Abstract
Aims
This study aims to establish the feasibility, safety, and efficacy of outpatient intravenous (IV) diuretic treatment for the management of decompensated heart failure (HF) for patients enrolled in the HeartFailure@Home service.
Methods and results
We retrospectively analysed the clinical episodes of decompensated HF for patients enrolled in the HeartFailure@Home service, managed by ambulatory IV diuretic treatment either at home or on a day‐case unit. A control group consisting of HF patients admitted to hospital for IV diuretics (standard‐of‐care) was also evaluated. In total, 203 episodes of decompensated HF (n = 154 patients) were evaluated. One hundred and fourteen episodes in 79 patients were managed exclusively by the ambulatory IV diuretic service—78 (68.4%) on a day‐case unit and 36 (31.6%) domiciliary; 84.1% of patient episodes under the HF@Home service were successfully managed entirely in an out‐patient setting without hospitalization. Eleven patients required admission in order to administer higher doses of IV diuretics than could be provided in the ambulatory setting. During follow‐up, there were 20 (17.5%) 30 day re‐admissions with HF or death in the ambulatory IV group and 29 (32.6%) in the standard‐of‐care arm (P = 0.02). There was no difference in 30 day HF readmissions between the two groups (14.9% ambulatory vs. 13.5% inpatients, P = 0.8), but 30 day mortality was significantly lower in the ambulatory group (3.5% vs. 21.3% inpatients, P < 0.001).
Conclusions
Outpatient ambulatory management of decompensated HF with IV diuretics given either on a day case unit or in a domiciliary setting is feasible, safe, and effective in selected patients with decompensated HF. This should be explored further as a model in delivering HF services in the outpatient setting during COVID‐19.
Keywords: Heart failure, Intravenous, Diuretics, Ambulatory, Elderly
Introduction
Heart failure (HF) is one of the commonest causes for unplanned hospitalization. 1 , 2 It accounts for approximately 2% of the total healthcare budget in the UK, and the majority of these costs are attributable to hospitalization. 3 Contemporary management of a long‐term condition ideally involves an outpatient service equipped to manage episodes of disease instability without hospital admission. 4 In cases where self‐care or supervised up‐titration of oral diuretics have proved ineffective, evidence is growing to support the safe and effective administration of intravenous (IV) diuretics in a community setting. 5 , 6 , 7 Previous work has demonstrated that community‐based IV diuresis is cost‐effective and popular with patients. 6 Despite these findings, adoption of ambulatory IV diuretic therapy has not been widespread and has yet to be formally recommended in either European or North American guidelines. Presently, the practice remains limited to a small number of centres. 5 , 8 , 9 , 10 , 11 , 12 Moreover, while the use of IV diuretics in a day‐unit setting for the treatment of decompensated HF has been described, there is little published on the utility and safety of domiciliary IV diuretics (i.e. administered in the patient's own home). 6 Faced with changes in healthcare delivery during the COVID‐19 pandemic where there is a need to deliver effective services while protecting our most vulnerable and highest risk patients from nosocomial COVID‐19 transmission, there is an urgent need to explore alternative management strategies that are at least as effective and safe as inpatient treatment. Older patients in particular, who are at a higher risk of COVID‐19 complications, have the most to gain from a shift in care from the inpatient to outpatient setting. 13 , 14 , 15 , 16 , 17 Finally, treating selected patients with decompensated HF outside hospital has the potential to improve patient experience, reduce in‐patient bed days, and reduce cost.
The ‘HeartFailure@Home’ service was introduced at our institution with the aim of providing ambulatory IV diuretics (both domiciliary and on a day‐unit) for selected patients with decompensated HF. The aim of the current study was to (i) examine the feasibility, safety, and efficacy of outpatient IV diuretic treatment for the management of decompensated HF and (ii) to examine healthcare utilization for patients enrolled in the HeartFailure@Home service compared with a consecutive sample of patients (controls) who received inpatient IV diuretics (usual care).
Methods
Study design and setting
A retrospective single site observational analysis was performed using data collected as part of routine clinical care (undertaken in accordance with the STROBE statement for reporting observational studies), 18 for patients aged 18 and over with decompensated HF undergoing intravenous (IV) diuretic treatment in an ambulatory setting (day‐unit or domiciliary treatment) between 1 June 2015 and 13 September 2018. The control group consisted of patients admitted to the hospital with an acute HF syndrome who were treated with IV diuretics as per usual guideline recommendations during the same time period.
Manchester Royal Infirmary (MRI) offers tertiary specialist cardiology services to the Greater Manchester region, as well as having a large Emergency Department and General Internal Medicine Department. The hospital typically sees 550 admissions annually with a primary diagnosis of HF, equating to approximately 8000 inpatient bed days. The ‘HeartFailure@Home’ ambulatory service was introduced in 2015 to offer ambulatory IV diuretics to selected patients with decompensated HF, either in the patient's home (home IV) or on a day unit to avoid admission to hospital. Clinical care is delivered by a multidisciplinary team of two consultant cardiologists and a team of specialist nurses.
The HeartFailure@Home model used existing clinical resources and services to facilitate the delivery of IV diuretics in an outpatient setting. We used the IV adult community therapy team (IV‐ACT), who typically administer domiciliary IV antibiotics, to facilitate IV diuresis in patient's own homes, and the hospital day unit (located within the hospital premises) to deliver IV diuretics in an ambulatory setting.
Participants
Ambulatory intravenous diuretic patients
Adults with a primary diagnosis of decompensated HF, refractory to escalating doses of oral diuretics and known to the HF service, were considered for ambulatory IV diuretics. Prior to referral to the HeartFailure@Home service, all patients were assessed by a HF specialist and confirmed to meet the inclusion/exclusion criteria shown in Table 1 and Figure 1 . Generally, higher risk patients on an active treatment strategy were favoured towards care on the day unit because this facilitated clinical review by an HF specialist if required.
Table 1.
Inclusion and exclusion criteria for management by the HeartFailure@Home service
| HeartFailure@Home patient inclusion criteria | |
| (1) | Adult patients in the community with decompensated chronic heart failure who have failed to respond to increasing doses of oral diuretic treatment |
| (2) | Inpatients with decompensated heart failure receiving IV diuretics who were willing and able to complete their IV diuretic treatment on an outpatient basis |
| HeartFailure@Home patient exclusion criteria | |
| (3) | Patients with haemodynamic instability or new oxygen requirement |
| (4) | Episode of decompensation deemed secondary to a new or uncontrolled atrial arrhythmia |
| (5) | Decompensated heart failure associated with acute kidney injury |
| (6) | Patients who require admission due to another acute medical illness |
| (7) | Patients with untreated severe valvular heart disease unless already assigned to a palliative management strategy |
| (8) | Patients unwilling to receive treatment as an outpatient |
| (9) | Patients requiring additional functional or social support which was not feasible to arrange in the community setting |
Figure 1.
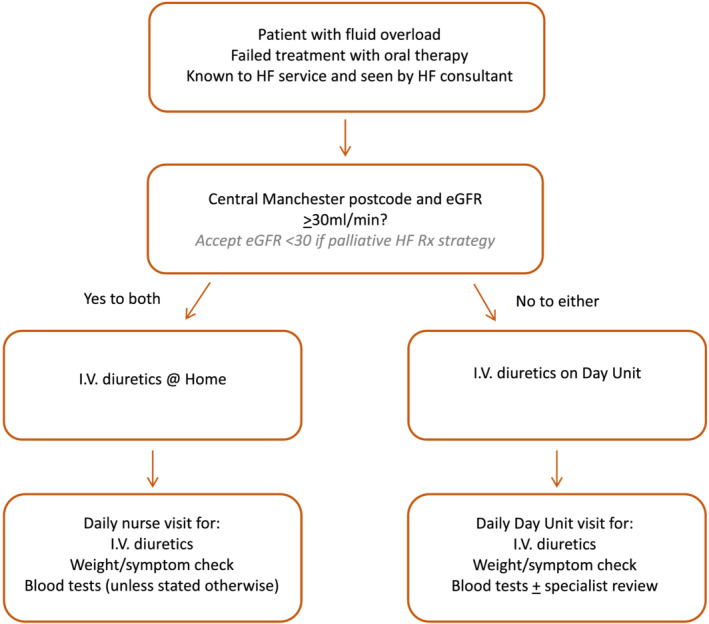
HeartFailure@Home pathway for ambulatory IV diuretics (domiciliary and day unit).
Intravenous diuretics were prescribed as a single daily infusion of furosemide (up to a maximum of 240 mg, given over a duration of up to 1 h, depending on dose). Patients were advised to restrict their fluid intake, usually to a daily limit of 1500 mL. General restriction of dietary sodium was also advised, although not to a pre‐specified limit. Depending on the degree of volume overload, haemodynamic status, and renal dysfunction, patients were advised to either stop, adjust, or continue their usual oral diuretics while receiving IV furosemide. In cases where recompensation of HF was not achieved due to inadequate diuresis at maximum diuretic dose, and provided both renal function and haemodynamics were satisfactory, adjunctive oral thiazide diuretic could be added at the discretion of the physician. For patients receiving IV diuretics at home, IV treatment was available 7 days per week. For patients receiving IV diuretics on the day unit, IV treatment was only available during week days; oral diuretics were given on weekend days.
For patients receiving home IV diuretics, treatment was administered by a specialist nurse from the IV‐ACT team. During the daily visit, vital signs (heart rate, blood pressure, oxygen saturation) and body weight were recorded, as well as a subjective assessment of change in overall clinical status, including severity of peripheral oedema. An intravenous cannula was inserted to administer IV furosemide, if not already present. Blood was taken daily for biochemistry (‘renal profile’, including serum sodium, potassium, urea, and creatinine, and ‘hepatic profile’, including serum alkaline phosphatase, alanine transaminase, albumin, total protein, and bilirubin); blood was taken for haematology (full blood count) every 3 days. All of these tasks were within the usual skillset of the IV‐ACT specialist nurses, and as such, no further specific clinical training was required for these nurses.
The aforementioned information (blood results, vital signs, weight, subjective clinical assessment, and dose of diuretic administered) was relayed to the specialist HF team in the hospital electronically each day; further instructions, including continuation, escalation, or discontinuation of IV therapy, were then relayed back to the IV‐ACT team for the following day.
For the purpose of this evaluation, a treatment episode for ambulatory IV patients began on the first day of IV diuretic treatment and ended on the last day of IV diuretic treatment.
Control group
A control group of ‘usual care’ patients admitted to hospital with decompensated HF via the emergency department or acute medical unit was also evaluated. Data for this group were obtained by screening HF admission records for the period between 20 June 2017 and 13 December 2018. Patients with a primary (i.e. at admission) diagnosis and discharge diagnosis of acute decompensated HF were included, to capture a group of patients with fluid congestion due to HF as their sole reason for hospitalization. All patients were commenced on IV diuretics within 48 h of admission and had no other identifiable acute illness. All patients were reviewed by the HF service during their inpatient stay and received HF follow‐up on discharge; all patients were given similar advice on fluid and salt restriction as for the ambulatory IV diuretic group. Patients with a new diagnosis of HF were excluded, as were patients with clinical evidence of significant pulmonary oedema or acute renal impairment at initial presentation, patients with an arrhythmia that contributed significantly to their hospitalization, e.g. atrial fibrillation with rapid ventricular rate, those who underwent invasive diagnostic or therapeutic procedures, cases requiring ITU care for circulatory support or invasive/non‐invasive ventilation, cases where admission was complicated by hospital acquired infection (HAI), or where the presence of social factors impacted on discharge. Patients in the usual care arm had not previously been assessed using the HeartFailure@Home criteria as they were admitted via the emergency department or acute medical unit and as such had not previously received ambulatory IV diuretics. Admission and discharge dates were used to establish start and end dates of an episode. Cases where admission weight was not recorded or where drug chart information was incomplete or not available were excluded. Cases where ambulatory diuretics were administered to facilitate early discharge were excluded from both arms of the analysis. Taking these criteria into account, we then included data from a sample size of patients similar to that of the ambulatory IV diuretic group.
Variables and data sources
Baseline demographic data were collected for all patients at the time of their index referral to the HeartFailure@Home service. Clinical records were reviewed for patients in the usual care arm (Table 2 ). Data concerning dose and duration of IV furosemide, whether the patient was prescribed their usual oral diuretics or their treatment supplemented with a thiazide diuretic, were recorded. Baseline weight, full blood count, and renal profile were measured prior to commencing IV diuretics. After commencing IV diuretics, clinical assessment, which included an assessment of peripheral oedema, measurement of blood pressure, pulse rate, oxygen saturations, and renal profile were assessed daily by specialist nurses, as described earlier. Body weight was monitored routinely, except in instances where the patient was immobile or nearing the end of life. Free text information was categorized retrospectively at the time of data extraction.
Table 2.
Patient characteristics
| In patients, n (%) | All HeartFailure@Home, n (%) | Inpatients vs. all HeartFailure@Home, P‐value | Heart Failure@Home | |||
|---|---|---|---|---|---|---|
| Day unit, n (%) | Home IV, n (%) | Day unit vs. home IV, P‐value | ||||
| Number of patients a | 75 | 79 | 53 | 32 | ||
| Total number of treatment episodes | 89 | 114 | 78 | 36 | ||
| Mean age (range) | 72 (36–94) | 77 (49–93) | 0.003* | 77 (60–92) | 77 (49–93) | 0.89 |
| Male (%) | 45 (60.0%) | 45 (57.0%) | 0.75 | 34 (64.2%) | 14 (43.8%) | 0.08 |
| HFREF (LVEF ≤40%) | 56 (74.7%) | 37 (46.8%) | 0.001* | 26 (49.1%) | 14 (43.8%) | 0.66 |
| Ischaemic heart disease | 38 (50.7%) | 40 (50.6%) | 1.00 | 30 (56.6%) | 15 (46.9%) | 0.5 |
| Atrial fibrillation/flutter | 40 (53.3%) | 52 (65.8%) | 0.14 | 34 (64.2%) | 20 (62.5%) | 1.00 |
| Chronic obstructive airways disease | 12 (16.0%) | 31 (39.2%) | 0.002* | 17 (32.1%) | 18 (56.3%) | 0.04* |
| Diabetes mellitus | 39 (52.0%) | 29 (36.7%) | 0.07 | 23 (43.4%) | 7 (21.9%) | 0.18 |
| Hypertension | 42 (57.3%) | 51 (64.6%) | 0.32 | 35 (66.0%) | 19 (59.4%) | 0.64 |
| CKD stage 3 or greater | 47 (62.7%) | 51 (64.6%) | 0.87 | 46 (86.8%) | 10 (31.3%) | <0.001* |
| Palliative management strategy | 5 (6.7%) | 25 (31.6%) | <0.001* | 20 (37.7%) | 10 (31.3%) | 0.64 |
| Patients with HFH in the 12 months prior to first episode | 25 (33.3%) | 40 (50.6%) | 0.03* | 25 (47.2%) | 20 (62.5%) | 0.19 |
| HFH in the 12 m prior to first episode | ||||||
| N = 0 | 50 (66.7%) | 39 (49.4%) | 28 (52.8%) | 12 (37.5%) | ||
| N = 1 | 15 (20.0%) | 20 (25.3%) | 13 (24.5%) | 8 (25.0%) | ||
| N = 2 | 3 (4.0%) | 11 (13.9%) | 5 (9.4%) | 8 (25.0%) | ||
| N ≥ 3 | 7 (9.3%) | 9 (11.4%) | 7 (13.2%) | 4 (12.5%) | ||
| Total number of inpatient days due to HFH in 12 months pre‐first episode | 606 | 1008 | 0.07 | 547 | 642 | 0.06 |
HF@H, Heart Failure at Home service; HFREF, heart failure with reduced ejection fraction; LVEF, left ventricular ejection fraction; CKD, chronic kidney disease.
Six patients used both home IV and day unit for different episodes.
Statistical significance (P < 0.05).
Hospitalization data concerning length of stay, 30 day readmissions, heart failure hospitalizations (HFH) in the 12 months before and after index treatment episode for patients in both groups, and 12 month mortality were recorded using electronic health records and local hospital episodes statistics (HES) data.
Definitions
Uncomplicated HeartFailure@Home episode
This was defined as (i) re‐compensation of a decompensated patient, where treatment was delivered entirely in an outpatient setting (admission avoidance).
Complicated HeartFailure@Home episode
Where treatment was complicated by (i) acute kidney injury (AKI) stage 1, defined as increased serum creatinine >1.5‐fold two‐fold from baseline, 19 or (ii) where hospitalization was necessitated prior to the end of that treatment episode (either related to the episode of decompensation that required a higher dose of diuretics than could be administered in an ambulatory setting, or due to alternative acute medical problem).
Uncomplicated heart failure hospitalization in the control group
This is defined as admission with subsequent re‐compensation and discharge from hospital, not complicated by AKI.
Complicated heart failure hospitalization in the control group
This is defined as admission where either the patients did not recompensate, developed AKI ≥ stage 1or died.
Statistical analysis
Data were collected and managed on Microsoft Excel 2016. Statistical analyses were performed using MATLAB version R2019a. Data are presented as mean (range), median (range/IQR), or N (%) as appropriate. Categorical data were compared using Fisher's exact test, and continuous data were compared using Student's t‐test in the case of normal distribution or Mann–Whitney U test in non‐normal distribution. A P value <0.05 was considered statistically significant: MD = mean difference, 95% CI = 95% confidence intervals, IQR = interquartile range, SD = standard deviation.
Results
Patient population
In total, 203 episodes of decompensated HF (n = 154 patients) were evaluated. One hundred and fourteen episodes of decompensated HF, occurring in 79 patients, were managed by the ambulatory HeartFailure@Home service. All patients were reviewed by a HF specialist and trialed on increased oral diuretics before being referred to either arm of the service and commencing IV diuretics; 78/114 (68.4%) episodes were managed on the day‐case unit; 36/114 (31.6%) were managed in the patient's own home. Twenty patients had more than one treatment episode, and six patients used both the day unit and domiciliary arms of the service during follow‐up. In the control group, 89 episodes of decompensated HF (n = 75 patients) were managed according to standard of care with inpatient IV diuretics.
Characteristics
Baseline demographic data are presented in Table 2 . This represents three heterogeneous groups [the ambulatory IV diuretic group, which was subdivided into groups of patients managed on the day unit or home IV group, and the usual care group (inpatients)]. Ambulatory IV diuretic patients (both day unit and home IV) were older than those managed as inpatients (77.1 vs. 71.2 years; MD = 5.9, 95% CI = 1.84–9.90, P = 0.005). Although the sex distribution was similar between all ambulatory IV patients and inpatients, a higher proportion of day unit patients were male (64.2% day unit vs. 43.8% home IV, P = 0.08). Significantly more patients in the day unit group had CKD ≥ stage 3 at baseline compared with both home IV patients (P < 0.001) and inpatients (P = 0.003).
Significantly more patients in the ambulatory group had a history of recent HF hospitalization (50.6% vs. 33.3%, P = 0.03). In the 12 months prior to their enrolment into the HeartFailure@Home service, 40 patients had been hospitalized on a total of 79 occasions with a primary diagnosis of HF, with nine patients (11.4%) hospitalized on three or more occasions during that period. A higher proportion of patients in the ambulatory IV diuretic were established on a palliative management pathway (commenced either prior to or during the treatment episode) compared with inpatients (31.6% vs. 6.7%; P < 0.001).
Diuretic treatment
Median duration of IV diuretic treatment was similar across both the inpatient group and ambulatory group [7 (IQR 5.75) vs. 6 (IQR 10) days, P = 0.3] (Table 2 ).
Concomitant use of thiazides was significantly higher among inpatients (36.0% vs. 14.1%; P < 0.01), as was mean weight loss from start to end of treatment (4.9 vs. 3.1 kg, MD = 1.8, 95% CI = 0.2–3.4, P = 0.03). There was no difference in mean weight loss per episode between home IV and day‐unit cases (3.1 kg).
Treatment outcomes
Similar proportions of patients, managed by the ambulatory service and as inpatients, had an uncomplicated treatment episode (84.1% vs. 82.1%; P = 0.84). AKI occurred more frequently in the standard of care group (AKI 8.3%, P = 0.03).
Episode outcomes (uncomplicated vs. complicated episode data) were evaluated for 172 (84.7%) episodes [84/89 (94.4%) standard of care and 88/114 (77.2%) HeartFailure@Home cases] (Table 3). Of these, 74 episodes (84.1%) were successfully managed by the HeartFailure@Home service and re‐compensated without hospitalization at any point during the treatment episode. Eleven patients (14.1%) in the day unit arm and two patients (5.6%) in the home IV arm required hospitalization. The majority of these were admitted in order to administer higher doses of intravenous diuretics than could be provided in an outpatient setting according to the protocol in place at the time (over 240 mg Furosemide once daily). One patient (1.2%) in the day unit arm developed AKI stage 1 requiring hospitalization during the course of treatment and was admitted for observation while treatment continued. There were no instances of AKI in the home IV arm.
Table 3.
Treatment episodes
| Inpatients (n) | HeartFailure@Home | |||
|---|---|---|---|---|
| All | Day unit | Home IV | ||
| Number of patients (n) | 75 | 79 a | 52 | 33 |
| Number of episodes (n, %) | 89 | 114 | 78 | 36 |
| Median duration of IV diuretic treatment (days, range) | 7, range 1–43 (data for 84 episodes) | 6 (range 0–36, data for 98) | 6, range 0–36, (data for 70 episodes) | 7, range 1–14 (data for 28 episodes) |
| Concomitant thiazide prescription (%) | 27 (36.0%) | 12 (14.1%) | 10 (19.2%) | 2 (6.1%) |
| Mean weight loss (kg, range) | −4.9 kg (−26.6 kg to +4.0 kg) (data for 77 episodes) | −3.1 kg (−8.9 to 1.2 kg) (data for 60 episodes) | −3.1 kg (−3.8 to +1.2 kg) (data for 44 episodes) | −3.1 kg (−8.2 to + 0.6) (data for 16 episodes) |
| Episode outcomes | ||||
| Uncomplicated episodes (n, %) | 69 (82.1%, data for 84 episodes) | 74 (84.1%, data for 88 episodes) | 52 (81.3%, data for 64 episodes) | 22 (91.7%, data for 24 episodes) |
| Complicated episodes b (n, %) | ||||
| Hospitalization | NA | 13 (11.4%) | 11 c (14.1%) | 2 d (5.6%) |
| AKI | 7 (8.3%, data for 84 episodes) | 1 (1.2%, data for 87 episodes) | 1 (1.6%, data for 63 episodes) | 0 (data for 24 episodes) |
| Died during episode | 12 (13.5%) (five expected and seven unexpected) | 2 (2%) | 1 (1.3%) (expected) | 1 (2.8%) (expected) |
Data available for all episodes unless otherwise stated.
Six patients used both home IV and day unit for different episodes.
Some patients experienced more than 1 complication (e.g. hospitalized and then died)
Ten for higher dose diuretics and one due to transport issues.
Hyponatraemia, higher dose diuretics.
Twenty (25.3%) patients used the HeartFailure@Home service on more than one occasion. Of these, seven (35%) patients used the service more than twice. Three patients used the service on five occasions.
Heart failure hospitalization and death after index treatment episode
During follow‐up, patients were either readmitted with a primary diagnosis of heart failure or died within 30 days following 20 (17.5%) episodes in the ambulatory IV diuretic group and 29 (32.6%) episodes in the standard of care arm (P = 0.02). At 12 months, this increased to 61 (53.5%) episodes in the ambulatory IV arm and 60 (67.4.%) episodes for the inpatient group (P = 0.06). Three of the four patients in the ambulatory care arm who died within 30 days of treatment were on an established palliative care plan.
There was no difference in 30 day HF readmissions between the two groups (14.9% ambulatory vs. 13.5% inpatients, P = 0.8), but 30 day mortality was significantly lower in the ambulatory group (3.5% vs. 21.3% inpatients, P < 0.001) (Table 4 ).
Table 4.
Follow‐up data
| In patients | HeartFailure@Home | |||
|---|---|---|---|---|
| All | Day unit | Home IV | ||
| HFH or death within 30 days of end of episode | 29/89 (32.6%, 12 HFH, 19 deaths) | 20/114 (17.5%) | 15/78 (19.2%, 14 HFH, 2 deaths) | 5/36 (13.9%, 3 HFH, 2 deaths) |
| HFH or death within 12 months of end of episode | 60/89 (67.4%, 38 HFH, 34 deaths) | 61/114 (53.5%) | 45/78 (57.7%, 25 HFH, 28 deaths) | 16/36 (44.4%, 9 HFH, 11 deaths) |
HFH, heart failure hospitalization; HF@H, Heart Failure at Home service.
Discussion
In this study, the largest UK report on ambulatory IV diuretics with data spanning almost 3 years, we demonstrate that ambulatory IV diuretic treatment for decompensated HF affords a safe and effective alternative to hospitalization. The majority of ambulatory IV patients had an uncomplicated treatment episode, despite patients in our study being more elderly, with a high prevalence of CKD and other co‐morbid conditions. In particular, the incidence of AKI was lower in the ambulatory IV diuretic group compared with those managed as inpatients, and 30 day outcomes (re‐admission with a primary diagnosis of HF, or death) favoured those managed by the HeartFailure@Home service. In addition, despite the HeartFailure@Home patients being older, with a higher proportion established on a palliative management strategy (31.6%), rates of HF hospitalization or death were significantly lower at 30 days compared with patients treated as inpatients.
To date, the majority of data concerning ambulatory IV diuretics has focused on admission avoidance through use of day‐units (Supporting Information, Table S1 ). 20 The current study is novel in that our service configuration allowed patients to be stratified to either ambulatory treatment in a day‐unit setting, or domiciliary treatment; almost one‐third of episodes were managed in the patient's own home. Renal function, relative haemodynamic stability, frailty, where the patient lived, and patient choice were factors considered when determining place of treatment. Domiciliary IV diuretic treatment was associated with the lowest rates of conversion to inpatient treatment (5.6%), and there were no instances of AKI in this group.
Despite significant improvements in drugs and therapeutic devices used to treat HF, the number of patients being hospitalized due to HF continues to increase, in part due to the rising prevalence of cardiovascular disease and an aging population. Many patients are resistant to escalating doses of oral diuretics, and the only way to manage these cases has been to admit to hospital for IV diuretics. Once commenced on IV diuretic treatment, patients typically remain in hospital until they have recompensated and have been re‐established on oral diuretics. Moreover, in many instances, discharge does not swiftly follow recompensation. A lack of physical activity during hospitalization can lead to deconditioning, requiring physical therapy, which may delay discharge. 21
Hospitalization of HF patients, who are typically older with multi‐morbidity, is not benign—it is associated with significant morbidity and mortality. 22 Furthermore, HF patients represent an at‐risk group of patients from mortality particularly if infected with COVID‐19. There has been a move to reconfigure cardiac services to minimize hospital‐acquired COVID‐19 infection of those most vulnerable to adverse outcomes, such as elderly patients with cardiovascular diseases. Ambulatory HF diuretic services represent an alternative to admission, designed to deliver care in an outpatient or home setting.
While treatment for domiciliary (home IV) patients is supervised by hospital‐based HF teams, there are relatively fewer in‐person assessments undertaken directly by the HF team. Instead, there is a reliance on virtual specialist review, performed using monitored physiological parameters communicated electronically by community‐based services (IV‐ACT). It is unclear whether this multi‐agency approach to delivering care in the community, with daily remote HF team review of patient data and a standard operating policy outlining acceptable physiological parameters, was in part responsible for the lower number of adverse outcomes observed in the ambulatory IV group. Multi‐agency involvement, and the fact that the care plan/medical records for home IV patients were held by the patient, may have potentially led to an increase in the amount of self‐management advice, both passive and active.
The HeartFailure@Home clinical pathway primarily managed older patients, who typically have a higher burden of co‐morbidity than younger patients and are at higher risk of HF decompensation. This is of particular significance, as the mean age reported in the current evaluation is higher than that reported in previous studies evaluating the efficacy of IV diuretics in an ambulatory cohort (Supporting Information, Table S1 ). 5 , 8 , 9 , 10 , 11 , 12 , 23 , 24 , 25
A history of HF hospitalization was observed more frequently among the ambulatory IV diuretics group. Prior to initial enrolment on the HeartFailure@Home programme, the majority of patients (50.6%) had been hospitalized at least once with HF in the preceding 12 months, accounting for 1008 inpatient bed days. After enrolment in the HeartFailure@Home programme, 20 (25.6%) patients used the HeartFailure@Home service on two or more occasions, highlighting that this is a population of patients who decompensate frequently. Six (7.7%) patients used both arms of the service, highlighting the ability to tailor treatment according to clinical need and patient choice.
Over 30% of patients in the HeartFailure@Home programme were on a palliative management strategy. The higher use of palliative management strategies may have been influenced by a number of factors including higher incidence of previous HF admissions, older age, familiarity with patient's prognosis, and increased consultant cardiologist input. When the fact that hospitalization is unlikely to improve the prognosis is recognized, then provision of care outside the hospital environment may represent a more patient‐centric model and inadvertently improve care. The use of outpatient IV diuresis as part of an individualized end‐of‐life care plan has the potential to rapidly relieve distressing symptoms in a more comfortable setting. Provision of hospice services and subcutaneous furosemide is heterogenous, and perhaps, this model of care can fill a gap in care provision. This requires further evaluation and a separate body of work in conjunction with palliative care services; however, work so far has been promising.
Nineteen of 79 (24.1%) patients managed by the HeartFailure@Home service were non‐white ethnic minorities. Although some patients did not speak English, this was not a barrier to delivering care, either in a domiciliary setting or on the day unit. Perceived barriers to treatment were easily circumvented, and treatment in an ambulatory setting may have provided greater patient autonomy (e.g. residing in their home environment with unfettered access to usual support networks, uninterrupted observation of religious practices) (Figure 2 ).
Figure 2.
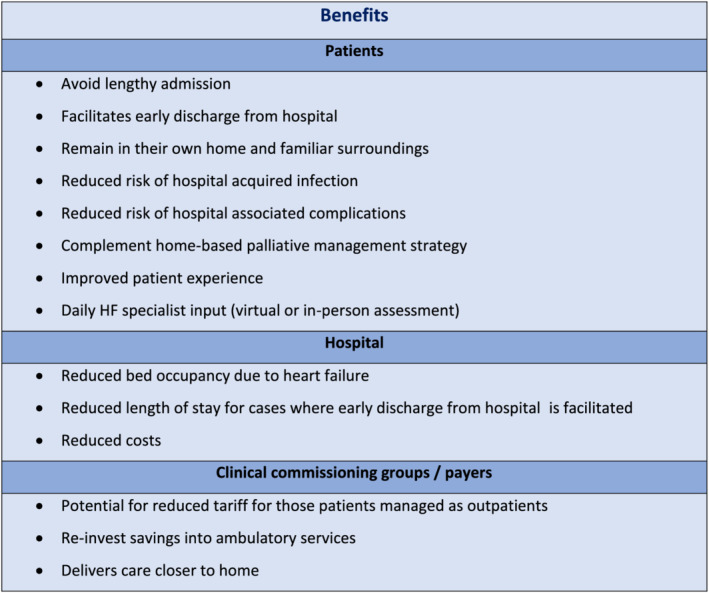
Potential beneficiaries of the HeartFailure@Home Service. Outlines the individuals/organizations who potentially stand to benefit from the HeartFailure@Home service. Crucially, the patient has the most to gain; they can remain in their own home for the duration of their treatment, avoiding exposure to hospital‐related complications such as infections, thrombosis, and functional decline. Care is overseen (virtually or in‐person) by an HF specialist.
The main clinical concern regarding safety of the HeartFailure@Home service was that IV diuretic therapy could precipitate hypotension and/or renal dysfunction, a particular concern in a domiciliary setting. Thirteen (11.4%) patient episodes on the clinical pathway required hospitalization, mainly for higher dose diuresis (one patient for hyponatraemia and one due to transport issues). No patient required hospitalization due to hypotension, and only one patient was hospitalized due to AKI. There is a paucity of published literature to compare our results with other centres. However, the admission rate for the HeartFailure@Home cohort is significantly lower than has been reported in previous studies. 5 , 7 , 26
Limitations
As a non‐randomized study the analysis is subject to the usual bias associated with observational data, and as described earlier, there were significant differences in the baseline characteristics between the groups. Additionally, the group sizes are small, limiting the strength of comparison between groups, and in particular interpretation of the outcome measures that we have reported should take this into account. Furthermore, the geographical area covered by the HeartFailure@Home service is relatively urban; thus, this model of care may not be generalizable to more rural areas or other healthcare systems. We report outcomes for a lower proportion of the HeartFailure@Home group (88/114 episodes; 77.2%) compared with the usual care group (84/89 episodes; 94.4%), in part due to the fact that treatment records for domiciliary and day unit patients were retained in the respective places of care, sometimes by the patient; this may introduce bias towards the HeartFailure@Home group by underestimating the number of complicated episodes in this group. Conversely, patients hospitalized with HF who experienced a HAI were excluded from this study in an attempt to closely match the two populations; had these patients been included, additional benefit from ambulatory IV diuretic treatment may have been more apparent. The relative impact of social circumstances on delays in discharge contributing increased length of stay was not examined. Finally, following the completion of domiciliary IV diuretic therapy, the home IV team would routinely visit the patient in their own home at ≤1 week to perform a repeat assessment of fluid status and check renal profile; the relative significance of this visit on downstream HFH is unclear and should be explored in future studies to assess the impact of post‐treatment domiciliary follow‐up on subsequent HFH.
Conclusions
Outpatient management of decompensated HF with IV diuretics is feasible, effective, and sustainable for patients of all ages. The HeartFailure@Home model of care has been achieved without specific additional funding or resource. A formal economic evaluation could provide a strong argument for nationwide service reconfiguration.
Conflict of interest
None declared.
Funding
F.Z.A. has previously received a research grant funded by Medtronic. F.Z.A. has received honoraria from Medtronic, Vifor, AstraZeneca, and Servier. J.K.T. has previously filled a research post funded by Medtronic. J.K.T. is currently funded by a British Heart Foundation Clinical Research Fellowship and is supported by the Peter Mount Award. A.M.Z. has received honoraria from Abbott, Boston Scientific, and Medtronic. C.C. has received speaking fees and honoraria from Medtronic and Abbott.
Supporting information
Table S1. Summary of published studies examining the role of ambulatory and domiciliary IV diuretic programmes.
Acknowledgements
We are grateful to Edward Doris, Claire Ashworth, Jane Fitchet, Christina Muldoon, Caroline Ustianowski, Ruth Wynn, and the IV‐ACT team who have supported delivery of this service.
Ahmed, F. Z. , Taylor, J. K. , John, A. V. , Khan, M. A. , Zaidi, A. M. , Mamas, M. A. , Motwani, M. , and Cunnington, C. (2021) Ambulatory intravenous furosemide for decompensated heart failure: safe, feasible, and effective. ESC Heart Failure, 8: 3906–3916. 10.1002/ehf2.13368.
References
- 1. Cowie MR, Anker SD, Cleland JGF, Felker GM, Filippatos G, Jaarsma T, Jourdain P, Knight E, Massie B, Ponikowski P, López‐Sendón J. Improving care for patients with acute heart failure: before, during and after hospitalization. ESC Heart Fail 2014; 1: 110–145. [DOI] [PubMed] [Google Scholar]
- 2. Braunschweig F, Cowie MR, Auricchio A. What are the costs of heart failure? EP Europace 2011; 13: ii13–ii17. [DOI] [PubMed] [Google Scholar]
- 3. Stewart S, Jenkins A, Buchan S, McGuire A, Capewell S, McMurray JJJV. The current cost of heart failure to the National Health Service in the UK. Eur J Heart Fail 2002; 4: 361–371. [DOI] [PubMed] [Google Scholar]
- 4. Collins SP, Pang PS, Fonarow GC, Yancy CW, Bonow RO, Gheorghiade M. Is hospital admission for heart failure really necessary?: the role of the emergency department and observation unit in preventing hospitalization and rehospitalization. J Am Coll Cardiol 2013; 61: 121–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ryder M, Murphy NF, McCaffrey D, O'Loughlin C, Ledwidge M, McDonald K. Outpatient intravenous diuretic therapy; potential for marked reduction in hospitalisations for acute decompensated heart failure. Eur J Heart Fail 2008; 10: 267–272. [DOI] [PubMed] [Google Scholar]
- 6. Brightpurpose . Evaluation of IV diuretics pilot for British Heart Foundation. Final report. June 2014.
- 7. Lee C, Beleznai T, Hassan S, Rawat A, Douglas H, Kanagala P, Sankaranarayanan R. Ambulatory management of acute decompensation in heart failure. Br J Hosp Med (Lond) 2019; 80: 40–45. [DOI] [PubMed] [Google Scholar]
- 8. Buckley LF, Carter DM, Matta L, Cheng JW, Stevens C, Belenkiy RM, Burpee LJ, Young MA, Weiffenbach CS, Smallwood JA, Stevenson LW, Desai AS. Intravenous diuretic therapy for the management of heart failure and volume overload in a multidisciplinary outpatient unit. JACC Heart Fail 2016; 4: 1–8. [DOI] [PubMed] [Google Scholar]
- 9. Makadia S, Simmons T, Augustine S, Kovell L, Harris C, Chibungu A, Parakh K. The diuresis clinic: a new paradigm for the treatment of mild decompensated heart failure. Am J Med 2015; 128: 527–531. [DOI] [PubMed] [Google Scholar]
- 10. Durango LF, Katz SD, Li HK, Wencker D. Abstract 1891: continuous furosemide infusion is safe and effective in outpatient treatment of refractory heart failure. Circulation 2006; 114: II_375–II_376. [Google Scholar]
- 11. Schipper JE, Domingo GR, Dickson VV, Katz SD. Implementation of tailored intravenous heart failure therapy in a non‐dedicated outpatient infusion center. J Card Fail 2012; 18: S104. [Google Scholar]
- 12. Hebert K, Dias A, Franco E, Tamariz L, Steen D, Arcement LM. Open access to an outpatient intravenous diuresis program in a systolic heart failure disease management program. Congest Heart Fail 2011; 17: 309–313. [DOI] [PubMed] [Google Scholar]
- 13. Kaye KS, Marchaim D, Chen TY, Baures T, Anderson DJ, Choi Y, Sloane R, Schmader KE. Effect of nosocomial bloodstream infections on mortality, length of stay, and hospital costs in older adults. J Am Geriatr Soc 2014; 62: 306–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Theisen S, Drabik A, Stock S. Pressure ulcers in older hospitalised patients and its impact on length of stay: a retrospective observational study. J Clin Nurs 2012; 21: 380–387. [DOI] [PubMed] [Google Scholar]
- 15. Deandrea S, Bravi F, Turati F, Lucenteforte E, la Vecchia C, Negri E. Risk factors for falls in older people in nursing homes and hospitals. A systematic review and meta‐analysis. Arch Gerontol Geriatr 2013; 56: 407–415. [DOI] [PubMed] [Google Scholar]
- 16. Cole MG. Delirium in elderly patients. Am J Geriatr Psychiatry 2004; 12: 7–21. [PubMed] [Google Scholar]
- 17. Rodríguez‐Pascual C, Vilches‐Moraga A, Paredes‐Galán E, Ferrero‐Marinez AI, Torrente‐Carballido M, Rodríguez‐Artalejo F. Comprehensive geriatric assessment and hospital mortality among older adults with decompensated heart failure. Am Heart J 2012; 164: 756–762. [DOI] [PubMed] [Google Scholar]
- 18. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, for the STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 2007; 4: e296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lopes JA, Jorge S. The RIFLE and AKIN classifications for acute kidney injury: a critical and comprehensive review. Clin Kidney J 2013; 6: 8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wierda E, Dickhoff C, Handoko ML, Oosterom L, Kok WE, Rover Y, Mol BAJM, Heerebeek L, Schroeder‐Tanka JM. Outpatient treatment of worsening heart failure with intravenous and subcutaneous diuretics: a systematic review of the literature. ESC Heart Fail 2020; 7: 892–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. De Klein K, Valkenet K, Veenhof C. Perspectives of patients and health‐care professionals on physical activity of hospitalized patients. Physiother Theory Pract 2019; 37: 307–314. [DOI] [PubMed] [Google Scholar]
- 22. Setoguchi S, Stevenson LW, Schneeweiss S. Repeated hospitalizations predict mortality in the community population with heart failure. Am Heart J 2007; 154: 260–266. [DOI] [PubMed] [Google Scholar]
- 23. Buckley LF, Stevenson LW, Cooper IM, Knowles DM, Matta L, Molway DW, Navarro‐Velez K, Rhoten MN, Shea EL, Stern GM, Weintraub JR. Ambulatory treatment of worsening heart failure with intravenous loop diuretics: a four‐year experience. J Card Fail 2019; 26: 798–799. [DOI] [PubMed] [Google Scholar]
- 24. Banerjee P, Tanner G, Williams L. Intravenous diuretic day‐care treatment for patients with heart failure. Clin Med (Lond) 2012; 12: 133–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Freimark D, Arad M, Matetzky S, DeNeen I, Gershovitz L, Morag NK, Hochberg N, Makmal Y, Shechter M. An advanced chronic heart failure day care service: a 5 year single‐center experience. Isr Med Assoc J 2009; 11: 419–425. [PubMed] [Google Scholar]
- 26. Barsuk JH, Gordon RA, Cohen ER, Cotts WG, Malkenson D, Yancy CW, Williams MV. A diuretic protocol increases volume removal and reduces readmissions among hospitalized patients with acute decompensated heart failure. Congest Heart Fail 2013; 19: 53–60. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Summary of published studies examining the role of ambulatory and domiciliary IV diuretic programmes.


