Abstract
Background
There are few studies on patients with heart failure (HF) hospitalized for COVID-19. Our aim is to describe the clinical characteristics of patients with HF hospitalized for COVID-19 and identify risk factors for in-hospital mortality upon admission.
Methods
We conducted a retrospective, multicenter study in patients with HF hospitalized for COVID-19 in 150 Spanish hospitals (SEMI-COVID-19 Registry). A multivariate logistic regression analysis was performed to identify admission factors associated with in-hospital mortality.
Results
A total of 1718 patients were analyzed (56.5% men; median age 81.4 years). The overall case fatality rate was 47.6% (n = 819). The independent risk factors at admission for in-hospital mortality were: age (adjusted odds ratio [AOR]: 1.03; 95% confidence interval [95%CI]: 1.02–1.05; p < 0.001); severe dependence (AOR: 1.62; 95%CI: 1.19–2.20; p = 0.002); tachycardia (AOR: 1.01; 95%CI: 1.00–1.01; p = 0.004); and high C-reactive protein (AOR: 1.004; 95%CI:1.002−1.004; p < 0.001), LDH (AOR: 1.001; 95%CI: 1.001−1.002; p < 0.001), and serum creatinine levels (AOR: 1.35; 95%CI: 1.18−1.54; p < 0.001).
Conclusions
Patients with HF hospitalized for COVID-19 have a high in-hospital mortality rate. Some simple clinical and laboratory tests can help to identify patients with a worse prognosis.
Keywords: Heart failure, Coronavirus disease-2019, Hospitalization, Risk factor, Mortality
Abstract
Introducción
Existen pocos estudios sobre pacientes con insuficiencia cardíaca (IC) ingresados por COVID-19. Nuestro objetivo es describir las características clínicas de los pacientes con IC ingresados por COVID-19 e identificar los factores de riesgo al ingreso de mortalidad intrahospitalaria.
Material y métodos
Estudio retrospectivo y multicéntrico de pacientes con IC ingresados por COVID-19 en 150 hospitales españoles (Registro SEMI-COVID-19). Se realizó un análisis de regresión logística para identificar los factores de riesgo al ingreso asociados a la mortalidad.
Resultados
Se analizaron 1.718 pacientes (56,5% varones; edad mediana 81,4 años). La tasa de mortalidad global fue del 47,6% (n = 819). Los factores de riesgo independientes al ingreso para mortalidad fueron: la edad (odds ratio ajustado [ORA]: 1,03; intervalo de confianza 95% [IC95%]: 1,02–1,05; p < 0,001), la dependencia severa (ORA: 1,62; IC95%: 1,19–2,20; p = 0,002), la taquicardia (ORA: 1,01; IC95%: 1,00–1,01; p = 0,004), la proteína C reactiva (ORA: 1,004; IC95%:1,002–1,004; p < 0,001), la LDH (ORA: 1,001; IC95%: 1,001–1,002; p < 0,001) y la creatinina sérica (ORA: 1,35; IC95%: 1,18–1,54; p < 0,001).
Conclusiones
Los pacientes con IC hospitalizados por COVID-19 tienen una alta mortalidad intrahospitalaria. Existen factores clínico-analíticos simples que pueden ayudar a identificar a los pacientes con peor pronóstico.
Palabras clave: Insuficiencia cardíaca, Enfermedad por coronavirus-2019, Hospitalización, Factor de riesgo, Mortalidad
Introduction
The coronavirus-2019 disease (COVID-19), caused by SARS-CoV-2, is associated with elevated morbidity and mortality1, 2. Since the onset of the pandemic, cardiovascular disease has been identified as a risk factor for COVID-19, with cardiovascular complications being common over the course of the disease3. Spain is one of the countries with the highest number of patients with SARS-CoV-2 in the world. The first case of COVID-19 infection was confirmed on 31 January 2020, with 2,670,102 confirmed cases as of 27 January 20214.
Heart failure (HF) in Spain represents 3% of hospital admissions and is the number one cause of hospitalisation in patients over the age of 655. The aging population and healthcare advancements are the main factors associated with this growing increase in admissions due to HF5, 6.
To date, few studies have been published regarding mortality in patients with HF and COVID-19 infection. Álvarez-García et al. found that patients with a history of HF show a significant increase in mortality and need for invasive mechanical ventilation associated with COVID-19 infection, regardless of their ventricular ejection fraction7. Rey et al. concluded that patients infected with COVID-19 are at higher risk of developing HF during hospital admission, with high mortality rates8.
Given the significant impact of both diseases independent of one another and their potential feedback when combined, the main aim of this study is to describe the clinical characteristics of patients with a history of HF and/or new-onset HF who are admitted for COVID-19, and to identify risk factors at admission for in-hospital mortality.
Material and methods
Study design
An observational, retrospective, multicentre national study was conducted with patients hospitalised due to COVID-19 from 01 March to 01 October 2020. The data was obtained from the SEMI-COVID-19 Registry from the Spanish Society for Internal Medicine (SEMI). A total of 150 Spanish hospitals participated in the registry9. The SEMI-COVID-19 Registry includes consecutive patients over the age of 18 with COVID-19 disease microbiologically confirmed via reverse transcription polymerase chain reaction testing (RT-PCR) obtained via nasal swab, saliva sample, or bronchoalveolar lavage9.
For this study, we selected those patients with a history of HF and/or that had suffered from HF as a complication during hospital admission due to COVID-19.
Variables
Clinical, epidemiological, radiological, and therapeutic variables were analysed as well as mortality during admission or early readmission, defined as a new episode of hospital admission within 30 days post-discharge.
The researchers collected the data from the SEMI-COVID-19 Registry database9.
Diagnosis of HF was determined according to the clinical congestion criteria (dyspnoea, oedema, and increased jugular venous pressure) in the medical history. The comorbidity burden of patients was established with the Age-Adjusted Charlson Comorbidity Index10.
The Barthel Index was used to establish functional condition prior to hospital admission11 (independent or slight dependency: 100-91; moderate dependency: 90-61; severe dependency: ≤60). Patients were considered to have arterial hypertension, diabetes mellitus, or dyslipidaemia if they had a prior diagnosis in their medical history or were receiving medical treatment for these diseases.
Diabetes mellitus was classified according to 2 subgroups: with target organ damage (brain, heart, kidney, or retinal involvement) or without target organ damage. Chronic lung disease was defined as a prior diagnosis of chronic obstructive pulmonary disease and/or asthma. Arteriosclerotic cardiovascular disease was defined as a prior history of ischaemic heart disease (acute myocardial infarction, acute coronary syndrome, angina, or coronary revascularization). Neoplastic disease included all non-metastatic solid tumours (excluding non-melanoma skin tumours). Moderate-severe kidney disease was defined as glomerular filtration < 45 mL/min/1.73 m2 according to the CKD-EPI equation12. Moderate-severe liver disease was defined as class B or C according to the Child-Pugh score13. Obesity was considered a body mass index ≥ 30 kg/m2. Comorbidities were recorded from the medical histories from each hospital.
The laboratory data (hemogram, biochemical profile, blood gas, coagulation tests) and imaging tests were collected at admission. Treatments used were classified as: (1) antimicrobial therapy (hydroxychloroquine, lopinavir/ritonavir or remdesivir); (2) immunomodulatory therapy (systemic glucocorticoids, immunoglobulins, baricitinib or tocilizumab); (3) anticoagulant therapy (low molecular weight heparin); (4) ventilator support (high flow nasal cannula, invasive and non-invasive mechanical ventilation), and (5) pronation therapy.
In-hospital complications included: admission to the intensive care unit (ICU) and presence of acute respiratory distress syndrome (ARDS), acute coronary syndrome, acute HF, arrhythmia, shock, sepsis, acute kidney failure, venous thromboembolism, or acute arterial ischaemia.
Statistical analysis
Patients were classified according to the categorical variable of mortality as deceased or not deceased. The categorical and continuous variables were expressed as absolute values and percentages and as medians (ranges), respectively. The differences between groups were analysed using Student’s t-test or the Mann–Whitney U test for continuous variables or Pearson's chi-squared test for categorical variables. A p-value <.05 was considered statistically significant; subsequently, a multivariate analysis was performed expressed as an adjusted odds ratio (AOR), with a 95% confidence interval (95% CI).
A logistic regression analysis was used to identify independent factors at admission for in-hospital mortality, including variables with statistical significance in the bivariate analysis and with a percentage of missing data of less than 20%. The statistical analysis was conducted with SPSS software version 26.0 (IBM SPSS Statistics©).
Ethical aspects
All the patients gave their informed consent. This study was conducted according to the Declaration of Helsinki and was approved by the Málaga Ethics Committee (Code: SEMI-COVID-19 27-03-20). The STROBE initiative for the publication of observational studies was followed (available at www.strobe-statement.org).
Results
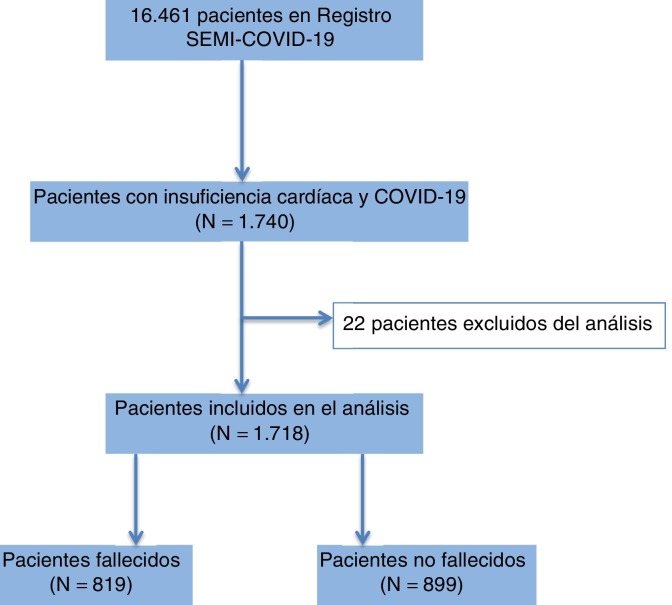
Of the 16,461 patients included in the SEMI-COVID-19 Registry, 1740 had documented history of HF and/or had suffered from HF as a complication during hospital admission due to COVID-199. A total of 22 patients were excluded due to a lack of basic data for correct demographics, meaning the final analysis was conducted with 1718 patients (10.4%). Of these, 819 (47.6%) died during admission (Fig. 1 ).
Figure 1.
Flow diagram of the study.
The clinical characteristics and laboratory data for the patients classified as deceased and not deceased are included in Table 1 . The patients who died were significantly older, were male, and had higher comorbidity and dependency. In addition, there was a higher proportion of diabetics with target organ damage, arterial hypertension, and moderate-severe kidney failure among the deceased. Other conditions that were also more frequent in the deceased patients were high heart rate, presence of tachypnoea, low oxygen saturation, and the present of bilateral pulmonary consolidation at admission. Likewise, high mortality was associated with higher blood levels of c-reactive protein (CRP), D-dimer, lactate dehydrogenase (LDH), urea, creatinine and lactate, and a lower number of lymphocytes at admission.
Table 1.
Clinical characteristics, presentation, and laboratory and radiology data for patients with heart failure hospitalised for COVID-19.
| Total (n = 1,718) | Deceased (n = 819) | Not deceased (n = 899) | p-value | |
|---|---|---|---|---|
| Age (years) | 81.4 (22–102.1) | 83.6 (26–102.1) | 79.4 (26.5–101.5) | <0.001 |
| Male sex | 971 (56.5%) | 489 (59.7%) | 482 (53.6%) | 0.011 |
| Comorbidities | ||||
| Charlson Index > 4 | 155 (9%) | 93 (11.3%) | 62 (6.8%) | 0.002 |
| Barthel Index ≤ 60 | 648 (37.7%) | 380 (46.3%) | 268 (29.8%) | <0.001 |
| Tobacco | 93 (5.4%) | 36 (4.3%) | 57 (6.3%) | 0.049 |
| DM without organ damage | 313 (18.2%) | 147 (17.9%) | 166 (18.4%) | 0.758 |
| DM with organ damage | 261 (15.1%) | 149 (18.2%) | 112 (12.5%) | 0.001 |
| Arterial hypertension | 1350 (78.5%) | 670 (81.9%) | 680 (75.7%) | 0.002 |
| Dyslipidaemia | 929 (54%) | 453 (55.4%) | 476 (53%) | 0.311 |
| COPD | 269 (15.6%) | 142 (17.3%) | 127 (14.2%) | 0.072 |
| Coronary artery disease | 312 (18.1%) | 157 (19.2%) | 155 (17.3%) | 0.311 |
| Atrial fibrillation | 709 (41.2%) | 357 (43.6%) | 352 (39.2%) | 0.065 |
| Chronic HF | 1167 (67.9%) | 526 (64.2%) | 641 (71.3%) | <0.001 |
| Solid neoplasm | 158 (9.1%) | 83 (10.1%) | 75 (8.4%) | 0.205 |
| Moderate-severe chronic kidney disease | 296 (17.2%) | 169 (20.7%) | 127 (14.1%) | <0.001 |
| Liver disease | 43 (2.5%) | 22 (2.7%) | 21 (2.3%) | 0.648 |
| Obesity | 435 (25.3%) | 190 (23.1%) | 245 (27.2%) | 0.135 |
| Physical examination | ||||
| HR (bpm) | 84 (34–180) | 85 (34–180) | 83 (34–170) | 0.004 |
| Tachypnoea (> 20 RR) | 785 (45.6%) | 459 (51.1%) | 326 (36.2%) | <0.001 |
| SatO2 (%) | 93 (53–100) | 92 (53–100) | 94 (54–100) | <0.001 |
| SBP (mmHg) | 129 (50–225) | 128 (50–225) | 130 (69–225) | 0.124 |
| Radiology | ||||
| Bilateral pulmonary consolidation | 515 (29.9%) | 297 (36.2%) | 218 (24.2%) | <0.001 |
| Laboratory | ||||
| CRP (mg/ L) | 69.5 (0–950) | 90 (0.4–950) | 55.1 (0–597) | <0.001 |
| D-dimer (ng/mL) | 946 (21–489,000) | 1205 (21–489,000) | 801 (1618–90,000) | <0.001 |
| LDH (U/L) | 342 (18–5209) | 390 (92–5209) | 316 (18–1735) | <0.001 |
| Leukocytes (x106/L) | 6860 (324–90,000) | 7500 (1618–90,000) | 6400 (324–90,000) | <0.001 |
| Lymphocytes (x106/L) | 850 (0–75,500) | 768 (0–57,830) | 910 (49–75,500) | <0.001 |
| Urea (mg/dL) | 58 (10–369) | 69.5 (10–369) | 50 (10–364) | <0.001 |
| Creatinine (mg/dL) | 1.18 (0.2–14.3) | 1.35 (0.33–14) | 1.02 (0.27–10) | <0.001 |
| Lactate (mmol/L) | 1.8 (0–100) | 1.9 (0.1–100) | 1.7 (0.1–100) | <0.001 |
The categorical and continuous variables were expressed as absolute values and percentages and as medians (ranges), respectively.
BPM: beats per minute; COPD: chronic obstructive pulmonary disease; COVID-19: disease caused by coronavirus-2019; CRP: C-reactive protein; DM: diabetes mellitus; HF: heart failure; HR: heart rate; LDH: lactate dehydrogenase; RR: respiratory rate (breaths per minute); SatO2: baseline oxygen saturation; SBP: systolic blood pressure.
A total of 1167 patients (67.9%) had a history of chronic HF prior to admission, and 526 of those died (45%). Mortality was higher for patients who experienced acute HF complications during admission than for those with a history of chronic HF prior to admission (53% vs. 45%, p < 0.05). The data for treatment and in-hospital complications can be seen in Table 2 .
Table 2.
Treatments and in-hospital complications of patients with heart failure hospitalised for COVID-19.
| Total (n = 1718) | Deceased (n = 819) | Not deceased (n = 899) | p-value | |
|---|---|---|---|---|
| Antimicrobial treatment | ||||
| Lopinavir-ritonavir | 776 (45.1%) | 348 (42.4%) | 428 (47.6%) | 0.039 |
| Remdesivir | 18 (1.0%) | 4 (0.4%) | 14 (1.5%) | 0.030 |
| Hydroxychloroquine | 1327 (77.2%) | 577 (70.4%) | 750 (83.4%) | <0.001 |
| Immunomodulators | ||||
| Tocilizumab | 132 (7.6%) | 66 (8.0%) | 66 (7.3%) | 0.575 |
| Immunoglobulins | 6 (0.3%) | 2 (0.2%) | 4 (0.4%) | 0.689 |
| Baricitinib | 8 (0.4%) | 1 (0.1%) | 7 (0.7%) | 0.072 |
| Glucocorticoids | 764 (44.4%) | 389 (47.4%) | 375 (41.7%) | 0.015 |
| Anticoagulant therapy | ||||
| LMWH | 1358 (79.8%) | 627 (46.2%) | 731(53.8%) | 0.013 |
| Ventilation support | ||||
| High-flow nasal cannula | 185 (10.7%) | 117 (14.2%) | 68 (7.5%) | <0.001 |
| NIMV | 139 (8.0%) | 92 (11.2%) | 47 (5.2%) | <0.001 |
| IMV | 141 (8.2%) | 86 (10.5%) | 55 (6.1%) | 0.001 |
| Pronation therapy | 219 (12.7%) | 130 (15.8%) | 89 (9.8%) | <0.001 |
| Complications | ||||
| Admission to ICU | 177 (10.3%) | 100 (12.2%) | 77 (8.5%) | 0.013 |
| PAD | 20 (1.1%) | 14 (1.7%) | 6 (0.6%) | 0.044 |
| VTE | 47 (2.7%) | 18 (2.1%) | 29 (3.2%) | 0.238 |
| Sepsis | 239 (13.9%) | 183 (22.3%) | 56 (6.2%) | <0.001 |
| Acute kidney failure | 602 (35.0%) | 389 (47.4%) | 213 (23.6%) | <0.001 |
| Shock | 174 (10.1%) | 140 (17.0%) | 34 (3.7%) | <0.001 |
| Acute coronary syndrome | 55 (3.2%) | 39 (4.7%) | 16 (1.7%) | <0.001 |
| Acute HF | 551 (32%) | 293 (35.7%) | 258 (28.6%) | <0.001 |
| Arrhythmia | 231 (13.4%) | 117 (14.2%) | 114 (12.6%) | 0.019 |
| ARDS | 889 (51.7%) | 629 (76.8%) | 260 (28.9%) | <0.001 |
The categorical variables are expressed in absolute values and percentages.
ARDS: acute respiratory distress syndrome; COVID-19: disease caused by coronavirus-2019; HF: heart failure; IMV: invasive mechanical ventilation; LMWH: low molecular weight heparin; NIMV: non-invasive mechanical ventilation; PAD: peripheral arterial disease; VTE: venous thromboembolism.
Following the logistic regression analysis, the risk factors at admission associated with higher in-hospital mortality were: age (>80 years), severe dependency class, tachycardia (>100 beats per minute), and elevated levels of CRP, LDH, and serum creatinine (Table 3 ).
Table 3.
Risk factors at admission associated with in-hospital mortality of patients with heart failure hospitalised due to COVID-19. Multiple regression analysis.
| AOR (95% CI) | p-value | |
|---|---|---|
| Age > 80 years | 1.035 (1.021−1.050) | <0.001 |
| Male sex | 1.33 (0.998−1.771) | 0.051 |
| Severe dependency | 1.625 (1.195−2.209) | 0.002 |
| Arterial hypertension | 1.23 (0.865−1.756) | 0.248 |
| SatO2 > 90% | 0.956 (0.934−0.979) | <0.001 |
| HR > 100 bpm | 1.011 (1.003−1.018) | 0.004 |
| CRP > 3 mg/L | 1.004 (1.002−1.004) | <0.001 |
| Creatinine > 1.17 mg/dL | 1.354 (1.185−1.548) | <0.001 |
| Lymphocytes < 1500 × 106/L | 1.000 (1.000−1.001) | 0.927 |
| LDH > 480 U/L | 1.001 (1.001−1.002) | <0.001 |
| D-dimer > 1000 ng/mL | 1.000 (1.000−1.000) | 0.474 |
95% CI: 95% confidence interval; AOR: adjusted odds ratio; BPM: beats per minute; CRP: C-reactive protein; HR: heart rate; LDH: lactate dehydrogenase; SatO2: baseline oxygen saturation.
Discussion
Heart failure represents one of the main reasons for hospitalisation in our environment14, 15. In recent years, the mortality rate for HF in Spain has been trending downwards thanks to the incorporation of different treatments that have shown significant benefits5, the high level of adherence to guidelines by health professionals15, and the change of components of disease decompensation such as ischaemic heart disease, which has also been decreasing in recent years16.
In a recent study, Bromage et al. showed a clear increase in the mortality of patients admitted for HF and COVID-19, though it is unknown whether this is due to true mortality or due to a selection of critical patients who were admitted during the pandemic17.
Our study has shown that the presence of HF, both in patients with a prior history and those who developed it as a complication during admission, is associated with high hospital mortality rates close to 50%. In addition, it makes clear that patients who experienced decompensation due to acute HF while admitted died at a higher rate than patients with a history of HF prior to admission, with the former affecting mortality more than the latter. This reflects the impact of COVID-19 on developing acute HF. These percentages represent a significant increase compared to the mortality described in previous studies of patients hospitalised with HF, which range from 9.5% to 11%18, 19.
The most frequent causes of death in patients with a history of HF have been described as decompensated HF, sudden death, and non-cardiovascular causes20, 21. At the present moment, as our study suggests, SARS-CoV-2 is the primary cause of death in hospitalised HF patients.
Older age, elevated comorbidity burden, and degree of dependency are characteristic elements of patients with HF hospitalised due to COVID-19 in our country. This clinical profile, with figures close to 80% for arterial hypertension, 40% for atrial fibrillation, 20% for diabetes mellitus, 17% for moderate-severe chronic kidney disease, 25% for obesity, and 38% for severe functional dependency, represents a continuation of previous studies performed in our setting which have reported similar figures for these HF-related pathologies22, 23.
The patients with HF hospitalised due to COVID-19 from our study presented a large number of complications. The most frequent complication was ARDS, which exposes the inflammatory process that occurs in this patient profile induced by SARS-CoV-2. The severe inflammatory response triggered in COVID-19 has been described in previous studies.
Old age and chronic conditions are just some of the various clinical conditioning factors that could favour its development and predispose patients to the onset of complications and adverse events24, 25. In this sense, in our study we identified factors at admission that have been associated as risk factors for mortality in patients with HF hospitalised due to COVID-19. Old age has been determined to be one of the main factors associated with higher mortality due to COVID-1925, and we confirmed this in our population with HF.
On the other hand, the importance of assessing clinical condition at the time of admission is worth mentioning. Patients who present in critical condition will have a significantly worse prognosis than those presenting with these characteristics, with the former requiring stricter monitoring and follow-up. Other studies have also stressed this issue and its severity in COVID-19 illness26, 27.
In addition, the presence of certain altered biological markers in patients with HF can be aggravated by COVID-19 infection. In this way, kidney failure and high CRP and LDH levels were significantly associated with an increase in mortality. However, other markers of poor prognosis in COVID-19, such as lymphopenia or elevated D-dimer levels28, were not related to higher mortality in our population of patients with HF.
In any case, though the variables of heart rate and elevated LDH and CRP have been statistically associated with mortality, we must bear in mind that the association of these factors has been less important from the clinical perspective than other variables such as dependency or age. All of these factors, which are easily identifiable when patients are being admitted to hospital, define a patient profile that requires special care due to the high risk of complications and death that they entail.
This study presents important data regarding the clinical profile of a large number of patients with HF hospitalised due to COVID-19 and identifies at admission diverse clinical and analytical factors that are associated with mortality. Though it is the first study with these characteristics in our country and one of few around the world, it does have some limitations.
First, as an observational and retrospective study focusing on hospitalised patients, we analysed patients with more critical clinical situations, which could limit the results of the patient profile and not allow it to be extrapolated to the rest of the population of patients with HF. In addition, despite conducting a multivariate regression analysis, the possibility of unmeasured confounding variables cannot be ruled out.
On the other hand, the data were collected by a large number of researchers from hospitals with different levels of care, which entails a great degree of heterogeneity in its processing. It is also worth noting that, despite the large number of variables included in this registry, we are lacking important data about the characterisation of HF such as aetiology, the New York Heart Association functional class, the left ventricular ejection fraction, the level of natriuretic peptides, and the proportion of patients receiving other treatments such as beta blockers, neprilysin receptor antagonists, aldosterone antagonists, or diuretics. Lastly, nor does the provided information include data on the degree of compliance or the duration of the treatments prior to admission.
In terms of the strength of our study, the large number of patients with HF included in our series is worthy of mention, as it represented different centres from around the entire country, offering a wide-reaching vision of this patient group.
Conclusions
This study shows that patients with HF hospitalised due to COVID-19 in Spain have a high rate of mortality. Older age, severe dependency class, greater severity at initial presentation, kidney function decline, and elevated inflammatory blood parameters have been identified as predictors of mortality.
Given the impact of HF on COVID-19 and the involvement of various factors, it is necessary to develop prognostic scales that are easy to implement for these patients.
Funding
This research did not receive any specific funding from agencies from the public sector, commercial sector, or not-for-profit organisations.
Conflicts of interest
The authors declare that they do not have any conflicts of interest.
Acknowledgements
We would like to thank all the researchers from the SEMI-COVID-19 group and the SEMI-COVID-19 Registry coordination centre for their data quality control and logistical and administrative support.
Footnotes
Please cite this article as: Salinas-Botrán A, Sanz-Cánovas J, Pérez-Somarriba J, Pérez-Belmonte LM, Cobos-Palacios L, Rubio-Rivas M, et al. Características clínicas y factores de riesgo de mortalidad al ingreso en pacientes con insuficiencia cardíaca hospitalizados por COVID-19 en España. Rev Clin Esp. 2022;222:255–265.
Appendix A. Members of the SEMI-COVID-19 Registry
Coordinator of the SEMI-COVID-19 Registry: José Manuel Casas Rojo.
Members of the SEMI-COVID-19 Registry Scientific Committee: José Manuel Casas Rojo, José Manuel Ramos Rincón, Carlos Lumbreras Bermejo, Jesús Millán Núñez-Cortés, Juan Miguel Antón Santos, Ricardo Gómez-Huelgas.
Members of the SEMI-COVID-19 Group:
H. U. 12 de Octubre. Madrid: Paloma Agudo de Blas, Coral Arévalo Cañas, Blanca Ayuso, José Bascuñana Morejón, Samara Campos Escudero, María Carnevali Frías, Santiago Cossío Tejido, Borja de Miguel Campo, Carmen Díaz Pedroche, Raquel Díaz Simón, Ana García Reyne, Lucia Jorge Huerta, Antonio Lalueza Blanco, Jaime Laureiro Gonzalo, Carlos Lumbreras Bermejo, Guillermo Maestro de la Calle, Barbara Otero Perpiña, Diana Paredes Ruiz, Marcos Sánchez Fernández, Javier Tejada Montes.
H. U. Gregorio Marañón. Madrid: Laura Abarca Casas, Álvaro Alejandre de Oña, Rubén Alonso Beato, Leyre Alonso Gonzalo, Jaime Alonso Muñoz, Crhistian Mario Amodeo Oblitas, Cristina Ausín García, Marta Bacete Cebrián, Jesús Baltasar Corral, María Barrientos Guerrero, Alejandro Bendala Estrada, María Calderón Moreno, Paula Carrascosa Fernández, Raquel Carrillo, Sabela Castañeda Pérez, Eva Cervilla Muñoz, Agustín Diego Chacón Moreno, María Carmen Cuenca Carvajal, Sergio de Santos, Andrés Enríquez Gómez, Eduardo Fernández Carracedo, María Mercedes Ferreiro-Mazón Jenaro, Francisco Galeano Valle, Alejandra García, Irene García Fernández-Bravo, María Eugenia García Leoni, María Gómez Antunez, Candela González San Narciso, Anthony Alexander Gurjian, Lorena Jiménez Ibáñez, Cristina Lavilla Olleros, Cristina Llamazares Mendo, Sara Luis García, Víctor Mato Jimeno, Clara Millán Nohales, Jesús Millán Núñez-Cortés, Sergio Moragón Ledesma, Antonio Muiño Miguez, Cecilia Muñoz Delgado, Lucía Ordieres Ortega, Susana Pardo Sánchez, Alejandro Parra Virto, María Teresa Pérez Sanz, Blanca Pinilla Llorente, Sandra Piqueras Ruiz, Guillermo Soria Fernández-Llamazares, María Toledano Macías, Neera Toledo Samaniego, Ana Torres do Rego, María Victoria Villalba García, Gracia Villarreal, María Zurita Etayo.
Hospital Universitari de Bellvitge. L'Hospitalet de Llobregat. Barcelona: Xavier Corbella, Narcís Homs, Abelardo Montero, José María Mora-Luján, Manuel Rubio Rivas.
H. U. La Paz-Cantoblanco-Carlos III. Madrid: Jorge Álvarez Troncoso, Francisco Arnalich Fernández, Francisco Blanco Quintana, Carmen Busca Arenzana, Sergio Carrasco Molina, Aranzazu Castellano Candalija, Germán Daroca Bengoa, Alejandro de Gea Grela, Alicia de Lorenzo Hernández, Alejandro Díez Vidal, Carmen Fernández Capitán, María Francisca García Iglesias, Borja González Muñoz, Carmen Rosario Herrero Gil, Juan María Herrero Martínez, Víctor Hontañón, María Jesús Jaras Hernández, Carlos Lahoz, Cristina Marcelo Calvo, Juan Carlos Martín Gutiérrez, Mónica Martínez Prieto, Elena Martínez Robles, Araceli Menéndez Saldaña, Alberto Moreno Fernández, José María Mostaza Prieto, Ana Noblejas Mozo, Carlos Manuel Oñoro López, Esmeralda Palmier Peláez, Marina Palomar Pampyn, María Angustias Quesada Simón, Juan Carlos Ramos Ramos, Luis Ramos Ruperto, Aquilino Sánchez Purificación, Teresa Sancho Bueso, Raquel Sorriguieta Torre, Clara Itziar Soto Abanedes, Yeray Untoria Tabares, Marta Varas Mayoral, Julia Vásquez Manau.
C. H. U. de Albacete. Albacete: José Luis Beato Pérez, María Lourdes Sáez Méndez.
Complejo Asistencial de Segovia. Segovia: Eva María Ferreira Pasos, Daniel Monge Monge, Alba Varela García.
H. U. Puerta de Hierro. Majadahonda. Madrid: María Álvarez Bello, Ane Andrés Eisenhofer, Ana Arias Milla, Isolina Baños Pérez, Javier Bilbao Garay, Silvia Blanco Alonso, Jorge Calderón Parra, Alejandro Callejas Díaz, José María Camino Salvador, Mª Cruz Carreño Hernández, Valentín Cuervas-Mons Martínez, Sara de la Fuente Moral, Miguel del Pino Jiménez, Alberto Díaz de Santiago, Itziar Diego Yagüe, Ignacio Donate Velasco, Ana María Duca, Pedro Durán del Campo, Gabriela Escudero López, Esther Expósito Palomo, Ana Fernández Cruz, Esther Fiz Benito, Andrea Fraile López, Amy Galán Gómez, Sonia García Prieto, Claudia García Rodríguez-Maimón, Miguel Ángel García Viejo, Javier Gómez Irusta, Edith Vanessa Gutiérrez Abreu, Isabel Gutiérrez Martín, Ángela Gutiérrez Rojas, Andrea Gutiérrez Villanueva, Jesús Herráiz Jiménez, Pedro Laguna del Estal, Mª Carmen Máinez Sáiz, Cristina Martín Martín, María Martínez Urbistondo, Fernando Martínez Vera, Susana Mellor Pita, Patricia Mills Sánchez, Esther Montero Hernández, Alberto Mora Vargas, Cristina Moreno López, Alfonso Ángel-Moreno Maroto, Víctor Moreno-Torres Concha, Ignacio Morrás De La Torre, Elena Múñez Rubio, Ana Muñoz Gómez, Rosa Muñoz de Benito, Alejandro Muñoz Serrano, José María Palau Fayós, Ilduara Pintos Pascual, Antonio Ramos Martínez, Isabel Redondo Cánovas del Castillo, Alberto Roldán Montaud, Lucía Romero Imaz, Yolanda Romero Pizarro, Mónica Sánchez Santiuste, David Sánchez Ortiz, Enrique Sánchez Chica, Patricia Serrano de la Fuente, Pablo Tutor de Ureta, Ángela Valencia Alijo, Mercedes Valentín-Pastrana Aguilar, Juan Antonio Vargas Núñez, José Manuel Vázquez Comendador, Gema Vázquez Contreras, Carmen Vizoso Gálvez.
H. Miguel Servet. Zaragoza: Gonzalo Acebes Repiso, Uxua Asín Samper, María Aranzazu Caudevilla Martínez, José Miguel García Bruñén, Rosa García Fenoll, Jesús Javier González Igual, Laura Letona Giménez, Mónica Llorente Barrio, Luis Sáez Comet.
H. U. La Princesa. Madrid: María Aguilera García, Ester Alonso Monge, Jesús Álvarez Rodríguez, Claudia Álvarez Varela, Miquel Berniz Gòdia, Marta Briega Molina, Marta Bustamante Vega, José Curbelo, Alicia de las Heras Moreno, Ignacio Descalzo Godoy, Alexia Constanza Espiño Álvarez, Ignacio Fernández Martín-Caro, Alejandra Franquet López-Mosteiro, Gonzalo Gálvez Márquez, María J. García Blanco, Yaiza García del Álamo Hernández, Clara García-Rayo Encina, Noemí Gilabert González, Carolina Guillamo Rodríguez, Nicolás Labrador San Martín, Manuel Molina Báez, Carmen Muñoz Delgado, Pedro Parra Caballero, Javier Pérez Serrano, Laura Rabes Rodríguez, Pablo Rodríguez Cortés, Carlos Rodríguez Franco, Emilia Roy-Vallejo, Mónica Rueda Vega, Aresio Sancha Lloret, Beatriz Sánchez Moreno, Marta Sanz Alba, Jorge Serrano Ballester, Alba Somovilla, Carmen Suarez Fernández, Macarena Vargas Tirado, Almudena Villa Martí.
H. U. de A Coruña. A Coruña: Alicia Alonso Álvarez, Olaya Alonso Juarros, Ariadna Arévalo López, Carmen Casariego Castiñeira, Ana Cerezales Calviño, Marta Contreras Sánchez, Ramón Fernández Varela, Santiago J. Freire Castro, Ana Padín Trigo, Rafael Prieto Jarel, Fátima Raad Varea, Laura Ramos Alonso, Francisco Javier Sanmartín Pensado, David Vieito Porto.
H. Clínico San Carlos. Madrid: Inés Armenteros Yeguas, Javier Azaña Gómez, Julia Barrado Cuchillo, Irene Burruezo López, Noemí Cabello Clotet, Alberto E. Calvo Elías, Elpidio Calvo Manuel, Carmen María Cano de Luque, Cynthia Chocron Benbunan, Laura Dans Vilán, Ester Emilia Dubon Peralta, Vicente Estrada Pérez, Santiago Fernandez-Castelao, Marcos Oliver Fragiel Saavedra, José Luis García Klepzig, María del Rosario Iguarán Bermúdez, Esther Jaén Ferrer, Rubén Ángel Martín Sánchez, Manuel Méndez Bailón, María José Núñez Orantos, Carolina Olmos Mata, Eva Orviz García, David Oteo Mata, Cristina Outon González, Juncal Pérez-Somarriba, Pablo Pérez Mateos, María Esther Ramos Muñoz, Xabier Rivas Regaira, Iñigo Sagastagoitia Fornie, Alejandro Salinas Botrán, Miguel Suárez Robles, Maddalena Elena Urbano, Miguel Villar Martínez.
H. Infanta Sofía. S. S. de los Reyes. Madrid: Rafael del Castillo Cantero, Rebeca Fuerte Martínez, Arturo Muñoz Blanco, José Francisco Pascual Pareja, Isabel Perales Fraile, Isabel Rábago Lorite, Llanos Soler Rangel, Inés Suárez García, José Luis Valle López.
H. U. Dr. Peset. Valencia: Juan Alberto Aguilera Ayllón, Arturo Artero, María del Mar Carmona Martín, María José Fabiá Valls, María de Mar Fernández Garcés, Ana Belén Gómez Belda, Ian López Cruz, Manuel Madrazo López, Elisabet Mateo Sanchis, Jaume Micó Gandía, Laura Piles Roger, Adela María Pina Belmonte, Alba Viana García.
H. Clínico de Santiago. Santiago de Compostela: María del Carmen Beceiro Abad, María Aurora Freire Romero, Sonia Molinos Castro, Emilio Manuel Páez Guillán, María Pazo Núñez, Paula María Pesqueira Fontán.
H. Nuestra Señora del Prado. Talavera de la Reina. Toledo: Sonia Casallo Blanco, Jeffrey Oskar Magallanes Gamboa.
H. U. Ramón y Cajal. Madrid: Luis Fernando Abrego Vaca, Ana Andréu Arnanz, Octavio Arce García, Marta Bajo González, Pablo Borque Sanz, Alberto Cozar Llisto, Sonia de Pedro Baena, Beatriz Del Hoyo Cuenda, María Alejandra Gamboa Osorio, Isabel García Sánchez, Andrés González García, Oscar Alberto López Cisneros, Miguel Martínez Lacalzada, Borja Merino Ortiz, Jimena Rey-García, Elisa Riera González, Cristina Sánchez Díaz, Grisell Starita Fajardo, Cecilia Suárez Carantoña, Adrián Viteri Noel, Svetlana Zhilina Zhilina.
H. Royo Villanova. Zaragoza: Nicolás Alcalá Rivera, Anxela Crestelo Vieitez, Esther del Corral, Jesús Díez Manglano, Isabel Fiteni Mera, María del Mar García Andreu, Martin Gerico Aseguinolaza, Claudia Josa Laorden, Raúl Martínez Murgui, Marta Teresa Matía Sanz.
H. U. Infanta Cristina. Parla. Madrid: Juan Miguel Antón Santos, Ana Belén Barbero Barrera, Coralia Bueno Muiño, Ruth Calderón Hernáiz, Irene Casado López, José Manuel Casas Rojo, Andrés Cortés Troncoso, Mayte de Guzmán García-Monge, Francesco Deodati, Gonzalo García Casasola Sánchez, Elena García Guijarro, Davide Luordo, María Mateos González, José A Melero Bermejo, Lorea Roteta García, Elena Sierra Gonzalo, Javier Villanueva Martínez.
H. de Cabueñes. Gijón. Asturias: Ana María Álvarez Suárez, Carlos Delgado Vergés, Rosa Fernández-Madera Martínez, Eva Fonseca Aizpuru, Alejandro Gómez Carrasco, Cristina Helguera Amezua, Juan Francisco López Caleya, María del Mar Martínez López, Aleida Martínez Zapico, Carmen Olabuenaga Iscar, María Luisa Taboada Martínez, Lara María Tamargo Chamorro.
H. de Urduliz Alfredo Espinosa. Urdúliz. Vizcaya: María Aparicio López, Asier Aranguren Arostegui, Paula Arriola Martínez, Gorka Arroita González, Mª Soledad Azcona Losada, Miriam García Gómez, Eduardo García López, Amalur Iza Jiménez, Alazne Lartategi Iraurgi, Esther Martínez Becerro, Itziar Oriñuela González, Isabel María Portales Fernández, Pablo Ramírez Sánchez, Beatriz Ruiz Estévez, Cristian Vidal Núñez.
H. Regional Universitario de Málaga. Málaga: Mª Mar Ayala Gutiérrez, Rosa Bernal López, José Bueno Fonseca, Verónica Andrea Buonaiuto, Luis Francisco Caballero Martínez, Lidia Cobos Palacios, Clara Costo Muriel, Francis de Windt, Ana Teresa Fernández-Truchaud Christophel, Paula García Ocaña, Ricardo Gómez Huelgas, Javier Gorospe García, María Dolores López Carmona, Pablo López Quirantes, Almudena López Sampalo, Elizabeth Lorenzo Hernández, Juan José Mancebo Sevilla, Jesica Martin Carmona, Luis Miguel Pérez-Belmonte, Araceli Pineda Cantero, Michele Ricci, Jaime Sanz Cánovas.
H. Santa Marina. Bilbao: María Areses Manrique, Ainara Coduras Erdozain, Ane Elbire Labirua-Iturburu Ruiz.
H. Moisès Broggi. Sant Joan Despí. Barcelona: Judit Aranda Lobo, José Loureiro Amigo, Isabel Oriol Bermúdez, Melani Pestaña Fernández, Nicolas Rhyman, Nuria Vázquez Piqueras.
H. HLA Moncloa. Madrid: Guillermo Estrada, Teresa García Delange, Isabel Jiménez Martínez, Carmen Martínez Cilleros, Nuria Parra Arribas.
H. del Henares. Coslada. Madrid: Jesús Ballano Rodríguez-Solís, Luis Cabeza Osorio, María del Pilar Fidalgo Montero, Mª Isabel Fuentes Soriano, Erika Esperanza Lozano Rincón, Ana Martín Hermida, Jesús Martínez Carrilero, José Ángel Pestaña Santiago, Manuel Sánchez Robledo, Patricia Sanz Rojas, Nahum Jacobo Torres Yebes, Vanessa Vento.
H. U. Torrevieja. Torrevieja. Alicante: Julio César Blázquez Encinar, Joaquín Fernández-Cuervo.
H. U. La Fe. Valencia: Dafne Cabañero, María Calabuig Ballester, Pascual Císcar Fernández, Ricardo Gil Sánchez, Marta Jiménez Escrig, Cristina Marín Amela, Laura Parra Gómez, Carlos Puig Navarro, José Antonio Todolí Parra.
H. San Pedro. Logroño: Diana Alegre González, Irene Ariño Pérez de Zabalza, Sergio Arnedo Hernández, Jorge Collado Sáenz, Beatriz Dendariena, Marta Gómez del Mazo, Iratxe Martínez de Narvajas Urra, Sara Martínez Hernández, Estela Menéndez Fernández, José Luis Peña Somovilla, Elisa Rabadán Pejenaute.
H. U. Ntra. Sra. Candelaria. Santa Cruz de Tenerife: Lucy Abella, Andrea Afonso Díaz, Selena Gala Aguilera García, Marta Bethencourt Feria, Eduardo Mauricio Calderón Ledezma, Sara Castaño Pírez, Guillermo Castro Gainett, José Manuel del Arco Delgado, Joaquín Delgado Casamayor, Diego García Silvera, Alba Gómez Hidalgo, Marcelino Hayek Peraza, Carolina Hernández Carballo, Rubén Hernández Luis, Francisco Javier Herrera Herrera, María del Mar López Gámez, Julia Marfil Daza, María José Monedero Prieto, María Blanca Monereo Muñoz, María de la Luz Padilla Salazar, Daniel Rodríguez Díaz, Alicia Tejera, Laura Torres Hernández.
H. U. San Juan de Alicante. San Juan de Alicante: David Balaz, David Bonet Tur, Carles García Cervera, David Francisco García Núñez, Vicente Giner Galvañ, Angie Gómez Uranga, Javier Guzmán Martínez, Isidro Hernández Isasi, Lourdes Lajara Villar, Juan Manuel Núñez Cruz, Sergio Palacios Fernández, Juan Jorge Peris García, Andrea Riaño Pérez, José Miguel Seguí Ripoll, Philip Wikman-Jorgensen.
H. U. San Agustín. Avilés: Andrea Álvarez García, Víctor Arenas García, Alba Barragán Mateos, Demelsa Blanco Suárez, María Caño Rubia, Jaime Casal Álvarez, David Castrodá Copa, José Ferreiro Celeiro, Natalia García Arenas, Raquel García Noriega, Joaquín Llorente García, Irene Maderuelo Riesco, Paula Martínez García, María José Menéndez Calderón, Diego Eduardo Olivo Aguilar, Marta Nataya Solís Marquínez, Luis Trapiella Martínez, Andrés Astur Treceño García, Juan Valdés Bécares.
H. de Mataró. Mataró: Raquel Aranega González, Ramon Boixeda, Carlos Lopera Mármol, Marta Parra Navarro, Ainhoa Rex Guzmán, Aleix Serrallonga Fustier.
H. U. Son Llàtzer. Palma de Mallorca: Andrés de la Peña Fernández, Almudena Hernández Milián.
H. Virgen de la Salud. Toledo: Ana María Alguacil Muñoz, Marta Blanco Fernández, Verónica Cano, Ricardo Crespo Moreno, Fernando Cuadra García-Tenorio, Blanca Díaz-Tendero Nájera, Raquel Estévez González, María Paz García Butenegro, Alberto Gato Díez, Verónica Gómez Caverzaschi, Piedad María Gómez Pedraza, Julio González Moraleja, Raúl Hidalgo Carvajal, Patricia Jiménez Aranda, Raquel Labra González, Áxel Legua Caparachini, Pilar López Castañeyra, Agustín Lozano Ancín, José Domingo Martín García, Cristina Morata Romero, María Jesús Moya Saiz, Helena Moza Moríñigo, Gemma Muñiz Nicolás, Enriqueta Muñoz Platón, Filomena Oliveri, Elena Ortiz Ortiz, Raúl Perea Rafael, Pilar Redondo Galán, María Antonia Sepúlveda Berrocal, Vicente Serrano Romero de Ávila, Pilar Toledano Sierra, Yamilex Urbano Aranda, Jesús Vázquez Clemente, Carmen Yera Bergua.
H. Juan Ramón Jiménez. Huelva: Francisco Javier Bejarano Luque, Francisco Javier Carrasco-Sánchez, Mercedes de Sousa Baena, Jaime Díaz Leal, Aurora Espinar Rubio, María Franco Huertas, Juan Antonio García Bravo, Andrés González Macías, Encarnación Gutiérrez Jiménez, Alicia Hidalgo Jiménez, Constantino Lozano Quintero, Carmen Mancilla Reguera, Francisco Javier Martínez Marcos, Francisco Muñoz Beamud, María Pérez Aguilera, Alicia Pérez Jiménez, Virginia Rodríguez Castaño, Álvaro Sánchez de Alcázar del Río, Leire Toscano Ruiz.
H. U. Reina Sofía. Córdoba: Antonio Pablo Arenas de Larriva, Pilar Calero Espinal, Javier Delgado Lista, María Jesús Gómez Vázquez, José Jiménez Torres, Laura Martín Piedra, Javier Pascual Vinagre, María Elena Revelles Vílchez, Juan Luis Romero Cabrera, José David Torres Peña.
H. Infanta Margarita. Cabra: María Esther Guisado Espartero, Lorena Montero Rivas, María de la Sierra Navas Alcántara, Raimundo Tirado-Miranda.
H. U. Virgen de las Nieves. Granada: Pablo Conde Baena, Joaquín Escobar Sevilla, Laura Gallo Padilla, Patricia Gómez Ronquillo, Pablo González Bustos, María Navío Botías, Jessica Ramírez Taboada, Mar Rivero Rodríguez.
H. Costa del Sol. Marbella: Victoria Augustín Bandera, María Dolores Martín Escalante.
H. San Juan de la Cruz. Úbeda: Marcos Guzmán García, Francisco Javier Vicente Hernández.
Complejo Asistencial Universitario de León. León: Rosario María García Die, Manuel Martin Regidor, Ángel Luis Martínez González, Alberto Muela Molinero, Raquel Rodríguez Díez, Beatriz Vicente Montes.
H. Clínic Barcelona. Barcelona: Júlia Calvo Jiménez, Aina Capdevila Reniu, Irene Carbonell De Boulle, Emmanuel Coloma Bazán, Joaquim Fernández Solà, Cristina Gabara Xancó, Joan Ribot Grabalosa, Olga Rodríguez Núñez.
C. H. U. de Ferrol. Ferrol: Hortensia Álvarez Díaz, Tamara Dalama López, Estefanía Martul Pego, Carmen Mella Pérez, Ana Pazos Ferro, Sabela Sánchez Trigo, Dolores Suarez Sambade, María Trigás Ferrín, María del Carmen Vázquez Friol, Laura Vilariño Maneiro.
H. Marina Baixa. Villajoyosa: Javier Ena, Santiago Pérez-Martín.
H. del Tajo. Aranjuez: Ruth González Ferrer, Raquel Monsalvo Arroyo.
H. Insular de Gran Canaria. Las Palmas de Gran Canaria: Marina Aroza Espinar, Jorge Orihuela Martín, Carlos Jorge Ripper, Selena Santana Jiménez.
H. U. Marqués de Valdecilla. Santander: Marta Fernández-Ayala Novo, José Javier Napal Lecumberri, Nuria Puente Ruiz, José Riancho, Isabel Sampedro García.
H. Torrecárdenas. Almería: Luis Felipe Díez García, Iris El Attar Acedo, Bárbara Hernández Sierra, Carmen Mar Sánchez Cano.
H. U. Severo Ochoa. Leganés: Yolanda Casillas Viera, Lucía Cayuela Rodríguez, Carmen de Juan Álvarez, Gema Flox Benítez, Laura García Escudero, Juan Martin Torres, Patricia Moreira Escriche, Susana Plaza Canteli, M. Carmen Romero Pérez.
H. Valle del Nalón. Riaño. Langreo: Sara Fuente Cosío, César Manuel Gallo Álvaro, Julia Lobo García, Antía Pérez Piñeiro.
H. U. del Vinalopó. Elche: Francisco Amorós Martínez, Erika Ascuña Vásquez, José Carlos Escribano Stablé, Adriana Hernández Belmonte, Ana Maestre Peiró, Raquel Martínez Goñi, M. Carmen Pacheco Castellanos, Bernardino Soldán Belda, David Vicente Navarro.
H. Alto Guadalquivir. Andújar: Begoña Cortés Rodríguez.
H. Francesc de Borja. Gandía: Alba Camarena Molina, Simona Cioaia, Anna Ferrer Santolaria, José María Frutos Pérez, Eva Gil Tomás, Leyre Jorquer Vidal, Marina Llopis Sanchís, Mari Ángeles Martínez Pascual, Álvaro Navarro Batet, Mari Amparo Perea Ribis, Ricardo Peris Sánchez, José Manuel Querol Ribelles, Silvia Rodríguez Mercadal, Ana Ventura Esteve.
H. G. U. de Castellón. Castellón de la Plana: Jorge Andrés Soler, Marián Bennasar Remolar, Alejandro Cardenal Álvarez, Daniela Díaz Carlotti, María José Esteve Gimeno, Sergio Fabra Juana, Paula García López, María Teresa Guinot Soler, Daniela Palomo de la Sota, Guillem Pascual Castellanos, Ignacio Pérez Catalán, Celia Roig Martí, Paula Rubert Monzó, Javier Ruiz Padilla, Nuria Tornador Gaya, Jorge Usó Blasco.
H. Santa Bárbara. Soria: Marta León Téllez.
C. A. U. de Salamanca. Salamanca: Gloria María Alonso Claudio, Víctor Barreales Rodríguez, Cristina Carbonell Muñoz, Adela Carpio Pérez, María Victoria Coral Orbes, Daniel Encinas Sánchez, Sandra Inés Revuelta, Miguel Marcos Martín, José Ignacio Martín González, José Ángel Martín Oterino, Leticia Moralejo Alonso, Sonia Peña Balbuena, María Luisa Pérez García, Ana Ramon Prados, Beatriz Rodríguez-Alonso, Ángela Romero Alegría, María Sánchez Ledesma, Rosa Juana Tejera Pérez.
H. U. de Canarias. Santa Cruz de Tenerife: Julio Cesar Alvisa Negrín, José Fernando Armas González, Lourdes González Navarrete, Iballa Jiménez, María Candelaria Martín González, Miguel Nicolas Navarrete Lorite, Paula Ortega Toledo, Onán Pérez Hernández, Alina Pérez Ramírez.
C. H. U. de Badajoz. Badajoz: Rafael Aragón Lara, Inmaculada Cimadevilla Fernández, Juan Carlos Cira García, Gema María García García, Julia González Granados, Beatriz Guerrero Sánchez, Francisco Javier Monreal Periáñez, María Josefa Pascual Pérez.
H. U. del Sureste. Arganda del Rey: Jon Cabrejas Ugartondo, Ana Belén Mancebo Plaza, Arturo Noguerado Asensio, Bethania Pérez Alves, Natalia Vicente López.
H. U. Quironsalud Madrid. Pozuelo de Alarcón. Madrid: Pablo Guisado Vasco, Ana Roda Santacruz, Ana Valverde Muñoz.
H. de Poniente. Almería: Juan Antonio Montes Romero, Encarna Sánchez Martín, José Luis Serrano Carrillo de Albornoz, Manuel Jesús Soriano Pérez.
H. U. Lucus Augusti. Lugo: Raquel Gómez Méndez, Ana Rodríguez Álvarez.
H. San Pedro de Alcántara. Cáceres: Ángela Agea García, Javier Galán González, Luis Gámez Salazar, Eva García Sardón, Antonio González Nieto, Itziar Montero Días, Selene Núñez Gaspar, Álvaro Santaella Gómez.
H. de Pozoblanco. Pozoblanco: José Nicolás Alcalá Pedrajas, Antonia Márquez García, Inés Vargas.
H. Virgen de los Lirios. Alcoy. Alicante: Mª José Esteban Giner.
H. Doctor José Molina Orosa. Arrecife. Lanzarote: Virginia Herrero García, Berta Román Bernal.
H. Nuestra Señora de Sonsoles. Ávila: Alaaeldeen Abdelhady Kishta.
H. G. U. de Elda. Elda: Carmen Cortés Saavedra, Jennifer Fernández Gómez, Borja González López, María Soledad Hernández Garrido, Ana Isabel López Amorós, María de los Reyes Pascual Pérez, Andrea Torregrosa García.
H. U. Puerta del Mar. Cádiz: José Antonio Girón González, Susana Fabiola Pascual Pérez, Cristina Rodríguez Fernández-Viagas, María José Soto Cárdenas.
H. Parc Tauli. Sabadell: Francisco Epelde, Isabel Torrente.
H. de Montilla. Montilla: Ana Cristina Delgado Zamorano, Beatriz Gómez Marín, Adrián Montaño Martínez, José Luis Zambrana García.
H. Infanta Elena. Huelva: María Gloria Rojano Rivero.
H. de la Axarquía. Vélez- Málaga: Antonio López Ruiz.
H. Virgen del Mar. Madrid: Thamar Capel Astrua, Paola Tatiana García Giraldo, María Jesús González Juárez, Victoria Márquez Fernández, Ada Viviana Romero Echevarry.
Hospital do Salnes. Vilagarcía de Arousa: Vanesa Alende Castro, Ana María Baz Lomba, Ruth Brea Aparicio, Marta Fernández Morales, Jesús Manuel Fernández Villar, María Teresa López Monteagudo, Cristina Pérez García, Lorena María Rodríguez Ferreira, María Begoña Valle Feijoo.
H. La Fuenfría. Cercedilla. Madrid: Daniel Arregui Gallego, Jorge Blanco Briones, Gonzalo M Muzquiz Rueda, Isabel Rodríguez Fraile, Javier Rodríguez Hernández, María Ángeles Ruiz Rodríguez, Mikaela Zubillaga Gómez.
References
- 1.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shafi A., Shaikh S., Shirke M., Iddawela S., Harky A. Cardiac manifestations in COVID-19 patients. A systematic review. J Card Surg. 2020;35:1988–2008. doi: 10.1111/jocs.14808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ministerio de Sanidad. Situación de COVID-19 en España. Centro de Coordinación de Alertas y Emergencias Sanitarias. Enfermedad por el coronavirus (COVID-19). [Accessed 27 Jan 2021]. Actualización_299_COVID-19.pdf (mscbs.gob.es).
- 5.Sayago-Silva I., García-López F., Segovia-Cubero J. Epidemiología de la insuficiencia cardíaca en España en los últimos 20 años. Rev Esp Cardiol. 2013;66:649–656. doi: 10.1016/j.rec.2013.03.012. [DOI] [PubMed] [Google Scholar]
- 6.Eurostat-Data Explorer Population: structure indicators. 2020. https://ec.europa.eu/eurostat/en/web/products-eurostat-news/-/edn-20170930-1 Accessed 30 June 2020.
- 7.Álvarez-García J., Lee S., Gupta A., Cagliostro M., Joshi A.A., Rivas-Lasarte M., et al. Prognostic impact of prior heart failure in patients hospitalized with COVID-19. J Am Coll Cardiol. 2020;76:2334–2348. doi: 10.1016/j.jacc.2020.09.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rey J.R., Caro-Codón J., Rosillo S.O., Iniesta A.M., Castrejón-Castrejón S., Marco-Clement I., et al. Heart failure in COVID-19 patients: prevalence, incidence and prognostic implications. Eur J Heart Fail. 2020;22:2205–2215. doi: 10.1002/ejhf.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Casas Rojo J.M., Antón Santos J.M., Millán Núñez-Cortés J., Lumbreras-Bermejo C., Ramos-Rincón J.M., Roy-Vallejo E., et al. Clinical characteristics of patients hospitalized with COVID-19 in Spain: results from the SEMI-COVID-19 registry. Rev Clin Esp. 2020;220:480–494. doi: 10.1016/j.rce.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rius C., Pérez G., Martínez J.M., Bares M., Schiaffino A., Gispert R., et al. An adaptation of Chalrson comorbidity index predicted subsequent mortality in a health survey. J Clin Epidemiol. 2004;57:403–408. doi: 10.1016/j.jclinepi.2003.09.016. [DOI] [PubMed] [Google Scholar]
- 11.Mueller A.L., McNamara M.S., Sinclair D.A. Why does COVID-19 disproportionately affect older people? Aging (Albany NY). 2020;12:9959–9981. doi: 10.18632/aging.103344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levey A.S., Stevens L.A., Schmid C.H., Zhang Y.L., Castro A.F., Feldman H.I., et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pugh R.N., Murray-Lyon I.M., Dawson J.L., Pietroni M.C., Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646. doi: 10.1002/bjs.1800600817. [DOI] [PubMed] [Google Scholar]
- 14.Laribi S., Aouba A., Nikolaou M., Lassus J., Cohen-Solal A., Plaisance P., et al. Trends in death attributed to heart failure over the past two decades in Europe. Eur J Heart Fail. 2012;14:234–239. doi: 10.1093/eurjhf/hfr182. [DOI] [PubMed] [Google Scholar]
- 15.Ponikowski P., Voors A., Anker S., Bueno H., Cleland J.G.F., Coats A.J.S., et al. Guía ESC 2016 sobre el diagnóstico y tratamiento de la insuficiencia cardíaca aguda y crónica. Rev Esp Cardiol. 2016;69 [Google Scholar]
- 16.Ferreira-González I. Epidemiología de la enfermedad coronaria. Rev Esp Cardiol. 2014;67:139–144. [Google Scholar]
- 17.Bromage D.I., Cannatà A., Rind I.A., Gregorio C., Piper S., Shah A.M., et al. The impact of COVID-19 on heart failure hospitalization and management: report from a Heart Failure Unit in London during the peak of the pandemic. Eur J Heart Fail. 2020;22:978–984. doi: 10.1002/ejhf.1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hermida Ameijeiras A., Pazo Núñez M., De la Fuente Cid R., Lado Lado F.L., Hernández Hernández L., Rodríguez López I. Factores epidemiológicos asociados a la hospitalización por descompensación de la insuficiencia cardíaca. An Med Interna. 2008;25:256–261. doi: 10.4321/s0212-71992008000600002. [DOI] [PubMed] [Google Scholar]
- 19.Formiga F., Chivite D., Manito N., Casas S., Riera A., Pujol R. Predictors of in-hospital mortality present at admission among patients hospitalised because of decompensated heart failure. Cardiology. 2007;108:73–78. doi: 10.1159/000095885. [DOI] [PubMed] [Google Scholar]
- 20.Grigorian Shamagian L., Gonzalez-Juanatey J.R., Varela Roman A., García Acuña J.M., Virgós Lamela A. The death rate among hospitalized heart failure patients with normal and depressed left ventricular ejection fraction in the year following discharge: evolution over a 10-year period. Eur Heart J. 2005;26:2251–2258. doi: 10.1093/eurheartj/ehi383. [DOI] [PubMed] [Google Scholar]
- 21.Pons F., Lupón J., Urrutia A., González B., Crespo E., Díez C., et al. Mortalidad y causas de muerte en pacientes con insuficiencia cardíaca: experiencia de una unidad especializada multidisciplinaria. Rev Esp Cardiol. 2010;63:303–314. [Google Scholar]
- 22.Ramos-Rincón J.M., Buonaiuto V., Ricci M., Martín-Carmona J., Paredes-Ruiz D., Calderón-Moreno M., et al. Clinical characteristics and risk factors for mortality in very old patients hospitalized with COVID-19 in Spain. J Gerontol A Biol Sci Med Sci. 2020;76:e28–37. doi: 10.1093/gerona/glaa243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mueller A.L., McNamara M.S., Sinclair D.A. Why does COVID-19 disproportionately affect older people? Aging (Albany NY). 2020;12:9959–9981. doi: 10.18632/aging.103344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rodilla E., Saura A., Jiménez I., Mendizábal A., Pineda-Cantero A., Lorenzo-Hernández E., et al. Association of hypertension with all-cause mortality among hospitalized patients with COVID-19. J Clin Med. 2020;9:3136. doi: 10.3390/jcm9103136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Promislow D.E.L. A geroscience perspective on COVID-19 mortality. J Gerontol A Biol Sci Med Sci. 2020;75:e30–e33. doi: 10.1093/gerona/glaa094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kashani K.B. Hypoxia in COVID-19: sign of severity or cause for poor outcomes. Mayo Clin Proc. 2020;95:1094–1096. doi: 10.1016/j.mayocp.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xie J., Covassin N., Fan Z., Singh P., Gao W., Li G., et al. Association between hypoxemia and mortality in patients with COVID-19. Mayo Clin Proc. 2020;95:1138–1147. doi: 10.1016/j.mayocp.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yan Q., Zuo P., Cheng L., Li Y., Song K., Chen Y., et al. Acute kidney injury is associated with in-hospital mortality in older patients with COVID-19. J Gerontol A Biol Sci Med Sci. 2021;76:456–462. doi: 10.1093/gerona/glaa181. [DOI] [PMC free article] [PubMed] [Google Scholar]