Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic has had a widespread significant impact on mental health. However, the effect of providing care to family members (informal caregiving) on changes in mental health status during the pandemic remains unclear.
Methods
Using cross-sectional data from a large internet survey conducted between August and September 2020, we investigated the association of informal caregiving status with the incidence of mental health deterioration (increased loneliness, self-reported deterioration in mental health, and new suicidal ideation) in Japan during the COVID-19 pandemic.
Results
Among 25,482 participants (mean age 48.8 [standard deviation 17.3]; 50.3% women), 2,500 (9.8%) were providing informal care during the pandemic. After adjusting for potential confounders, informal caregivers were more likely than non-caregivers to experience increased loneliness (adjusted odds ratio [aOR] 2.16; 95% confidence interval [CI] 1.70–2.76), self-reported deterioration in mental health (aOR 1.54; 95% CI 1.14–2.08), and new incidence of suicidal ideation (aOR 3.65; 95% CI 1.92–6.92). The degree of mental health deterioration depended on the intensity of care. For example, the incidence rates of new suicidal ideation were 15.0%, 5.2%, and 3.6% for individuals who provided high-intensity caregiving, those who provided low-intensity caregiving, and non-caregivers, respectively (p-for-trend<0.001). The stratified analysis by gender showed that informal caregiving was associated with self-reported deterioration in mental health status among women (aOR 2.19; 95% CI 1.49–3.21) but not men (aOR 1.08; 95% CI 0.75–1.56).
Conclusion
Informal caregivers were more likely to experience mental health deterioration than non-caregivers during the COVID-19 pandemic.
Keywords: Informal caregiving, Caregivers, COVID-19, Mental health, Loneliness, Suicidal ideation, Japan
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has been the largest global public health crisis in a century, with more than 100 million confirmed cases and 2 million deaths as of the end of January 2021. The pandemic has also had a detrimental impact on the mental health status of many people globally(Czeisler et al., 2020; Fancourt, Steptoe & Bu, 2021; Fiorillo et al., 2020; Gilan et al., 2020; Kikuchi et al., 2020; O'Connor et al., 2020; Pierce et al., 2020; Twenge & Joiner, 2020; Ueda, Stickley, Sueki & Matsubayashi, 2020). Increased suicidal ideation, an extreme consequence of psychological problems, has been reported in the United Kingdom and the United States(Czeisler et al., 2020; O'Connor et al., 2020). The suicide rate has been rising in Japan since the second wave of the COVID-19 outbreak (around July to October 2020), especially among women(Nomura et al., 2021; Tanaka & Okamoto, 2021). Previous studies of the general public have reported that socially disadvantaged populations, such as women (Fancourt et al., 2021; Fiorillo et al., 2020; O'Connor et al., 2020; Pierce et al., 2020), young adults (Fancourt et al., 2021; O'Connor et al., 2020; Twenge & Joiner, 2020; Ueda et al., 2020), lower-income groups (Fancourt et al., 2021; Kikuchi et al., 2020; Ueda et al., 2020), people with lower education attainment (Fancourt et al., 2021), lower socioeconomic groups (O'Connor et al., 2020), and unemployed persons (Ueda et al., 2020) had a higher risk of a depressive state during the pandemic. People living alone (Fancourt et al., 2021) or with children (Fancourt et al., 2021, Pierce et al., 2020; Twenge & Joiner, 2020) are also more likely to suffer in their mental health.
Individuals who provide informal care to their family members—also known as informal caregivers—are known to experience higher mental distress than the general population, even before the current pandemic (Roth, Fredman & Haley, 2015). During the pandemic, disruptions in the formal care system (World Health Organization, 2020) and medical care system (Rubin, 2020; Wright, Salazar, Mirica, Volk & Schiff, 2020) have increased the necessity of more intense informal care at home. Moreover, the nature of COVID-19, with its particularly high fatality rate in the elderly (Docherty et al., 2020; Matsunaga et al., 2020), may have required caregivers to take stricter precautions against infection in their daily lives. These issues raise concerns that mental health deterioration might be more severe among informal caregivers during the pandemic. In Japan, which has the highest proportion of people aged ≥65 in the world (World Health Organization, 2015), there are about 7 million informal caregivers in 2016 (Statistics Bureau of Japan, 2016). Although the long-term care insurance system was introduced in 2000, the role of informal caregivers is still important (Tamiya et al., 2011; Tokunaga, Hashimoto & Tamiya, 2015). Therefore, the negative effect of the COVID-19 pandemic on mental health of informal caregivers in Japan, if any, is a matter of great interest for Japanese people and policy makers. This topic also should be informative for the other countries experiencing the increasing number of older people and informal caregivers (World Health Organization, 2015).
To date, limited evidence has documented the mental health deterioration among caregivers during the COVID-19 pandemic. Studies have reported increased subjective psychological burden and stress (Archer, Reiboldt, Claver & Fay, 2021; Borges-Machado, Barros, Ribeiro & Carvalho, 2020; Carpinelli Mazzi et al., 2020; Giebel et al., 2021; Rainero et al., 2021; Sheth, Lorig, Stewart, Parodi & Ritter, 2021; Tsapanou et al., 2021), reduced self-rated wellbeing (Borges-Machado et al., 2020), worsened depressive symptoms (Altieri & Santangelo, 2021), and more concerns or excessive demands due to COVID-19 (Budnick et al., 2021) among informal caregivers of persons with dementia. Female gender (Carpinelli Mazzi et al., 2020), longer periods of lockdown isolation (Carpinelli Mazzi et al., 2020), and reduced social support service use (Giebel et al., 2021) have also been associated with more severe anxiety and depression among informal caregivers of people living with dementia. However, existing research has compared mental health before and after the pandemic only among informal caregivers. Given that mental health has also worsened among the general population (Czeisler et al., 2020; Fiorillo et al., 2020; Gilan et al., 2020; Kikuchi et al., 2020; O'Connor et al., 2020; Pierce et al., 2020; Twenge & Joiner, 2020; Ueda et al., 2020), whether mental health among caregivers was more affected compared to non-caregivers remains unclear. Only one study from the United States reported that perceived food insecurity and financial worries during the pandemic were more likely to be worse among caregivers compared to non-caregivers (Beach, Schulz, Donovan & Rosland, 2021) . Still, it remains unclear whether the psychological effect of the pandemic was larger among caregivers compared to non-caregivers in Japan, where formal care services under the long-term care insurance system have been provided.
To bridge this knowledge gap, we used a large-scale nationwide internet survey in Japan to examine the following three questions. First, was informal caregiving associated with mental health deterioration during the pandemic? Second, did the association between informal caregiving and changes in mental health depend on caregiving intensity? Third, did this association vary by caregiver gender?
2. Methods
2.1. Data source and study population
We used the data of individuals aged 15–79 years from the Japan COVID-19 and Society Internet Survey (JACSIS) study. JACSIS is a nationwide, web-based, self-reported survey to investigate how the COVID-19 pandemic affected people's daily lives in Japan (Miyawaki, Tabuchi, Tomata & Tsugawa, 2021; Okubo et al., 2021). The survey was managed by a major internet research agency with 2.3 million qualified individuals (Rakuten Insight, 2021) that has been used in previous studies (Tabuchi et al., 2016; Tabuchi, Shinozaki, Kunugita, Nakamura & Tsuji, 2019). We distributed the questionnaire to 224,389 individuals aged 15–79 years from August 25, 2020, to September 30, 2020, using stratified random sampling by gender, age, and prefecture category, covering all 47 prefectures in Japan. We distributed the questionnaire until the number of participants reached the target for each gender, age, and prefecture category (28,000 in total), and the final participation rate was 12.5% (28,000 of 224,389). Individuals who consented to participate in the survey accessed the designated website to answer the questionnaire about their health conditions, sociodemographic characteristics, lifestyle, and informal caregiving status. Participants had the options of not responding to any part of the survey and discontinuing the survey at any point. We excluded 2518 individuals with unnatural or inconsistent responses based on the algorithm we developed (Tabuchi et al., 2016, 2019) (Supplementary Methods 1). The final participants consisted of 25,482 individuals (91.0% of the total survey respondents). This study was approved by the Ethics Committees of the Osaka International Cancer Institute (No. 20084) and the University of Tokyo (No. 2020337NI).
2.2. Exposure variables
The primary exposure variable was participants’ informal caregiving status. Caregiving status was dichotomized (1 = “Providing care primarily” or “Providing care, but not primarily”; 0 = “Not providing”) according to the question “Are you currently caring for family members who are 40 years or older?” The secondary exposure variable was the intensity of informal caregiving, measured based on hours spent on care per day. For participants who provided informal care, we asked the intensity of informal caregiving using four choices: “Almost all day,” “About half a day,” “Two or three hours a day,” and “When needed.” We subcategorized informal caregivers to the “high intensity” group (“Almost all day,” “About half a day,” or “Two or three hours a day”) and the “low intensity” group (“When needed”) (Miyawaki et al., 2020). The participants were thus classified into “high intensity,” “low intensity,” and “caregiving, no.”
2.3. Outcome variables
The primary outcomes consisted of three mental health deterioration indicators: increased loneliness, self-reported deterioration in mental health, and incidence of new suicidal ideation during the pandemic.
We identified whether the participants developed the increased loneliness according to the response to the question “Do you feel lonely more frequently compared to before the COVID-19 pandemic (January 2020)?” and dichotomized the answer (1 = always, often, sometimes, occasionally; 0 = never). We also determine whether the participants incurred the self-reported deterioration in mental health according to the response to the question “How did mental health change in the past month from before the COVID-19 pandemic (January 2020)?” and dichotomized the answer (1 = much worsened, little worsened; 0 = much improved, improved, not sure). We also asked, “Have you wished to die since April 2020?”, with three mutually exclusive responses (“experienced for the first time,” “experienced since before April 2020,” and “never”). After excluding 2060 individuals who had experienced suicidal ideation since before April 2020 (response 2) according to this question, the incidence of new suicidal ideation was dichotomized (1 = experienced for the first time; 0 = never).
2.4. Adjustment variables
We adjusted for the participants’ demographics (gender and age [15–19 years old and 10-year age groups from 20 to 79]), socioeconomic status, and health-related characteristics. Socioeconomic status included marital status (married, never married, widowed, and separated), education attainment (junior high school, high school, college or higher, and others), employment status (employer, self-employed, regular employee, non-regular employee, and unemployed), and income level. Income level was based on self-reported household income and categorized into four groups using the tertiles of household equivalent income (high = more than 4.3 million JPY [reference], medium = 2.5 to 4.3 million JPY, or low = less than 2.5 million JPY) and an indicator for those who refused to respond to this question. Health-related characteristics included self-rated good health and dummy variables for eight self-reported past medical histories (hypertension, diabetes, asthma, coronary artery disease, stroke, chronic obstructive pulmonary disease, cancer, and mental illness). We defined self-rated good health as “very good” or “good” on the 5-point Likert scale question, which asked whether self-rated health status was “very good,” “good,” “moderate,” “bad,” or “very bad.”
2.5. Statistical analysis
First, we compared the participants’ demographics, socioeconomic status, and health-related characteristics between informal caregivers and non-caregivers. To account for the possibility that those who responded to the internet-based survey may have differed from the general population, we adjusted our estimates with inverse probability weighting (IPW), using the inverse of the estimated probability of participating in the survey, i.e., propensity score (Schonlau, 2009). To calculate the propensity score, we combined the data of the survey (JACSIS) with a widely-used nationwide population-based survey representative of the Japanese population (the 2016 Comprehensive Survey of Living Conditions of People on Health and Welfare by the Ministry of Health, Labour and Welfare) (Ministry of Health, Labour & Welfare, a) and fitted a logistic regression model including demographics, socioeconomic status, and health-related characteristics. The same approach of IPW using the same survey (JACSIS) has been used in previous studies (Miyawaki et al., 2021; Okubo et al., 2021), and the details of the IPW calculation are described in Supplementary Methods 2.
Second, we examined the association between informal caregiving status and the incidence of mental health deterioration: increased loneliness, self-reported deterioration in mental health, and new suicidal ideation. For each outcome, we constructed a weighted multivariable logistic regression model that adjusted for demographics, socioeconomic status, and health-related characteristics. We used standard errors clustered at the prefecture level to account for the potential correlation of participants in the same prefecture. To calculate adjusted rates of mental health deterioration, we used marginal standardization (also known as predictive margins or margins of response). For each participant, we calculated predicted probabilities of mental health deterioration with the exposure fixed at each category and then averaged over the distribution of the adjustment variables in our sample.
Third, we repeated the analyses by substituting the intensity of informal caregiving for the exposure. Fourth, we conducted stratified analyses by participants’ gender. We formally tested whether the association between informal caregiving and the outcomes varied by the participants’ genders (i.e., whether the difference in the differential effect of informal caregiving was statistically significant) following the method of Karaca-Mandic, Norton and Dowd (2012). The threshold for significance was P<0.05. All statistical analyses were conducted using Stata version 15 (College Station, TX, USA; StataCorp LLC.)
2.6. Sensitivity analyses
We conducted several sensitivity analyses. First, we additionally adjusted for indicators of participants’ residential prefectures (prefecture fixed effects) to effectively compare caregivers and non-caregivers within the same prefecture. Second, to investigate whether the association between caregiving status and mental health deterioration varied depending on regional COVID-19 outbreak situations, we stratified the participants into two groups based on the median of the cumulative number of confirmed cases (44.7 cases) per 100,000 population between January 15, 2020 (the day the first case of COVID-19 was identified in Japan), and August 24, 2020 (the day before starting the survey) (J.A.G, 2021). Third, to consider the possible different characteristics of informal caregivers younger than 18 years old (“young caregivers”) (Wong, 2017), we compared the results after excluding individuals younger than 18 years old.
3. Results
3.1. Characteristics of participants
Of the 25,482 participants analyzed, 12,809 (50.3%) were women and 2500 (9.8%) provided informal care. Informal caregivers were less likely than non-caregivers to be married and more likely to report comorbidities (Table 1 ). Among 2500 informal caregivers, 1326 (53.0%) were the high-intensity caregivers. By the kinship of the care recipient, provision of care to a parent, a parent-in-law, a grandparent (including in-law), and a spouse accounted for 49.2%, 17.3%, 11.1% and 9.0%, respectively. 85.5% of individuals caring for their spouse were high-intensity caregivers, while the high-intensity caregivers consisted of only 37.5% among informal caregivers of their parent. Informal caregivers younger than 18 years old (young caregivers) accounted for 1.1% in our population.
Table 1.
Characteristics of participants by informal caregiving status.
| Total (n = 25,482) | Caregiving, Yes (n = 2500) | Caregiving, No (n = 22,982) | P-value* | |
|---|---|---|---|---|
| Female | 12,809 (50.3) | 1047 (41.9) | 11,762 (51.2) | 0.09 |
| Age, Mean (SD), yr | 48.8 (17.4) | 46.3 (15.9) | 49.1 (17.3) | 0.31 |
| Income level | 0.060 | |||
| High | 7336 (28.8) | 905 (36.2) | 6431 (28.0) | |
| Medium | 6817 (26.8) | 554 (22.1) | 6264 (27.3) | |
| Low | 5733 (22.5) | 716 (28.6) | 5018 (21.8) | |
| Unanswered | 5595 (22.0) | 326 (13.0) | 5270 (22.9) | |
| Employment status | 0.047 | |||
| Employer | 1008 (4.0) | 217 (8.7) | 791 (3.4) | |
| Self-employed | 2008 (7.9) | 391 (15.6) | 1617 (7.0) | |
| Regular employee | 7876 (30.9) | 592 (23.7) | 7284 (31.7) | |
| Non-regular employee | 4869 (19.1) | 462 (18.5) | 4407 (19.2) | |
| Unemployed | 9722 (38.2) | 838 (33.5) | 8884 (38.7) | |
| Marital status | <0.001 | |||
| Married | 16,100 (63.2) | 1305 (52.2) | 14,796 (64.4) | |
| Never married | 6046 (23.7) | 396 (15.9) | 5649 (24.6) | |
| Widowed | 1949 (7.7) | 697 (27.9) | 1252 (5.5) | |
| Divorced | 1387 (5.4) | 102 (4.1) | 1284 (5.6) | |
| Educational Attainment | 0.25 | |||
| Junior high school | 1732 (6.8) | 98 (3.9) | 1634 (7.1) | |
| High school | 9640 (37.8) | 875 (35.0) | 8766 (38.1) | |
| College or higher | 13,903 (54.6) | 1518 (60.7) | 12,385 (53.9) | |
| Others | 207 (0.8) | 10 (0.4) | 197 (0.9) | |
| Self-rated health (good or very good) | 10,249 (40.2) | 1004 (40.2) | 9245 (40.2) | 0.99 |
| Comorbidities | ||||
| Hypertension | 6963 (27.3) | 1124 (45.0) | 5839 (25.4) | <0.001 |
| Diabetes | 2711 (10.6) | 746 (29.8) | 1966 (8.6) | <0.001 |
| Asthma | 3573 (14.0) | 808 (32.3) | 2765 (12.0) | <0.001 |
| Acute coronary syndrome | 1686 (6.6) | 621 (24.8) | 1065 (4.6) | <0.001 |
| Stroke | 1288 (5.1) | 603 (24.1) | 686 (3.0) | <0.001 |
| COPD | 1103 (4.3) | 584 (23.4) | 520 (2.3) | <0.001 |
| Cancer | 2185 (8.6) | 590 (23.6) | 1594 (6.9) | <0.001 |
| Depression, Mental disorder | 3807 (14.9) | 891 (35.6) | 2916 (12.7) | <0.001 |
The numbers are No. (%), except for age. The analyses were weighted to account for selection in an internet survey. Due to weighting, the sum of caregivers and non-caregivers did not necessarily equal to the number of total participants. Self-rated good health was defined as “very good” or “good” for the 5-point Likert scale question, which asked if self-rated health status was “very good,” “good,” “moderate,” “bad,” or “very bad.”.
COPD: Chronic obstructive pulmonary disease.
P values were calculated using t-test for age and chi-square test for the other discrete variables.
3.2. Informal caregiving and mental health deterioration
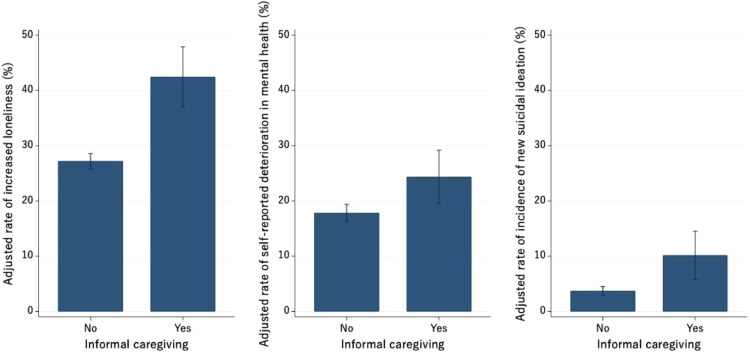
Crude incidence rates of increased loneliness, self-reported deterioration in mental health, and new suicidal ideation were higher among informal caregivers compared to non-caregivers (Table 2 ). After adjusting for potential confounders, informal caregivers were more likely to experience increased loneliness (adjusted incidence rate 42.5% vs. 27.2%; adjusted odds ratio [aOR] 2.16; 95% confidence interval [CI] 1.70–2.76; p<0.001), self-reported deterioration in mental health (24.4% vs. 17.8%; aOR 1.54; 95% CI 1.14–2.08; p = 0.004), and new suicidal ideation (10.1% vs. 3.7%; aOR 3.65; 95% CI 1.92–6.92; p<0.001), compared to non-caregivers (Fig. 1 and Table 2).
Table 2.
Association of informal caregiving with increased loneliness, self-reported deterioration in mental health, and incidence of new suicidal ideation.
| No. of participants | Incidence, n (%) | Adjusted rate,% (95% CI) | Adjusted OR (95% CI) | P-value | |
|---|---|---|---|---|---|
| Increased loneliness | |||||
| Caregiving, Yes | 2500 | 1301 (52.0) | 42.5 (37.1, 47.9) | 2.16 (1.70, 2.76) | <0.001 |
| Caregiving, No | 22,982 | 6007 (26.1) | 27.2 (25.8, 28.6) | Reference | |
| Self-reported deterioration in mental health | |||||
| Caregiving, Yes | 2500 | 641 (25.6) | 24.4 (19.5, 29.2) | 1.54 (1.14, 2.08) | 0.004 |
| Caregiving, No | 22,982 | 4079 (17.8) | 17.8 (16.3, 19.4) | Reference | |
| Incidence of new suicidal ideation | |||||
| Caregiving, Yes | 2033 | 275 (13.5) | 10.1 (5.8, 14.5) | 3.65 (1.92, 6.92) | <0.001 |
| Caregiving, No | 21,389 | 760 (3.6) | 3.7 (2.9, 4.5) | Reference |
OR, odds ratio; CI, confidence interval.
We used multivariable logistic regression models using inverse probability weighting. The analyses were weighted to account for selection in an internet survey. Standard errors were clustered at the prefectural level to account for the potential correlation of participants in the same prefecture. We adjusted for caregiver gender, age, marital status, educational attainment, self-rated health, income, employment status, and indicators of comorbidities. Adjusted rates were calculated using marginal standardization. In the analysis for the incidence of new suicidal ideation, we excluded 2060 participants who had suicidal ideation before the COVID-19 pandemic.
Fig. 1.
Adjusted rates of increased loneliness, self-reported deterioration in mental health, and incidence of new suicidal ideation by informal caregiving.
Adjusted rates of increased loneliness, self-reported deterioration in mental health, and incidence of new suicidal ideation by informal caregiving status were estimated using marginal standardization (also known as predictive margins or margins of response). Logistic regression models with standard errors clustered at the prefecture level was applied with adjustment for the caregiver gender, age, marital status, educational attainment, self-rated health, income, employment status, and indicators of comorbidities. In the analysis for the incidence of new suicidal ideation, we excluded 2060 participants who had suicidal ideation before the COVID-19 pandemic. Error bars show the 95% confidence intervals.
3.3. Intensity of informal caregiving and mental health deterioration
Individuals who provided high-intensity caregiving had the highest adjusted rate of increased loneliness at 46.1%, followed by 39.6% for individuals who provided low-intensity caregiving and 27.1% for non-caregivers (p-for-trend<0.001; Table 3 ). This “dose–response” relationship was found for self-reported deterioration in mental health (25.6% for the high-intensity group, 23.4% for the low-intensity group, and 17.8% for the non-caregivers; p-for-trend=0.022) and new suicidal ideation (15.0%, 5.2%, and 3.6%; p-for-trend<0.001).
Table 3.
Association of informal caregiving with increased loneliness, self-reported deterioration in mental health, and incidence of new suicidal ideation, by intensity of caregiving.
| No. of participants | Incidence, n (%) | Adjusted rate,% (95% CI) | Adjusted OR (95% CI) | P-value | P-value for trend* | |
|---|---|---|---|---|---|---|
| Increased loneliness | <0.001 | |||||
| Caregiving, High intensity | 1326 | 841 (63.4) | 46.1 (34.4, 57.8) | 2.56 (1.52, 4.31) | <0.001 | |
| Caregiving, Low intensity | 1174 | 460 (39.2) | 39.6 (34.8, 44.3) | 1.89 (1.51, 2.37) | <0.001 | |
| Caregiving, No | 22,982 | 6007 (26.1) | 27.1 (25.7, 28.5) | Reference | ||
| Self-reported deterioration in mental health | 0.022 | |||||
| Caregiving, High intensity | 1326 | 358 (27.0) | 25.6 (15.4, 35.7) | 1.66 (0.91,3.02) | 0.100 | |
| Caregiving, Low intensity | 1174 | 283 (24.1) | 23.4 (19.8, 27.0) | 1.45 (1.15, 1.83) | 0.002 | |
| Caregiving, No | 22,982 | 4079 (17.8) | 17.8 (16.3, 19.4) | Reference | ||
| Incidence of new suicidal ideation | <0.001 | |||||
| Caregiving, High intensity | 990 | 235 (23.7) | 15.0 (6.9, 23.1) | 6.39 (2.73, 14.94) | <0.001 | |
| Caregiving, Low intensity | 1043 | 40 (3.8) | 5.2 (2.7, 7.7) | 1.56 (0.83, 2.93) | 0.17 | |
| Caregiving, No | 21,389 | 760 (3.6) | 3.6 (2.9, 4.4) | Reference |
OR, odds ratio; CI, confidence interval.
We used multivariable logistic regression models using inverse probability weighting. The analyses were weighted to account for selection in an internet survey. Standard errors were clustered at the prefectural level to account for the potential correlation of participants in the same prefecture. We adjusted for caregiver gender, age, marital status, educational attainment, self-rated health, income, employment status, and indicators of comorbidities. Adjusted rates were calculated using marginal standardization. According to the hours of caregiving, individuals providing informal care were categorized to “high intensity (2–3 h per day or more)” and “low intensity (Support when needed).” In the analysis for the incidence of new suicidal ideation, we excluded 2060 participants who had suicidal ideation before the COVID-19 pandemic. *P values for trend tests assessed the trends in the incidence of outcomes.
3.4. Informal caregiving and mental health deterioration, by caregiver gender
Among both women and men, informal caregivers were more likely to experience increased loneliness (43.7% vs. 28.5%; p<0.001 for women and 58.0% vs. 23.7%; p<0.001 for men) and new suicidal ideation (12.5% vs. 4.1%; p<0.001 for women and 14.4% vs. 3.0%; p = 0.002 for men) than non-caregivers. In contrast, informal caregiving was associated with self-reported deterioration in mental health among women (aOR 2.19; 95% CI 1.49–3.21; p<0.001) but not men (aOR 1.08; 95% CI 0.75–1.56; p = 0.69; Table 4 ). The difference in the differential effect of informal caregiving between genders was statistically significant (p = 0.013).
Table 4.
Association of informal caregiving with increased loneliness, self-reported deterioration in mental health, and incidence of new suicidal ideation, by gender.
| Women (n = 12,809) | Men (n = 12,673) | |||||||
|---|---|---|---|---|---|---|---|---|
| No. of participants | Incidence, n (%) | Adjusted OR (95% CI) |
P-value | No. of participants | Incidence, n (%) | Adjusted OR (95% CI) |
P-value | |
| Increased loneliness | ||||||||
| Caregiving, Yes | 1047 | 457 (43.7) | 2.06 (1.48, 2.87) | <0.001 | 1454 | 843 (58.0) | 2.30 (1.56, 3.37) | <0.001 |
| Caregiving, No | 11,762 | 3351 (28.5) | Reference | 11,219 | 2656 (23.7) | Reference | ||
| Self-reported deterioration in mental health* | ||||||||
| Caregiving, Yes | 1047 | 353 (33.7) | 2.19 (1.49, 3.21) | <0.001 | 1454 | 288 (19.8) | 1.08 (0.75, 1.56) | 0.69 |
| Caregiving, No | 11,762 | 2333 (19.8) | Reference | 11,219 | 1746 (15.6) | Reference | ||
| Incidence of new suicidal ideation | ||||||||
| Caregiving, Yes | 917 | 114 (12.5) | 4.42 (2.22, 8.80) | <0.001 | 1117 | 161 (14.4) | 2.41 (1.39, 4.17) | 0.002 |
| Caregiving, No | 10,800 | 444 (4.1) | Reference | 10,588 | 316 (3.0) | Reference | ||
OR, odds ratio; CI, confidence interval. We used multivariable logistic regression models using inverse probability weighting. Because of weighting, the sum of men and women did not necessarily equal to the number of total respondents. The analyses were weighted to account for selection in an internet survey. Standard errors were clustered at the prefectural level to account for the potential correlation of participants in the same prefecture. We adjusted for caregiver gender, age, marital status, educational attainment, self-rated health, income, employment status, and indicators of comorbidities. Adjusted rates were calculated using marginal standardization. In the analysis for the incidence of new suicidal ideation, we excluded 1092 women and 968 men who had suicidal ideation before the COVID-19 pandemic. *The difference in the differential effect of informal caregiving between genders was statistically significant (p = 0.013) for self-reported deterioration in mental health.
3.5. Sensitivity analyses
Our findings were largely unaffected by including prefecture fixed effects (Supplementary Tables 1–3). When stratified by the local COVID-19 epidemic level, informal caregivers were more likely to experience increased loneliness, self-reported deterioration in mental health, and new suicidal ideation, regardless of the epidemic level (Supplementary Table 4 and Supplementary Table 5). Analyses excluding the study participants younger than 18 years old showed the similar results (Supplementary Table 6 and Supplementary Table 7).
4. Discussion
In this cross-sectional study of 25,482 individuals from the general population in Japan using a nationwide survey, we showed that informal caregivers were more likely to experience increased loneliness, self-reported deterioration in mental health, and new suicidal ideation than non-caregivers during the COVID-19 pandemic. We also observed higher incidence rates of mental health deterioration associated with increased intensity of caregiving. Stratified analysis by gender showed informal caregiving was associated with self-reported deterioration in mental health only among women. Taken together, our findings reveal that caregivers were more vulnerable to the pandemic compared to non-caregivers.
4.1. Comparisons with previous studies
Our findings add to a body of work that has explored the mental condition of caregivers during the COVID-19 pandemic. One study from the United States reported worse mental health and fatigue among informal caregivers compared to non-caregivers during the pandemic (Park, 2021). Another from Japan identified informal caregiving as one of the risk factors for worse mental health during the pandemic (Yoshioka et al., 2021). However, these studies did not focus on the change in mental health from before to during the pandemic. Caregivers have a higher rate of mental health problems than non-caregivers, even before the pandemic. Thus, to uncover whether mental health has been more affected among informal caregivers than non-caregivers during the pandemic, comparing their changes in mental health status is essential. A recent study from the United States compared perceived changes in loneliness, food insecurity, and financial worries due to COVID-19 between caregivers and non-caregivers, reporting worse changes among caregivers in food insecurity and financial worries but not loneliness (Beach et al., 2021). In contrast, our data showed the mental health deterioration during the pandemic among informal caregivers was more severe than that of non-caregivers, especially when providing high-intensity care. The different results between the United States and Japan regarding increased loneliness may be partly due to different epidemic levels between the two countries. The United States has experienced a much worse pandemic situation (with total case numbers per million people by the end of September 2020, of 680 in Japan and 22,000 in the United States (The World Bank, 2021, World Health Organization, 2021). The general population in the United States, regardless of informal caregiving status, might have experienced serious loneliness due to stricter physical distancing policies. A strength of the current study was that we compared the psychological effect of the pandemic among caregivers and non-caregivers using nationwide participants, covering a broad population.
Self-reported deterioration in mental health was more prominent among women caregivers than men. Our finding is compatible with a previous study from the United States, reporting worse physical, psychological, and social outcomes among women caregivers (Beach et al., 2021) . Using a large national survey of more than 25,000 participants, we showed that this gender difference also exists in Japan regarding the self-reported deterioration in mental health between informal caregivers and non-caregivers.
We observed no statistically significant difference by prefecture epidemic level in the association between informal caregiving and mental health deterioration. A report from Italy showed longer isolation due to lockdown was associated with more serious anxiety and depression in caregivers of persons with dementia (Carpinelli Mazzi et al., 2020). In Japan, the number of COVID-19 cases has been much smaller than in Italy (with total case numbers per million people by the end of September 2020, of 680 in Japan and 5400 in Italy (The World Bank, 2021, World Health Organization, 2021), and Japan did not implement strict lockdown with penalties like Italy(Yamamoto, Uchiumi, Suzuki, Yoshimoto & Murillo-Rodriguez, 2020). Therefore, fewer regional differences existed in the lockdown situation by prefecture in Japan. Accordingly, we may not have observed a statistically significant difference in the epidemic level by residential prefecture. Regional differences may be revealed with analysis by smaller areas such as local municipalities, but this is beyond the scope of our study.
4.2. Possible mechanisms
Several possible mechanisms could explain the worse mental health deterioration among informal caregivers. First, the COVID-19 pandemic might have amplified the concern of informal caregivers about the health of care recipients. Individuals requiring care, mostly older people with underlying diseases, are at higher risk of severe disease if they become infected (Docherty et al., 2020; Matsunaga et al., 2020). Therefore, it is plausible for informal caregivers to fear COVID-19. Second, limited access to formal care services might have increased informal caregivers’ burden and negatively impacted the mental health of caregivers, even under the long-term care insurance system, which has been introduced since 2000 in Japan (Tamiya et al., 2011). One study from Japan observed a reduction in the use of outpatient formal care services during the COVID-19 pandemic (Ito et al., 2021), and another from the United Kingdom reported that reduced access to social support services during the pandemic was associated with worse wellbeing of caregivers of people living with dementia (Giebel et al., 2021) . Home confinement of people with dementia has also been reported to deteriorate activities of daily living and worsen behavioral and psychological symptoms (Borges-Machado et al., 2020), leading to higher needs for informal care. Therefore, the observed mental health deterioration among informal caregivers might be partly due to decreased use of formal care services and increased burden of informal care.
Stratified by gender, we found self-reported deterioration in mental health was more severe among women informal caregivers. Even before the current pandemic, women caregivers were more likely to experience physical and psychological health issues than were men caregivers (Pinquart & Sörensen, 2003). A meta-analysis reported women caregivers were more likely to provide with higher number of tasks and for longer hours of care (Pinquart & Sörensen, 2003), and another report from Japan indicated that female informal caregivers tended to care for older recipients and with more severe cognitive impairment (Sugiura, Ito & Mikami, 2004), resulting in a greater burden than for male caregivers. Other studies have suggested that informal caregiving was associated with higher incidence and mortality rates of cardiovascular disease, especially among women (Miyawaki et al., 2017; Miyawaki, Tanaka, Kobayashi & Kawachi, 2019). Additionally, previous studies of the general population have reported that female gender was associated with worse mental health during the COVID-19 pandemic (Fancourt et al., 2021; Fiorillo et al., 2020; O'Connor et al., 2020; Pierce et al., 2020). Our findings may indicate that women informal caregivers, who were already facing a higher level of distress before the pandemic, have been more affected psychologically by it. For example, the nationwide school closure from March to April or May 2020, in Japan (Hiraoka & Tomoda, 2020) might have forced women caregivers to take care of their children at the same time. Also, female caregivers, who provided care more intensely than male caregivers, may have been affected more severely by the limited accessibility of formal care services during the pandemic than male caregivers (Ito et al., 2021).
4.3. Implications
Our study highlights that informal caregivers experienced more serious mental health deterioration during the COVID-19 pandemic. Appropriate support to mitigate informal caregivers’ burden is urgently required. In particular, prioritizing vulnerable populations such as women and high-intensity informal caregivers is essential. For example, support for formal care services providers are important to make sure care recipients and informal caregivers have access to necessary formal care services. Since April 2020, the Ministry of Health, Labour and Welfare of Japan has begun the subsidy program for home care services providers (Ministry of Health, Labour & Welfare, b). In this subsidy program, if a home care services user suspended the use of formal care service for longer than one month for some reason, home care service providers are encouraged to confirm the suspending user's wish and to assess the necessary support for them. This kind of support could improve the access to the formal care services and alleviate the stress of care recipients and their informal caregivers.
4.4. Limitations
This study has several limitations. First, it was limited to respondents to an internet-based survey, which had a low response rate (12.5%). This could lead to the possibility of sampling bias, and caution is needed when applying the results of this study to the general population. However, to reduce these limitations, we adjusted our estimates with IPW using a nationally representative sample to maximize the external validity of the study. Second, although we evaluated longitudinal change in mental health status during the pandemic, the possibility of reverse causation remains, due to the cross-sectional design of the study. For example, a person who quits their job due to mental health deterioration might be pushed to provide care to their parent. Third, we evaluated mental health deterioration by self-reported responses to a single question for each outcome, and not by validated indicators, which should be addressed in future studies. Fourth, we used a self-reported response to measure the intensity of informal care and categorized informal caregivers to the “high intensity” group (“Almost all day,” “About half a day,” or “Two or three hours a day”) and the “low intensity” group (“When needed”), following the previous study which defined the provision of care for longer than 3 hour a day as “long-hours of informal caregiving” (Miyawaki et al., 2020). Still, provision of care “when need”, categorized into a “low intensity” group, could be subjective, and the actual intensity may vary from person to person. Fifth, we could not consider some factors which could influence informal caregivers’ burden, such as the underlying diseases of care recipients and the type of formal care services they use, because these data were not available in this survey. Particular diseases of care recipients or lack of certain types of formal care services may be related to even worse mental health deterioration among informal caregivers, which should be investigated in future studies.
5. Conclusion
This study using a nationwide survey in Japan showed that informal caregivers experienced a higher rate of mental health deterioration during the COVID-19 pandemic compared to non-caregivers. In particular, informal caregivers providing high-intensity care and women caregivers were more likely to experience mental health deterioration during the pandemic, suggesting an unequal burden of care in the midst of a pandemic. Our findings highlight the importance of support for informal caregivers during the current and future pandemics.
CRediT authorship contribution statement
Yuta Taniguchi: Conceptualization, Methodology, Formal analysis, Software, Writing – original draft. Atsushi Miyawaki: Conceptualization, Methodology, Formal analysis, Software, Visualization, Writing – review & editing. Yusuke Tsugawa: Writing – review & editing. Hiroshi Murayama: Writing – review & editing. Nanako Tamiya: Writing – review & editing. Takahiro Tabuchi: Supervision, Methodology, Resources, Data curation, Investigation, Funding acquisition, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.archger.2021.104531.
Appendix. Supplementary materials
References
- Altieri M., Santangelo G. The psychological impact of COVID-19 pandemic and lockdown on caregivers of people with dementia. The American Journal of Geriatric Psychiatry: Official Journal of the American Association for Geriatric Psychiatry. 2021;29(1):27–34. doi: 10.1016/j.jagp.2020.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Archer J., Reiboldt W., Claver M., Fay J. Caregiving in quarantine: Evaluating the impact of the COVID-19 pandemic on adult child informal caregivers of a parent. Gerontology & Geriatric Medicine. 2021;7 doi: 10.1177/2333721421990150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach S.R., Schulz R., Donovan H., Rosland A.M. Family caregiving during the COVID-19 pandemic. The Gerontologist. 2021;61(5):650–660. doi: 10.1093/geront/gnab049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges-Machado F., Barros D., Ribeiro Ó., Carvalho J. The effects of COVID-19 home confinement in dementia care: Physical and cognitive decline, severe neuropsychiatric symptoms and increased caregiving burden. American Journal of Alzheimer's Disease and Other Dementias. 2020;35 doi: 10.1177/1533317520976720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budnick A., Hering C., Eggert S., Teubner C., Suhr R., Kuhlmey A., et al. Informal caregivers during the COVID-19 pandemic perceive additional burden: Findings from an ad-hoc survey in Germany. BMC Health Services Research. 2021;21(1):353–357. doi: 10.1186/s12913-021-06359-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpinelli Mazzi M., Iavarone A., Musella C., De Luca M., de Vita D., Branciforte S., et al. Time of isolation, education and gender influence the psychological outcome during COVID-19 lockdown in caregivers of patients with dementia. European Geriatric Medicine. 2020;11(6):1095–1098. doi: 10.1007/s41999-020-00413-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M.É., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R., et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic - United States, June 24-30, 2020. MMWR.Morbidity and Mortality Weekly Report. 2020;69(32):1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Docherty A.B., Harrison E.M., Green C.A., Hardwick H.E., Pius R., Norman L., et al. Features of 20 133 UK patients in hospital with COVID-19 using the ISARIC WHO clinical characterisation protocol: Prospective observational cohort study. BMJ (Clinical research ed.) 2020;369:m1985. doi: 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fancourt D., Steptoe A., Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: A longitudinal observational study. The Lancet Psychiatry. 2021;8(2):141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiorillo A., Sampogna G., Giallonardo V., Del Vecchio V., Luciano M., Albert U., et al. Effects of the lockdown on the mental health of the general population during the COVID-19 pandemic in Italy: Results from the COMET collaborative network. European Psychiatr. 2020;63(1):e87. doi: 10.1192/j.eurpsy.2020.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giebel C., Lord K., Cooper C., Shenton J., Cannon J., Pulford D., et al. A UK survey of COVID-19 related social support closures and their effects on older people, people with dementia, and carers. International Journal of Geriatric Psychiatry. 2021;36(3):393–402. doi: 10.1002/gps.5434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilan D., Röthke N., Blessin M., Kunzler A., Stoffers-Winterling J., Müssig M., et al. Psychomorbidity, resilience, and exacerbating and protective factors during the SARS-CoV-2 pandemic. Deutsches Arzteblatt International. 2020;117(38):625–630. doi: 10.3238/arztebl.2020.0625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiraoka D., Tomoda A. Relationship between parenting stress and school closures due to the COVID-19 pandemic. Psychiatry and Clinical Neurosciences. 2020;74(9):497–498. doi: 10.1111/pcn.13088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ito T., Hirata-Mogi S., Watanabe T., Sugiyama T., Jin X., Kobayashi S., et al. Change of use in community services among disabled older adults during COVID-19 in Japan. International Journal of Environmental Research and Public Health. 2021;18(3):1148. doi: 10.3390/ijerph18031148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karaca-Mandic P., Norton E.C., Dowd B. Interaction terms in nonlinear models. Health Services Research. 2012;47:255–274. doi: 10.1111/j.1475-6773.2011.01314.x. 1 Pt 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kikuchi H., Machida M., Nakamura I., Saito R., Odagiri Y., Kojima T., et al. Changes in psychological distress during the COVID-19 pandemic in Japan: A longitudinal study. Journal of Epidemiology. 2020;30(11):522–528. doi: 10.2188/jea.JE20200271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsunaga N., Hayakawa K., Terada M., Ohtsu H., Asai Y., Tsuzuki S., et al. Clinical epidemiology of hospitalized patients with COVID-19 in Japan: Report of the COVID-19 REGISTRY JAPAN. Clinical Infectious Diseases. 2020 doi: 10.1093/cid/ciaa1470. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The World Bank. (2021). World bank open data. Retrieved from https://data.worldbank.org/indicator/SP.POP.TOTL. Accessed September 16, 2021.
- J.A.G JAPAN. (2021). Dashboard of coronavirus COVID-19 Japan case (2019-nCoV).https://gis.jag-japan.com/covid19jp/. Accessed September 19, 2021.
- Ministry of Health, Labour and Welfare. (2021a). Comprehensive survey of living conditions. Retrieved from https://www.mhlw.go.jp/english/database/db-hss/cslc-index.html. Accessed September 20, 2021.
- Ministry of Health, Labour and Welfare. (2021b). Emergency comprehensive support program for COVID-19 (for long-term care). https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000121431_00144.html. Accessed September 19, 2021.
- Miyawaki A., Kobayashi Y., Noguchi H., Watanabe T., Takahashi H., Tamiya N. Effect of reduced formal care availability on formal/informal care patterns and caregiver health: A quasi-experimental study using the Japanese long-term care insurance reform. BMC Geriatrics. 2020;20(1):207. doi: 10.1186/s12877-020-01588-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyawaki A., Tabuchi T., Tomata Y., Tsugawa Y. Association between participation in the government subsidy programme for domestic travel and symptoms indicative of COVID-19 infection in Japan: Cross-sectional study. BMJ open. 2021;11(4) doi: 10.1136/bmjopen-2021-049069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyawaki A., Tanaka H., Kobayashi Y., Kawachi I. Informal caregiving and mortality―Who is protected and who is not? A prospective cohort study from Japan. Social Science & Medicine. 2019;223:24–30. doi: 10.1016/j.socscimed.2019.01.034. [DOI] [PubMed] [Google Scholar]
- Miyawaki A., Tomio J., Kobayashi Y., Takahashi H., Noguchi H., Tamiya N. Impact of long-hours family caregiving on non-fatal coronary heart disease risk in middle-aged people: Results from a longitudinal nationwide survey in Japan. Geriatrics & Gerontology International. 2017;17(11):2109–2115. doi: 10.1111/ggi.13061. [DOI] [PubMed] [Google Scholar]
- Nomura S., Kawashima T., Yoneoka D., Tanoue Y., Eguchi A., Gilmour S., et al. Trends in suicide in Japan by gender during the COVID-19 pandemic, up to September 2020. Psychiatry Research. 2021;295 doi: 10.1016/j.psychres.2020.113622. [DOI] [PubMed] [Google Scholar]
- O'Connor R., Wetherall K., Cleare S., McClelland H., Melson A.J., Niedzwiedz C.L., et al. Mental health and well-being during the COVID-19 pandemic: Longitudinal analyses of adults in the UK COVID-19 mental health & wellbeing study. The British Journal of Psychiatry. 2020:1–8. doi: 10.1192/bjp.2020.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okubo R., Yoshioka T., Nakaya T., Hanibuchi T., Okano H., Ikezawa S., et al. Urbanization level and neighborhood deprivation, not COVID-19 case numbers by residence area, are associated with severe psychological distress and new-onset suicidal ideation during the COVID-19 pandemic. Journal of Affective Disorders. 2021;287:89–95. doi: 10.1016/j.jad.2021.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S.S. Caregivers' mental health and somatic symptoms during COVID-19. The Journals of Gerontology.Series B, Psychological Sciences and Social Sciences. 2021;76(4):e235–e240. doi: 10.1093/geronb/gbaa121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A., et al. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. The Lancet Psychiatry. 2020;7(10):883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M., Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychology and Aging. 2003;18(2):250–267. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- Rainero I., Bruni A.C., Marra C., Cagnin A., Bonanni L., Cupidi C., et al. The impact of COVID-19 quarantine on patients with dementia and family caregivers: A nation-wide survey. Frontiers in Aging Neuroscience. 2021;12 doi: 10.3389/fnagi.2020.625781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth D.L., Fredman L., Haley W.E. Informal caregiving and its impact on health: A reappraisal from population-based studies. The Gerontologist. 2015;55(2):309–319. doi: 10.1093/geront/gnu177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin R. COVID-19′s crushing effects on medical practices, some of which might not survive. JAMA. 2020;324(4):321–323. doi: 10.1001/jama.2020.11254. [DOI] [PubMed] [Google Scholar]
- Schonlau K.A. Selection bias in web surveys and the use of propensity scores. Sociological Methods & Research. 2009;37(3):291–318. [Google Scholar]
- Sheth K., Lorig K., Stewart A., Parodi J.F., Ritter P.L. Effects of COVID-19 on informal caregivers and the development and validation of a scale in English and Spanish to measure the impact of COVID-19 on caregivers. Journal of Applied Gerontology. 2021;40(3):235–243. doi: 10.1177/0733464820971511. [DOI] [PubMed] [Google Scholar]
- Sugiura K., Ito M., Mikami H. Evaluation of gender differences of family caregivers with reference to the mode of caregiving at home and caregiver distress in Japan. [Nihon Koshu Eisei Zasshi] Japanese Journal of Public Health. 2004;51(4):240–251. [PubMed] [Google Scholar]
- Tabuchi T., Kiyohara K., Hoshino T., Bekki K., Inaba Y., Kunugita N. Awareness and use of electronic cigarettes and heat-not-burn tobacco products in Japan. Addiction (Abingdon, England) 2016;111(4):706–713. doi: 10.1111/add.13231. [DOI] [PubMed] [Google Scholar]
- Tabuchi T., Shinozaki T., Kunugita N., Nakamura M., Tsuji I. Study profile: The Japan "society and new tobacco" internet survey (JASTIS): A longitudinal internet cohort study of heat-not-burn tobacco products, electronic cigarettes, and conventional tobacco products in Japan. Journal of Epidemiology. 2019;29(11):444–450. doi: 10.2188/jea.JE20180116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamiya N., Noguchi H., Nishi A., Reich M.R., Ikegami N., Hashimoto H., et al. Population ageing and wellbeing: Lessons from Japan's long-term care insurance policy. Lancet (London, England) 2011;378(9797):1183–1192. doi: 10.1016/S0140-6736(11)61176-8. [DOI] [PubMed] [Google Scholar]
- Tanaka T., Okamoto S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nature Human Behaviour. 2021;5(2):229–238. doi: 10.1038/s41562-020-01042-z. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2020). Preventing and managing COVID-19 across long-term care services: Policy brief, 24 July 2020. Retrieved from https://apps.who.int/iris/handle/10665/333074.
- Statistics Bureau of Japan. (2016). Survey on time use and leisure activities. Retrieved from http://www.stat.go.jp/english/data/shakai/index.html. Accessed September 19, 2021.
- Tokunaga M., Hashimoto H., Tamiya N. A gap in formal long-term care use related to characteristics of caregivers and households, under the public universal system in Japan: 2001–2010. Health policy (Amsterdam, Netherlands) 2015;119(6):840–849. doi: 10.1016/j.healthpol.2014.10.015. [DOI] [PubMed] [Google Scholar]
- Tsapanou A., Papatriantafyllou J.D., Yiannopoulou K., Sali D., Kalligerou F., Ntanasi E., et al. The impact of COVID-19 pandemic on people with mild cognitive impairment/dementia and on their caregivers. International Journal of Geriatric Psychiatry. 2021;36(4):583–587. doi: 10.1002/gps.5457. [DOI] [PubMed] [Google Scholar]
- Twenge J.M., Joiner T.E. Mental distress among U.S. adults during the COVID-19 pandemic. Journal of Clinical Psychology. 2020;76(12):2170–2182. doi: 10.1002/jclp.23064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ueda M., Stickley A., Sueki H., Matsubayashi T. Mental health status of the general population in Japan during the COVID-19 pandemic. Psychiatry and Clinical Neurosciences. 2020;74(9):505–506. doi: 10.1111/pcn.13105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong S. Young carers in the NHS. The British Journal of General Practice. 2017;67(664):527–528. doi: 10.3399/bjgp17X693425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; Geneva: 2015. World report on ageing and health. [Google Scholar]
- Wright A., Salazar A., Mirica M., Volk L.A., Schiff G.D. The invisible epidemic: Neglected chronic disease management during COVID-19. Journal of General Internal Medicine. 2020;35(9):2816–2817. doi: 10.1007/s11606-020-06025-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto T., Uchiumi C., Suzuki N., Yoshimoto J., Murillo-Rodriguez E. The psychological impact of 'mild lockdown' in Japan during the COVID-19 pandemic: A nationwide survey under a declared state of emergency. International Journal of Environmental Research and Public Health. 2020;17(24):9382. doi: 10.3390/ijerph17249382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshioka T., Okubo R., Tabuchi T., Odani S., Shinozaki T., Tsugawa Y. Factors associated with serious psychological distress during the COVID-19 pandemic in Japan: A nationwide cross-sectional internet-based study. BMJ open. 2021;11(7) doi: 10.1136/bmjopen-2021-051115. e051115-051115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2021). WHO coronavirus (COVID-19) dashboard. Retrieved from https://covid19.who.int. Accessed August 11, 2021.
- Rakuten Insight, Inc. (2021). About us: Rakuten insight. Retrieved from https://insight.rakuten.co.jp/en/aboutus.html. Accessed September 19, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.