Abstract
The infection fatality ratio (IFR) is the risk of death per infection and is one of the most important epidemiological parameters. Enormous efforts have been undertaken to estimate the IFR for COVID-19. This study examined the pros and cons of several approaches. It is found that the frequently used approaches using serological survey results as the denominator and the number of confirmed deaths as the numerator underestimated the true IFR. The most typical examples are South Africa and Peru (before official correction), where the confirmed deaths are one-third of the excess deaths. We argue that the RT-PCR-based case fatality ratio (CFR) is a reliable indicator of the lethality of COVID-19 in locations where testing is extensive. An accurate IFR is crucial for policymaking and public-risk perception.
Keywords: Infection fatality ratio, Case fatality rate, RT-PCR, Serological survey
Introduction
The infection fatality ratio (IFR) and case fatality ratio (CFR) define the risk of death per infection and per case, respectively. The difference between IFR and CFR depends on the definition of the case. If infection is defined as case, then CFR equals IFR. It is very important to determine the IFR because it influences the control policy and individual risk perception. It would be straightforward to determine the IFR in a closed, small population, such as the Diamond Princess Cruise, where the CFR was 1.3% without age standardization (Russell et al. 2020) and 0.5% after age standardization (Faust and Del Rio 2020). However, it is not easy to determine the true IFR in a large population because different approaches to estimate IFR have been proposed in a large population (Meyerowitz-Katz and Merone 2020; Levin et al. 2020b; Brazeau et al. 2020; Ioannidis 2021). Meyerowitz-Katz and Merone conducted a meta-analysis and found an IFR of 0.68% (0.53–0.82%) for COVID-19 (Meyerowitz-Katz and Merone 2020). The current study examined the pros and cons of these approaches to estimate IFR. It found that the RT-PCR-based crude CFR with correction accounting for under-reporting of asymptomatic cases in locations where testing is extensive should be a reliable indicator of the lethality of COVID-19.
To estimate the IFR, the number of deaths and the number of related infections are needed.
Levin et al. (Levin et al. 2020b), Brazeau et al. (Brazeau et al. 2020) and Ioannidis (Ioannidis 2021) used serological surveys to infer the number of infections. Levin et al.’s work was based on data up to June 2020, while many countries such as Australia experienced a severe wave in July–August 2020. A longer time interval, particularly covering large-scale community outbreaks, is preferable for reliable estimation. Even though different data and approaches were used, the age-stratified IFRs (IFR for different age groups) are largely consistent in different studies. Furthermore, Randolph and Barreiro (Randolph and Barreiro 2020) linked CFR with herd immunity to guide the distribution of health resources.
Perspective on classification for IFR/CFR estimation methods
RT-PCR CFR
If the real time RT-PCR-confirmed COVID-19 cases and deaths are only considered, the crude CFR may be defined, denoted hereafter as RT-PCR CFR, which is the reported COVID-19 deaths divided by the reported COVID-19 cases. Although the real-time RT-PCR misses a significant proportion of cases, the numbers of RT-PCR-confirmed cases are important indicators for informing control policies. The RT-PCR CFR is influenced by the testing policy (e.g., if only symptomatic or severe cases are tested, then RT-PCR CFR will be much larger than the IFR).
Sero-RT-PCR IFR
When the numbers of deaths are RT-PCR confirmed, while the numbers of infections are inferred via serological surveys, sero-RT-PCR IFR is obtained. This approach seems to be an improvement over the RT-PCR CFR because the under-reporting of the infections (i.e., the denominator) is addressed. Nonetheless, it has obvious limitations, given that under-reporting in deaths still exists and could be severe. For example, in South Africa and Peru, it was reported that the excess deaths (most are likely from COVID-19) tripled the reported COVID-deaths (Sguazzin 2021; Dyer 2021). The excess deaths typically mean the difference between all-cause deaths in a pandemic year and the average number of all-cause deaths in the five years before the pandemic. This underreporting of COVID-19 deaths is common in all countries without sufficient testing. Unless postmortem serological testing can be used, the sero-RT-PCR IFR will underestimate the true IFR by a factor of as large as one-third. Alternatively, excess deaths may be used to improve the numerator.
Sero-excess IFR
When the numbers of excess deaths are used as a proxy for COVID-19 deaths and the numbers of infections are inferred via serological surveys, a sero-excess IFR is obtained. This should be the most ideal approach with which to estimate the overall and age IFR of COVID-19 in a location where COVID-19 has caused community-wide outbreaks. Among these three approaches, the sero-excess IFR is the best in principle, but may not be feasible at present owing to data availability.
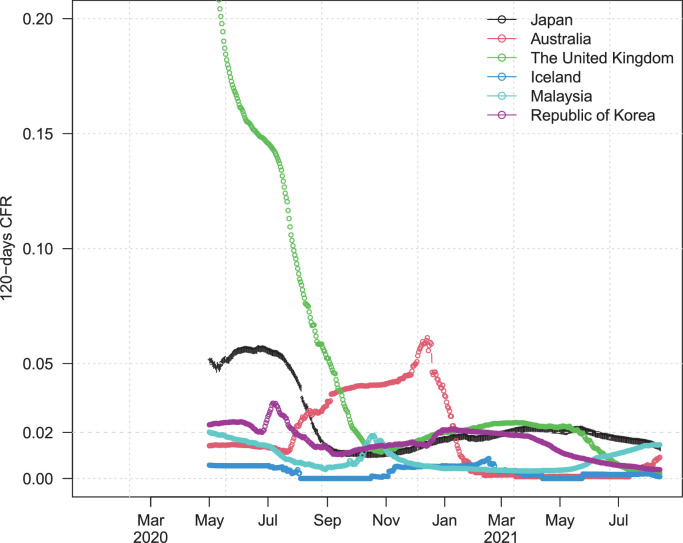
Moreover, some previous studies were carried out in the early phase of the pandemic (e.g., up to June 2020) (Levin et al. 2020a). COVID-19 had not yet caused a large-scale community-wide outbreak in some countries before June 2020 (e.g., Australia). This made the estimate in these countries less representative of the true scenario. Figure 1 shows the instantaneous RT-PCR CFR for several countries to illustrate the effects of the choice of time interval.
Figure 1.
Time-varying instantaneous RT-PCR CFR, which was calculated in a sliding window of 120 days for six countries. The RT-PCR CFR varied over time, which could be because of different testing policies implemented over time.
It is argued that the RT-PCR CFR in locations where testing is extensive should be a reliable indicator of the lethality of COVID-19. The mean annual income of the population in these locations is generally high, death reports are of high quality, and the medical systems have avoided a breakdown under large-scale community-wide outbreaks. Under these conditions, their RT-PCR CFR is of reference value. To show this, data from the beginning of the pandemic up to March 2021 were included, which was much longer than the previous studies. The effects of vaccination, however, were not yet evident.
Results for selected RT-PCR data
This study collected COVID-19 RT-PCR cases and deaths and tests for 221 countries and regions from https://www.worldometers.info/coronavirus/coronavirus-cases/. It divided countries/regions into different categories according to the level of successful control (thus avoiding a medical system breakdown) in terms of deaths/million population. Particularly, countries/regions where total deaths/million were between 20–100 were selected, which indicated large-scale community transmission but without breaking the medical system, owing to successful control measures such as extensive testing. Extensive testing typically leads to a low positive rate (i.e., a low proportion of positive tests out of all tests). High deaths/million population (> 100 deaths/million) or low deaths/million population (< 20 deaths/million) would imply either a breakdown of the medical system or no large-scale community-wide spread, respectively. However, this study was interested in the typical scenario of a large-scale community-wide spread without a medical system breakdown. Furthermore, it selected countries/regions with a testing positive rate < 5% (share of tests returning a positive result), which suggests extensive testing and that the pandemic is under control in a location (WHO 2020). RT-PCR CFR was calculated using total deaths divided by the total number of confirmed cases. Although there should be a delay between the death cases and confirmed cases (about two weeks), this was omitted for simplicity. Finally, there were 14 countries/regions that satisfied the above selection criteria. The summary of selected countries/regions and the estimates of RT-PCR CFR are given in the supplementary information. The key findings have been summarized as follows:
Generally, the RT-PCR CFR fell into the range (0.005, 0.02), which is partly consistent with the serological results estimated by Levin et al. (Levin et al. 2020b). On the one hand, the IFR range for countries with comprehensive tracing programs from Levin et al.’s estimates was (0.005, 0.018). On the other hand, Levin et al.’s estimates for countries with a large population (e.g., South Korea) were significantly lower than the current estimation. The data used by Levin et al. was up to June 2020 when the instantaneous CFR was low.
For these locations under selection criteria, the RT-PCR CFR had a median of 1.37%. Locations such as Hong Kong, Australia, Japan, and South Korea that have a relatively successful control of the pandemic with measures including extensive testing, a large population size, and strong ties to other regions (e.g., Hong Kong is an important hub, and Hong Kong's data were not used in many previous studies due to the lack of large-scale serological surveys in Hong Kong ) had a higher CFR than those with small populations like Iceland. It was noted that wide use of self-testing kits (e.g., in Japan) could lead to a higher positive testing rate due to the under-reporting of negative results in self-testing. This did not impact the estimates, as long as the deaths and cases were from the same positive pool. Using RT-PCR CFR avoided underestimation of IFR based on sero-RT-PCR IFR in previous studies, because of under-reporting of COVID-19 deaths in places such as Peru and South Africa (O'Driscoll et al. 2021). The Peru government (Sala Situacional 2021) nearly tripled its death data after completion of the study.
Discussions and Comparisons
This study had some limitations. It was noted that the estimated RT-PCR CFR was 1.37%, which was higher than the true IFR. However, it is unlikely to be vastly different owing to implementation of extensive testing. It be can assumed that 80% of infections are reported in Hong Kong, South Korea, Japan, and Australia, due to extensive testing and/or universal testing. Thus, the 1.37% could be corrected to 1.37%*0.8=1.096% in a typical large population with community-wide outbreak but without medical breakdown. If the reporting rate was much lower than 80%, the successful control in these selected locations would be difficult to explain. Particularly in Hong Kong, universal testing of 1.5 million people only found a few cases. In Hong Kong, reported numbers include both symptomatic and asymptomatic cases. Suspected COVID-19 deaths are rigorously screened. In Hong Kong, 22% cases are imported cases, which are healthier than the local cases. The CFR among imported cases is 1/10 that of the local cases. Excluding imported cases is unlikely to change the conclusion.
As the contribution of reinfection is assumed as low, it can be ignored for now. All large-scale studies found that the rate of reinfection is < 1% (Falahi and Kenarkoohi 2020; Roy 2020; Sheehan, Reddy, and Rothberg 2021; Okhuese 2020). In Peru, the reported deaths (excess deaths) reached a level of 0.5% in the whole population. If the reinfection was ignored and it was assumed that 80% of the population had been infected, the IFR would be 0.625%. In an extreme scenario (very unlikely), if 100% of the population had been infected, the IFR would be 0.5%.
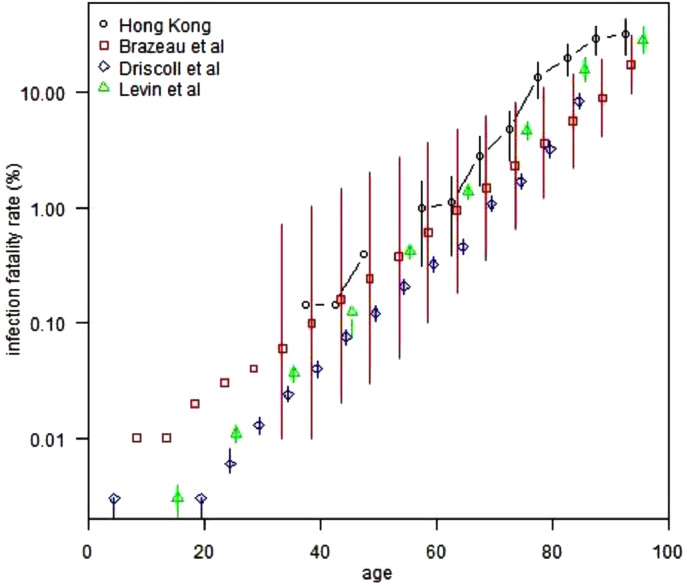
The overall IFR in a population is influenced by several factors: time interval, population age profile, and the availability of medical supplies. Previous studies looked at age-stratified IFR. Figure 2 compares the results from Hong Kong with three age-specific IFR estimations in previous studies (Levin et al. 2020b; Brazeau et al. 2020; O'Driscoll et al. 2021; Tao et al. 2021). The RT-PCR CFR in Hong Kong matched the age-specific IFR from previous studies for most age groups, which confirms that the current RT-PCR CFR, obtained effortlessly, should be a useful indicator of the lethality of COVID-19. Using the population age profile and age-specific IFR should be avoided to infer an overall IFR in a location without considering the current selection criteria, particularly the condition of the medical system and the availability of medical supplies.
Figure 2.
Comparison of IFR estimations from four studies.
Figure 2 lists the point estimation and confidence interval of the study in Hong Kong (RT-PCR CFR) and another three studies. The RT-PCR CFR well matched the other three studies in most age groups; this confirms the argument that the RT-PCR CFR is a good proxy of IFR. In the elderly group (age ≥ 75 years), the RT-PCR CFR of Hong Kong was higher, which could mean that other studies are underestimates because of improper use of serological survey in the denominator and RT-PCR-confirmed deaths in the numerator.
Conclusions
In conclusion, there are pros and cons of different approaches to estimate IFR. The argument is that the RT-PCR CFR in locations under certain criteria (e.g., with large-scale community transmission, without medical breakdown, with extensive testing) should be considered as a reliable reference value for policymaking. The sero-RT-PCR CFR may be severely biased towards low value (e.g., in South Africa and Peru) owing to different rules applied for the numerator and denominator values.
Competing interests
The authors declare that they have no competing interests.
Acknowledgments
Acknowledgments
None.
Funding
The work described in this paper was partially supported by a grant from the Research Grants Council of the Hong Kong Special Administrative Region, China (HKU C7123-20G) and by the National Natural Science Foundation of China (Grant Nos. 11905120 and 11947416)..
Contributions
All authors conceived the study, carried out the analysis, wrote the draft, discussed the results, revised the manuscript critically, and approved it for publishing.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
References
- Brazeau Nicholas F, Verity Robert, Jenks Sara, Fu Han, Whittaker Charles, Winskill Peter, Dorigatti Ilaria, Walker Patrick, Riley Steven, Schnekenberg Ricardo P, Hoeltgebaum Henrique, Mellan Thomas A, Mishra Swapnil, Juliette T Unwin H, Watson Oliver J, Cucunubá Zulma M, Baguelin Marc, Whittles Lilith, Bhatt Samir, Ghani Azra C, Ferguson Neil M, Okell Lucy C. Imperial College London; 2020. COVID-19 Infection Fatality Ratio: Estimates from Seroprevalence. [Google Scholar]
- Dyer Owen. Covid-19: Peru's official death toll triples to become world's highest. BMJ (Clinical research ed.) 2021;373:n1442. doi: 10.1136/bmj.n1442. [DOI] [PubMed] [Google Scholar]
- Falahi S., Kenarkoohi A. COVID-19 reinfection: prolonged shedding or true reinfection? New Microbes and New Infections. 2020;38 doi: 10.1016/j.nmni.2020.100812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faust Jeremy Samuel, Del Rio Carlos. Assessment of deaths from COVID-19 and from seasonal influenza. JAMA internal medicine. 2020;180:1045–1046. doi: 10.1001/jamainternmed.2020.2306. [DOI] [PubMed] [Google Scholar]
- Ioannidis J.P.A. Infection fatality rate of COVID-19 inferred from seroprevalence data. Bull World Health Organ. 2021;99:19–33f. doi: 10.2471/BLT.20.265892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin Andrew T, Hanage William P, Owusu-Boaitey Nana, Cochran Kensington B, Walsh Seamus P, Meyerowitz-Katz Gideon. Assessing the age specificity of infection fatality rates for COVID-19: systematic review, meta-analysis, and public policy implications. European J Epidemiolgy. 2020:1–16. doi: 10.1007/s10654-020-00698-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin Andrew T., Hanage William P., Owusu-Boaitey Nana, Cochran Kensington B., Walsh Seamus P., Meyerowitz-Katz Gideon. Assessing the age specificity of infection fatality rates for COVID-19: systematic review, meta-analysis, and public policy implications. European journal of epidemiology. 2020;35:1123–1138. doi: 10.1007/s10654-020-00698-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyerowitz-Katz Gideon, Merone Lea. A systematic review and meta-analysis of published research data on COVID-19 infection fatality rates. International Journal of Infectious Diseases. 2020;101:138–148. doi: 10.1016/j.ijid.2020.09.1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Driscoll Megan, Santos Gabriel Ribeiro Dos, Wang Lin, Cummings Derek A.T., Azman Andrew S., Paireau Juliette, Arnaud Fontanet, Simon Cauchemez, Henrik Salje. Age-specific mortality and immunity patterns of SARS-CoV-2′. Nature. 2021;590:140–145. doi: 10.1038/s41586-020-2918-0. [DOI] [PubMed] [Google Scholar]
- Okhuese, Victor Alexander. 2020. 'Estimation of the probability of reinfection with COVID-19 coronavirus by the SEIRUS model', medRxiv: 2020.04.02.20050930.
- Randolph Haley E., Barreiro Luis B. Herd Immunity: Understanding COVID-19. Immunity. 2020;52:737–741. doi: 10.1016/j.immuni.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy Sayak. COVID-19 Reinfection: Myth or Truth? SN Comprehensive Clinical Medicine. 2020;2:710–713. doi: 10.1007/s42399-020-00335-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell Timothy W, Hellewell Joel, Jarvis Christopher I, van Zandvoort Kevin, Abbott Sam, Ratnayake Ruwan, Flasche Stefan, Eggo Rosalind M, Edmunds W.John, Kucharski Adam J, CMMID COVID-19 working group Estimating the infection and case fatality ratio for coronavirus disease (COVID-19) using age-adjusted data from the outbreak on the Diamond Princess cruise ship, February 2020. Eurosurveillance. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.12.2000256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sala Situacional. 2021. 'Covid 19 en el Perú - Ministerio del Salud'. https://covid19.minsa.gob.pe/sala_situacional.asp.
- Sguazzin, Antony. 2021. 'Real South African Covid-19 Death Toll May Be Around 200,000′, Bloomberg.com.
- Sheehan, Megan M., Anita J. Reddy, and Michael B. Rothberg. 2021. 'Reinfection Rates among Patients who Previously Tested Positive for COVID-19: a Retrospective Cohort Study', medRxiv: 2021.02.14.21251715. [DOI] [PMC free article] [PubMed]
- Tao Jun, Zhang Xiaoyu, Musa Salihu S, Yang Lin, He Daihai. High Infection Fatality Rate Among Elderly and Risk Factors Associated With Infection Fatality Rate and Asymptomatic Infections of COVID-19 Cases in Hong Kong. Frontiers in Medicine. 2021;8:763. doi: 10.3389/fmed.2021.678347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . World Health Organization; 2020. Public health criteria to adjust public health and social measures in the context of COVID-19: annex to considerations in adjusting public health and social measures in the context of COVID-19, 12 May 2020.https://apps.who.int/iris/handle/10665/332073 Accessed July 08. [Google Scholar]