Abstract
Aim
To identify the prevalence of mental health problems and sleep disturbances among nursing students during the COVID-19 pandemic.
Background
As a future professional workforce, nursing students are expected to play a role in controlling the COVID-19 pandemic; however, physical and mental health problems may hinder their willingness to stay in the nursing profession. Evidence of the prevalence of the health problems among nursing students related to COVID-19 may allow educators to manage their students’ health problems and make them feel more positive about their future careers.
Design
Systematic review and meta-analysis. This study was prospectively registered with PROSPERO.
Data sources
Databases, including CINAHL, Embase, PubMed and Web of Science, were searched for all related journal articles, from database inception to June 29, 2021, published between 2020 and 2021.
Methods
This review was conducted following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines using a PICOS search strategy. A DerSimonian–Laird random-effects model was used to estimate the prevalence and potential heterogeneity among the selected studies using the Cochran Q statistic and I-square test. Publication bias was assessed using the Egger intercept test.
Results
Seventeen studies were included in the meta-analysis, representing 13,247 nursing students. During the COVID-19 pandemic, the prevalence of four health problems and sleep disturbances were identified. The health problem with the highest prevalence in nursing students was depression (52%). Other COVID-19-related health problems were fear (41%), anxiety (32%) and stress (30%) and sleep disturbances (27%).
Conclusions
The findings from this study showed that strategies are necessary to manage nursing students’ teaching and learning during the COVID-19 pandemic or similar future situations. Our results suggest that preparing modified distance learning might reduce the prevalence of health problems related to the educational process. In addition, providing regular mental health assessments or online mental health services to students may improve their mental health and increase their well-being. Nursing education policies regarding clinical practice remain to be formulated to ensure the achievement of competencies to support future careers while considering the mental readiness and safety of students.
Keywords: Mental health problems, Sleep disturbances, Nursing students, Prevalence, Meta-analysis
1. Introduction
The coronavirus disease 2019 (COVID-19) has caused devastating effects by spreading rapidly throughout society worldwide since it was identified at the end of December 2019 in Wuhan City, China (Zhu et al., 2020). As of June 25, 2021, COVID-19 had been diagnosed in at least 179,686,071 individuals globally and was associated with 3899,172 deaths (World Heath Organization, 2021) and this number is increasing every day in most countries, with some even reaching their second or third wave of rising cases. As a result, nurses in the healthcare workforce face heavy workloads and high psychological stress due to the many cases and deaths. Furthermore, the negative psychological effects experienced by nurses may affect the mentality of nursing students (Heilferty et al., 2021, Swift et al., 2020).
Several policies were adopted to control the COVID-19 pandemic. Generally, to prevent and reduce the spread of COVID-19, a comprehensive approach was implemented in the early phase of the pandemic; this approach entailed limiting community activities and requiring home isolation, regional quarantine, social distancing, postponing of planned social and public events, restrictions on mass transit and travel restrictions (Atalan, 2020, Meo et al., 2020, Usher et al., 2020). Academic institutions’ concern about the COVID-19 pandemic led most universities worldwide to postpone or cancel all campus events, such as face-to-face teaching, workshops or conferences, sports and clinical practice (O'Flynn-Magee et al., 2021, Sahu, 2020, Viner et al., 2020). Furthermore, students have expressed concern that the interruption of their education would interfere with their competence and future career achievements (Dewart et al., 2020, O'Flynn-Magee et al., 2021). In addition to the impact of the COVID-19 pandemic itself, policies and measures aimed at preventing large gatherings of people, both in general and in academic settings, need to be considered in terms of their impact on mental health.
Nursing students across the world have experienced mental health problems as a result of the COVID-19 pandemic. The impact of COVID-19 goes beyond the most fundamental aspects of daily life, such as sleep patterns (Brouwer et al., 2021, Gol and Erkin, 2021). For example, a study from Turkey found that nursing students reported high levels of anxiety and fear due to COVID‐19. Their anxiety levels increased because of the strict implementation of lockdowns and having family members or relatives who tested positive for COVID‐19 (Alici and Copur, 2021). In addition, a study from the Philippines explained that nursing students who feared COVID‐19 experienced poor sleep quality and developed the intention to leave nursing school. The fear of COVID-19 that the students experienced was due to the current high-risk environment, which requires high self-sacrifice in the nursing profession, whereas the intention to quit nursing school was caused by a lack of basic knowledge, skills in nursing and a lack of maturity in professional values (De Los Santos et al., 2021). Moreover, a study from the USA found that during a lockdown, nursing students reported higher stress, anxiety and depression (Kim et al., 2021).
The sequelae from the COVID-19 pandemic affected nursing students’ mental health problems and sleep, putting them at high risk of contracting COVID-19, especially during clinical practice and altering their academic achievements (Okwuikpo et al., 2021, Tomietto et al., 2020). Nursing schools adopted various regulations to reduce these issues. Some institutions temporarily closed the university and delayed clinical practicums (Joob and Wiwanitkit, 2020, O'Flynn-Magee et al., 2021, Rothstein and Olympia, 2020). However, such regulations were found to have additional impacts on student achievements. According to a survey from the International Council of Nurses (ICN), the delay in clinical practice has affected nursing students’ academic achievements and delayed their graduations (ICN, 2021). Other challenges arise when clinical practices reopen. For instance, previous studies reported that the implementation of clinical practice during the COVID-19 period experienced many challenges because the current situation required nurses’ energy and thoughts to be devoted to dealing with COVID-19, which burdened them and prevented them from guiding students properly (Franzoi and Cauduro, 2020, ICN, 2021, Okwuikpo et al., 2021). Therefore, it is necessary to carefully mitigate the potential risk of nursing students contracting COVID-19 during their clinical practicum (Alshutwi, 2021, Dewart et al., 2020, Swift et al., 2020).
Although, in general, all nurses are experiencing the same COVID-related stresses, evidence suggests that the youngest nurses have more difficulty coping with this situation (Sherman, 2021). Younger nurses represent the future workforce of nursing professionals, especially those who belong to Generation Z, defined as individuals born between 1995 and 2010 (Seemiller and Grace, 2017) and studies suggest that they have experienced difficulties during the COVID-19 pandemic (Sherman, 2021). Younger nurses self-reported high levels of stress, anxiety and depression during the COVID-19 pandemic (Czeisler et al., 2020, Kim et al., 2021), which may be associated with a lack of experience with adversity and a general aversion to risks and adverse events. Furthermore, Generation Z students how been found to have lower resilience compared with other generations (Ang et al., 2021). Building the resilience of nursing students is important to maintain their mental and psychological health during the COVID-19 pandemic (Labrague, 2021).
As mental health problems and sleep disturbances have been identified in previous studies, the prevalence of these problems may be of interest to educators. Understanding these issues is necessary because nursing students are expected to play a larger role in the current crisis than laypeople by volunteering, educating the public and increasing awareness of the COVID-19 pandemic (Mustafa et al., 2020, Sun et al., 2020). Previous research from before the COVID-19 pandemic reported that the prevalence of depression among nursing students was 34.0% (Tung et al., 2018). Another meta-analysis of university students during the COVID-19 pandemic found that the prevalence of anxiety was 31% and depression was 34% (Chang et al., 2021), but these results are likely different in the case of nursing students during COVID-19. Therefore, systematically synthesizing all the available evidence to estimate its prevalence is warranted. Thus, this systematic meta-analysis aimed to identify the prevalence of mental health problems and sleep disturbances among nursing students during the COVID-19 pandemic.
2. Methods
2.1. Design
This study was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Page et al., 2021). The study was registered with the International Prospective Register of Systematic Reviews (PROSPERO: CRDxxxxxxxxxxx).
2.2. Eligibility criteria
The inclusion criteria were determined according to the PICOS method (population, issue of interest, comparison, outcome and study design) (Amir-Behghadami and Janati, 2020). The population (P) was nursing students; the issue of interest (I) was the COVID-19 pandemic; the outcomes (O) were the prevalence of mental health problems and sleep disturbances; and the study designs (S) were cohort studies, case-control studies, or cross-sectional studies. Additional inclusion criteria applied were study participants were nursing students, studies reported the number (%) of cases, full-text articles were available and articles were published in the English or Indonesian language. Studies were excluded if the study population comprised a mix of nursing students and other health professional students ( Table 1).
Table 1.
Inclusion and exclusion criteria.
| Inclusion criteria | Exclusion criteria |
|---|---|
| Participants consisting of only nursing students. The study designs were cohort studies, case-control studies, or cross-sectional studies. Studies that reported the number (%) of cases. Full text articles Published in English or Indonesian language |
Participants do not consist of nursing students but comprised a mix of nursing students and other health professional students. Other types of studies such as experimental study. Studies that not reported number (%) of cases, such as mean, median. Articles that were not peer-reviewed, such as theses. Articles that were not in English or Indonesian. |
2.3. Search strategy
To identify relevant studies, four databases were accessed through various vendors (EBSCO: CINAHL, Elsevier: Embase, National Institute of Health [NIH]: PubMed and Clarivate Analytics: Web of Science) and searched from June 23 to June 29, 2021. This literature search was performed with the aid of a librarian and included studies published between1 January 2020 and 29 June 2021. The search strategies, including all identified keywords (nursing students, mental health problems, fear, depression, anxiety, post-traumatic stress disorder (PTSD), sleep disturbances and COVID-19) and index terms, were adapted for each database. The detailed search strategy is described in.
2.4. Study screening and selection
All studies identified by the search strategy were imported into Endnote X9 to identify and remove duplicate studies. Two reviewers (MM and SIT) screened all titles and abstracts of the remaining studies and assessed the full-text articles for eligibility criteria. Any disagreements were discussed and resolved by a third reviewer (BOL).
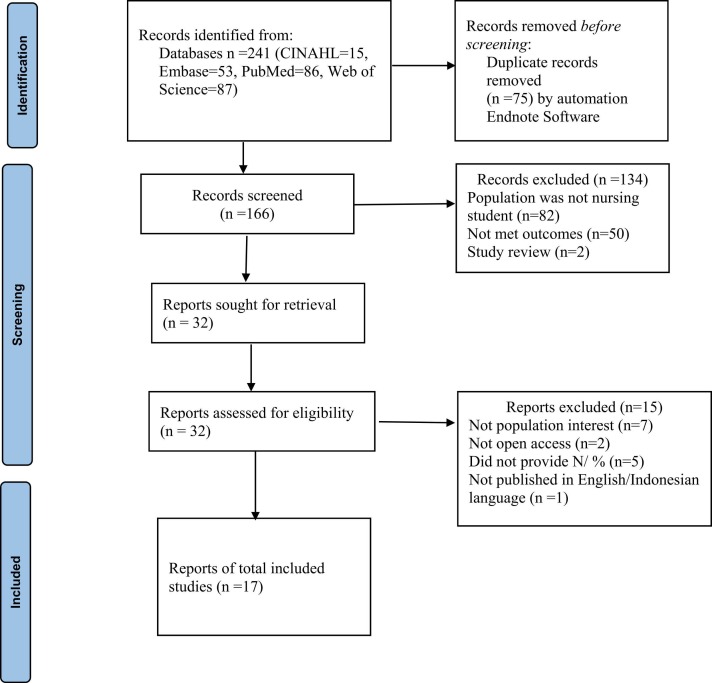
The initial search of the four databases yielded 241 articles. After importing all studies into EndNote X9 software, 75 studies were identified as duplicates and excluded. The titles and abstracts of 166 articles were screened and 134 articles were excluded for various reasons: 82 articles were excluded because the population was not nursing students, 50 studies did not report mental health problems or sleep disturbances and two studies were literature reviews. After the initial title and abstract screening, a total of 32 full-text articles were screened for eligibility. During eligibility screening, 15 articles were removed: seven articles were removed because they did not include the population of interest, two articles were not open-access, five articles did not provide N (%) and one study was not published in English or Indonesian. Thus, 17 articles were included in our final analysis ( Fig. 1).
Fig. 1.
PRISMA Diagram – process of study selection.
2.5. Data abstraction and quality appraisal
Two reviewers (MM, SIT) performed comprehensive data extraction from each study based on the inclusion criteria. Prevalence was defined as the total number of nursing students with mental health problems and sleep disturbances during the COVID-19 pandemic divided by the total population (Spronk et al., 2019). The extracted data included the author, year of the study, the country where the study was conducted, study design, total population, age, sex, students’ degree, time of data collection, fear cases, depression cases, anxiety cases, stress cases, PTSD cases, sleep disturbance cases and measurements. All discrepancies during the data extraction process were discussed and the final decision was made by the third reviewer.
Two reviewers (MM, SIT) independently performed quality appraisals using the tool developed by the Joanna Briggs Institute (JBI) (The Joanna Briggs Institute, 2017). This study applied the eight-question JBI tool for cross-sectional studies. Each item was scored between 0 (high risk of bias) and 1 (low risk of bias) and a score of ≤ 4 was categorized as low quality, whereas a score of > 4 indicated high quality ( Table 3). All differences of opinion were resolved by deliberation until consensus was reached or resolved by the decision of a third reviewer. The results of the discussion were used as the final results for the quality appraisal of the included studies.
Table 3.
Quality assessment of cross-sectional studies.
| No | JBI checklist question | Cici and Yilmazel (2021) | Dalcali et al. (2021) | Deo et al. (2020) | Fitzgerald and Konrad (2021) | Gol and Erkin (2021) | Kalkan Uğurlu et al. (2021) | Kochuvilayil et al. (2021) |
|---|---|---|---|---|---|---|---|---|
| 1 | Were the criteria for inclusion in the sample clearly defined? | Y | N | Y | Y | Y | Y | Y |
| 2 | Were the study subjects and the setting described in detail? | Y | Y | Y | Y | Y | Y | Y |
| 3 | Was the exposure measured in a valid and reliable way? | Y | Y | Y | Y | Y | Y | Y |
| 4 | Were objective standard criteria used for measurement of the condition? | Y | Y | Y | Y | Y | Y | Y |
| 5 | Were confounding factors identified? | N | N | N | N | N | N | N |
| 6 | Were strategies to deal with confounding factors stated? | N | N | N | N | N | N | N |
| 7 | Were the outcomes measured in a valid and reliable way? | Y | Y | Y | Y | Y | Y | Y |
| 8 | Was appropriate statistical analysis used? | Y | Y | Y | Y | Y | Y | Y |
| Overall Appraisal | Include: 6 | Include: 5 | Include: 6 | Include: 6 | Include: 6 | Include: 6 | Include: 6 | |
| Exclude: 2 | Exclude: 3 | Exclude: 2 | Exclude: 2 | Exclude: 2 | Exclude: 2 | Exclude: 2 | ||
| Level of evidence | 4.c case series | 4.c case series | 4.c case series | 4.c case series | 4.c case series | 4.c case series | 4.c case series | |
| No | JBI checklist question | Kusuma et al. (2021) | Li et al., 2021a, Li et al., 2021b | Mundakir et al. (2021) | Rosenthal et al. (2021) | Santoso et al. (2020) | Savitsky et al. (2021) | Sun et al. (2020) |
| 1 | Were the criteria for inclusion in the sample clearly defined? | N | Y | Y | N | N | N | Y |
| 2 | Were the study subjects and the setting described in detail? | Y | Y | Y | Y | Y | Y | Y |
| 3 | Was the exposure measured in a valid and reliable way? | Y | Y | Y | Y | Y | Y | Y |
| 4 | Were objective standard criteria used for measurement of the condition? | Y | Y | Y | Y | Y | Y | Y |
| 5 | Were confounding factors identified? | N | Y | N | N | N | Y | Y |
| 6 | Were strategies to deal with confounding factors stated? | N | N | N | N | N | Y | Y |
| 7 | Were the outcomes measured in a valid and reliable way? | Y | Y | Y | Y | Y | Y | Y |
| 8 | Was appropriate statistical analysis used? | Y | Y | Y | Y | Y | Y | Y |
| Overall Appraisal | Include: 5 | Include: 7 | Include: 6 | Include: 5 | Include: 5 | Include: 7 | Include: 8 | |
| Exclude: 3 | Exclude: 1 | Exclude: 2 | Exclude: 3 | Exclude: 3 | Exclude: 1 | Exclude: 0 | ||
| Level of evidence | 4.c case series | 4.c case series | 4.c case series | 4.c case series | 4.c case series | 4.c case series | 4.c case series | |
| No | JBI checklist question | Turan et al. (2021) | Vitale et al. (2020) | Zhu et al. (2021) | ||||
| 1 | Were the criteria for inclusion in the sample clearly defined? | N | Y | N | ||||
| 2 | Were the study subjects and the setting described in detail? | Y | Y | Y | ||||
| 3 | Was the exposure measured in a valid and reliable way? | Y | Y | Y | ||||
| 4 | Were objective standard criteria used for measurement of the condition? | Y | Y | Y | ||||
| 5 | Were confounding factors identified? | N | N | Y | ||||
| 6 | Were strategies to deal with confounding factors stated? | N | N | Y | ||||
| 7 | Were the outcomes measured in a valid and reliable way? | Y | Y | Y | ||||
| 8 | Was appropriate statistical analysis used? | Y | Y | Y | ||||
| Overall Appraisal | Include: 5 | Include: 6 | Include: 7 | |||||
| Exclude: 3 | Exclude: 2 | Exclude: 1 | ||||||
| Level of evidence | 4.c case series | 4.c case series | 4.c case series | |||||
Yes: 1, No= 0
2.6. Statistical analysis
Comprehensive Meta-Analysis® Software Version 3.3 was used for all analyses (Biostat, Englewood, NJ, USA). The DerSimonian–Laird random-effects model was used to estimate the prevalence of mental health and sleep disturbances among nursing students with a 95% confidence interval (CI) (Borenstein et al., 2010). The potential heterogeneity among the selected studies was assessed using Cochrane Q statistic and I-square (I 2) test. Considerable heterogeneity was considered to be present if the Cochran Q and I 2 values were < 0.05 and at least 50%, respectively (Borenstein et al., 2017). To assess the robustness of the initial results, sensitivity analyses were carried out by removing the study with the greatest weighting in the pooled analysis. Publication bias was assessed by the Egger intercept test and a p-value of < 0.05 indicated statistically significant publication bias (Sterne and Egger, 2001, Sterne et al., 2000).
3. Results
3.1. Study characteristics
Studies were published between 2020 and 2021 and a total of 17 studies had cross-sectional designs. Five studies were conducted in Turkey (Cici and Yilmazel, 2021, Dalcali et al., 2021, Gol and Erkin, 2021, Kalkan Uğurlu et al., 2021, Turan et al., 2021), three studies were conducted in China (D. Li et al., 2021b; Sun et al., 2020; Zhu et al., 2021), three studies were conducted in Indonesia (Kusuma et al., 2021, Mundakir et al., 2021, Santoso et al., 2020), two studies were conducted in the USA (Fitzgerald and Konrad, 2021, Rosenthal et al., 2021), one study was conducted in Israel (Savitsky et al., 2021), one study was conducted in Italy (Vitale et al., 2020), one study was conducted in Nepal (Deo et al., 2020) and one study was conducted in both India and Australia (Kochuvilayil et al., 2021).
A total of 13,247 nursing students were enrolled across the 17 studies, 80.90% of whom were women. The various mental health problems and sleep disturbances among nursing students across studies were as follows: 10 studies reported anxiety, eight studies reported depression, three studies reported stress, three studies reported fear, one study reported PTSD and five studies reported sleep disturbances. The ranges of the prevalence of mental health problems were as follows: anxiety, 6–54.97%; depression, 22.28–81.40%; stress, 6.52–63.74%, fear, 11.7–70%; and sleep disturbances, 4.4–52.71%. The included studies are summarized in Table 2.
Table 2.
Summary of selected studies on mental health problems, and sleep disturbances in nursing students during COVID-19 pandemic.
| Author, Year/Country | Sample size | Age | Female N (%) | Data collection (as of Deo 2019) | Mental health problems & Sleep disturbances (N/%) |
Measurement | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Fear N/% | Anxiety N/% | Stress N/% | Depression N/% | PTSD N/% | Sleep Disturbances N/% | ||||||
| Cici and Yilmazel (2021)/Turkey | 233 | 20.8 | 178/76.4 | <3 Month | 203/63.04 | The survey questions | |||||
| Dalcali et al. (2021)/Turkey | 283 | 20.39 | 232/82.0 | 3–6 Month | 33/11.7 | 147/51.9 | 80/28.26 | The survey questions, STAI, VAS | |||
| Deo et al. (2020)/Nepal | 184 | 20–22 | NA | 3–6 Month | 52/28.26 | 12/6.52 | 41/22.28 | 97/52.71 | DASS,ISI | ||
| Fitzgerald and Konrad (2021)/USA | 50 | 18–21 | 42/84 | ≥6 Month | 30/70 | 16/32 | The survey questions | ||||
| Gol and Erkin (2021)/Turkey | 2.630 | 21.30 | 2.159/82.1 | 3–6 Month | 450/17.1 | The survey questions | |||||
| Kalkan Uğurlu et al. (2021)/Turkey | 411 | 20.60 | 326/79.3 | 3–6 Month | 209/50.85 | 262/63.74 | 228/55.47 | DASS 42 | |||
| Kochuvilayil et al. (2021)/Australia (A)&India (I) | A: 99 I: 113 |
A: 20.01 I: 20.2 |
191/90 | – | A:45 (46.4) I: 5 (4.4) |
The survey questions | |||||
| Kusuma et al. (2021)/Indonesia | 235 | NA | 209/88.9 | – | 166/70.63 | The PHQ-9 | |||||
| Li et al., 2021a, Li et al., 2021b/China | 6.348 | NA | 5.737/90.37 | <3 Month | 2.220/34.97 | 2.553/40.22 | 950/14.97 | The GAD-7, The PHQ-9, The PCL-C |
|||
| Mundakir et al. (2021)/Indonesia | 619 | 20–60 | 510/82.4 | – | 37/6.0 | The survey questions | |||||
| Rosenthal et al. (2021)/USA | 222 | NA | NA | 3–6 Month | 63/28.37 | 83/37.38 | 82/36.93 | The DASS-21 | |||
| Santoso et al. (2020)/Indonesia | 148 | 18–20 | NA | – | 70/47.29 | The BDI II | |||||
| Savitsky et al. (2021)/Israel | 215 | NA | NA | <3 Month | 92/42.8% | The GAD-7 | |||||
| Sun et al. (2020)/China | 474 | 20–22 | 402/84.8 | <3 Month | 59/12.44 | The SAS | |||||
| Turan et al. (2021)/Turkey | 456 | 21.09 | 366/80.3 | 3–6 Month | 197/43.2 | The Anxiety Scale. | |||||
| Vitale et al. (2020)/Italy | 285 | 21–30 | 245/85.97 | <3 Month | 232/81.40 | The PHQ-9 | |||||
| Zhu et al. (2021)/China | 342 | 20.73 | 297/86.8 | <3 Month | 188/54.97 | 193/56.43 | The GAD-7, The PHQ-9 | ||||
Visual Analog Sleep (VAS) Scale, State‐trait anxiety inventory (STAI), Depression Anxiety and Stress Scale (DASS), Generalized Anxiety Disorder 7-Item Scale (GAD-7), Patient Health Questionnaire 9-Item Scale (PHQ-9), Post Traumatic Stress Disorder Check List – Civilian version (PCL-C), Self-rating Anxiety Scale (SAS), Patient Health Questionnaire-9, (PHQ-9), Depression, anxiety, and stress scale (DASS-21), Insomnia Severity Index (ISI), Beck Depression Inventory-II (BDI-II)
3.2. Risk of bias
The assessment of studies’ risk of bias using the JBI tool for cross-sectional studies reported a score of 8 out of 8 in one study (Sun et al., 2020), 7 out of 8 in three studies (D. Li et al., 2021b; Savitsky et al., 2021; Zhu et al., 2021), 6 out of 8 in eight studies (Cici and Yilmazel, 2021, Deo et al., 2020, Fitzgerald and Konrad, 2021, Gol and Erkin, 2021, Kalkan Uğurlu et al., 2021, Kochuvilayil et al., 2021, Mundakir et al., 2021, Vitale et al., 2020) and 5 out of 8 in five studies (Dalcali et al., 2021, Kusuma et al., 2021, Rosenthal et al., 2021, Santoso et al., 2020, Turan et al., 2021). All scores in this study were > 4 points, which indicated a low risk of bias. In general, all included studies had a low risk of bias, although we identified some concerns for risk of bias due to identified confounding factors and strategies to deal with confounding factors (Table 3).
3.3. Prevalence and types of mental health problems and sleep disturbances
3.3.1. Anxiety
Ten studies involving 9554 students were included to estimate the prevalence of anxiety during the COVID-19 pandemic. The studies were assessed using the State-Trait Anxiety Inventory (STAI), the Depression Anxiety and Stress Scale (DASS), the Generalized Anxiety Disturbances 7-Item Scale (GAD-7), the Self-Rating Anxiety Scale (SAS), the Self-Developed Anxiety Scale and survey questions. The pooled prevalence of anxiety determined by the random-effects model was 32% (95% CI: 0.24–0.42) and there was considerable heterogeneity (Q = 409.68, degrees of freedom (df) = 9, p < 0.001, I 2 = 98%) ( Fig. 2). This result reveals that approximately one-third of the nursing students enrolled in the included studies experienced anxiety during the COVID-19 pandemic.
Fig. 2.
Proportion of anxiety, depression, stress, fear, and sleep disturbances in nursing students during COVID-19 pandemic.
3.3.2. Depression
Eight studies enrolling 8175 students were assessed to estimate the prevalence of depression during the COVID-19 pandemic. The studies were assessed using the DASS, the Patient Health Questionnaire-9 (PHQ-9) and the Beck Depression Inventory-II (BDI-II). The pooled prevalence of depression determined by the random-effects model was 52% (95% CI: 0.40–0.63) and there was considerable heterogeneity (Q = 303.20, df = 7, p < 0.001, I 2 = 98%) (Fig. 2). This result indicates that half of the nursing students in the included studies developed depression during the COVID-19 pandemic.
3.3.3. Stress
Three studies involving 817 students were included to estimate the prevalence of stress during the COVID-19 pandemic. All three studies assessed used the DASS. The pooled prevalence of stress determined by the random-effects model was 30% (95% CI: 0.10– 0.63) and there was a considerable heterogeneity (Q = 123.54, df= 2, p < 0.001, I 2 = 98%) (Fig. 2). This result suggests that one-third of the nursing students in the included studies experienced stress during the COVID-19 pandemic.
3.3.4. Fear
Three studies involving 817 students were included to estimate the prevalence of stress during the COVID-19 pandemic. All three studies assessed used survey questions. The pooled prevalence of stress determined by the random-effects model was 41% (95% CI: 0.11–0.80) and there was considerable heterogeneity (Q = 141.20, df = 2, p < 0.001, I 2 = 98%) (Fig. 2). This result demonstrates that almost half of the nursing students in the included studies experienced fear during the COVID-19 pandemic.
3.3.5. Post-traumatic stress disorder
Only one study reported the prevalence of PTSD among nursing students during the COVID-19 pandemic. This study assessed PTSD using the Post-Traumatic Stress Disorder Checklist—Civilian Version (PCL-C). Since only one study reporting this outcome was identified, the pooled prevalence could not be calculated. Instead, the prevalence of PTSD was narratively reported. This study, which included 6348 nursing students, reported that 15% (95% CI: 0.14–0.16) developed PTSD during the COVID-19 pandemic.
3.3.6. Sleep disturbances
Six studies that included a total of 3359 students were included to estimate the prevalence of sleep disturbances during the COVID-19 pandemic. The studies assessed the Visual Analog Sleep (VAS) Scale, the Insomnia Severity Index (ISI) and survey questions. The pooled prevalence of sleep disturbances determined by the random-effects model was 27% (95% CI: 0.15–0.43) and there was considerable heterogeneity (Q = 176.45, df = 5, p < 0.001, I 2 = 97%) (Fig. 2). This result indicates that approximately a quarter of the nursing students in the included studies developed sleep disturbances during the COVID-19 pandemic.
3.3.7. Publication bias
The assessment of publication bias using Egger’s regression intercept test indicated no significant publication bias for anxiety (intercept = −0.97, t = 0.27, p = 0.79), depression (intercept= 4.89, t = 1.58, p = 0.16), stress (intercept= −17.13, t = 3.79, p = 0.16), fear (intercept = –7.79, t = 0.42, p = 0.74), or sleep disturbances (intercept = 4.40, t = 1.14, p = 0.31).
3.3.8. Sensitivity analysis
The robustness of principal findings was confirmed by removing the study with the highest weight. The pooled prevalence of anxiety was decreased to 32% (95% CI: 0.21– 0.46) when the study by Li et al., 2021a, Li et al., 2021b was removed. When the study by Deo et al. (2020) was excluded, the pooled prevalence of sleep disturbances was elevated to 23% (95% CI: 0.14–0.36). In sum, removing the study with the highest weight did not significantly impact the overall results.
4. Discussion
This study aimed to identify the prevalence of mental health problems and sleep disturbances among nursing students during the COVID-19 pandemic. The pooled prevalences for anxiety, depression, stress, fear and sleep disturbances were 32%, 52%, 30%, 41% and 27%, respectively. Although most data collection was conducted six months after the initial outbreak of COVID-19, many countries are still struggling against the disease. Mental health problems during the COVID-19 pandemic can reduce motivation and concentration, introduce difficulties in the learning process, reduce learning quality and reduce student academic achievement (Alici and Copur, 2021, Lovrić et al., 2020). In addition to having an impact on educational performance, mental health issues can affect an individual’s clinical practice and subsequent quality of life (Mohamed Sanad, 2019). Nevertheless, the findings from this study should encourage nursing schools to provide approaches that improve mental health and sleep quality and mitigate the students’ vulnerability to these health problems.
Educational stakeholders may need to focus on increasing the availability of software and computer equipment and associated distanced learning policies to help nursing students cope with the consequences of COVID-19. First, educational adaptations during the COVID-19 pandemic have included a shift from face-to-face learning to online or flexible learning paradigms (O'Flynn-Magee et al., 2021, Pokhrel and Chhetri, 2021, Sahu, 2020). Studies have found that students face additional learning challenges when adjusting to these different learning modalities (Dewart et al., 2020, Majrashi et al., 2021, Wallace et al., 2021), including internet problems, technological issues, the absence of experimental/practical classes and reduced interactions with peers and educators (W. Li et al., 2021a; Thapa et al., 2021). Faculty members required more time to prepare for online classes and were forced to learn how to navigate and deliver the course content online (Agu et al., 2021, Almahasees et al., 2021). A lack of interactions between nursing educators and students added to the difficulties administering online courses and holding students’ attention, resulting in variable outcomes for classroom management and students’ learning (Agu et al., 2021, Almahasees et al., 2021, Lynn and Ward-Smith, 2021). Educational stakeholders may require collaborations with the government to improve the online teaching infrastructure, support student readiness to learn and provide technology training for educators in how to effectively deliver online education (Almahasees et al., 2021, Farsi et al., 2021, Pokhrel and Chhetri, 2021).
Second, online learning cannot replace clinical practice placements, which are necessary for skills development (Agu et al., 2021, Aslan and Pekince, 2021). Policies regarding the replacement of clinical experience with simulations have been trialed in developing countries, tailored to help nursing students cope, adapt and recover as quickly as possible in times of crisis (Agu et al., 2021). The use of simulations is also viewed positively by the newer generation of students, who have expressed a preference for using technology-based simulations as a learning component (Mulyadi et al., 2021, Palancia Esposito and Sullivan, 2020, Shea and Rovera, 2021). Stakeholders involved in nursing education should develop policies related to multiple pedagogies, including online teaching and clinical practice placements.
When implementing clinical practice during a pandemic, some essential aspects should be considered, such as the mental resilience of nursing students and the ability to protect their health through available vaccines and protective equipment, in addition to potential changes in the teaching methods used by educators (Kregar Velikonja et al., 2021, Labrague, 2021, Manning et al., 2021). Coordination with stakeholders in the field of practice is also essential, including their readiness to accept students, their ability to provide a healthy learning environment and the readiness of human resources to guide the practice of nursing students (Hernández-Martínez et al., 2021, Okwuikpo et al., 2021). The results of the current review are important and can influence policy-making by both academic institutions and stakeholders regarding the delivery of nursing education and clinical practice.
The pooled prevalence from ten studies indicated that approximately one-third (32%) of nursing students experienced anxiety during the COVID-19 pandemic. This percentage was higher than that determined by a previous meta-analysis of medical students, which reported an anxiety prevalence of 28% based on eight studies (Lasheras et al., 2020). Anxiety among nursing students was related to several factors, including the changing situations and living conditions during the COVID-19 pandemic, social isolation, economic instability, risk of infection, the incidence of COVID-19 infection in students’ families or friends and challenges related to technical problems of distance learning (Alici and Copur, 2021, Savitsky et al., 2020). Another factor related to anxiety in terms of academic achievement is the clinical practicum. Clinical practicum requires nursing students to be in direct contact with patients and because students expressed concerns about the transmission of the COVID-19 virus and the unpredictable situation of the COVID-19 pandemic, this condition endangers their mental health (Kim et al., 2021). Furthermore, a study reported that higher anxiety levels during COVID-19 tend to be reported by students who perceive the nursing profession as a high-risk profession (Turan et al., 2021). Thus, understanding student anxiety, providing assistance and encouraging students to continue to pursue the nursing profession is vital because the profession will always need nurses during critical situations, such as disasters, epidemics, or pandemics (Al Harthi et al., 2020, Turan et al., 2021). This implies that nursing students should learn appropriate coping skills and educators should prepare quality online education to meet student needs and implement strategies to improve students’ mental health (Alici and Copur, 2021, Bdair, 2021; Li et al., 2021a).
The results drawn from eight studies indicated that approximately half (52%) of nursing students developed depression during the COVID-19 pandemic. This prevalence was higher than that of a previous study, which found a 34% prevalence of depression among nursing students before the COVID-19 pandemic (Tung et al., 2018). Before the COVID-19 pandemic, the mental health problems of nursing students were triggered by a competitive educational environment among students, along with expectations from parents and the students themselves for educational achievement. During the COVID-19 pandemic, nursing students’ depression was triggered by disruption of study plans, restrictions on student activities and sudden changes in learning methods (Zhu et al., 2021). Existing evidence has noted that depressive thoughts during COVID-19 occur because of temporary restrictions on individual freedom, increased social distancing, social isolation, lack of exercise and spending large amounts of time at home (Kalkan Uğurlu et al., 2021; Li et al., 2021b; Qiu et al., 2020). Furthermore, individuals who are separated from their families and social lives tend to have higher depression scores (Ustun, 2021), whereas depression decreases when people are around (Kalkan Uğurlu et al., 2021). Because of the nature of nursing school, nursing students may not live with their families; instead, they may live in boarding houses and are thus prone to depression. Therefore, the role of nursing schools is crucial in recognizing the risk of depression and preparing appropriate psychological interventions for students who experience social restrictions, regardless of whether they are isolated at home or in boarding houses (Li et al., 2021b).
Approximately one-third (30%) of nursing students experience stress during the COVID-19 pandemic. This prevalence is lower than that of a previous study, which reported a stress prevalence of 48.1% among Chinese people (Bareeqa et al., 2021). A possible explanation for the lower prevalence observed in the present study may be that several studies in our meta-analysis were conducted in other countries, whereas China previously experienced a major impact from the COVID-19 outbreak. However, stress among nursing students remains a concern because it can have an impact on students’ health and future careers (Huang et al., 2020). Some findings from this study may be valuable and warrant discussion. First, Deo et al. (2020) found that approximately 6.52% of students experienced increased stress when hearing the news or reading information related to increased COVID-19 cases. In addition, other studies found that younger nursing students reported higher stress levels (Aslan and Pekince, 2021), which represents a particular concern among students belonging to Generation Z, who are known to be social media enthusiasts (Vizcaya-Moreno and Pérez-Cañaveras, 2020). Effective supervision and sharing suitable information sources regarding COVID-19 through social media are also expected to reduce stress. Second, Kalkan Uğurlu et al. (2021) argued that 63.74% of students felt mild to moderate stress because of the data collection conducted in the first five months of the pandemic and under temporary quarantine. Third, this study focused on the academic field, where the COVID-19 pandemic resulted in the inability to continue with the clinical experience required for students to graduate on time (Rosenthal et al., 2021). Thus, early recognition of mental health problems among nursing students is crucial because these health problems may worsen during the pandemic.
This study suggested that almost half of nursing students (41%) experienced fear during the COVID-19 pandemic. The explanation for this may be that the COVID-19 pandemic is perceived to be a prominent source of fear among students because of its rapid transmission, the growing number of infected people, deaths from COVID-19, distrust of the health system and disinformation about COVID-19 (Muller et al., 2021, Rodriguez-Hidalgo et al., 2020). In this review, three included studies found that nursing students were afraid of being infected with COVID-19 (Cici and Yilmazel, 2021, Dalcali et al., 2021, Fitzgerald and Konrad, 2021); however, all studies used survey questionnaires that may have been brief and yielded biased responses. Furthermore, some conditions, such as financial instability, the health of nursing students’ friends and family and the death of a friend due to COVID-19, can increase students’ fears (Fitzgerald and Konrad, 2021). Thus, nursing educators must be aware of students’ needs for mental assessment; providing appropriate information about COVID-19 and facilitating mental services are highly recommended.
Only one study assessed PTSD and revealed a prevalence of 14.97% among nursing students. Despite the relatively small number of studies, potential trauma in nursing students may be due to students’ concern for themselves and their families, along with their future careers, in light of the COVID-19 pandemic (Fowler and Wholeben, 2020). Therefore, nursing educators play a key role in maximizing individual student coping and preparing psychological interventions to reduce the risk of PTSD.
Another adverse psychological impact on nursing students was sleep disturbances. Approximately a quarter (27%) of nursing students suffered from sleep disturbances during COVID-19. The present study revealed a lower prevalence of sleep disturbances than a previous meta-analysis of healthcare professionals, which reported a sleep disturbance prevalence of 31% and a higher prevalence than a general population study, which reported a prevalence of 18% (Alimoradi et al., 2021). Sleep problems cannot be ignored because persistent sleep problems may have serious consequences (Shaffique et al., 2020, Sher, 2020). A study reported that sleep disturbances were correlated with mental health problems, such as anxiety, stress and depression (Xiao et al., 2020); furthermore, increased sleep difficulties were found in people with more mental health problems (Cellini et al., 2020). Given that nursing students are at high risk for mental problems and sleep disturbances, further exploration to develop appropriate psychological support services may be warranted.
This review is the first to assess the mental health problems and sleep disturbances during the COVID-19 pandemic among nursing students to the best of the authors’ knowledge. Furthermore, this meta-analysis provides a complete picture of the prevalence of health problems in nursing students, namely fear, anxiety, stress, depression and sleep disturbances. Although the mental health problems in this study were assessed using standardized tools, they were not clinically diagnosed. However, as the COVID-19 pandemic is ongoing in several countries, these results can be used for decision-making or policy-making in nursing education. The results of this study implied that nursing students are prone to mental health problems and sleep disturbances. Considering their future careers and public expectations, the health problems of nursing students must be recognized early and adequately managed through academic and non-academic approaches. For example, modifications to distanced learning can be implemented to increase students’ engagement and simulation-based learning methods can be used to replace delayed clinical practice. In addition, non-academic approaches may include regular mental health assessments, making online mental health services available, or providing individual counseling. Policies must be developed for the implementation of clinical practice, with various considerations, such as the mental readiness and resilience of studies; physical resilience through vaccination and protective equipment; and the readiness of the practice area to provide student guidance methods during the COVID-19 adaptation period.
4.1. Limitations
This study has several limitations. First, the literature search only searched four major databases, which may limit the scope of the search. Second, this review only included research papers published in English and Indonesian, potentially overlooking valuable studies published in other languages. Third, some of the outcomes examined involved a small number of articles. For example, the prevalence of PTSD was reported narratively because only one study reporting PTSD outcomes was identified. In addition, the pooled prevalences for fear and stress were each obtained from only three studies. The small number of studies may affect the generalizability of the pooled results. Fourth, not all studies reported complete student characteristics, such as the students’ degrees or places of residence, limiting the ability to conduct subgroup analyses or meta-regression to examine detailed conclusions from these results.
5. Conclusions
This study provides evidence that nursing students have experienced numerous mental health problems and suffered from sleep disturbances during the COVID-19 pandemic. Therefore, effective strategies for managing nursing students’ education and implementing mental health services during the COVID-19 pandemic and similar future situations remain necessary. Additional data on the prevalence of mental health problems and sleep disturbances is crucial for policy development regarding both classroom-based education and clinical practice. The nursing profession requires that students obtain hands-on experience caring for patients; therefore, adequate preparation of the clinical practice environment, with considerations for mental resilience, physical preparation and practice area readiness, is necessary to allow nurses to safely obtain clinical experience. Future studies should assess the specific factors associated with mental health problems and sleep disturbances among nursing students during the COVID-19 pandemic.
Funding statement
No external funding.
CRediT authorship contribution statement
Study conception and design: MM, BOL; Data collection: MM, SIT; Data analysis and interpretation: MM, SIT, BOL, WTL; Drafting of the article: MM, SIT, BOL, SL; Critical revision of the article, and final approval of the version: All authors.
Declaration of Competing Interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.nepr.2021.103228.
Appendix A. Supplementary material
Supplementary material
.
References
- Agu C.F., Stewart J., McFarlane-Stewart N., Rae T. COVID-19 pandemic effects on nursing education: looking through the lens of a developing country. Int. Nurs. Rev. 2021;68(2):153–158. doi: 10.1111/inr.12663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Harthi M., Al Thobaity A., Al Ahmari W., Almalki M. Challenges for nurses in disaster management: a scoping review. Risk Manag. Health Policy. 2020;13:2627–2634. doi: 10.2147/RMHP.S279513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alici N.K., Copur E.O. Anxiety and fear of COVID-19 among nursing students during the COVID-19 pandemic: a descriptive correlation study. Perspect. Psychiatr. Care. 2021 doi: 10.1111/ppc.12851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alimoradi Z., Brostrom A., Tsang H.W.H., Griffiths M.D., Haghayegh S., Ohayon M.M., Lin C.Y., Pakpour A.H. Sleep problems during COVID-19 pandemic and its’ association to psychological distress: a systematic review and meta-analysis. EClinicalMedicine. 2021;36 doi: 10.1016/j.eclinm.2021.100916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almahasees Z., Mohsen K., Amin M.O. Faculty’s and students’ perceptions of online learning during COVID-19. Front. Educ. 2021:6. doi: 10.3389/feduc.2021.638470. [DOI] [Google Scholar]
- Alshutwi S.S. Senior nursing students and interns’ concerns and willingness to treat patients with COVID-19: a strategy to expand national nursing workforce during the COVID-19 pandemic [Article] Risk Manag. Health Policy. 2021;14:39–48. doi: 10.2147/RMHP.S279569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amir-Behghadami M., Janati A. Population, intervention, comparison, outcomes and study (PICOS) design as a framework to formulate eligibility criteria in systematic reviews. Emerg. Med J. 2020;37:387. doi: 10.1136/emermed-2020-209567. [DOI] [PubMed] [Google Scholar]
- Ang W.H.D., Shorey S., Lopez V., Chew H.S.J., Lau Y. Generation Z undergraduate students’ resilience during the COVID-19 pandemic: a qualitative study. Curr. Psychol. 2021:1–15. doi: 10.1007/s12144-021-01830-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aslan H., Pekince H. Nursing students’ views on the COVID‐19 pandemic and their percieved stress levels. Perspect. Psychiatr. Care. 2021;57(2):695–701. doi: 10.1111/ppc.12597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atalan A. Is the lockdown important to prevent the COVID-9 pandemic? Effects on psychology, environment and economy-perspective. Ann. Med Surg. (Lond.) 2020;56:38–42. doi: 10.1016/j.amsu.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bareeqa S.B., Ahmed S.I., Samar S.S., Yasin W., Zehra S., Monese G.M., Gouthro R.V. Prevalence of depression, anxiety and stress in china during COVID-19 pandemic: a systematic review with meta-analysis. Int. J. Psychiatry Med. 2021;56(4):210–227. doi: 10.1177/0091217420978005. [DOI] [PubMed] [Google Scholar]
- Bdair I.A. Nursing students’ and faculty members’ perspectives about online learning during COVID-19 pandemic: a qualitative study. Teach. Learn. Nurs. 2021;16(3):220–226. doi: 10.1016/j.teln.2021.02.008. [DOI] [Google Scholar]
- Borenstein M., Hedges L.V., Higgins J.P.T., Rothstein H.R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res. Synth. Methods. 2010;1(2):97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- Borenstein M., Higgins J.P.T., Hedges L.V., Rothstein H.R. Basics of meta-analysis: I2 is not an absolute measure of heterogeneity. Res. Synth. Methods. 2017;8(1):5–18. doi: 10.1002/jrsm.1230. [DOI] [PubMed] [Google Scholar]
- Brouwer K.R., Walmsley L.A., Parrish E.M., McCubbin A.K., Welsh J.D., Braido C.E.C., Okoli C.T.C. Examining the associations between self-care practices and psychological distress among nursing students during the COVID-19 pandemic. Nurse Educ. Today. 2021;100 doi: 10.1016/j.nedt.2021.104864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cellini N., Canale N., Mioni G., Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep. Res. 2020;29(4) doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang J.J., Ji Y., Li Y.H., Pan H.F., Su P.Y. Prevalence of anxiety symptom and depressive symptom among college students during COVID-19 pandemic: a meta-analysis. J. Affect Disord. 2021;292:242–254. doi: 10.1016/j.jad.2021.05.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cici R., Yilmazel G. Determination of anxiety levels and perspectives on the nursing profession among candidate nurses with relation to the COVID-19 pandemic. Perspect. Psychiatr. Care. 2021;57(1):358–362. doi: 10.1111/ppc.12601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M.E., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R., Weaver M.D., Robbins R., Facer-Childs E.R., Barger L.K., Czeisler C.A., Howard M.E., Rajaratnam S.M.W. Mental health, substance use and suicidal ideation during the COVID-19 pandemic — United States, June 24–30, 2020. Cent. Dis. Control Prev. Morb. Mortal. Wkly. Rep. 2020;Vol. 69 /(No. 32):1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalcali B.K., Durgun H., Tas A.S. Anxiety levels and sleep quality in nursing students during the COVID-19 pandemic. Perspect. Psychiatr. Care. 2021 doi: 10.1111/ppc.12839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Santos J.A.A., Labrague L.J., Falguera C.C. Fear of COVID-19, poor quality of sleep, irritability and intention to quit school among nursing students: a cross-sectional study. Perspect. Psychiatr. Care. 2021 doi: 10.1111/ppc.12781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deo P.K., Budhathoki S., Raut J., Adhikari B., Shrestha J. Factors associated with perceived stress, anxiety, depression, insomnia during COVID-19 outbreak among nursing students. Int. J. Sci. Res. (IJSR) 2020;9(9) doi: 10.21275/SR20826170002. [DOI] [Google Scholar]
- Dewart G., Corcoran L., Thirsk L., Petrovic K. Nursing education in a pandemic: academic challenges in response to COVID-19. Nurse Educ. Today. 2020;92 doi: 10.1016/j.nedt.2020.104471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farsi Z., Sajadi S.A., Afaghi E., Fournier A., Aliyari S., Ahmadi Y., Hazrati E. Explaining the experiences of nursing administrators, educators and students about education process in the COVID-19 pandemic: a qualitative study. BMC Nurs. 2021;20(1):151. doi: 10.1186/s12912-021-00666-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgerald A., Konrad S. Transition in learning during COVID-19: Student nurse anxiety, stress and resource support. Nurs. Forum. 2021;56(2):298–304. doi: 10.1111/nuf.12547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowler K., Wholeben M. COVID-19: outcomes for trauma-impacted nurses and nursing students [Editorial] Nurse Educ. Today. 2020;93 doi: 10.1016/j.nedt.2020.104525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franzoi M.A.H., Cauduro F.L.F. AtuaÇÃo De Estudantes De Enfermagem Na Pandemia De Covid-19. Cogitare Enferm. 2020;39:25–3305. doi: 10.5380/ce.v25i0.73491. [DOI] [Google Scholar]
- Gol I., Erkin O. Mental status of nursing students assessed using the general health questionnaire during the COVID-19 pandemic in Turkey. Perspect. Psychiatr. Care. 2021 doi: 10.1111/ppc.12740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heilferty C.M., Phillips L.J., Mathios R. Letters from the pandemic: Nursing student narratives of change, challenges and thriving at the outset of COVID-19. J. Adv. Nurs. 2021;77:3436–3445. doi: 10.1111/jan.14862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernández-Martínez A., Rodríguez-Almagro J., Martínez-Arce A., Romero-Blanco C., García-Iglesias J.J., Gómez-Salgado J. Nursing students’ experience and training in healthcare aid during the COVID-19 pandemic in Spain. J. Clin. Nurs. 2021 doi: 10.1111/jocn.15706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang L., Lei W., Xu F., Liu H., Yu L. Emotional responses and coping strategies in nurses and nursing students during Covid-19 outbreak: a comparative study [Article] PLoS One. 2020;15(8 August) doi: 10.1371/journal.pone.0237303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ICN. (2021). INTERNATIONAL COUNCIL OF NURSES POLICY BRIEF: Nursing education and the emerging nursing workforce in COVID-19 pandemic. April 2021. 〈https://www.icn.ch/sites/default/files/inline-files/ICN%20Policy%20Brief_Nursing%20Education.pdf〉.
- Joob B., Wiwanitkit V. COVID-19, school closings and weight gain. Obesity (Silver Spring) 2020;28(6):1006. doi: 10.1002/oby.22825. [DOI] [PubMed] [Google Scholar]
- Kalkan Uğurlu Y., Mataracı Değirmenci D., Durgun H., Gök Uğur H. The examination of the relationship between nursing students’ depression, anxiety and stress levels and restrictive, emotional and external eating behaviors in COVID‐19 social isolation process. Perspect. Psychiatr. Care. 2021;57(2):507–516. doi: 10.1111/ppc.12703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S.C., Sloan C., Montejano A., Quiban C. Impacts of coping mechanisms on nursing students’ mental health during COVID-19 lockdown: a cross-sectional survey. Nurs. Rep. 2021;11(1):36–44. doi: 10.3390/nursrep11010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochuvilayil T., Fernandez R.S., Moxham L.J., Lord H., Alomari A., Hunt L., Middleton R., Halcomb E.J. COVID-19: Knowledge, anxiety, academic concerns and preventative behaviours among Australian and Indian undergraduate nursing students: a cross-sectional study. J. Clin. Nurs. 2021;30(5–6):882–891. doi: 10.1111/jocn.15634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kregar Velikonja N., Dobrowolska B., Stanisavljevic S., Erjavec K., Globevnik Velikonja V., Verdenik I. Attitudes of nursing students towards vaccination and other preventive measures for limitation of COVID-19 pandemic: cross-sectional Study in three European countries. Healthcare (Basel) 2021;9(7) doi: 10.3390/healthcare9070781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kusuma M.D.S., Nuryanto I.K., Sutrisna I.P.G. Tingkat Gejala Depresi Pada Mahasiswa Program Studi Sarjana Keperawatan Di Institut Teknologi Dan Kesehatan (Itekes) Bali. J. Ris. Kesehat. Nas. 2021;5(1):29. 〈http://ojs.itekes-bali.ac.id/index.php/jrkn/article/view/310/138〉 [Google Scholar]
- Labrague L.J. Resilience as a mediator in the relationship between stress-associated with the Covid-19 pandemic, life satisfaction and psychological well-being in student nurses: a cross-sectional study. Nurse Educ. Pr. 2021;56 doi: 10.1016/j.nepr.2021.103182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasheras I., Gracia-Garcia P., Lipnicki D.M., Bueno-Notivol J., Lopez-Anton R., de la Camara C., Lobo A., Santabarbara J. Prevalence of anxiety in medical students during the COVID-19 pandemic: a rapid systematic review with meta-analysis. Int J. Environ. Res Public Health. 2020;17(18) doi: 10.3390/ijerph17186603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, D., Zou, L., Zhang, Z., Zhang, P., Zhang, J., Fu, W., Mao, J., & Cao, S. (2021b). The Psychological Effect of COVID-19 on Home-Quarantined Nursing Students in China, Original Res. 12 (373). 10.3389/fpsyt.2021.652296. [DOI] [PMC free article] [PubMed]
- Li W., Gillies R., He M., Wu C., Liu S., Gong Z., Sun H. Barriers and facilitators to online medical and nursing education during the COVID-19 pandemic: perspectives from international students from low- and middle-income countries and their teaching staff. Hum. Resour. Health. 2021;19(1):64. doi: 10.1186/s12960-021-00609-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovrić R., Farčić N., Mikšić Š., Včev A. Studying during the COVID-19 pandemic: a qualitative inductive content analysis of nursing students’ perceptions and experiences. Educ. Sci. 2020;10(7) doi: 10.3390/educsci10070188. [DOI] [Google Scholar]
- Lynn J.J., Ward-Smith P. Teaching during COVID-19: perceptions of nursing faulty. J. Nurs. Educ. Pract. 2021;11(6):43. doi: 10.5430/jnep.v11n6p43. [DOI] [Google Scholar]
- Majrashi A., Khalil A., Nagshabandi E.A., Majrashi A. Stressors and coping strategies among nursing students during the COVID-19 pandemic: scoping review. Nurs. Rep. 2021;11(2):444–459. doi: 10.3390/nursrep11020042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manning M.L., Gerolamo A.M., Marino M.A., Hanson-Zalot M.E., Pogorzelska-Maziarz M. COVID-19 vaccinationreadiness among nurse faculty and student nurses. Nurs. Outlook. 2021;69:565–573. doi: 10.1016/j.outlook.2021.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meo S.A., Abukhalaf A.A., Alomar A.A., AlMutairi F.J., Usmani A.M., Klonoff D.C. Impact of lockdown on COVID-19 prevalence and mortality during 2020 pandemic: observational analysis of 27 countries. Eur. J. Med Res. 2020;25(1):56. doi: 10.1186/s40001-020-00456-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller A.E., Himmels J.P.W., Van de Velde S. Instruments to measure fear of COVID-19: a diagnostic systematic review. BMC Med. Res. Method. 2021;21(1):82. doi: 10.1186/s12874-021-01262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulyadi M., Tonapa S.I., Rompas S.S.J., Wang R.H., Lee B.O. Effects of simulation technology-based learning on nursing students’ learning outcomes: a systematic review and meta-analysis of experimental studies. Nurse Educ. Today. 2021;107 doi: 10.1016/j.nedt.2021.105127. [DOI] [PubMed] [Google Scholar]
- Mundakir M., Efendi F., Susanti I.A. Study of knowledge, attitude, anxiety and perception of mental health needs among nursing students in Indonesia during COVID19 pandemic. Indones. Nurs. J. Educ. Clin. (INJEC) 2021;6(1) doi: 10.24990/injec.v6i1.366. [DOI] [Google Scholar]
- Mustafa R.M., Alrabadi N.N., Alshali R.Z., Khader Y.S., Ahmad D.M. Knowledge, attitude, behavior and stress related to COVID-19 among undergraduate health care students in Jordan. Eur. J. Dent. 2020;14(S 01):S50–S55. doi: 10.1055/s-0040-1719212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Flynn-Magee K., Hall W., Segaric C., Peart J. GUEST EDITORIAL: the impact of Covid-19 on clinical practice hours in pre-licensure registered nurse programs. Teach. Learn Nurs. 2021;16(1):3–4. doi: 10.1016/j.teln.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okwuikpo M., Abazie O., Adetunji A., Nweke C. Coronavirus: nursing students’ knowledge and risk perception of clinical practice during the pandemic. Nurs. Midwifery Stud. 2021;10(2) doi: 10.4103/nms.nms_76_20. [DOI] [Google Scholar]
- Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., Chou R., Glanville J., Grimshaw J.M., Hróbjartsson A., Lalu M.M., Li T., Loder E.W., Mayo-Wilson E., McDonald S., McGuinness L.A., Stewart L.A., Thomas J., Tricco A.C., Welch V.A., Whiting P., Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palancia Esposito C., Sullivan K. Maintaining clinical continuity through virtual simulation during the COVID-19 pandemic. J. Nurs. Educ. 2020;59(9):522–525. doi: 10.3928/01484834-20200817-09. [DOI] [PubMed] [Google Scholar]
- Pokhrel S., Chhetri R. A literature review on impact of COVID-19 pandemic on teaching and learning. High. Educ. Future. 2021;8(1):133–141. doi: 10.1177/2347631120983481. [DOI] [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen. Psychiatr. 2020;33(2) doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Hidalgo A.J., Pantaleon Y., Dios I., Falla D. Fear of COVID-19, stress and anxiety in university undergraduate students: a predictive model for depression. Front Psychol. 2020;11 doi: 10.3389/fpsyg.2020.591797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal L., Lee S., Jenkins P., Arbet J., Carrington S., Hoon S., Purcell S.K., Nodine P. A survey of mental health in graduate nursing students during the COVID-19 pandemic. Nurse Educ. 2021;46(4):215–220. doi: 10.1097/nne.0000000000001013. [DOI] [PubMed] [Google Scholar]
- Rothstein R., Olympia R.P. School nurses on the front lines of healthcare: the approach to maintaining student health and wellness during COVID-19 school closures. NASN School Nurse. 2020;35(5):269–275. doi: 10.1177/1942602X20935612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahu P. Closure of universities due to coronavirus disease 2019 (COVID-19): impact on education and mental health of students and academic staff. Cureus. 2020;12(4) doi: 10.7759/cureus.7541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santoso A., Ardi W.R., Prasetya R.L., Dwidiyanti M., Wijayanti D.Y., Mu’in M., Ulliya S., Handayani F., Sulisno M., Ni’mah M., Aisah N.A. Tingkat Depresi Mahasiswa Keperawatan di Tengah Wabah COVID-19. J. Holist. Nurs. Health Sci. 2020;3(1):1–8. 〈https://ejournal2.undip.ac.id/index.php/hnhs〉 [Google Scholar]
- Savitsky B., Findling Y., Ereli A., Hendel T. Anxiety and coping strategies among nursing students during the covid-19 pandemic. Nurse Educ. Pr. 2020;46 doi: 10.1016/j.nepr.2020.102809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savitsky B., Findling Y., Ereli A., Hendel T. Nursing students in crisis mode: fluctuations in anxiety during the COVID-19-related lockdown. Nurse Educ. 2021;46(3):E33–e38. doi: 10.1097/nne.0000000000000955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seemiller C., Grace M. Generation Z: educating and engaging the next generation of students. Campus. 2017;22(3):21–26. doi: 10.1002/abc.21293. [DOI] [Google Scholar]
- Shaffique S., Farooq S.S., Anwer H., Asif H.M., Akram M., Jung S.K. Meta-analysis of prevalence of depression, anxiety and stress among University Students. RADS J. Biol. Res. Appl. Sci. 2020;11(1):1–6. June 2020. [Google Scholar]
- Shea K.L., Rovera E.J. Preparing for the COVID-19 pandemic and its impact on a nursing simulation curriculum. J. Nurs. Educ. 2021;60(1):52–55. doi: 10.3928/01484834-20201217-12. [DOI] [PubMed] [Google Scholar]
- Sher L. COVID-19, anxiety, sleep disturbances and suicide. Sleep Med. 2020;70:124. doi: 10.1016/j.sleep.2020.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman R.O. Keeping an eye on generation Z nurses. Nurse Lead. 2021;19(1):6–7. doi: 10.1016/j.mnl.2020.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spronk I., Korevaar J.C., Poos R., Davids R., Hilderink H., Schellevis F.G., Verheij R.A., Nielen M.M.J. Calculating incidence rates and prevalence proportions: not as simple as it seems. BMC Public Health. 2019;19(1):512. doi: 10.1186/s12889-019-6820-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterne J.A.C., Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J. Clin. Epidemiol. 2001;54(10):1046–1055. doi: 10.1016/S0895-4356(01)00377-8. [DOI] [PubMed] [Google Scholar]
- Sterne J.A.C., Gavaghan D., Egger M. Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. J. Clin. Epidemiol. 2000;53(11):1119–1129. doi: 10.1016/S0895-4356(00)00242-0. [DOI] [PubMed] [Google Scholar]
- Sun Y., Wang D., Han Z., Gao J., Zhu S., Zhang H. Disease Pprevention knowledge, anxiety and professional identity during COVID-19 pandemic in nursing students in Zhengzhou, China. J. Korean Acad. Nurs. 2020;50(4):533–540. doi: 10.4040/jkan.20125. [DOI] [PubMed] [Google Scholar]
- Swift A., Banks L., Baleswaran A., Cooke N., Little C., McGrath L., Meechan-Rogers R., Neve A., Rees H., Tomlinson A., Williams G. COVID-19 and student nurses: a view from England. J. Clin. Nurs. 2020;29(17–18):3111–3114. doi: 10.1111/jocn.15298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thapa P., Bhandari S.L., Pathak S. Nursing students’ attitude on the practice of e-learning: a cross-sectional survey amid COVID-19 in Nepal. PLoS One. 2021;16(6) doi: 10.1371/journal.pone.0253651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Joanna Briggs Institute. (2017). The Joanna Briggs Institute Critical Appraisal tools for use in JBI Systematic Reviews. 〈http://joannabriggs.org/research/critical-appraisal-tools.html〉.
- Tomietto M., Comparcini D., Simonetti V., Cicolini G. Nursing education: challenges and perspectives in a COVID-19 age. Prof. Inferm. 2020;73(3):131–132. doi: 10.7429/pi.2020.733131. [DOI] [PubMed] [Google Scholar]
- Tung Y.J., Lo K.K.H., Ho R.C.M., Tam W.S.W. Prevalence of depression among nursing students: A systematic review and meta-analysis. Nurse Educ. Today. 2018;63:119–129. doi: 10.1016/j.nedt.2018.01.009. [DOI] [PubMed] [Google Scholar]
- Turan G.B., Ozer Z., Ciftci B. Analysis of anxiety levels and attitudes of nursing students toward the nursing profession during the COVID-19 pandemic. Perspect. Psychiatr. Care. 2021 doi: 10.1111/ppc.12766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usher K., Bhullar N., Jackson D. Life in the pandemic: social isolation and mental health. J. Clin. Nurs. 2020;29(15–16):2756–2757. doi: 10.1111/jocn.15290. [DOI] [PubMed] [Google Scholar]
- Ustun G. Determining depression and related factors in a society affected by COVID-19 pandemic. Int. J. Soc. Psychiatry. 2021;67(1):54–63. doi: 10.1177/0020764020938807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viner R.M., Russell S.J., Croker H., Packer J., Ward J., Stansfield C., Mytton O., Bonell C., Booy R. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc. Health. 2020;4(5):397–404. doi: 10.1016/s2352-4642(20)30095-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitale E., Moretti B., Notarnicola A., Covelli I. How the Italian nursing student deal the pandemic COVID-19 condition. Acta Biomed. 2020;91(12–S):1–10. doi: 10.23750/abm.v91i12-S.9860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vizcaya-Moreno M.F., Pérez-Cañaveras R.M. Social media used and teaching methods preferred by generation z students in the nursing clinical learning environment: a cross-sectional research study. Int J. Environ. Res. Public Health. 2020;17(21):1–10. doi: 10.3390/ijerph17218267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace S., Schuler M.S., Kaulback M., Hunt K., Baker M. Nursing student experiences of remote learning during the COVID-19 pandemic. Nurs. Forum. 2021;56:612–618. doi: 10.1111/nuf.12568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Heath Organization. (2021). WHO Coronavirus (COVID-19) Dashboard. Retrieved June 26, 2021 from 〈https://covid19.who.int/〉.
- Xiao H., Zhang Y., Kong D., Li S., Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Med. Sci. Monit. 2020;26 doi: 10.12659/MSM.923921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu H., Wei L., Niu P. The novel coronavirus outbreak in Wuhan, China. Glob. Health Res Policy. 2020;5:6. doi: 10.1186/s41256-020-00135-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Wang H., Wang A. An evaluation of mental health and emotion regulation experienced by undergraduate nursing students in China during the COVID-19 pandemic: a cross-sectional study. Int J. Ment. Health Nurs. 2021;30:1160–1169. doi: 10.1111/inm.12867. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material