Abstract
Background
Radial probe endobronchial ultrasound-guided transbronchial lung biopsy (RP-EBUS-TBLB) has improved the diagnostic yield of bronchoscopic biopsy of peripheral pulmonary lesions (PPLs). The diagnostic yield and complications of RP-EBUS-TBLB for PPLs vary depending on the technique, such as using a guide sheath (GS) or fluoroscopy. In this study, we investigated the utility of RP-EBUS-TBLB using a GS without fluoroscopy for diagnosing PPLs.
Methods
We retrospectively reviewed data from 607 patients who underwent RP-EBUS of PPLs from January 2019 to July 2020. TBLB was performed using RP-EBUS with a GS without fluoroscopy. The diagnostic yield and complications were assessed. Multivariable logistic regression analyses were used to identify factors affecting the diagnostic yields.
Results
The overall diagnostic accuracy was 76.1% (462/607). In multivariable analyses, the size of the lesion (≥20 mm; odds ratio [OR], 2.06; 95% confidence interval [CI], 1.27–3.33; p=0.003), positive bronchus sign in chest computed tomography (OR, 2.30; 95% CI, 1.40–3.78; p=0.001), a solid lesion (OR, 2.40; 95% CI, 1.31–4.41; p=0.005), and an EBUS image with the probe within the lesion (OR, 6.98; 95% CI, 4.38–11.12; p<0.001) were associated with diagnostic success. Pneumothorax occurred in 2.0% (12/607) of cases and chest tube insertion was required in 0.5% (3/607) of patients.
Conclusion
RP-EBUS-TBLB using a GS without fluoroscopy is a highly accurate diagnostic method in diagnosing PPLs that does not involve radiation exposure and has acceptable complication rates.
Keywords: Bronchoscopy, Diagnosis, Peripheral, Ultrasonography
Introduction
Bronchoscopy has evolved over the past few decades and endobronchial ultrasound (EBUS) is widely used in clinical practice. Among EBUS techniques, radial probe (RP) EBUS-guided biopsy is commonly used to diagnose peripheral pulmonary lesions (PPLs) [1].
This method offers high diagnostic yield and low complication rates for the diagnosis of PPLs. A meta-analysis that applied this method investigated 57 studies with a total of 7,872 PPLs and reported an overall weighted diagnostic yield of 70.6% (95% confidence interval [CI], 68%–73.1%). The overall complication rate was 2.8% [2]. A more recent meta-analysis updated these results and reported a pooled sensitivity of 0.72 and complication rate of 0.7%; sensitivity varied among institutions [3]. The method of RP-EBUS–guided transbronchial lung biopsy (RP-EBUS-TBLB) varies significantly among institutions regarding the use of additional guidance tools such as a guide sheath (GS) or fluoroscopy [2-4].
The GS technique provides access to target bronchial lesions for repeated sampling and protecting against bleeding from the biopsy site by wedging the GS into the target lesion [5]. The use of fluoroscopic guidance in addition to RP-EBUS can improve diagnostic yield while administering acceptable radiation doses to patients and clinicians [6-8]. However, fluoroscopy still exposes patients and practitioners to radiation, and consumes additional space, manpower, and costs (e.g., to install a shield room) [9].
Few studies have explored the efficacy and safety of RP-EBUS-TBLB using a GS without fluoroscopy for PPLs [10-13]. Hence, in this study, we evaluated the diagnostic yield and complications of RP-EBUS-TBLB in diagnosing PPLs and identified factors associated with the diagnostic yield.
Materials and Methods
1. Study design and subjects
We performed a retrospective observational study on 607 consecutive patients who underwent RP-EBUS for PPLs from January 2019 to July 2020 at Yeungnam University Hospital (a 930-bed, university-affiliated, tertiary referral hospital in Daegu, South Korea). All EBUS-visualized lesions (n=537) were biopsied via RP-EBUS-TBLB (Figure 1).
Fig. 1.
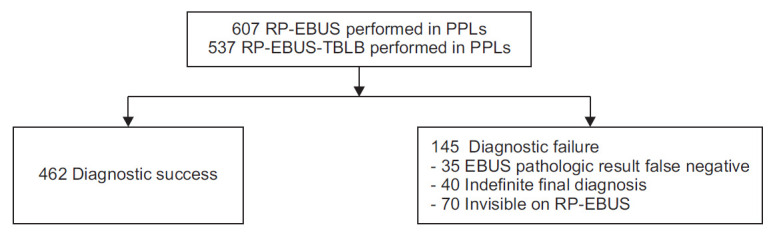
Study flowchart. PPLs: peripheral pulmonary lesions; RP-EBUS-TBLB: radial probe endobronchial ultrasound-guided transbronchial lung biopsy.
2. CT and bronchoscopy
All patients underwent thin-section chest computed tomography (CT) (0.75 mm slice thickness at intervals of 0.75 mm; SOMATOM Definition AS 64-slice CT system, Siemens Healthcare, Erlangen, Germany) less than seven days before RP-EBUS. Experienced pulmonologists reviewed the chest CT images before the procedure and planned a bronchial route to access the target lesion. The bronchus sign in CT was defined as the presence of a bronchus leading to the target lesion. The distance from the lesion to the pleura was measured as the shortest distance on an axial plane CT scan, as described previously [14].
All bronchoscopy procedures were performed by three pulmonologists, each with more than 5 years of experience in respiratory medicine. Patients were sedated with 2.5–5.0 mg of intravenous midazolam and 25–50 μg fentanyl. A 4 mm bronchoscope (BF P260F, Olympus, Tokyo, Japan) was used to reach the bronchus closest to the target lesion. Then, a RP-EBUS (UM S20–17S, Olympus) was inserted inside a GS through the bronchoscope working channel. Following the discovery of the PPL, the RP was then removed, leaving the GS in place. Then, bronchial brush and biopsy forceps were introduced into the GS and brushings and biopsy specimens were collected. When TBLB was performed at our hospital, the lesion was identified with the RP, performed gain on the first three lung tissue samples, re-inserted the RP to ensure that the GS was not re-positioned in the lesion, and then performed an extra biopsy. X-ray fluoroscopy was not used.
Figure 2 shows representative cases of RP-EBUS-TBLB with GS and without fluoroscopy in patients with suspected lung cancer.
Fig. 2.
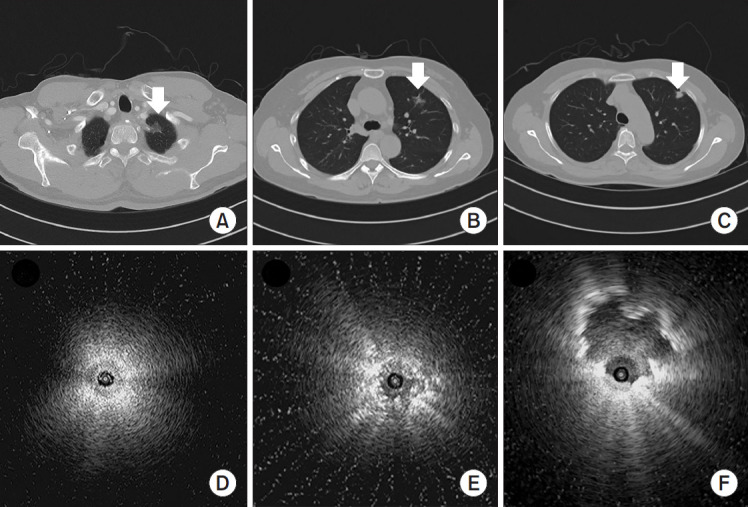
Representative cases. (A) Computed tomography (CT) scan showing a 20 mm ground glass nodule (arrow). (B) CT scan showing a 16 mm part-solid nodule (arrow). (C) CT scan showing a 15 mm speculated subpleural solid nodule (arrow). (D) Radial probe endobronchial ultrasound (RP-EBUS) shows a subtle increase in the intensity and radius of the whitish acoustic shadow, known as the blizzard sign, after which biopsy was performed and adenocarcinoma was diagnosed. (E) RP-EBUS shows diffuse heterogeneity with several hyperechoic dots (the mixed-blizzard sign), after which biopsy was performed and adenocarcinoma was diagnosed. (F) RP-EBUS in the anterior segment of the left upper lobe showing an EBUS image containing the probe and biopsy revealed adenocarcinoma.
3. Diagnostic classification
A final diagnosis of malignancy was made based on the definite histological evidence of malignancy, or clinical features consistent with malignancy. Benign lung lesion was diagnosed according to the following criteria: identification of definite benign features, regression of the lesion with medical treatment, and a stable size for at least 12 months. Lung lesion that was neither benign nor malignant was defined as indefinite. Lesions diagnosed as benign both at the beginning and at the end were considered as true-negative. Lesions initially diagnosed as benign but finally diagnosed with malignancy (EBUS pathologic result false-negative) were designated as false-negative. Indefinite final diagnosis and invisible on RP-EBUS cases were also considered as false-negative.
4. Statistical analyses
Continuous variables were compared to Student’s t test or the Mann-Whitney U test and were expressed as means±standard deviations. Categorical variables were compared using chi-square or Fisher exact tests and were described as frequencies (percentages). We calculated the diagnostic yield by dividing the number of diagnostic successes by the total number of cases. To explore factors that affected diagnostic yield, the study population was divided into two groups: a diagnostic success group (true-positive and true-negative results) and a diagnostic failure group (false-positive, and false-negative results). Univariable and multivariable (using the factors with p<0.1 in univariable analyses) logistic regression analyses were performed to identify factors affecting the diagnostic yields. In all analyses, p<0.05 under a two-tailed test was considered as statistically significant. All statistical procedures were performed using SPSS version 24.0 (IBM Corp., Armonk, NY, USA).
5. Ethics statement
This study was conducted in accordance with the tenets of the Declaration of Helsinki, and its protocol was reviewed and approved by the institutional review board of Yeungnam University Hospital (YUH IRB 2020–09–025). The requirement for informed consent was waived because of the retrospective study design.
Results
1. Baseline characteristics
The baseline characteristics of the 607 patients according to diagnostic success status are presented in Table 1. Their mean age was 67.8±12.0 years and 395 patients were men (65.1%). Chronic obstructive pulmonary disease (COPD; n=167, 27.5%) was the most common underlying lung disease, followed by old pulmonary tuberculosis (n=41, 6.8%), asthma (n=16, 2.6%), idiopathic pulmonary fibrosis (n=12, 2.0%), combined pulmonary fibrosis and emphysema (n=6, 1.0%), and pneumoconiosis (n=6, 1.0%). The mean percent of predicted forced expiratory volume in 1 second was 83.0%±19.5%. The most common location of the lung lesion was the right upper lobe (n=172, 28.3%), and the mean distance from the pleura to the lung lesion was 13.4±13.2 mm. The PPLs were significantly larger in the diagnostic success group than in the diagnostic failure group (32.8±16.2 mm vs. 23.5±13.7 mm, p<0.001). The lung lesions were classified as solid (n=355, 58.5%), part-solid (n=53, 8.7%), ground-glass opacity (n=24, 4.0%), cavity (n=71, 11.7%), and consolidation (n=104, 17.1%). An EBUS image with the probe within the lesion was observed considerably more frequently in the diagnostic success group (82.3% vs. 31.0%, p<0.001). The mean procedure time was 18.2±8.1 minutes.
Table 1.
Baseline characteristics of the patients according to diagnostic success status
| Characteristic | Total (n=607) | Diagnostic success (n=462) | Diagnostic failure (n=145) | p-value |
|---|---|---|---|---|
| Patients | ||||
| Age, yr | 67.8±12.0 | 68.2±12.0 | 66.6±11.8 | 0.170 |
| Male sex | 395 (65.1) | 300 (64.9) | 95 (65.5) | 0.898 |
| Underlying lung disease | 0.579 | |||
| COPD | 167 (27.5) | 126 (27.3) | 41 (28.3) | |
| Asthma | 16 (2.6) | 14 (3.0) | 2 (1.4) | |
| IPF | 12 (2.0) | 11 (2.4) | 1 (0.7) | |
| CPFE | 6 (1.0) | 6 (1.3) | 0 (0) | |
| Old pulmonary TB | 41 (6.8) | 33 (7.1) | 8 (5.5) | |
| Pneumoconiosis | 6 (1.0) | 5 (1.1) | 1 (0.7) | |
| Pulmonary function test, % | ||||
| FEV1 | 83.0±19.5 | 82.2±18.9 | 85.7±20.9 | 0.061 |
| FVC | 82.0±16.8 | 81.1±16.7 | 84.9±17.2 | 0.017 |
| FEV1/FVC | 73.2±11.4 | 73.2±11.3 | 73.3±11.8 | 0.927 |
| Lung lesions | ||||
| Location | 0.820 | |||
| RUL | 172 (28.3) | 130 (28.1) | 42 (29.0) | |
| RML | 32 (5.3) | 24 (5.2) | 8 (5.5) | |
| RLL | 151 (24.9) | 119 (25.8) | 32 (22.1) | |
| LUL | 161 (26.5) | 118 (25.5) | 43 (29.6) | |
| LLL | 91 (15.0) | 71 (15.4) | 20 (13.8) | |
| Distance from pleura (mm) | 13.4±13.2 | 13.3±13.2 | 13.8±13.2 | 0.691 |
| Size (mm) | 31.0±16.1 | 32.8±16.2 | 23.5±13.7 | <0.001 |
| Characteristics | <0.001 | |||
| Solid | 355 (58.5) | 276 (59.7) | 79 (54.5) | |
| Part-solid | 53 (8.7) | 32 (6.9) | 21 (14.5) | |
| Ground-glass opacity | 24 (4.0) | 11 (2.4) | 13 (9.0) | |
| Cavity | 71 (11.7) | 54 (11.7) | 17 (11.7) | |
| Consolidation | 104 (17.1) | 89 (19.3) | 15 (10.3) | |
| Bronchus sign in CT | <0.001 | |||
| Positive | 476 (78.4) | 399 (86.4) | 77 (53.1) | |
| Negative | 131 (21.6) | 63 (13.6) | 68 (46.9) | |
| Procedure | ||||
| EBUS image | <0.001 | |||
| Within | 425 (70.0) | 380 (82.3) | 45 (31.0) | |
| Adjacent | 112 (18.5) | 82 (17.7) | 30 (20.7) | |
| Invisible | 70 (11.5) | 0 (0.0) | 70 (48.3) | |
| No. of forceps biopsies per lesion* (n=537) | 5.1±1.8 | 5.3±1.7 | 4.0±2.1 | <0.001 |
| Procedure time, min | 18.2±8.1 | 19.3±7.9 | 17.4±8.1 | <0.001 |
Values are presented as mean±standard deviation or number (%).
Number excluding lesions that failed to perform biopsies due to invisible case.
COPD: chronic obstructive pulmonary disease; IPF: idiopathic pulmonary fibrosis; CPFE: combined pulmonary fibrosis and emphysema; TB: tuberculosis; FEV1: forced expiratory volume in one second; FVC: forced vital capacity; RUL: right upper lobe; RML: right middle lobe; RLL: right lower lobe; LUL: left upper lobe; LLL: left lower lobe; CT: computed tomography; EBUS: endobronchial ultrasound.
2. Pathologic results and diagnostic performance
The initial pathologic results and final diagnosis are listed in Table 2. Out of the 607 lung lesions, 373 (61.4%) were diagnosed as malignant, 178 (29.3%) as benign, and 56 (9.2%) as indefinite. Among the malignant lesions (n=373), 304 (81.5%) were diagnosed by RP-EBUS-TBLB. Lesions with false-negatives (n=69) were diagnosed as malignant by percutaneous transthoracic needle biopsy (n=36), surgical resection (n=20), EBUS-guided transbronchial needle aspiration (n=11), and bone biopsy (n=2). Adenocarcinoma of the lung (n=228, 61.1%) was the most common diagnosis among definitive malignant diagnoses. Among the benign lesions, pneumonia (n=79, 44.4%) was the most common diagnosis among definitive benign features. The diagnostic performance of RP-EBUS-TBLB according to the size of the PPLs is summarized in Table 3. The sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy of RP-EBUS-TBLB were 67.8% (305/450), 100% (157/157), 100% (305/305), 52.0% (157/302), and 76.1% (462/607), respectively. The diagnostic performance of RP-EBUS-TBLB was best for PPLs>30 mm group (87.7%), followed by the 20–30 mm group (78.2%) and <20 mm group (54.7%).
Table 2.
Initial pathologic results and final diagnosis
| Initial pathologic results (n=607) | Final diagnosis (n=607) | |
|---|---|---|
| Malignant | 304 | 373 |
| Adenocarcinoma | 194 | 228 |
| Adenosquamous cell carcinoma | 3 | 3 |
| Squamous cell carcinoma | 57 | 72 |
| NSCLC, NOS | 31 | 38 |
| SCLC | 9 | 11 |
| Metastatic carcinoma | 6 | 15 |
| Neuroendocrine tumor | 1 | 3 |
| Malignant lymphoma | 3 | 3 |
| Benign | 233 | 178 |
| Pneumonia | 16 | 79 |
| Pulmonary TB | 11 | 45 |
| Nontuberculous mycobacteria | 4 | 18 |
| Aspergillosis | 4 | 5 |
| Actinomycosis | 1 | 2 |
| Cryptococcosis | 1 | 1 |
| Chondroid hamartoma | 1 | 3 |
| Nonspecific benign features | 88 | 25 |
| Negative for malignant cell | 44 | - |
| Atypical pneumocytes | 10 | - |
| Chronic granulomatous inflammation | 21 | - |
| Anthracosis | 11 | - |
| Total necrosis | 2 | - |
| Chronic inflammation | 126 | - |
| No definitive diagnosis | - | 56 |
| Invisible on EBUS | 70 | - |
NSCLC: non-small cell lung cancer; NOS: not otherwise specified; SCLC: small cell lung cancer; TB: tuberculosis; EBUS: endobronchial ultrasound.
Table 3.
Diagnostic performance of RP-EBUS-TBLB according to the size of PPLs
| Parameter | <20 mm (n=159) | 20–30 mm (n=188) | >30 mm (n=260) | Diagnostic performance (n=607) |
|---|---|---|---|---|
| True-positive, n | 54 | 102 | 149 | 305 |
| True-negative, n | 33 | 45 | 79 | 157 |
| False-positive, n | 0 | 0 | 0 | 0 |
| False-negative, n | 72 | 41 | 32 | 145 |
| EBUS pathologic result false negative, n | 15 | 12 | 8 | 35 |
| Indefinite final diagnosis, n | 19 | 8 | 13 | 40 |
| Invisible on EBUS | 38 | 21 | 11 | 70 |
| Sensitivity, % | 42.9 | 71.3 | 82.3 | 67.8 |
| Specificity, % | 100.0 | 100.0 | 100.0 | 100.0 |
| PPV, % | 100.0 | 100.0 | 100.0 | 100.0 |
| NPV, % | 31.4 | 52.3 | 71.2 | 52.0 |
| Diagnostic accuracy | 54.7 | 78.2 | 87.7 | 76.1 |
RP-EBUS-TBLB: radial probe endobronchial ultrasound-guided transbronchial lung biopsy; PPL: peripheral pulmonary lesion; PPV: positive predictive value; NPV: negative predictive value.
3. Factors affecting diagnostic success
In patients with definitive final diagnoses, we investigated factors affecting diagnostic success (Table 4). Univariable analyses revealed that larger size (≥20 mm; odds ratio [OR], 4.25; 95% CI, 2.85–6.35; p<0.001), positive bronchus sign in chest CT (OR, 5.59; 95% CI, 3.67–8.52; p<0.001), a solid lesion (OR, 3.00; 95% CI, 1.82–4.90; p<0.001), and an EBUS image with the probe within the lesion (OR, 10.30; 95% CI, 6.73–15.75 p<0.001) were significantly associated with diagnostic success. Based on multivariable analyses, larger size (≥20 mm; OR, 2.06; 95% CI, 1.27–3.33; p=0.003), positive bronchus sign in chest CT (OR, 2.30; 95% CI, 1.40–3.78; p=0.001), a solid lesion (OR, 2.40; 95% CI, 1.31–4.41; p=0.005), and an EBUS image with the probe within the lesion (OR, 6.98; 95% CI, 4.38–11.12; p<0.001) were independent factors affecting diagnostic success.
Table 4.
Factors affecting diagnostic success of RP-EBUS-TBLB using a GS without fluoroscopy for diagnosing PPLs
| Diagnostic success (n=462) | Diagnostic failure (n=145) | Univariable analyses |
Multivariable analyses |
||||
|---|---|---|---|---|---|---|---|
| Odds ratio (95% confidence interval) | p-value | Odds ratio (95% confidence interval) | p-value | ||||
| Age, yr | 68.2±12.0 | 66.6±11.8 | 1.01 (0.99–1.03) | 0.170 | - | - | |
| Male sex | 300 (64.9) | 95 (65.5) | 1.03 (0.69–1.52) | 0.898 | - | - | |
| Size, mm | 32.8±16.2 | 23.5±13.7 | 1.05 (1.04–1.07) | <0.001 | - | - | |
| ≥20 | 375 (81.2) | 73 (50.3) | 4.25 (2.85–6.35) | <0.001 | 2.06 (1.27–3.33) | 0.003 | |
| <20 | 87 (18.8) | 72 (49.7) | 1.00 | - | - | - | |
| Bronchus sign in chest CT | - | - | - | - | - | - | |
| Positive | 399 (86.4) | 77 (53.1) | 5.59 (3.67–8.52) | <0.001 | 2.30 (1.40–3.78) | 0.001 | |
| Negative | 63 (13.6) | 68 (46.9) | 1.00 | - | - | - | |
| Characteristic | |||||||
| Solid | 419 (90.7) | 111 (76.6) | 3.00 (1.82–4.90) | <0.001 | 2.40 (1.31–4.41) | 0.005 | |
| Non-solid | 43 (9.3) | 34 (23.4) | 1.00 | - | - | - | |
| EBUS image | |||||||
| Within | 380 (82.3) | 45 (31.0) | 10.30 (6.73–15.75) | <0.001 | 6.98 (4.38–11.12) | <0.001 | |
| Adjacent to the lesion or outside | 82 (17.7) | 100 (69.0) | 1.00 | - | - | - | |
Values are presented as mean±standard deviation or number (%) unless otherwise indicated.
RP-EBUS-TBLB: radial probe endobronchial ultrasound-guided transbronchial lung biopsy; GS: guide sheath; PPL: peripheral pulmonary lesion; CT: computed tomography; Solid: solid+cavity+consolidation; Non-solid: part solid+ground-glass opacity.
4. Complications
Among the 607 patients who underwent RP-EBUS, there were 12 cases of pneumothorax (2.0%). Nine patients (1.5%) recovered with oxygen therapy and three (0.5%) required chest tube insertion.
Discussion
This study confirms that RP-EBUS-TBLB using a GS without fluoroscopy is a highly safe diagnostic method in patients with PPLs. The sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy of RP-EBUS-TBLB were 67.8%, 100%, 100%, 52.0%, and 76.1%, respectively. The diagnostic performance of RP-EBUS-TBLB was better in larger PPLs. Larger lesions (≥20 mm), positive bronchus sign in chest CT, a solid lesion, and an EBUS image with the probe within the lesion were independent factors affecting diagnostic success. Pneumothorax occurred in 2.0% of patients, and 0.5% required chest tube insertion. To the best of our knowledge, this is the largest study to have analyzed the utility of RP-EBUS-TBLB using a GS without fluoroscopy.
Kurimoto et al. [5] developed a technique for EBUS using a GS, and mentioned that EBUS-GS is a useful method for collecting samples from PPLs even when the lesions are too small to be detectable under fluoroscopy. In PPLs ≤20 mm, TBLB with GS showed a higher diagnostic sensitivity than the TBLB without GS for the diagnosis of PPLs [15]. In addition, fluoroscopy was not helpful to confirm whether the forceps were within the lesion, and the diagnostic yield was the same regardless of the use of fluoroscopy for PPLs≤20 mm. Advantages of the GS technique are that it provides access to bronchial lesions for repeated sampling and protects against bleeding from the biopsy site by wedging the GS into the bronchial lumen [5]. In diagnosing PPLs ≤20 mm, the diagnostic yield of our study (using a GS without fluoroscopy) was 54.7%, comparable to other studies using a GS with fluoroscopy [16-19]. In our experience, if GS is appropriately used, a high diagnostic rate can be expected if accurate localization and EBUS image findings are achieved, even if fluoroscopy is not used.
Regarding fluoroscopy, it may be combined with TBLB to confirm whether the forceps are within the lesion. Fluoroscopy can be more helpful in performing biopsy at lower lobe lesions with a high probability of re-positioning of GS due to respiration or coughing. As described in the methods section, the lesion was identified with the RP, perform gain on the first three lung tissue samples, re-inserted the RP to ensure that the GS was not re-positioned in the lesion, and then performed an extra biopsy. Using this approach, we addressed the disadvantages of not using fluoroscopy. As a result, the diagnostic success rate of the right lower lobe (78.8%, 119/151) and left lower lobe (78.0%, 71/91) was not different from the rate of other lobes, as shown in Table 1. It is important to improve the diagnosis of PPLs and reduce radiation exposure during the examination. Fluoroscopy has disadvantages, including excessive radiation exposure for patients and practitioners. In addition, fluoroscopy consumes additional space, manpower, and cost for installing a shield room. Thus, in institutions where fluoroscopy is difficult to use, RP-EBUS-TBLB using a GS without fluoroscopy can be considered as a useful method for diagnosing PPLs.
A few studies have explored the efficacy and safety of RP-EBUS-TBLB using a GS without fluoroscopy for PPLs. Yoshikawa et al. [10] were the first to publish the outcomes of RP-EBUS-TBLB in 123 PPLs using a GS without fluoroscopy. A total of 61.8% of PPLs were diagnosed, and the diagnostic yield for PPLs >20 mm (75.6%) was higher than PPLs ≤20 mm (29.7%). Lesions >2 cm and the location (middle lobe and the lingular segment) of the PPLs were independent predictors of diagnostic success [10]. It can be estimated that our research is a little superior in terms of diagnostic accuracy. The diagnostic accuracy was significantly different in PPLs smaller than 3 cm. The difference in baseline characteristics of PPLs between two studies may have affected the results. There was no difference in size of PPLs between the two studies. However, positive bronchus sign in chest CT was higher in our study (476 of 607 lesions, 78.5%) compared to the previous study (76 of 123 lesions, 61.8%). The high percentage of solid lesion in our study (87.3%) compared to the previous study (67.0%) may have also affected the diagnostic accuracy. Eberhardt et al. [11] conducted a randomized trial of multimodality diagnostic arms; in subgroup analyses, a diagnostic yield of 69% was achieved in EBUS-GS without fluoroscopy in 39 PPLs. Minami et al. [15] reported that the diagnostic sensitivity of 60 PPLs with EBUS-GS was 83.3%. Minezawa et al. [12] analyzed 149 PPLs who underwent EBUS-GS without fluoroscopy for small PPLs (≤30 mm) and a total diagnostic yield of 72.5% was reported. CT bronchus sign positive was an independent factor associated with diagnostic success. Zhu et al. [13] reported diagnosis rate of 64.0% for EBUS-GS without fluoroscopy among 150 PPLs. Our study analyzed 607 PPLs and the diagnostic accuracy was 76.1%. As reported in previous studies, lesions ≥20 mm, positive bronchus sign in chest CT, a solid lesion, and EBUS probe within the lesion were independent factors of diagnostic success.
Complication rates of RP-EBUS-TBLB were low in previous studies and most of the complications were small pneumothorax and minimal bleeding problems. One meta-analysis revealed that the overall complications were 2.8%, and chest tube insertion was required in 0.2% of cases [2]. One observational study focusing on complications of RP-EBUS-TBLB in 965 PPLs showed overall complication rates of 1.3%. Pneumothorax occurred in 0.8% of patients, and 0.3% of the patients required chest tube drainage [20]. Our study demonstrated that pneumothorax occurred in 12 patients (2.0%) and chest tube insertion was required in three patients (0.5%). The relatively high incidence of pneumothorax compared to other studies is thought to be due to the high proportion of COPD patients (27.8%). Indeed, all three patients who required chest tube insertion were COPD patients with emphysema.
This study had several limitations. First, since it was a retrospective study conducted at a single center with PPLs, the results cannot be generalized, and selection bias cannot be excluded. However, the pulmonologists performed RP-EBUS as a first-choice biopsy modality in their everyday routine practice, not just in selected patients. Second, although our patients were followed-up for at least 12 months, there were 56 patients who still had nodules with an indefinite diagnosis. Although most previously published articles in the fields of RP-EBUS excluded PPLs with an indefinite diagnosis to calculate diagnostic yield, our study included indefinite diagnosis cases in the calculation of diagnostic yield. Given the high diagnostic yield of RP-EBUS-TBLB with GS without fluoroscopy and the acceptable rates of complications, our study showed that it can be performed in routine clinical settings for diagnosing PPLs without fluoroscopy. Moreover, our results highlighted the important role of RP-EBUS in diagnosing PPLs, which required early diagnosis.
In conclusion, RP-EBUS-TBLB using a GS without fluoroscopy is a highly accurate diagnostic method without exposure to radiation and with acceptable complication rates for diagnosing PPLs. Lesions ≥20 mm, positive bronchus sign in chest CT, a solid lesion, and having the probe within the lesion were important for diagnostic success.
Footnotes
Authors’ Contributions
Conceptualization: Hong KS, Ahn H, Jang JG, Ahn JH. Data curation: Hong KS, Ahn H, Jang MH, Jang JG, Ahn JH. Investigation: Hong KS, Ahn H, Jang JG, Ahn JH. Supervision: Hong KS, Ahn H, Lee KH, Chung JH, Shin KC, Jin HJ, Lee SS, Jang JG, Ahn JH. Writing-original draft: Hong KS, Ahn JH. Writingreview & editing: Ahn JH.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Funding
This research was supported by the Bio & Medical Technology Development Program of the National Research Foundation (NRF) funded by the Ministry of Science & ICT (grant number 2021M3E5D1A0201526521 and 2021R1C1C100950811).
References
- 1.Ahn JH. An update on the role of bronchoscopy in the diagnosis of pulmonary disease. Yeungnam Univ J Med. 2020;37:253–61. doi: 10.12701/yujm.2020.00584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ali MS, Trick W, Mba BI, Mohananey D, Sethi J, Musani AI. Radial endobronchial ultrasound for the diagnosis of peripheral pulmonary lesions: a systematic review and meta-analysis. Respirology. 2017;22:443–53. doi: 10.1111/resp.12980. [DOI] [PubMed] [Google Scholar]
- 3.Sainz Zuniga PV, Vakil E, Molina S, Bassett RL, Jr, Ost DE. Sensitivity of radial endobronchial ultrasound-guided bronchoscopy for lung vancer in patients with peripheral pulmonary lesions: an updated meta-analysis. Chest. 2020;157:994–1011. doi: 10.1016/j.chest.2019.10.042. [DOI] [PubMed] [Google Scholar]
- 4.Steinfort DP, Khor YH, Manser RL, Irving LB. Radial probe endobronchial ultrasound for the diagnosis of peripheral lung cancer: systematic review and meta-analysis. Eur Respir J. 2011;37:902–10. doi: 10.1183/09031936.00075310. [DOI] [PubMed] [Google Scholar]
- 5.Kurimoto N, Miyazawa T, Okimasa S, Maeda A, Oiwa H, Miyazu Y, et al. Endobronchial ultrasonography using a guide sheath increases the ability to diagnose peripheral pulmonary lesions endoscopically. Chest. 2004;126:959–65. doi: 10.1378/chest.126.3.959. [DOI] [PubMed] [Google Scholar]
- 6.Steinfort DP, Einsiedel P, Irving LB. Radiation dose to patients and clinicians during fluoroscopically-guided biopsy of peripheral pulmonary lesions. Respir Care. 2010;55:1469–74. [PubMed] [Google Scholar]
- 7.Lee SC, Kim EY, Chang J, Lee SH, Han CH. Diagnostic value of the combined use of radial probe endobronchial ultrasound and transbronchial biopsy in lung cancer. Thorac Cancer. 2020;11:1533–40. doi: 10.1111/1759-7714.13425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Casutt A, Prella M, Beigelman-Aubry C, Fitting JW, Nicod L, Koutsokera A, et al. Fluoroscopic-guided radial endobronchial ultrasound without guide sheath for peripheral pulmonary lesions: a safe and efficient combination. Arch Bronconeumol. 2015;51:338–43. doi: 10.1016/j.arbres.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 9.Lee K. New wine into new wineskins: radial endobronchial ultrasound for parenchymal lung infiltration. Tuberc Respir Dis. 2019;82:264–5. doi: 10.4046/trd.2019.0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yoshikawa M, Sukoh N, Yamazaki K, Kanazawa K, Fukumoto S, Harada M, et al. Diagnostic value of endobronchial ultrasonography with a guide sheath for peripheral pulmonary lesions without X-ray fluoroscopy. Chest. 2007;131:1788–93. doi: 10.1378/chest.06-2506. [DOI] [PubMed] [Google Scholar]
- 11.Eberhardt R, Anantham D, Ernst A, Feller-Kopman D, Herth F. Multimodality bronchoscopic diagnosis of peripheral lung lesions: a randomized controlled trial. Am J Respir Crit Care Med. 2007;176:36–41. doi: 10.1164/rccm.200612-1866OC. [DOI] [PubMed] [Google Scholar]
- 12.Minezawa T, Okamura T, Yatsuya H, Yamamoto N, Morikawa S, Yamaguchi T, et al. Bronchus sign on thin-section computed tomography is a powerful predictive factor for successful transbronchial biopsy using endobronchial ultrasound with a guide sheath for small peripheral lung lesions: a retrospective observational study. BMC Med Imaging. 2015;15:21. doi: 10.1186/s12880-015-0060-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhu J, Tang F, Gu Y. A prospective study on the diagnosis of peripheral lung cancer using endobronchial ultrasonography with a guide sheath and computed tomography-guided transthoracic needle aspiration. Ther Adv Med Oncol. 2018;10:1758834017752269. doi: 10.1177/1758834017752269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tay JH, Irving L, Antippa P, Steinfort DP. Radial probe endobronchial ultrasound: factors influencing visualization yield of peripheral pulmonary lesions. Respirology. 2013;18:185–90. doi: 10.1111/j.1440-1843.2012.02276.x. [DOI] [PubMed] [Google Scholar]
- 15.Minami D, Takigawa N, Morichika D, Kubo T, Ohashi K, Sato A, et al. Endobronchial ultrasound-guided transbronchial biopsy with or without a guide sheath for diagnosis of lung cancer. Respir Investig. 2015;53:93–7. doi: 10.1016/j.resinv.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 16.Kikuchi E, Yamazaki K, Sukoh N, Kikuchi J, Asahina H, Imura M, et al. Endobronchial ultrasonography with guide-sheath for peripheral pulmonary lesions. Eur Respir J. 2004;24:533–7. doi: 10.1183/09031936.04.00138603. [DOI] [PubMed] [Google Scholar]
- 17.Asahina H, Yamazaki K, Onodera Y, Kikuchi E, Shinagawa N, Asano F, et al. Transbronchial biopsy using endobronchial ultrasonography with a guide sheath and virtual bronchoscopic navigation. Chest. 2005;128:1761–5. doi: 10.1378/chest.128.3.1761. [DOI] [PubMed] [Google Scholar]
- 18.Boonsarngsuk V, Kanoksil W, Laungdamerongchai S. Comparison of diagnostic performances among bronchoscopic sampling techniques in the diagnosis of peripheral pulmonary lesions. J Thorac Dis. 2015;7:697–703. doi: 10.3978/j.issn.2072-1439.2015.04.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen A, Chenna P, Loiselle A, Massoni J, Mayse M, Misselhorn D. Radial probe endobronchial ultrasound for peripheral pulmonary lesions: a 5-year institutional experience. Ann Am Thorac Soc. 2014;11:578–82. doi: 10.1513/AnnalsATS.201311-384OC. [DOI] [PubMed] [Google Scholar]
- 20.Hayama M, Izumo T, Matsumoto Y, Chavez C, Tsuchida T, Sasada S. Complications with endobronchial ultrasound with a guide sheath for the diagnosis of peripheral pulmonary lesions. Respiration. 2015;90:129–35. doi: 10.1159/000431383. [DOI] [PubMed] [Google Scholar]


