Abstract
Introduction
Online MRI guided adaptive radiotherapy (MRIgRT) is resource intensive. To maintain and increase uptake traditional roles and responsibilities may need refining. This novel study aims to provide an in-depth understanding and subsequent impact of the roles required to deliver on-line adaptive MRIgRT by exploring the current skills and knowledge of radiographers.
Method
A purposive sampling approach was used to invite radiographers, clinicians and physicists from centres with experience of MRIgRT to participate. Focus Group Interviews were conducted with two facilitators using a semi-structure interview guide (Appendix 1). Four researchers independently familiarised themselves and coded the data using framework analysis. A consensus thematic framework of ptive Radiotherapy codes and categories was agreed and systematically applied.
Results
Thirty participants took part (Radiographers: N = 18, Physicists: N = 9 and Clinicians: N = 3). Three key themes were identified: ‘Current MRIgRT’, ‘Training’ and ‘Future Practice’. Current MRIgRT identified a variation in radiographers' roles and responsibilities with pathways ranging from radiographer-led, clinician-light-led and MDT-led. The consensus was to move towards radiographer-led with the need to have a robust on-call service heavily emphasised. Training highlighted the breadth of knowledge required by radiographers including MRI, contouring, planning and dosimetry, and treatment experience. Debate was presented over timing and length of training required. Future Practice identified the need to have radiographers solely deliver MRIgRT, to reduce staff present which was seen as a main driver, and time and resources to train radiographers seen as the main barriers.
Conclusion
Radiographer-led MRIgRT is an exciting development because of the potential radiographer role development. A national training framework created collaboratively with all stakeholders and professions involved would ensure consistency in skills and knowledge.
Implications for practice
Role development and changes in education for therapeutic radiographers.
Keywords: Advanced practice, Adaptive radiotherapy, Professional roles, Workflow
Introduction
Advances in technology, such as image-guided radiotherapy (IGRT) and intensity-modulated radiotherapy (IMRT), have enabled delivery of increasing dose to tumours whilst minimising that to normal tissues and, thus, improving patient outcomes. Adaptive radiotherapy (ART) has potential to further improve patient outcomes by delivering radiotherapy according to the position of the patient and tumour at the time of treatment, and also the shape of the tumour and relative positions of organs at risk. On-line ART delivered using Magnetic Resonance Image (MRI) guidance (MRIgRT) involves adapting the treatment plan each day which brings a new level of responsibilities to the linac/patient interface. The main difference between conventional treatment delivery and MRIgRT is the former normally involves two radiographers and the latter a multidisciplinary team (MDT) comprising radiographers, doctors and physicists. The new workflow is therefore staff and delivery-time intensive.1,2
MRIgRT has only recently been clinically implemented with the first clinical treatment in 2014.2 Although uptake is increasing and more than 20 centres are delivering worldwide,2 this is small compared to conventional radiotherapy. To ensure widespread uptake and increased patient accessibility, the number of staff involved in the workflow will need to be reduced and refined which may mean traditional roles and responsibilities are no longer suitable.3 Previously, therapeutic radiographers' responsibilities have evolved alongside developments in treatment delivery and has included evaluating treatment portal images,4 verification images for hypofractionated treatments,5 and more recently selecting plan-of-the-day.6
Two workflows are available for use on Unity MR Linac (Elekta, Crawley, UK): Adapt to Shape (ATS) where target and/or organs at risk are recontoured and a new plan created, and Adapt to Position (ATP), a dose shift which requires adapting the multi leaf collimator leaves according to translational corrections. Roles and responsibilities of radiographers working on the MR Linac and delivering ATP workflow have been described in a single centre narrative.7 Although this workflow is similar to IGRT delivered on a C-arm linac, additional skills and knowledge were identified and focused on MRI aspects of the workflow. The additional skills required for on-line ART are acknowledged.7
This qualitative study aimed to provide an in-depth understanding of current and future roles and the impact on radiographer role when delivering on-line adaptive MRIgRT by exploring skills and knowledge required, at this early stage of technological advances.
Method
A purposive sampling approach and maximum variation sample strategy was used to recruit radiographers, clinicians and physicists from centres delivering MRIgRT via email. Participants from six centres were chosen to reflect varied experience (Table 1): two early implementation centres, two recently implemented and two yet to deploy MRIgRT. Local Committee for Clinical Research (CCR), Health Regulations Authority, and Health and Care Research Wales approval was obtained.
Table 1.
Focus group (FG) and individual interview (II) participants.
| Study No. | Location | Centres represented | Type | Participant information | Total |
|---|---|---|---|---|---|
| FG 1 | MRL consortium | 2: Over 2 years experience – The Netherlands | Focus group | Therapeutic Radiographers (n = 3) | 3 |
| FG 2 | MRL consortium | 2: Not started – Australia and UK | Focus group | Therapeutic Radiographers (n = 4) and Physicist (n = 1) | 5 |
| FG 3 | UK Hospital Site | 1: 0–2 years experience - UKa | Focus group | Therapeutic Radiographers (n = 3), Physicists (n = 4) and Clinician (n = 1) | 8 |
| FG 4 | UK Hospital Site | 1: 0–2 years experience - UKa | Focus group | Therapeutic Radiographers (n = 5) and Physicist (n = 1) | 6 |
| FG 5 | UK Hospital Site | 1: 0–2 years experience - UKb | Focus group | Therapeutic Radiographers (n = 2), Diagnostic Radiographer (n = 1), Physicists (n = 3) and clinician (n = 1) | 7 |
| II 6 | UK Hospital Site | 1: 0–2 years experience - UKb | Individual interview | Clinician (n = 1) | 1 |
Same UK centre.
Same UK centre.
Data collection through Focus Group Interviews (FGIs) were chosen to allow participants to expand on each other's responses and the researcher to obtain several perspectives and reach consensus.8, 9, 10 FGIs were limited to between 6 and 8 members10 and conducted with two facilitators using a semi-structure interview guide (Appendix 1).
Participants were consented prior to FGI, informed they were able to withdraw at any point and were assured of anonymity and dissemination. FGIs lasted between 40 and 120 minutes and were recorded and transcribed verbatim. Individual interviews were offered if a key member of the MRIgRT pathway was unavailable to attend the FGI sessions and one was performed.
Framework Analysis9,11 was used to synthesise the data. Four researchers, two familiar with the workflow (EJ, HMcN) and two who had only observed (GO’G, TW) independently conducted preliminary analysis on the same FGIs. A consensus thematic framework of codes and categories was developed and systematically applied (EJ). The final framework was agreed by all.
Results
A total of thirty professionals participated in FGIs. Participants represented three main professional groups involved in MRIgRT (Table 1); Radiographers (n = 18), Physicists (n = 9) and Clinicians (n = 3). Prior experience varied: radiographers (minimum:4 years), physicists (minimum:3 years). All clinicians were consultant clinical oncologists (minimum:2 years).
From the framework analysis (Appendix 2), three key themes were identified (Table 2): -
-
(i)
Current MRIgRT practice-roles of professional groups across different workflows used in MRIgRT and impact on the team.
-
(ii)
Training - methods, timings and processes.
-
(iii)
Future practice - barriers and drivers present in developing and implementing MRIgRT.
Table 2.
Key themes.
| Current ART practice | Roles |
| Responsibilities | |
| Professional feelings | |
| Training | Prior experience/Baseline knowledge and experience |
| Pre-MRL | |
| Current | |
| Future requirements | |
| Radiographer-led ART | Barriers |
| Drivers | |
| Operational gaps |
Current MRIgRT practice
Descriptions of roles and responsibilities of professional groups varied throughout FGIs due to differences in MRIgRT pathways used (Table 3).
Table 3.
Workflows used by each Focus group (FG).
| Study No. | Pathway | Sites? | Patient set-up | Image acquisitions | Image registrations | Contouring tumour | Contouring organs at risk | Decision to replan/recontour | Plan creation | Plan checking | Decision to treat with adapted plan | On-call provision |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FG1 | Radiographer-led ATS | All standard sites | R | R | R | R | R | R | R | R | R | R, P, C |
| Radiographer-led ATS with clinician present #1 | Complex cases – discussed in meeting prior to treatment | R | R | R | R | R | R + C | R | R | C | R, P | |
| FG3 | Clinician-light ATP | Prostate | R | R | R | N/A | N/A | P | P | P | R | C |
| FG4 | Clinician-light ATP | Prostate | R | R | R | N/A | N/A | P | P | P | R | C |
| FG5 | MDT-led ATS | All standard sites | R | R | R | C | C | C | P | P | R + C | N/A |
| II6 | MDT-led ATS | All standard sites | R | R | R | C | C | C | P | P | R + C | N/A |
R: Radiographer. P: Physicist. C: Clinician.
Note: FG 2 excluded as not yet treating or finalised workflow and pathway (FG: Focus group. II: Individual interview. ATP: Adapt to position. ATS: Adapt to shape).
Roles
Some participants mentioned that radiographers were trained to undertake the entire MRIgRT pathway which had eliminated the need for other professionals. This was achieved by splitting radiographers into two profiles: A) MRI application and planning, and B) MRI application, clinical image processing and contouring. Other participants described training occurring ‘on-the-job’. For radiographer-led treatments, most participants mentioned the need to reduce numbers of professionals present to limit resources required. However, there was a comment about expansion of the MDT for complex cases:
“If we moved to an area like Hepatobiliary, is whether you'd then bring your radiologist … it's how confident that clinician would be at contouring certain tumours” (FG5)
An inclusive rota, to ensure adequate skill-mix, was described as two-three radiographers always present with on-call availability of physicists and clinicians. It was agreed that having a clinician present was not sustainable and the importance of sufficiently trained on-call staff expressed:
“Some doctors who have been charged with being the on-call doctor to make those decisions aren't necessarily experts in that tumour site or on the MR Linac” (FG3)
The importance of continuity and only relevant staff present in designated areas when treatment is undertaken was highlighted.
Responsibilities
Radiographers remained responsible for setup, patient safety and equipment in addition to image acquisition and treatment delivery (Table 3). Clear and defined roles and responsibilities prior to implementation, despite treatment pathway differences, was asserted:
‘‘It really needs that roles and responsibilities … that says … this is your role. These are the decisions that you're making in relation to these aspects, and at the end of your decision making it goes to the next person over there’’ (FG2)
Participants specified that all MRIgRT professionals were responsible for keeping the working environment free from distractions to maintain patient focus, and a high level of professional demeanour and respect was always required. Particularly within the high-pressured environment of MRIgRT where each task is performed online and observed by all professionals. Exceptional communication and dynamic professional working styles were highlighted:
“There's a lot of communication before we start with the patient” (FG1)
‘‘…as long as people respect each other and it's a clear line of what the actions should be,then it's great to have the experience and the input of different groups’’ (FG2)
“That communication tool comes in handy then because if it's not the same physicist and notthe same on-call physicist tomorrow”
“everybody either knew that information or could access it very quickly to make those decisions on the day’’ (FG3)
Weekly MDT meetings were expressed as an effective way to maintain communication whilst developing and refining working practices and provide an effective forum to develop and review documentation, thus producing a robust safety framework:
‘‘You've got people who've got different skills … going through the whole process and the scenarios … as a team … that's essential’’ (FG2)
‘‘MRI radiographers wanted to just double check that we were being sensible’’
“There's been quite good learning together and building the team, as well as building the work practices so that you're all fitting into the jigsaw'” (FG3)
Professional feelings
Participants were positive about tangible patient benefit alongside integration of new technology into current practice:
“We're using this equipment to its fullest capabilities … We're reassured that there's so many inbuilt checking procedures … we're doing something that's quite pioneering, it's also quite safe. Safety and accuracy is what radiotherapy is all about” (FG3)
To facilitate professionals other than radiographers in control areas, adjustments were necessary. Negative impressions included it being ‘dire’ at the beginning (radiographers), being ‘watched’ whilst undertaking their role (physicists) and lack of engagement amongst some professionals. However, all commented on positive aspects of working as an MDT:
“It is challenging to do … offline you do it in a fairly quiet environment. I think online can be quite busy … things going on, and to focus on what you're supposed to be picking up on is difficult”
“It's been really interesting … the MR-linac is that kind of pinnacle of cross-professional sort of working. It involves input from so many different people to get each stage of the adaptive workflow doing what it needs to do” (FG5)
A strong working MDT environment, not only internally for the team and patients but also externally with consortium collaboration and wider MDT, was agreed. Radiographer participants were positive about validation received from other professional groups. Those working in radiographer-led pathways confirmed the presence of other professional groups was missed, however, they still felt part of the wider MDT and it was empowering to deliver MRIgRT:
“I really … enjoyed working as part of a multi-disciplinary team, which is probably the first time I've really done that since I've worked here” (FG2)
“Every day's different … It's a lot closer together with … other members of the MDT. I've never spent quite so much time with the doctors and the physicists. I've sat next to them working with them rather than just you might be near them … we work together every day now” (FG3)
Training
Baseline knowledge: The level of baseline knowledge and prior experience varied across FGIs. All participants mentioned the need to have extensive experience regarding patient position, problem-solving, soft-tissue knowledge and imaging, gained by working on conventional C-Arm linacs which remained important in the MRIgRT pathway. Some expressed that many centres had experience with ART such as plan-of-the-day and on-line brachytherapy, and these skills could be transferable. Some radiographers expressed that planning and dosimetry experience was essential to implement radiographer-led pathways, whereas others mentioned this experience would be ideal.
Although a desired skill mentioned was MRI knowledge, there was variation across groups. In some centres a level of competence was required; others deemed it part of initial training. There was concern about gaining familiarity and experience in centres without MRI access and resources. It was also expressed that mixed modality imaging was the future of radiotherapy and undergraduate and postgraduate training programmes should account for this:
“That's something that needs addressing for radiotherapy in general … it's only going to become more important … I've had no formal training in it whatsoever. I've just had to pick it up over the years that I've been using it” (FG2)
All radiographers agreed that excellent communication skills and the ability to work in and create an environment that promotes feedback and reflection within the MDT was important.
Pre-MRIgRT and On-MRIgRT: All groups reported internal and external resources in multiple formats by multiple professionals were available to supplement MRI training (Table 4). Most stated the majority of training needed to be undertaken in the pre-MRIgRT stage and a vital component was gaining experience in diagnostic MRI. Apprehension was expressed in centres with no MRI on-site to facilitate training.
Table 4.
Pre and current MRIgRT training in each focus group.
| Study No. | Occurrence | MR: Physics, patient set-up, safety, image interpretation and application | Planning and dosimetry experience | Contouring | Run-throughs |
|---|---|---|---|---|---|
| Focus group 1 | Pre | In-depth training programme for all radiographers | In-depth training programme for all radiographers | Occurs | |
| Focus group 1 | Current | One-week intensive top-up | One-week intensive top-up | In-depth training programme per site | |
| Focus group 3 | Pre | Rotation into MR department for core radiographers | Lack of available resources | Occurs | |
| Focus group 3 | Current | New radiographers have a rotational placement | No formal training | Initial training sessions for prostate | |
| Focus group 4 | Pre | Informal training not moderated or planned | Lack of available resources | Occurs | |
| Focus group 4 | Current | Practical workbook | No formal training | No formal training | |
| Focus group 5 | Pre | Current | Lack of available resources | Occurs | |
| Focus group 5 | Current | Practical workbook | No formal training | No formal training |
One group demonstrated a training programme for planning and dosimetry pre-MRIgRT for radiographers, and others expressed a preference for such a programme. Participants relayed the optimal way to achieve and maintain competency was through clinical experience for planning and dosimetry and with the planning system, but there was no consensus on length of time needed to reach competence for the MRIgRT pathway. Physicists participants placed emphasis on the experience required to problem solve, especially for additional patient information that may affect dose constraints:
“‘What clinical impact does that change have?‘ … knowing and understanding that … that comes from guidance from your doctors and your physics … which again isn't something that comes immediately. It will come with time … going from, not making clinical decisions and then just saying, right, it's green, I'm going to go treat” (FG2)
“I'd say, multiple years of experience with treatment planning and can't be realistically handed over” (FG3)
Some participants stated that lack of resources and formal contour training affected their confidence because it was not possible to practice and gain experience.
Participants agreed practice run-throughs were essential to refine workflow for efficient treatment and allowed appreciation of potential issues and patient selection, but the critical point was to ensure familiarity with process because pressure could be intense when online:
“Make sure you're comfortable with the tools you are using and the workflow because once you're under pressure its totally exacerbated” (II6)
Participants expressed that familiarity with the software during the pre-MRIgRT stage was essential and should include on-line and off-line aspects:
“Monaco was a completely new planning system for us, a lot … was just familiarisation, as you'd have to get to grips with any new planning system” (FG4)
“If a centre has used Monaco before, then it's an instant head start”
“Having to fully commission the Monaco and fully commission the MR-linac is very challenging” (FG5)
MRIgRT training models ranged from training a core team who would cascade, to providing all aspects of training to the whole team. The use of assessments also varied. It was stressed that although training could be delivered in many forms, it was advantageous to be delivered within an MDT setting and consistency was essential. Allocating time to train was important and the value of educational, practical and simulation sessions accentuated:
‘‘I don't think we have the timeframe to be able to upscale the radiographers to a level where you need or would like them to be … maybe we don't need to be able to actually plan, but we need to have educational sessions that help us in helping make those decisions’’ (FG2)
‘‘It's two days of talks, lectures and then a day and a half of peer-to-peer … radiographers go off with the radiographers, the physicists go with the physicists, and you do specific tasks’’
‘‘We've adapted that in our training competencies … we felt that it was a really good way of getting radiographers … messing with the parameters and … and what that does to your image’’ (FG5)
Standard vendor and application training were documented by all and praised as an introduction of the basics of the system and software.
Future Practice
Radiographer-led MRIgRT emerged as future practice, with corresponding barriers and drivers all themed around training and responsibilities (Table 5). Time and access to both MRI and planning/dosimetry were identified as main issues:
“MR definitely is a gap … we don't have that insight. So that's been a steep learning curve, and … will continue” (FG2)
“We are practicing anyway behind the scenes … Again for familiarisation … It's the time isn't it, getting the contours checked and reviewed by someone who has the final say” (FG4)
Table 5.
Barriers and drivers for rad-led MRIgRT.
| Barriers | Drivers |
|---|---|
| Training opportunities difficult to arrange due to MDT availability | Radiographers could learn on-the-job and professions would always be available for support |
| Difficult to arrange consistent training | Radiographers want to take on their empowering role when the training programme is sufficient |
| Radiographers with little to no experience in planning and dosimetry and MR | Physicists envision radiographers taking on their role |
| Timescale to train radiographers is short | Professions have confidence in radiographers |
| Staffing and logistics of a radiographer-led pathway and on-call service | Radiographers will need to be able to perform the workflow as the demand is already too high on other professionals. |
| De-skilling of physicists | The chance of progression for all roles |
The need and desire for radiographers to deliver MRIgRT were the main drivers:
“If it became just two radiographers … it would be quite empowering because we would essentially be developing our roles” (FG3)
“It's just not sustainable to have the oncologist there full-time … we're very keenly aware … we need to upskill our professions” (FG2)
Discussion
This study has shown that although professional roles are comparable to conventional C-arm linacs, traditional roles are no longer fit for purpose,3 and radiographer-led MRIgRT will be vital in the future. The importance of rigorous assessment of new technology has been identified12 and to enable this, MRIgRT efficiency must be improved.13,14 Additional training and education will be required for the radiographer role to adapt to the changes in working practice. Requirements include contouring of targets and organs and risk, complex planning, dosimetry knowledge and experience, MRI applications, image recognition and registration skills, recognising individual patient requirements, and comprehensive general radiotherapy experience.
Roles and responsibilities
The online environment impacted all professionals. The unfamiliarity of physicists being ‘on-the-frontline’ and having multiple members of the MRIgRT MDT present created pressure of being watched under a time-limit despite having experience with other adaptive techniques such as on-line brachytherapy. Radiographers, in contrast, expressed role validation because of being used to working ‘on-the-frontline’.13 Pressure was focused on undertaking new roles and responsibilities, and the confidence needed to do so. When oncology nurses undertook new roles, confidence was shown to vary between individuals. It is therefore important to invest in radiographer training and experiential learning to instil appropriate confidence across therapeutic radiographers undertaking these new roles.15
The support of other professionals who have relinquished responsibility is an important aspect to consider when roles advance.16 MRIgRT creates opportunity for therapeutic radiographers to develop their roles in delivering adaptive radiotherapy, reflecting their diagnostic colleagues when reporting X-Rays.17, 18, 19 A multifaceted role is needed to ensure dynamic practice that increases care to the entire MRIgRT pathway in a shared environment rather than a direct medical replacement, as demonstrated in nursing experience of role development.20,21 There was concern regarding de-skilling of other professionals by radiographers taking on these roles, as identified in diagnostic practice.14 However, the need for radiographers to undertake this extended role was identified as a priority. There is also an opportunity for radiographers to be a source of continuity for other professionals’ training in the future as shown with advanced nursing, diagnostic radiographer practice and physician associate training.13,21 Although the role is currently limited to the MRIgRT pathway, it is important that the skills are passed to all therapeutic radiographers and not a select few.21
Being the sole profession delivering radiotherapy is common practice and returning to this from the wider MDT delivery will not be a radical change, especially knowing that confidence and validation from others is present, and key to multi-professional working.22 A radiographer-led pathway in radiology was demonstrated as an effective use of resources,14,17,23 with focus on alleviating other professionals’ time and increasing patient throughput as well as increasing job satisfaction and developing professional standing, an important factor for recruitment/retention.3,14,24
The Ionising Radiation (Medical Exposure) regulations (IRMER) must be considered in the change of traditional roles.25,26 However, although radiographer-led ART involves amendments of the target and organs at risk contours, the initial plan and prescription remain justified and authorised by the clinical oncologist (practitioner) prior to the first treatment. The radiographer is therefore an entitled operator. This process must be clearly defined under local authorisation guidelines. In addition, the planning objectives and constraints must be clearly defined to enable an operator (physicist or radiographer) to approve the plan.26 Only three clinical oncologists participated in the focus groups because of the limited number available with relevant experience, and scheduling clashes. All gave positive feedback regarding radiographer-led MRIgRT.
It must be added that although it is not viable to always have a clinician present for MRIgRT, there are times when they will be needed. A comprehensive on-call rota and close location are important factors to ensure optimum skill-mix as demonstrated in diagnostic pathways.14 The ability to be on-call but work remotely, especially for clinicians who often work away from the trust, was suggested. This could be a feature that software manufacturers explore and develop.
Communication
The need for excellent communication and good relationships within the MRIgRT MDT, and professional respect particularly supports the Health Education England Professional Framework documentation.22 The universal consensus that the MDT should develop and create all documentation relating to MRIgRT pathways (protocols, policies, guidelines) ensures all knowledge and experience is shared.27 Robust quality assurance procedures, constraints and thresholds are particularly important for ART.28
When one professional group replaces another, it is crucial that the scope-of-practice is well-defined and understood by all.22 Findings show the positive relationship between MDT members is continued in radiographer-led pathways. The environment created allows for shared learning, teaching and synergistic working, which is an asset of the MRIgRT pathway, and an important attribute for potentially difficult technology implementation.27 Apprehension and concerns will be elevated in centres that ‘stand-alone’ without support from MDT members and those with little access to diagnostic services, as their involvement is crucial for radiographers blurring established professional boundaries, and it strengthens the foundation of MRIgRT.14 Comprehension of MRI acquisition is unfamiliar to many and being able to rely on diagnostic services for support is indispensable. The introduction of a diagnostic MRI radiographer to the MRIgRT team in one centre to advise and review procedures and input vital information to training programmes and protocols for the team was seen as advantageous.13
For effective day-to-day running of MRIgRT, appropriate staffing and efficient decision-making is critical. A handover log was demonstrated as useful for radiographers in decision making, which is a requirement of advanced practice,22,23,29 and would also ensure information is appropriately shared.
Training
Training and competency are complex issues in healthcare and must be tailored as demonstrated by other professions22 in order to improve knowledge retention.30 Transition from theory to practice is recognised as challenging even in pre-registration education,31 and there was conflict between prior training and ‘on-the-job’ training. Although ‘on-the-job’ training may have disadvantages, it would allow faster progression of radiographers to deliver radiographer-led treatments and theoretical training only partially replaces clinical experience, as seen with other adaptive techniques.32
Despite a strong desire for training to be delivered as a complete package to increase confidence and allow radiographers to deliver treatment independently, there was conflict regarding timing and length. This may be due to the different training requirements for radiographers. New aspects in MRIgRT require planning experience, particularly for UK radiographers where dosimetry experience is lacking, as other professions dominate the field or require specialist radiographers.33, 34, 35, 36 Yet, in countries where radiographers have dosimetry experience, additional image recognition and contouring was required. Little documentation exists surrounding MRI education to specialist groups and post-graduation education has been suggested previously37,38 as opposed to current on-the-job learning and teaching.39 The need for standardised MRI education has been critically expressed, with focus on clinical time, so there is a minimum level of safe practice.39 To deliver the training described, multiple methods30,32,40,41 or a more blended learning approach may be needed to supplement training previously given by MDT members.41
Non routine, novel treatments and techniques risk variation in training. For example, the initial staff involved compared to subsequent staff, or MDT members expert in one tumour site with a high workload, compared to another team with few patients. This could lead to potential stress, as seen in skeletal reporting with diagnostic radiographers, so it is essential to develop a strong safety culture23 through formal, consistent assessment and audit-led training.40 One option is to introduce a high-quality accreditation programme, as used with other advanced techniques, to establish a minimum education benchmark and uniform protocol adherence.39,41 A national core curriculum has been shown to be effective.32,38 The Advanced Practice Framework in England22 also asserted the need to have a succession plan for the service and workforce, expressed as the ability to gate radiotherapy treatment using real-time imaging,42 however MRIgRT must be included and would merit a stand-alone module and/or post graduate certificate.
Even with automated planning and checking, an asset for MRIgRT because of the need to calculate and quality assure a new plan daily, clinical judgement to check for inherent errors is required, for which a radiographer with appropriate training would be best placed43 and would reduce the time span of the pathway.44 Support for cost and effectiveness will be needed and has previously been available from central European services.45
Simulations were emphasised as important and should be integral to training packages to give exclusive insight to the process. It is also an excellent tool to assess new, or changed, workflows as well as uniting a team, and virtual reality has been a successful tool in advanced radiotherapy training.40 Another consideration for training is exposure to planning software as lack of familiarity was identified as a barrier and early introduction a priority need.
There is not a clear described method for auditing aspects of the pathway for example online contouring variability and who is responsible, but the need and rationale for such is present within radiotherapy.2,46,47 Although peer mentorship was not identified, possibly because individuals had not experienced this model, it has been shown, in combination with relevant training, to increase competence.14,17,21 Peer support could also be used to increase skills amongst radiographers as with physician associates.21,32
Lack of time for training was often mentioned and has been previously identified alongside the need for MDT teaching and learning.14 High demands of current roles on MDT staff make attending and delivering training sessions difficult. Education and training of all professionals was recognised as essential to support IGRT48 and increases confidence and self-belief in radiographers.14,23 Indeed, central funding was provided to develop guidelines and support such implementation throughout the NHS and a similar approach may be required.48 The introduction of a MRIgRT national programme will need substantial resources and appropriate collaboration from national and professional bodies as well as Government and manufactures to allow streamlined and uniform implementation.49
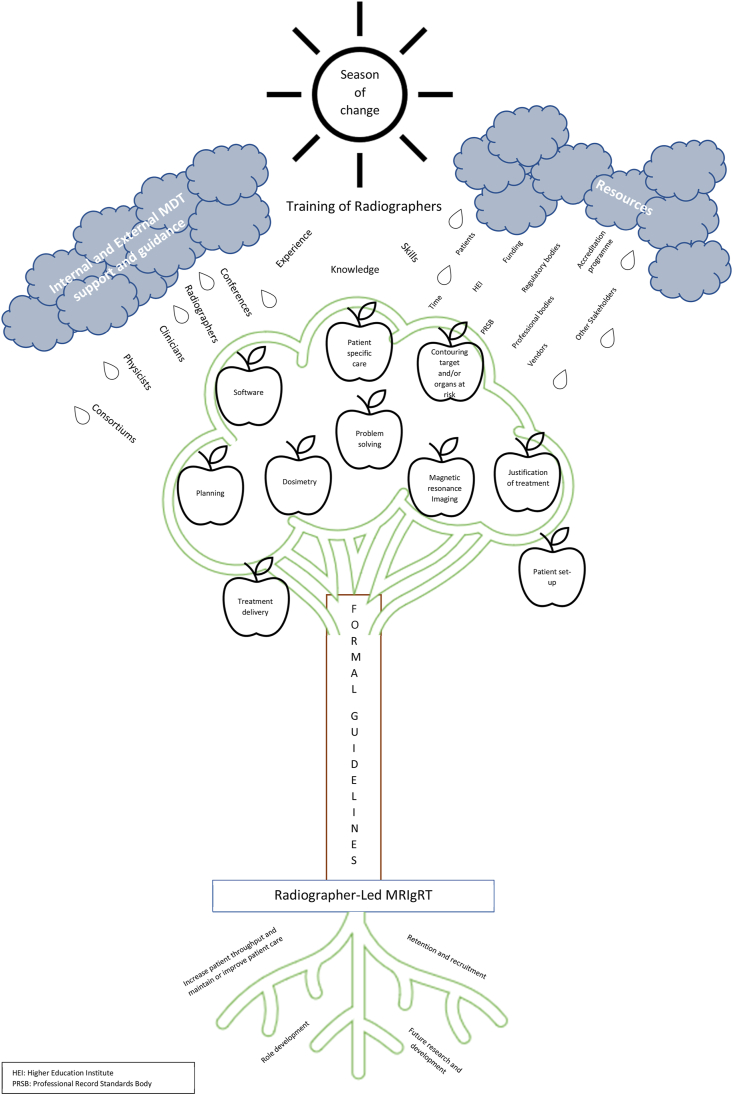
There is a clear requirement for education providers to work collaboratively with clinical partners to create learning support packages that consider the variables evident in the data collected. Such packages would need to include base line audit of current skills and confidence in delivering MRIgRT in order to accommodate sites at different stages of implementation and a mode of delivery that recognises competing priorities within an MDT e.g., a blended approach. The decision on who should engage with a learning package will be driven by context specific issues such as service delivery - including out-of-hours provision and desire for increased capacity in application of MRIgRT. The components of such an education and training framework are illustrated in Fig. 1.
Figure 1.
'Season of change' - Proposed requirements of an education and training framework for MRIgRT.
Consultation with a public patient involvement group, created for the NIHR grant (grant number in acknowledgment) demonstrated that they understood rapid advancements in technology and that the radiographer role must adapt to align with this. There was no concern expressed regarding radiographers taking on new roles and appreciation that it would allow other professionals skills to be utilised elsewhere. It was felt that radiographers currently involved in MRIgRT should be at the forefront of developing and implementing accreditation MRIgRT skills.
Conclusion
The roles for radiographers in MRIgRT are evolving in this early stage of implementation and the role validation experienced is an important factor in job satisfaction and could improve recruitment/retention. An MDT culture, with effective communication which encourages and promotes shared learning is essential for development and transfer of roles. Roles must be created with sufficient support and robust governance to enable evaluation of effectiveness, impact, ongoing sustainability and responsiveness. To prepare for the future, training and education is key, and a national framework is required to prevent variable practice. MRIgRT implementation will increase and radiographers must be prepared to be actively involved in this radiography step-change.
Conflict of interest statement
None.
Acknowledgements
This report is independent research funded by the National Institute for Health Research and Health Education England (HEE/NIHR ICA Programme Senior Clinical Lectureship, Dr Helen McNair, ICA-SCL-2018-04-ST2-002) and supported by the NIHR Biomedical Research Centre at The Royal Marsden NHS Foundation Trust and the Institute of Cancer Research, London. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health and Social Care. Research at The Institute of Cancer Research is supported by Cancer Research UK under Programme C33589/A28284. The Institute of Cancer Research is part of the Elekta MR-linac Consortium. Gratitude is expressed to all those who participated in the Focus Group Interviews and to the Public and Patient Involvement group involved with the NIHR grant.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.radi.2021.04.012.
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
References
- 1.Lamb J., Cao M., Kishan A., Agazaryan N., Thomas D.H., Shaverdian N. Online adaptive radiation therapy: implementation of a new process of care. Cureus. 2017;9(8):e1618. doi: 10.7759/cureus.1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McNair H.A., Wiseman T., Joyce E., Peet B., Huddart R.A. International survey; Current practice in On-line adaptive radiotherapy (ART) delivered using Magnetic Resonance Image (MRI) guidance. Tech Innov Patient Support Radiat Oncol. 2020;16:1–9. doi: 10.1016/j.tipsro.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Duffton A., Devlin L., Tsang Y., Mast M., Leech M., Estro R.T.T.C. Advanced practice: an ESTRO RTTC position paper. Tech Innov Patient Support Radiat Oncol. 2019;10:16–19. doi: 10.1016/j.tipsro.2019.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Suter B., Shoulders B., Maclean M., Balyckyi J. Machine verification radiographs: an opportunity for role extension? Radiography. 2000;6(4) doi: 10.1053/radi.2000.0275. 245-5. [DOI] [Google Scholar]
- 5.Hudson J., Doolan C., McDonald F., Locke I., Ahmed M., Gunapala G. Are Therapeutic Radiographers able to achieve clinically acceptable verification for stereotactic lung radiotherapy treatment (SBRT)? J Radiother Pract. 2015;14(1):10–17. doi: 10.1017/S1460396914000478. [DOI] [Google Scholar]
- 6.McNair H.A., Hafeez S., Taylor H., Lalondrelle S., McDonald F., Hansen V.N. Radiographer-led plan selection for bladder cancer radiotherapy: initiating a training programme and maintaining competency. Br J Radiol. 2015;88(1048):20140690. doi: 10.1259/bjr.20140690. [DOI] [PubMed] [Google Scholar]
- 7.Hales R.B., Rodgers J., Whiteside L., McDaid L., Berresford J., Budgell G. Therapeutic radiographers at the helm: moving towards radiographer-led MR-guided radiotherapy. J Med Imag Radiat Sci. 2020;51(3):364–372. doi: 10.1016/j.jmir.2020.05.001. [DOI] [PubMed] [Google Scholar]
- 8.McKim C. The value of mixed methods research: a mixed methods study. J Mix Methods Res. 2017;11(2):202–222. doi: 10.1177/1558689815607096. [DOI] [Google Scholar]
- 9.Lewis J., Ritchie J., Ormston R., Morrell G. In: Qualitative research practice: a guide for social science students and researchers. 2nd ed. Ritchie J., Lewis J., McNaughton Nicholls C., Ormston R., editors. SAGE; London. Thousand Oaks. New Delhi: 2014. Generalising from qualitative research; pp. p347–p366. [Google Scholar]
- 10.Barbour R., Kitzinger J. 1st ed. SAGE; London: 1999. Developing focus group research: politics, theory and practice. [Google Scholar]
- 11.Gale N., Heath G., Cameron E., Rashid S., Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:117. doi: 10.1186/1471-2288-13-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van Herk M., McWilliam A., Dubec M., Faivre-Finn C., Choudhury A. Magnetic resonance imaging-guided radiation therapy: a short strengths, weaknesses, opportunities, and threats analysis. Int J Radiat Oncol Biol Phys. 2018;101(5):1057–1060. doi: 10.1016/j.ijrobp.2017.11.009. [DOI] [PubMed] [Google Scholar]
- 13.Eccles C.L., Campbell M. Keeping up with the hybrid magnetic resonance linear accelerators: how do radiation therapists stay current in the era of hybrid technologies? J Med Imag Radiat Sci. 2019;50(2):195–198. doi: 10.1016/j.jmir.2019.04.001. [DOI] [PubMed] [Google Scholar]
- 14.Cutherbertson L.M., Robb Y.A., Blair S. The journey to advanced practice: an Interpretative Phenomenological Analysis of reaching destination and beyond for reporting radiographers in Scotland. Radiography. 2019;26(3):214–219. doi: 10.1016/j.radi.2019.11.093. [DOI] [PubMed] [Google Scholar]
- 15.Faithful S., Samuel C., Lemanska A., Warnock C., Greenfield D. Self-reported competence in long term care provision for adult cancer survivors: a cross sectional survey of nursing and allied health care professionals. Int J Nurs. 2016;53:85–94. doi: 10.1016/j.ijnurstu.2015.09.001. [DOI] [PubMed] [Google Scholar]
- 16.Edwards L.D., Till A., McKimm J. Leading the integration of physician associates into the UK health workforce. Br J Hosp Med. 2019;80(1):18–21. doi: 10.12968/hmed.2019.80.1.18. [DOI] [PubMed] [Google Scholar]
- 17.Brealey S., Scally A., Hahn S., Thomas N., Godfrey C., Coomarasamy A. Accuracy of radiographer plain radiograph reporting in clinical practice: a meta-analysis. Clin Radiol. 2005;60(2):232–241. doi: 10.1016/j.crad.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 18.Henderson I., Mathers S.A., McConnell J. Advanced and extended scope practice of diagnostic radiographers in Scotland: exploring strategic imaging service imperatives. Radiography. 2017;23(3):181–186. doi: 10.1016/j.radi.2017.02.009. [DOI] [PubMed] [Google Scholar]
- 19.Crouch R., Brown R. Advanced clinical practitioners in emergency care: past, present and future. Br J Hosp Med. 2018;79(9):511–515. doi: 10.12968/hmed.2018.79.9.511. [DOI] [PubMed] [Google Scholar]
- 20.Gray A. Advanced or advancing nursing practice: what is the future direction for nursing? Br J Nurs. 2016;25(1):8–13. doi: 10.12968/bjon.2016.25.1.8. [DOI] [PubMed] [Google Scholar]
- 21.Cahill H. Role definition: nurse practitioners or clinicians' assistants? Br J Nurs. 1996;5(22):1382–1386. doi: 10.12968/bjon.1996.5.22.1382. [DOI] [PubMed] [Google Scholar]
- 22.Health Education England . 2017. Multi-professional framework for advanced clinical practice in England. [Online]https://www.hee.nhs.uk/sites/default/files/documents/Multi-professional%20framework%20for%20advanced%20clinical%20practice%20in%20England.pdf Available at: [Google Scholar]
- 23.Cuthbertson L.M. Skeletal trauma reporting; perceptions and experiences of radiographer practitioners exposed to the reporting role. Radiography. 2020;26(1):35–41. doi: 10.1016/j.radi.2019.06.010. [DOI] [PubMed] [Google Scholar]
- 24.Probst H., Griffiths S., Adams R., Hill C. Burnout in therapy radiographers in the UK. Br J Radiol. 2012;85(1017):e760–e765. doi: 10.1259/bjr/16840236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ionising Radiation (Medical Exposure) Regulations 2017. The stationery office, London, SI 2017/1322. The ionising radiation (medical exposure) regulations 2017 (legislation.gov.UK).
- 26.Ionising Radiation (Medical Exposure) Regulations . The Royal College of Radiologists; London: 2020. implications for clinical practice in radiotherapy. Guidance form the radiotherapy board. Ionising Radiation (Medical Exposure) Regulations: Implications for clinical practice in radiotherapy Guidance from the Radiotherapy Board (rcr.ac.uk) [Google Scholar]
- 27.Edmondson A.C. Framing for learning: lessons in successful technology implementation. Calif Manag Rev. 2003;45(2):34–54. doi: 10.2307/41166164. [DOI] [Google Scholar]
- 28.Green O.L., Henke L.E., Hugo G.D. Practical clinical workflows for online and offline adaptive radiation therapy. Semin Radiat Oncol. 2019;29(3):219–227. doi: 10.1016/j.semradonc.2019.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hardy M., Snaith B. Role extension and role advancement – is there a difference? A discussion paper. Radiography. 2006;12(4):327–331. doi: 10.1016/j.radi.2005.09.004. [DOI] [Google Scholar]
- 30.Alfieri J., Portelance L., Souhami L., Steinert Y., McLeod P., Gallant F. Development and impact evaluation of an e-learning radiation oncology module. Int J Radiat Oncol Biol Phys. 2012;82(3):e573–e580. doi: 10.1016/j.ijrobp.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 31.Sá Dos Reis C., Pires Jorge J.A., York H., Flaction L., Johansen S., Mæhle S. A comparative study about motivations, expectations and future plans for professional development in four European radiography programs. Radiography. 2018;24(4):e91–e97. doi: 10.1016/j.radi.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 32.Tagliaferri L., Kovács G., Aristei C., De Sanctis V., Barbera F., Morganti A.G. Current state of interventional radiotherapy (brachytherapy) education in Italy: results of the INTERACTS survey. J Contemp Brachytherapy. 2019;11(1):48–53. doi: 10.5114/jcb.2019.83137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Couto J.G., McFadden S., McClure P., Bezzina P., Hughes C. Competencies of therapeutic radiographers working in the linear accelerator across Europe: a systematic search of the literature and thematic analysis. Radiography. 2020;26(1):82–91. doi: 10.1016/j.radi.2019.06.004. [DOI] [PubMed] [Google Scholar]
- 34.Cowling C. A global overview of the changing roles of radiographers. Radiography. 2008;14(1):e28–e32. doi: 10.1016/j.radi.2008.06.001. [DOI] [Google Scholar]
- 35.Eddy A. Advanced practice for therapy radiographers – a discussion paper. Radiography. 2008;14(1):24–33. doi: 10.1016/j.radi.2006.07.001. [DOI] [Google Scholar]
- 36.Williamson K., Mundy L. Graduate radiographers' expectations for role development – the potential impact of misalignment of expectation and valence on staff retention and service provision. Radiography. 2010;16(1):40–47. doi: 10.1016/j.radi.2009.05.001. [DOI] [Google Scholar]
- 37.Westbrook C. Opening the debate on MRI practitioner education - is there a need for change? Radiography. 2017;23(S1):S70–S74. doi: 10.1016/j.radi.2016.12.011. [DOI] [PubMed] [Google Scholar]
- 38.Eccles C.L., Webb J., Flynn A., Mcwillian A., Sanneh A., van Herk M. Piloting an educational framework for the enhanced role of RTTs in MRI-guided adaptive radiotherapy. Radiother Oncol. 2019;133(S1):S1218–S1219. doi: 10.1016/S0167-8140(19)32632-5. [DOI] [Google Scholar]
- 39.Eccles C.L., McNair H.A., Armstrong S.E.A., Helyer S.J., Scurr E.D. In response to Westbrook - opening the debate on MRI practitioner education. Radiography. 2017;23(S1):S75–S76. doi: 10.1016/j.radi.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 40.Boejen A., Vestergaard A., Hoffmann L., Ellegaard M.B. A learning programme qualifying radiation therapists to manage daily online adaptive radiotherapy. Acta Oncol. 2015;54(9):1697–1701. doi: 10.3109/0284186X.2015.1062914. [DOI] [PubMed] [Google Scholar]
- 41.Pham D., Hardcastle N., Foroudi A., Kron T., Bressel M., Hilder B. A multidisciplinary evaluation of a web-based eLearning training programme for SAFRON II (TROG 13.01): a multicentre randomised study of stereotactic radiotherapy for lung metastases. Clin Oncol. 2016;28(9):e101–e108. doi: 10.1016/j.clon.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 42.Kiser K.J., Smith B.D., Wang J., Fuller C.D. “Après mois, le déluge”: preparing for the coming data flood in the MRI-guided radiotherapy era. Front Oncol. 2019;29:258–273. doi: 10.3389/fonc.2019.00983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Moore K.L. Automated radiotherapy treatment planning. Semin Radiat Oncol. 2019;29(3):209–218. doi: 10.1016/j.semradonc.2019.02.003. [DOI] [PubMed] [Google Scholar]
- 44.Boldrini L., Cusumano D., Cellini F., Azario L., Mattiucci G.C., Valentini V. Online adaptive magnetic resonance guided radiotherapy for pancreatic cancer: state of the art, pearls and pitfalls. Radiat Oncol J. 2019;14(1):71. doi: 10.1186/s13014-019-1275-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Grau C., Defourny N., Malicki J., Dunscombe P., Borras J.M., Coffey M. Radiotherapy equipment and departments in the European countries: final results from the ESTRO-HERO survey. Radiother Oncol. 2014;112(2):155–164. doi: 10.1016/j.radonc.2014.08.029. [DOI] [PubMed] [Google Scholar]
- 46.Tsang Y., Baker A., Patel E., Miles E. A new era for clinical trial quality assurance: a credentialing programme for RTT led adaptive radiotherapy. Tech Innov Patient Support Radiat Oncol. 2018;5:1–2. doi: 10.1016/j.tipsro.2017.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Miles E., Venables K. Radiotherapy quality assurance: facilitation of radiotherapy research and implementation of technology. Clin Oncol. 2012;24(10):710–712. doi: 10.1016/j.clon.2012.06.006. [DOI] [PubMed] [Google Scholar]
- 48.The National Cancer Action Team . 2012. National radiotherapy implementation group report, image guided radiotherapy (IGRT), guidance for implementation and use.https://www.sor.org/sites/default/files/document-versions/National%20Radiotherapy%20Implementation%20Group%20Report%20IGRT%20Final.pdf [Online] Available at: [Google Scholar]
- 49.Keall P., Poulsen P., Booth J.T. See, think, and act: real-time adaptive radiotherapy. Semin Radiat Oncol. 2019;29(3):228–235. doi: 10.1016/j.semradonc.2019.02.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.