Abstract
While weightbearing computed tomography (WBCT) allows 3D visualization of the distal syndesmosis, image interpretation has largely relied on 1D distance and, more recently, 2D area measurements. This study aimed to, 1)determine the sensitivity and specificity of 2D area and 3D volume WBCT measurements towards detecting subtle syndesmotic instability, 2)evaluate whether the patterns of changes in the 3D shape of the syndesmosis can be attributed to the type of ligament injury. A total of 24 patients with unilateral subtle syndesmotic instability and 24 individuals with uninjured ankles (controls) with bilateral ankle WBCT were assessed retrospectively. First, 2D areas at 0,1,3,5,10cm, and 3D volumes at 1,3,5, and 10cm above the tibial plafond were measured bilaterally. Secondly, the 3D model of the distal tibiofibular space was created based on WBCT in a subset of 8 patients out of 24 in whom the type of ligament injury was recognized via MRI. The 3D model of the injured side was superimposed on the uninjured contralateral side to visualize the pattern of changes in different planes. Volume measurement up to 5cm above the tibial plafond showed the lowest p-value (<0.001 vs. other methods), higher sensitivity (95.8%, 95%CI:87.8-100), and specificity (83.3%, 95%CI:68.4-98.2) for detection of syndesmotic instability. No specific pattern of changes in the 3D shape could be attributed to a type of ligament rupture. We suggest 3D volume measurements, best measured up to 5cm proximal to the plafond, as a promising means of diagnosing syndesmotic instability, particularly for subtle cases that are hard to detect.
Keywords: Syndesmosis, Weightbearing CT, Accuracy, Sensitivity, Specificity, Image interpretation, stress imaging
Introduction
The ankle is a mortise joint whose stability is inherently dependent on a complex series of syndesmotic ligaments that bind the fibula to the tibia, enabling them to effectively bracket the talus. These ligaments span in multiple planes because the stability they afford must constrain fibular motion through the syndesmosis and relative to the tibia in a three-dimensional (3D) manner - namely the coronal, sagittal, and rotational planes (1). In turn, untreated syndesmotic instability can precipitate irreversible morbidity, including pain, poor function, mortise incongruence, and early arthritis (1).
Various non-invasive imaging modalities have been utilized to diagnose syndesmotic instability including radiographs, ultrasound, magnetic resonance imaging (MRI), conventional computed tomography (CT), and weightbearing CT (WBCT), each with its own advantages and limitations (1-6). Radiographs are widely available but are two-dimensional (2D) and have a low sensitivity towards diagnosing syndesmotic instability unless severe. MRI has an incredibly high sensitivity to identify injury to the syndesmotic ligaments, but its unstressed nature and inability to evaluate the contralateral side as a comparison limits its utility, especially as instability becomes more subtle. WBCT has the advantage of providing a 3D view of the syndesmosis in multiple planes, incorporating weight-bearing dynamism, and affording a view of the contralateral ankle as an internal control (7).
While cross-sectional imaging affords a 3D view of the ankle, clinicians have historically interpreted CT images of the syndesmosis in a 1D manner using distal tibiofibular distance or, more recently, in a 2D manner using the distal tibiofibular area (7). However, a 3D problem is arguably better evaluated using a 3D modality. Therefore, more recent studies have explored the use of 3D evaluation of the distal tibiofibular articulation (5, 8, 9). These studies have indicated that 3D evaluation of the ankle joint and the syndesmosis can overcome the limitations of 2D assessment in terms of measuring the hindfoot angle, fibular rotation, and detecting syndesmotic instability using 3D volume estimation on WBCT. However, the specificity and sensitivity of 3D volume measurements and whether they better identify syndesmotic instability as compared to 2D measurements remains to be determined. In addition, determining specific cut-off values for both 2D and 3D measurements based on WBCT can help clinicians in the interpretation of these images. Furthermore, from an anatomic point of view, no study has evaluated whether there are specific patterns of changes in the 3D shape of distal tibiofibular space that can be attributed to the type of syndesmotic ligament rupture.
We hypothesized that the 3D volume WBCT measurement technique is superior to 1D and 2D methods for diagnosis of subtle syndesmotic instability; moreover, through 3D evaluation of the syndesmosis, there can be a specific pattern of changes in the 3D shape of the syndesmosis for each type of syndesmotic ligament injury. Hence, the aims of this study were: 1) to determine the sensitivity and specificity of WBCT towards detecting subtle syndesmotic instability when using 2D area and 3D volume measurement techniques. We also determined specific cut-off values to detect syndesmotic instability in subtle cases for each measurement technique. 2) to perform a preliminary image analysis study to determine whether there are specific patterns of changes in the 3D shape of the syndesmosis that can be attributed to the type of ligament injury.
Materials and Methods
Level of evidence: Retrospective case-control study; level 3
After obtaining institutional research board (IRB) approval (No. 2015P000464), a total of 368 bilateral ankle WBCT scans (PedCAT™; Curvebeam, Warrington, PA) were obtained at an academic medical center between 2015 and 2020 were retrospectively evaluated. Inclusion criteria in the subtle syndesmotic instability cohort consisted of, 1) age ≥18 years, 2) a surgically confirmed diagnosis of unilateral syndesmotic instability either by arthroscopic or open means, and 3) availability of a preoperative bilateral ankle WBCT scan extending at least up to 10 cm above the tibial plafond (n=24) (5, 7, 10). Subtle syndesmotic instability was described as an unstable syndesmosis that was not appreciated through radiological evaluation but was diagnosed through direct visualization via arthroscopy or intraoperatively (5, 7, 10). In these patients, although the instability was not detected in the primary radiological assessments, due to the continuation of the symptoms patients were revisited, scheduled for operative treatment, and instability was confirmed intraoperatively. Among these patients, a subgroup in whom the type of ligamentous rupture was reported by an expert radiologist based on a preoperative ankle MRI, were selected (n=8) to achieve the second aim of the study. Binary classification of the ligaments (ruptured/non-ruptured) was used in MRI assessment; a ligament was considered ruptured merely when there was a complete discontinuity of the ligamentous fibers in the image (11). The ruptured ligaments reported in MRI were also confirmed by an orthopaedic surgeon intraoperatively. The Exclusion criteria included patients younger than 18 years of age, patients with bilateral ankle injuries, syndesmotic instability accompanied by a posterior malleolar fracture, and the presence of a distal tibial fracture extending to the incisura.
The median (IQR) time between the date of injury and the date of WBCT for the entire cohort was 11 (5-15.5) weeks. As a subgroup of this cohort, patients who had also undergone an MRI were acute injuries with a median (IQR) time span of 4.5 (2.8-6) weeks between injury and WBCT and 3 (2.5-5) weeks between WBCT and MRI.
A control group of 24 patients who had undergone bilateral WBCT scans for midfoot or forefoot conditions, including Lisfranc injuries (14 patients) and forefoot conditions (10 patients), were also identified. Inclusion criteria consisted of age ≥18 years and the absence of any injuries to the ankle joint.
Sensitivity, Specificity, and Predictive Values
To perform the 2D and 3D measurements of the syndesmosis, 24 patients with unilateral subtle syndesmotic instability were compared to the control group of 24 individuals with otherwise uninjured ankles. The areas of the joint were measured at 0, 1, 3, 5, and 10 cm cross-sections proximal to the tibial plafond. The area of the syndesmosis was defined as the space between two tangential lines adjoining the anterior and posterior cortices of the tibia and the fibula as described by Hagemeijer et al. (12). The volume of the syndesmosis was measured extending from the tibial plafond to a height of 1, 3, 5, and 10 cm proximally (5). All the measurements were conducted in a single-blind manner by two research fellows (SAE and RB) who were experts in performing 2D and 3D WBCT measurements of the syndesmosis. The intraclass correlation coefficient (ICC) was used to assess the interobserver agreement (13). In this method, the ICC value between 0.81 and 1.0 is considered as a substantial agreement between the observers. ICC was calculated between the two observers for each 2D area and 3D volume measurement method.
In order to calculate the volume, the following formula was used: ; where “T” is the thickness of WBCT cross-sections (thickness = 0.3 mm), “A” is the area of the syndesmosis in each cross-section, and “n” is the number of measured WBCT cross-sections using axial views. Visage® software (Ver. 7, Visage Imaging Inc., Sandiego, CA) was used to perform 2D area and 3D volume measurements.
The difference (delta) between the area of the injured side in patients (right side in the controls) and the uninjured contralateral side (left side in the controls) and the percentage of change were calculated in each participant by using the following formulas:
Δ (Delta) Area (cm2) = Area of the injured/right joint – Area of the uninjured/left joint.
The syndesmotic WBCT volumes were measured extending from the tibial plafond to the heights of 1, 3, 5, and 10 cm proximally (5). The differences between the syndesmotic volumes of the injured side in the patients (right side in the controls) and that of the contralateral uninjured side (left side in the controls) as well as the percentage of change were calculated in each participant using the following formulas:
Δ Volume (cm3) = Volume of the injured/right joint - Volume of the uninjured/left joint.
In order to determine the cut-off values, 2D and 3D measurements were performed on the uninjured ankles (n=72). The uninjured ankles comprised the left and right ankles in the control group (n=48) and the uninjured ankles in the patients (n=24). The cut-off values for each 2D and 3D WBCT measurement were calculated using the following formula (14):
| (3) |
Subsequently, the sensitivity, specificity, negative predictive value (NPV), positive predictive value (PPV), and accuracy were determined. The cut-off value for the area at 0 cm was not determined since there are robust shape variations in the tibial plafond and syndesmotic area at 0 height which makes this level less reliable for evaluation of the instability of the syndesmosis (15). The accuracy for each measurement method was calculated according to the following formula (16): ; where TP is true positives, TN is true negatives, FN is false negatives, and FP is false positives, as compared with the relative cut-off value.
Correlation between the 3D Syndesmotic Space and the Severity of Ligamentous Injury
Eight patients with subtle syndesmotic instability in whom the type of ruptured ligament was determined using MRI, were labeled according to the torn ligaments. The syndesmotic ligaments included anterior inferior tibiofibular ligament (AITFL), posterior inferior tibiofibular ligament (PITFL), and interosseous ligament (IOL).
The pattern of changes in the shape of the distal tibiofibular space were assessed in 2D and 3D manners as follows. To perform the 2D evaluation, we first converted the 2D axial cross-sections obtained at 0, 1, 3, 5, and 10 cm above the plafond into binary gray and white images. To modify the images we used Adobe Photoshop Software (Adobe™, San Jose, CA) (Figure 1). These heights were introduced and used by previous researchers to measure the tibiofibular diastasis aiming to detect syndesmosis instability (5, 7-9). Then, the 2D images of the injured side of the patients were superimposed on the uninjured contralateral side to perform a descriptive evaluation of the alterations in the shape of the areas at different heights. Utilizing 3D Slicer software, an open-source software platform for biomedical research, 3D models of the syndesmotic space, tibia, and fibula, extending up to 10 cm proximal to the tibial plafond, were created based on the WBCT images. For the superimposition of the 3D models of the syndesmosis, we utilized Rhinoceros 3D software (Robert McNeel & Associates, Washington DC, USA). The 3D model of the injured ankle was superimposed on the uninjured contralateral side using the tibia as the reference point for matching the images. The alignment was performed manually using Standard Triangle Language (STL) file formats of the 3D model. After the tibia of one side was matched on the other side, the patterns of changes in the 3D shape of the distal tibiofibular space were observed in comparison to the uninjured contralateral side (Figure 1). We assessed the 2D and 3D alterations in the syndesmotic space in a descriptive manner in order to figure out whether a specific type of ligament rupture can bring about a specific change pattern or a specific shape that can be attributed to a specific type of ligament tear. Moreover, given the volume measurement at the level of 5 cm proximal to the platform as the most sensitive and specific method introduced in this study, we compared the measured syndesmotic volumes in this subgroup of 8 patients to assess the pattern of changes in the values regarding the volume of the syndesmosis in each type of ligament rupture.
Figure 1.
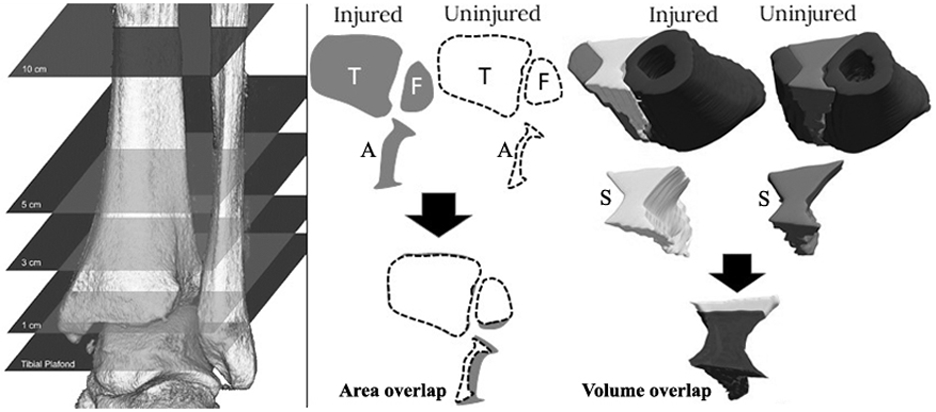
The schematic of 2D and 3D assessment of the pattern of changes in the syndesmotic space in unilateral syndesmotic instability using weightbearing CT. Using axial view, the 2D shape of the syndesmotic area (A), Tibia (T), and Fibula (F) were rendered at different levels of 0, 1, 3, 5, and 10 cm proximal to the tibial plafond. The 3D model of the distal tibiofibular space (S) was created extending up to 10 cm proximal to the plafond. The 2D and 3D models of the injured side were superimposed on the uninjured contralateral side. The patterns of changes were then described in different planes in patients with different types of ligament rupture. This preliminary study did not show any specific pattern of changes in the 2D or 3D shapes of the syndesmotic space that could be attributed to a specific type of ligament rupture.
Statistical Analysis
To determine differences in area and the volume measurements between the controls and the patients Mann-Whitney U test was utilized. To evaluate the differences in the areas and volumes measured at different levels within the 8 individuals with syndesmotic instability the one-sample t-test was used. To adjust for multiple comparisons the Holm-Bonferroni correction method was applied (17). All analyses were performed using Stata 13.0 (Stata Corp LP, College Station, TX).
Results
Predictive values of 2D and 3D Syndesmotic Measurements
The demographic data of the controls and the patients are summarized in Table 1. There was no significant difference between the two cohorts concerning age, gender, and BMI. Comparisons of the changes in the areas and the volumes measured at different levels among the patients (n=24) and the controls (n=24) are shown in Table 2. The reported ICCs in this study for 2D area WBCT measurements at different heights were 0.88 (95% CI: 0.86-0.91) at 0 cm, 0.93 (95% CI: 0.91-0.95) at 1cm, and 0.91 (95% CI: 0.88-0.92) at 3cm, 0.94 (95% CI: 0.92-0.96) at 5cm, and 0.93 (95% CI: 0.91-0.95) at 10cm from the tibial plafond. The ICCs for 3D volume measurements at 1, 3, 5, and 10 cm from the tibial plafond were 0.93 (95% CI: 0.91-0.95), 0.93 (95% CI:0.89-0.95), 0.94 (95% CI: 0.90-0.96), and 0.91 (95% CI: 0.88-0.93), respectively. The ICCs indicate substantial interobserver agreement. Volumetric measurement extending to 5 cm proximal to the tibial plafond showed the lowest p-value concerning the changes in the injured ankle versus the uninjured contralateral ankle. Measurements at this level also had a higher sensitivity (95.8%, 95%, CI: 87.8-100) and specificity (83.3%, 95%, CI: 68.4-98.2), corresponding to a cut-off value of 11.6 cm3 and 25.4% change in the volume of the syndesmotic space (Table 3). This suggests volumetric measurement up to 5 cm above the tibial plafond as the most accurate measurement for detecting subtle syndesmotic instability.
Table 1.
Demographic characteristics of individuals in the patients and the control group.
| Control group (N=24) | Patient group (N=24) | p-value | |||
|---|---|---|---|---|---|
| Gender | Female | 37.5% (n=9) | Female | 50% (n=12) | 0.38 |
| Male | 62.5% (n=15) | Male | 50% (n=12) | ||
| Age (years; mean ± SD) | 36.7±17.6 | 37.9±14.4 | 0.79 | ||
| BMI (kg/m2; mean ± SD) | 27.2±4.2 | 28.7±6.1 | 0.31 | ||
Abbreviations: BMI, body mass index; SD, standard deviation.
Table 2.
The percentage of increases in the areas and volumes of the syndesmotic joint in the control group and the patient group. The uninjured contralateral ankle (right side in the control group) was considered as the reference for normal values.
| Area increase (%) Median (IQR) |
Volume increase (%) Median (IQR) |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Height from TP |
0 cm | 1 cm | 3 cm | 5 cm | 10 cm | 1 cm | 3 cm | 5 cm | 10 cm |
| Controls (N=24) | 3.2% (1.7-4.5) | 3.3% (3.1-4.4) | 3.5% (1.3-4.8) | 2.9% (1.6-7.1) | 4.5% (3.9-5.2) | 6.2% (3.2-8.4) | 4.1% (3.7-5.0) | 5.0% (3.9-5.9) | 4.2% (3.1-6.2) |
| Patients (N=24) | 19.2% (12.4-39.32) | 24.1% (15.9-37.1) | 27.3% (16.4-39.3) | 28% (12.1-34) | 29.3% (15.2-38.9) | 31.2% (18.2-35.6) | 26.5% (16.7-38.4) | 25.4% (20-39.1) | 24.7% (22.1-32) |
| p-value | 0.004 * | 0.002 * | 0.003 * | 0.002 * | 0.003 * | 0.003 * | 0.001 * | <0.001 * | 0.004 * |
Significant p-values using Mann-Whitney U test and Holm-Bonferroni correction for multiple comparisons.
Abbreviations: TP, tibial plafond; IQR, interquartile range; %, percentage
Table 3.
Cut-off values of area and volume of the distal syndesmosis and their corresponding sensitivities and specificities for the detection of syndesmotic instability. Cut-off values are calculated based on 2D area and 3D volume measurements performed on weightbearing CT scan of 72 uninjured ankles (24 uninjured ankles in the patients and 48 in the control group).
| Measurements | Cut-off Value |
Sensitivity (%) |
95% CI | Specificity (%) |
95% CI | PPV (%) |
NPV (%) |
Accuracy (%) |
|---|---|---|---|---|---|---|---|---|
| Area at 1cm above TP | 1.4 cm2 | 70 | [38.5-81.5] | 81.6 | [76.8-92.1] | 82.6 | 69.2 | 75.1 |
| Area at 3cm above TP | 2.5 cm2 | 60 | [33.2-76.8] | 79.6 | [69.3-93.2] | 78.6 | 65.4 | 70 |
| Area at 5cm above TP | 3.2 cm2 | 62.5 | [43.1-81.9] | 80.3 | [68.4-96.2] | 78.9 | 69.9 | 72.5 |
| Area at 10cm above TP | 4.6 cm2 | 50 | [35.9-64.1] | 71 | [57.9-83.7] | 63.2 | 58.6 | 60.4 |
| Volume at 1cm above TP | 1.5 cm3 | 62.5 | [43.1-81.9] | 80 | [67.6-92.4] | 78.9 | 64 | 70.4 |
| Volume at 3cm above TP | 5.3 cm3 | 76.2 | [63.3-89.1] | 81.3 | [77.2-92.8] | 72.7 | 87.2 | 82 |
| Volume at 5cm above TP | 11.6 cm3 | 95.8 | [87.8-100] | 83.3 | [68.4-98.2] | 85.7 | 95.2 | 90 |
| Volume at 10cm above TP | 29.2 cm3 | 83.3 | [72.8-93.9] | 79.2 | [67.7-90.1] | 80 | 82.6 | 81.3 |
Abbreviations: TP, tibial plafond; PPV, positive predictive value; NPV, negative predictive value; SD, standard deviation; %, percentage; CI, confidence interval.
Correlation of the 3D Shape and the Extent of Ligamentous Injury
The subgroup of 8 patients consisted of 3 males and 5 females were labeled according to the type of torn ligaments as follows: 1- AITFL (1 patient), 2- PITFL (1 patient), 3- AITFL+PITFL (1 patient), 4-AITFL+IOL (1 patient), 5-PITFL+IOL (1 patient), 6-AITFL+PITFL+IOL (3 patients).
The mean age, height, and BMI in these 8 patients were 33.3± 11.1 years, 171.5± 9.12 cm, and 28.1±6.4 kg/m2, respectively. Based on the outcome of this preliminary study on these patients with different types of syndesmotic ligament injury, we did not find any specific alteration pattern in 2D and 3D models of the syndesmotic space which can be attributed to a specific ligamentous tear. However, we observed that in patients with IOL rupture in addition to other ligamentous injuries, the volume increased by ≥39% at 5 cm height while without IOL injury the volume increase was up to 26% (Figure 2). We adjusted the p-values using the Holm-Bonferroni correction method. The outcome of the one-sample t-test comparing the means for percentages of change in 2D areas and 3D volumes within these 8 patients showed significant differences in areas at 0 cm (18%±6.6; p=0.008), 1 cm (22.6%±11.6; p=0.005), 3 cm (25.1±13.2; p=0.006), 5 cm (31.4±15.6; p=0.003), and 10 cm (34.7±17.3; p=0.003) as well as volumes at 1 (29.6±12.3; p=0.005), 3 (32.5±16.6; p=0.004), 5 (35.3±10.9; p<0.001), and 10 cm (31.4±15.1; p<0.001) proximal to the tibial plafond.
Figure 2.
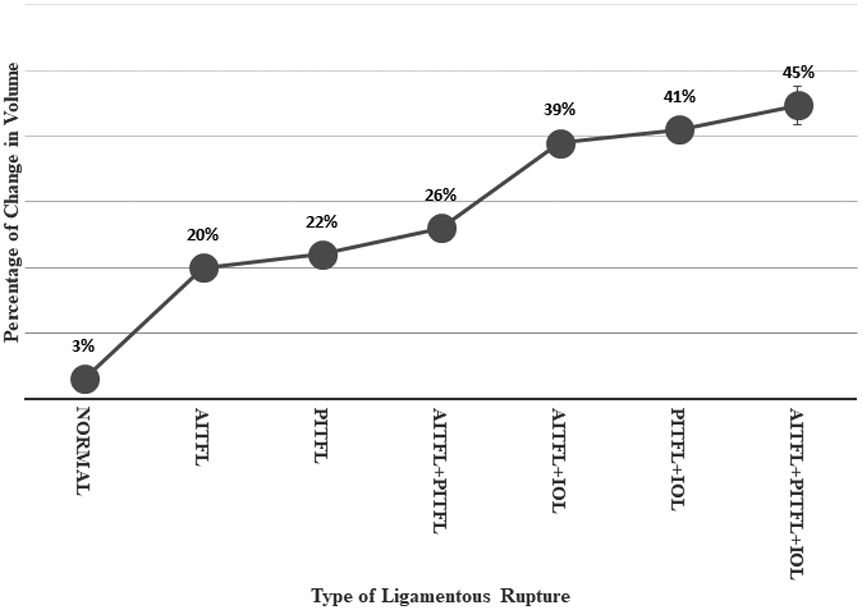
The trend of increase in the syndesmotic volume measuring up to 5 cm above the tibial plafond on weightbearing CT. The patients comprised AITFL (n=1), PITFL (n=1), AITFL+PITFL (n=1), AITFL+IOL (n=1), PITFL+IOL (n=1), AITFL+PITFL+IOL (n=3). A significant difference was seen in the values between the group of patients with interosseous ligament rupture and those with intact ligament according to the one-sample t-test (p<0.05).
Discussion
Diagnosing syndesmotic instability becomes increasingly difficult as the instability becomes more subtle. While ankle arthroscopy has historically served as the gold standard by virtue of allowing direct visualization of the distal tibiofibular articulation, its utility is limited by its invasive nature, its cost, and, notably, its inability to afford a contralateral comparison. In addition to the physical exam, imaging modalities are therefore the preferred initial means of diagnosing subtle syndesmotic instability.
As a general strategy, imaging has tried to maximize its ability to identify subtler instability by either being cross-sectional in nature, allowing a contralateral comparison, or examining the ankle in a stressed or physiologically loaded state. The advantages and disadvantages of each modality tend to flow from these three facets. Radiographs allow a contralateral comparison under physiologic load but are not cross-sectional. MRI is cross-sectional but does not afford a contralateral comparison nor examination under physiologic load. In contrast, WBCT attempts to bridge all these three imaging characteristics – it is cross-sectional, affords a contralateral comparison, and examines the distal tibiofibular articulation in weight-bearing conditions (5, 7).
As with any diagnostic test, however, the ability of one to effectively interpret the imaging modality is as critical as its inherent characteristics. Cross-sectional imaging such as WBCT of the ankle affords a 3D view of the syndesmosis. This superimposes nicely on the fact that syndesmotic instability itself is a 3D process, in which the fibula may translate in the coronal, sagittal, and rotational planes. Hitherto, however, efforts to identify instability at the tibiofibular articulation have not capitalized on this, and have largely been 1D or, more recently, 2D in nature. Linear distance measurements between the fibula and tibia at the level of the incisura (1D) are accessible to most practitioners and readily available in most viewing programs. Other studies have examined area measurements (2D) at the distal tibiofibular articulation with promising results (7, 18, 19). Krahenbuhl et al. in a cadaveric study have simulated the weight-bearing condition by applying axial load and torque on specimens with syndesmotic injuries while obtaining digital radiographs and CT scans (20). They declared that performing 2D measurements in this condition improves the diagnostic ability of both imaging modalities in syndesmotic injuries. However, given the 3D nature of syndesmotic instability, the value of spatial evaluation of the syndesmosis using volumetric measurements, particularly in subtle cases, has recently been suggested by several clinical and cadaveric studies (5, 9, 18, 19).
This study attempts to validate this new volume-based strategy in a number of ways. First, arthroscopic studies have demonstrated that injury to all three syndesmotic ligaments (AITFL, IOL, and PITFL), or partial syndesmotic injury (AITFL, IOL) with additional injury to the deltoid ligament, are required to destabilize the syndesmosis (10, 21, 22). As an anatomic correlate using MRI, increasingly severe syndesmotic injuries that incorporate a progressively higher number of syndesmotic ligaments do seem to result in incrementally higher volume measurements at the distal tibiofibular articulation on WBCT (Figure 2). When all three syndesmotic ligaments are injured, a severity repeatedly demonstrated to result in syndesmotic instability during arthroscopy, volume increases by 45% at the distal tibiofibular articulation as compared to the uninjured side.
This study highlights the non-binary nature of syndesmotic instability. While clinicians gravitate towards threshold values for a number of reasons, ranging from non-availability of a contralateral comparison to the incidental fact that arthroscopy probes tend to be manufactured in lengths of 2mm or 3mm, syndesmotic instability instead resides on a spectrum. The distinct capabilities of WBCT and 3D volume modeling to demonstrate this may predicate that, as we increasingly identify subtle asymmetries between the injured and uninjured ankles, our treatment of syndesmotic instability evolves to be less algorithmic and more tailored to an individual patient’s clinical complaints. For reasons that are yet to be explained, one patient may become more symptomatic at lower volume increases, or perhaps a volume increase from an injured PITFL (22%) may not be as critical as that from an injured AITFL (20%) because of the propensity of the fibula to externally rotate during normal motion (Figure 2). Additional studies are necessary to explore this and help us understand what drives the need for surgical stabilization.
In the present study, we also examined the patterns of alterations in the 3D spatial model and 2D shapes of the syndesmotic space as well as the pattern of changes in volume measurement at the level of 5 cm above the tibial plafond. We aimed to understand whether the type of ligamentous injury in patients with syndesmotic instability can be attributed to a specific pattern in 2D and 3D characteristics of the joint in different planes. Based on our descriptive analyses of the syndesmosis, although no specific patterns were seen concerning each type of ligament rupture both in 2D and 3D manners, the volume of the joint (measured from the plafond to 5 cm proximally) was increased by more than 20% in patients with an IOL rupture compared to those with an intact IOL. In other words, while patients with instability demonstrate a volume increase of more than 20% in the injured side compared to the uninjured contralateral ankle, those with IOL injury had more than 40% increase in the volume of the syndesmosis, highlighting the critical contribution of IOL to stabilizing the joint.
This study also attempts to validate this new technology by establishing the sensitivity, specificity, PPV, NPV, and accuracy of WBCT volume measurements as compared to area measurements – in essence, 3D versus 2D. To our knowledge, this is the first study to provide such values for WBCT in a clinical setting. Establishing this first and foremost requires one to define how to measure volumes at the distal tibiofibular articulation. Volumetric shapes were created at the distal tibiofibular interspace starting at the tibial plafond and then extending to 1, 3, 5, and 10 cm proximally (Table 2). This was based on prior studies by Bhimani et al. that prescribed volume measurements at heights of 5 cm and 10 cm (5); these volumetric values were compared to area measurements at a level of 1cm above the tibial plafond, the latter height having been described in prior studies (8, 12, 19). In the present study, we determined cut-off values for each 2D and 3D measurement method both in terms of measurement in metric scale and also as a percentage of change in the value in contrast with the uninjured contralateral ankle. The percentage of change in the value shows to what extent the value has changed (increase) compared to the contralateral ankle. Our results demonstrated a 95.8% sensitivity, 83.3% specificity, and accuracy of 90% for volume measurements when assessed to a height 5cm above the tibial plafond (Cut-off value = 11.6 cm3 or 25.4% change in the volume), superseding the values of volume measurements extending to other heights. Thus, when assessing the syndesmosis using WBCT, we would recommend a volumetric figure spanning the interspace between the distal fibula and tibia and extending from the plafond to a height of 5cm proximally as the preferred method to diagnose instability.
This study has a number of limitations. First, as the inclusion criteria for the second aim were patients with subtle syndesmotic instability confirmed surgically who had previously undergone bilateral WBCT as well as an MRI of the affected ankle, the number of patients added to this cohort was limited while there was also a wide variety of ligament injuries. Provided that larger numbers are clearly desirable in future studies, the lockstep increase of the severity of ligamentous injury on MRI with volume measurements at the distal syndesmosis on WBCT highlights the anatomic validity of this new technology. Second, while in this study we provided the cut-off values and percentage of change in the values as two methods for detecting syndesmotic instability for the clinicians, a larger cohort from different healthcare centers and measured by diverse clinicians may in the future make these values more valid and reliable. On the other hand, paying attention to normal variations and diversity among the patients in terms of race, gender, weight, height, and age, and individualize the cut-off values and thresholds based on these differences may lead to higher accuracy in the detection of subtle instabilities. To achieve this, using cluster analysis methods might be useful in the future based on a greater population. Moreover, we did not include patients with ankle fractures (i.e. Weber B ankle fractures) in this study. These patients are also prone to syndesmotic instability and the validity and reliability of 3D evaluation of the syndesmosis should also be examined in these patients as well. Lastly, the volume measurement technology used in this study is not yet readily available in image viewing programs currently utilized by the vast majority of clinicians. The incorporation of such technology into viewing programs will be critical prior to its widespread adoption.
Conclusion
In summary, 3D volume measurements using WBCT are best-measured from the tibial plafond to a level 5cm proximally, where a sensitivity of 95.8%, a specificity of 83.3%, and an accuracy of 90% are reached. This method was seen to outperform other 2D and 3D measurement techniques in the diagnosis of syndesmotic instability, particularly if the instability is subtle. The contralateral limb should be used as an internal control in unilateral injuries given the variability in joint morphology between individuals. We have introduced the percentage of change for the injured side compared to the uninjured side (i.e. 25.4% for the 3D volume measured up to 5 cm proximal to the tibial plafond); however, in the absence of the contralateral uninjured side for comparison, the cut-off values in a metric scale (i.e. 12.4 cm3 for the volume up to 5 cm proximal to the tibial plafond) can be useful to determine the instability, though the comparison between the two sides remains more accurate. Moreover, using the percentage of change helps the clinician assess the joint when the image is not calibrated to be able to use metric scales, or the measuring units differ in the image interpretation program (i.e. inch versus centimeter). Our preliminary data could not describe any specific pattern in 2D and 3D alterations of the syndesmotic space; however, we showed that IOL has a critical contribution in maintaining the stability of the syndesmosis as the volume of the joint measured at 5 cm height from the plafond increased significantly after IOL rupture. While widespread adoption of this diagnostic technology will require its incorporation into image viewing programs currently employed by most clinicians, further exploration of the features and capabilities of WBCT technology with a greater database is still of great importance and should be considered in future studies.
Clinical Significance:
The ability to compare the ankle joints bilaterally in a 3D manner under physiologic weight provided by weightbearing CT has led to a more accurate diagnostic method. Using volumetric measurement up to 5 cm above the tibial plafond showed higher sensitivity and specificity for recognizing an unstable syndesmosis, especially in subtle cases. However, our preliminary investigations showed that the pattern of 3D alterations in the distal tibiofibular joint space based on WBCT images does not indicate the type of syndesmotic ligamentous injury. Our results can also help image viewing programs to improve their measurement tools in order to facilitate 3D measurement for the syndesmosis as well as other conditions that may benefit from 3D evaluation of the clinical images.
Acknowledgments
This work was conducted with support from Harvard Catalyst, the Harvard Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health Award UL 1TR002541), and financial contributions from Harvard University and its affiliated academic healthcare centers. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University, and its affiliated academic healthcare centers, or the National Institutes of Health.
References
- 1.Van Zuuren W, Schepers T, Beumer A, Sierevelt I, van Noort A, Van Den Bekerom M. Acute syndesmotic instability in ankle fractures: a review. Foot and Ankle Surgery. 2017;23(3):135–41. [DOI] [PubMed] [Google Scholar]
- 2.Prakash AA. Syndesmotic stability: is there a radiological normal?—A systematic review. Foot and Ankle Surgery. 2018;24(3):174–84. [DOI] [PubMed] [Google Scholar]
- 3.Park YH, Yoon MA, Choi WS, Choi GW, Hong SJ, Kim HJ. The predictive value of MRI in the syndesmotic instability of ankle fracture. Skeletal Radiology. 2018;47(4):533–40. [DOI] [PubMed] [Google Scholar]
- 4.Abdelaziz M, Massri-Pugin J, Lubberts B, Vopat B, Guss D, Hosseini A, et al. Arthroscopic Characterization of Syndesmotic Instability: Exactly What Measurement Matters? Foot & Ankle Orthopaedics. 2018;3(2):2473011418S00002. [Google Scholar]
- 5.Bhimani R, Ashkani-Esfahani S, Lubberts B, Guss D, Hagemeijer NC, Waryasz G, et al. Utility of Volumetric Measurement via Weight-Bearing Computed Tomography Scan to Diagnose Syndesmotic Instability. Foot & Ankle International. 2020:1071100720917682. [DOI] [PubMed] [Google Scholar]
- 6.Mei-Dan O, Kots E, Barchilon V, Massarwe S, Nyska M, Mann G. A dynamic ultrasound examination for the diagnosis of ankle syndesmotic injury in professional athletes: a preliminary study. The American journal of sports medicine. 2009;37(5):1009–16. [DOI] [PubMed] [Google Scholar]
- 7.Hagemeijer NC, Chang SH, Abdelaziz ME, Casey JC, Waryasz GR, Guss D, et al. Range of normal and abnormal syndesmotic measurements using weightbearing CT. Foot & Ankle International. 2019;40(12):1430–7. [DOI] [PubMed] [Google Scholar]
- 8.Burssens A, Peeters J, Peiffer M, Marien R, Lenaerts T, Isg W, et al. Reliability and correlation analysis of computed methods to convert conventional 2D radiological hindfoot measurements to a 3D setting using weightbearing CT. International journal of computer assisted radiology and surgery. 2018;13(12):1999–2008. [DOI] [PubMed] [Google Scholar]
- 9.Burssens A, Vermue H, Barg A, Krähenbühl N, Victor J, Buedts K. Templating of syndesmotic ankle lesions by use of 3D analysis in weightbearing and nonweightbearing CT. Foot & Ankle International. 2018;39(12):1487–96. [DOI] [PubMed] [Google Scholar]
- 10.Lubberts B, Guss D, Vopat BG, Johnson AH, Van Dijk CN, Lee H, et al. The arthroscopic syndesmotic assessment tool can differentiate between stable and unstable ankle syndesmoses. Knee Surgery, Sports Traumatology, Arthroscopy. 2020;28(1):193–201. [DOI] [PubMed] [Google Scholar]
- 11.Clanton TO, Ho CP, Williams BT, Surowiec RK, Gatlin CC, Haytmanek CT, et al. Magnetic resonance imaging characterization of individual ankle syndesmosis structures in asymptomatic and surgically treated cohorts. Knee Surgery, Sports Traumatology, Arthroscopy. 2016;24(7):2089–102. [DOI] [PubMed] [Google Scholar]
- 12.Hagemeijer NC, Chang SH, Abdelaziz ME, Casey JC, Waryasz GR, Guss D, et al. Range of Normal and Abnormal Syndesmotic Measurements Using Weightbearing CT. Foot Ankle Int. 2019;40(12):1430–7. [DOI] [PubMed] [Google Scholar]
- 13.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychological bulletin. 1979;86(2):420. [DOI] [PubMed] [Google Scholar]
- 14.Singh G Determination of cutoff score for a diagnostic test. Internet J Lab Med. 2006;2:1–4. [Google Scholar]
- 15.Krähenbühl N, Weinberg MW, Davidson NP, Mills MK, Hintermann B, Saltzman CL, et al. Imaging in syndesmotic injury: a systematic literature review. Skeletal radiology. 2018;47(5):631–48. [DOI] [PubMed] [Google Scholar]
- 16.Baratloo A, Hosseini M, Negida A, El Ashal G. Part 1: simple definition and calculation of accuracy, sensitivity and specificity. 2015. [PMC free article] [PubMed] [Google Scholar]
- 17.Aickin M, Gensler H. Adjusting for multiple testing when reporting research results: the Bonferroni vs Holm methods. American journal of public health. 1996;86(5):726–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Malhotra K, Welck M, Cullen N, Singh D, Goldberg AJ. The effects of weight bearing on the distal tibiofibular syndesmosis: a study comparing weight bearing-CT with conventional CT. Foot and Ankle Surgery. 2019;25(4):511–6. [DOI] [PubMed] [Google Scholar]
- 19.Patel S, Malhotra K, Cullen N, Singh D, Goldberg A, Welck M. Defining reference values for the normal tibiofibular syndesmosis in adults using weight-bearing CT. The bone & joint journal. 2019;101(3):348–52. [DOI] [PubMed] [Google Scholar]
- 20.Krähenbühl N, Bailey TL, Weinberg MW, Davidson NP, Hintermann B, Presson AP, et al. Impact of torque on assessment of syndesmotic injuries using weightbearing computed tomography scans. Foot & ankle international. 2019;40(6):710–9. [DOI] [PubMed] [Google Scholar]
- 21.Massri-Pugin J, Lubberts B, Vopat BG, Guss D, Hosseini A, DiGiovanni CW. Effect of sequential sectioning of ligaments on syndesmotic instability in the coronal plane evaluated arthroscopically. Foot & Ankle International. 2017;38(12):1387–93. [DOI] [PubMed] [Google Scholar]
- 22.Massri-Pugin J, Lubberts B, Vopat BG, Wolf JC, DiGiovanni CW, Guss D. Role of the deltoid ligament in syndesmotic instability. Foot & ankle international. 2018;39(5):598–603. [DOI] [PubMed] [Google Scholar]


