng/g to 2890 ng/g among the countries. In addition, the individual phthalate between countries showed the same result (p varied from 0.058 to 0.926) except for DEP and DPP (with p values of 0.001 and 0.035, respectively). The median concentrations of the DEP and DPP were both highest in the USA samples, with the mean values of 108 ng/g and 86.0 ng/g, respectively. The total and individual concentrations of the masks from South Korea seemed lower than those from other countries, however, the sample number was limited and the representativeness should be further investigated. These results indicated that the phthalate contents in the masks from different countries were similar on the whole, which goes against previous studies on children’s clothing (Tang et al., 2020) and sanitary napkin samples (Tang et al., 2019). The phthalate concentrations differed significantly in clothing and sanitary napkin between countries due to various use of materials and individual phthalates by countries. For the mask, the raw material and producing process were generally similar in the world and therefore the phthalate content showed consistent results.
Fig. 1.
Total concentrations (C) of phthalates in masks from different countries.
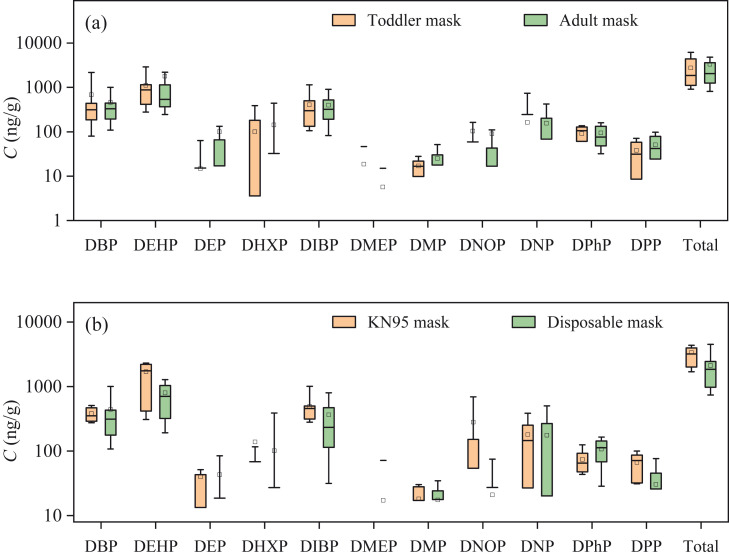
The phthalate contents were compared among the masks with different production standards and different applicable users. The detected levels of the masks were shown in Fig. 2. Significance test exhibited that there was no significant difference between phthalate levels in the masks for adults and toddlers (p ranged from 0.157 to 0.825). Similar result was also observed between the KN95 and disposable masks for most phthalates (p ranged from 0.059 to 0.926) except for DPP (p = 0.001) and DPhP (p = 0.019). The median levels for DPP and DPHP were 71.5 ng/g and 65.3 ng/g for the KN95 mask, while 23.5 ng/g and 115.2 ng/g for the disposable mask. No matter whether the mask was KN95 type or disposable type, for adults or toddlers, they were produced according to the production standards. While the essential difference among these standards was about filtration efficiency, appearance, respiratory resistance and leaking test, but not about materials or additives. In fact, most of the masks were made of hot melt adhesive and non-woven fabric, and therefore the masks had similar phthalate content.
Fig. 2.
Concentrations (C) of phthalates in different masks. The box plots show the 25th to the 75th percentiles of the data; upper and lower whiskers represent the 10th and 90th concentrations, respectively. The horizontal line within the box indicates the median value and the square indicates the mean value. The dot represents exception value.
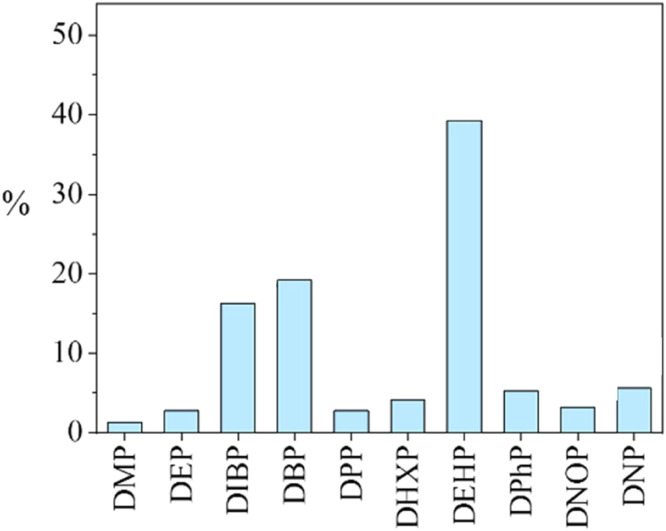
In all the samples (n = 56), significant differences (p < 0.05) in concentrations between individual phthalates were observed. The composition profile of phthalates in the mask samples was shown in Fig. 3. Although the DEHP has been reported to be replaced gradually in the global market (ECHA, 2013), it still showed the highest percentage (39.3%) among the plasticizers in all mask samples. DBP has also been reported to be gradually replaced by DiBP, the result showed that their levels were both predominant (19.2% and 16.3%, respectively). Similar compositions for these three phthalates were also observed in infant cotton clothing and sanitary napkin samples (Li et al., 2019, Gao et al., 2019), indicating DEHP, DBP and DiBP are the most common phthalate plasticizers in the textiles and skin contacted products.
Fig. 3.
Composition of phthalates in mask samples (the level ratios of the phthalates were obtained by first calculating the ratios of the individual phthalate for each mask sample and then calculating the average level ratios of each phthalate in all the mask samples).
3.3. Estimation of phthalate exposure
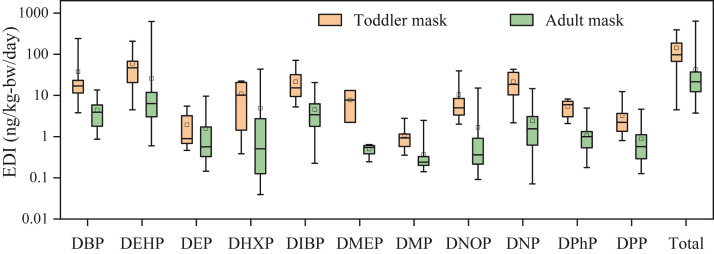
The estimated daily intakes (EDIs) of phthalates from the 56 masks were calculated and the results were listed in Table S5. The total EDIs of the 11 detected phthalates ranged from 3.71 ng/kg-bw/day to 639 ng/kg-bw/day, with a median value of 33.9 ng/kg-bw/day. Among the detected phthalates, DEHP had the highest contribution for the phthalates exposure accounting for 39.1% (mean value), followed by DiBP and DBP with mean contributions of 16.2% and 19.2%, respectively. Similar results for these three predominant phthalates were also observed in phthalate exposure from sanitary napkins (Gao et al., 2019). Fig. 4 showed the EDIs of the 11 detected phthalates in toddler and adult masks. The median EDIs of the phthalates in masks for the toddler were approximately 4–5 times higher than those for the adult. This can be explained by the two main influence factors for the EDI values (Eq. (1)). The weight and corresponding phthalate content of the adult masks were generally 2 times higher than those for the toddler masks. However, the body weight of the adults was much higher than that of the toddlers, leading to higher EDIs for the toddler group.
Fig. 4.
EDIs of phthalates in masks for adults and toddlers. The box plots show the 25th to the 75th percentiles of the data; upper and lower whiskers represent the 10th and 90th concentrations, respectively. The horizontal line within the box indicates the median value and the square indicates the mean value. The dot represents exception value.
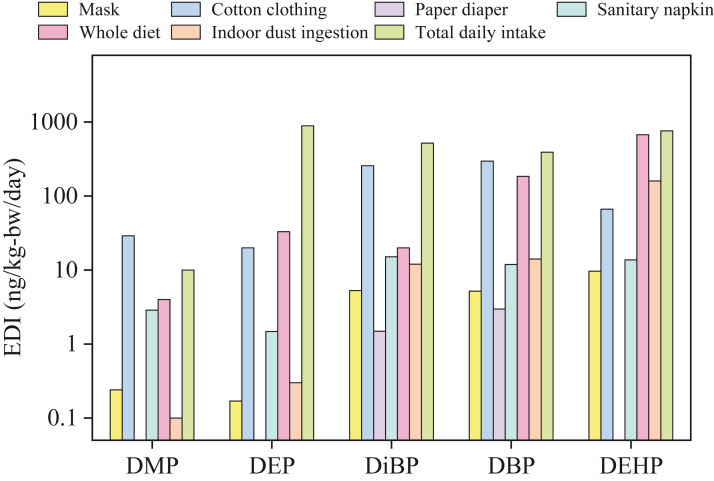
The EDIs of the five predominant phthalates (DMP, DEP, DiBP, DBP and DEHP) from the masks were compared with those from other pathways reported by previous studies ( Fig. 5 and Table S6) (Li et al., 2019, Ishii et al., 2015, Guo and Kannan, 2011, Schecter et al., 2013, Giovanoulis et al., 2018). For the four skin contacted products, the EDIs from the mask showed significant difference with those from sanitary napkin, paper diaper and cotton clothing. In detail, for DMP and DEP, the EDIs from the mask were approximately 10 times lower than those from the sanitary napkin, and much lower than those from the cotton clothing. For DiBP and DBP, the EDIs from the mask were approximately 2–3 times higher than those from the paper diaper, but 2–3 times lower than those from the sanitary napkin. The EDIs of DEHP from the mask were comparable with those from sanitary napkin, and about 2 orders of magnitude higher than those from paper diaper. Overall, the mask is a moderate phthalate exposure source comparing with other skin-contacted products. In addition, the median values of the EDIs from the mask were generally lower than those from indoor dust ingestion and diet, indicating phthalate exposure from the masks was lower than those from dust and food. The EDIs from the mask were also compared with the total daily intake of phthalates estimated by Giovanoulis et al. (2018). The EDIs (based on median values) of DMP, DEP, DiBP, DBP and DEHP represented 2.4%, 0.02%, 1.0%, 1.3% and 1.3%, respectively, of the total phthalate exposure. However, for the maximum EDI values, the five phthalates even accounted for 27.9%, 1.1%, 13.6%, 61.9% and 81.9%, respectively, of the total phthalate exposure, indicating the mask can be a non-negligible source of the phthalate exposure.
Fig. 5.
EDIs of phthalates from masks and other exposure pathways.
3.4. Risk assessment
The risks of the phthalate exposure to adults and toddlers were estimated respectively and the results were shown in Table S7. The median hazard index (HI) of the phthalate exposure to adults and toddlers were 7.08 × 10−4 and 3.92 × 10−3, respectively, which were both much lower than the safe value. Even the maximum HI values for the adult mask and toddler masks were 3.17 × 10−2 and 1.44 × 10−2, indicating the 11 detected phthalates in the masks were within the acceptable levels in terms of non-carcinogenic risks. Similar results were also found for other skin contacted products, such as sanitary napkin, paper diaper and cotton clothing (Li et al., 2019, Gao et al., 2019, Ishii et al., 2015).
According to previous studies, the CR value of 1 × 10−6 was regarded as an acceptable limit. As can be seen from Table S7, the cumulative CR values of phthalate exposure to adults and toddlers were in the range of 5.30 × 10−7 – 1.45 × 10−5 and 6.29 × 10−8 – 4.26 × 10−5, respectively. It should be noted that the cumulative CR values for 50 mask samples (accounting for 89.3% of the mask samples) were higher than 1 × 10−6, indicating their potential adverse effects to human health. Thus, the potential carcinogenic effects of phthalates from the mask should not be ignored.
4. Conclusion
In this study, the occurrence, exposure and risks of phthalates from face mask were investigated. Twelve phthalates were determined in 56 mask samples from different countries. The total concentrations of the phthalates in the masks ranged from 115 ng/g to 37,700 ng/g, with a median level of 1950 ng/g. Significance test showed that there was no significant difference for the phthalate concentrations in the masks from different countries. Based on the results of determination, the estimated daily intakes (EDIs) of phthalates from the masks were calculated with a median value of 33.9 ng/kg-bw/day. In addition, The EDIs of the phthalates from masks for toddlers were approximately 4–5 times higher than those for adults. In the risk assessment, the hazard index of phthalate exposure from all masks located in acceptable levels. However, 50 mask samples could exhibit carcinogenic risks to humans. The face mask has made a great contribution to the fighting against the epidemic and wearing masks will still last for a long time. This study convinced the face mask as a novel source of phthalate exposure. The results can be beneficial for awareness of management on additives in the face mask production.
CRediT authorship contribution statement
Huaijun Xie: Methodology, Investigation, Writing − original draft. Wenjing Han: Conceptualization, Supervision. Qing Xie: Data curation. Tong Xu: Writing − review & editing. Minghua Zhu: Writing − original draft. Jingwen Chen: Conceptualization, Project administration, Writing − review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
This study was supported by the National Key R&D Program of China (2018YFE0110700, 2018YFC1801604), the National Natural Science Foundation of China (No. 21661142001) and the China National Postdoctoral Program for Innovative Talents (BX20190053).
Editor: Dr. S. Nan
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.jhazmat.2021.126848.
Appendix A. Supplementary material
Supplementary material
.
References
- Aerts O., Dendooven E., Foubert K., Stappers S., Ulicki M., Lambert J. Surgical mask dermatitis caused by formaldehyde (releasers) during the COVID‐19 pandemic. Contact Dermat. 2020;2020:1–2. doi: 10.1111/cod.13626. [DOI] [PubMed] [Google Scholar]
- Aragaw T.A. Surgical face masks as a potential source for microplastic pollution in the COVID-19 scenario. Mar. Pollut. Bull. 2020;159 doi: 10.1016/j.marpolbul.2020.111517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatia R., Sindhuja T., Bhatia S., Dev T., Gupta A., Bajpai M., Gupta S. Iatrogenic dermatitis in times of COVID‐19: a pandemic within a pandemic. J. Eur. Acad. Dermatol. Venereol.: JEADV. 2020;34:563. doi: 10.1111/JDV.16710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornehag C.-G., Carlstedt F., Jönsson B.A., Lindh C.H., Jensen T.K., Bodin A., Jonsson C., Janson S., Swan S.H. Prenatal phthalate exposures and anogenital distance in Swedish boys. Environ. Health Perspect. 2015;123(1):101–107. doi: 10.1289/ehp.1408163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camargo M.C. d, Martinez-Silveira M.S., Lima A.A., Bastos B.P., Santos D.L. d, Mota S.E. d C., Silva R.B., Toledo I.P. d. Effectiveness of the use of non-woven face mask to prevent coronavirus infections in the general population: a rapid systematic review. Cienc. Saude coletiva. 2020;25:3365–3376. doi: 10.1590/1413-81232020259.13622020. [DOI] [PubMed] [Google Scholar]
- Cheng V.C., Wong S.-C., Chuang V.W., So S.Y., Chen J.H., Sridhar S., Chan K.K., Hung J.F., Ho I.F. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J. Infect. 2020;81:107–114. doi: 10.1016/j.jinf.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ECHA, 2013, Evaluation of new scientific evidence concerning DINP and DIDP in relation to Entry 52 of Annex XVII to Reach Regulation (EC) No. 1907/2006 (final review report).
- Fadare O.O., Okoffo E.D. Covid-19 face masks: a potential source of microplastic fibers in the environment. Sci. Total Environ. 2020;737 doi: 10.1016/j.scitotenv.2020.140279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao C.-J., Wang F., Shen H.-M., Kannan K., Guo Y. Feminine hygiene products—a neglected source of phthalate exposure in women. Environ. Sci. Technol. 2019;54(2):930–937. doi: 10.1021/acs.est.9b03927. [DOI] [PubMed] [Google Scholar]
- Giovanoulis G., Bui T., Xu F., Papadopoulou E., Padilla-Sanchez J.A., Covaci A., Haug L.S., Cousins A.P., Magnér J., Cousins I.T. Multi-pathway human exposure assessment of phthalate esters and DINCH. Environ. Int. 2018;112:115–126. doi: 10.1016/j.envint.2017.12.016. [DOI] [PubMed] [Google Scholar]
- Gong M., Weschler C.J., Zhang Y. Impact of clothing on dermal exposure to phthalates: observations and insights from sampling both skin and clothing. Environ. Sci. Technol. 2016;50(8):4350–4357. doi: 10.1021/acs.est.6b00113. [DOI] [PubMed] [Google Scholar]
- Guo Y., Kannan K. A survey of phthalates and parabens in personal care products from the United States and its implications for human exposure. Environ. Sci. Technol. 2013;47(24):14442–14449. doi: 10.1021/es4042034. [DOI] [PubMed] [Google Scholar]
- Guo Y., Kannan K. Comparative assessment of human exposure to phthalate esters from house dust in China and the United States. Environ. Sci. Technol. 2011;45(8):3788–3794. doi: 10.1021/es2002106. [DOI] [PubMed] [Google Scholar]
- Ishii S., Katagiri R., Minobe Y., Kuribara I., Wada T., Wada M., Imai S. Investigation of the amount of transdermal exposure of newborn babies to phthalates in paper diapers and certification of the safety of paper diapers. Regul. Toxicol. Pharmacol. 2015;73(1):85–92. doi: 10.1016/j.yrtph.2015.06.010. [DOI] [PubMed] [Google Scholar]
- Jung S., Lee S., Dou X., Kwon E.E. Valorization of disposable COVID-19 mask through the thermo-chemical process. Chem. Eng. J. (Lausanne, Switz.: 1996) 2021;405 doi: 10.1016/j.cej.2020.126658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kay V.R., Chambers C., Foster W.G. Reproductive and developmental effects of phthalate diesters in females. Crit. Rev. Toxicol. 2013;43(3):200–219. doi: 10.3109/10408444.2013.766149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H., Yanilmaz M., Toprakci O., Fu K., Zhang X. A review of recent developments in membrane separators for rechargeable lithium-ion batteries. Energy Environ. Sci. 2014;7(12):3857–3886. [Google Scholar]
- Li T., Liu Y., Li M., Qian X., Dai S.Y. Mask or no mask for COVID-19: a public health and market study. PloS One. 2020;15(8) doi: 10.1371/journal.pone.0237691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H.-L., Ma W.-L., Liu L.-Y., Zhang Z., Sverko E., Zhang Z.-F., Song W.-W., Sun Y., Li Y.-F. Phthalates in infant cotton clothing: occurrence and implications for human exposure. Sci. Total Environ. 2019;683:109–115. doi: 10.1016/j.scitotenv.2019.05.132. [DOI] [PubMed] [Google Scholar]
- Lukiw W.J., Pogue A., Hill J.M. SARS-CoV-2 infectivity and neurological targets in the brain. Cell. Mol. Neurobiol. 2020:1–8. doi: 10.1007/s10571-020-00947-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martino‐Andrade A.J., Chahoud I. Reproductive toxicity of phthalate esters. Mol. Nutr. Food Res. 2010;54(1):148–157. doi: 10.1002/mnfr.200800312. [DOI] [PubMed] [Google Scholar]
- Negev M., Berman T., Reicher S., Sadeh M., Ardi R., Shammai Y. Concentrations of trace metals, phthalates, bisphenol A and flame-retardants in toys and other children’s products in Israel. Chemosphere. 2018;192:217–224. doi: 10.1016/j.chemosphere.2017.10.132. [DOI] [PubMed] [Google Scholar]
- Net S., Sempéré R., Delmont A., Paluselli A., Ouddane B. Occurrence, fate, behavior and ecotoxicological state of phthalates in different environmental matrices. Environ. Sci. Technol. 2015;49(7):4019–4035. doi: 10.1021/es505233b. [DOI] [PubMed] [Google Scholar]
- Patricio Silva A.L., Prata J.C., Walker T.R., Duarte A.C., Ouyang W., Barcelo D., Rocha-Santos T. Increased plastic pollution due to COVID-19 pandemic: Challenges and recommendations. Chem. Eng. J. 2021;405 doi: 10.1016/j.cej.2020.126683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prather K.A., Marr L.C., Schooley R.T., McDiarmid M.A., Wilson M.E., Milton D.K. Airborne transmission of SARS-CoV-2. Science. 2020;370(6514):303–304. doi: 10.1126/science.abf0521. [DOI] [PubMed] [Google Scholar]
- Radke E.G., Braun J.M., Meeker J.D., Cooper G.S. Phthalate exposure and male reproductive outcomes: a systematic review of the human epidemiological evidence. Environ. Int. 2018;121:764–793. doi: 10.1016/j.envint.2018.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman M., Brazel C.S. The plasticizer market: an assessment of traditional plasticizers and research trends to meet new challenges. Prog. Polym. Sci. 2004;29(12):1223–1248. [Google Scholar]
- Rovira J., Domingo J.L. Human health risks due to exposure to inorganic and organic chemicals from textiles: a review. Environ. Res. 2019;168:62–69. doi: 10.1016/j.envres.2018.09.027. [DOI] [PubMed] [Google Scholar]
- Schecter A., Lorber M., Guo Y., Wu Q., Yun S.H., Kannan K., Hommel M., Imran N., Hynan L.S., Cheng D. Phthalate concentrations and dietary exposure from food purchased in New York State. Environ. Health Perspect. 2013;121(4):473–479. doi: 10.1289/ehp.1206367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang Z., Chai M., Cheng J., Wang Y., Huang Q. Occurrence and distribution of phthalates in sanitary napkins from six countries: implications for women’s health. Environ. Sci. Technol. 2019;53(23):13919–13928. doi: 10.1021/acs.est.9b03838. [DOI] [PubMed] [Google Scholar]
- Tang Z., Chai M., Wang Y., Cheng J. Phthalates in preschool children’s clothing manufactured in seven Asian countries: occurrence, profiles and potential health risks. J. Hazard. Mater. 2020;387 doi: 10.1016/j.jhazmat.2019.121681. [DOI] [PubMed] [Google Scholar]
- Vasquez-Bonilla W.O., Orozco R., Argueta V., Sierra M., Zambrano L.I., Muñoz-Lara F., López-Molina D.S., Arteaga-Livias K., Grimes Z., Bryce C. A review of the main histopathological findings in coronavirus disease 2019. Hum. Pathol. 2020;105:74–83. doi: 10.1016/j.humpath.2020.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vieira M.G.A., da Silva M.A., dos Santos L.O., Beppu M.M. Natural-based plasticizers and biopolymer films: a review. Eur. Polym. J. 2011;47(3):254–263. [Google Scholar]
- Wang Q., Ye X., Niu Z., Luo X., Li J. Determination of nine phthalate esters in pressure-sensitive adhesive and its products by high performance liquid chromatography–mass spectrometry. J. Instrum. Anal. 2011;30:720–726. [Google Scholar]
- WHO Coronavirus Disease (COVID-19) Dashboard. 〈https://covid19.who.int/〉 (accessed 3 March 2021).
- Xie Z., Yang Y.X., Zhang H. Mask‐induced contact dermatitis in handling COVID‐19 outbreak. Contact Dermat. 2020;2020:1–2. doi: 10.1111/cod.13599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yost E.E., Euling S.Y., Weaver J.A., Beverly B.E., Keshava N., Mudipalli A., Arzuaga X., Blessinger T., Dishaw L., Hotchkiss A. Hazards of diisobutyl phthalate (DIBP) exposure: a systematic review of animal toxicology studies. Environ. Int. 2019;125:579–594. doi: 10.1016/j.envint.2018.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang R., Li Y., Zhang A.L., Wang Y., Molina M.J. Identifying airborne transmission as the dominant route for the spread of COVID-19. Proc. Natl. Acad. Sci. 2020;117:14857–14863. doi: 10.1073/pnas.2009637117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material