Abstract
Background:
In 2020, primary care practices adopted telemedicine as an alternative to in-person visits. Little is known about whether access to telemedicine was equitable, especially among older patients. Our objectives were to (1) examine older adults’ use of telemedicine versus in-person primary care visits; and (2) compare hospitalization for ambulatory care sensitive conditions (ACSCs) between the groups.
Methods:
In this retrospective cross-sectional study of 17,103 patients aged ≥65 years seen at 32 clinics in the Mid-Atlantic, primary care patients were classified into two groups – telemedicine vs. in-person – based on the first visit between March-May, 2020 and followed for 14 days. Using multivariable logistic regression, we measured the odds of being seen via telemedicine vs. in-person as a function of patient demographics, comorbidities, and week of study period. We then measured the odds of ACSC hospitalization by visit modality.
Results:
Mean age was 75.1 years (SD, 7.5), 60.6% of patients were female, 64.6% White, 28.1% Black, and 2.0% Hispanic. Overall, 60.3% of patients accessed primary care via telemedicine. Black (vs. White) patients had higher odds of using telemedicine (aOR, 1.30; 95% CI, 1.14–1.47) and Hispanic (vs. not Hispanic) patients had lower odds (aOR, 0.63; 95% CI, 0.42–0.92). Compared to the in-person group, patients in the telemedicine group had lower odds of ACSC hospitalization (aOR 0.78; 95% CI, 0.61–1.00). Among patients who used telemedicine, Black patients had 1.43 higher odds of ACSC hospitalization (95% CI, 1.02– 2.01), compared to White patients. Patients aged 85 or older seen via telemedicine had higher odds of an ACSC hospitalization (aOR 1.60; 95% CI, 1.03–2.47) compared to patients ages 65 to 74.
Conclusions:
These findings support the use of telemedicine for primary care access for older adults. However, the observed disparities highlight the need to improve care quality and equity regardless of visit modality.
Keywords: older adults, access to primary care, ambulatory care sensitive hospitalizations, telemedicine, health disparities
Introduction
The COVID-19 pandemic has disrupted traditional primary care delivery within the U.S. Prior to March 2020, the vast majority of primary care visits were performed in person. An analysis of a large commercial data base showed that despite relative growth over the past decade, the rate of telemedicine visits was low – 6.6 per 1,000 members – and less than half (39%) of those were for primary care.1 To mitigate the spread of COVID-19 and preserve capacity to address urgent health concerns, primary care practices rapidly adopted telemedicine as an alternative visit modality.2,3,4 However, little is known about the differential effects of access to in-person primary care visits on outcomes for older adults. On one hand, the risks associated with in-person visits during the pandemic may be particularly high for older patients who are at increased risk for morbidity and mortality from COVID.5 On the other hand, older adults may be particularly vulnerable to adverse consequences of reduced in-person access to clinicians.6
General consensus suggests that telemedicine is a safe alternative to in-person visits and may improve health outcomes for patients who cannot access care in-person.7 Nevertheless, prior to the pandemic, a dearth of empiric evidence supporting the use of telemedicine as an alternative to the traditional primary care visit resulted in a slow rate of adoption of telemedicine even in states with reimbursement parity rules.8 The rate of telemedicine visits for primary care sky-rocketed during the 1st wave of the pandemic.9 Italy and New York City – areas hard hit during the first half of 2020 - reported sharp decreases in the number of in-person medical visits and a corresponding rise in out-of-hospital cardiac arrests, raising concerns that lack of access to primary care was contributing to preventable deaths.10 Health systems and independent primary care practices had to urgently expand their telemedicine services and shift providers to telemedicine visits.
The limited literature evaluating telemedicine prior to the pandemic has also raised concerns that vulnerable subgroups of patients may experience adverse consequences of receiving care via telemedicine. For example, for telehealth visits to succeed, patients need access to and knowledge of how to use telemedicine platforms, which can pose a challenge to certain groups of patients, such as older adults6 and people with low incomes, who have less access to technology and the internet.11 A study of 148,000 primary care and subspecialty visits in 2020 found that patients whose preferred language was not English were 16% less likely to complete a visit via telemedicine compared to patients whose preferred language was English.11 Reduced in-person clinical support may also affect the quality of ambulatory care delivered to older adults who are more likely to have vision or hearing difficulties or cognitive impairments that make virtual visits more challenging.6,12,13 However, existing studies did not evaluate outcomes of primary care and did not focus on older adults.6, 9, 11, 14 Thus, the COVID-19 pandemic presents an opportunity to explore the effects of restrictions to in-person clinical supports on the outcomes of primary care for older adults. Furthermore, a better understanding of the role of in-person supports is urgently needed to inform health system practices and state policies related to telemedicine use. Our objectives in this study were to (1) examine older adults’ use of telemedicine versus in-person visits for primary care during the 1st wave of COVID-19 pandemic; and (2) evaluate the quality of primary care by comparing subsequent hospitalization rates between the two groups (patients seen initially via telemedicine vs. in-person visits).
Methods
Design overview
This was a retrospective cross-sectional study of patients aged 50 or older treated at 32 primary care clinics affiliated with a large health system in the Mid-Atlantic. The majority of practices were urban (56%), while the rest were suburban or exurban. Electronic medical records of patients with visits between March 1, 2020 and May 31, 2020 were collected, including demographics, diagnoses, clinic visit dates and modality (telemedicine vs. in-person), hospital admission and discharge dates, and diagnoses codes. The first primary care visit during the study period was identified for each patient. The quality of primary care patients received was assessed by measuring any hospital admissions for ambulatory care sensitive conditions (ACSCs) in the 14 days following the initial visit. Because patients with non-urgent complaints may have been triaged to telemedicine encounters but subsequently referred for in-person visits for additional evaluation, patients with telemedicine visits that were followed by an in-person visit within 14 days were classified in the telemedicine group.
Setting and participants
All patients aged 65 or older seen for a new or return visit in any primary care practice affiliated with the health system during the study period were included in the study. During the study interval, the practices implemented rapid changes to the scheduling process for primary care visits. Between March 13, 2020 and May 1, 2020, patients scheduled to be seen in person were contacted over the phone by a nurse to determine the urgency of the appointment and whether they needed to be seen in-person. Patients were preferentially triaged to telemedicine, unless they had an acute complaint requiring physical examination or expressed a strong preference for an in-person visit. Patients evaluated by telemedicine or via telephone and determined to require in-person evaluation were scheduled for a follow-up in-person visit. After May 1, 2020, patients were triaged to in-person visits “based on medical condition, risk for disease progression or sequelae, need for physical examination, and timely evaluation and management.”15 There was no difference in the proportion of visits conducted by telemedicine between the two periods (90.6% vs. 90.4%, p=0.79).
Telemedicine visits included a video option but this was not required (for example, if the patient did not have video equipment or declined to use it). Patients who requested an in-person visit or reported complaints during the telemedicine encounter that required additional evaluation were offered a follow-up visit in-person. Because this study was designed to evaluate access to primary care, we treated subsequent visits (if any) as a component of the initial visit. Thus, patients were classified in two groups – telemedicine vs. in-person – based on the first encounter during the study interval and followed for 14 days. We chose to use 14 days for follow-up for two main reasons: 1) it was sufficiently short to reasonably attribute a hospital visit to the preceding ambulatory visit, and 2) it was long enough to allow time for the patient and care team to implement the primary care clinician’s recommendations to mitigate hospitalization risk.
Key Variables
Our primary outcome of interest was the modality of initial visit to primary care during the study period. This information was obtained from the medical record, which included a visit type field. Telephone calls that were documented in the medical record but did not include an evaluation by a provider (e.g., medication refills, scheduling calls) were excluded from the analysis. Because some telephone calls could be considered telemedicine encounters, we also performed a sensitivity analysis including telephone calls in the telemedicine group. Telemedicine visits could be conducted via videoconference or by telephone alone. Our dataset did not include information about whether a telemedicine visit was conducted via video.
Our secondary outcome of interest was 14-day hospitalization following the primary care visit. We measured two secondary outcome variables – hospitalizations for ACSCs and all-cause hospitalizations. Hospitalizations for ACSCs represent a subset of all-cause hospitalizations that are thought to be avoidable with high quality primary care,16 and has been adopted to measure ACSC hospital use in prior studies.17–19 To implement this approach, we first determined whether a patient was hospitalized within 14 days of their ambulatory encounter. Then, we checked whether that hospitalization was for conditions in the list of ACSC diagnoses. Conditions relevant only to populations excluded from this analysis (e.g., “asthma in young adults”) were excluded. For patients with more than one hospitalization, the first hospitalization in the 14 days following the initial primary care visit was considered.
To measure disparities in access to care and outcomes, we examined patient race and ethnicity. Race and ethnicity were self-reported by the patient during the intake process.20 We also examined patient age (categorized as 50 to 64 years, 65 to 74 years, 75 to 84 years, and 85 years or older), gender, and comorbid conditions. The weighted Charlson Comorbidity Index (CCI) was calculated as a measure of multimorbidity.21,22
Statistical analyses
Differences in patient characteristics between telemedicine and in-person visits were compared using χ2 and Cochran-Mantel-Haenszel tests. To measure the association of sociodemographic factors with a telemedicine visit, we first estimated a multivariable logistic regression model with telemedicine visits as the dependent variable and age, sex, race, ethnicity, and the weighted Charlson Comorbidity Index as independent variables. To account for temporal trends in visits during the pandemic, the model included week of study period as an independent variable. Thus, we measured the associations between visit modality and patient characteristics within each week of the study period.
Next, to measure the association of visit modality (telemedicine vs. in-person) with hospitalizations, we estimated two multivariable logistic regression models – one with ACSC hospitalization as the dependent variable and the other with all-cause hospitalization as the dependent variable. The models included age categories, gender, race, ethnicity, and Charlson comorbidities as independent variables.
Third, we evaluated whether the relationship between visit modality and hospitalization differed by patient age, race, or ethnicity. To test this directly, we re-estimated the multivariate logistic models for hospitalization outcomes with the following interaction terms included the in the model: between the race categories and visit modality, between ethnicity and visit modality, and between the age categories and visit modality.
Additional analyses
First, we conducted sensitivity analyses including telephone calls that were not billed for as telemedicine in the telemedicine group. Second, to estimate the potential effect of unobserved hospital use on our findings, we used a separate dataset to measure the proportion of primary care patients in the clinics included in this study who were hospitalized in hospitals unaffiliated with this health system during the study interval. To do so, we used a compendium dataset of post-discharge visits implemented by 66 hospitals in the greater Philadelphia area as part of a value-based payments initiative. We found that 77.4% of all hospitalizations in our patient population occurred in affiliated facilities.
All statistical testing was 2-tailed, with p-value < 0.05 considered statistically significant. All statistical analyses were performed using SAS, version 9.4 (SAS Institute Inc).
The Institutional Review Board of the University of Pennsylvania, Philadelphia, reviewed and approved the study protocol with a waiver of informed consent.
Results
Of the 17,103 patients in our sample, 60.6% were female, 64.6% were White, 28.1% Black, 1.9% Asian, and 5.4% other race, and 2.0% were Hispanic (Table 1). Half of the patients in the sample were 65 to 74 years old (56.6%), 31.4% were 75 to 84 years old, and 12.0% were 85 years or older. Of the patients in the sample, 60.3% had their first primary care visit via telemedicine and 39.7% were seen in-person. Patients who were Black or 75 years or older represented a higher proportion of patients who accessed primary care by telemedicine (Table 1).
Table 1.
Baseline Cohort Characteristics
| Characteristic | Overall | Telemedicine | In-Person | P-value |
|---|---|---|---|---|
| n (%) | 17103 | 10311 (60.3) | 6792 (39.7) | |
| Age categories, years | 75.1±7.5 | 75.2±7.5 | 74.8±7.4 | |
| 65–74 | 9684 (56.6) | 5742 (55.7) | 3942 (58.0) | 0.01 |
| 75–84 | 5367 (31.4) | 3297 (32.0) | 2070 (30.5) | |
| ≥85 | 2052 (12.0) | 1272 (12.3) | 780 (11.5) | |
| Gender | ||||
| Female | 10372 (60.6) | 6240 (60.5) | 4132 (60.8) | 0.68 |
| Male | 6731 (39.4) | 4071 (39.5) | 2660 (39.2) | |
| Race | ||||
| White | 11043 (64.6) | 6542 (63.5) | 4501 (66.3) | <0.001 |
| Black | 4811 (28.1) | 3038 (29.5) | 1773 (26.1) | |
| Asian | 326 (1.9) | 176 (1.7) | 150 (2.2) | |
| Other | 923 (5.4) | 555 (5.4) | 368 (5.4) | |
| Ethnicity | ||||
| Not Hispanic | 16656 (97.4) | 10048 (97.5) | 6608 (97.3) | 0.14 |
| Hispanic | 337 (2.0) | 190 (1.8) | 147 (2.2) | |
| Unknown | 110 (0.6) | 73 (0.7) | 37 (0.5) | |
| Charlson Comorbidity Index | ||||
| 0 | 8,940 (52.3) | 5,303 (51.4) | 3,637 (53.6) | 0.01 |
| ≥1 and <3 | 5,492 (32.1) | 3,340 (32.4) | 2,152 (31.7) | |
| ≥3 | 2,671 (15.6) | 1,668 (16.2) | 1,003 (14.8) |
Table 2 shows the association of patient demographics and clinical conditions with the odds of accessing primary care via telemedicine vs. in-person visit. Patients who were aged 85 or older had non-significantly higher odds of having a telemedicine visit (aOR 1.18; 95% CI, 1.00–1.41; p=0.06), compared to patients who were 65 to 74 years old. Black patients had a higher odds of using telemedicine (aOR 1.30; 95% CI, 1.14–1.47; p<0.001) compared to White patients. Hispanic patients had a lower odds of using telemedicine (aOR 0.63; 95% CI, 0.42–0.92; p=0.02) compared to non-Hispanic patients (Table 2).
Table 2.
Association of Patient Characteristics and In-Person vs. Telemedicine Use
| Variable | Level | aOR of telemedicine visit (95% CI) | P-value |
|---|---|---|---|
| Week of study interval | 2.44 (2.38–2.50) | <0.001 | |
| Age (reference, 65–74 years) | 75–84 | 1.10 (0.97–1.24) | 0.13 |
| ≥85 | 1.18 (1.00–1.41) | 0.06 | |
| Hispanic (reference, Not Hispanic) | Hispanic | 0.63 (0.42–0.92) | 0.02 |
| Unknown | 1.19 (0.59–2.42) | 0.63 | |
| Race (reference, White) | Black | 1.30 (1.14–1.47) | <0.001 |
| Asian | 0.73 (0.47–1.12) | 0.15 | |
| Other | 1.25 (0.99–1.59) | 0.07 | |
| Gender (reference, Male) | Female | 1.11 (0.99–1.24) | 0.08 |
| Charlson Comorbidity Index | 1.07 (1.03–1.10) | <0.001 |
Abbreviations: aOR, adjusted odds ratio.
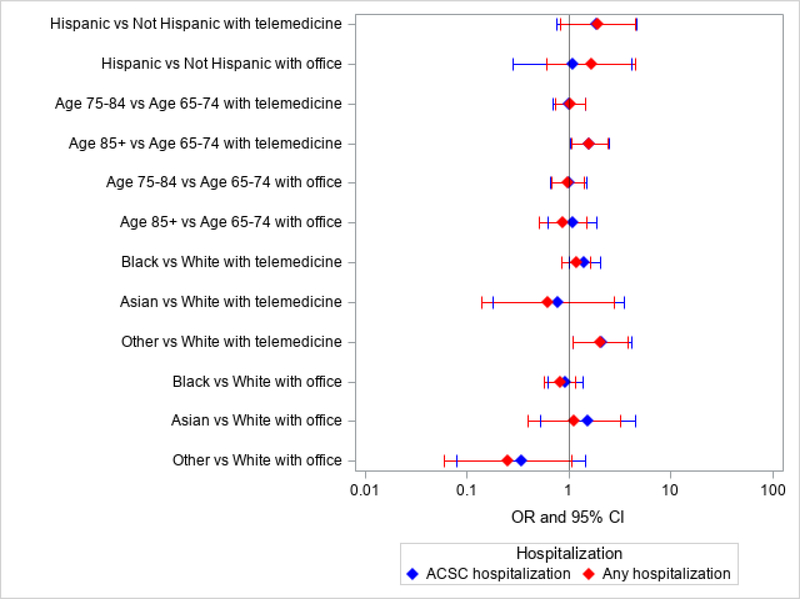
Patients who accessed primary care via telemedicine had lower odds of 14-day hospitalization compared to those with an in-person visit (ACSC hospitalization aOR 0.78; 95% CI, 0.61–1.00; p=0.049; and all-cause hospitalization aOR 0.72; 95% CI, 0.57–0.90; p=0.004) (Table 3). The figure shows the relative odds of hospitalization by visit type and race, age, and ethnicity. Patients who were aged 85 or older who were seen via telemedicine had higher odds of having an ACSC hospitalization (aOR 1.60; 95% CI, 1.03–2.47; p=0.04) or any hospitalization (aOR 1.60; 95% CI, 1.06–2.41; p=0.03), compared to patients who were 65 to 74 years old who were seen via telemedicine. Patients who were Black and used telemedicine to access primary care had 1.43 higher odds of ACSC hospitalization (95% CI: 1.02– 2.01; p=0.04) compared to White patients who used telemedicine (Figure).
Table 3.
Association of Visit Type and Hospitalization
| Variable | Level | aOR of ACSC hospitalization (95% CI) | P-value | aOR of any hospitalization (95% CI) | P-value |
|---|---|---|---|---|---|
| Telemedicine (reference, in-person visit) | 0.78 (0.61–1.00) | 0.049 | 0.72 (0.57–0.90) | 0.004 | |
| Age, years (reference, 65–74) | 75–84 | 1.01 (0.77–1.32) | 0.96 | 1.02 (0.79–1.30) | 0.90 |
| ≥85 | 1.37 (0.98–1.93) | 0.07 | 1.26 (0.91–1.73) | 0.17 | |
| Hispanic (reference, Not Hispanic) | Hispanic | 1.53 (0.73–3.21) | 0.27 | 1.79 (0.94–3.41) | 0.08 |
| Unknown | 0.48 (0.06–3.81) | 0.49 | 0.42 (0.05–3.32) | 0.41 | |
| Race (reference, White) | Black | 1.18 (0.91–1.54) | 0.21 | 1.01 (0.79–1.29) | 0.96 |
| Asian | 1.28 (0.55–2.97) | 0.57 | 0.97 (0.42–2.25) | 0.95 | |
| Other | 1.23 (0.68–2.21) | 0.50 | 1.10 (0.64–1.91) | 0.73 | |
| Gender (reference, Male) | Female | 0.88 (0.69–1.13) | 0.31 | 0.96 (0.76–1.21) | 0.73 |
| Charlson Comorbidity Index | 1.75 (1.68–1.82) | <0.001 | 1.74 (1.67–1.81) | <0.001 |
Abbreviations: aOR, adjusted odds ratio.
Figure. Differences in the Association between Telemedicine Use and Hospitalization by Ethnicity, Age, and Race.
The forest plot displays the adjusted odds of being hospitalized after being seen via telemedicine for patients stratified by race, ethnicity, and age categories. The odds for preventable hospitalizations due to ambulatory care sensitive conditions (ACSC) are displayed in blue, whereas the odds for all-cause hospitalizations are displayed in red.
Including all telephone encounters in the telemedicine group resulted in generally similar associations between patient demographics and telemedicine use, except that female patients had higher odds of telemedicine use compared to male patients (aOR 1.15; 95% CI, 1.06–1.24; p<0.001 (Supplementary Table S1). The associations between visit modality and hospitalization were not sensitive to including telephone-only visits in the telemedicine group, except that the association between telemedicine and ACSC hospitalizations was no longer statistically significant (Supplementary Table S2).
Discussion
Social distancing has become critical during the current COVID-19 pandemic, particularly for older adults who are at increased risk for morbidity and mortality from COVID-19. Telemedicine has been instrumental in enabling safe real-time access to clinical expertise. Nevertheless, restrictions to in-person clinical interactions have raised concerns about potential unintended health consequences for older patients. In particular, some have anticipated challenges in accessing care via telemedicine compared to the traditional in-person visit among older patients and racial and ethnic minorities, with potential adverse health consequences.6 In this study, we did not observe disparities negatively affecting access to primary care via telemedicine among older adults by age or racial background. In fact, Black race was associated with higher odds of telemedicine use. However, we found that Hispanic patients were less likely to access primary care by telemedicine. We further found that patients using telemedicine were less likely to be hospitalized than those who were seen in the office. This may be an effect of lower-risk patients being identified and appropriately triaged to telemedicine.
Other studies have found that during the COVID-19 pandemic, older adults (ages 55 or older compared to younger than age 55) were less likely to complete a telemedicine visit and less likely to use video during their telemedicine visits.11 In New York City, patients aged 65 or older had the lowest odds of using telehealth compared to emergency department or office visits, and Black and Hispanic patients had lower odds of using telehealth than White or Asian patients.23 A study of primary care visits in Northern California found that patients aged 65 or older were less likely to use telemedicine.24 However, that study was conducted prior to the COVID-19 pandemic, when patients did not have to consider the additional risks of infection from an in-person visit. In contrast to the study conducted in New York City, we found that Black older adults were more likely to use telemedicine. This may be due to Black patients self-triaging to higher risk due to COVID; a survey of internet-users in the U.S. found that Black respondents were most likely to report using telehealth due to the pandemic, particularly when they perceive the pandemic as a minor health threat.14 Similar to the New York City study, we found that Hispanic patients were less likely to access primary care via telemedicine. These mixed findings may stem from differences in patient populations. The older Black, Latinx, and Asian populations in New York City may differ in terms of their diversity, socio-economic status, and English language proficiency to other parts of the country. Different findings observed in studies conducted in different regions of the US highlight the need for a national prospective study to evaluate the use of telemedicine among older adults that measures these contextual factors.
Our study extends prior work by evaluating telemedicine as the first encounter, allowing for subsequent visits in-person if necessary, an approach which more closely reflects how telemedicine has been incorporated into primary care practices. Our findings suggest that racial disparities in outcomes of in-person primary care persist in telemedicine encounters. For example, we observed that Black patients who used telemedicine had higher odds of ACSC hospitalization, compared to White patients who used telemedicine. Although we controlled for clinical conditions using the Charlson comorbidity index, the diagnoses codes may not fully reflect possible differences in chronic disease status prior to COVID between Black and White patients. However, these findings highlight potential concerns regarding the use of telemedicine as a substitute for in-person primary care or a strategy to reduce racial disparities in health outcomes. Future studies evaluating the use of telemedicine to conduct lower-risk visits that do not require an in-person evaluation should incorporate this real-world approach rather than comparing telemedicine only vs. in-person only visits.
This study has clinical implications. Older adults are at particularly high risk of morbidity and mortality from COVID, and these risks are compounded among older adults who are racial or ethnic minorities.25 Our findings provide evidence in support of using telemedicine as a viable alternative to maintain access to care while reducing the risks associated with COVID for these high risk groups. However, the findings that Black patients seen via telemedicine had higher odds of hospitalization compared to White patients and that patients aged 85 years or older seen via telemedicine had higher odds of hospitalization compared to those 65 to 74 years old are concerning. Efforts to understand and address these disparities in outcomes are urgently needed.
The study has several limitations. First, the cross-sectional study design precludes inferences regarding causality. Second, we did not evaluate patient hospitalizations in facilities unaffiliated with the included hospital system. We used a relatively short follow-up period (14 days) and have no a priori reason to suspect differential use of unaffiliated hospital facilities by participants in the telemedicine vs. in-person group. Although nearly 80% of hospitalizations in our patient population occurred in affiliated facilities, the proportion of hospitalizations in non-affiliated facilities increased slightly during the study period (from 80% in March to 76% in May 2020). Some hospitalizations may have been missed in our analysis. Third, we did not have access to a primary diagnosis code for inpatient visits, so preventable hospitalizations may be overestimated. Furthermore, the pandemic may have influenced medical coding and/or decision making regarding whether to admit a patient from the emergency department or send them home. Future work should evaluate whether these findings are generalizable to time periods following the pandemic. Fourth, a smaller proportion of patients self-identified as Hispanic in this study compared to 4% of individuals over 65 reported by the US Census in 2019.26 Despite Hispanic patients being under-represented in our sample, we observed lower access to telemedicine among this subgroup of patients, similar to other studies.
In conclusion, telemedicine has played a vital role during the COVID-19 pandemic, especially for older and minority populations who are at elevated risk for morbidity and mortality. In this study, we did not find disparities in access to primary care via telemedicine among older adults by age or racial background. Similar to prior studies, Hispanic patients were less likely to access primary care via telemedicine. Overall, we found that patients using telemedicine were less likely to be hospitalized compared to those seen in the office, suggesting that telemedicine is not associated with poorer quality of care in this population. However, among patients who used telemedicine, Black patients and patients who were 85 or older had higher odds of hospitalization compared to White patients and patients aged 65 to 74 years old, highlighting the need to address disparities in primary care outcomes among these high-risk groups.
Supplementary Material
Supplementary Tables S1 and S2. These tables contain the results of sensitivity analyses conducted to test whether the findings were stable with a more liberal definition of telemedicine. In these analyses, we considered telephone calls that were not billed for as telemedicine in the telemedicine group. Supplementary Table S1 shows the association of patient characteristics and visit modality. Supplementary Table S2 shows the odds of ACSC and all-cause hospitalizations by visit modality.
Key Points.
1. Patients who were Black (vs. White) and non-Hispanic (vs. Hispanic) had higher odds of using telemedicine.
2. Patients in the telemedicine group had lower odds of potentially preventable hospitalizations compared to the in-person group.
3. Among patients who used telemedicine, Black patients had higher odds of potentially preventable hospitalizations compared to White patients and patients aged 85 or older had a higher odds of hospitalization compared to patients ages 65 to 74.
Why does this paper matter?
During the COVID-19 pandemic, primary care practices rapidly adopted telemedicine as an alternative to in-person visits. Little is known about whether access to telemedicine was equitable, especially among vulnerable populations including older adults and older racial/ethnic minorities.
Acknowledgments
Funding sources and related paper presentations: This work was supported by grant K08AG052572 from the National Institute on Aging at the National Institutes of Health (Dr. Ryskina) and by grant K76AG057016 from the National Institute on Aging at the National Institutions of Health and the American Federation for Aging Research (Dr. Brown). This study was presented as an oral abstract at the American Geriatrics Society Annual Scientific Meeting in May 2021.
Funding, presentations, and preprint disclosures: This work was supported by grant K08AG052572 from the National Institute on Aging at the National Institutes of Health (Dr. Ryskina) and by grant K76AG057016 from the National Institute on Aging at the National Institutions of Health and the American Federation for Aging Research (Dr. Brown). This study was presented as an oral abstract at the American Geriatrics Society Annual Scientific Meeting in May 2021, and as a poster at the SGIM Annual Meeting in April 2021 and at Academy Health Annual Research Meeting in June 2021. There are no other preprints of this or related manuscripts.
Sponsor’s role: The funding sources had no role in the design or conduct of the study; in the collection, analysis, or interpretation of the data; in the preparation, review, or approval of the manuscript; or in the decision to submit the manuscript for publication.
Footnotes
Conflict of interest.
References
- 1.Barnett ML, Ray KN, Souza J, Mehrotra A. Trends in telemedicine use in a large commercially insured population, 2005–2017. JAMA. November 27 2018;320(20):2147–2149. doi: 10.1001/jama.2018.12354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. June 1 2020;27(6):957–962. doi: 10.1093/jamia/ocaa067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alexander GC, Tajanlangit M, Heyward J, Mansour O, Qato DM, Stafford RS. Use and content of primary care office-based vs telemedicine care visits during the COVID-19 pandemic in the US. JAMA Netw Open. October 1 2020;3(10):e2021476. doi: 10.1001/jamanetworkopen.2020.21476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. April 30 2020;382(18):1679–1681. doi: 10.1056/NEJMp2003539 [DOI] [PubMed] [Google Scholar]
- 5.Azar KMJ, Shen Z, Romanelli RJ, et al. Disparities in outcomes among COVID-19 patients in a large health care system In California. Health Aff (Millwood). July 2020;39(7):1253–1262. doi: 10.1377/hlthaff.2020.00598 [DOI] [PubMed] [Google Scholar]
- 6.Lam K, Lu AD, Shi Y, Covinsky KE. Assessing telemedicine unreadiness among older adults in the United States during the COVID-19 pandemic. JAMA Intern Med. October 1 2020;180(10):1389–1391. doi: 10.1001/jamainternmed.2020.2671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Daniel H, Sulmasy LS, for the Public Policy Committee of the American College of Physicians. Policy recommendations to guide the use of telemedicine in primary care settings: an American College of Physicians position paper. Ann Intern Med. November 17 2015;163(10):787–9. doi: 10.7326/M15-0498 [DOI] [PubMed] [Google Scholar]
- 8.Lacktman NM, Acosta JN, Levine SJ. 50-State survey of telehealth commercial payer statutes.. Telemedicine. December 2019; Accessed on June 2, 2021 at https://www.foley.com/-/media/files/insights/health-care-law-today/19mc21486-50state-survey-of-telehealth-commercial.pdf [Google Scholar]
- 9.Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Trends in outpatient care delivery and telemedicine during the COVID-19 pandemic in the US. JAMA Intern Med. November 16 2020;doi: 10.1001/jamainternmed.2020.5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baldi E, Lombardia C, Primi R, et al. Out-of-hospital cardiac arrest incidence in the different phases of COVID-19 outbreak. Resuscitation. February 2021;159:115–116. doi: 10.1016/j.resuscitation.2020.12.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eberly LA, Kallan MJ, Julien HM, et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open. December 1 2020;3(12):e2031640. doi: 10.1001/jamanetworkopen.2020.31640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J Telemed Telecare. January 2018;24(1):4–12. doi: 10.1177/1357633X16674087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cimperman M, Brencic MM, Trkman P, Stanonik ML. Older adults’ perceptions of home telehealth services. Telemed J E Health. October 2013;19(10):786–90. doi: 10.1089/tmj.2012.0272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Campos-Castillo C, Anthony D. Racial and ethnic differences in self-reported telehealth use during the COVID-19 pandemic: a secondary analysis of a US survey of internet users from late March. J Am Med Inform Assoc. January 15 2021;28(1):119–125. doi: 10.1093/jamia/ocaa221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.University of Pennsylvania Health System. Project Resurgence: Ambulatory Practices. 2020. Internal memorandum issued to primary care practice leaders on May 1, 2020. [Google Scholar]
- 16.Agency for Healthcare Research and Quality. Quality Indicator User Guide: Prevention Quality Indicators (PQI) Composite Measures Version 2020. Published online 2020:6. Accessed on April 5, 2021 at https://www.qualityindicators.ahrq.gov/Downloads/Modules/PQI/V2020/PQI_Composite_Development.pdf
- 17.Bhattacharya R, Shen C, Sambamoorthi U. Depression and ambulatory care sensitive hospitalizations among Medicare beneficiaries with chronic physical conditions. Gen Hosp Psychiatry. 2014; 36(5): 460–465. doi: 10.1016/j.genhosppsych.2014.05.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Himelhoch S, Weller WE, Wu AW, Anderson GF, Cooper LA. Chronic medical illness, depression, and use of acute medical services among Medicare beneficiaries. Med Care. 2004; 42(6):512–521. doi: 10.1097/01.mlr.0000127998.89246.ef [DOI] [PubMed] [Google Scholar]
- 19.Ryskina KL, Konetzka RT, Werner RM. Association Between 5-Star Nursing Home Report Card Ratings and Potentially Preventable Hospitalizations. Inquiry. July 20, 2018; 55: 1–14 10.1177/0046958018787323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Amutah C, Greenidge K, Mante A, et al. Misrepresenting Race - The Role of Medical Schools in Propagating Physician Bias. N Engl J Med. March 4 2021;384(9):872–878. doi: 10.1056/NEJMms2025768 [DOI] [PubMed] [Google Scholar]
- 21.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. [DOI] [PubMed] [Google Scholar]
- 22.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. June 1992;45(6):613–9. doi: 10.1016/0895-4356(92)90133-8 [DOI] [PubMed] [Google Scholar]
- 23.Weber E, Miller SJ, Astha V, Janevic T, Benn E. Characteristics of telehealth users in NYC for COVID-related care during the coronavirus pandemic. J Am Med Inform Assoc. December 9 2020;27(12):1949–1954. doi: 10.1093/jamia/ocaa216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reed ME, Huang J, Graetz I, et al. Patient Characteristics Associated With Choosing a Telemedicine Visit vs Office Visit With the Same Primary Care Clinicians. JAMA Netw Open. June 1 2020;3(6):e205873. doi: 10.1001/jamanetworkopen.2020.5873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chatters LM, Taylor HO, Taylor RJ. Older Black Americans During COVID-19: Race and Age Double Jeopardy. Health Educ Behav. December 2020;47(6):855–860. doi: 10.1177/1090198120965513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.U.S. Census Quickfacts, Philadelphia city, Pennsylvania: (2019). Accessed on April 5, 2021 at https://www.census.gov/quickfacts/fact/table/philadelphiacitypennsylvania/PST045219 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Tables S1 and S2. These tables contain the results of sensitivity analyses conducted to test whether the findings were stable with a more liberal definition of telemedicine. In these analyses, we considered telephone calls that were not billed for as telemedicine in the telemedicine group. Supplementary Table S1 shows the association of patient characteristics and visit modality. Supplementary Table S2 shows the odds of ACSC and all-cause hospitalizations by visit modality.