Abstract
Background/Objectives:
Electronic Health (eHealth) tools offer opportunities for people to access health information online; yet, most tools are not designed to meet the unique needs of diverse older adults, leading to health disparities. Our goal was to provide guidance for the development of eHealth tools for diverse older populations for use in geriatric care models.
Design:
Guidance for eHealth tools was compiled from user design resources and eHealth design literature. Pragmatic examples were provided from an evidenced-based eHealth tool called PREPAREforYourCare.org (PREPARE). We used quantitative feasibility data from PREPARE research studies and qualitative analysis of PREPARE focus groups, cognitive interviews, and feedback from randomized trials to further inform our recommendations.
Results:
Guidance and lessons learned include: 1) define clear objectives and a conceptual framework; 2) co-create with the target population; 3) optimize the design and layout for accessibility and ease of use, such as text at the 5th grade reading level, closed captioning, etc.; 4) use simple, standardized navigation design; 5) use actionable information to enhance behavior change, such as modeling of behaviors; 6) align accompanying written materials with the eHealth tool; and 7) create tracking mechanisms for ongoing user feedback. PREPARE is used as a case example to provide pragmatic illustrations for how the guidance may be operationalized.
Conclusion:
eHealth tools can be tailored to the unique characteristics, preferences, and needs of diverse older populations. Following the “lessons learned” may help decrease health disparities among diverse older adults and ensure eHealth tools are readily accessible and culturally appropriate.
Keywords: e-Health tools, health literacy, computer literacy, advance care planning, health disparities
INTRODUCTION
Globally, populations are aging and the burden of serious health-related suffering is increasing.1 New geriatric care models that include electronic health (eHealth) technologies are increasingly being developed to help older adults access health information and engage in disease self-management, and development of high-quality eHealth tools is one of the Healthy People 2020 objectives.2,3 During the COVID-19 pandemic, eHealth platforms have never been more salient,4 and they must be age-friendly and culturally appropriate to address health disparities.5–7
Older adults often lack computer literacy,2 despite their growing engagement with the internet.3 The prevalence of limited health literacy is also high among older adults (up to 50%), and is associated with poor access to health care and decreased use of the internet.8,9 Furthermore, older adults are at increased risk of visual and hearing deficits, which affect their access to eHealth information. Cultural background may also influence preferences for digital devices (e.g., phone or tablet), content display and layout, and eHealth platform use.10 For example, Black, Latinx, and Filipinx seniors are less likely than non-Hispanic and Chinese-Americans to own digital devices or use the internet.11
To prevent disparities, eHealth tools must be easy to understand and address the unique characteristics, preferences, and needs of diverse older adults. This is particularly important for those experiencing systemic patterns of disadvantage, such as non-English speaking older adults and those with limited health and computer literacy.3,12,13 Although some feasibility reviews have been conducted of web-based and mobile applications,14–17 and online resources are available,18–20 practical guidance for the development of eHealth tools for diverse older adults does not yet exist in the geriatrics literature. Therefore, the goal of this paper is to provide guidance for the development and refinement of eHealth tools for diverse, older populations and provide pragmatic examples from an evidenced-based eHealth tool called PREPARE for Your Care (www.PREPAREforYourCare.org).
METHODS
Developing Guidance and Lessons Learned for eHealth Tools
Guidance for developing eHealth tools and clear health communication principles were reviewed from user design textbooks,21–23 eHealth design and health literacy literature,3,24–28 and online resources.18–20,29,30 These sources include recommendations for graphical representation, organization, navigation, content utility, purpose, simplicity and readability. These published recommendations provide general guidance for eHealth tools on any topic. In addition, we use PREPARE as a successful example of these published guidelines and draw on our learnings and feasibility data from diverse English and Spanish-speaking older adults from several PREPARE studies.31–34 We also provide lessons learned about sustainability of eHealth tools from our own experience.
We chose the multi-media, interactive PREPARE eHealth tool, focused on advance care planning,35 as a case example because it was created by our co-author (RS), has undergone over a decade of development, refinement, and testing among English and Spanish-speaking communities, and has been shown in randomized trials to be effective among diverse English and Spanish-speaking older adults with limited health and computer literacy.33,34 For PREPARE, each developmental method led to a series of rigorous user testing, refinements, prototypes and versions (Figure 1). All materials have been meticulously co-created with culturally diverse communities and stakeholders, including geriatricians, and refined over many years. To provide illustrative examples, we identified content from the most recent PREPARE version and analyzed feedback from 700 randomized trial participants and additional user testing. Using content analysis, themes were independently identified by three authors (CS, JG, CF) and discrepancies were resolved by consensus.36 This work was approved by the University of California, San Francisco Institutional Review Board.
Figure 1:
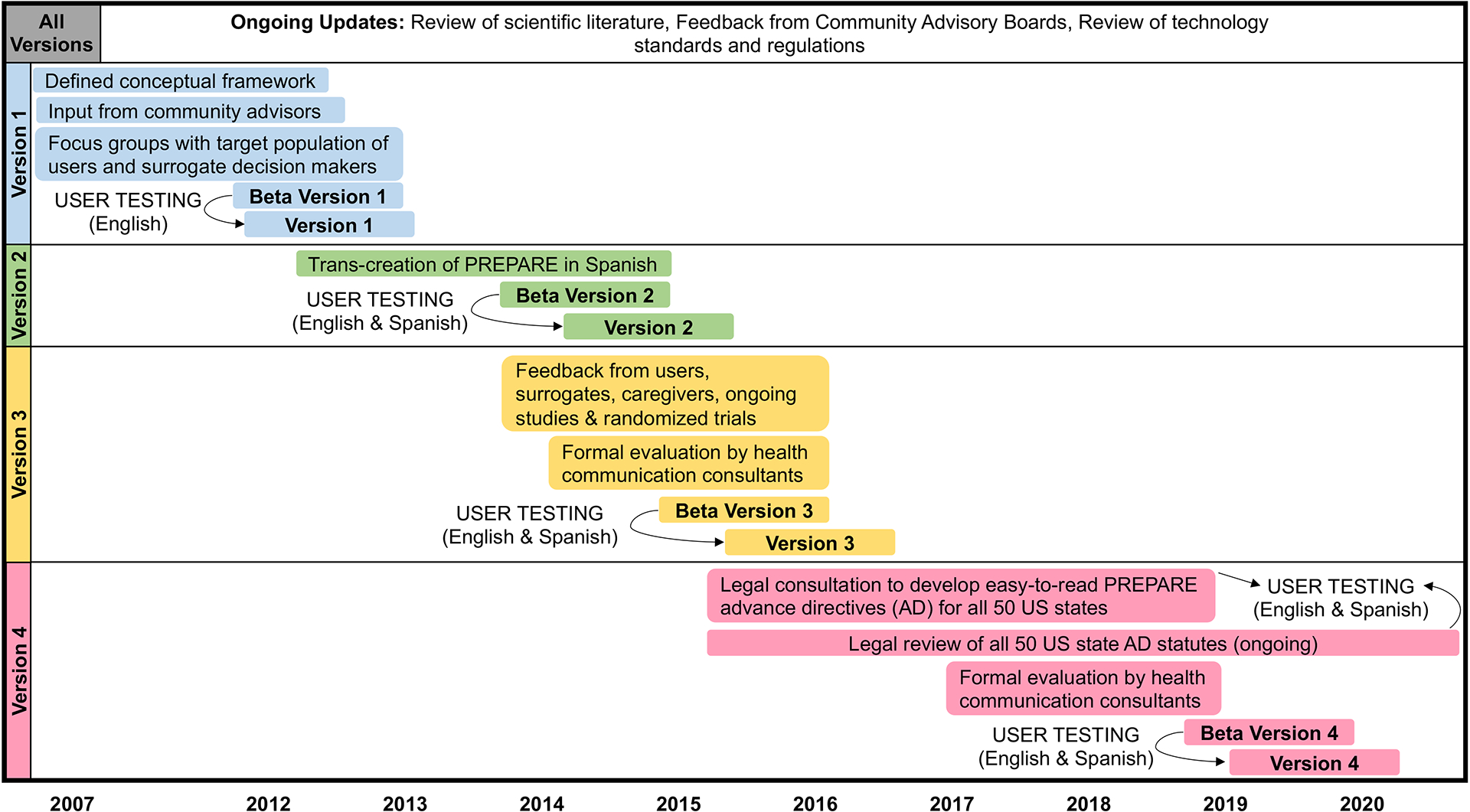
This flow chart depicts four versions and ongoing refinements of PREPARE (Y axis) since 2007 (years along the X axis). Beta versions are draft versions tested with the target population before official launch to the public (versions). User testing includes focus groups, one-on-one cognitive interviews, and direct observation.
RESULTS
We identified eight key lessons learned when developing eHealth tools for diverse, older populations (Table 1). By adhering to these lessons (Figure 2), PREPARE has been shown in randomized trials to engage over 98% of English and Spanish-speaking older adults in ACP behaviors and to be appropriately tailored to older adults’ literacy and language needs.33,34 In addition, PREPARE has had over 350,000 unique users with over 3.6 million pageviews in 115 countries.
Table 1.
Lessons Learned for eHealth Tool Development for Diverse, Older Adults
| 1. Develop clear objectives and a conceptual framework |
| a. Identify gaps in scientific literature and eHealth landscape to create an innovative solution |
| b. Identify a conceptual framework to guide the content of the eHealth tool |
| c. Conduct ongoing review of current technology standards and regulations |
| 2. Co-create with key community advisors and the target population |
| a. Identify key community advisors from the target population |
| b. Co-create all materials with the target population and key community to tailor to the end user’s unique needs, culture, and language (i.e., transcreation) |
| c. Base tech/content decisions on target population needs, not only eHealth conventions |
| d. Conduct ongoing, iterative user testing cycles with users from the target population |
| 3. Optimize design and layout for accessibility and ease of use |
| To address limited literacy, limited health literacy, and/or cognitive impairment, use clear health communication best practices: |
| a. Target text to the 5th-grade reading level and avoid jargon |
| b. Use short sentences of no more than 8–10 words in the active voice |
| c. Ensure white space for ease of review of page content |
| d. Ensure key content is listed first and is most visible on each webpage |
| e. Use non-text multimedia (e.g. pictures, videos, icons, colors) chosen by the target population that help explain the text |
| To address visual impairments (also helpful for limited health literacy and/or cognitive impairment): |
| f. Ensure text is large and readable, e.g. equivalent to 14-pt printed font or larger |
| g. Use a high contrast text color scheme, e.g. black text on white background |
| h. Offer speak aloud narration for text |
| To address hearing impairments: |
| i. Offer closed captioning for video content |
| j. Offer text scripts of video content |
| 4. To address limited computer literacy, use a simple navigation design |
| a. Ensure core navigation elements stand out, such as large intuitive buttons, with clearly labeled actions, such as “next” or “click here” |
| b. Decrease scrolling if possible |
| c. Use limited, standardized formatting and navigation labels throughout the eHealth tool |
| d. Provide a linear option through the program for passive users, such as a step-by-step navigation process |
| e. Provide a non-linear option for active users to skip to desired content (e.g., menus) |
| f. Use progress indicators, such as progress bars |
| g. To prevent users getting lost, avoid links that skip to other parts of the program |
| h. Get users to the key content with as few barriers and clicks as possible, such as not requiring users to sign in |
| 5. Use actionable information to enhance behavior change |
| a. Consider adhering to behavior change theories and techniques to engage users |
| b. Consider “how to” content and videos that model the health behavior of interest |
| c. Consider offering users the ability to create an action plan to follow up on desired behaviors |
| d. Tailor information based on users interest and personal experiences |
| 6. Provide accompanying written materials that align with the eHealth tool |
| a. Follow clear health communication principles for text/layout (see Lesson 3) |
| b. Align formatting, layout, and multimedia with the eHealth tool |
| c. Decrease access barriers to materials, such as not requiring users to sign in |
| 7. Create tracking mechanisms for ongoing input and feedback |
| 8. Consider the sustainability of the eHealth tool |
| a. Consider funding sources, ownership/copyright, and marketing. |
| b. Consider design decisions that may affect complexity and cost (e.g., providing static education versus an interactive platform, etc.). |
Figure 2:
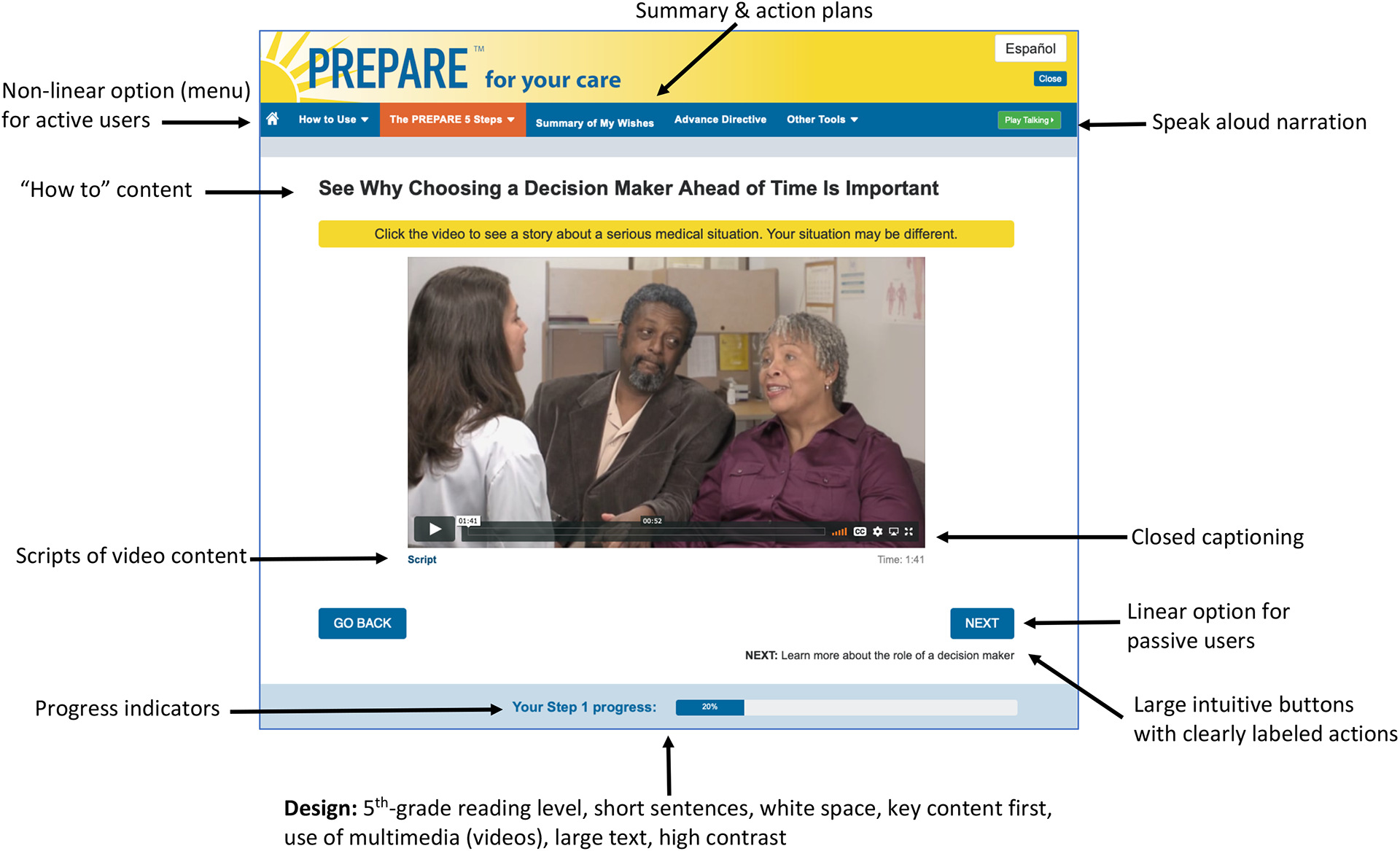
Example webpage from the PREPAREforYourCare.org eHealth tool (i.e., Step 1, Choose a Medical Decision Maker). This figure demonstrates key lessons for the development and design of eHealth tools for diverse, older populations.
Lessons Learned for eHealth Tool Development:
1. Develop clear objectives and a conceptual framework
Conduct in-depth reviews of the literature and available eHealth tools to identify how the proposed tool will be novel and best meet the needs of the target population (Lesson 1.a). For PREPARE’s initial development, we determined that easy-to-read, evidenced-based, literacy-, culturally-, and linguistically-appropriate eHealth ACP tools were needed.32
Next, identify a conceptual framework to guide the content and structure of the tool to enhance adoption (Lesson 1.b).37 For PREPARE, the conceptual framework includes behavior change constructs from Social Cognitive Theory, the Interpersonal Communication Competence Model, the Theory of Planned Behavior, and Behavior Change Theory.32 To operationalize this framework, PREPARE includes training in communication, goal-setting exercises, and videos that model ACP behaviors.
Then, after engaging with a website developer, conduct ongoing reviews of current technology standards and regulations to ensure compliance (Lesson 1.c). Decisions about which technologies to use will determine the complexity and cost of the eHealth tool. For example, because personalization has been shown to increase engagement and decrease health disparities,38 PREPARE is tailored and interactive, which is more costly than an education-only, non-tailored, non-interactive tool. In addition, to ensure user’s privacy and safety, we invest in HIPAA compliant servers and ongoing legal analysis of the advance directives.39 With technology changes, PREPARE uses a responsive web design to optimize formatting for tablets and smart phones.
2. Co-create with key community advisors and the target population
Identify key community advisors and engage them throughout the development and refinement process (Lesson 2.a).40 In addition to including experts in geriatrics, the choice of advisors will be unique for each target population. From its inception, PREPARE continues to consult key community advisors including: patients, caregivers, clinicians, community organizations (e.g., senior centers, Department on Disability and Aging), health system leaders, as well as experts in ACP, health literacy (e.g., the Institute for Healthcare Advancement, iha4health.org), geriatrics, social work, nursing, palliative care, case management, behavior change and health communication.
Additionally, co-create eHealth tools with the target population and consider using the Cultural Adaptation Process model and “transcreation” principles (i.e., the simultaneous translation and creation of linguistically and culturally adapted materials) for versions developed in new cultural contexts or languages (Lesson 2.b).41,42 It is important to learn about the needs of the target population through qualitative methods, and create draft versions of the tool (e.g., sample text, storyboards, pictures, or website outline) to obtain input during development and refinement. This can ensure that health and computer literacy principles and cultural preferences are addressed, and that each iteration continues to meet the target population’s needs. For PREPARE, we conducted 13 focus groups with diverse English and Spanish-speaking older adults and surrogate decision makers to identify the unique barriers and facilitators to ACP for diverse older adults and to identify stories that could be used for the PREPARE content.31 Transcreation of materials into other languages may involve team members with relevant cultural backgrounds. For example, the PREPARE team includes culturally diverse staff and those who speak Spanish as a first language.
It may also be necessary to base technology decisions on the target population’s needs, rather than solely on eHealth conventions (Lesson 2.c).18–21,24,25,27–29 For example, PREPARE includes instructions for how to use a computer and the PREPARE website; however, we learned that some individuals could not navigate the interactive content. Therefore, we provide a PREPARE “movie” option so users will not need to navigate the website. Consequently, the movie version is used to facilitate group medical visits.43 In addition, to help ensure users would not lose their place in PREPARE, we use non-conventional “pop up” videos when more than one video can be played on a webpage, rather than navigating users away from that webpage (also see Lesson 4.g).
Furthermore, conduct ongoing, iterative user testing and feedback cycles with the target population (Lesson 2.d).21,40–42 For PREPARE, we use in-depth “think aloud” cognitive interviewing techniques and direct observation of how users interact with beta versions.20 In addition, we continue to obtain feedback from research participants and users of the public website and work with health communication experts to conduct external audits and user testing.
3. Optimize design and layout for accessibility and ease of use
Use clear health communication best practices for the design and layout to address limited health literacy and/or cognitive impairment.23,28,30 Target the text to the 5th grade reading level (the average reading level of older adults), avoid or define jargon, use short sentences with a target of no more than 8 to 10 words, use the active voice, and ensure white space around text or pictures (Lesson 3.a-c). Also, ensure key content is listed first, such as on the home page or the top of the webpage (Lesson 3.d). Consider judicial use of multi-media elements, such as pictures, videos, and icons so as not to overwhelm or distract users (Lesson 3.e). Multi-media elements are most beneficial if they are chosen by the target population and they help to explain the text. In our PREPARE trials, we learned that participants of all literacy levels, including those with high literacy, prefer easy-to-read materials.44 Using clear health communication principles in PREPARE and multi-media elements (e.g., videos and pictures chosen by the target audience) helps users with understanding (e.g., “…the language was very easy to understand” and “Pictures made the visuals good and easier to understand.”).
To address potential visual impairments for older adults and those with limited literacy, guidelines recommend using text that is large and readable (Lesson 3.f).18 For example, use a font size of 19 pixels or more (equivalent to 14-point font). Using a high contrast color scheme, such as dark text on a light background, has also been shown to be the easiest to read (Lesson 3.g). For PREPARE, we use 24-point font size for all main headings, a 20-point font for second-level headings, and 18-point font for the body text. We also use black or dark blue on a bright white background for text. We use light text on a dark background to provide contrast for the navigation buttons, as this appealed to our target audience (e.g., “Larger letters should be used, or highlighting, to differentiate the different steps more clearly”, etc.). In addition, consider offering a speak-aloud narration option for the text (Lesson 3.h). PREPARE users, particularly those with reading difficulty or visual impairment, find this to be beneficial (e.g., “The voice taking you through it was very helpful,” etc.), but it should be “optional” as it may not appeal to all users.
To address hearing impairments, use closed-captioning for video content, and consider including video transcripts for users who prefer to read the content (Lesson 3.i-j).18–21,24,25,29 PREPARE users report these options as beneficial (e.g., “The audio was good. The videos were excellent. Having multiple viewing options were outstanding” etc.) and prefer that it be optional (e.g., “I liked the idea that you could turn on and off the sound and closed captioning” etc.).
4. Use a simple navigation design to address limited computer literacy
Ensure core navigation elements stand out, such as large intuitive buttons, with clearly labeled actions, such as “click here” (Lesson 4.a).18–21,24,25,29 Make sure the most important content appears above the fold or scroll line and that scrolling is kept to a minimum (Lesson 4.b). If content must continue below the fold, guidelines recommend that the best cue to scroll is the use of paragraph text that crosses the scroll line.18,29 Use a limited number of standardized formatting and navigation labels throughout the tool (Lesson 4.c). PREPARE uses standardized navigation elements (e.g., identical title cases, navigation bars/buttons, color schemes, and formatting) and short action labels such as ‘Click Here to Start PREPARE.’
To accommodate passive users, consider providing a linear, step-by step navigation option to help users progress through the tool (Lesson 4.d). This linear approach may include a button that can take users to the next page and may include a short overview of the content users will see on the next page. In PREPARE, we use ‘Next’ and ‘Back’ buttons to good effect for passive users (e.g., “It really walks your through all of it…”etc.). We also include a short overview of what to expect on the next page such as, ‘See how to ask someone to be a decision maker’ under the ‘Next’ button.
To keep experienced users engaged, provide a non-linear option, such as the use of menus (Lesson 4.e). Progress indicators, such as progress bars or check marks, have also been shown to keep users oriented and motivated to continue (Lesson 4.f).18–21,27,29 Avoid links that skip to other parts of the program to help prevent users getting lost (Lesson 4.g). In addition to a progress bar, PREPARE includes a click-and-select menu based on user feedback (“I would have liked a bar chart on the top of the website to show how much progress I have gone through. Also, the bar can say encouraging statements like you are almost done or you are halfway done”, etc.).
Help users get to the key content with as few barriers and “clicks” as possible, such as not requiring a sign in to get into the eHealth tool (Lesson 4.h).18–21,24,25,29 Based on feedback, we learned that some potential users had concerns regarding internet privacy. Hence, we allow users to gain access to the most important PREPARE content as a guest, such as the steps, videos, and advance directives, without having to sign in. Based on user testing, we remind users upon leaving the website to consider creating an account or signing in if they want to save their information (e.g., “It’s helpful because I can log in back into whenever I have time to review the topics”).
5. Use actionable information to enhance behavior change
Use actionable information, such as adhering to behavior change theories and techniques to engage users (Lesson 5.a).45,46 This includes use of “how to” content, including vignettes and/or videos that show users, through modeling, how to engage in the health behavior of interest (Lesson 5.b). Based on the PREPARE conceptual framework, modeling helps to increase self-efficacy and set social norms that increase the likelihood of the desired behavior.32 Modeling of ACP behaviors in the PREPARE videos (e.g., asking someone to be a medical decision maker, etc.) has shown to help users engage in ACP communication and documentation more than an advance directive alone (e.g., “The videos are encouraging to people to start planning this process. I feel motivated to update my decision maker”).33,34,47 In addition, consider offering users the ability to create an action plan (i.e., mini contracts to complete a behavior) as they increase desired behaviors (Lesson 5.c) (e.g., “it challenged me to…develop my plan. It gave me a way to ensure my plans will get done…“).48
Furthermore, tailor information to users’ interests and personal experiences (recommendation 5.d).38 Based on key community advisor recommendations, PREPARE content is tailored based on the availability of a surrogate decision maker (in prior studies up to 15% of patients reported lacking a potential surrogate)44 and whether users prefer that other people make medical decisions for them (in prior studies up to 18% prefer others make decisions).49 PREPARE also includes a range of video stories with varying care goals (e.g., “ranging from life prolongation to comfort care,” etc.).31
6. Provide accompanying written materials that align with the eHealth tool
Diverse older adults may still prefer written information, which should continue to follow clear health communication principles (Lesson 6.a).23,28,30 To decrease confusion, align written materials with the eHealth tool in terms of formatting (e.g., color schemes), layout, and multimedia (e.g., use of the same pictures) (Lesson 6.b, Figure 3). For example, PREPARE advance directives and the website initially had different color schemes and questions which created confusion (e.g., “Where are my website answers?” and “Why does this form not look the same?”). Hence, all written materials are standardized with the eHealth tool. Attempt to also decrease barriers to obtaining written materials (Lesson 6.c). For example, PREPARE does not require users to sign in to gain access to written materials.
Figure 3.
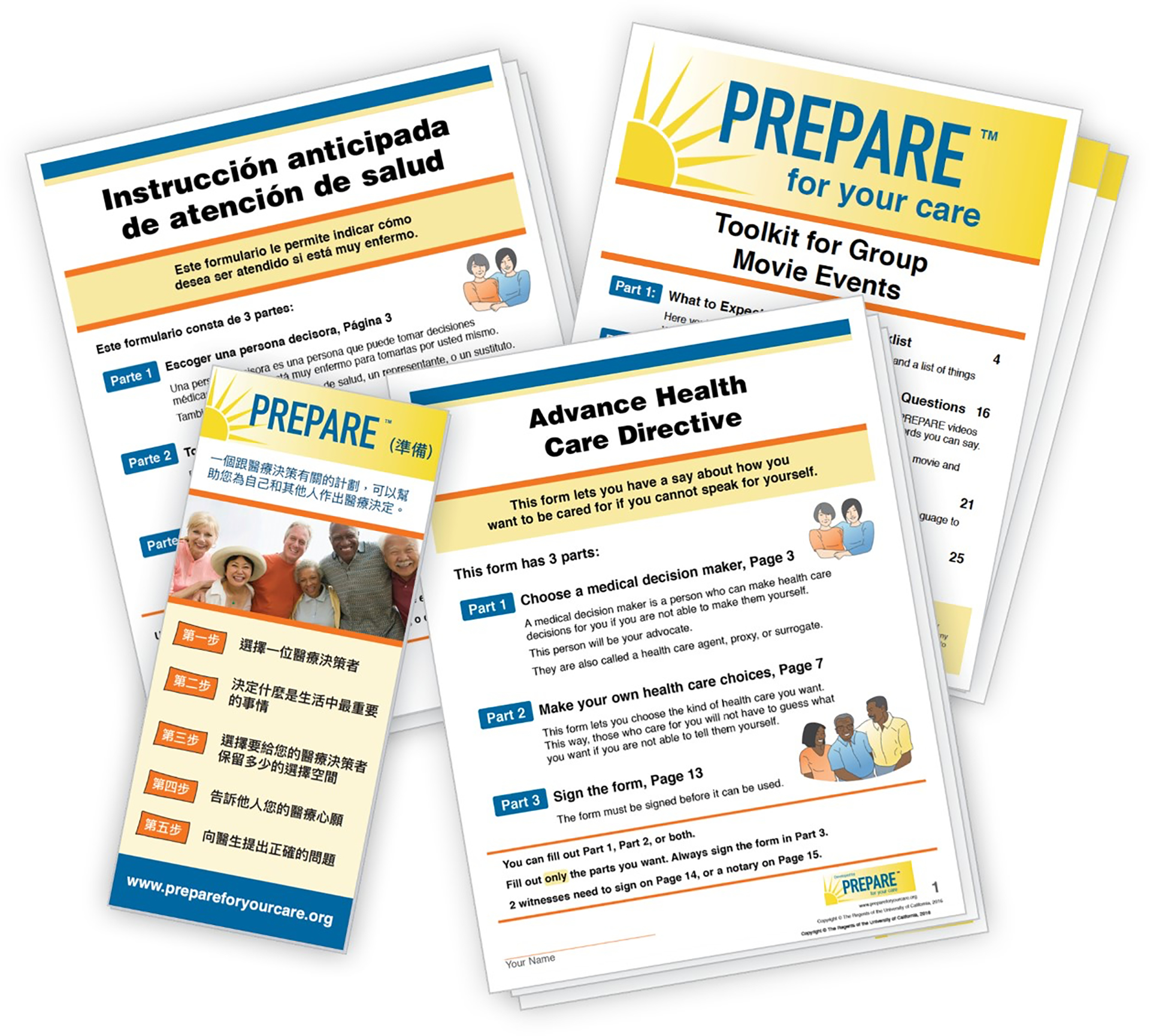
Examples of format and color scheme alignment with the PREPARE eHealth tool and accompanying written documents (e.g., the PREPARE easy-to-read advance directive in English and Spanish, the PREPARE pamphlet, and the Toolkit for PREPARE Group Movie Events). More written materials are available on the PREPARE website.
7. Create tracking mechanisms for ongoing input and feedback
End users’ needs may change due to changing social norms, changing technology, or changing clinical environments.40 For example, development and refinement of PREPARE with input from diverse stakeholders has been ongoing since 2007, and we continue to obtain feedback from research participants and users of the public website. This helps our team plan for updates when funding is available. For example, our team pivoted quickly to provide easy-to-use information about ACP and COVID-19 based on multiple stakeholder requests.50
8. Consider the sustainability of the eHealth tool
There are no published sustainability guidelines; therefore, we present observations from our experience. First, consider the source of funds to develop the tool and therefore, who may own the copyright. For example, the University of California Regents holds the copyright for PREPARE. Furthermore, while typical research funding agencies often support the testing of eHealth tools, alternative funding may be needed for development, maintenance, implementation and dissemination. When able, consider budgeting for marketing and dissemination. For example, PREPARE is sustained through a combination of foundation and philanthropic support as well as paid licenses for the use of our tools for research, quality improvement projects, and custom use within health systems. Academic developers may consider co-development with commercial support and/or consider the NIH Small Business Innovation Research grant mechanisms.
Some design decisions may also affect complexity and cost. Choose developers and contractors wisely, in terms of cost and collegiality, as they will often become long-term partners. Consider whether there is funding to adequately culturally adapt the eHealth tool into other languages. The PREPARE website is currently available in English and Spanish – the most common US languages. Although several written materials are in Chinese and other languages, we continue to seek funding to support the significant undertaking of culturally adapting the website into other languages. Finally, consider the initial and subsequent maintenance costs of design elements. For example, in collaboration with PREPARE key community advisors, we provide tailored, multi-media content (rather than static education), house the website on HIPAA-compliant servers to protect user data, and offer a free version to the public. These decisions meet our target populations’ needs and add sustainability challenges.
DISCUSSION
To our knowledge, this is the first paper to collate user centered design, cultural adaptation, transcreation, and clear health communication principles to provide practical guidance for the development of eHealth tools specifically for diverse, older adults. This guidance is particularly pertinent for individuals experiencing systemic patterns of disadvantage, such as non-English speaking older adults and those with limited health and computer literacy. The eight lessons learned include defining clear objectives and a conceptual framework; co-creating materials with key community advisors and the target population; optimizing the design for accessibility and ease of use; using simple, standardized navigation design; using actionable information to enhance behavior change; aligning accompanying written materials with the eHealth tool; creating tracking mechanisms for ongoing user feedback; and considering a sustainability model.
The lessons were collated from published eHealth, health literacy, and user design textbooks, websites, and literature.18–21,23–30,37,38 They were also informed by the co-creation of the evidenced-based PREPARE website with older, diverse adults, surrogates, and key community advisors. The use of co-creation principles has been shown to improve the acceptability and implementation of eHealth tools designed for diverse older adults.40–42 In addition, ongoing user testing with relevant stakeholders and a robust organizational structure to collect and act on ongoing feedback is important to continue to meet the target population’s needs.40
Furthermore, clear health communication principles, including addressing limited health and computer literacy as well as vision and hearing impairments, should be implemented in every aspect of the eHealth tool. Not accommodating diverse older adults’ needs may introduce digital health disparities.5–7 For example, while there has been an exponential increase in the number of eHealth tools, the quality found in usability testing has not increased at an equivalent rate.14–16 Furthermore, in a recent review of the feasibility of eleven web-based ACP eHealth tools, the authors concluded that there was insufficient evidence to recommend use by individuals with limited health or computer literacy due to poor design quality.16 In contrast, by adhering to these eHealth lessons, PREPARE has been shown to be efficacious and feasible among diverse English and Spanish-speaking older adults.33,34
Limitations
The lessons for diverse older adults are pertinent for tools designed for all ages, although lessons concerning visual, hearing, and cognitive impairment may be specific to older adults and individuals with those impairments. The PREPARE example is focused on advance care planning and was developed in San Francisco (USA), which may decrease generalizability for other types of eHealth tools in other locations. However, San Francisco is culturally diverse and PREPARE has been viewed in over 100 countries. While our feedback tracking has matured, we did not have access to feedback of earlier PREPARE versions. As we obtain funding to make updates, the PREPARE examples may change over time.
Conclusion
eHealth tools need to address diverse older adults’ unique characteristics, preferences, and needs by adhering to the aforementioned key lessons learned. This guidance may help decrease health disparities among diverse, older adults and ensure that eHealth tools are readily accessible, easy to understand, culturally appropriate, and able to meet the needs of the target population.
Key Points:
Most eHealth tools are not designed to meet the needs of diverse older adults, leading to health disparities.
Key lessons for development include using a conceptual framework; co-creating materials with communities; optimizing the design for universal accessibility; using actionable information to enhance behavior change; aligning written and eHealth materials; and tracking ongoing user feedback.
This guidance may decrease health disparities by ensuring that eHealth tools are readily accessible, easy to understand, and culturally appropriate for older adults.
Why does this Paper Matter?
Geriatric care models are increasingly using eHealth tools; yet practical guidance for eHealth tool development for diverse older adults does not yet exist. This article provides practical guidance and lessons learned for the development of eHealth tools to help decrease digital health disparities.
Acknowledgments
Conflict of Interest
The authors have no conflicts of interest to disclose. PREPAREforYourCare.org is copyrighted through the University of California (UC) Regents. PREPARE is free to the public. Licensing through the UC Regents is available for research, quality improvement, branding and data reporting purposes. However, no royalties are collected and all proceeds, by agreement with the UC Regents, is used solely to maintain the PREPARE program and keep it free for the public.
Sponsor’s Role
Sponsors had no role in the design, methods, subject recruitment, data collections, analysis and preparation of this paper.
Funding:
Dr. Sudore is funded in part by the National Institute on Aging, National Institutes of Health (K24AG054415). Dr. Scheerens is funded by the Belgian American Educational Foundation (B.A.E.F.) and Dr. Gilissen is funded by the Global Brain Health Institute (GBHI). The PREPARE program was supported by the S. D. Bechtel Jr. Foundation, the California Health Care Foundation, and the Gordon and Betty Moore Foundation. The published research of the PREPARE program referenced in this publication was supported by the National Institutes of Health (NIH) - National Institute on Aging (NIA) (R01AG045043), Patient-Centered Outcomes Research Institute, the National Palliative Care Research Center, and the US Department of Veterans Affairs. The funding sources had no role in the design or conduct of this publication.
References
- 1.Sleeman KE, de Brito M, Etkind S, et al. The escalating global burden of serious health-related suffering: projections to 2060 by world regions, age groups, and health conditions. Lancet Glob Health. 2019;7(7):e883–e892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Watkins I, Xie B. eHealth literacy interventions for older adults: a systematic review of the literature. J Med Internet Res. 2014;16(11):e225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kreps GL, Neuhauser L. New directions in eHealth communication: opportunities and challenges. Patient Educ Couns. 2010;78(3):329–336. [DOI] [PubMed] [Google Scholar]
- 4.Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020;26(5):309–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mitchell UA, Chebli PG, Ruggiero L, Muramatsu N. The Digital Divide in Health-Related Technology Use: The Significance of Race/Ethnicity. Gerontologist. 2019;59(1):6–14. [DOI] [PubMed] [Google Scholar]
- 6.Kampmeijer R, Pavlova M, Tambor M, Golinowska S, Groot W. The use of e-health and m-health tools in health promotion and primary prevention among older adults: a systematic literature review. BMC Health Serv Res. 2016;16 Suppl 5:290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van Haasteren A, Gille F, Fadda M, Vayena E. Development of the mHealth App Trustworthiness checklist. Digit Health. 2019;5:2055207619886463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chesser AK, Keene Woods N, Smothers K, Rogers N. Health Literacy and Older Adults: A Systematic Review. Gerontol Geriatr Med. 2016;2:2333721416630492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bailey SC, O’Conor R, Bojarski EA, et al. Literacy disparities in patient access and health-related use of Internet and mobile technologies. Health Expect. 2015;18(6):3079–3087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chau PYK, Cole M, Massey AP, Montoya-Weiss M, O’Keefe RM. Cultural differences in the online behavior of consumers. Commun Acm. 2002;45(10):138–143. [Google Scholar]
- 11.Gordon NP, Hornbrook MC. Differences in Access to and Preferences for Using Patient Portals and Other eHealth Technologies Based on Race, Ethnicity, and Age: A Database and Survey Study of Seniors in a Large Health Plan. J Med Internet Res. 2016;18(3):e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ware P, Bartlett SJ, Pare G, et al. Using eHealth Technologies: Interests, Preferences, and Concerns of Older Adults. Interact J Med Res. 2017;6(1):e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hall AK, Bernhardt JM, Dodd V. Older Adults’ Use of Online and Offline Sources of Health Information and Constructs of Reliance and Self-Efficacy for Medical Decision Making. Journal of health communication. 2015;20(7):751–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maramba I, Chatterjee A, Newman C. Methods of usability testing in the development of eHealth applications: A scoping review. Int J Med Inform. 2019;126:95–104. [DOI] [PubMed] [Google Scholar]
- 15.McDarby M, Llaneza D, George L, Kozlov E. Mobile Applications for Advance Care Planning: A Comprehensive Review of Features, Quality, Content, and Readability. The American journal of hospice & palliative care. 2020:1049909120959057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van der Smissen D, Overbeek A, van Dulmen S, et al. The Feasibility and Effectiveness of Web-Based Advance Care Planning Programs: Scoping Review. J Med Internet Res. 2020;22(3):e15578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim H, Xie B. Health literacy in the eHealth era: A systematic review of the literature. Patient Educ Couns. 2017;100(6):1073–1082. [DOI] [PubMed] [Google Scholar]
- 18.Health Literacy Online - A Guide for Simplifying the User Experience. (ODPHP) Office of Disease Prevention and Health Promotion (online). https://health.gov/healthliteracyonline/. Accessed November 25, 2020.
- 19.Developing Websites for Older People: How Web Content Accessibility Guidelines (WCAG) 2.0 Applies. Web Accessibility Initiative WAI (online). https://www.w3.org/WAI/older-users/developing/. Accessed November 25, 2020.
- 20.Usability.gov – Improving the User Experience: How To & Tools. Usability.gov (online). https://www.usability.gov/how-to-and-tools/index.html. Accessed November 25, 2020.
- 21.Nielsen J, Loranger H. Prioritizing Web Usability, 1st Ed. Berkeley, CA: New Riders; 2006. [Google Scholar]
- 22.Hilfiker SW, Santana S, Freedman M, Harris LM. In: Health Literacy in Clinical Practice and Public Health. Vol 269. IOS Press; 2020:324 – 331. [DOI] [PubMed] [Google Scholar]
- 23.Doak CC DL, Root JH. Teaching patients with low literacy skills. Philadelphia, PA: JB Lippincott; 1996. [Google Scholar]
- 24.Garett R, Chiu J, Zhang L, Young SD. A Literature Review: Website Design and User Engagement. Online J Commun Media Technol. 2016;6(3):1–14. [PMC free article] [PubMed] [Google Scholar]
- 25.Li H, Rau P-LP, Fujimura K, Gao Q, Wang L. Designing Effective Web Forms for Older Web Users. Educational Gerontology. 2012;38(4):271–281. [Google Scholar]
- 26.Craig Lefebvre R, Tada Y, Hilfiker SW, Baur C. The Assessment of User Engagement with eHealth Content: The eHealth Engagement Scale1. Journal of Computer-Mediated Communication. 2010;15(4):666–681. [Google Scholar]
- 27.Patsoule E, Koutsabasis P. Redesigning websites for older adults: a case study. Behaviour & Information Technology. 2013;33(6):561–573. [Google Scholar]
- 28.Sudore RL, Schillinger D. Interventions to Improve Care for Patients with Limited Health Literacy. Journal of clinical outcomes management : JCOM. 2009;16(1):20–29. [PMC free article] [PubMed] [Google Scholar]
- 29.Making Your Website Senior-Friendly. National Library of Medicine (online). https://nnlm.gov/mar/guides/making-your-website-senior-friendly. Accessed November 25, 2020.
- 30.Health Literacy Studies. Harvard T.H. Chan School of Public Health (online). Practice: Strategies and Tools Web site. https://www.hsph.harvard.edu/healthliteracy/practice-strategies-and-tools-2/. Accessed November 25, 2020.
- 31.McMahan RD, Knight SJ, Fried TR, Sudore RL. Advance care planning beyond advance directives: perspectives from patients and surrogates. J Pain Symptom Manage. 2013;46(3):355–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sudore RL, Knight SJ, McMahan RD, et al. A novel website to prepare diverse older adults for decision making and advance care planning: a pilot study. J Pain Symptom Manage. 2014;47(4):674–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sudore RL, Boscardin J, Feuz MA, McMahan RD, Katen MT, Barnes DE. Effect of the PREPARE Website vs an Easy-to-Read Advance Directive on Advance Care Planning Documentation and Engagement Among Veterans: A Randomized Clinical Trial. JAMA Intern Med. 2017;177(8):1102–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sudore RL, Schillinger D, Katen MT, et al. Engaging Diverse English- and Spanish-Speaking Older Adults in Advance Care Planning: The PREPARE Randomized Clinical Trial. JAMA Intern Med. 2018;178(12):1616–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sudore RL, Lum HD, You JJ, et al. Defining Advance Care Planning for Adults: A Consensus Definition From a Multidisciplinary Delphi Panel. J Pain Symptom Manage. 2017;53(5):821–832 e821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bernard HR. Research Methods in Anthropology: Qualitative and Quantitative Approaches. Thousand Oaks, CA: Sage Publications; 1994. [Google Scholar]
- 37.Kavandi H, Jaana M. Factors that affect health information technology adoption by seniors: A systematic review. Health Soc Care Community. 2020;28(6):1827–1842. [DOI] [PubMed] [Google Scholar]
- 38.Jerant A, Sohler N, Fiscella K, Franks B, Franks P. Tailored interactive multimedia computer programs to reduce health disparities: opportunities and challenges. Patient Educ Couns. 2011;85(2):323–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Castillo LS, Williams BA, Hooper SM, Sabatino CP, Weithorn LA, Sudore RL. Lost in translation: the unintended consequences of advance directive law on clinical care. Ann Intern Med. 2011;154(2):121–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Minkler M, Wallerstein N. Community-based participatory research for health: from process to outcomes, 2nd Ed. San Francisco, CA: Jossey-Bass; 2008. [Google Scholar]
- 41.Domenech Rodriguez MM, Baumann AA, Schwartz AL. Cultural adaptation of an evidence based intervention: from theory to practice in a Latino/a community context. Am J Community Psychol. 2011;47(1–2):170–186. [DOI] [PubMed] [Google Scholar]
- 42.Napoles AM, Stewart AL. Transcreation: an implementation science framework for community-engaged behavioral interventions to reduce health disparities. BMC Health Serv Res. 2018;18(1):710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zapata C, Lum HD, Wistar E, Horton C, Sudore RL. Feasibility of a Video-Based Advance Care Planning Website to Facilitate Group Visits among Diverse Adults from a Safety-Net Health System. J Palliat Med. 2018;21(6):853–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sudore RL, Landefeld CS, Barnes DE, et al. An advance directive redesigned to meet the literacy level of most adults: a randomized trial. Patient Educ Couns. 2007;69(1–3):165–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. [DOI] [PubMed] [Google Scholar]
- 46.Taj F, Klein MCA, van Halteren A. Digital Health Behavior Change Technology: Bibliometric and Scoping Review of Two Decades of Research. JMIR Mhealth Uhealth. 2019;7(12):e13311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Freytag J, Street RL Jr., Barnes DE, et al. Empowering Older Adults to Discuss Advance Care Planning During Clinical Visits: The PREPARE Randomized Trial. Journal of the American Geriatrics Society. 2020;68(6):1210–1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.MacGregor K, Handley M, Wong S, et al. Behavior-change action plans in primary care: a feasibility study of clinicians. Journal of the American Board of Family Medicine : JABFM. 2006;19(3):215–223. [DOI] [PubMed] [Google Scholar]
- 49.Chiu C, Feuz MA, McMahan RD, Miao Y, Sudore RL. “Doctor, Make My Decisions”: Decision Control Preferences, Advance Care Planning, and Satisfaction With Communication Among Diverse Older Adults. J Pain Symptom Manage. 2016;51(1):33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Block BL, Smith AK, Sudore RL. During COVID-19, Outpatient Advance Care Planning Is Imperative: We Need All Hands on Deck. Journal of the American Geriatrics Society. 2020;68(7):1395–1397. [DOI] [PMC free article] [PubMed] [Google Scholar]


