Critical limb ischemia (CLI) is on the rise due to diabetes and chronic kidney disease (CKD). It is the most severe form of peripheral artery disease with patients presenting with rest pain and/or tissue loss. The current reported amputation and mortality rates at 1 year are 20 to 25%. 1 CLI patients often present with multilevel disease and extensively calcified long chronic total occlusions (CTOs) in the infrapopliteal arteries. Successful CTO crossing can make the difference in terms of preventing amputation and salvaging the limb. Unfortunately, crossing CTOs often results in longer procedure times; higher radiation dose to the physician, staff, and patient; and an increased chance for arterial dissection and perforation. Depending on an operator's experience, the failure rate of CTO crossing can be 20% or greater. Given the importance of a successful revascularization in this high-risk patient population, it is vital that endovascular specialists become experts at below-the-knee CTO crossing using the various techniques available today.
Technique
When assessing a patient with CLI, the first step is to obtain noninvasive imaging from the groins to the toes. This helps exclude aorta–iliac (inflow), common femoral, deep femoral, superficial femoral, and above-knee popliteal artery disease, as these would require treatment prior to more distal disease.
If no significant disease is present in these territories, antegrade access into the common femoral or proximal superficial femoral artery is achieved with ultrasound guidance, and a 6-Fr vascular sheath is introduced as distal as possible (typically in the P2 or P3 segment of the popliteal artery). A 6-Fr sheath optimizes imaging and allows the use of two guidewires/catheters/balloon systems if needed, and the distal position optimizes visualization of CTO cap morphology, collaterals, and reconstitution points. Antegrade access also allows for more push-ability, torque-ability, and a shorter distance to travel for disease below the knee and below the ankle, and the ergonomics are better when performing procedures on either leg in terms of radiation exposure to the operator's arms and hands. If safe antegrade access is unattainable secondary to inflow disease or disease in the common femoral or proximal superficial femoral arteries, scarring from previous surgery, or morbid obesity, then a retrograde contralateral femoral approach may be used (“crossover” technique). 2
In some instances, an alternative access and treatment technique is called for. Tibio-pedal arterial minimally invasive (TAMI) revascularization differs from previously described access techniques in that the only access obtained is in a vessel near the ankle, from which all interventions are performed. The availability of low-profile sheaths, balloons, stents, and atherectomy devices has allowed for these small caliber and more fragile arteries to be used in this way. TAMI technique stems from the concept that the distal cap of a CTO is easier to cross than the proximal cap, which has the added benefit of reducing procedure time, decreasing contrast volume, and reducing radiation exposure. The technique provides benefits in patient comfort and reduces the incidence of groin complications (such as hematomas, pseudoaneurysms, nerve compression, arteriovenous fistula formation, and retroperitoneal bleeds), which also decreases the likelihood of postoperative blood transfusions. TAMI is also advantageous in patients who are obese, have hostile groins from radiation or prior surgery, and who are unable to lay flat. 3
Angiograms are obtained using an anteroposterior (AP) or slight ipsilateral oblique (fibula overlying the tibia) projection, which profiles the origins of the tibial–peroneal arteries. AP and lateral views of the foot are also obtained to evaluate and determine the status of the pedal arch. This initial evaluation helps determine treatment strategy including direct versus indirect revascularization, the need for additional pedal access, and the expected method of CTO crossing such as intraluminal or subintimal. 4 In addition, when crossing an infrapopliteal artery CTO, techniques will vary based on whether single- or dual-arterial access has been obtained.
Single-Access CTO Crossing Techniques
Penetration and Drilling
The standard antegrade approach of “penetration” and “drilling” is the preferred initially attempted technique, as this gives the operator the best chance for intraluminal crossing of a CTO. With the “penetration” technique, a medium to heavy tip load guidewire is rotated in short and quick clockwise and counter-clockwise directions while concurrently applying gentle forward pressure. The “drilling” technique requires a complete 360-degree rotation while also adding gentle forward pressure. In this way, recanalization is performed via the micro-channels within the CTO. 2 Higher tip load guidewires improve crossing ability but also increase the chance for vessel perforation and decrease tactile feel. 5 6 If the CTO crossing attempt is unsuccessful after 15 minutes, then escalation from 0.014–0.018 to 0.035 inch guidewires and the use of higher tip load guide wires are employed. 6 7 If this escalation also fails to provide a proximal to distal CTO recanalization, which occurs approximately 20% of the time, then the alternative techniques and access pathways discussed below are considered ( Fig. 1 ).
Fig. 1.

Penetration and drilling technique for chronic total occlusion recanalization. Top image shows penetration technique with back and forth rotation of guidewire and slight forward pressure. Bottom image shows drilling technique with 360-degree continuous rotation of guidewire with slight forward pressure.
Parallel Wire
CTO crossing is initially started using a standard approach; however, when the initial guidewire enters a false or subintimal channel, it is left in place. This initial guidewire marks the dissection location, helps reduce tortuosity of the vessel, prevents a second guidewire from entering the same channel, and reduces the likelihood of an extramural hematoma which can lead to collapse of the true lumen. A second guidewire, sometimes of higher tip load and a different tip bend, is then used to cross the CTO. This second guidewire can be advanced alone or can be supported by a catheter or balloon to recanalize the CTO ( Fig. 2 ). 8 9 10
Fig. 2.

Parallel wire technique. First guidewire enters a subintimal channel; so, it is left in place and a second guidewire or catheter system is then used to perform the recanalization.
See-Saw Wire
A variant of the parallel wire technique is known as the see-saw wire technique. The principles behind this technique are identical to that of the parallel wire technique. In this technique, when the second guidewire also takes a subintimal path, it is also left in place. In this setting, the first wire is retracted and is used to try and recanalize the CTO. Similar to the parallel wire technique, the guide-wires may be advanced alone or using a support catheter or balloon, with care taken to avoid entanglement of the wires ( Fig. 3 ). 11 12
Fig. 3.

See-saw wire technique. Two catheter-guidewire systems or two wires are used simultaneously. When one system courses into a subintimal plane it is left in place ( a ) and the other wire is then used to recanalize ( b ). When this second wire courses into a subintimal plane, it is left in place ( c ) and the first wire is then retracted and used again for recanalization. This “see-saw” process is repeated until the chronic total occlusion is crossed successfully ( d ).
Knuckle Wire
Another approach to recanalize long-segment CTOs is the knuckle wire technique. This technique is commonly used with a single access, but it can also be used in cases of dual access. A hydrophilic low tip load guidewire is intentionally prolapsed upon itself forming a small loop at its tip which is then used to create a subintimal dissection plane. This loop is advanced continually through the subintimal plane until it spontaneously reenters the true lumen. In some cases, the loop is advanced until it gets close to the reentry site where other techniques can be used to achieve through and through access. When dual access is present as in the case of antegrade and pedal approaches, a guidewire from the opposite direction can be used to recanalize into the created subintimal channel for successful CTO crossing. In general, this technique is favored for long-segment CTOs ( Fig. 4 ). 12 13
Fig. 4.

Knuckle wire technique. In this case of dual access, a hydrophilic, low tip load guidewire is intentionally prolapsed creating a loop and advanced from below to create a subintimal channel. The guidewire from above is then used for recanalization into this channel for through and through access and successful chronic total occlusion crossing.
Jenali
Similar to the knuckle wire technique, the Jenali technique uses a hydrophilic low tip load guidewire which is prolapsed upon itself and twisted to wrap around the distal tip of the catheter. This creates a “screw-like” appearance. This catheter-loop system is then advanced as a single unit while rotating it. Recanalization with this technique often occurs in a subintimal dissection plane. The system either spontaneously reenters the true lumen or remains in a subintimal plane near the reentry site, where other CTO techniques can be used. The CTO catheter gives the wire more support and “push-ability” during the recanalization than wire-alone techniques ( Fig. 5 ). 14
Fig. 5.
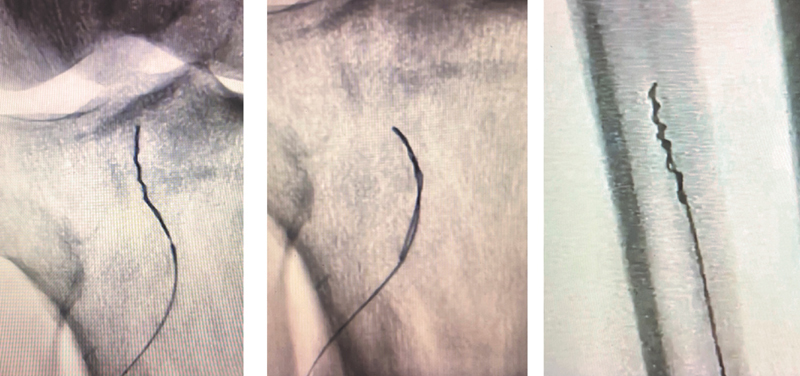
Jenali technique. A low tip load guidewire is prolapsed to form a loop and then twisted around the tip of the catheter to achieve a “screw-like appearance.” The entire system is then rotated continuously while pushing to recanalize the chronic total occlusion.
Transcollateral
This technique is used when antegrade crossing of a CTO has failed and distal access is not feasible or desired. Using antegrade access, a catheter and/or a guidewire are passed through a collateral vessel to recanalize the CTO in a retrograde fashion. Two specific techniques for this type of recanalization are used. First, if a large collateral is present and can be crossed with a 0.014-inch guidewire, a low-profile angioplasty balloon can be advanced through the collateral and angioplasty performed. In cases where the collateral vessel has a small caliber or is very tortuous, crossing with a balloon catheter may not be possible. In this situation, retrograde passage of only the guidewire may be sufficient to create a track for a second guidewire to be passed in an antegrade fashion. Oftentimes, a microcatheter (coaxially with a 4-Fr diagnostic catheter) needs to be used to enhance push-ability and steer-ability of the retrograde guidewire. In extremely tortuous collaterals, it may be necessary to use guidewires smaller than 0.014 inch ( Fig. 6 ).
Fig. 6.

Transcollateral technique. ( a ) Tibioperoneal (TP) artery trunk occlusion could not be recanalized using antegrade approach. ( b ) Transcollateral technique was used to perform retrograde recanalization via collateral. ( c ) Final angiography showing revascularization of the TP artery trunk. (Reprinted with permission from Zander T, Gonzalez G, Alba LD, Rivero O, Maynar M. Transcollateral approach for percutaneous revascularization of complex superficial femoral artery and TP trunk occlusions. J Vasc Interv Radiol 2012;23:691–695).
Advantages of transcollateral CTO crossing technique include the following: there is no need for additional access site; no specific tools are needed for distal access; hemostasis at the distal puncture site is not needed; there is less risk of radiation exposure to the operator's hands; and the technique can be used in cases when distal arteries are small, diseased, calcified, or difficult or impossible to puncture. Obviously, robust and large collaterals are needed to be successful and care should be taken to avoid damaging any potential surgical anastomotic sites. An attempt at crossing the last available collateral should never be performed, since arterial injury of the one vascular supply could result in an acutely ischemic extremity. 15
Dual-Access CTO Crossing Techniques
Oftentimes, below-knee CTOs cannot be crossed from one direction only and require access from above and below the CTO. This can be accomplished by accessing a patent or occluded distal arterial segment with ultrasound or fluoroscopic guidance. 16 When dual access can be obtained, several additional CTO crossing techniques can be used.
CART and Reverse CART
Controlled antegrade and retrograde subintimal tracking (CART) was first described by Surmely et al. 17 These techniques are commonly used when guidewires advanced through a CTO from above and below access points are in separate subintimal planes, and the operator is unable to gain through and through access. The wires are left in the subintimal space and a balloon measuring 1.5 to 3 mm is advanced from below (CART) or from above (reverse CART) to the tip of the other guidewire. The balloon is then inflated to profile, creating a larger focal dissection plane that allows for easier navigation of the other guidewire into this space to obtain through and through access. The advantage of these techniques is that subintimal crossing can be limited to a shorter length of the CTO ( Figs. 7 and 8 ). 18 19
Fig. 7.

CART technique. Guidewires in two separate subintimal planes within a chronic total occlusion. Balloon is used from below to create a larger subintimal space which allows the guidewire from above to enter this channel for through and through access.
Fig. 8.

Reverse CART technique. Guidewires in two separate subintimal planes within a chronic total occlusion. Balloon is used from above to create a larger subintimal space which allows the guidewire from below to enter this channel for through and through access.
Navi-Bossing
In addition to CART and reverse CART techniques, when antegrade and retrograde catheter/wire systems are in different subintimal planes, “Navi-Bossing” can be used. An antegrade 4-Fr Navicross catheter (Terumo, Somerset, NJ) is rotated slightly in one direction and then the other while it is advanced back and forth through a portion of the CTO. This disrupts the tissues between both subintimal planes, eventually allowing through and through access of the wire and/or microcatheter from below. The retrograde wire or catheter/wire system can then be externalized through the Navicross catheter. This technique relies heavily on the operator's tactile sense to ensure the catheter is still within the CTO and does not perforate outside the artery. If needed, extravascular ultrasound can also be used to guide the catheter during this recanalization, as it gives good visualization of both the CTO and catheter ( Fig. 9 ). 20
Fig. 9.

Navi-Bossing technique. Antegrade and retrograde catheter/guidewire systems are in two separate subintimal planes. An antegrade Navicross catheter (Terumo, Somerset, NJ) is rotated slightly in one direction and then the other and at the same time advanced back and forth in the chronic total occlusion on each side of the guidewire from below. This disrupts the tissues between both subintimal planes eventually allowing through and through access of the wire and/or 0.018-inch catheter from below. The retrograde wire or catheter/wire system can then be externalized through the 4-Fr Navicross catheter.
SAFARI
First described by Spinosa et al in 2005, the Subintimal Arterial Flossing with Antegrade-Retrograde Intervention (SAFARI) technique can be used when antegrade crossing of a CTO into the distal true lumen is unsuccessful. For this technique, the antegrade access is retained in the subintimal space. Retrograde access is then achieved below the level of the CTO using fluoroscopic or ultrasound guidance into a distal vessel. Then a guidewire and a support catheter are advanced into the subintimal space created by the antegrade catheter, resulting in through and through access ( Fig. 10 ).
Fig. 10.

Double-balloon technique. Used when antegrade and retrograde chronic total occlusion crossing is unsuccessful with catheter and guidewire systems alone. Angioplasty balloons are used from above and below to create larger subintimal spaces to achieve through and through access.
Double-Balloon Technique
The double-balloon technique is a combination of multiple CTO crossing techniques including SAFARI, CART, and reverse CART. It is used when through and through access from antegrade and retrograde sites cannot be achieved with catheter and wire systems alone. For this technique, angioplasty balloons are advanced via the antegrade and retrograde directions while ensuring that they approach each other closely. They are simultaneously inflated while taking the necessary precautions to avoid overlapping of the two balloons (which prevents perforation of the artery). Finally, a guidewire from above or below is then tracked into the larger subintimal channel created and ultimately into the true lumen for through and through access. 21
Important Tibial CTO Imaging Signs
Jenali Gap
A radiographic finding of importance is the “Jenali Gap.” This finding is described as a tibial artery segment of little to no calcification seen on ultrasound or computed tomography between two heavily calcified segments. While this may be confused with a relatively healthy arterial segment with little arterial calcification, it instead represents a negatively remodeled segment of artery. In the final stages of arterial cell death, medial calcification in the arterial wall is resorbed and replaced with dense intraluminal scarring. On imaging, this noncalcified scarring appears as a gap. These gaps can make intraluminal crossing impossible by routine endovascular techniques and may require the patient to undergo a surgical bypass ( Fig. 11 ). 22
Fig. 11.

White stop sign and Jenali gaps. White stop sign is depicted by the dense calcification completely filling the lumen of the tibial artery. Jenali gaps are the noncalcified segments between this heavy calcification representing the negatively remodeled arterial wall. Both findings can result in crossing catheters and guidewires perforating through the adventitial wall, making crossing impossible using traditional techniques. (Reprinted with permission from Mustapha JA, Sevensma M, Diaz-Sandoval LJ, Saab F. Technique: ultrasound guidance for lower extremity interventions. Endovasc Today 2013;12(5):68–70, 72.).
White Stop Sign
Another critically important imaging sign when attempting tibial artery CTO crossing is the “white stop sign.” When viewed under gray-scale transverse ultrasound imaging, the tibial artery may appear as a hyperechoic dot (white dot) or, under longitudinal gray-scale imaging, as a hyperechoic linear density filling the lumen. 14 This pattern of severe calcification usually results in crossing catheters and guidewires perforating through the adventitial wall, making crossing impossible and perhaps even dangerous using traditional techniques ( Fig. 11 ).
Vessel Preparation and Treatment
Once a CTO is successfully crossed, vessel preparation (VP) is an important step in the treatment process. This is especially true when there is marked calcification, as angioplasty without VP can result in a higher likelihood of dissection, rupture, suboptimal luminal gain, and suboptimal local drug delivery in the case of drug-coated devices. VP is often performed using cutting balloons, scoring balloons, and various atherectomy devices. 23 Once it is completed, treatment can proceed as usual. While VP and treatment are very important steps in successful below-the-knee disease therapy, they are beyond the scope of this article; the reader is referred to multiple in-depth reviews of these specific topics.
Conclusion
CLI is on the rise due to diabetes and CKD with a significant percentage of these patients presenting with infrapopliteal artery CTOs. These CTOs are technically challenging to cross due to their long length and diffuse calcification. Given the importance of successful CTO crossing in salvaging a CLI patient's limb, all endovascular physicians must be proficient with the numerous basic and advanced CTO crossing techniques described in this article.
Conflict of Interest None declared.
Disclosures
A.J.R. has no disclosures.
S.T. is a course faculty, speaker, and consultant for Bard Peripheral Vascular Inc., Abbott Vascular, Cardiovascular Systems Inc., and Terumo Interventional Systems.
References
- 1.Mustapha J A, Katzen B T, Neville R F.Critical limb ischemia: a threat to life and limbEndovascular Today 2019;18(05):
- 2.Pernès J M, Auguste M, Borie H. Infrapopliteal arterial recanalization: a true advance for limb salvage in diabetics. Diagn Interv Imaging. 2015;96(05):423–434. doi: 10.1016/j.diii.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 3.Mustapha J A, Saab F, McGoff T. Tibio-pedal arterial minimally invasive retrograde revascularization in patients with advanced peripheral vascular disease: the TAMI technique, original case series. Catheter Cardiovasc Interv. 2014;83(06):987–994. doi: 10.1002/ccd.25227. [DOI] [PubMed] [Google Scholar]
- 4.Saab F, Jaff M R, Diaz-Sandoval L J. Chronic total occlusion crossing approach based on plaque cap morphology: the CTOP classification. J Endovasc Ther. 2018;25(03):284–291. doi: 10.1177/1526602818759333. [DOI] [PubMed] [Google Scholar]
- 5.Murarka S, Heuser R R. Chronic total occlusions in peripheral vasculature: techniques and devices. Expert Rev Cardiovasc Ther. 2009;7(10):1283–1295. doi: 10.1586/erc.09.107. [DOI] [PubMed] [Google Scholar]
- 6.Wong G B, Price M J, Teirstein P S. CRC Press; 2007. Guidewire techniques and technologies: hydrophilic versus stiff wire selection; p. 11. [Google Scholar]
- 7.Mariano Palena L. Below-the-knee CTO crossing strategies. Endovascular Today. 2020;19(05):61–62. [Google Scholar]
- 8.EuroCTO Club . Sianos G, Werner G S, Galassi A R. Recanalisation of chronic total coronary occlusions: 2012 consensus document from the EuroCTO club. EuroIntervention. 2012;8(01):139–145. doi: 10.4244/EIJV8I1A21. [DOI] [PubMed] [Google Scholar]
- 9.Timmis A D. Percutaneous transluminal coronary angioplasty: catheter technology and procedural guidelines. Br Heart J. 1990;64(01):32–35. doi: 10.1136/hrt.64.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Murarka S LJ, Waters K L, Scherger S, Heuser R R. Cath Lab Digest; 2010. Chronic total occlusions in the coronary vasculature; p. 18. [Google Scholar]
- 11.Giubilato S, Tomasello S D, Galassi A R. InTech Open Access Publisher; 2013. Percutaneous Recanalization of Chronic Total Occlusion (CTO) Coronary Arteries: Looking Back and Moving Forward. [Google Scholar]
- 12.Dave B. Recanalization of chronic total occlusion lesions: a critical appraisal of current devices and techniques. J Clin Diagn Res. 2016;10(09):OE01–OE07. doi: 10.7860/JCDR/2016/21853.8396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brilakis E S, Mashayekhi K, Tsuchikane E. Guiding principles for chronic total occlusion percutaneous coronary intervention. Circulation. 2019;140(05):420–433. doi: 10.1161/CIRCULATIONAHA.119.039797. [DOI] [PubMed] [Google Scholar]
- 14.Mustapha J, Saab F.My favorite wires in tibial and plantar circulation: a case-based presentationCath Lab Digest 2018;26(02):
- 15.Van Den Berg J.Use of Collaterals for Retrograde Recanalization Endovascular Today; 201572–74., 97 [Google Scholar]
- 16.Chung J. Endovascular devices and revascularization techniques for limb-threatening ischemia in individuals with diabetes. J Diabetes Sci Technol. 2017;11(05):904–913. doi: 10.1177/1932296817702169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Surmely J F, Tsuchikane E, Katoh O. New concept for CTO recanalization using controlled antegrade and retrograde subintimal tracking: the CART technique. J Invasive Cardiol. 2006;18(07):334–338. [PubMed] [Google Scholar]
- 18.Dash D. Guidewire crossing techniques in coronary chronic total occlusion intervention: A to Z. Indian Heart J. 2016;68(03):410–420. doi: 10.1016/j.ihj.2016.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Michael T T, Papayannis A C, Banerjee S, Brilakis E S. Subintimal dissection/reentry strategies in coronary chronic total occlusion interventions. Circ Cardiovasc Interv. 2012;5(05):729–738. doi: 10.1161/CIRCINTERVENTIONS.112.969808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tummala S.Below the knee interventionsPresented at Society of Interventional Radiology Global PAD Bootcamp #2. July 18,2020
- 21.Ikushima I, Hirai T, Ishii A, Iryo Y, Yamashita Y. Confluent two-balloon technique: an alternative method for subintimal recanalization of peripheral arterial occlusion. J Vasc Interv Radiol. 2011;22(08):1139–1143. doi: 10.1016/j.jvir.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 22.Mustapha J.Patterns of vessel calcification in BTK arteries and implications for vessel preparation and atherectomyLINC2018
- 23.Langhoff R. The importance of vessel preparation. Endovascular Today. 2018;6:4–7. [Google Scholar]


